Varicella in pregnancy
Chickenpox during pregnancy | March of Dimes
Chickenpox is an infection caused by a virus. If you get it during pregnancy, it can cause problems for you and your baby.
You’re probably safe from chickenpox if you’ve had it before or if you’ve had the vaccine. Both of these help make you immune to chickenpox.
Talk to your health care provider to make sure you’re immune to chickenpox before you get pregnant or early in pregnancy.
What is chickenpox?
Chickenpox is an infection caused by a virus called the varicella-zoster virus. Chickenpox used to be a common infection, especially in children under age 12. It’s less common now because a vaccine is available to help prevent it. A vaccine is medicine that makes you immune to certain diseases.
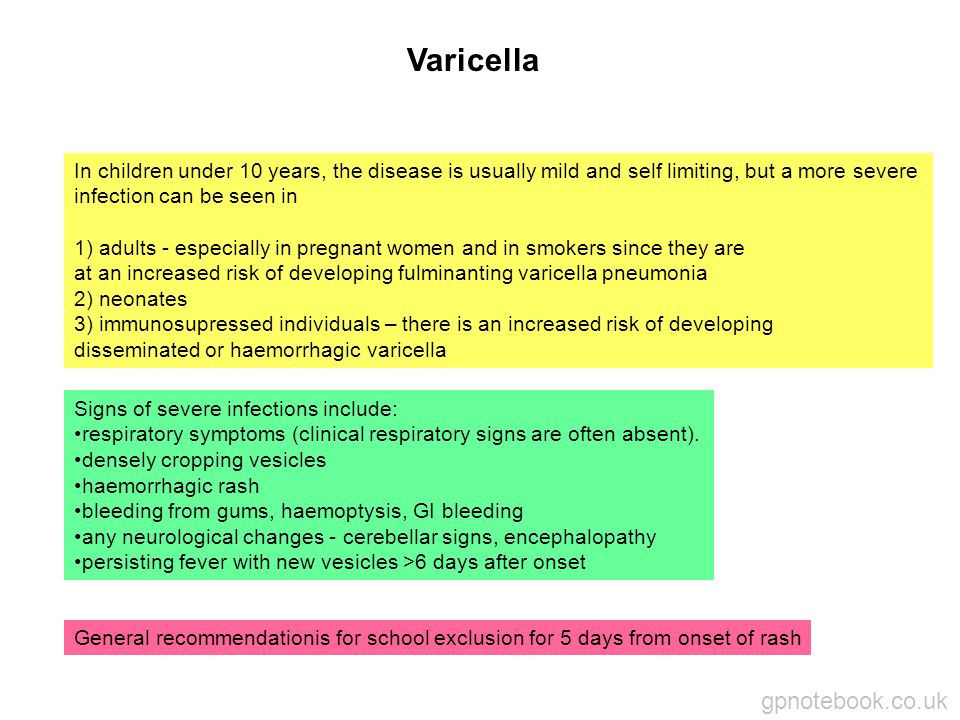
Chickenpox usually isn’t dangerous in children. But some people are at higher risk for complications from chickenpox, including pregnant people and newborns.
The chances of getting chickenpox during pregnancy are low. Most pregnant people are immune to chickenpox because they’ve had the infection before or they’ve been vaccinated against it. Talk with your health care provider to make sure you’re immune to chickenpox before you get pregnant or early in pregnancy.
What are the symptoms of chickenpox?
Chickenpox causes an itchy rash that turns into blisters and then scabs. The rash usually starts on the chest, back, and face and spreads all over the body. The rash appears about 10 to 21 days after you’re infected and can last 5 to 10 days.
Other symptoms can include fever, headache, being tired and not being hungry. These symptoms may appear 1 to 2 days before the rash.
How does chickenpox spread?
If you’re not immune to chickenpox, you can get it easily by being in contact with someone who has the infection. A person with chickenpox can spread the infection starting about 2 days before the rash appears and until all the blisters are covered by scabs.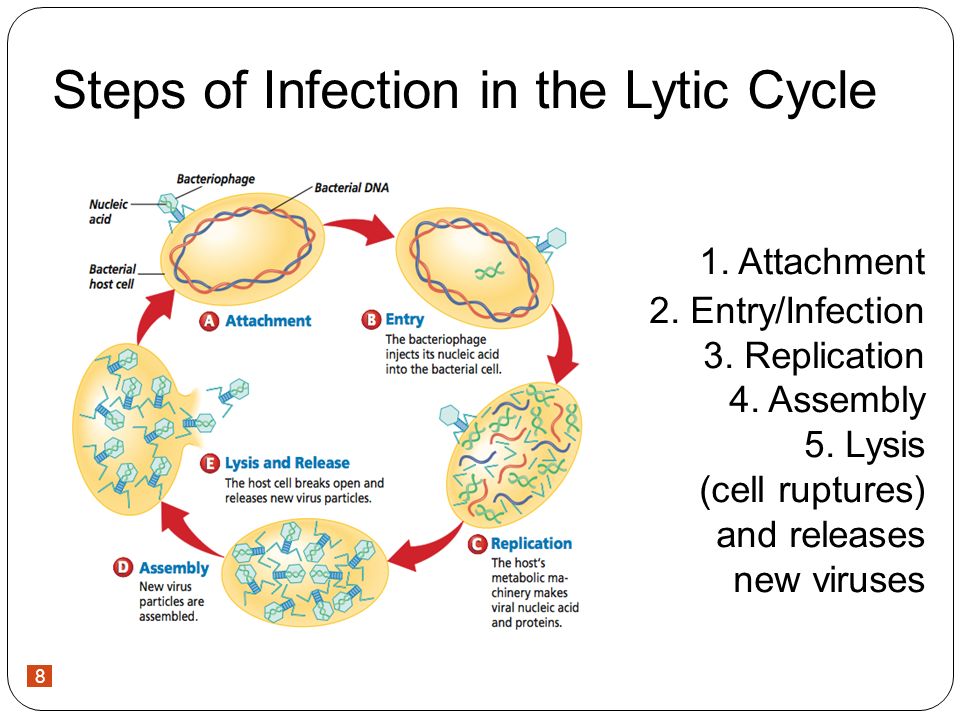 It can spread through:
It can spread through:
- Droplets in the air when someone with chickenpox coughs or sneezes
- The saliva (spit) or mucus of someone with chickenpox
- Touching a chickenpox rash
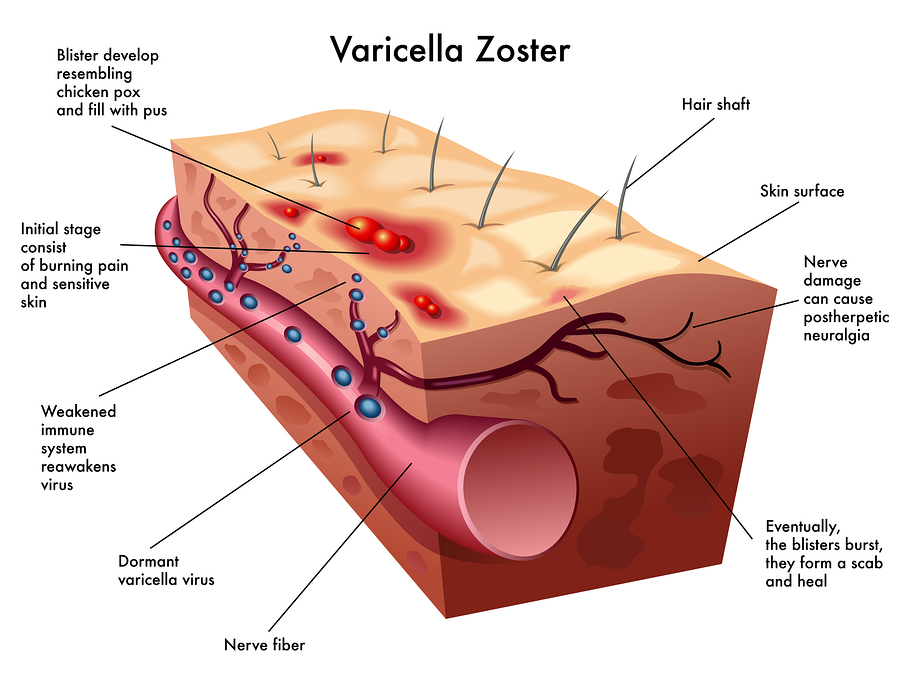
If you’re not immune to chickenpox, you can also get it through close contact with someone who has shingles. Shingles is an infection caused by the same virus that causes chickenpox. If you’ve had chickenpox before, the virus stays in your body and can come back later as shingles. Shingles causes a painful rash on one side of the face or body. People with shingles can spread chickenpox to other people, but they can’t spread shingles to other people.
Can chickenpox during pregnancy cause problems for you and your baby?
Yes. Having chickenpox during pregnancy can increase your risk of getting pneumonia and can even be life-threatening. Pneumonia is a lung infection that can be very serious. The symptoms of pneumonia include cough, chest pain when you breathe or cough, fever, fatigue (being very tired) and shortness of breath.
Chickenpox during pregnancy can cause these problems for your baby:
If you get chickenpox during the first 20 weeks of pregnancy, your baby may have an increased risk for congenital varicella syndrome. This is a rare group of serious birth defects that can cause:
- Scars on the skin
- Problems with the arms, legs, brain and eyes
- Gastrointestinal complications
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
If you get chickenpox between 2 weeks before birth to 2 weeks after birth, you can pass the infection to your baby. If this happens, the infection in your baby usually is mild.
If you get chickenpox immediately before or right after birth (5 days before birth to 2 days after birth), your baby may have an increased risk for a serious infection called neonatal varicella. This infection can be life-threatening, but treatment is helping more babies survive.
If you have a preterm birth, your newborn may be at higher risk of complications from chickenpox. Preterm birth is birth that happens before 37 weeks of pregnancy.
Can you prevent chickenpox?
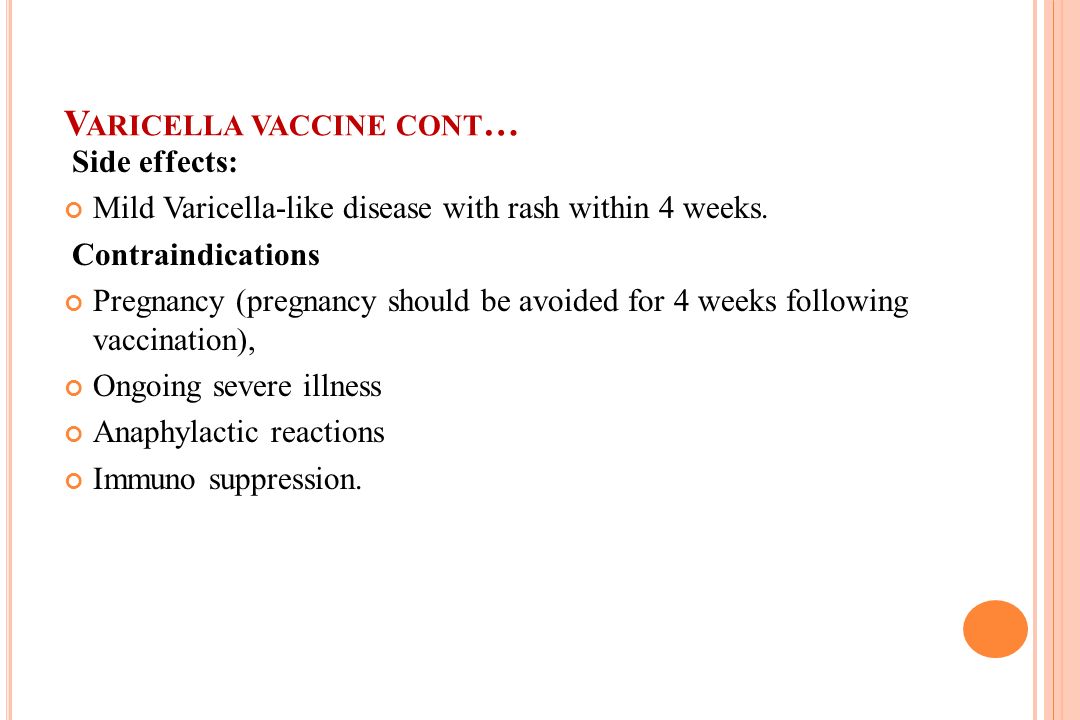
Yes. The varicella vaccine can protect you from chickenpox. In fact, this vaccine prevents more than 3.5 million cases of chickenpox each year. But the vaccine is not safe to get during pregnancy.
Talk to your provider if you’re pregnant or planning a pregnancy and you’re not sure if you've had the vaccine or had chickenpox before. Your provider can do a blood test to find out if you’re immune.
If you aren’t immune, how can you protect yourself from chickenpox during pregnancy?
If you’re planning a pregnancy and the blood test shows you’re not immune, get vaccinated. You get the vaccine in two doses. It’s best to wait 3 months after the second dose before getting pregnant.
If you’re already pregnant, don’t get the vaccine until after you give birth. In the meantime, stay away from anyone who has chickenpox or shingles.
In the meantime, stay away from anyone who has chickenpox or shingles.
Tell your provider right away if you’re pregnant and you come into contact with someone who has chickenpox. Your provider can treat you with medicine that has chickenpox antibodies. Antibodies help the body fight infections. It’s important to get treatment within 10 days after you’ve come into contact with chickenpox to help prevent the infection or make it less serious. And tell your provider if you come in contact with a person who has shingles. Your provider can decide if you need treatment to help prevent you from getting infected.
How is chickenpox diagnosed?
Your provider can tell you if you have chickenpox by doing a physical exam. Your provider may do a blood test or take a swab of the rash and send it to a laboratory for testing to be sure it’s chickenpox.
How is chickenpox treated during pregnancy?
If you get chickenpox during pregnancy, your provider may give you an antiviral medicine such as acyclovir or valacyclovir.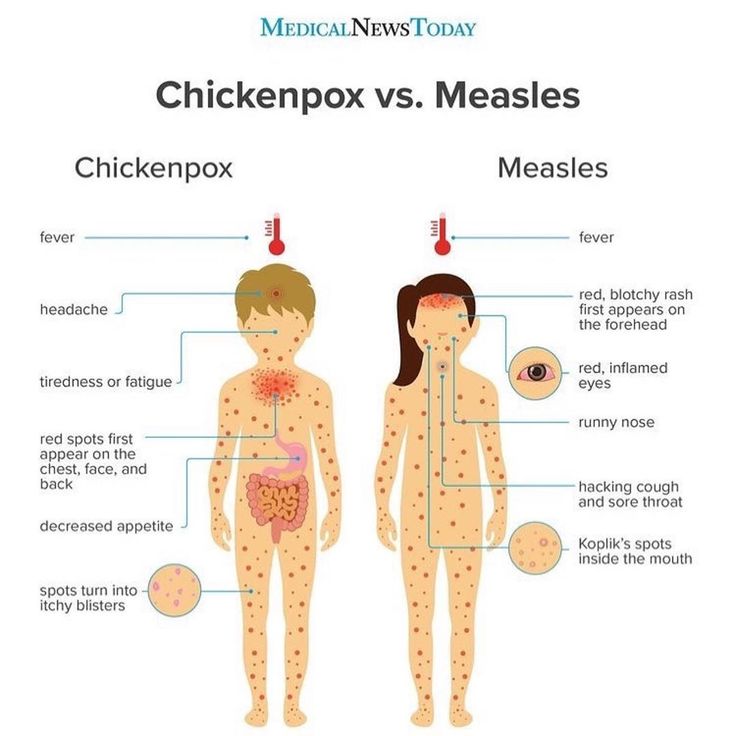 An antiviral is a medicine to treat infections caused by viruses. These medicines are safe to use during pregnancy. They work best when given within 24 hours of the chickenpox rash appearing.
An antiviral is a medicine to treat infections caused by viruses. These medicines are safe to use during pregnancy. They work best when given within 24 hours of the chickenpox rash appearing.
If you have chickenpox and develop signs or symptoms of pneumonia, your provider may want you to stay in the hospital and be treated with acyclovir through an IV (through a needle into a vein).
If you get chickenpox during pregnancy, how is your baby treated after birth?
If you have chickenpox during pregnancy, your baby’s provider may treat your baby right after birth with medicine that has chickenpox antibodies. The medicine can help prevent chickenpox in your baby or make it less dangerous. If your baby gets chickenpox in the 2 weeks after birth, your baby may also be treated with antiviral medicine.
Can you get chickenpox from someone who has gotten the vaccine?
Yes, but it’s rare. If a vaccinated person gets chickenpox, they can still spread it to others. But the vaccine is more than 90 percent effective at preventing chickenpox. Providers recommend that children get their first dose of the varicella vaccine at 12 to 15 months of age and the second dose at age 4 to 6.
But the vaccine is more than 90 percent effective at preventing chickenpox. Providers recommend that children get their first dose of the varicella vaccine at 12 to 15 months of age and the second dose at age 4 to 6.
Last reviewed: May 2021
Varicella Zoster Virus (Chickenpox) Infection in Pregnancy
1. World Health Organization. Epidemiology of chickenpox. 1977–1990. Wkly Epidemiol Rec. 1992;67(16):118–119. [PubMed] [Google Scholar]
2. Prevention of varicella. Update recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1999;48(RR-6):1–5. [PubMed] [Google Scholar]
3. Lolekha S, Tanthiphabha W, Sornchai P, Kosuwan P, Sutra S, Warachit B, et al. Effect of climatic factors and population densityon varicella zoster virus epidemiology within a tropical country. Am J Trop Med Hyg. 2001;64(3–4):131–136. [PubMed] [Google Scholar]
4. Lee BW. Review of varicella zoster seroepidemiology in India and Southeast Asia 1. Trop Med Int Health. 1998;3(11):886–890. [PubMed] [Google Scholar]
Trop Med Int Health. 1998;3(11):886–890. [PubMed] [Google Scholar]
5. Fairley CK, Miller E. Varicella-zoster virus epidemiology--a changing scene? J Infect Dis. 1996;174 (Suppl 3):S314–S319. [PubMed] [Google Scholar]
6. Enders G, Miller E. Varicella and herpes zoster in pregnancy and the newborn. In: Arvin AM, Gershon AA, editors. Varicella-Zoster Virus Virology and Clinical Mangement. Cambridge University Press; 2000. pp. 317–347. [Google Scholar]
7. Gray GC, Palinkas LA, Kelley PW. Increasing incidence of varicella hospitalizations in United States Army and Navy personnel: are today’s teenagers more susceptible? Should recruitsbe vaccinated? Pediatrics. 1990;86(6):867–873. [PubMed] [Google Scholar]
8. Leikin E, Figueroa R, Bertkau A, Lysikiewicz A, Visintainer P, Tejani N. Seronegativity to varicella-zoster virus in a tertiary care obstetric population. Obstet Gynecol. 1997;90(4 Pt 1):511–513. [PubMed] [Google Scholar]
9. Miller E, Vardien J, Farrington P.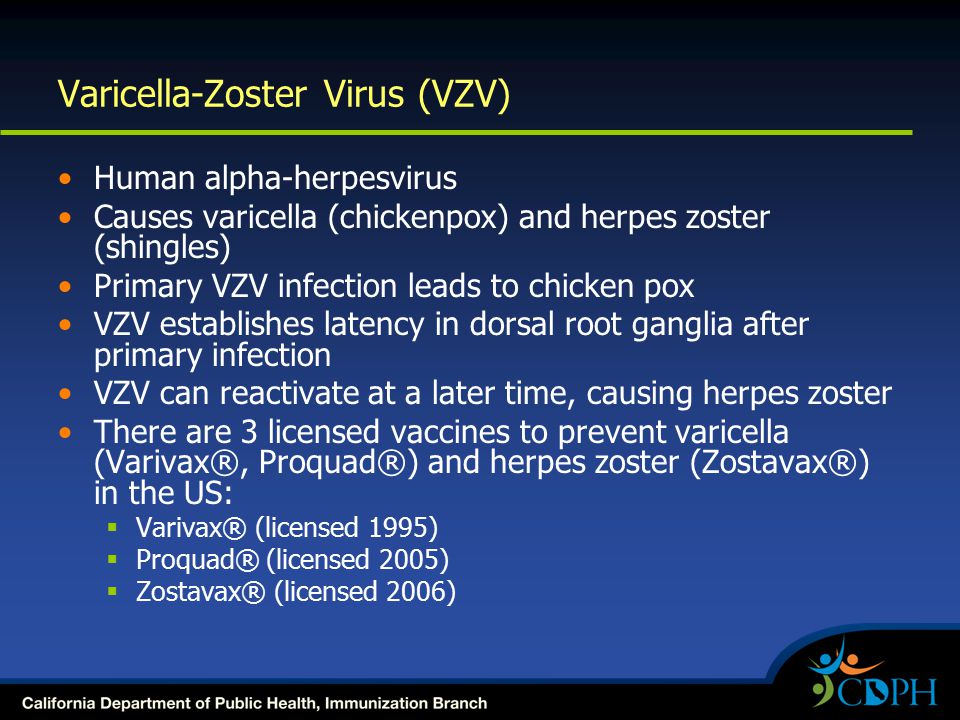 Shift in age in chickenpox. Lancet. 1993;341(8840):308–309. [PubMed] [Google Scholar]
Shift in age in chickenpox. Lancet. 1993;341(8840):308–309. [PubMed] [Google Scholar]
10. Morgan-Capner P, Crowcroft NS. Guidelines on the management of, and exposure to, rash illness in pregnancy (including consideration of relevant antibody screening programmes in pregnancy) Commun Dis Public Health. 2002;5(1):59–71. [PubMed] [Google Scholar]
11. Decline in annual incidence of varicella--selected states, 1990–2001. MMWR Morb Mortal Wkly Rep. 2003;52(37):884–885. [PubMed] [Google Scholar]
12. Kido S, Ozaki T, Asada H, Higashi K, Kondo K, Hayakawa Y, et al. Detection of varicella-zoster virus (VZV) DNA in clinical samples from patients with VZV by the polymerase chain reaction. J Clin Microbiol. 1991;29(1):76–79. [PMC free article] [PubMed] [Google Scholar]
13. Gershon AA. Varicella-zoster virus: prospects for control. Adv Pediatr Infect Dis. 1995;10:93–124. [PubMed] [Google Scholar]
14. Hall S, Maupin T, Seward J, Jumaan AO, Peterson C, Goldman G, et al. Second varicella infections: are they more common than previously thought? Pediatrics.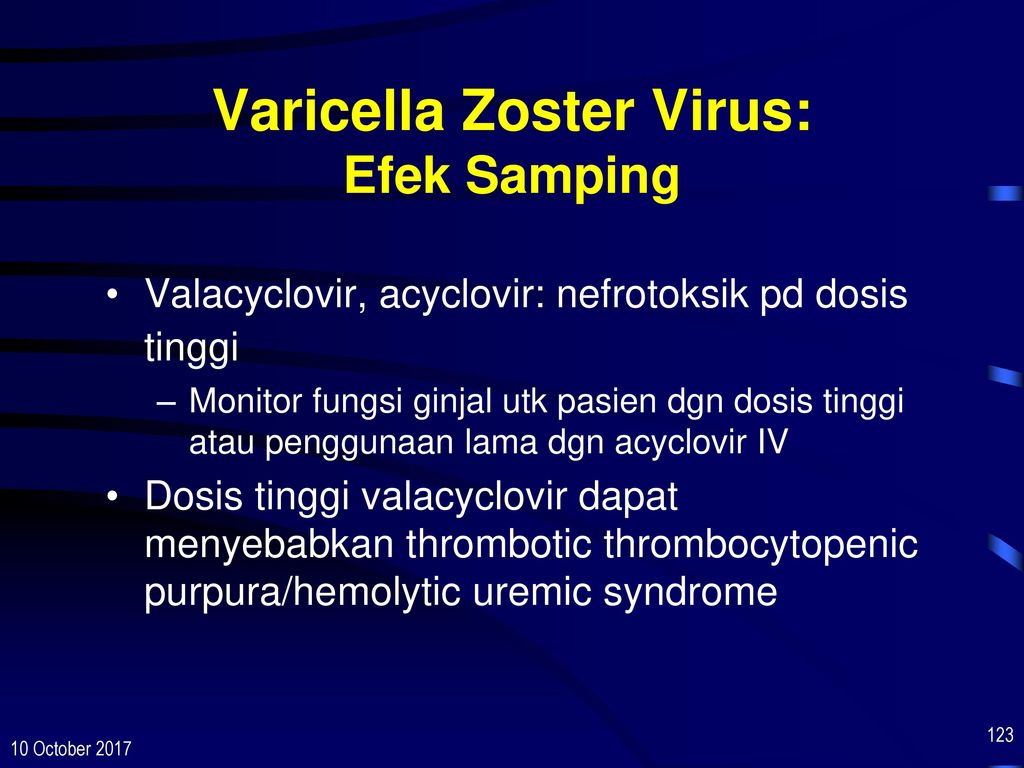 2002;109(6):1068–1073. [PubMed] [Google Scholar]
2002;109(6):1068–1073. [PubMed] [Google Scholar]
15. Paryani SG, Arvin AM. Intrauterine infection with varicella-zoster virus after maternal varicella. N Engl J Med. 1986;314(24):1542–1546. [PubMed] [Google Scholar]
16. Martin KA, Junker AK, Thomas EE, Van Allen MI, Friedman JM. Occurrence of chickenpox during pregnancy in women seropositive for varicella-zoster virus. J Infect Dis. 1994;170(4):991–995. [PubMed] [Google Scholar]
17. Jones KL, Johnson KA, Chambers CD. Offspring of women infected with varicella during pregnancy: a prospective study. Teratology. 1994;49(1):29–32. [PubMed] [Google Scholar]
18. Pastuszak AL, Levy M, Schick B, Zuber C, Feldkamp M, Gladstone J, et al. Outcome after maternal varicella infection in the first 20 weeks of pregnancy. N Engl J Med. 1994;330(13):901–905. [PubMed] [Google Scholar]
19. Siegel M. Congenital malformations following chickenpox, measles, mumps, and hepatitis. Results of a cohort study. JAMA. 1973;226(13):1521–1524. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
20. Sauerbrei A, Wutzler P. Varicella-Zoster Virus Infections During Pregnancy: Epidemiology, Clinical Symptoms, Diagnosis, Prevention and Therapy. Current Pediatric Reviews. 2005;1:205–215. [Google Scholar]
21. Sauerbrei A, Wutzler P. Das fetale Varizellen-syndrome. Monatsschrift Kinderheilkunde. 2003;151:209–213. [Google Scholar]
22. Birthistle K, Carrington D. Fetal varicella syndrome--a reappraisal of the literature. A review prepared for the UK Advisory Group on Chickenpox on behalf of the British Society for the Study of Infection. J Infect. 1998;36 (Suppl 1):25–29. [PubMed] [Google Scholar]
23. Schulze A, Dietzsch HJ. The natural history of varicella embryopathy: a 25-year follow-up. J Pediatr. 2000;137(6):871–874. [PubMed] [Google Scholar]
24. Prober CG, Gershon AA, Grose C, McCracken GH, Jr, Nelson JD. Consensus: varicella-zoster infections in pregnancy and the perinatal period. Pediatr Infect Dis J. 1990;9(12):865–869. [PubMed] [Google Scholar]
25. Tan MP, Koren G. Chickenpox in pregnancy: revisited. Reprod Toxicol. 2006;21(4):410–420. [PubMed] [Google Scholar]
Tan MP, Koren G. Chickenpox in pregnancy: revisited. Reprod Toxicol. 2006;21(4):410–420. [PubMed] [Google Scholar]
26. Cotlier E. Congenital varicella cataract 1. Am J Ophthalmol. 1978;86(5):627–629. [PubMed] [Google Scholar]
27. Scheffer IE, Baraitser M, Brett EM. Severe microcephaly associated with congenital varicella infection 1. Dev Med Child Neurol. 1991;33(10):916–920. [PubMed] [Google Scholar]
28. Andreou A, Basiakos H, Hatzikoumi I, Lazarides A. Fetal varicella syndrome with manifestations limited to the eye 1. Am J Perinatol. 1995;12(5):347–348. [PubMed] [Google Scholar]
29. Mattson SN, Jones KL, Gramling LJ, Schonfeld AM, Riley EP, Harris JA, et al. Neurodevelopmental follow-up of children of women infected with varicella during pregnancy: a prospective study 1. Pediatr Infect Dis J. 2003;22(9):819–823. [PubMed] [Google Scholar]
30. Higa K, Dan K, Manabe H. Varicella-zoster virus infections during pregnancy: hypothesis concerning the mechanisms of congenital malformations. Obstet Gynecol. 1987;69(2):214–222. [PubMed] [Google Scholar]
Obstet Gynecol. 1987;69(2):214–222. [PubMed] [Google Scholar]
31. Grose C. Congenital varicella-zoster virus infection and the failure to establish virus-specific cell-mediated immunity. Mol Biol Med. 1989;6(5):453–462. [PubMed] [Google Scholar]
32. Mustonen K, Mustakangas P, Valanne L, Professor MH, Koskiniemi M. Congenital varicella-zoster virus infection after maternal subclinical infection: clinical and neuropathological findings. J Perinatol. 2001;21(2):141–146. [PubMed] [Google Scholar]
33. Alkalay AL, Pomerance JJ, Rimoin DL. Fetal varicella syndrome. J Pediatr. 1987;111(3):320–323. [PubMed] [Google Scholar]
34. Enders G, Miller E, Cradock-Watson J, Bolley I, Ridehalgh M. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 1994;343(8912):1548–1551. [PubMed] [Google Scholar]
35. Sauerbrei A, Muller D, Eichhorn U, Wutzler P. Detection of varicella-zoster virus in congenital varicella syndrome: a case report 1.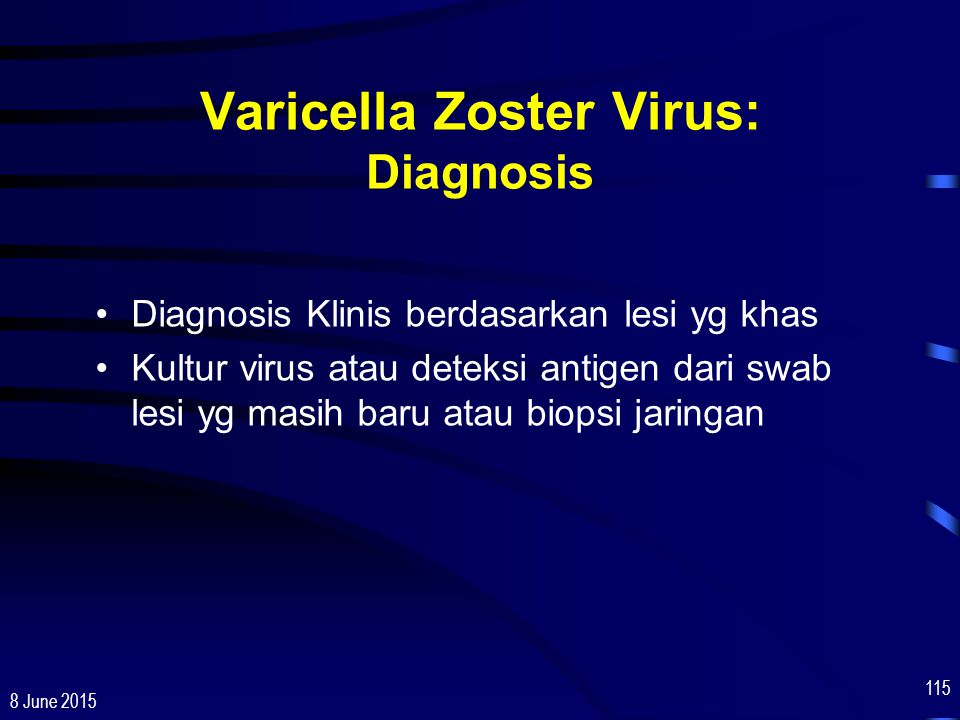 Obstet Gynecol. 1996;88(4 Pt 2):687–689. [PubMed] [Google Scholar]
Obstet Gynecol. 1996;88(4 Pt 2):687–689. [PubMed] [Google Scholar]
36. Johansson AB, Rassart A, Blum D, Van BD, Liesnard C. Lower-limb hypoplasia due to intrauterine infection with herpes simplex virus type 2: possible confusion with intrauterine varicella-zoster syndrome. Clin Infect Dis. 2004;38(7):e57–e62. [PubMed] [Google Scholar]
37. Koskimies O, Lapinleimu K, Saxen L. Infections and other maternal factors as risk indicators for congenital malformations: a case-control study with paired serum samples 1. Pediatrics. 1978;61(6):832–837. [PubMed] [Google Scholar]
38. Sauerbrei A, Gluck B, Jung K, Bittrich H, Wutzler P. Congenital skin lesions caused by intrauterine infection with coxsackievirus B3 1. Infection. 2000;28(5):326–328. [PubMed] [Google Scholar]
39. Al-Katawee YA, Al-Hasoun YA, Taha MN, Al-Moslem K. Congenital varicella-zoster virus infection. A rare case of severe brainand ocular malformations without limb or cutaneous involvement in a newborn after maternal subclinical infection 1. Saudi Med J. 2005;26(5):869–871. [PubMed] [Google Scholar]
Saudi Med J. 2005;26(5):869–871. [PubMed] [Google Scholar]
40. Kerkering KW. Abnormal cry and intracranial calcifications: clues to the diagnosis of fetal varicella-zoster syndrome. J Perinatol. 2001;21(2):131–135. [PubMed] [Google Scholar]
41. Bruder E, Ersch J, Hebisch G, Ehrbar T, Klimkait T, Stallmach T. Fetal varicella syndrome: disruption of neural development and persistent inflammation of non-neural tissues 1. Virchows Arch. 2000;437(4):440–444. [PubMed] [Google Scholar]
42. Petignat P, Vial Y, Laurini R, Hohlfeld P. Fetal varicella-herpes zoster syndrome in early pregnancy: ultrasonographic and morphological correlation 1. Prenat Diagn. 2001;21(2):121–124. [PubMed] [Google Scholar]
43. Pretorius DH, Hayward I, Jones KL, Stamm E. Sonographic evaluation of pregnancies with maternal varicella infection. J Ultrasound Med. 1992;11(9):459–463. [PubMed] [Google Scholar]
44. Sauerbrei A, Wutzler P. The congenital varicella syndrome. J Perinatol. 2000;20(8 Pt 1):548–554.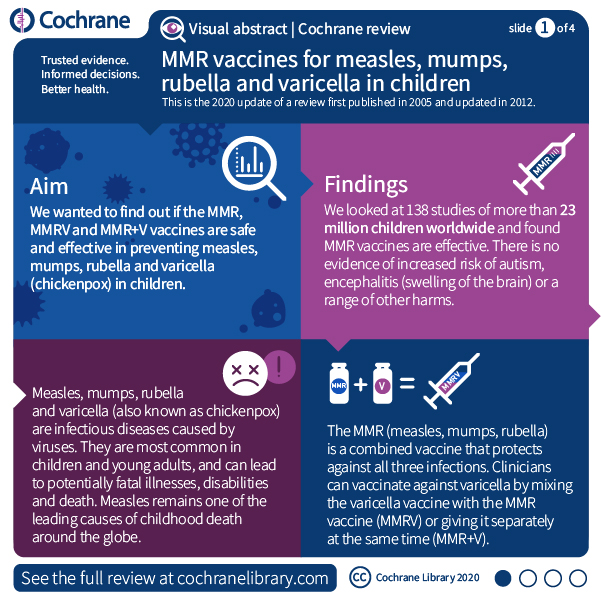 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
45. Miller E, Cradock-Watson JE, Ridehalgh MK. Outcome in newborn babies given anti-varicella-zoster immunoglobulin after perinatal maternal infection with varicella-zoster virus. Lancet. 1989;2(8659):371–373. [PubMed] [Google Scholar]
46. Sever J, White LR. Intrauterine viral infections 3. Annu Rev Med. 1968;19:471–486. [PubMed] [Google Scholar]
47. Miller E, Marshall R, Vurdien J. Epidemiology, outcome and control of varicella-zoster infection. Rev Med Microbiol. 1993;4(4):222–230. [Google Scholar]
48. Centers for Disease Control and Prevention. Varicella-related deaths among adults--United States, 1997. MMWR Morb Mortal Wkly Rep. 1997;46(19):409–412. [PubMed] [Google Scholar]
49. Gardella C, Brown ZA. Managing varicella zoster infection in pregnancy. Cleve Clin J Med. 2007;74(4):290–296. [PubMed] [Google Scholar]
50. Rawson H, Crampin A, Noah N. Deaths from chickenpox in England and Wales 1995–7: analysis of routine mortality data. BMJ. 2001;323(7321):1091–1093. [PMC free article] [PubMed] [Google Scholar]
BMJ. 2001;323(7321):1091–1093. [PMC free article] [PubMed] [Google Scholar]
51. Cox SM, Cunningham FG, Luby J. Management of varicella pneumonia complicating pregnancy. Am J Perinatol. 1990;7(4):300–301. [PubMed] [Google Scholar]
52. Greffe BS, Dooley SL, Deddish RB, Krasny HC. Transplacental passage of acyclovir. J Pediatr. 1986;108(6):1020–1021. [PubMed] [Google Scholar]
53. Landsberger EJ, Hager WD, Grossman JH., III Successful management of varicella pneumonia complicating pregnancy. A report of three cases. J Reprod Med. 1986;31(5):311–314. [PubMed] [Google Scholar]
54. Sauerbrei A, Wutzler P. Neonatal varicella. J Perinatol. 2001;21(8):545–549. [PubMed] [Google Scholar]
55. Chandra PC, Patel H, Schiavello HJ, Briggs SL. Successful pregnancy outcome after complicated varicella pneumonia. Obstet Gynecol. 1998;92(4 Pt 2):680–682. [PubMed] [Google Scholar]
56. Harger JH, Ernest JM, Thurnau GR, Moawad A, Momirova V, Landon MB, et al. Risk factors and outcome of varicella-zoster virus pneumonia in pregnant women. J Infect Dis. 2002;185(4):422–427. [PubMed] [Google Scholar]
J Infect Dis. 2002;185(4):422–427. [PubMed] [Google Scholar]
57. Schutte TJ, Rogers LC, Copas PR. Varicella pneumonia complicating pregnancy: a report of seven cases. Infect Dis Obstet Gynecol. 1996;4(6):338–346. [PMC free article] [PubMed] [Google Scholar]
58. Royal College of Obstetricians and Gynaecologists. Green-top Guideline No. 13. London: Royal College of Obstetricians and Gynaecologists; 2010. Chickenpox in Pregnancy; pp. 1–11. Ref Type: Report. [Google Scholar]
59. Nathwani D, Maclean A, Conway S, Carrington D. Varicella infections in pregnancy and the newborn. A review prepared for the UK Advisory Group on Chickenpox on behalf of the British Society for the Study of Infection. JInfect. 1998;36 (Suppl 1):59–71. [PubMed] [Google Scholar]
60. EHRLICH RM, TURNER JA, CLARKE M. Neonatal varicella; a case report with isolation of the virus. J Pediatr. 1958;53(2):139–147. [PubMed] [Google Scholar]
61. Meyers JD. Congenital varicella in term infants: risk reconsidered.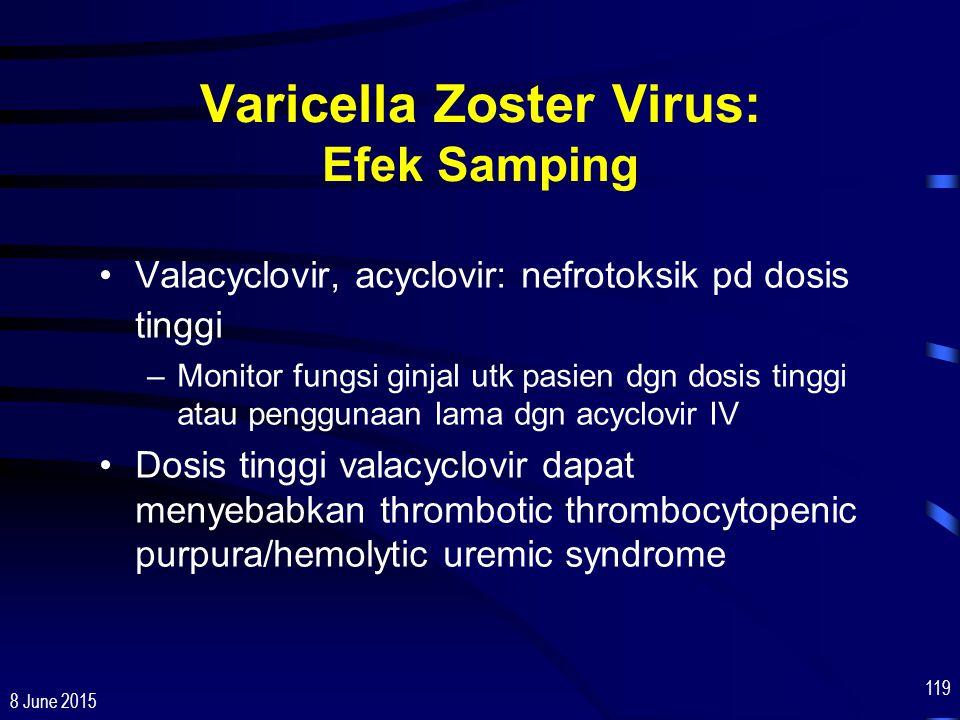 J Infect Dis. 1974;129(2):215–217. [PubMed] [Google Scholar]
J Infect Dis. 1974;129(2):215–217. [PubMed] [Google Scholar]
62. Gershon AA. Varicella in mother and infants: problems old and new. In: Krugman S, Gershon AA, editors. Infections of the fetus and the newborn infant: progress in clinical and biological research. Vol. 3. New York: Alan R Liss Inc; 1985. pp. 79–85. [Google Scholar]
63. Baba K, Yabuuchi H, Takahashi M, Ogra PL. Immunologic and epidemiologic aspects of varicella infection acquired during infancy and early childhood. J Pediatr. 1982;100(6):881–885. [PubMed] [Google Scholar]
64. Heidl M. Varicella-Zoster-Virus-Infektion in der Schwangerschaft, beim Neugeborenen und jungen Saugling. Z Klin Med. 1985;40:245–250. [Google Scholar]
65. Centers for Disease Control and Prevention. Prevention of varicella. Update recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1999;48(RR-6):1–5. [PubMed] [Google Scholar]
66. Akisu M, Yalaz M, Aksu G, Arslanoglu S, Genel F, Kutukculer N, et al.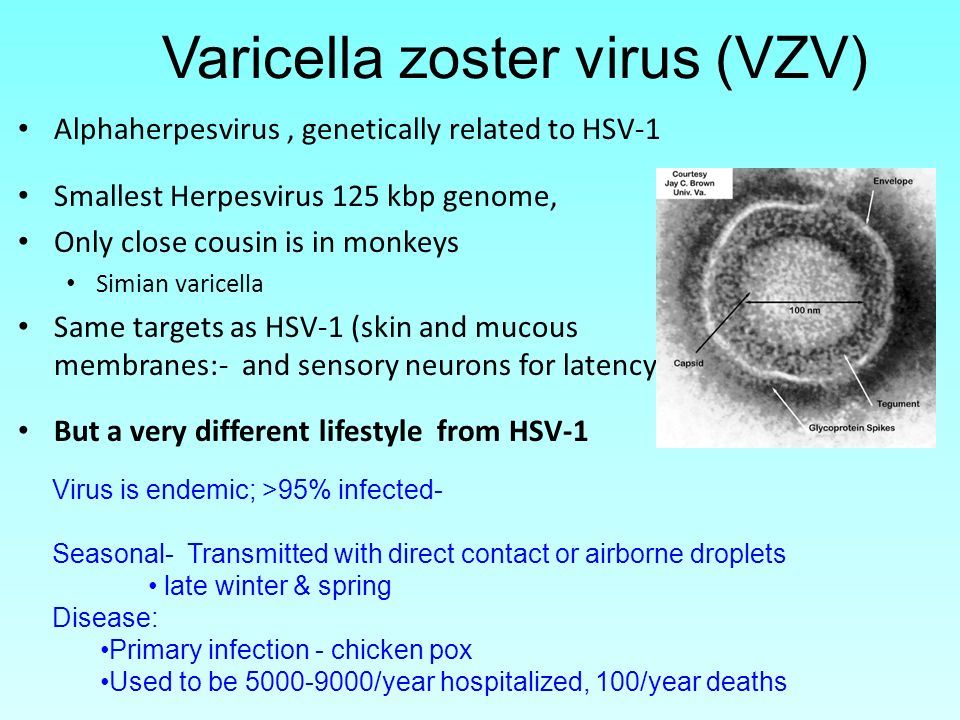 Maternally acquired varicella-zoster virus antibodies disappear at 6 months of age in prematurely born children 1. Panminerva Med. 2003;45(2):155–156. [PubMed] [Google Scholar]
Maternally acquired varicella-zoster virus antibodies disappear at 6 months of age in prematurely born children 1. Panminerva Med. 2003;45(2):155–156. [PubMed] [Google Scholar]
67. Gershon AA, Raker R, Steinberg S, Topf-Olstein B, Drusin LM. Antibody to Varicella-Zoster virus in parturient women and their offspring during the first year of life 1. Pediatrics. 1976;58(5):692–696. [PubMed] [Google Scholar]
68. Ferson MJ. Varicella vaccine in post-exposure prophylaxis. Commun Dis Intell. 2001;25(1):13–15. [PubMed] [Google Scholar]
69. Watson B, Seward J, Yang A, Witte P, Lutz J, Chan C, et al. Postexposure effectiveness of varicella vaccine. Pediatrics. 2000;105(1 Pt 1):84–88. [PubMed] [Google Scholar]
70. Centers for Disease Control and Prevention. Prevention of varicella: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Centers for Disease Control and Prevention. MMWR Recomm Rep. 1996;45(RR-11):1–36. [PubMed] [Google Scholar]
71. Australian Technical Advisory Group on Immunisation. The Australian Immunisation Handbook. 9. Canberra: Australian Government Department of Health and Ageing, Office of Health Protection; 2008. 9-4-2010. Ref Type: Report. [Google Scholar]
The Australian Immunisation Handbook. 9. Canberra: Australian Government Department of Health and Ageing, Office of Health Protection; 2008. 9-4-2010. Ref Type: Report. [Google Scholar]
72. American Academy of Pediatrics. Committee on Infectious Diseases. Varicella vaccine update. Pediatrics. 2000;105(1 Pt 1):136–141. [PubMed] [Google Scholar]
73. Shields KE, Galil K, Seward J, Sharrar RG, Cordero JF, Slater E. Varicella vaccine exposure during pregnancy: data from the first 5 years of the pregnancy registry. Obstet Gynecol. 2001;98(1):14–19. [PubMed] [Google Scholar]
74. Salzman MB, Sharrar RG, Steinberg S, LaRussa P. Transmission of varicella-vaccine virus from a healthy 12-month-old child to his pregnant mother. J Pediatr. 1997;131(1 Pt 1):151–154. [PubMed] [Google Scholar]
75. Watson B. Varicella: a vaccine preventable disease? J Infect. 2002;44(4):220–225. [PubMed] [Google Scholar]
76. Vazquez M, Shapiro ED. Varicella vaccine and infection with varicella-zoster virus.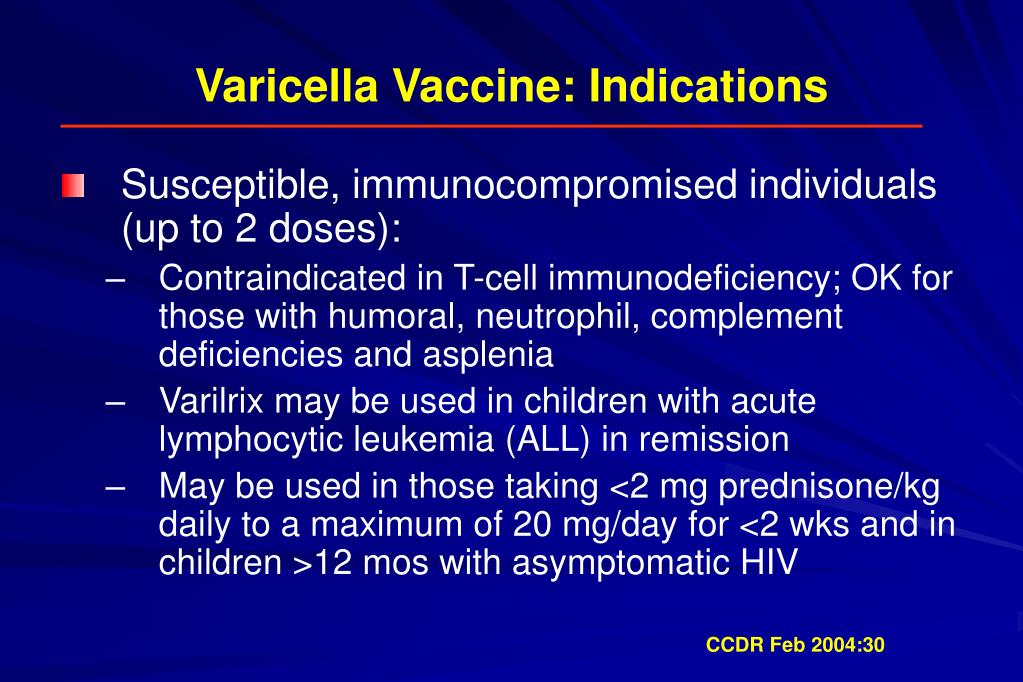 N Engl J Med. 2005;352(5):439–440. [PubMed] [Google Scholar]
N Engl J Med. 2005;352(5):439–440. [PubMed] [Google Scholar]
77. Bohlke K, Galil K, Jackson LA, Schmid DS, Starkovich P, Loparev VN, et al. Postpartum varicella vaccination: is the vaccine virus excreted in breast milk? Obstet Gynecol. 2003;102(5 Pt 1):970–977. [PubMed] [Google Scholar]
78. Dolbear GL. A pilot study: is attenuated varicella virus present in breast milk after postpartum immunization? Obstet Gynecol. 2003;101(4 suppl):47S. Ref Type: Abstract. [Google Scholar]
79. Daley AJ, Thorpe S, Garland SM. Varicella and the pregnant woman: prevention and management. Aust N Z J Obstet Gynaecol. 2008;48(1):26–33. [PubMed] [Google Scholar]
80. Smith WJ, Jackson LA, Watts DH, Koepsell TD. Prevention of chickenpox in reproductive-age women: cost-effectiveness of routine prenatal screening with postpartum vaccination of susceptibles. Obstet Gynecol. 1998;92(4 Pt 1):535–545. [PubMed] [Google Scholar]
81. Frenkel LM, Brown ZA, Bryson YJ, Corey L, Unadkat JD, Hensleigh PA, et al.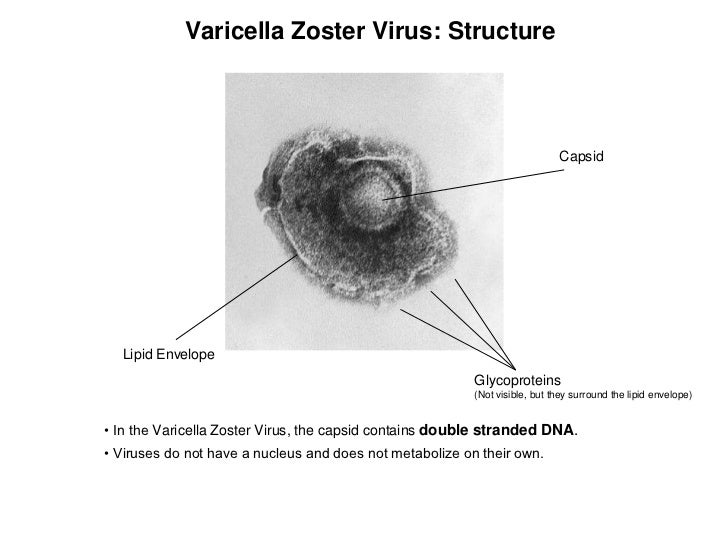 Pharmacokinetics of acyclovir in the term human pregnancy and neonate. Am J Obstet Gynecol. 1991;164(2):569–576. [PubMed] [Google Scholar]
Pharmacokinetics of acyclovir in the term human pregnancy and neonate. Am J Obstet Gynecol. 1991;164(2):569–576. [PubMed] [Google Scholar]
82. Kimberlin DF, Weller S, Whitley RJ, Andrews WW, Hauth JC, Lakeman F, et al. Pharmacokinetics of oral valacyclovir and acyclovir in late pregnancy 1. Am J Obstet Gynecol. 1998;179(4):846–851. [PubMed] [Google Scholar]
83. Beutner KR. Valacyclovir: a review of its antiviral activity, pharmacokinetic properties, and clinical efficacy 1. Antiviral Res. 1995;28(4):281–290. [PubMed] [Google Scholar]
84. Huang YC, Lin TY, Lin YJ, Lien RI, Chou YH. Prophylaxis of intravenous immunoglobulin and acyclovir in perinatal varicella 22. Eur J Pediatr. 2001;160(2):91–94. [PubMed] [Google Scholar]
85. Mori T, Komori S, Fukuda Y, Naito S, Tanaka H, Koyama K. The primary varicella infectionnear term: a case report 13. Arch Gynecol Obstet. 2003;268(2):128–130. [PubMed] [Google Scholar]
86. Suga S, Yoshikawa T, Ozaki T, Asano Y. Effect of oral acyclovir against primary and secondary viraemia in incubation period of varicella 2.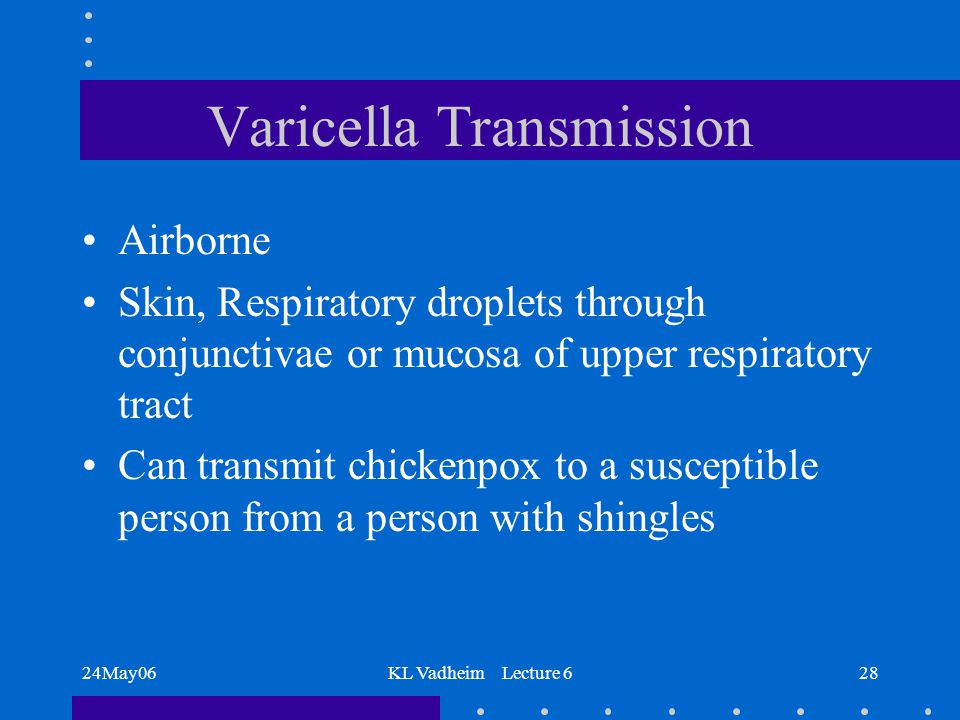 Arch Dis Child. 1993;69(6):639–642. [PMC free article] [PubMed] [Google Scholar]
Arch Dis Child. 1993;69(6):639–642. [PMC free article] [PubMed] [Google Scholar]
87. Wallace MR, Bowler WA, Murray NB, Brodine SK, Oldfield EC., III Treatment of adult varicella with oral acyclovir. A randomized, placebo-controlled trial 2. Ann Intern Med. 1992;117(5):358–363. [PubMed] [Google Scholar]
88. Mohsen AH, McKendrick M. Varicella pneumonia in adults. Eur Respir J. 2003;21(5):886–891. [PubMed] [Google Scholar]
89. Smego RA, Jr, Asperilla MO. Use of acyclovir for varicella pneumonia during pregnancy. Obstet Gynecol. 1991;78(6):1112–1116. [PubMed] [Google Scholar]
90. Haddad J, Simeoni U, Paira M, Lokiec F, Messer J, Willard D. [Transplacentalpassage of acyclovir] 1. Presse Med. 1987;16(37):1864. [PubMed] [Google Scholar]
91. Ogilvie MM. Antiviral prophylaxis and treatment in chickenpox. A review prepared for the UK Advisory Group on Chickenpox on behalf of the British Society for the Study of Infection. J Infect. 1998;36 (Suppl 1):31–38. [PubMed] [Google Scholar]
92. McIntosh D, Isaacs D. Varicella zoster virus infection in pregnancy. Arch Dis Child. 1993;68(1 Spec):1–2. [PMC free article] [PubMed] [Google Scholar]
McIntosh D, Isaacs D. Varicella zoster virus infection in pregnancy. Arch Dis Child. 1993;68(1 Spec):1–2. [PMC free article] [PubMed] [Google Scholar]
93. Sauerbrei A, Pawlak J, Luger C, Wutzler P. Intracerebral varicella-zoster virus reactivation in congenital varicella syndrome 1. Dev Med Child Neurol. 2003;45(12):837–840. [PubMed] [Google Scholar]
94. Schulze-Oechtering F, Roth B, Enders G, Grosser R. [Congenital varicella syndrome -is it infectious?] 5. Z Geburtshilfe Neonatol. 2004;208(1):25–28. [PubMed] [Google Scholar]
95. Ratanajamit C, Vinther SM, Jepsen P, Chongsuvivatwong V, Olsen J, Sorensen HT. Adverse pregnancy outcome in women exposed to acyclovir during pregnancy: a population-based observational study 8. Scand J Infect Dis. 2003;35(4):255–259. [PubMed] [Google Scholar]
96. Stone KM, Reiff-Eldridge R, White AD, Cordero JF, Brown Z, Alexander ER, et al. Pregnancy outcomes following systemic prenatal acyclovir exposure: Conclusions from the international acyclovir pregnancy registry, 1984–1999 1.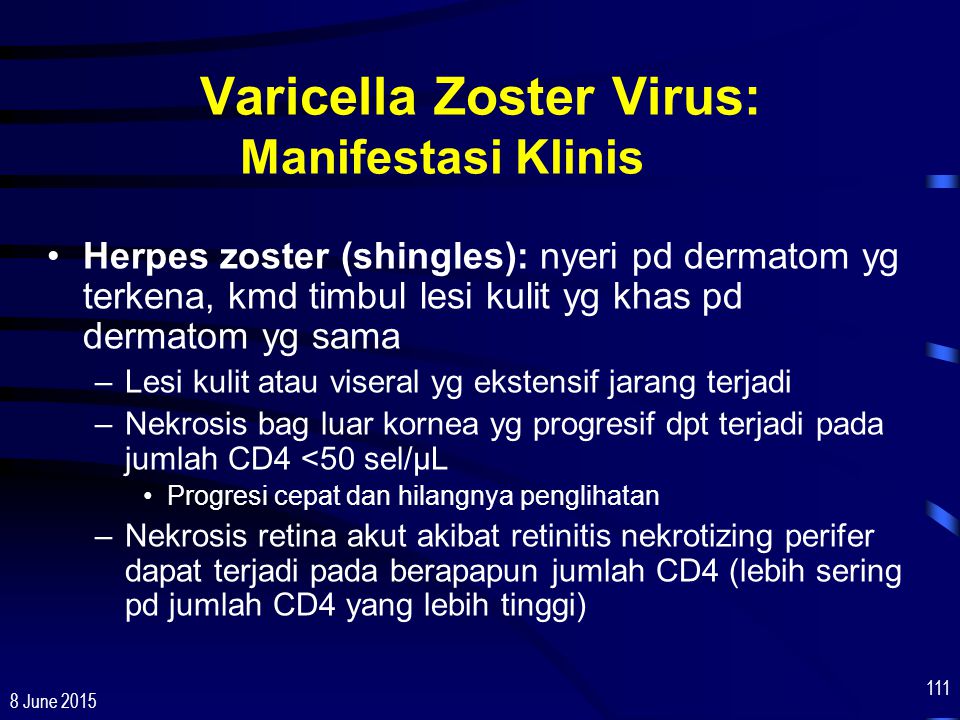 Birth Defects Res A Clin Mol Teratol. 2004;70(4):201–207. [PubMed] [Google Scholar]
Birth Defects Res A Clin Mol Teratol. 2004;70(4):201–207. [PubMed] [Google Scholar]
97. Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Frenkel LM, Gruber WC, et al. Natural history of neonatal herpes simplex virus infections in the acyclovir era 1. Pediatrics. 2001;108(2):223–229. [PubMed] [Google Scholar]
98. Sheffield JS, Hill JB, Hollier LM, Laibl VR, Roberts SW, Sanchez PJ, et al. Valacyclovir prophylaxis to prevent recurrent herpes at delivery: a randomized clinical trial 1. Obstet Gynecol. 2006;108(1):141–147. [PubMed] [Google Scholar]
99. Tyring SK, Baker D, Snowden W. Valacyclovir for herpes simplex virus infection: long-term safety and sustained efficacy after 20 years’ experience with acyclovir 1. J Infect Dis. 2002;186 (Suppl 1):S40–S46. [PubMed] [Google Scholar]
100. Brunell PA, Ross A, Miller LH, Kuo B. Prevention of varicella by zoster immune globulin 1. N Engl J Med. 1969;280(22):1191–1194. [PubMed] [Google Scholar]
101. Heuchan AM, Isaacs D. The management of varicella-zoster virus exposure and infection in pregnancy and the newborn period.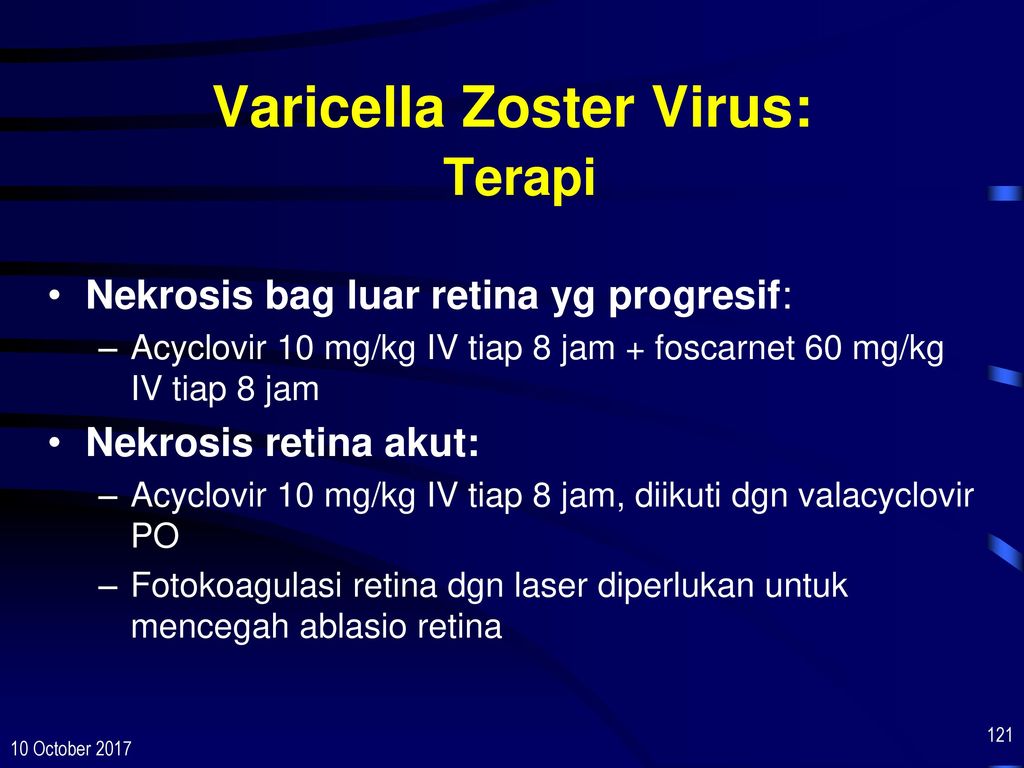 Australasian Subgroup in Paediatric Infectious Diseases of the Australasian Society for Infectious Diseases 1. Med J Aust. 2001;174(6):288–292. [PubMed] [Google Scholar]
Australasian Subgroup in Paediatric Infectious Diseases of the Australasian Society for Infectious Diseases 1. Med J Aust. 2001;174(6):288–292. [PubMed] [Google Scholar]
102. Brunell PA. Varicella in pregnancy, the fetus, and the newborn: problems in management. J Infect Dis. 1992;166 (Suppl 1):S42–S47. [PubMed] [Google Scholar]
103. Grose C. Varicella vaccination of children in the United States: assessment after the first decade 1995–2005. J Clin Virol. 2005;33(2):89–95. [PubMed] [Google Scholar]
104. Salisbury D, Ramsay M, Noakes K. Immunisation Against Infectious Disease -The Green Book. 3. London: The Department of Health; 2006. [Google Scholar]
105. Grose C. Varicella infection during pregnancy. Herpes. 1999;6:33–37. [Google Scholar]
106. Centers for Disease Control and Prevention. A new product (VariZIG) for postexposure prophylaxis of varicella available under an investigational new drug application expanded access protocol. MMWR Morb Mortal Wkly Rep. 2006;55(8):209–210. [PubMed] [Google Scholar]
2006;55(8):209–210. [PubMed] [Google Scholar]
107. Sauerbrei A, Wutzler P. Herpes simplex and varicella-zoster virus infections during pregnancy: current concepts of prevention, diagnosis and therapy. Part 2: Varicella-zoster virus infections. Med Microbiol Immunol. 2007;196(2):95–102. [PubMed] [Google Scholar]
108. Koren G, Money D, Boucher M, Aoki F, Petric M, Innocencion G, et al. Serum concentrations, efficacy, and safety of a new, intravenously administered varicella zoster immune globulin in pregnant women. J Clin Pharmacol. 2002;42(3):267–274. [PubMed] [Google Scholar]
109. Carter-Spaulding DE. Varicella infection in pregnancy 1. J Obstet Gynecol Neonatal Nurs. 2001;30(6):667–673. [PubMed] [Google Scholar]
110. Paulman PM, McLellan R. Varicella during pregnancy: the timing of effective treatment 1. J Am Board Fam Pract. 1990;3(2):121–123. [PubMed] [Google Scholar]
111. Zieger W, Friese K, Weigel M, Becker KP, Melchert F. [Varicella infection at birth] 1. Z Geburtshilfe Perinatol. 1994;198(4):134–137. [PubMed] [Google Scholar]
Z Geburtshilfe Perinatol. 1994;198(4):134–137. [PubMed] [Google Scholar]
112. Brown NW, Parsons AP, Kam PC. Anaesthetic considerations in a parturient with varicella presenting for Caesarean section 1. Anaesthesia. 2003;58(11):1092–1095. [PubMed] [Google Scholar]
113. Miller E. Varicella zoster virus infection in pregnancy 1. Arch Dis Child Fetal Neonatal Ed. 1994;70(2):F157–F158. [PMC free article] [PubMed] [Google Scholar]
114. Holland P, Isaacs D, Moxon ER. Fatal neonatal varicella infection 1. Lancet. 1986;2(8516):1156. [PubMed] [Google Scholar]
115. King SM, Gorensek M, Ford-Jones EL, Read SE. Fatal varicella-zoster infection in a newborn treated with varicella-zoster immunoglobulin 1. Pediatr Infect Dis. 1986;5(5):588–589. [PubMed] [Google Scholar]
116. Lipton SV, Brunell PA. Management of varicella exposure in a neonatal intensive care unit 1. JAMA. 1989;261(12):1782–1784. [PubMed] [Google Scholar]
Questions about chickenpox during pregnancy
How dangerous is chickenpox for a pregnant woman and is it necessary to be vaccinated? Doctors of medical clinics "Art-Med" answer questions about the danger of chickenpox for pregnant women.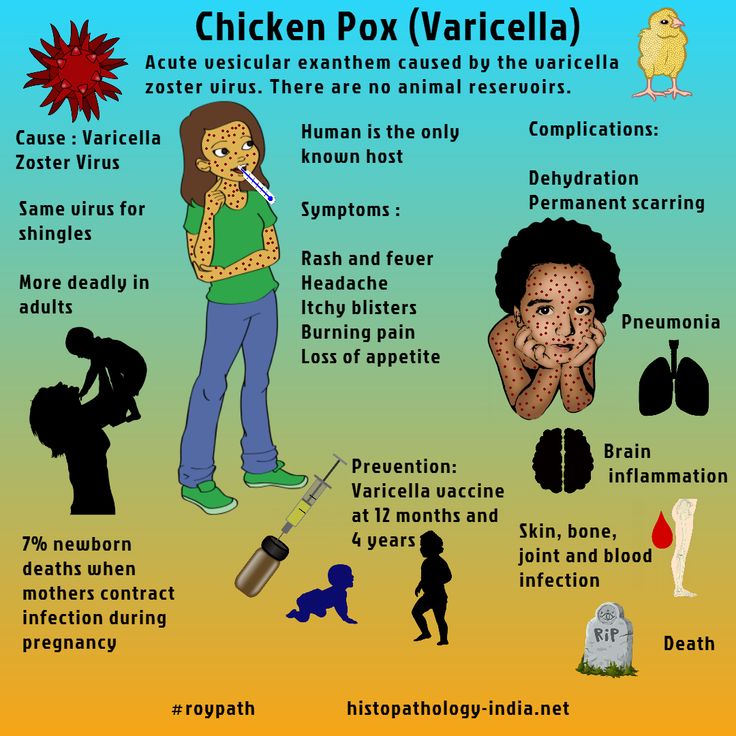
Ask a Question
Pregnancy 22-23 weeks, 4-year-old daughter fell ill with chickenpox. I didn't get chicken pox. What are the consequences for the fetus?
Since you are constantly in contact with your daughter who is already ill, it makes little sense to isolate her from you - the infection could have already occurred. Chickenpox in the middle of pregnancy does not pose a great danger to the development of the fetus.
My wife has chickenpox, she is 12-13 weeks pregnant. She had chicken pox as a child. What consequences can be for the child, if so, how to determine?
Chickenpox in the early stages of pregnancy is not an absolute indication for abortion, the probability of any damage to the fetus is usually estimated at 2-3% (some authors up to 8%) - this is a low risk.
Is there a threat to the fetus if his mother (pregnancy 3 months) communicated with a person who is in the incubation period of chickenpox, although the mother herself had chickenpox in childhood? Is a carrier of infection a person who had chickenpox in childhood, but in this period of time is in daily contact with a sick chickenpox?
1. There is no threat to the fetus. 2. No, it is not.
There is no threat to the fetus. 2. No, it is not.
I am 24 years old, 22 weeks pregnant, I got chickenpox. How will this affect the child, what pathologies can there be?
If chickenpox occurs in mid-pregnancy, the risk of adverse effects on the fetus is low, to reduce the severity of the clinical manifestations of chickenpox, discuss with your doctor the possibility of using immunoglobulin.
My twins in the garden (their group) are in chickenpox quarantine. Two children fell ill in a week, my children did not get chickenpox. I am 38 weeks and 2 days pregnant. What should I do? How dangerous is this for an unborn baby? If there was contact, are the children already infected?
You have a very ambiguous situation. If you get sick, the chances that the unborn baby will suffer greatly is very high. Therefore, if possible, completely exclude contact with twins until the end of the incubation period, do not take them to the garden, because if someone else in the group gets sick, the incubation period will be extended. Then it will be dangerous for you to return home with a newborn. If the babies do not get sick within two days, consider that you and your baby in utero have happily avoided chickenpox.
Then it will be dangerous for you to return home with a newborn. If the babies do not get sick within two days, consider that you and your baby in utero have happily avoided chickenpox.
My pregnancy is 24-25 weeks. The windmill has started. No temperature yet. What is the danger to the child? What research needs to be done and when?
Chicken pox in mid-pregnancy does not lead to developmental defects in the fetus, since the main organ formation has already been completed. The risk of intrauterine infection of the fetus (pneumonia) is slightly increased. The situation does not require termination of pregnancy. Regarding the need for any therapeutic measures (introduction of immunoglobulin, etc.), consult with an infectious disease specialist. The most commonly used expectant tactics, symptomatic treatment. Be sure to observe quarantine so as not to infect others, refrain from visiting the antenatal clinic and other medical centers for the next 3 weeks.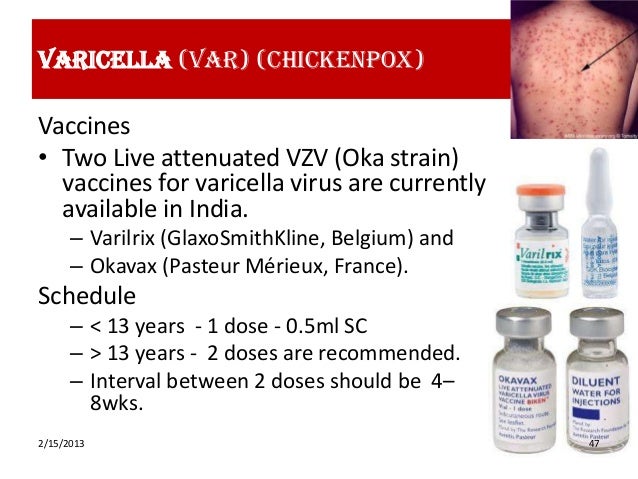
My wife fell ill with chickenpox at the 11th week of pregnancy, before that she had been on sick leave for about a month. By the time she recovered, she was already 13 weeks old. They passed the necessary blood tests from an infectious disease specialist, the tests do not predict anything bad. All doctors say to give birth, but no one has ever said about possible pathologies. What is the risk?
Chickenpox transferred in the early stages of pregnancy is not an absolute indication for termination of pregnancy, the risk of adverse effects on the fetus is present, but not high - about 2-3%. Therefore, in your case, termination of pregnancy was not offered. To exclude gross anomalies in fetal development, a standard prenatal screening program is recommended - ultrasound - 3-4 times during pregnancy, blood tests for AFP, hCG, free estriol at 16-20 weeks.
My sister got chicken pox when she was four months pregnant.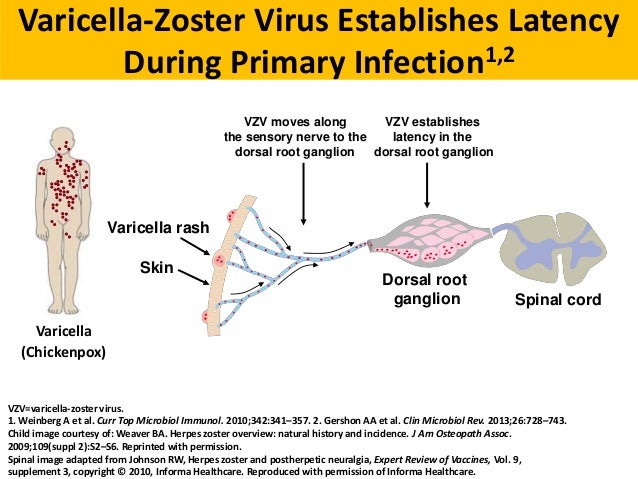 Is there a chance that the baby will be born healthy or not?
Is there a chance that the baby will be born healthy or not?
If you have had chicken pox in the second trimester of pregnancy, the likelihood of such an event remains low. Recommendations in such a situation are standard - to exclude gross anomalies in the development of the fetus, do a blood test for AFP, hCG and St. estriol at 16-20 weeks and ultrasound at 22-23 weeks of fundamental or expert level. In order not to create a threat of infecting other patients, you can contact the medical institution no earlier than 3-4 weeks after the onset of the rash.
At 17 weeks pregnant, I had contact with a recent chickenpox survivor with residual signs of the disease. I didn't get sick as a child. How big are the chances of getting sick? And is it worth it to vaccinate in this situation?
How likely you are to get chickenpox after exposure depends on your individual susceptibility to infections. Pregnant women should not be vaccinated against chickenpox. In order to prevent severe clinical manifestations, it is desirable to carry out treatment to support immunity - the introduction of specific immunoglobulin, immunocorrective drugs. To do this, I recommend contacting a virologist.
In order to prevent severe clinical manifestations, it is desirable to carry out treatment to support immunity - the introduction of specific immunoglobulin, immunocorrective drugs. To do this, I recommend contacting a virologist.
I am 32 years old, second pregnancy, 5-6 weeks. My son got chickenpox in the garden, we live together. As a child, I had chickenpox, how dangerous is it for the fetus?
Childhood varicella usually provides lifelong immunity, relapse is rare. That is, you are likely to have reliable protection against this infection. It makes no sense to carry out any quarantine measures to isolate the child - if infection were possible, then it would have already happened.
My daughter goes to kindergarten, a child in her group got chicken pox a week ago. One of these days we will go to Moscow and would like to meet our friend. She is pregnant - about 5 months. I don't know if she had chickenpox or not. My child did not have chickenpox. Do you think we can meet with our friend or is it better to wait?
My child did not have chickenpox. Do you think we can meet with our friend or is it better to wait?
If you can, please specify if your friend has had chicken pox. If not, then it is better to refrain from contact.
My wife (she is 36 years old) developed chickenpox at about the seventh week of pregnancy, she contracted it from her sick son. Information is very different both on the Internet and from doctors, including geneticists. What is the likelihood of fetal damage?
The probability of damage to the fetus is not very high - about 3.5%. A born baby may experience congenital pneumonia, and a child may also be born with a syndrome of congenital chickenpox (areas of skin scarring, hypoplasia of the bones and muscles of the limbs in the same places, neurological disorders, including mental retardation, rarely - eye damage).
Is chickenpox transmitted through objects, such as door handles, dishes? I live with my husband in the family, my husband's sister often comes to visit us, and she has one child seriously ill with chicken pox, and after 2 weeks the other fell ill.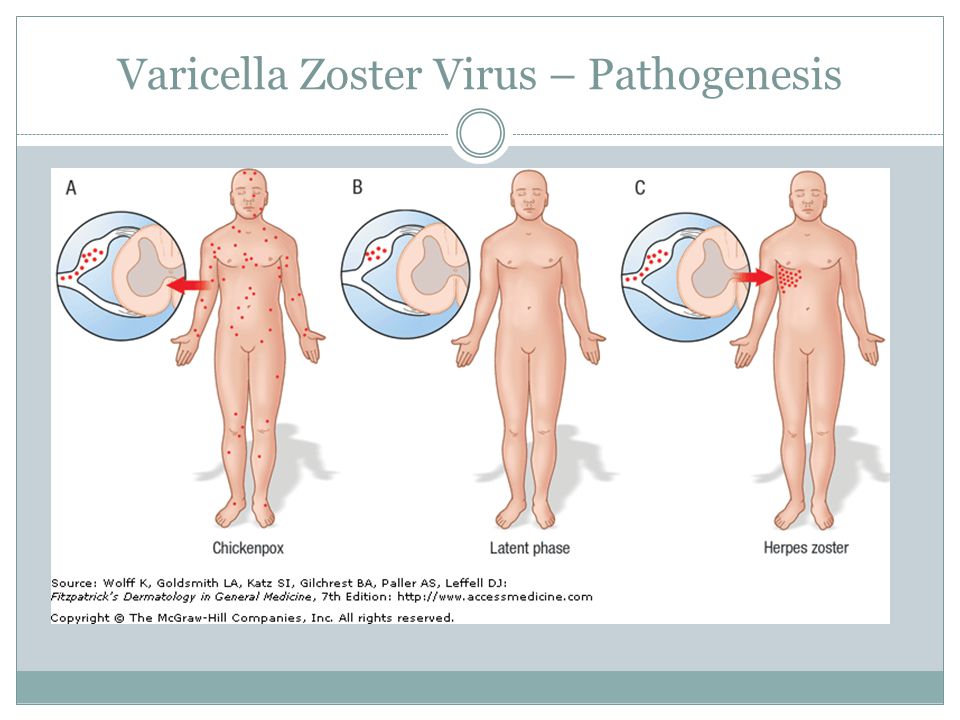 I am pregnant, the term is 6 weeks, my daughter (she is 3 years old) communicated with patients for only a couple of minutes. After that, I washed her hands and face with soap. I did not get sick in childhood, I did everything for myself and my daughter. What to do? How does chickenpox affect pregnancy?
I am pregnant, the term is 6 weeks, my daughter (she is 3 years old) communicated with patients for only a couple of minutes. After that, I washed her hands and face with soap. I did not get sick in childhood, I did everything for myself and my daughter. What to do? How does chickenpox affect pregnancy?
Chickenpox is an acute viral disease that is transmitted by airborne droplets (not through objects). The causative agent of chickenpox is unstable in the external environment and enters the body through the mucous membranes of the upper respiratory tract. The incubation period (from the moment of infection to the manifestation of the disease) lasts an average of 14 days (from 11 to 21 days). The patient is subject to isolation at home until the 5th day from the moment the last element of the rash appears. Disinfection is not carried out. Children under the age of 3 who have been in contact with a patient with chickenpox and who have not had it before are separated from the 11th to the 21st day, counting from the moment of contact.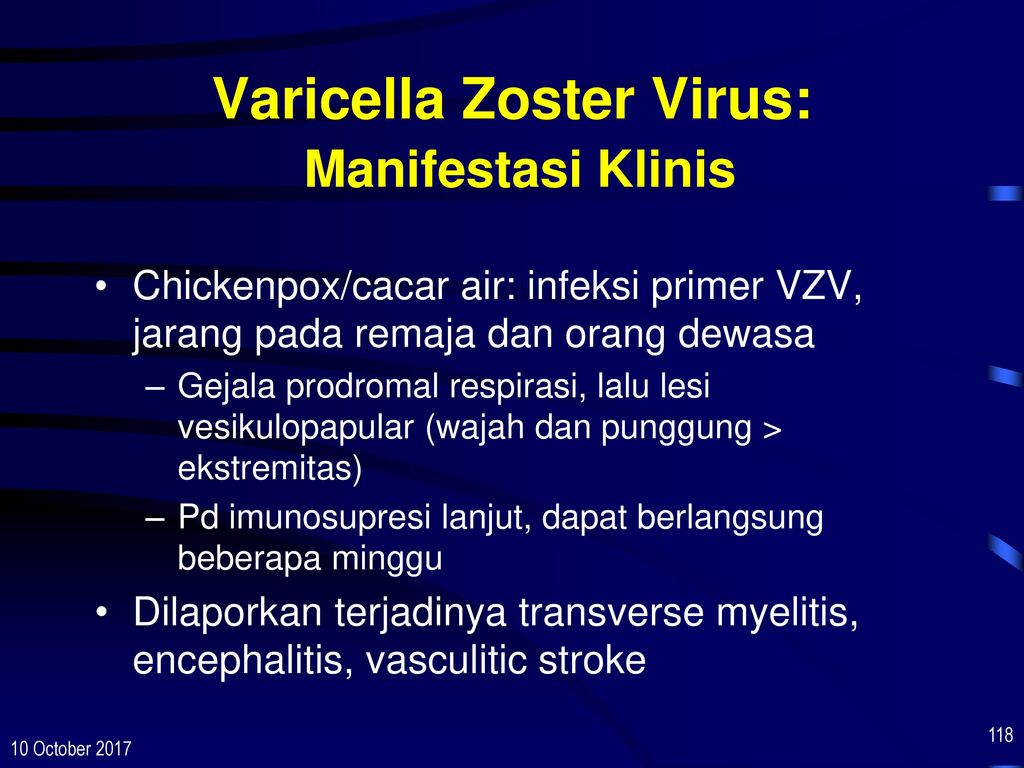 If your child did not get sick, then the infection probably did not pass on to you either. If you have any doubts, please contact your doctor for examination.
If your child did not get sick, then the infection probably did not pass on to you either. If you have any doubts, please contact your doctor for examination.
I am 17 weeks pregnant and 26 years old. At 14-15 weeks I had chicken pox. What does this mean for the child? What research needs to be done and which specialists to visit?
The varicella-zoster virus rarely causes harm to the fetus. You need to do an ultrasound at 18-24 weeks of pregnancy. Just tell the doctor about the infection, let him pay attention to the development of the bones of the skull and limbs. You can make an appointment with an obstetrician-gynecologist for a consultation and conduct examinations at the ART-MED clinic.
I am 34 weeks pregnant, I will have close contact with a child with chickenpox (rash, fever), I had chickenpox as a child, is this a threat to me and my child?
Cases of reinfection with varicella are rare, but nonetheless known. Intrauterine chickenpox transferred by the fetus can be complicated by pneumonia, neurological disorders, and even intrauterine death. Therefore, it is better not to take risks and exclude close contact with a sick child for at least 3-4 weeks.
Intrauterine chickenpox transferred by the fetus can be complicated by pneumonia, neurological disorders, and even intrauterine death. Therefore, it is better not to take risks and exclude close contact with a sick child for at least 3-4 weeks.
My wife had chickenpox when she was a child. She is pregnant at 24 weeks. Had contact with a child who has chickenpox. Can a fetus get chickenpox?
Chickenpox usually acquired during childhood provides lifelong immunity, although rare cases of recurrence are known. In your situation, short-term contact of the wife with a sick child is unlikely to lead to any adverse consequences.
I have a question for you. I am 28 weeks pregnant, I already had chickenpox as a child, an employee (we are in the same office) has a child with chickenpox at the moment. Can this affect my child, I heard that if I myself had been ill, then for me it is not dangerous, but dangerous for the fetus.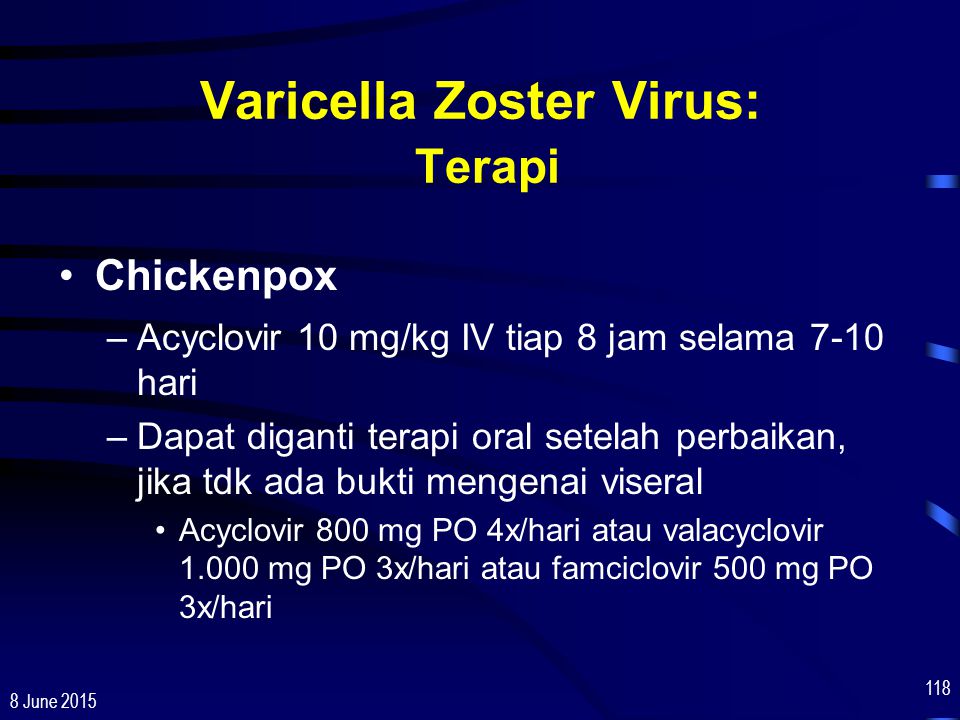 Is it true? Goodbye.
Is it true? Goodbye.
Chickenpox usually acquired in childhood gives lifelong immunity; cases of recurrence are rare. Find out if your co-worker is immune to varicella—if so, the risk to your fetus seems negligible.
I am 22 years old, at 13 weeks I got chickenpox. No temperature, only dots covered. Doctors, without really explaining anything, sent me for interruption. But I want to keep the baby. What is the percentage that he will be born healthy and what tests can be done for pathology?
The risk of damage to the fetus in case of chickenpox in the first trimester of pregnancy is at least 8%. Methods of prenatal diagnostics (ultrasound, blood tests, invasive methods) may be powerless in the search for defects in the development of the central system of the fetus, vision, hearing, immune system, etc. Doctors' recommendations for termination of pregnancy in your case seem justified. I do not invite you to a face-to-face consultation in the near future, since chickenpox is a very contagious disease and can be dangerous for other pregnant patients.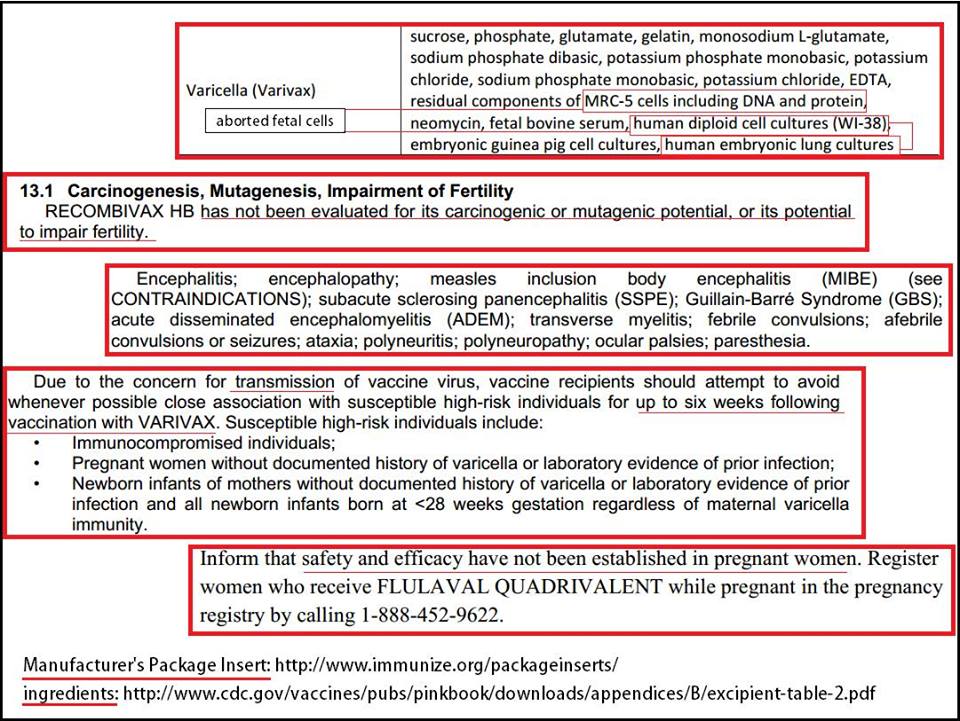 If pregnancy persists, I recommend ultrasound at 20-22 weeks, a triple test at 18-20 weeks.
If pregnancy persists, I recommend ultrasound at 20-22 weeks, a triple test at 18-20 weeks.
I am 25 years old. First pregnancy. Term 9 weeks. I got sick with chickenpox. What are the consequences of the disease?
Chicken pox at 9 weeks of pregnancy is a very unpleasant event. Although this infection is not an official indication for termination of pregnancy (as is the case with rubella), nevertheless, the risk of fetal abnormalities is estimated to be at least 8%. It is unrealistic to predict what specific problems with the development of the fetus may appear, the possibilities of prenatal diagnosis in this case are rather limited. If you are a healthy woman, and there were no problems with the onset of pregnancy, then in such a situation, you can discuss the possibility of terminating the pregnancy. I can’t invite you to a face-to-face consultation in the next month, because chickenpox is very contagious and can be dangerous for other pregnant patients. If the pregnancy persists, follow the standard screening program (“sieving”) for gross fetal developmental defects - ultrasound 3-4 times, a triple test at 16-20 weeks.
If the pregnancy persists, follow the standard screening program (“sieving”) for gross fetal developmental defects - ultrasound 3-4 times, a triple test at 16-20 weeks.
I had chickenpox as a child. Now my husband and I want to have a baby, and I'm not 100% sure that the pregnancy has not yet come, 10 more days before menstruation. Next week I will have contact with a child who has had chickenpox for a week. What is the risk of infection itself and the fetus (or complications?). Asking because I can avoid contact, but it's work.
It is generally accepted that chickenpox suffered in childhood gives a stable lifelong immunity. Although in practice rare cases of repeated infection are known. The risk of contracting chickenpox in the situation you describe is likely low. But if you are planning a pregnancy, then planned contacts with infectious patients, especially with viral infections, should be excluded. To find out about the presence of pregnancy for a period of 1-2 weeks, a blood test for hCG will help.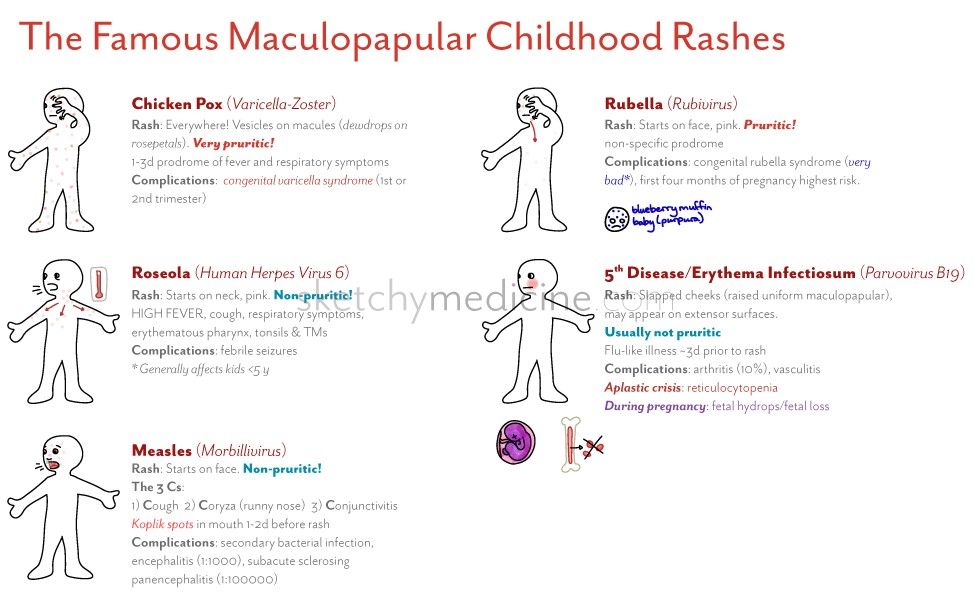
My wife is 40 weeks old and has contracted chickenpox. Characteristic Rash on the body, temperature, in general, all the symptoms of chickenpox. It is most likely that she is. Of course, we called the doctor, but I would like to know the following. What is the prognosis for chickenpox at this time, for the mother and for the fetus? What could be the consequences? What maternity hospitals with infectious diseases departments are there in Moscow? Which one is the best and what should you pay attention to when choosing such a maternity hospital?
First of all, you should finally make sure that your wife really has chicken pox. This requires consultation with an infectious disease specialist. Since the pregnancy is already full-term, it is advisable for the patient to deliver. The disease at this stage of pregnancy will most likely not have any effect on the child. It is important not to infect it after birth. In Moscow, there are only two maternity hospitals that accept patients with such infectious diseases for childbirth - the maternity hospital at the 2nd Clinical Infectious Diseases Hospital and at the 36th City Clinical Hospital.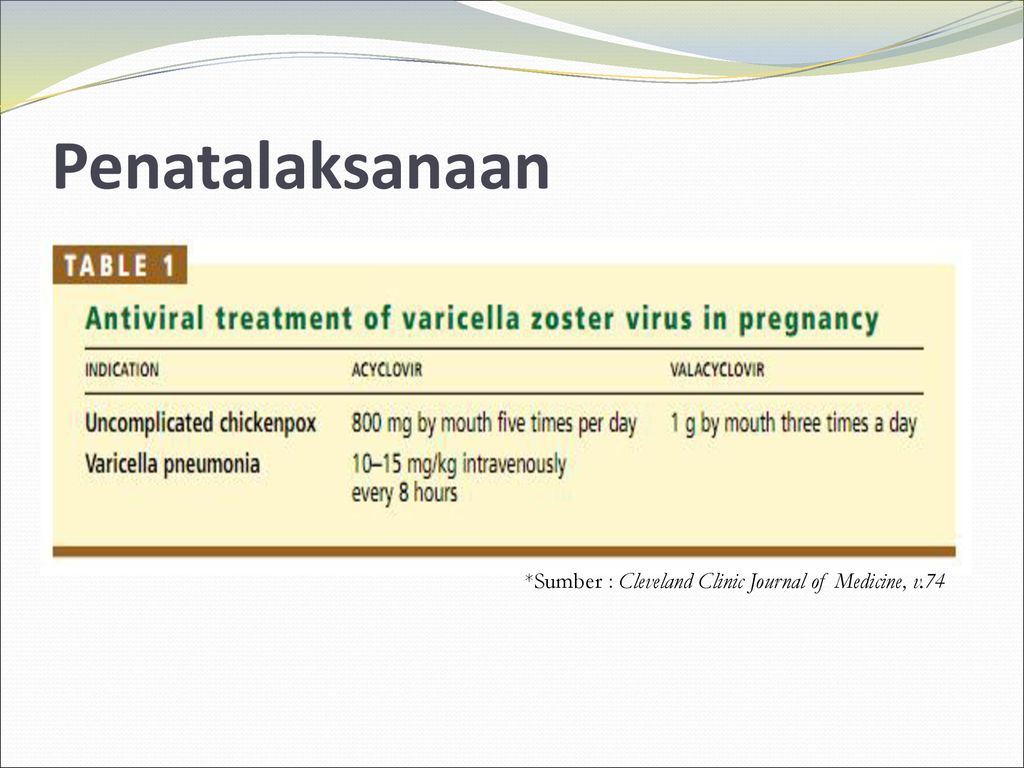 Both maternity hospitals are identical, and you should probably pay attention only to their location in relation to the location of your residence.
Both maternity hospitals are identical, and you should probably pay attention only to their location in relation to the location of your residence.
I am 30 years old, 4 weeks pregnant, diagnosed with chickenpox, temperature 38.5, itching. Is it possible to leave the fetus, what could be the consequences, if so, what medicines can be taken?
Chicken pox in such early stages of pregnancy is an unpleasant situation. Officially, this disease is not a reason for terminating a pregnancy, but the risk of fetal developmental defects, including those that are not amenable to any diagnostic methods, is usually estimated at at least 8%. To resolve this issue, it is necessary to compare the chances of being able to still have a pregnancy and the risk of anomalies in the fetus. Given that you have an infection that is dangerous for other patients, I do not invite you to a face-to-face consultation in the next month. If you keep the pregnancy, then do an ultrasound scan every 4 weeks, biochemical tests do not develop fetal defects at 10-14 weeks and 16-20 weeks.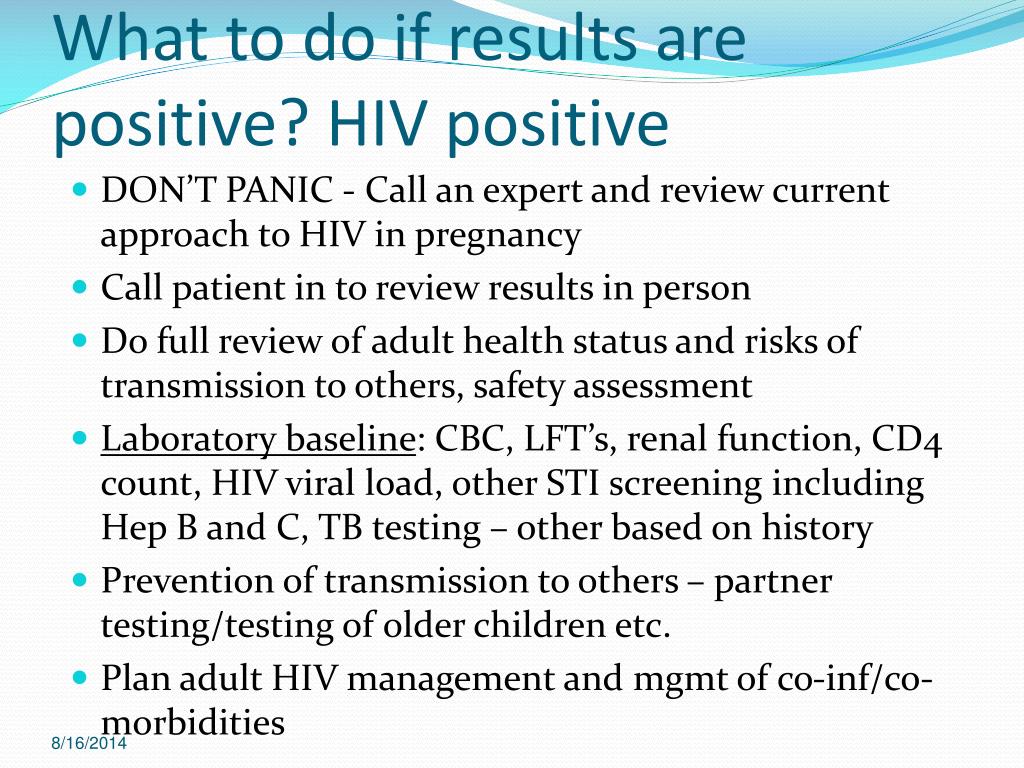
Pregnancy 10 weeks, at 6-7 weeks she had a rotovirus infection. Is it possible to find out with the help of three-dimensional ultrasound whether the disease affected the child, that is, to identify malformations?
There are not enough observations about the possibility of the impact of rotavirus infection on the growing fetus. For viral infections in early pregnancy, only for one there is a categorical recommendation for termination of pregnancy - this is rubella. For other types of viral infections (respiratory, hepatitis, CMV, herpes, chicken pox, measles), there are no such unambiguous recommendations, pregnancy is usually continued, although some risk to the fetus remains. Probably, it is better for you to consult with an infectious disease specialist at the Research Institute of Epidemiology and Microbiology. G. N. Gabrichevsky. Given the significant uncertainty in the prognosis for the fetus and the lack of reliable diagnosis of intrauterine infection with rotovirus in a woman with intact childbearing function, the possibility of abortion can be discussed. Three-dimensional ultrasound cannot reveal the entire spectrum of developmental anomalies, including damage to the organs of hearing, vision, and the immune system.
Three-dimensional ultrasound cannot reveal the entire spectrum of developmental anomalies, including damage to the organs of hearing, vision, and the immune system.
May 26 will be 36 weeks pregnant (first day of last period September 16). From 18 weeks I take ginipral and up to 36 weeks (as prescribed in the antenatal clinic) due to cramping uterine contractions and tone, as well as a slightly open cervix by 1 finger. Almost the entire pregnancy I tried to lie down, because. any action causes petrification in the abdomen. And today (May 24), my eldest daughter was diagnosed with chickenpox, I was in contact with her and now I’m horrified (I didn’t get chickenpox as a child), I don’t know what to do, because if I cancel ginipral and childbirth can come soon and plus I I can get chickenpox and a newborn (which is very dangerous) from me. Maybe you need to do a caesarean without waiting for a natural birth?
First of all, don't panic, as it won't help anyway. You need to continue treatment aimed at maintaining pregnancy and not necessarily with the help of Ginepral. This treatment should be carried out only in a hospital setting, as the risk of preterm birth remains. The threat of premature birth and the risk of getting chickenpox are not indications for a caesarean section. It is not at all necessary that you will get this disease and, moreover, it is not necessary that the newborn will suffer from this. You should completely isolate yourself from the sick eldest daughter and go to the hospital under the supervision of doctors.
You need to continue treatment aimed at maintaining pregnancy and not necessarily with the help of Ginepral. This treatment should be carried out only in a hospital setting, as the risk of preterm birth remains. The threat of premature birth and the risk of getting chickenpox are not indications for a caesarean section. It is not at all necessary that you will get this disease and, moreover, it is not necessary that the newborn will suffer from this. You should completely isolate yourself from the sick eldest daughter and go to the hospital under the supervision of doctors.
The gestational age is 34-35 weeks, the oldest child in the garden, but not in his group, has chickenpox, my son was ill with it a year ago, but I myself did not get sick in childhood. I didn’t get sick even when my son was sick, although there was close contact (and kissed him, the bubbles burst when I smeared them and the liquid from the bubbles got into my eyes). Chickenpox was severe in my son with a temperature of 38.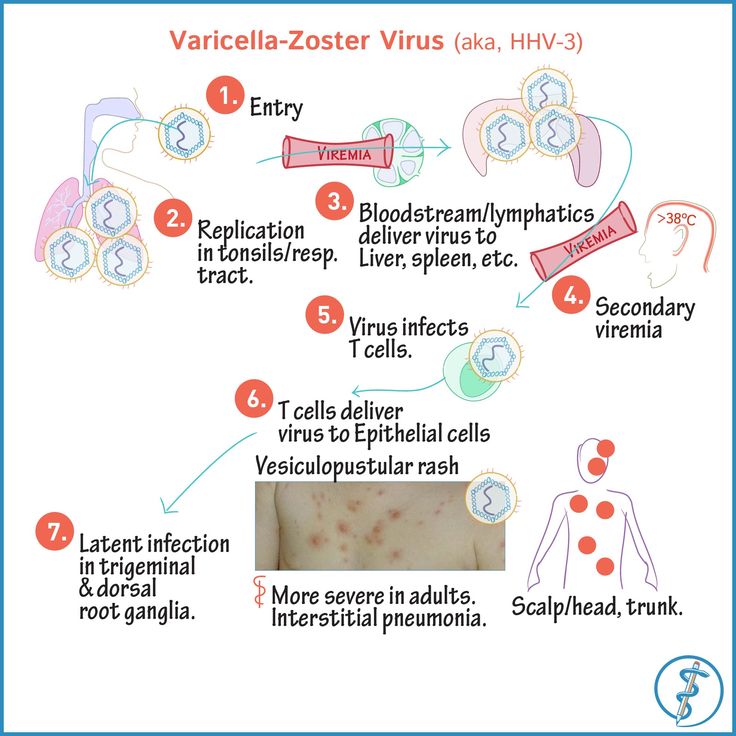 5 and a severe rash. Is chickenpox dangerous for me and for my unborn child. To take the child to the garden or not? Can I get infected if I didn't get infected through closer contact?
5 and a severe rash. Is chickenpox dangerous for me and for my unborn child. To take the child to the garden or not? Can I get infected if I didn't get infected through closer contact?
Chicken pox poses a certain risk to pregnancy. Based on the situation you presented, the probability for you to get chickenpox is no greater than for everyone else, since there is no direct contact with a child who has fallen ill in another group of kindergarten. If you still have doubts, it is better not to take your child to the kindergarten for the period of quarantine.
Chickenpox ("chickenpox"): why is this "childhood" infection dangerous for pregnant women?
| Attention, chicken pox! How to protect a pregnant woman from infection if someone in the family gets sick |
| after the last rash appeared) If someone in your family had contact with a sick person and could potentially be infected. It may manifest the first manifestations of the disease in the period from 7 to 21 days from the moment of contact with the patient. 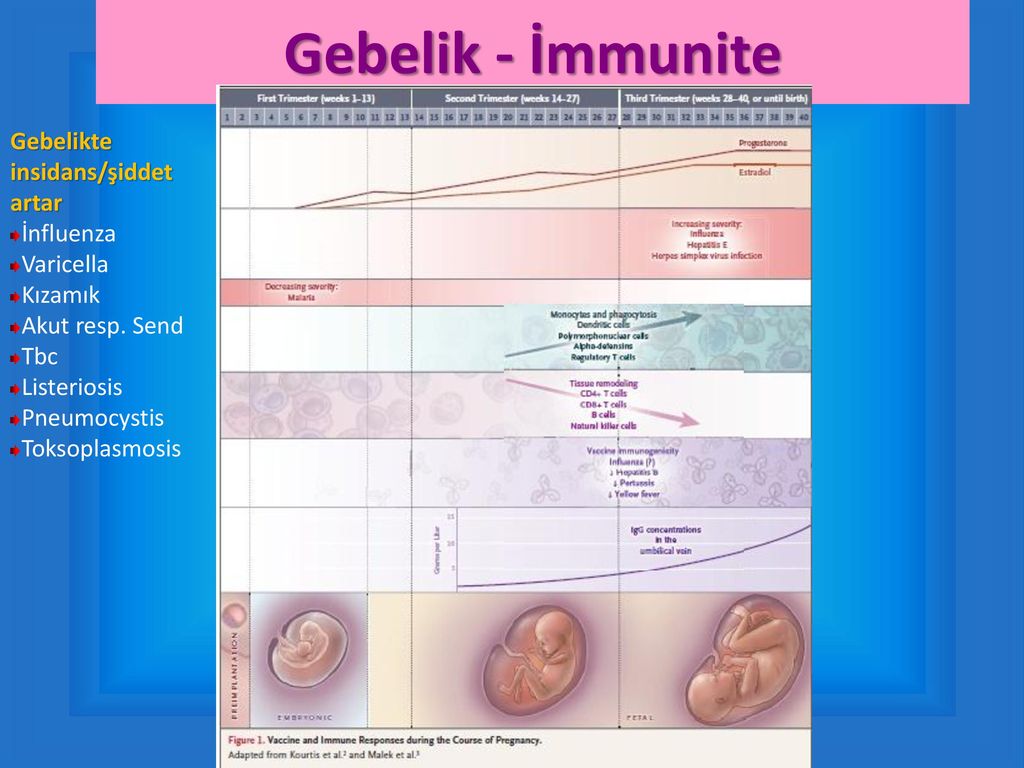 According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because in case of illness, there is a risk of infection. According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because in case of illness, there is a risk of infection. |
Varicella (chicken pox)
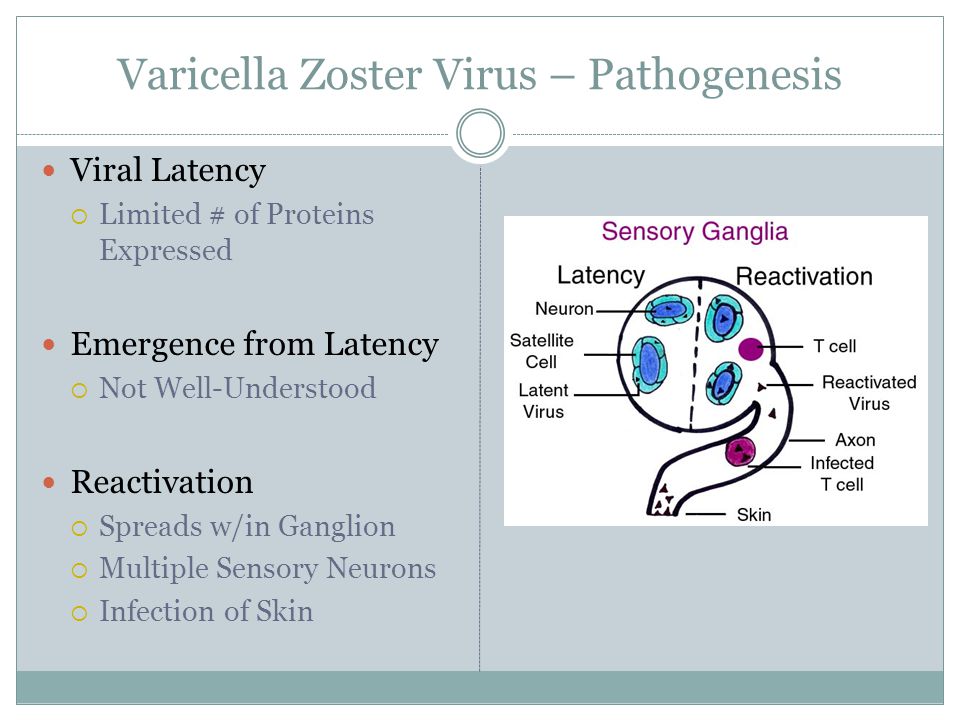
Pathogen - DNA-containing herpes virus type 3 Varicella-Zoster
Incubation period - from 7 to 17 days
Rash - appears simultaneously with an increase in temperature or several hours later. First, small spots form, which quickly turn into papules and vesicles. Vesicles are usually unicameral. Rashes are located on the skin of the trunk, face, limbs, scalp, less often on the mucous membranes of the mouth, respiratory tract, eyes, and external genitalia.
Rash may be accompanied by itching. On the mucous membranes, the elements of the rash quickly macerate with the formation of superficial erosions that heal within 1-2 days. On the skin, the bubbles gradually dry out and become covered with crusts. After exfoliation of the crusts, light pigmentation remains in their place for a long time, in rare cases - scars.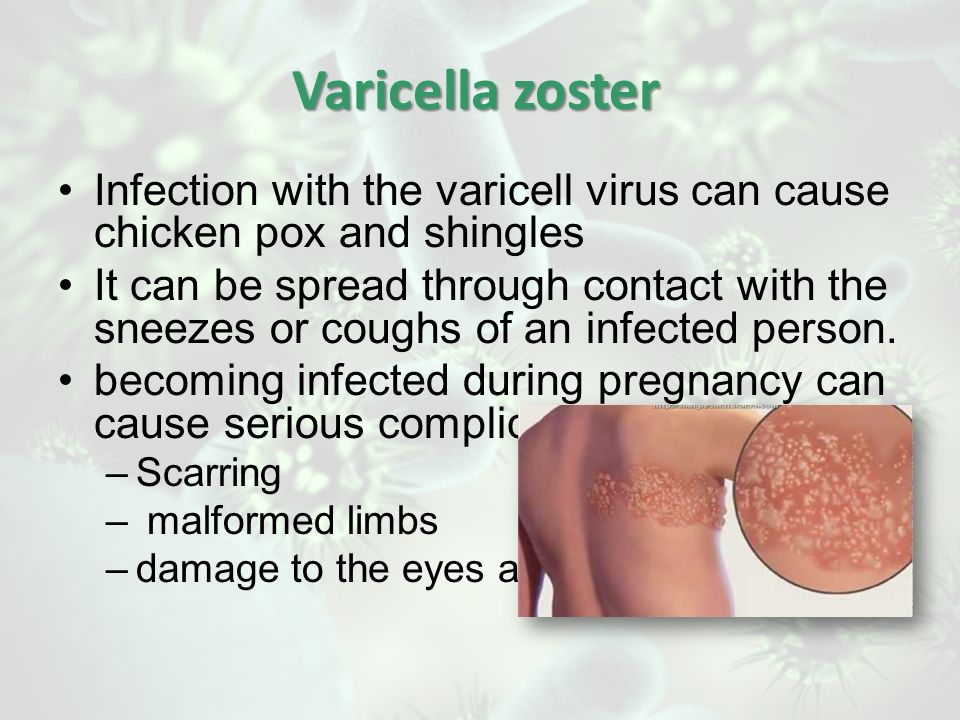 The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
There is a false polymorphism of the rash.
Infectiousness period - 10-12 days 1-2 days before the appearance of the rash, the entire period of the rash, up to 5 days after the
appearance of the last rash (blister - vesicles).
Danger for pregnant women - the most unfavorable first trimester and the last week before delivery. Fetal risk is lowest between 20 and 35 weeks. Infection of a pregnant woman in the 1st trimester may result in the death of the embryo. When infected before the 20th week of pregnancy, there is a danger of the formation of congenital vitrine syndrome. This pathology is characterized by: a violation of the normal development of the limbs, brain, organs of vision, the formation of scars on the skin, as well as a general delay in intrauterine development. A pregnant woman, who fell ill on the eve of childbirth, may have a child with chickenpox of a newborn.
In general, the pathology of pregnancy is not common, so the disease is not a direct indication for termination of pregnancy. Pregnant women must undergo prenatal screening (double and triple tests), ultrasound (especially for a period of 20-22 weeks). In some cases, a study of amniotic fluid by PCR for the presence of virus DNA in them.
Prevention - isolation of the patient up to 5 days after the last rash. Contacts up to 3 years old, not sick, are isolated from 11 to 21 days from the moment of contact. Isolation of patients for 4 days from the onset of the disease, newborns with congenital rubella ─ up to 1 year. Contacts are not allowed in children's groups for 21 days (from the moment of isolation of the patient), monitoring of contacts.
Prophylactic vaccination available. The virus persists in the body for life, but recurrence after an illness is very rare. When the virus is activated, another form of infection develops - herpes zoster (zoster).
Emergency prophylaxis on contact (if the patient has not previously been ill and has no vaccination data) - passive immunization: donor immunoglobulin 0. 2-0.5 ml / kg in the first 2 days.
2-0.5 ml / kg in the first 2 days.
Conclusion: If you have a family member with chickenpox, they need to be isolated for 10 to 12 days: 12 days before the rash appears and up to 5 days after the rash appears. To avoid infecting others, especially pregnant women, stay at home and avoid contact with anyone for six days after the rash begins to appear.
3. Visipans are located on the trunk, face, limbs, less often on the mucous membranes of the mouth, eyes, and respiratory tract.
for pregnant women!
Pregnant women must undergo prenatal screening (double and triple tests) and ultrasound (especially at 20-22 weeks).
2. Emergency prophylaxis by contact (if the patient has not been ill before and has no data on vaccinations) - passive immunization: donor immunoglobulin in the first 2 days.
How to protect a pregnant woman from
infection if someone in the family gets sick
If someone in your family had contact with a sick person and could potentially be infected.
It may manifest the first manifestations of the disease in the period from 7 to 21 days from the moment of contact with the patient. According to such a person, during this period it is also not advisable to communicate with a pregnant woman, because in case of illness, the risk of infecting others occurs 1-2 days before the
rash appears. and then the entire period of rash. According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because it is possible not to notice the early manifestations of the disease, and during this period the transmission of the infection is already potentially possible.