Why is my nipple cracking
Cracked nipples: Causes, treatment, and remedies
Cracked nipples most often result from chafing during sports and due to breastfeeding.
Cracked nipples are characterized by red, irritated, and scabbed skin on or around the nipple. Using gentle creams and avoiding harsh soaps, chemicals, and tight clothing can help treat and prevent nipple cracking.
An estimated 38% of people who experience problems with breastfeeding or chestfeeding have sore or cracked nipples. This can make future breastfeeding sessions uncomfortable.
This article discusses why cracked nipples occur and how to treat them. It takes a close look at how to manage this symptom when breastfeeding, including pain relief and tips for preventing further damage.
Share on PinterestA person may experience cracked nipples when they are breastfeeding.Cracked nipples are most often due to nipple trauma. It can affect both men and women as a result of chafing against clothing or tissue damage from cuts or blows. It may be more likely if the nipples protrude more.
During breastfeeding, causes of cracked nipples include:
- problems with the baby’s latch
- not finding the optimal position
- not finding the ideal technique
- using a breast pump, particularly if the pump flange is too small
Cracked nipples are most likely to occur in the first month postpartum, according to an article in the journal BMC Pregnancy and Childbirth.
As a baby is learning to nurse, they may take additional time and effort to latch onto the breast. The friction can irritate and sensitize the nipple. The nipple can also become dry, leading to cracked skin and occasional bleeding.
Using a bottle to feed a baby before trying breastfeeding may also increase the chance of cracked nipples. This is because a baby will typically use a different sucking technique when using a bottle compared with a breast. If they are more used to a bottle, they may be more likely to cause nipple trauma.
If a baby needs supplemental milk in the early days or weeks of life, lactation consultants tend to recommend spoon, cup, or syringe feeding, rather than using a bottle. Using a spoon, cup, or syringe is less likely to have an adverse effect on the baby’s latch and long-term breastfeeding success.
To treat cracked nipples, a person can:
- Apply emollient creams, such as lanolin-based creams or coconut oil, to the nipples after breastfeeding. This can soften the skin and reduce cracking. Some people even apply breast milk to the nipples and allow it to dry, which can prevent cracking and has antibacterial properties.
- Apply a corticosteroid cream immediately after breastfeeding for no longer than 2 weeks at a time. Applying steroids for a longer time period could cause thinning of the nipple’s skin. Only try this if a healthcare professional has recommended it.
- Avoid wearing bras that are too tight, as this can increase friction on the nipples.
- Avoid using harsh soaps, deodorants, body powders, and other substances that could dry out the nipples.

Allowing time to heal and finding improved ways for a baby to latch onto the breast should also help cracked nipples heal.
A lactation consultant can help people struggling with breastfeeding to identify ways to improve the experience. This can enhance comfort and reduce nipple trauma that leads to cracked nipples.
Examples include evaluating:
- how the baby latches
- infant positioning
- parental positioning
- the nipple’s appearance after feeding
A lactation consultant can make recommendations after observing a feeding. They may suggest trying the following.
- Sit in a chair or in bed, leaning slightly back in a position that feels comfortable. Use as many pillows as needed to feel supported.
- Hold the baby “belly to belly,” so that the front of their body is against the front of the parent’s. The baby should not have to turn their head to the side to reach the breast.
- Before latching the baby, position them so that their nose is aligned with the nipple.

- Gently rub the nipple back and forth over the baby’s mouth. This should encourage them to open their mouth. Squeezing a little bit of milk or colostrum out of the breast can also help get the baby’s attention.
- Once the baby’s mouth is open, they should take the full areola into their mouth, not just the tip of the nipple. Generally, their chin will touch the breast first.
- If the baby’s latch starts to hurt, use a finger on the corner of their mouth, moving around the lips until their mouth breaks the seal.
If this approach does not work, try different hold options. Some examples include the “football” hold and the cradle position.
The “football” hold positions the baby’s body on the same side they are feeding from. Breastfeeding consultants often recommend this hold for people who had a cesarean birth, as the baby’s body will not cross the surgical incision.
The cradle position involves holding the baby in a cross-body position. A breastfeeding pillow, or a pillow underneath the baby, brings them up to breast height, and the parent will cradle the baby until the baby is securely against the chest and stomach. The baby should not have to turn their head to access the breast.
The baby should not have to turn their head to access the breast.
Nipple discomfort and tenderness is common when someone first starts breastfeeding or chestfeeding. However, taking the following preventive steps can help prevent cracked nipples:
- Ensure that the baby is adequately latching onto the breast. The nipple should be fully inside the baby’s mouth, with most of the areola in the mouth, too. A person should talk to a lactation consultant as soon as possible if they are not sure that the baby is latching well.
- Hand-express a small amount of breast milk before feeding the baby, so that the breasts are not engorged (overfull and hard). Breast engorgement can make it more difficult for the baby to latch well.
- Wash the breasts with warm water only and avoid using hard soaps to prevent dryness.
- Apply nipple ointment or allow breast milk to dry on the breasts.
- Consider wearing breast pads made from natural materials, as these can reduce friction on the breasts.

- Always allow the baby to come off the breast naturally.
Pain associated with breastfeeding is a common cause of stopping breastfeeding early, according to the Academy of Breastfeeding Medicine. Even if a parent has cracked nipples, they can usually continue to breastfeed while they heal.
To do so:
- Continue to vary nursing positions. This can reduce the stress on the nipples and help a person find a position that works best for them and their baby.
- Start by nursing on the side that is less sore until the breast milk letdown occurs. Then, switch to the other side, where the baby will not need to suck on the breast as hard because the milk will come out more easily.
- Apply breast milk or lanolin to the nipples after breastfeeding and allow them to air dry.
Sometimes, a lactation consultant might recommend using a silicone nipple shield for a while, to allow the nipples to heal without interrupting nursing.
If a person continues to experience cracked nipples, they can speak to their midwife or obstetrician, who may recommend seeking further lactation consulting or prescribe creams to help the nipples heal.
Cracked nipples can be a common side effect when establishing breastfeeding.
A person does not usually need to stop breastfeeding when they have cracked nipples, but this symptom might indicate that they need to improve the baby’s latch to reduce pain and enhance overall breastfeeding success.
If a person is concerned about cracked nipples or worried about infection, they can see their lactation consultant, midwife, or doctor for advice.
Cracked Nipples Symptoms, Causes & Common Questions
Understand your cracked nipples symptoms, including 2 causes & common questions.
8 most common causes
Breast Pain
Breast Abscess
Contact Dermatitis
Illustration of a health care worker swabbing an individual.Mastitis (breast infection)
Illustration of a doctor beside a bedridden patient.Breastfeeding Complications
Illustration of a doctor beside a bedridden patient.Physiologic breast discharge
Illustration of a person thinking with cross bandaids.
Plugged breast duct
Illustration of a doctor beside a bedridden patient.High prolactin hormone level
Cracked nipples quiz
Take a quiz to find out what's causing your cracked nipples.
Take cracked nipples quiz
Cracked nipples symptoms
Anyone, either male or female, can experience cracked nipples. The areola, the area of skin surrounding the nipple, and the nipple, are more delicate and prone to injury than most of the skin on the rest of the body. Cracked nipples can be caused by breastfeeding, chafing, or underlying skin conditions.
Common characteristics of cracked nipples
Cracked nipples may be described by:
- Splitting skin that oozes: The tissue of the areolas may split, bleed, or ooze.
- Pain: The area around the nipple may be tender, if not outright painful.
- Cracks might peel or become crusted over
Cracked nipples causes
The following details may help you better understand your symptoms. See a lactation specialist if you continue to have trouble breastfeeding, or a physician if your cracked nipples persist for other reasons.
See a lactation specialist if you continue to have trouble breastfeeding, or a physician if your cracked nipples persist for other reasons.
Breastfeeding
Breastfeeding is not supposed to hurt. While it may not be comfortable, there is something wrong if breastfeeding is considered painful. Pain commonly occurs with either improper positioning of the baby on the breast or a poor latch. It may be difficult to properly position infants with torticollis, a stiff, painful neck, sometimes the result of difficult labor or birth. Babies with ankyloglossia (tongue-tie) may not be able to latch properly.
Friction-related causes
Friction can cause nipples to become chafed and cracked. Runners refer to this as "jogger's nipple," surfers call it "surfer's nipple," and divers call it "wetsuit rub." Any athletic (or sexual) activity which involves constant friction on the nipples can cause them to crack.
Other skin conditions
Dermatitis, eczema, psoriasis, and allergic reactions are all conditions that can cause skin rashes. If the rash is over the nipples, the skin of can become dry, scaly, and split. These cracks may bleed or become infected and start oozing.
If the rash is over the nipples, the skin of can become dry, scaly, and split. These cracks may bleed or become infected and start oozing.
2 cracked nipples conditions
The list below shows results from the use of our quiz by Buoy users who experienced cracked nipples. This list does not constitute medical advice and may not accurately represent what you have.
Plugged breast duct
If you're making milk faster than it's getting expressed, it can get backed up in the duct. When this happens, the tissue around the duct may become swollen and inflamed and press on the duct, causing a blockage.
You can safely treat this condition on your own by continuing nursing and draining your breast as much as possible after each feeding. If you develops a fever or significant discomfort, contact your physician.
Physiologic breast discharge
Physiologic breast discharge is any fluid that comes out of the nipple area in your breast.
You should visit your primary care physician to evaluate the discharge and discuss treatment options.
Non-specific breast pain
Nonspecific breast pain, also called mastalgia or mastodynia, refers to tenderness or pain in the breast with no obvious cause. It almost always proves to have a benign (non-cancerous) cause.
Breast pain is most common in women aged 35 to 50 and still experiencing menstruation. Fibrocystic changes are common in this age group, where tiny, fluid-filled sacs form within breast tissue and might be felt as small, tender, but non-cancerous lumps.
Birth control pills, hormone replacement therapy, caffeine, and soy can cause breast tenderness in women of any age. A breast infection can cause painful lumps.
A medical provider should be seen, in order to rule out any serious condition and get treatment for the discomfort.
Diagnosis is made through patient history; physical examination; mammogram or breast ultrasound; and sometimes biopsy.
A breast infection will be treated with antibiotics. Large, painful cysts may have the fluid drained or be surgically removed. Lifestyle improvements regarding diet and exercise are often helpful, as well as adjustments to birth control pills or hormone therapy.
Lifestyle improvements regarding diet and exercise are often helpful, as well as adjustments to birth control pills or hormone therapy.
Cracked nipples quiz
Take a quiz to find out what's causing your cracked nipples.
Take cracked nipples quiz
High prolactin hormone level
Hyperprolactinemia means the pituitary gland secretes too much prolactin, the hormone responsible for producing milk in a new mother. The condition can appear in both women and men.
It can be caused by pregnancy; by an ovulatory disorder; by some psychiatric medications; or by a prolactin-secreting tumor of the pituitary (prolactinoma.)
Women with other reproductive disorders, such as polycystic ovary syndrome (PCOS,) are most susceptible. Hyperprolactinemia is also seen in those with hypothyroidism and chronic renal failure. Many patients on hemodialysis have elevated prolactin levels.
Symptoms in both women and men include reduced libido (sex drive) and infertility. Men may show breast enlargement and women may develop breast milk.
Men may show breast enlargement and women may develop breast milk.
If not treated, hyperprolactinemia can result in loss of bone density in both women and men.
Diagnosis is made through blood testing to measure hormone levels, and sometimes MRI of the pituitary gland underneath the brain.
Treatment may include "watchful waiting," or a period spent observing the symptoms to see if they change; drug therapy; or surgery.
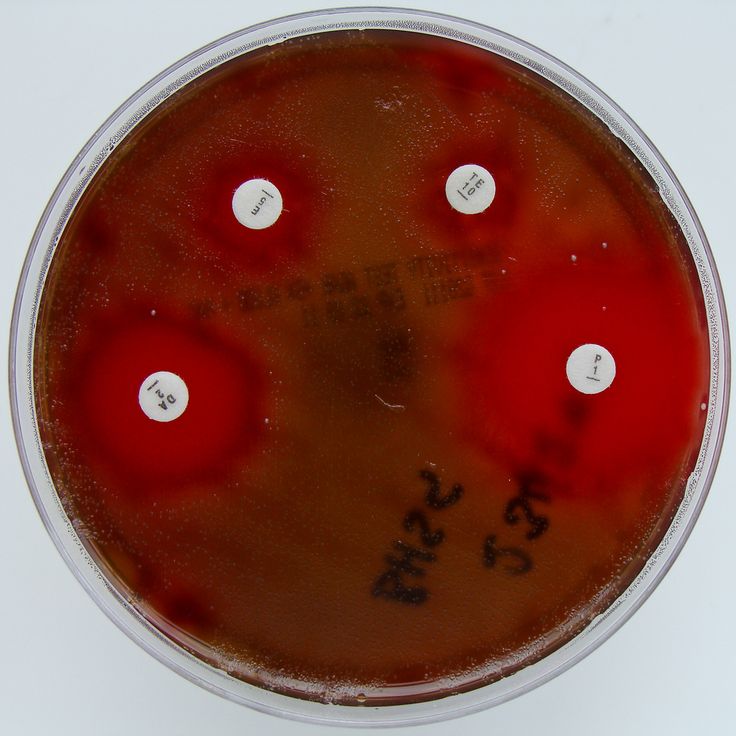
Breast infection (mastitis)
Mastitis is an infection of the breast tissue that results in breast pain, swelling, warmth and redness of the breast. Mastitis most commonly affects women who are breast-feeding (lactation mastitis), although sometimes this condition can occur in women who aren't breast-feeding.
You should visit your primary care physician to confirm the diagnosis and discuss treatment options, such as antibiotics.
Rarity: Uncommon
Top Symptoms: fatigue, nausea, breast pain, signs of breast inflammation like redness, swelling or fever, fever
Symptoms that always occur with breast infection (mastitis): breast pain, signs of breast inflammation like redness, swelling or fever
Urgency: Primary care doctor
Breast abscess
Breast abscess is a complication of mastitis, which is an inflammation of the breast tissue. An abscess is a pocket of pus that forms within the breast, usually just under the skin.
An abscess is a pocket of pus that forms within the breast, usually just under the skin.
Most susceptible are women who are breastfeeding. Bacteria can be transferred into the milk ducts from the skin or from the infant's mouth. Women not breastfeeding can be infected through a sore nipple or from a nipple piercing.
If a milk duct is blocked through trauma, compression, or incomplete emptying, bacteria can gain a foothold and an abscess can form.
The abscess forms a hot, reddened, painful lump in the breast. There will be flu-like symptoms of fever, chills, fatigue, and body aches.
Diagnosis is made through physical examination and sometimes a milk sample.
Treatment is with antibiotics along with rest, fluids, and over-the-counter pain relievers. Unless otherwise directed by the medical provider, it is safe to continue nursing the baby. If the abscess persists, it may be drained under local anesthesia with a needle and syringe.
Allergic contact dermatitis of the chest
Allergic contact dermatitis means the skin has touched something that provoked an allergic reaction, causing inflammation and irritation.
"Contact" means the allergic reaction came from touching something, not from consuming something. The first exposure to the substance sensitizes the immune system, and then the second exposure actually causes the symptoms.
The most common causes of allergic contact dermatitis are:
- Nickel, a metal often used in belt buckles, the buttons on pants, and jewelry, including piercing jewelry.
- Poison ivy.
- Various types of perfumes, including those founds in soaps, fabric softeners, and detergents.
- Of course, there are many more.
Symptoms include red, itching, scaling, flaking skin that may be painful due to the irritation and inflammation.
Diagnosis is made through first avoiding contact with any suspected substance, to see if the dermatitis clears. Patch testing can be done if the results are not certain.
Treatment involves fully avoiding the allergy-provoking substance and using topical steroid cream as prescribed. Cool compresses and calamine lotion can help to ease the discomfort.
Rarity: Common
Top Symptoms: chest redness, chest itch, scabbed area of the chest
Symptoms that always occur with allergic contact dermatitis of the chest: chest redness
Urgency: Self-treatment
Cracked nipples treatments and relief
If the cause of your cracked nipples is related to breastfeeding or friction, treatment can begin at home and will likely be effective.
When to see a doctor
If your difficulty breastfeeding persists, you should reach out to your physician or a lactation specialist. If the severity of your symptoms worsens or persists, you should consult your physician as well.
Tips for proper latching
With breastfeeding, positioning the baby properly on the breast is essential to preventing and treating cracked nipples. There are many ways to hold a baby while breastfeeding. In all holds, the baby needs to be close, with their ear, shoulder, and hip aligned.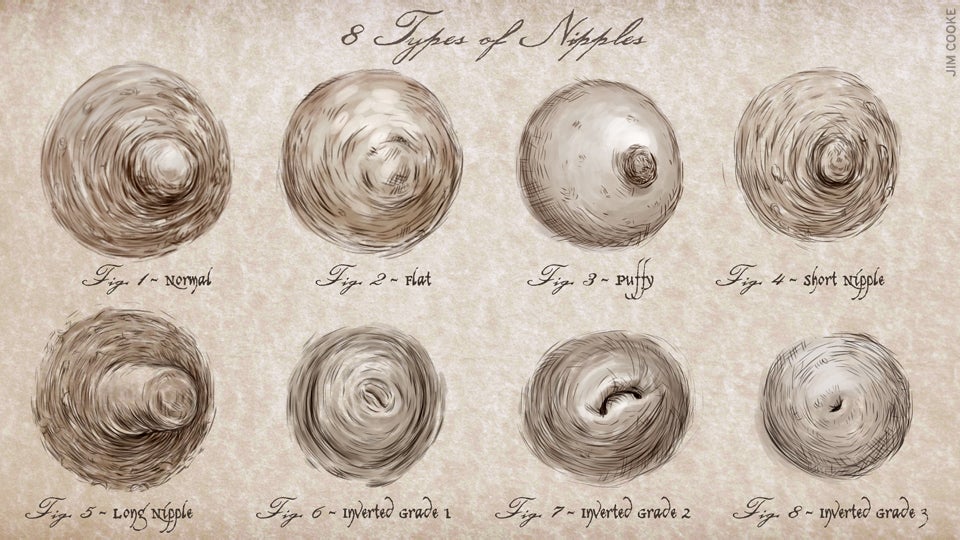 Recognizing a poor latch is a learning process. Some indications of a proper latch include the following.
Recognizing a poor latch is a learning process. Some indications of a proper latch include the following.
- The baby's nose is almost touching the breast
- The baby's lips are flared open: Think fish lips, instead of tucked in or over the gums.
- Painless: While there might be discomfort, there should not be any nipple or breast pain.
- Good coverage: The baby's mouth covers about a half inch of the areola, not just the nipple itself.
At-home treatments for breastfeeding
Treatments to address cracked nipples from breastfeeding include the following.
- Apply topical lanolin
- Apply colostrum or breast milk to the injured area
- Keep the nipples open to air
- Adjust: Rotate the baby's position on the breast to take the pressure off the cracked area.
- Pump by hand: Temporarily pump or express breast milk by hand.
- Start each feed on the uninjured breast
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), the preferred NSAID while breastfeeding, for pain.
At-home treatments to reduce friction
"Jogger's nipple," is most likely to happen during winter or other dry weather conditions. Surfers and divers experience wetsuit rub from the constant friction of a wetsuit or surfboard against the chest. If your nipples are severely cracked, you may need to avoid similar activities temporarily. Antiseptic creams (such as Neosporin) can facilitate healing. All Purpose Nipple Ointment (APNO), made up of betamethasone, miconazole, and mupirocin, is available by prescription. To avoid friction-related cracked nipples you can also try to:
- Avoid wearing clothing made of coarse material
- Avoid wearing loose-fitting clothing
- Wear a supportive bra made of soft material
- Apply a balm or a topical, waterproof emollient prior to activities
- Wear nipple covers or cover nipples with band-aids
When it is an emergency
Seek immediate treatment or call 911 for the following.
- Symptoms of infection: Such as a pus-like discharge from the crack in the nipple
- Your breast is red: Especially if the skin takes on a texture similar to an orange peel
- The condition does not respond to home remedies
- Fever
- Your breast becomes hard or painful
Cracked nipples quiz
Take a quiz to find out what's causing your cracked nipples.
Take cracked nipples quiz
FAQs about cracked nipples
Here are some frequently asked questions about cracked nipples.
Why do I have cracked nippled while breastfeeding?
Nipple injury usually is due to incorrect breastfeeding technique, particularly poor position or latch-on. Other factors may include harsh breast cleansing, use of potentially irritating products, and biting by an older infant. In addition, skin conditions such as dermatitis as well as bacterial or fungal infections are more common in women who are breastfeeding or lactating. Any of these conditions can lead to cracked, painful, or bleeding nipples.
Any of these conditions can lead to cracked, painful, or bleeding nipples.
Why I do have cracked nipples with pus?
If you have cracked nipples with pus, it is very likely that you have an infection in the breast tissue or milk ducts. Women who are lactating or breastfeeding are at higher risk for infection of the nipple or breast, but anyone can get a breast infection. The presence of pus suggests a bacterial infection, which is also common among women who are breastfeeding or lactating. Cracking of the nipples may be a symptom of the infection. It is also possible that the nipples were cracked from breastfeeding or other trauma, and then became secondarily infected.
What do cracked nipples mean when I'm not breastfeeding?
Chafing is a common cause of cracked or bleeding nipples in men, especially men who participate in endurance sports. Chafing of the nipple can occur with women as well. Other possible causes of cracked nipples include benign conditions of the breast, such as eczema, dermatitis caused by contact irritation, and nipple adenoma. However, cracked nipples can also be a sign of breast cancer (Paget disease of the breast) or skin cancers (such as squamous carcinoma of the epidermis, basal cell carcinoma, and superficial spreading malignant melanoma).
However, cracked nipples can also be a sign of breast cancer (Paget disease of the breast) or skin cancers (such as squamous carcinoma of the epidermis, basal cell carcinoma, and superficial spreading malignant melanoma).
Can I still breastfeed with cracked nipples?
Most doctors recommend continuing to breastfeed with cracked nipples, as long as the pain is tolerable. If one nipple is cracked, it is possible to breastfeed on the other side to give the cracked nipple a chance to heal. It is also possible to pump breast milk while the nipples heal, and then continue breastfeeding. Typically, cracked nipples during lactation and breastfeeding indicate there is a problem with infant positioning or latch. Education on proper positioning and attachment of the infant may be the best intervention for alleviating nipple pain.
Can cracked nipples become infected?
Yes. The protective barrier of the skin is disrupted as nipples become cracked, which increases the susceptibility to infection. It is common for women who are lactating or breastfeeding to experience cracked nipples from improper positioning, improper latch, or possible trauma from biting in older infants. Bacteria in the infant's mouth can then enter the breast tissue and cause an infection. It is also possible for women who are not breastfeeding or men to experience cracked nipples that then become secondarily infected. If you suspect you have a nipple infection, seek medical treatment.
It is common for women who are lactating or breastfeeding to experience cracked nipples from improper positioning, improper latch, or possible trauma from biting in older infants. Bacteria in the infant's mouth can then enter the breast tissue and cause an infection. It is also possible for women who are not breastfeeding or men to experience cracked nipples that then become secondarily infected. If you suspect you have a nipple infection, seek medical treatment.
Questions your doctor may ask about cracked nipples
- Have you been feeling more tired than usual, lethargic or fatigued despite sleeping a normal amount?
- Did you suffer from any complications during pregnancy or childbirth?
- When did you have your most recent child?
- Are you currently pregnant?
Self-diagnose with our free Buoy Assistant if you answer yes on any of these questions.
Jeffrey M. Rothschild, MD, MPH.
Associate Professor of Medicine, Brigham and Women’s Hospital
Dr. Rothschild has been a faculty member at Brigham and Women’s Hospital where he is an Associate Professor of Medicine at Harvard Medical School. He currently practices as a hospitalist at Newton Wellesley Hospital. In 1978, Dr. Rothschild received his MD at the Medical College of Wisconsin and trained in internal medicine followed by a fellowship in critical care medicine. He also received an MP...
Rothschild has been a faculty member at Brigham and Women’s Hospital where he is an Associate Professor of Medicine at Harvard Medical School. He currently practices as a hospitalist at Newton Wellesley Hospital. In 1978, Dr. Rothschild received his MD at the Medical College of Wisconsin and trained in internal medicine followed by a fellowship in critical care medicine. He also received an MP...
Read full bio
Was this article helpful?
4 people found this helpful
Tooltip Icon.Copied to clipboard
Nipple fissure - health articles
11/10/2022
Nipple fissure - defect, damage to the integrity of the skin on the nipples of the mammary glands. It is manifested by a sharp soreness with irradiation to the shoulder blade when feeding a child. It can be complicated by infection of wounds, the development of candidiasis on the nipple, mastitis. If cracks become infected, there is a risk of infection of the child during feeding.
Treatment of cracked nipples begins with the elimination of their cause. In parallel, they carry out the prevention of their infection, use means that promote the speedy healing.
Causes
The main reason for the appearance of cracks is the lack of breastfeeding during feeding. When properly applied to the breast, the nipple rests against the baby's palate in a fixed motionless position, the child squeezes the areola with its jaws, contributing to the outflow of milk. In this case, the lower lip of the child is tucked up. If the nipple is not inserted to the proper depth, then it ends up on the tongue, gaining mobility, the lower lip injures the nipple and areola, and the jaws compress the breast in the most sensitive and easily damaged place. As a result of constant irritation of the nipple and areola areas, damage to the skin occurs - cracks form.
The second most common cause of cracked nipples may be improper weaning. Often, when feeding, mothers do not support the child's head, and also place his stomach not towards himself, but up. As a result, at the end of feeding, the child turns away from the breast, pinching the nipple in the jaws. There is pressure on areas of the nipple that are not intended for this.
As a result, at the end of feeding, the child turns away from the breast, pinching the nipple in the jaws. There is pressure on areas of the nipple that are not intended for this.
Another common cause is washing your nipples too often. Modern medicine does not support the need to wash the breast after each feeding. With frequent washing, the nipples are washed off their natural lubricant, which is secreted by special glands in the skin of the areola (Montgomery's glands) and the nipples lose one of their natural protective mechanisms.
Fissures can also develop when feeding older children as a result of bites from erupted teeth.
The development of thrush contributes to the occurrence of cracked nipples.
Symptoms
Symptoms that may appear both in the early periods of feeding and later:
- solitary or multiple lesions of the skin of the breast, nipples and areals;
- superficial cracks that will show up on contact with underwear;
- subcutaneous fissures, characterized by severe pain;
- bleeding;
- slight suppuration;
- increased sensitivity and soreness of the nipples;
- Excessively dry skin around the nipples and areolas.
Even if you notice that at least one of the above symptoms appears from time to time and then disappears, this can also be an important signal of a possible infection or the presence of any other disease.
Treatment of cracked nipples
If it is a small cracked nipple, treatment can be started at home. The first step is to prevent infection. Change your underwear every day, iron your bra after washing with a hot iron. Put disposable sterile pads inside the bra and change them when they become damp.
It is not worth washing the breast after each feeding, so as not to violate the natural protection. Mother's milk itself is a good antiseptic, so it can be used as a cream for cracked nipples, squeezing a few drops after feeding. Be sure to let the milk dry, hold your chest open for a few minutes.
Earlier, when nipple cracks appeared, treatment was started with green paint. You should not do this, as it has been proven that brilliant green is quite toxic. It is better to use a methylene blue aqueous or alcohol solution as an antiseptic, this antiseptic will also serve to prevent thrush in a child. It should be noted that antiseptics cannot solve the problem of how to treat nipple cracks, they only prevent infection.
It is better to use a methylene blue aqueous or alcohol solution as an antiseptic, this antiseptic will also serve to prevent thrush in a child. It should be noted that antiseptics cannot solve the problem of how to treat nipple cracks, they only prevent infection.
Cracked nipples can be lubricated with castor oil to soften the skin and heal quickly. It can be replaced with sea buckthorn or rosehip oil. Oil is applied to cracked nipples after feeding. Be sure to wait until it dries, and only then put on a bra.
Compresses for cracked nipples can be made from butter and applesauce. Apples need to be rubbed on a grater, add butter to them in a ratio of 1: 1 and attach to the chest. Hold the compress for 2-3 hours.
Kalanchoe or aloe juice has an excellent healing effect. The leaves of the plants are cut in half and smeared with pulp on the cracks in the nipples. Juice can be squeezed out and compresses can be made from it.
Cracked nipples during feeding can also be treated with products from a pharmacy. A good effect is given by preparations based on lanolin. This substance does not give allergies and is safe enough for the child.
A good effect is given by preparations based on lanolin. This substance does not give allergies and is safe enough for the child.
Cracked nipples | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs A. et al., "Recommendations S -3 for the management of inflammatory breast disease during breastfeeding: AWMF guidelines , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R. A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent maternal sore nipples", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012).
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma.