When is your pregnancy safe
The 12-week pregnancy rule: Why is the first trimester shrouded in secrecy?
The first trimester of pregnancy can often be the hardest.
Pregnancy hormones, extreme fatigue, nausea and vomiting, tender breasts, and perpetually needing to wee make life growing a human no easy feat.
For many women, it's made harder by an unwritten social rule that says they should keep their news quiet — at least for the first 12 weeks.
In Australia and elsewhere in the West, waiting until the end of the first trimester to announce a pregnancy is considered a social norm.
This shroud of secrecy is linked to the uncertain early weeks of a pregnancy, where the risk of miscarriage is much higher.
In Australia, up to one in four pregnancies end in miscarriage, and the expectation to remain silent in early pregnancy means many women and couples are left to grieve privately, sometimes without the support they need.
So where does the "12-week rule" come from? And why does it persist?
No 'right time' to tell
From a medical point of view, at 12 weeks a pregnancy is generally considered to be "safe".
While a miscarriage (or later, stillbirth) can happen at any point during gestation, the odds are highest in the first trimester.
Research shows at eight weeks, the chances of having a live baby are 92 per cent. At 12 weeks, those odds increase to 97 per cent.
According to Penny Sheehan, an obstetrician at the Royal Women's Hospital in Melbourne, there are no clinical guidelines stipulating when a woman should or should not announce her pregnancy.
"I've never told any woman to not tell anyone. In fact, I would usually say to share it with a support person and some close family and friends, so that you do have some support," she says.
Dr Sheehan says at 12 weeks, most women can "believe with some confidence" that their pregnancy will be ongoing.
But she says it's up to each individual (or couple) to decide when the time is right for them to share the big news.
"There is a risk of miscarriage, and if you do come out and tell people earlier, then you might be faced with the prospect of discussing that," Dr Sheehan says.
Women need support at every stage
It's a conversation Sam Rowe, 39, has had to have more than once.
"I've had one stillbirth, five miscarriages, and a chemical pregnancy. I have no living children as of today," she says.
Sam is now a passionate advocate for challenging the 12-week rule.
"Our third pregnancy was identical twin girls, who unfortunately, at 15 weeks, tangled their cords and passed away," she says.
"As it was my third pregnancy — and it was two babies — I started to become quite round quite quickly.
"I held off announcing until about 10 weeks … and it just breaks my heart because we could have had a lot longer to enjoy that happy news."
Sam says it's important women feel supported to announce their pregnancies earlier if they choose to, so that they have both an opportunity to celebrate, and to receive support in the event of a pregnancy loss.
"It doesn't matter what the gestation is that you lose [a baby]," she says.
"You didn't want that baby any less because it was six weeks or eight weeks, versus 19 weeks or 22 weeks.
"You love that baby and you wanted that baby and you're heartbroken that baby is gone."
Ultrasound makes it 'real'
The decision to wait 12 weeks before announcing a pregnancy is a relatively recent phenomenon, according to Meredith Nash, a sociologist from the University of Tasmania.
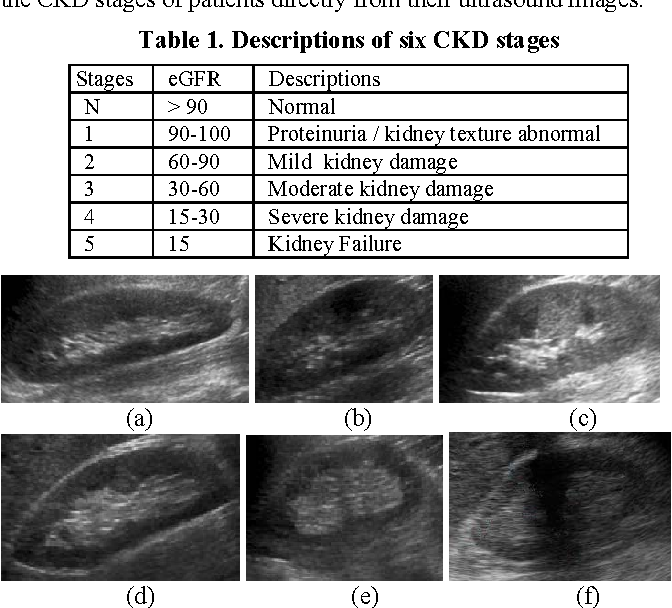
"For the most part, the 12-week rule exists because most woman have an ultrasound scan at 12 weeks," she says.
"That's really become the benchmark for women to feel like the pregnancy is real."
Dr Nash says historically, the 12-week ultrasound either did not exist or was not standard practice during pregnancy.
Instead, women would wait for the baby to move or flutter in their belly, which typically happens between 15 and 20 weeks gestation.
"Prior to ultrasound, pregnancy and foetuses were imagined. We are now a society that relies on the visual to believe that something is real and true," she says.
"Ultrasound has had a profound effect on the way that we think about foetuses, and the moment that foetus becomes a baby."
She adds that seeing the foetus on the screen for the time is an important moment for many expectant mothers.
"Even though women know they are pregnant, they often don't believe it's real until medicine tells them it's real. It's quite a recent phenomenon," she says.
Genetic screening also a factor
Medically speaking, the risk of miscarriage isn't the only reason why some women and couples choose to keep news of their pregnancy private in the first trimester.
At 12 weeks, some people may also choose to find out if their child has a genetic condition such as Down syndrome.
Tears of miscarriage: Men share their devastation and the impact of loss
Matt Whiting did not fully understand the ramifications of miscarriage before his own experience.
Dr Nash says it can be an ethical minefield.
"No pregnancy book tells you what to do in that situation," she says.
"You can get some really devastating results … I've had women in studies who have had to make life-changing decisions about how they are going to proceed with a pregnancy."
According to data from the Australian Medical Association, 80 to 90 per cent of Australian women who receive a pre-natal diagnosis of Down syndrome choose not to continue with their pregnancy.
Dr Sheehan says while miscarriage may be a topic some people are comfortable discussing with their friends and family, the decision to terminate a pregnancy is "definitely very personal".
"It's certainly not something that most people would be wanting to disclose … and that is a lot about judgement and pressure," she says.
A personal decision
Genetic testing and miscarriage aside, Dr Nash says there are a multitude of personal factors that influence a woman's decision to announce her pregnancy.
"Women will often tell one or two people, a close friend or family member, because on one level, they of course want support," she says.
"If something goes wrong in the pregnancy, or if they end up having a miscarriage, they want to be able to turn to someone and talk about it."
Anita Guyett from SANDS, a not-for-profit organisation supporting parents dealing with miscarriage, stillbirth and neonatal death, says it's important people experiencing pregnancy loss are able to properly acknowledge and deal with their grief.
"We don't do grief well at all. We tend to shy away from it, and I think communication really is the key," she says.
"It's recognising that a pregnancy did exist and recognising the hopes and dreams that you actually had for that pregnancy.
"I just think it validates that the baby existed, and it also validates the grief."
Sam says she wants women to feel empowered and able to make their own decision about when they want to announce their pregnancy — whether that's abiding by the 12-week rule or not.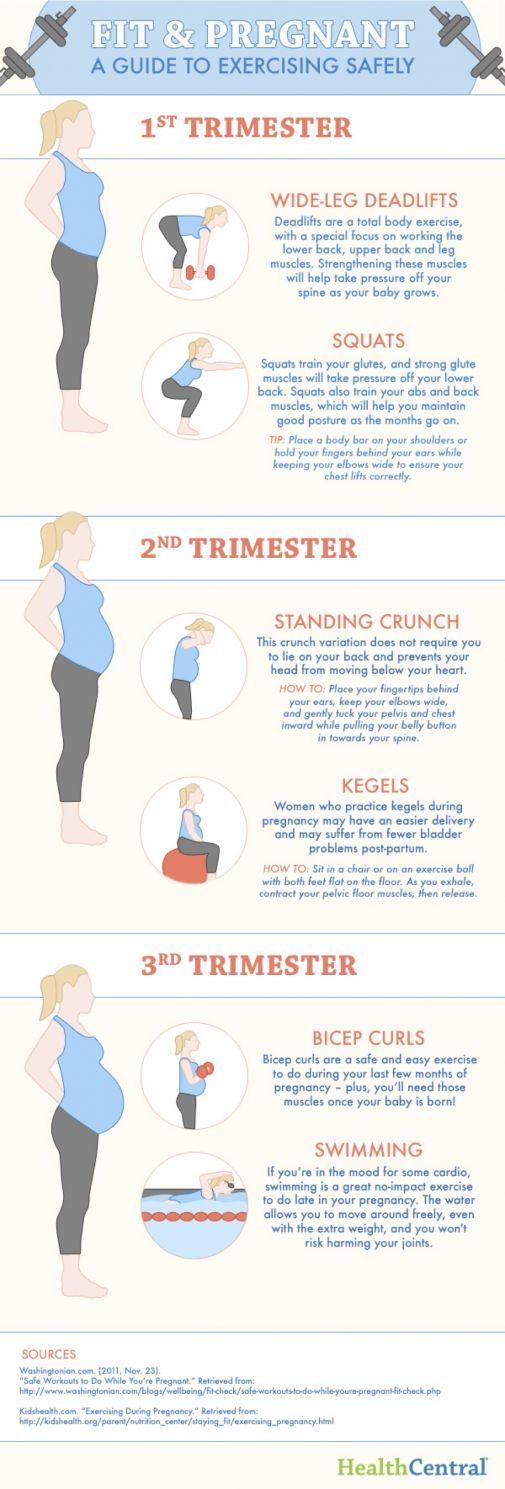
"If you want to tell at six weeks, tell. If you want to tell at 20 weeks, tell," she says.
"Whatever feels right for you is right for you."
Have you experienced pregnancy loss? What do you wish people had said or done to help you feel supported? Ladies, We Need to Talk wants to hear from you. Email [email protected]
Health in your inbox
Get the latest health news and information from across the ABC.
Email address
When Is the Best Time to Announce Pregnancy?
When Is the Best Time to Announce Pregnancy?- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Deborah Weatherspoon, Ph. D., MSN — By Ashley Marcin on December 6, 2018
D., MSN — By Ashley Marcin on December 6, 2018
Announcing your pregnancy
One of the most exciting times in your pregnancy is getting that first positive test. You probably want to tell the whole world you’re expecting. But when is the best time to announce your pregnancy?
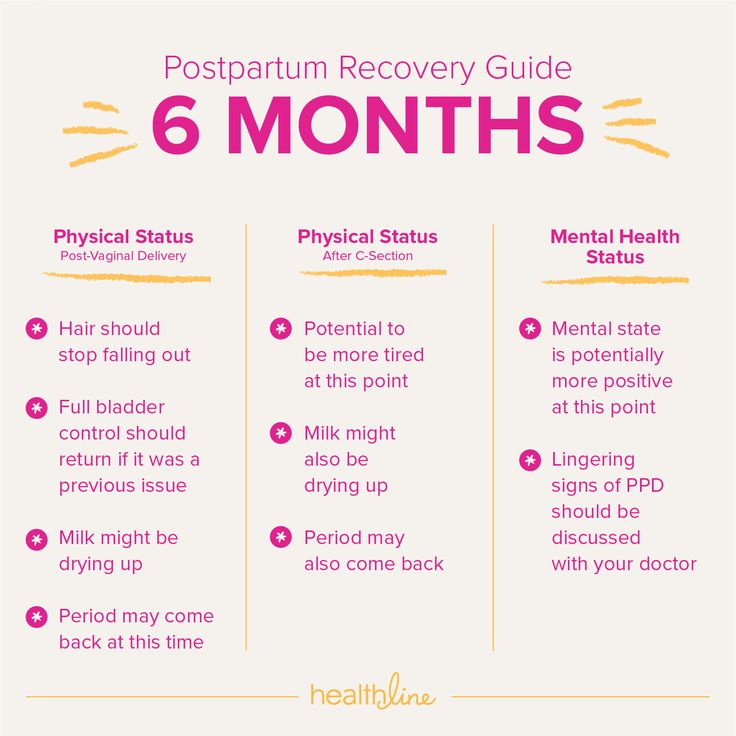
Many parents-to-be wait until the end of the first trimester — around week 13 — to tell friends and family about their pregnancy. A number of factors influence why people wait until this time to share the news.
Still, the most important part of your decision should revolve around what makes you the most comfortable. Read on to find out more about what to consider before you decide to announce your pregnancy.
The risk of miscarriage
The first trimester is a tremendous time of development and change for you and your little one. With all that change comes some risk that the pregnancy might not carry to term.
Between 10 and 25 percent of known pregnancies end in miscarriage, and roughly 80 percent of these miscarriages occur in the first trimester.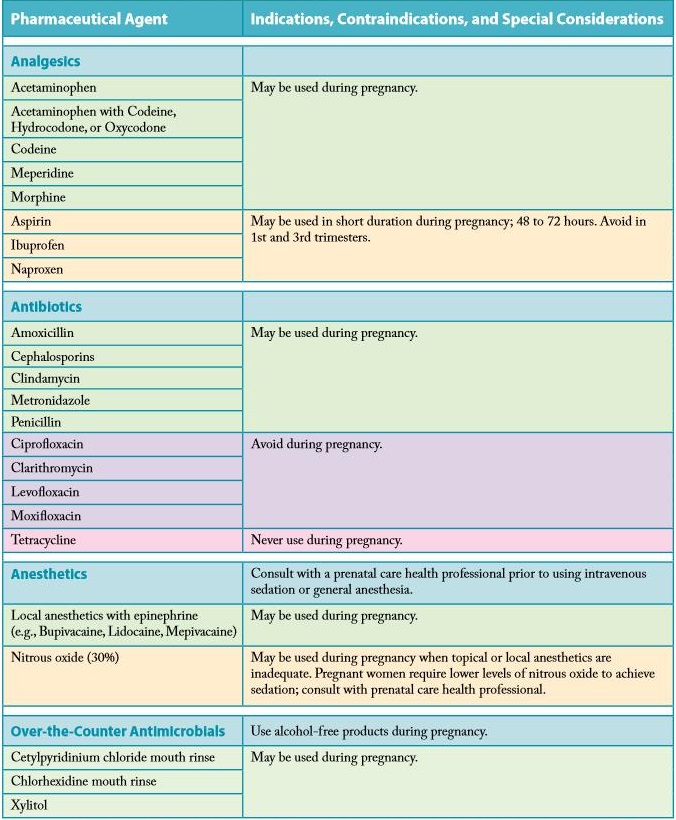
Most miscarriages are caused by factors beyond a mother’s control. About half are caused by chromosomal abnormalities. This means that the baby doesn’t develop properly.
Other causes of first trimester miscarriage include:
- illness in mother
- luteal phase defect (problem with a woman’s monthly cycle)
- hormone imbalances
- adhesions (scar-like tissue) in uterus
Age is another factor that affects miscarriage. Here is the miscarriage risk by age:
- Women ages 35 and under: 15 percent
- Women ages 35 to 45: 20 to 35 percent
- Women ages 45 and older: 50 percent
If a developing baby lives to 7 weeks with a heartbeat, the risk of miscarriage drops to 10 percent. In those beginning weeks when the risk is highest, you may not even know you’re pregnant unless you’ve taken an early test. After week 12, the risk of miscarriage falls to 5 percent for the rest of the pregnancy.
Given these statistics, it’s understandable that many parents wait until the risk of miscarriage drops before they announce. Most women don’t want to have to tell people the sad news of a miscarriage shortly after announcing their pregnancy.
Most women don’t want to have to tell people the sad news of a miscarriage shortly after announcing their pregnancy.
The first prenatal visit
Another reason couples wait until the end of the first trimester to share has to do with prenatal checkups. Your first appointment may be around week 8 of pregnancy, or even later.
During the first visit, your provider will run tests to confirm your pregnancy, estimate your due date, screen for infections, and determine the general health of you and your baby.
For some couples, hearing that heartbeat for the first time or having an ultrasound to date the pregnancy is reassuring before announcing it to everyone.
Recurrent pregnancy loss
If you’ve experienced a previous loss, your risk of having another miscarriage may be slightly higher, depending on your health history.
This news can be disheartening, especially in the case of recurrent pregnancy loss (RPL). Your doctor will likely examine you, order blood tests, and do some other testing to determine the cause of your losses.
The good news is that with the right treatment, your chances of carrying a baby to term may increase. But you might feel more comfortable waiting until after this treatment to announce your pregnancy to everyone.
The pros of waiting to announce your pregnancy
If you’ve had difficulty conceiving, had a previous pregnancy loss, or had a stillbirth, you may want to wait even longer than 12 weeks to share news of your pregnancy. It’s also fine to share later than the traditional first trimester cutoff. It’s entirely up to you and what you feel is best.
Though loss in the second and third trimesters is rare, couples may feel sensitive or worried that something will happen.
In these cases, you may choose to share news about the following instead:
- having an ultrasound that shows the baby is healthy
- finding out the sex of the baby
- reaching the halfway mark of pregnancy (week 20)
- reaching a personal milestone (e.g., when you start showing)
Sometimes letting a close friend or family member know can be helpful, especially if you’re feeling anxious.
If you’re still not comfortable sharing the news, your doctor may be able to refer you to a therapist or support group where you can express your feelings in a safe space.
Another option is to search online for forums with women who have gone through similar situations. Examples of online support groups include:
- Pregnancy After Loss Support
- Subsequent Pregnancy After Loss Support
Pros of Waiting
- The risk of miscarriage usually decreases after the first trimester.
- You might feel more comfortable after you’ve had an ultrasound, heard your baby’s heartbeat, or reached a pregnancy milestone.
- There’s anonymity for you and your partner.
The cons of waiting to share the news
If you’d rather have a support network in place regardless of your pregnancy outcome, feel free to share the news right away.
The first trimester may be tough for some women because of fatigue, nausea, vomiting, and other unpleasant symptoms. Letting a few key people know may help ease the burden. And if you do end up miscarrying, you might not want to have to go through it alone.
You may also want to tell your employer about your pregnancy right away if your job requires you to do physical labor that might be dangerous. These hazards might include:
- bending repeatedly at your waist (more than 20 times per day)
- standing for long periods of time
- lifting heavy things, like boxes, more than once every five minutes
- being exposed to chemicals
Your job may require these tasks. The data isn’t concrete on whether or not these activities directly lead to miscarriage, but it’s still worth considering in the overall picture. Speak with your doctor about the recommendations for lifting during pregnancy for more specifics.
Cons of Waiting
- The first trimester might be difficult without support.
- You might be exposed to workplace hazards if you don’t tell your employer.
- Friends and family might find out from other sources instead of you telling them directly.
Announcing to different groups
It might make sense to announce your pregnancy to different groups at different times. You may want to first tell a few close family members and then some friends before you announce it publicly on social media or tell your co-workers.
Family
Consider telling only your family to start. Your pregnancy will be major news for your parents, especially if this is their first grandchild. You might want to think of a creative way to tell your mother, father, and siblings so you can be there to witness their reaction firsthand.
If you choose to announce to just your family early on in your pregnancy, you’ll have plenty of people to celebrate with, but you won’t have to explain things over and over again if something does go wrong.
Friends
You’ll most likely want to tell your closest friends first. Then, whenever you feel more comfortable, you can broaden the group, or make an official announcement on social media. But be aware that the news might slip out of even the most well-meaning friend or relative.
Social networking is probably the easiest way to get the news out to friends and family who live far away. Posting a picture online of your ultrasound can get the news out in an instant.
Employer
You will have to tell your employer sooner or later, especially if you’re going to be taking parental leave or time off work. As mentioned above, it’s a good idea to tell your workplace right away if your job involves physical labor that might be dangerous.
Once your employer knows of your pregnancy, you’re protected against discrimination under the Pregnancy Discrimination Act of 1978. Your employer is required to provide you with reasonable accommodation if you’re unable to perform your work activities safely while pregnant.
If your job doesn’t involve physical labor, you can wait until you’re comfortable letting them know. Just make sure you give your employer a reasonable amount of time to prepare for your time away.
You will most likely want to tell your direct manager first so you two can plan together how to tell others you work with. It’s completely fine to ask your manager to keep this information confidential until you’re ready to tell others.
If you don’t want to inform your immediate superior right away, feel free to meet with your company’s human resources department to discuss your options. Be prepared to discuss their concerns about how your pregnancy will affect your job.
Being professional and prepared will help reassure your workplace of your commitment to making this a smooth transition.
What should you do?
In the end, the choice over when to share your pregnancy is entirely up to you. You can tell friends and family right away, or wait until you know more about the health of you and your baby.
To help make your decision, you may want to ask yourself these questions:
- Do I have a high-risk pregnancy or other factors that increase my miscarriage risk?
- Will telling everyone make me feel more comfortable, or less comfortable?
- Do I have certain work or lifestyle factors that make telling sooner important?
- Do I want a large network of support if something happens?
The takeaway
The beginning of pregnancy can be both exciting and frightening. Try to relax and enjoy the journey.
A lot of women choose to announce their pregnancy at the end of the first trimester because the risk of miscarriage is greatly reduced and their pregnancy “bump” may no longer be easy to hide. Of course, announcing at the 12-week mark isn’t required and the choice is entirely up to you.
Whether or not you tell the whole world right away, make sure to tell your doctor if you’re pregnant or trying to get pregnant. Schedule a prenatal appointment, take your vitamins, and keep up with good eating and exercise habits.
Try to take care of yourself and your baby-to-be. No matter when you share the news, it’ll surely be reason to celebrate.
Share on Pinterest
Last medically reviewed on December 6, 2018
- Parenthood
- Pregnancy
- 1st Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Mayo Clinic Staff. (2013). Miscarriage.
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298 - Miscarriage. (2015).
americanpregnancy.org/pregnancy-complications/miscarriage/ - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage.aspx - Reproductive health and the workplace. (2015).
cdc.gov/niosh/topics/repro/physicaldemands.html - Second trimester pregnancy loss. (2007).
aafp.org/afp/2007/1101/p1341.html - Your first prenatal visit. (2015).
americanpregnancy.org/planning/first-prenatal-visit/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 6, 2018
Written By
Ashley Marcin
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Deborah Weatherspoon, Ph. D., MSN
Share this article
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN — By Ashley Marcin on December 6, 2018
related stories
When You Should Take a Pregnancy Test
Can I Tell If I’m Pregnant Before I Miss My Period?
The First Trimester of Pregnancy
What to Expect at 1 Month Pregnant
Can I Take a Pregnancy Test at Night?
Read this next
When You Should Take a Pregnancy Test
Medically reviewed by Nancy Carteron, M.D., FACR
Trying to figure out if you need to take a pregnancy test? These five important signs will help you decide.
READ MORE
Can I Tell If I’m Pregnant Before I Miss My Period?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
While some women do experience pregnancy symptoms earlier than others, the only way to confirm a pregnancy is with a test.
Here's what you need to…
READ MORE
The First Trimester of Pregnancy
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Understanding a pregnancy week by week can help you make informed decisions and prepare for the big changes that lie ahead.
READ MORE
What to Expect at 1 Month Pregnant
Medically reviewed by Joshua Copel, MD
At 1 month pregnant, your belly may already be a little swollen — but it's more likely to be bloat than baby. Here's what else to expect at this stage.
READ MORE
Can I Take a Pregnancy Test at Night?
Medically reviewed by Amanda Kallen, MD
When pregnancy is possible, it‘s natural to want to know — now. So can you take a pregnancy test at night and get accurate results? Here‘s what you…
READ MORE
The State of Fertility Report 2017
Medically reviewed by Aimee Eyvazzadeh, MD, MPH
As featured on Good Morning America, we examine expert opinions and survey data in a comprehensive overview of the current fertility landscape in 2017.
READ MORE
The Best Parkinson’s Disease Blogs of 2021
The exact cause of Parkinson’s disease is unknown. Until a cure is found, a vast online network exists to help those living with Parkinson’s, and…
READ MORE
Healthy Sex for Women
Medically reviewed by Emelia Arquilla, DO
For women, sexual health significantly impacts overall health. Practicing safe sex, using contraception properly, and getting screened regularly for…
READ MORE
The Best Women’s Health Books of the Year
From navigating a healthy diet to your mental health, these books will help shed some light on the complex world of women's health.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby.
We'll tell you what to avoid — and some good…
READ MORE
Late pregnancy and childbirth - age, risks, myths, benefits, diagnosis, preparation
Myths about late pregnancy and childbirth
How and where to prepare for late pregnancy and childbirth
Modern living conditions and the rapid pace of development of medicine have had a significant impact on the age of women planning a pregnancy. Despite the recommendations of the World Health Organization, according to which the most favorable period for the realization of reproductive potential is the age of 19up to 35 years, today there is a trend of “late birth” all over the world - after 35-40 years.
According to Rosstat, in our country, the average age of a woman at the birth of her first child is increasing, today it is 28 years, while more and more women are postponing the issue of childbearing to a later date. And indeed, in recent years, giving birth at the age of 40 is no surprise to anyone, it has become quite commonplace.
Moreover, in many developed countries of the world, the number of women who gave birth after 40 already exceeds the number of those who carry out reproduction before the age of 20. nine0003
Despite the development of reproductive technologies and advances in medicine, pregnancy and childbirth still place a huge burden on all organs and systems of the mother's body. In this regard, women are wondering how safe late childbirth and pregnancy are.
Myths about late pregnancy and childbirth
Interest in this issue has led to a number of myths and fears associated with late birth. But is it worth giving up childbearing because of them, planning a pregnancy at a younger age, without psycho-emotional and social preparation? nine0003
According to psychologists, the realization of reproductive potential at a more mature age, after 30-35 years, is more favorable in terms of the psychological comfort of the baby and the preparedness of parents.
The medical aspects of late labor and pregnancy have also changed. If earlier there was an opinion that with increasing age, the risks of severe pregnancy and childbirth complications increase, but today most of these myths have been dispelled by clinical studies and new possibilities of modern medicine. nine0003
It is known that with age in the body of both women and men, the number of somatic, acquired mutations increases, which significantly increase the risk of having children with a genetic pathology. However, the current level of development of medical genetics and the possibilities of molecular genetic research make it possible to diagnose most of these diseases at the earliest stages of pregnancy.
For this purpose, screening of the first trimester is carried out, during which biochemical markers of chromosomal pathologies are determined, and the condition of the fetus is assessed using an ultrasound method. The most modern method for diagnosing fetal genetic abnormalities is a non-invasive prenatal test. By 9At the 10th week of pregnancy, a sufficient amount of fetal (fetal) DNA is determined in the blood of the future mother, with the help of which it is possible to calculate the risk of developing the most common chromosomal abnormalities in the unborn child with a probability of 99.9%.
There are also invasive diagnostic methods: chorion biopsy, which is performed at 8-12 weeks of gestation, amniocentesis, which is the aspiration of amniotic fluid at 16-24 weeks of pregnancy, cordocentesis - puncture of the fetal umbilical cord at 22-25 weeks of gestation. These methods allow with a high degree of probability to assume the presence of genetic diseases in the fetus. nine0003
Another myth about late birth is the need for a caesarean section for all women over 30-35 years of age. Indeed, in this age group, there is a high risk of developing complications such as weakness of labor activity, fetal hypoxia. However, dynamic monitoring during the entire period of pregnancy, timely examinations and doctor's control allow today patients over 30-35 years old to give birth on their own, without threats to the health of mother and baby.
There is also concern among women of older reproductive age about general physical health. It is known that the frequency of diseases of the cardiovascular, respiratory, urinary systems, as well as the development of diabetes, obesity, metabolic syndrome, neurological diseases is higher in women over 30 years old. But do not forget that the level of development of modern medicine today has stepped far forward and allows you to diagnose and treat all diseases at the stage of pregnancy preparation, while minimizing the risks both during pregnancy and during delivery. nine0013
How and where to prepare for late pregnancy and childbirth
Based on this, we can conclude that pregnancy after 35-40 years is a bold and responsible step that you can and should prepare for: during pregnancy planning, check your health by undergoing a full examination of both spouses. It is also worth consulting a geneticist.
Approximately 3-6 months before pregnancy, you should stop smoking and get your body in good shape. Under the guidance of an obstetrician-gynecologist, the preparation of the body for this important event in your life will be as comfortable and correct as possible. The doctor will advise you on which vitamins and mineral preparations you need to take before conception and which specialists you should contact. nine0003
In the Polyclinika.ru network of medical centers, we manage both uncomplicated pregnancies and high-risk pregnancies. Pregnant patients of absolutely different age groups trust us with their health and the health of their baby, since pregnancy management in our centers in Moscow is traditionally considered high-quality, highly qualified and safe.
The author of the article:
Grigoryan Syuzanna Vovaevna
obstetrician-gynecologist, Head of the gynecological department
work experience 4 years
reviews leave a review
Clinic
m. Sukharevskaya
Reviews
Services
- Title
- Initial appointment, consultation of an obstetrician-gynecologist3590
- Reception, consultation of an obstetrician-gynecologist repeated2200
- Pregnancy obstetrician-gynecologist primary appointment (examination, consultation)4000 905 years.
Red Gates. AvtozavodskayaPharmacy. Glades. Sukharevskaya. st. Academician Yangelam. Frunzenskaya Zelenograd
Okocha Victoria Alexandrovna
obstetrician-gynecologist, reproductologist, gynecologist-endocrinologist, ultrasound doctor
reviews Make an appointment
Clinic
m. Frunzenskaya
Ellinskaya Anastasia Aleksandrovna
obstetrician-gynecologist, ultrasound doctor
reviews Make an appointment
Clinic
m. Smolenskaya
m. PolyankaAkabirova Shakhlooy Anvarovna
obstetrician-gynecologist, endocrinologist, ultrasound doctor, KMN
reviews Make an appointment
Clinic
m.
Red Gate
m. AvtozavodskayaShklyar Aleksey Alekseevich
obstetrician-gynecologist, surgeon, KMN, head of the direction "Obstetrics and Gynecology"
reviews Make an appointment
Clinic
m. Sukharevskaya
Gazdieva Irina Khasanovna
obstetrician-gynecologist
reviews Make an appointment nine0003
Clinic
m. Street 1905 Goda
Zharova Natalya Anatolyevna
obstetrician-gynecologist
reviews Make an appointment
Clinic
m. Street 1905 Goda
Zotova Natalya Yurievna
obstetrician-gynecologist
reviews Make an appointment nine0003
Clinic
m.
Street 1905 Goda
Meshcheryakova Elena Alexandrovna
obstetrician-gynecologist, ultrasound doctor, online consultations
reviews Make an appointment
Clinic
m. Sukharevskaya
Rodina Tatyana Lvovna
obstetrician-gynecologist
reviews Make an appointment nine0003
Clinic
m. Avtozavodskaya
Ryabova Olga Borisovna
obstetrician-gynecologist, ultrasound doctor
reviews Make an appointment
Clinic
m. Taganskaya
Easy and safe pregnancy
With the joy of pregnancy come fears for the health of the child, and the desire that the whole process of pregnancy went smoothly, without complications.
In this article, we have compiled a list of basic procedures and checks to make your pregnancy safe and not harm your unborn baby. nine0003
Author Elena Levina
With the joy of pregnancy comes fears for the health of the child, and the desire that the whole process of pregnancy go smoothly, without complications. In this article, we have compiled a list of procedures and checks recommended by Israeli gynecologists to make your pregnancy safe and not harm the unborn baby.
Tests
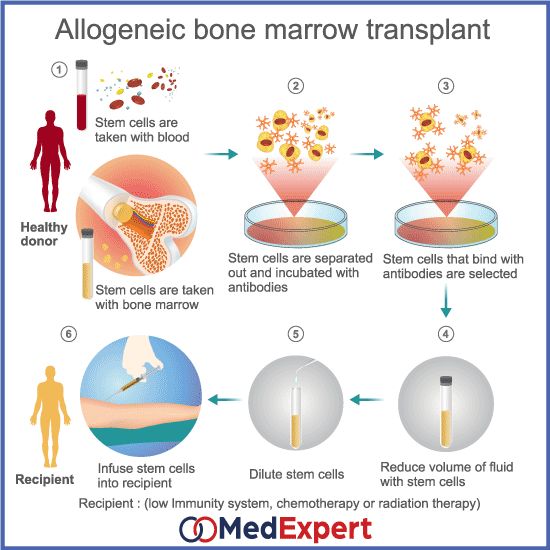
Today, there are many tests that are recommended during the months of pregnancy: genetic testing, antibody tests, a test for fetal chromosomal abnormalities, ultrasound - every expectant mother goes through all these checks. But it is important to know what innovations exist, what else is desirable to go through in order to feel calm. One of the novelties offered by medicine today is the verifi test. nine0003
The Verifi test is designed to assess the risk of a fetus having a congenital or hereditary abnormal number of chromosomes.
The test is a simple blood test. A simple non-invasive procedure can detect the frequency of chromosomal abnormalities of the fetus, starting from the 10th week of pregnancy. The test is suitable for both pregnancy with twins and pregnancy resulting from egg donation. The Israeli Association of Geneticists is of the opinion that all pregnant women at risk should be tested. nine0003
As already emphasized, Verifi is a non-invasive test, unlike amniocentesis, which is associated with an increased risk of miscarriage. The test is usually offered to women with an identified risk of developing fetal chromosomal abnormalities. There are two types of test: simple and extensive. With a simple Verifi test, 5 main types of chromosomes are checked, which can cause the most common syndromes - Down syndrome, Edwards syndrome, Turner and Klinefelter syndrome, triple X chromosome syndrome. nine0013 Extended Verifi test checks for 15 genetic syndromes.
Important to know!
If during the test you received a positive result for the presence of chromosomal abnormalities, you must confirm it with the help of additional diagnostic procedures - undergo an amniocentesis or chorionic villus biopsy.
The test is suitable for women in labor, over 35 years of age, and women in whom the results of an ultrasound or other screening test (blood test) performed in the first / second trimester have revealed a risk of chromosomal disorders. Women with a family history of these disorders are also at risk. nine0003
Food additives
There is not much innovation in this area, but it is important to recall that there are two types of dietary supplements that are important to keep in mind during pregnancy.
Folic acid: is actually a vitamin B, the presence of which is necessary for a woman to prevent disorders of the fetal nervous system. Therefore, gynecologists recommend that when planning a pregnancy, start taking folic acid three months before pregnancy, and continue taking it. nine0003
Iron : This mineral is recommended from the end of the third month of pregnancy until six weeks after childbirth. The recommended dose is 30 mg per day.
Women require more iron during pregnancy due to increased blood volume and to meet the needs of the unborn child. Iron deficiency anemia can lead to increased fatigue, weakness, headaches, and other symptoms.
Vaccinations
Influenza vaccine: According to the Israeli Ministry of Health, pregnant women are at increased risk of severe influenza and its complications. That is why gynecologists recommend mandatory vaccination during pregnancy. Recent research data show that the influenza vaccine is also effective for the unborn child: the risk of influenza in newborns up to 6 months is reduced by 63%.
Whooping cough vaccine: is one of the most serious childhood illnesses, especially for babies under 6 months of age. In recent years, in Israel, as well as throughout the world, an increase in the incidence of whooping cough has been witnessed. The main reason is related to low protective immunity. In Israeli hospitals, all pregnant women must be vaccinated against whooping cough between 27-39weeks of pregnancy.