White dots on baby face
Milia Condition, Treatments and Pictures for Infants
Milia are tiny cysts that occur for unknown reasons in infants.
Milia are tiny (about an 1/8 to 1/4 inch in diameter) cysts.
Milia are smooth, white cysts often found on the face.
This image displays milia, the small, white bumps at the center of the forehead.
Though they are white in color, milia are filled with skin scale (keratin), not pus.
Images of Milia (5)
Milia are tiny (1–2 mm) pearly white cysts on the surface of the skin that are common in people of all ages, but are more noticeable in infants since they are present on the face. Milia form because the oil gland in the infant is still developing, and the skin does not slough off normally but will instead remain trapped in a pocket in the skin. Milia are classified into 2 types: primary milia, which occur on normal, healthy skin; and secondary milia, which are typically found on skin affected by another skin condition. Milia that are found on the roof of the mouth in infants are called Epstein pearls and are normal in newborns.
Who's At Risk?
Milia can occur in all populations and ages. Primary milia are so common in newborns (occurring in up to 50%) that they are considered normal. Secondary milia are less common in infants but may appear if there is any injury to the skin.
Signs & Symptoms
The most common locations for primary milia in infants include:
- Around the nose
- Around the eye (periorbital area)
- Cheeks
- Chin
- Forehead
Very rarely, infants may develop milia in the following locations:
- Trunk
- Limbs
- Penis
- Mucous membranes such as inside the mouth
A milium appears as a small (1–2 mm), white to yellow, dome-shaped bump in the superficial skin.
Take a picture of your skin condition with Aysa
Symptom checkers like Aysa can help narrow down possible skin conditions by analyzing a skin photo.
Self-Care Guidelines
Although milia are found in the superficial layers of skin, they are difficult to remove without the proper tools. Trying to extract them at home is not a good idea as it may lead to scarring.
Primary milia found in infants tend to resolve on their own within several weeks, though they may persist for 2 or 3 months.
Advertisement
Treatments
If the doctor diagnoses primary milia in an infant, no treatment is necessary, as the condition will resolve on its own within a few weeks.
However, persistent and stubborn milia may occasionally be treated with the following:
- Topical retinoid cream such as tretinoin, tazarotene, or adapalene
- Removal with a sterile lancet or scalpel followed by use of a special tool (a comedone extractor)
Visit Urgency
Any new bump on your child’s skin should be evaluated by a dermatologist or by another physician.
Trusted Links
- MedlinePlus: Common Infant and Newborn Problems
- Clinical Information and Differential Diagnosis of Milia
Advertisement
References
Bolognia, Jean L.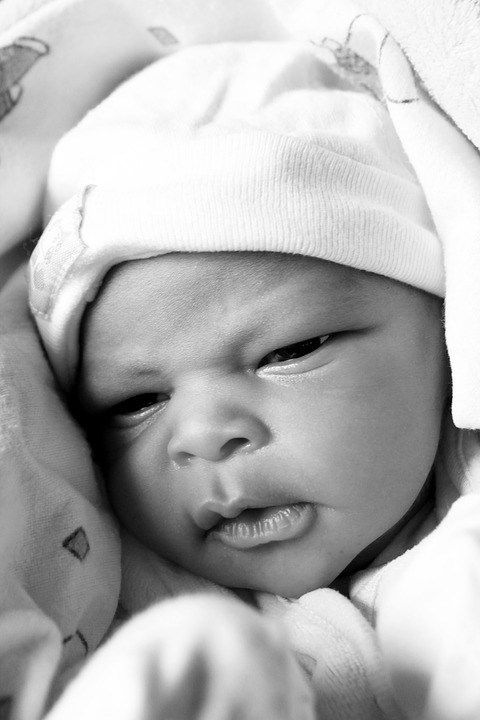 , ed. Dermatology, pp.1722-1723. New York: Mosby, 2003.
, ed. Dermatology, pp.1722-1723. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed. pp.601, 604, 780. New York: McGraw-Hill, 2003.
Disease Groups: Mouth Sores and Lip Conditions
What You Need to Know About Milia and Baby Acne
This entry was posted in New Babies, newborn and tagged baby acne, infant skin conditions, milia, neonatal acne on by Jamie Spence.In our third installment covering infant skin issues, we’ll be discussing milia and baby acne. Unlike some of the skin conditions we’ve covered, milia and baby acne are not rashes.
Milia are tiny white bumps that appear on a baby’s nose, chin, cheeks, or eyelids. These bumps tend to appear in groups or clusters of small white or yellowish bumps. A single milium can range from less than 1 millimeter up to 3 millimeters in size. Although they are very common in newborn babies, they can appear at any age.
Although they are very common in newborn babies, they can appear at any age.
There are two basic types of milia:
- Primary: the most common form of milia, especially on babies, appears on healthy skin. They frequently occur on the eyelids, forehead, cheeks, or genitals.
- Secondary: also known as traumatic milia, this type appears on skin that has acne, infection, or is in otherwise damaged condition. Secondary milia often appear on skin that has been damaged by burns, rashes, blisters, reaction to a topical cream/ointment, or even excessive exposure to sunlight. The milia develop as the skin heals. In this instance, it is more common to occur on older children or adults than on newborns.
Milia are caused by keratin from dead skin cells, accumulating just under the surface of the skin. In essence, they are tiny, benign cysts caused by a buildup of skin flakes. However, they do not require removal like some other types of cysts.
Milia doesn’t require treatment at all unless the bumps become red or inflamed, or if the area develops a crusty appearance. If you see the area developing redness, swelling, or forming crust around the milia, call our office for an appointment. It is possible that an infection or underlying skin condition could be causing the milia.
If you see the area developing redness, swelling, or forming crust around the milia, call our office for an appointment. It is possible that an infection or underlying skin condition could be causing the milia.
Milia do not cause pain or itching for your baby. Attempting to squeeze milia bumps like a pimple can cause the skin to become sore or even infected. Untreated infection can result in scarring, so it is best to leave milia bumps be. You will simply want to keep your baby’s skin clean and avoid any irritating lotions or heavily scented products on the area that could cause irritation.
While milia cannot be prevented, the bumps will usually clear on their own in a few weeks to a month.
Baby acne is also known as “neonatal acne.” It is not a true type of acne and is only temporary in duration, usually lasting 1 to 3 months. It is believed to be caused by an inflammatory reaction to yeast on the skin. The condition is very common, occurring in more than 20% of healthy newborns.
Baby acne often presents around two weeks of age, with tiny bumps and pustules on a baby’s forehead, cheeks, eyelids, or chin. These small pustules can extend into the scalp, as well. Occasionally, the pustules will appear on the neck and upper trunk. Unlike true acne, baby acne does not consist of any blackheads or whitehead pustules.
Baby acne differs from infantile acne. Infantile acne is much less common and can present with open comedones or blackheads, while baby acne does not. Cysts or nodules are also sometimes seen with infantile acne and the condition can result in scarring without treatment. Infantile acne can persist until the baby is two years old.
While the cause of baby acne is unknown, some studies link the condition to maternal or infant hormones, while others believe it to be caused by an inflammatory reaction to yeast on the skin.
Baby acne will usually clear without medical treatment. If your baby’s acne does not resolve on its own within 3 months, contact our office for an appointment. If treatment is necessary, an antifungal cream such as ketoconazole or a low-potency topical steroid such as hydrocortisone may be prescribed. Also, if you see other symptoms such as a fever, irritability, decreased appetite, or other skin conditions developing, we would recommend an appointment with our office as soon as possible.
If treatment is necessary, an antifungal cream such as ketoconazole or a low-potency topical steroid such as hydrocortisone may be prescribed. Also, if you see other symptoms such as a fever, irritability, decreased appetite, or other skin conditions developing, we would recommend an appointment with our office as soon as possible.
How to remove milia - white dots or wen on the face
August 8LikbezZdorovye
If they do not bother you, you can not touch them.
Share
0What are milia
Milia are small (1-2 mm), hard, round, benign cysts on the skin filled with the protein keratin. They are also called whiteheads, whiteheads, or wen.
Milia do not hurt, itch or harm health. They are yellow and white and usually appear in places with thin skin - near the eyes and mouth, on the forehead, also found on the cheeks, nose, chin, rarely on the genitals. Millets can occur individually, or they can be in whole clusters.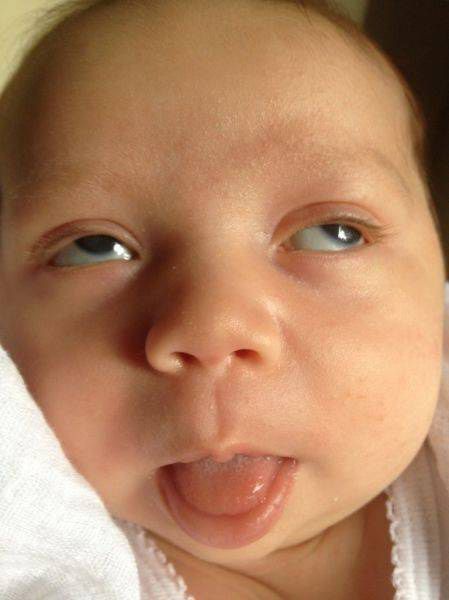
They are common in people of all ages, including half of newborns.
Why milia appear
When the skin is exfoliated, old cells fall off to make room for new ones. If for some reason they remain, then after some time they harden and form a cyst - primary milia.
There are also secondary milia. They may appear:
- due to damage to the skin in places where there was an injury, rash or sunburn;
- long-term use of corticosteroids;
- genetic or autoimmune diseases.
Who is more likely to have milia
Very often whiteheads occur in newborns, because their skin is just learning to exfoliate old cells.
But milia can happen to anyone. The risk is higher in people who:
- do not clean their skin enough;
- use oily or comedogenic cosmetics;
- do not sleep enough;
- have skin conditions such as seborrhea or rosacea;
- take steroids for a long time.

How to get rid of milia in children
Milia in newborns do not need to be treated. It is enough to wash the child with warm water every day. Sometimes with a mild baby cleanser. At the same time, it is important not to rub the delicate skin, but to pat it, and then blot it with a towel.
But wiping the skin with lotions, oils and exfoliating cosmetics for adults is not allowed. Also, in no case do not try to squeeze milia or remove them with a needle: this can leave scars and cause an infection.
If the prosyanki do not disappear in a few months, you need to inform the pediatrician about this at the next scheduled examination.
How to get rid of milia in adults
As we already wrote, whiteheads do not harm health in any way, so they can not be treated. In addition, in adults, milia can also go away on their own.
If you don't want to wait, you can try exfoliating products, for example with weak acids, which are allowed for home care.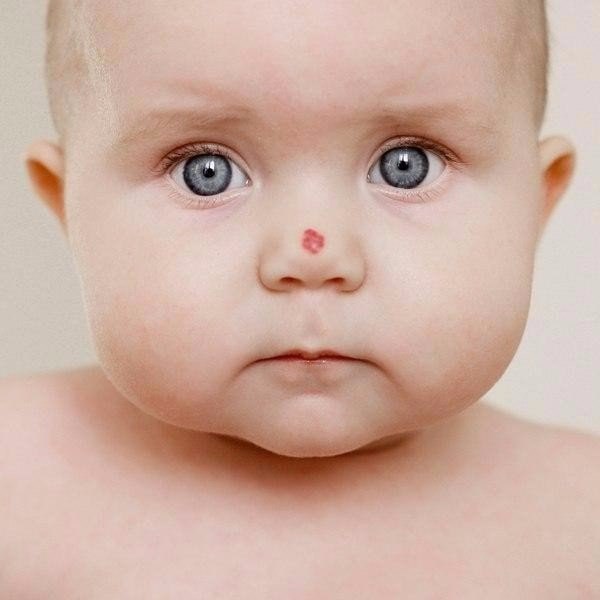 But before that, you should ask a dermatologist or cosmetologist if they are suitable for your case.
But before that, you should ask a dermatologist or cosmetologist if they are suitable for your case.
It is strictly forbidden to open milia at home. Scars may remain at the site of the cysts, and bacteria may enter the wound.
If home treatment fails, milia can be removed at a dermatologist's appointment. To do this, use the following methods:
- excision - mechanical peeling;
- cryotherapy - quick freezing with liquid nitrogen;
- diathermy - cauterization with high frequency alternating current;
- laser surgery;
- chemical peels;
- dermabrasion - mechanical skin resurfacing.
Less commonly, your doctor may prescribe topical or systemic retinoids.
How to make milia less frequent
The best way to prevent whiteheads is to take care of your skin. This means:
- Wash your face twice a day.
- Use deep cleansing two to three times a week.
 You can consult with a beautician which products are best suited.
You can consult with a beautician which products are best suited. - Wear sunscreen with SPF 30 even on cloudy days.
Read also 🚰🧼🧴
- Is facial biorevitalization worth it for smooth and beautiful skin
- 7 TikTok skin care trends that dermatologists recommend avoiding
- How to take care of your skin as a man: tips and essential cosmetics
- How to know if you have rosacea and what to do next
- Rules for radiant skin: how to care for the face in 20, 30, 40 and 50 years old
What do white spots on the face mean?
Many people at some point in their life may develop white spots of varying sizes on their face, arms or chest. Below are the top 5 causes of white spots on the face.
- Milia
Milia are small, round, hard white dots on the face that are often mistaken for whiteheads. They develop when the protein keratin found in the top layer of the skin and other components of dead skin cells build up under the surface of the skin.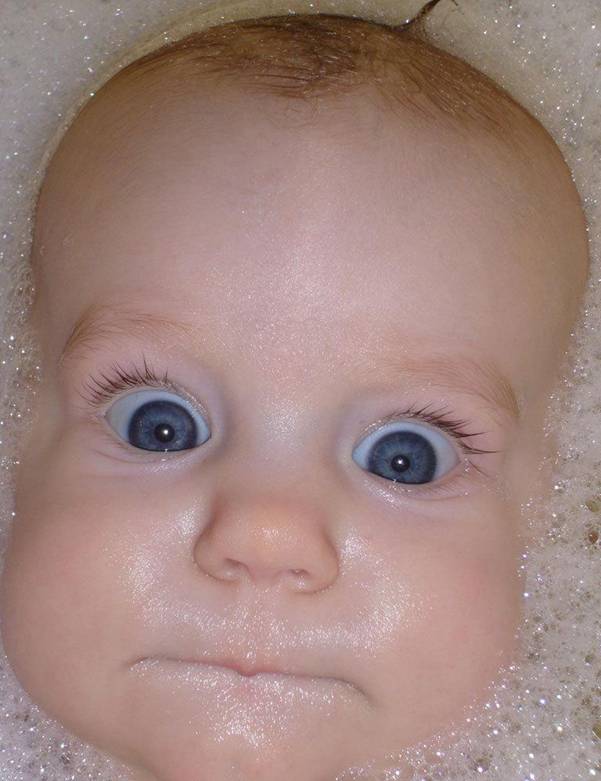 The most common areas for milia to appear are around the eyes, cheeks, and nose. Milia can be noted in all age groups in both men and women. It is also common among very young children and is then called milk spots.
The most common areas for milia to appear are around the eyes, cheeks, and nose. Milia can be noted in all age groups in both men and women. It is also common among very young children and is then called milk spots.
Milia can be caused by an allergic reaction to face cream or sun damage.
A person usually gets better without treatment within a few weeks. Dermatologists recommend not squeezing or punching rashes at home. Changing the face cream or other products that may have caused the allergic reaction may help.
If the condition does not improve on its own, a doctor or dermatologist can treat milia in a variety of ways: opening the capsules (to extract keratin with a medical needle), applying a retinoid cream (on the face, but not around the eyes), microdermabrasion (a procedure that removes the most upper layers of the affected area).
- Seborrheic eczema
The disease looks like pale pink or red scaly inflammations on the skin. They often appear on the face and hands. Seborrheic eczema is more noticeable in dark-skinned individuals or after sun exposure. The condition is mainly noted in children and adolescents. The causes of the disease are unknown.
They often appear on the face and hands. Seborrheic eczema is more noticeable in dark-skinned individuals or after sun exposure. The condition is mainly noted in children and adolescents. The causes of the disease are unknown.
Spots usually disappear within a few months, but may last up to several years. There is no specific treatment for seborrheic eczema, but a doctor can treat any symptoms of itching or discomfort with steroid or nonsteroidal creams, as well as treat dry skin.
- Vitiligo
Vitiligo appears as spots on the skin that have lost their color pigment. They can appear anywhere, including the face. The disease occurs in about 1% of people worldwide. White spots can be small and remain so, and sometimes gradually increase and cover almost the entire body. Vitiligo can occur at any age, but about half of people develop the disease before age 20.
Heredity is a risk factor for the development of the disease. Vitiligo occurs in people with various skin tones, but is most noticeable on dark skin. The disease is not contagious. Some scientists believe that vitiligo patches develop when the body produces an antibody against melanin and breaks it down.
Vitiligo occurs in people with various skin tones, but is most noticeable on dark skin. The disease is not contagious. Some scientists believe that vitiligo patches develop when the body produces an antibody against melanin and breaks it down.
There are several possible treatments for vitiligo. The choice of method depends on the severity of the condition. Individuals with vitiligo should always wear sunscreen and avoid sun exposure as the affected skin will burn more easily. You can also use special creams to hide the difference in skin color. Your doctor may recommend anti-inflammatory creams, such as corticosteroids. However, long-term use of corticosteroids can cause unwanted side effects, such as thinning of the skin, so doctors may prescribe other types of anti-inflammatory creams.
Vitiligo is sometimes treated with artificial ultraviolet (UV) light therapy or phototherapy, often for several months. Laser treatment can also be used to treat certain areas of the skin. Surgical therapy has been developed, but is not yet a common practice.
Surgical therapy has been developed, but is not yet a common practice.
- Pityriasis versicolor ( Pityriasis versicolor)
Pityriasis versicolor is a common disease caused by a yeast infection. In this case, spots of various shades of any localization appear on the skin and are accompanied by dry skin and itching. Sometimes the spots are small, and sometimes they become noticeable only when the skin is tanned. Pityriasis multicolor is more common in adolescents and young adults, and is more common in the tropics and subtropical regions. In temperate climates, discolored patches may disappear during the cooler months.
More than 90% of adults have a yeast called Malassezia on their skin. This is a natural phenomenon and usually does not cause any problems. However, sometimes they provoke the development of multi-colored lichen. This may be due to several factors such as:
- hot and humid weather;
- oily skin;
- weak immune system;
- hormonal changes.

Pityriasis versicolor can occur during pregnancy but is not dangerous.
There are many different ways to successfully treat tinea versicolor with antifungal creams and lotions, cleansers, and antifungal tablets.
- Idiopathic guttate hypomelanosis
Idiopathic guttate hypomelanosis, also known as white sunspots, is characterized by the appearance of flat white spots 1 to 10 mm in diameter. These spots can occur on the face, arms, upper back, and lower legs. Although they most commonly develop in fair-skinned individuals, they can also occur in dark-skinned individuals.
Idiopathic guttate hypomelanosis occurs due to prolonged exposure to the sun on the skin. This skin condition appears more often in people over the age of 40, which may be due to the fact that the disease takes a long time to develop.
There is no specific treatment. Steroid creams, masks, and dermabrasion may be used to reduce the appearance of blemishes.