When do babies start getting ear infections
Ear Infections in Babies and Toddlers
Featured Expert:
Ear infections in babies and toddlers are extremely common. In fact, according to the National Institutes of Health, five out of six children will experience an ear infection before their third birthday.
"Many parents are concerned that an ear infection will affect their child's hearing irreversibly—or that an ear infection will go undetected and untreated," says David Tunkel, M.D., Johns Hopkins Medicine pediatric otolaryngologist (ENT). "The good news is that most ear infections go away on their own, and those that don't are typically easy to treat."
Childhood Ear Infections Explained
Ear infections happen when there is inflammation— usually from trapped bacteria—in the middle ear, the part of the ear connects to the back of the nose and throat. The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
If your child has a sore throat, cold, or an upper respiratory infection, bacteria can spread to the middle ear through the eustachian tubes (the channels that connect the middle ear to the throat). In response to the infection, fluid builds up behind the eardrum.
Children are more likely to suffer from ear infections than adults for two reasons:
- Their immune systems are underdeveloped and less equipped to fight off infections.
- Their eustachian tubes are smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
"In some cases, fluid remains trapped in the middle ear for a long time, or returns repeatedly, even when there's no infection," Tunkel explains.
Ear Infection Signs and Symptoms
The telltale sign of an ear infection is pain in and around the ear. Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
- Tugging or pulling the ear
- Crying and irritability
- Difficulty sleeping
- Fever, especially in younger children
- Fluid draining from the ear
- Loss of balance
- Difficulty hearing or responding to auditory cues
Signs that require immediate attention include high fever, severe pain, or bloody or pus-like discharge from the ears.
Pediatric Otolaryngology
Our pediatric otolaryngologists provide compassionate and comprehensive care for children with common and rare ear, nose, and throat conditions. As part of the Johns Hopkins Children's Center, you have access to all the specialized resources of a children's hospital.
Learn more about Pediatric Otolaryngology
Ear Infection Treatments
Most ear infections go away without treatment. "If your child isn't in severe pain, your doctor may suggest a 'wait-and-see' approach coupled with over-the-counter pain relievers to see if the infection clears on its own," Tunkel says.
The reason: Treating an infection with antibiotics may cause the bacteria causing the infections to become resistant to those antibiotics—and that makes treating future infections more difficult. Equally important, in most cases antibiotics aren't necessary. Otitis media tends to get better without them. While you may be tempted to treat your child's ear infection with homeopathic or natural medicine, Tunkel warns they aren’t well studied.
Your best bet is to work with your child's health care provider to determine the appropriate course of action. In nearly every case, treatment decisions depend on the child’s age, degree of pain and presenting symptoms.
Under 6 months
Babies under six months almost always receive antibiotics. At this age, children are not fully vaccinated. Equally important, there's no research about the safety of skipping antibiotics for babies under 6 months of age — and complications from ear infections can be more severe when they occur in young babies. Bacteria trapped behind the eardrum can spread to other parts of the body and cause serious infections.
6 months to 2 years
For children between the ages of 6 months and 2 years, the American Academy of Pediatrics (AAP) recommends shared decision-making between parents and providers about whether to treat ear infections that are not severe. The best course is often to watch the child for two to three days before prescribing antibiotic treatment. If the child is in pain, or the ear infection is advanced, your child's doctor may suggest immediate antibiotic treatment.
Over 2 years
With children over the age of 2, ear infections that are not severe are likely to clear on their own, without treatment. "In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
"In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
Unfortunately, some children suffer from recurrent ear infections, sometimes up to five or six a year. Kids who get repeated infections may benefit from a surgical procedure where doctors insert small tubes in the eardrums to improve air flow and prevent fluid buildup. "Tubes don't prevent all ear infections, but they make managing them significantly easier," Tunkel explains.
Ear Infection Prevention
There are several steps you can take to reduce your child's risk of developing ear infections, including:
- Vaccinate your child: Children who are up-to-date on their vaccines get fewer ear infections than their unvaccinated counterparts. The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria.
- Consider breastfeeding: Breast milk contains antibodies that may help reduce the risk of ear infections and a host of other ailments. Whether you feed milk or formula, make sure your child sits up during feedings to prevent fluid from flowing into the middle ear.
- Wash your hands frequently: The best way to protect your child against cold and flu is to keep your hands clean. Wash your hands with soap and water and scrub them clean for a full 20 seconds each time you visit the sink.
- Steer clear of sick people: Don't allow your child to spend time with children or adults who are sick.
- Avoid secondhand smoke: Studies show that children who are exposed to secondhand smoke are up to three times more likely to develop ear infections than those who don't have those exposures.
Whether your child has ear infections or not, it's important to ensure they're able to hear well. "No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
"No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
Ear infections in babies and children
Ear infections in babies and children | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Ear infections are common in babies and young children, especially between the ages of 6 and 18 months. Often the infection clears up by itself within a few days. While it might be painful for 2 or 3 days, pain relief medication can help.
What are the types of ear infection?
There are 2 common types of ear infection:
- middle ear infections, also called otitis media, occur on the inner side of the ear drum
- outer ear infections, which occur in the ear canal outside the eardrum
Read more about the ears here.
Middle ear infection
Middle ear infection is the most common. This infection is caused by bacteria or viruses entering the ear from the throat via the Eustachian tube, which runs from the back of the throat to the middle ear. Because children have short and narrow Eustachian tubes, they are prone to middle ear infections. As they grow, their Eustachian tubes grow longer, and they become less likely to develop ear infections.
A sinus allergy can also cause swelling and blockage of the Eustachian tube, leading to infection.
Infections lead to a build-up of fluid inside the ear, causing pressure and pain. This fluid usually drains in a few days without any treatment.
If it doesn’t drain quickly enough, the eardrum may burst and you may find a yellow or bloody discharge. Once this happens, the pain goes away because the pressure has been relieved. A burst eardrum usually heals without treatment, but you should take care to prevent further infection.
Outer ear infection
Outer ear infection is often caused by excess moisture in the ear canal, sometimes after swimming in dirty water.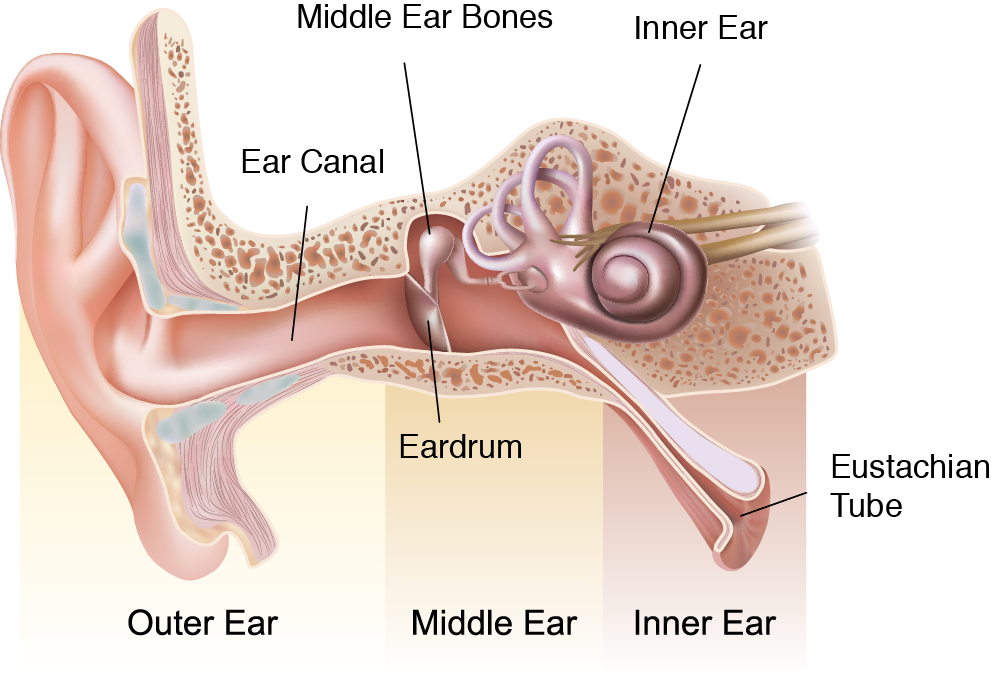 It is also called otitis externa or ‘swimmer’s ear’.
It is also called otitis externa or ‘swimmer’s ear’.
Damage to the ear canal, such as from cleaning ears with cotton buds, can also trigger infection.
Some kids also get outer ear infections after poking beads, insects or other objects into their ears.
Glue ear
Glue ear is not an infection but a common condition that can follow middle ear infections. Fluid builds up in the middle ear and doesn’t drain away. It might not cause pain, but it can make it hard for your child to hear.
Persistent glue ear can affect a child’s language development, so it’s important to treat it.
What are the symptoms of ear infections?
Ear infections can be very painful. While older children can tell you this, younger ones can’t. You might see them pulling at or poking their ear. Children also might develop a fever, vomiting or problems with their balance.
An outer ear infection can make the ear and the area around it red, swollen and painful to touch.
How are ear infections diagnosed?
If your doctor suspects your child has an ear infection, they will look into their ear to see the ear canal and eardrum. They can also test the pressure in the middle ear with a quick test that measures the movement of the eardrum.
How are ear infections treated?
Most ear infections clear up without treatment in a few days. Antibiotics generally don’t help, so the main treatment is pain relief.
You can:
- give your child pain relief medicine in the doses recommended for their age
- use anaesthetic or antibiotic ear drops for an outer ear infection, if recommended by your doctor
You should not:
- clean the ear with cotton buds or cotton wool
- give ear drops unless recommended by a doctor or pharmacist
- let your child get water in their ears if their eardrum has burst, until it has mended
If your child has recurrent infections or glue ear for more than 3 months, your doctor might refer them to an ear, nose and throat (ENT) specialist for treatment. Options include long courses of antibiotics and grommets to allow drainage. Your doctor will be able to explain more about these.
Options include long courses of antibiotics and grommets to allow drainage. Your doctor will be able to explain more about these.
If there is a foreign body in your child’s ear, it needs to be taken out. This can usually be done in a doctor’s surgery or at a hospital emergency department. Very occasionally, surgery is needed.
Can ear infections be prevented?
Middle ear infections generally occur after a cold, so keeping your child generally healthy will help. Keep your child away from cigarette smoke, which reduces fluid drainage in the ear.
Wearing ear plugs when swimming can help protect your child from swimmer’s ear.
When should I see the doctor?
You should see a doctor if:
- your child is unwell with an ear infection
- your child is getting a lot of infections
- there is redness and tenderness behind your child’s ear
- you are worried about your child’s hearing
- you are worried about your child’s language development
Sources:
Cochrane Database of Systematic Reviews (Antibiotics for acute otitis media in children), Cochrane Database of Systematic Reviews (Antibiotics for otitis media with effusion in children), Cochrane Database of Systematic Reviews (Paracetamol (acetaminophen) or non-steroidal anti-inflammatory drugs, alone or combined, for pain relief in acute otitis media in children), Queensland Government (Ear infection in children), Healthline (Tympanometry), Raising Children Network (Middle ear infection), Raising Children Network (External ear infection), Royal Children’s Hospital Melbourne (Ear infections and glue ear), Otolaryngology–Head and Neck Surgery (Plain Language Summary: Otitis Media with Effusion)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2020
Back To Top
Related pages
- Your child's health
Need more information?
Otitis Media (Middle Ear Infection) | Sydney Children's Hospitals Network
What is Otitis Media? Otitis Media is a common childhood condition which affects the ears
Read more on Sydney Children's Hospitals Network website
Otitis media in children - MyDr.com.au
Otitis media (middle ear infection) is a common childhood illness causing earache and fever. It usually gets better quickly with pain relievers but sometimes antibiotics are needed.
Read more on myDr website
Ear infections - Better Health Channel
It is estimated that around four out of five children will experience a middle ear infection at least once.
Read more on Better Health Channel website
Middle ear infections - Better Health Channel
Middle ear infections often happen during or after a child has a cold.
Read more on Better Health Channel website
Middle ear infection: babies, kids & teens | Raising Children Network
Children with middle ear infections usually have pain or discomfort in the ear. If you think your child has a middle ear infection, it’s best to see a GP.
Read more on raisingchildren.net.au website
Middle ear infection and grommets - MyDr.com.au
A grommet is a tiny tube inserted into the eardrum to allow air to enter the middle ear. Grommets can treat glue ear and recurrent middle ear infections.
Grommets can treat glue ear and recurrent middle ear infections.
Read more on myDr website
Ear problems in children - Better Health Channel
Babies and young children are more likely to develop middle ear infections because they are still building up their immunity.
Read more on Better Health Channel website
Ears - Glue ear and grommets | Sydney Children's Hospitals Network
What is glue ear? The lining of the middle ear keeps moist by making a watery liquid
Read more on Sydney Children's Hospitals Network website
Healthy Hearing Outback - Ear Science Institute Australia
Since 2014, our team has worked arm in arm with the PAMS to provide children and adults in remote Pilbara communities with tertiary ear and hearing care.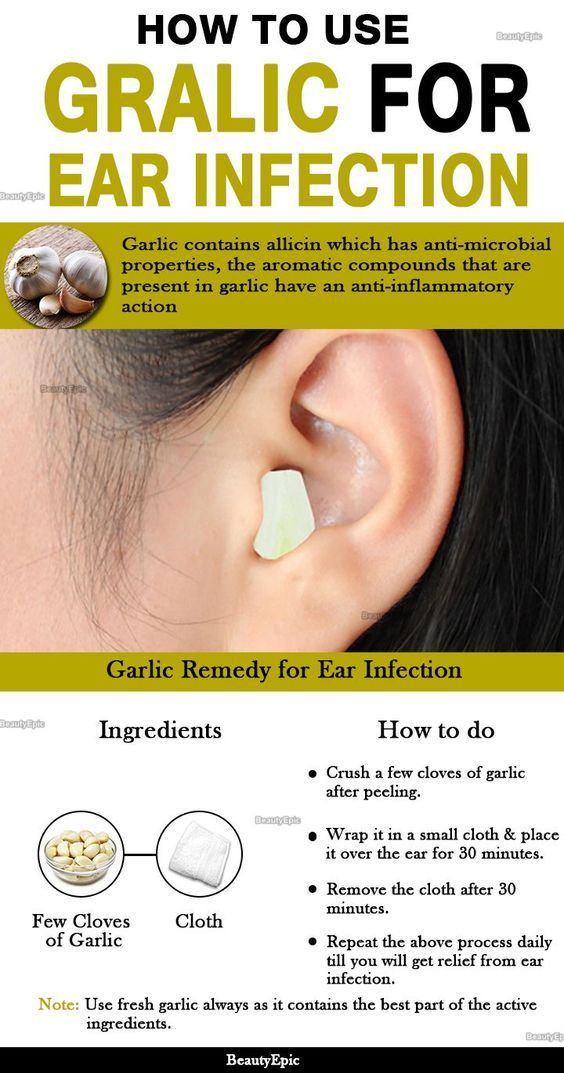
Read more on Ear Science Institute Australia website
Hearing Loss in Children - Ear Science Institute Australia
Hearing and communication can have a significant effect on a child’s development. For hearing loss in babies and hearing loss in call us today!
Read more on Ear Science Institute Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.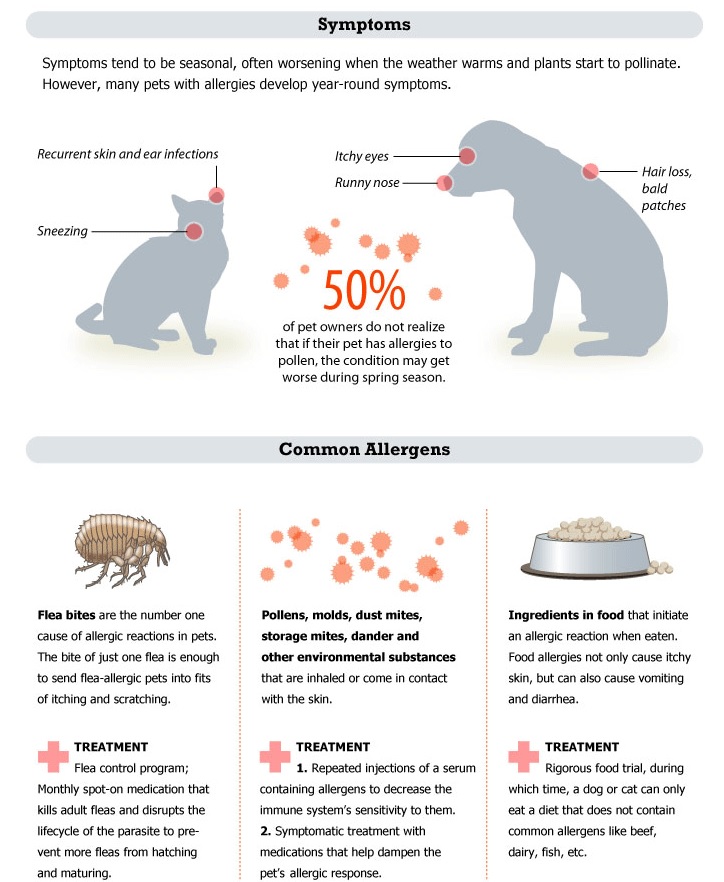
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Article "When babies have ears hurt"
Yulia Selskaya,
otorhinolaryngologist, head of the otorhinolaryngology clinic, doctor of the highest category, Ph.D.
If the child has a fever, does not sleep, tosses and turns, cries, and when you try to check the ears, the crying intensifies, the baby may have otitis media.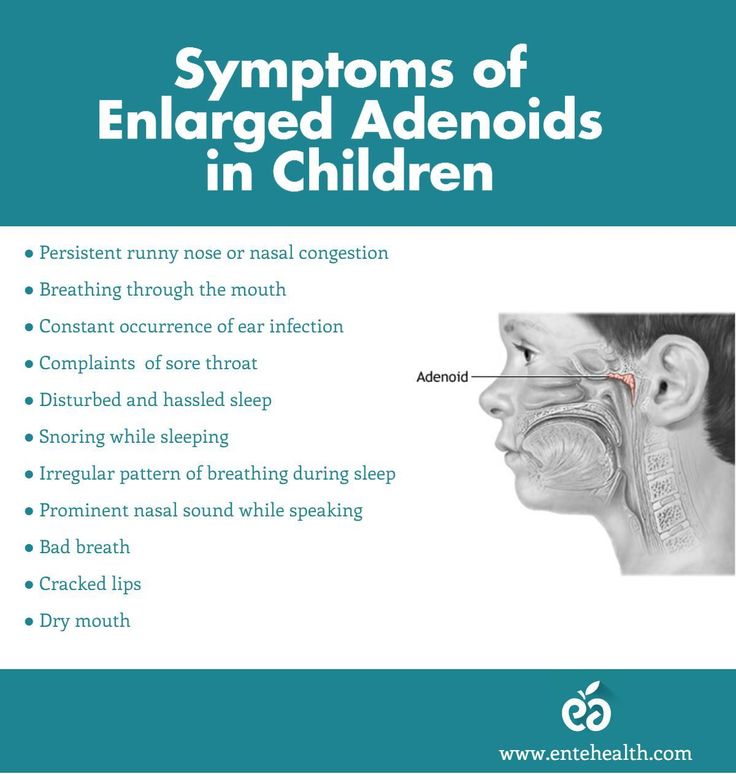
Features of the structure of the ears in children
nine0002 In terms of the frequency of diseases in babies, otitis media (ear inflammation) is in second place after a cold. At the age of up to a year, 62% of children suffer from otitis media once, 17% - three or more. Most often, children are prone to this disease in the period from three months to three years. Why do children get sick so often? There are many reasons. It is during this age period that the child has an incompletely formed immune system, it is difficult for the body to resist infections. The anatomical features of the structure of the middle ear contribute to the disease. In newborns and young children, the ear canal is short, the closer to the eardrum, the narrower. The border of the outer and middle ear is the tympanic membrane. The middle ear is located in the temporal part and consists of several elements. The most important is the auditory tube, which connects the nasopharynx and the inner ear.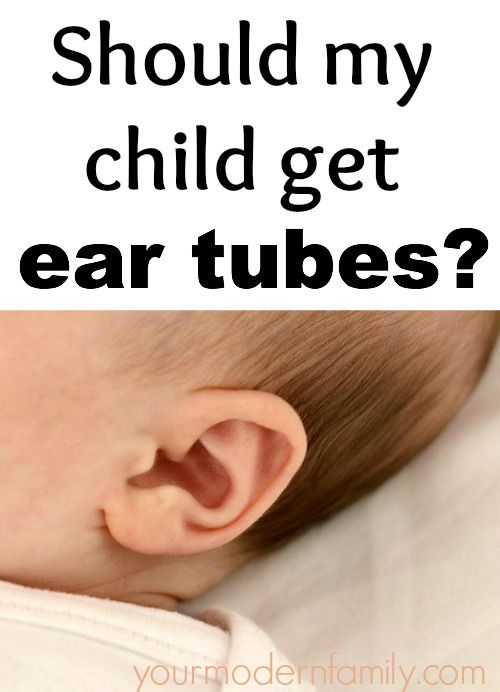 Unlike adults in babies, it is short, wide and more horizontal. This structure contributes to the penetration of infection from the nasopharynx into the middle ear, where instead of a smooth thin mucous membrane and air, there is loose gelatinous connective tissue with a small number of blood vessels. An ideal environment for the development of microorganisms. Acute otitis media develops when inflammation passes from the mucous membrane of the nasal cavity and nasopharynx to the auditory tube. Ventilation and drainage functions are disturbed, and bloody fluid accumulates in the tympanic cavity. nine0003
Unlike adults in babies, it is short, wide and more horizontal. This structure contributes to the penetration of infection from the nasopharynx into the middle ear, where instead of a smooth thin mucous membrane and air, there is loose gelatinous connective tissue with a small number of blood vessels. An ideal environment for the development of microorganisms. Acute otitis media develops when inflammation passes from the mucous membrane of the nasal cavity and nasopharynx to the auditory tube. Ventilation and drainage functions are disturbed, and bloody fluid accumulates in the tympanic cavity. nine0003
The reason for the violation of the patency of the auditory tube can be adenoids, which clog its mouth, congenital anomalies, allergic reactions.
Pneumococci, streptococci and acute eating disorders also cause otitis media. With improper feeding of the baby, the ingress of mixture or breast milk from the nasopharynx can cause inflammation.
Depending on the location of the lesion, otitis media can be external, medial, or internal. The most common at this age is acute otitis media, which develops against the background of SARS, tonsillitis, scarlet fever, measles. According to disease statistics, acute otitis media occurs in 70% of cases, external - about 20%, internal - up to 10% of the total number of otitis media. In young children, acute otitis media is even more common, up to 90%.
Breast-fed children are twice as likely to develop acute otitis media as artificial children. The causes of impaired patency of the auditory tube may also be associated with mechanical blockage of its mouth by adenoids, may be associated with congenital anomalies, allergic reactions.
Diagnosis of otitis in a child
The disease begins suddenly, the temperature rises to 39-40C. The baby is restless, cries a lot, sleeps poorly, sucks sluggishly at the breast. During feeding, it breaks away from the breast with a cry and cries. From the age of four months, the child closes the sore ear with a pen or rubs it against the pillow. If the inflammatory process has affected the eardrum, mucus, pus, and ichor are released from the ear. In a severe form of otitis media in infants, vomiting and diarrhea are possible. The kid throws back his head, strains his arms and legs, his neck does not bend. nine0003
From the age of four months, the child closes the sore ear with a pen or rubs it against the pillow. If the inflammatory process has affected the eardrum, mucus, pus, and ichor are released from the ear. In a severe form of otitis media in infants, vomiting and diarrhea are possible. The kid throws back his head, strains his arms and legs, his neck does not bend. nine0003
Moms ask: how to quickly see a doctor with symptoms of otitis media? Do you need a specialist or will a pediatrician prescribe treatment? You need to see a doctor immediately or within a few hours after the first symptoms appear: emergency care should be provided without an appointment. Only an ENT doctor should diagnose the disease, he will also prescribe treatment.
But there are situations when it is necessary to act without delay. Swelling behind the ear, the child lies with his head thrown back, legs bent to the tummy and convulsions, this may indicate dangerous complications - meningitis or meningoencephalitis. "Ambulance" in such cases is called immediately. Complications are treated in a pediatric ENT hospital, if necessary, an incision in the tympanic membrane is made - myringotomy or tympanostomy (simultaneously with the incision of the tympanic membrane, the tympanic cavity is sanitized and ventilation tubes-aerators are installed). The surgeon performs the operation using a microscope under general or local anesthesia. The purpose of the procedure is to ensure the free outflow of pus from the middle ear cavity. After the operation, the child's condition improves. nine0003
"Ambulance" in such cases is called immediately. Complications are treated in a pediatric ENT hospital, if necessary, an incision in the tympanic membrane is made - myringotomy or tympanostomy (simultaneously with the incision of the tympanic membrane, the tympanic cavity is sanitized and ventilation tubes-aerators are installed). The surgeon performs the operation using a microscope under general or local anesthesia. The purpose of the procedure is to ensure the free outflow of pus from the middle ear cavity. After the operation, the child's condition improves. nine0003
Under the supervision of an ENT doctor
An ENT doctor prescribes treatment - antibiotic therapy, painkillers, local procedures and physiotherapy. Recovery usually occurs within 5-10 days. After the baby has recovered, rehabilitation therapy is carried out.
In the treatment of acute otitis in children under two years of age, the doctor will definitely prescribe antibiotics. These can be tablets, syrups, intramuscular injections, in severe cases - intravenous administration of drugs. nine0003
Antibiotics are prescribed for children older than two years in a serious condition, when the ear hurts a lot and the temperature is above 38C.
Many parents are skeptical about the use of antibiotics for otitis, fearing that the baby's immune system is being harmed. There is no reason to worry: modern drugs are well excreted from the body and the negative consequences of their use are minimal. If otitis media is not treated or done without medical supervision, cicatricial processes in the tympanic cavity, hearing loss, chronic purulent otitis media, which require complex surgical treatment, may occur. In extremely severe cases - mastoiditis, meningitis. nine0003
First aid for otitis media
Mom can give first aid to the baby. If the temperature is elevated, it is worth giving the child antipyretic and analgesic drugs based on paracetamol. Analgin and aspirin can not be used! For sanitation of the nose, spray and drops with sea water are used. Otitis is often accompanied by rhinitis. You can gently remove mucus from the front of the nose. Vasoconstrictor drops are not prescribed for infants.
Otitis is often accompanied by rhinitis. You can gently remove mucus from the front of the nose. Vasoconstrictor drops are not prescribed for infants.
If the baby is over a year old, with severe swelling of the nasal mucosa, medicines are prescribed for the common cold. nine0003
Compresses, warming and fatty ointments should not be used for otitis media, otherwise the inflammation will increase. For children prone to frequent otitis, parents put cotton wool in their ears, trying to protect them from the disease. This cannot be done - ideal conditions are created in the external auditory canal for the reproduction of microorganisms, including fungi.
When bathing a child, cotton wool with vaseline oil is placed on children who have a perforation of the eardrum, otherwise the water that enters the eardrum can cause inflammation. With a complete membrane, water entering the external auditory canal does not threaten anything; after bathing, simply pat your ears dry with a towel. nine0003
nine0003
Author: Julia Selskaya, otorhinolaryngologist, head of the Otorhinolaryngology Clinic, doctor of the highest category, Ph.D.
Why do my child's ears hurt?
Sore ears in a child is the most common reason for parents to visit a pediatrician or pediatric ENT doctor. There are several main reasons why children's ears hurt:
- inflammation of the middle ear (otitis media)
- sore throat (tonsillitis, tonsillitis)
- obstructed eustachian tubes (due to swelling or inflammation)
- inflammation of the external auditory canal (sulfur plug, pus, foreign body)
- teething
- trigeminal inflammation
- inflammation of the salivary gland (mumps)
- inflammation of the mandibular lymph nodes
- mastoiditis (inflammation of the mastoid process of the temporal bone)
Why does a child have earaches with otitis media? nine0085
Otitis media with effusion occurs when the Eustachian tube, which connects the middle ear to the back of the nose, becomes blocked due to swelling or enlarged tonsils, and fluid from the ear cannot drain.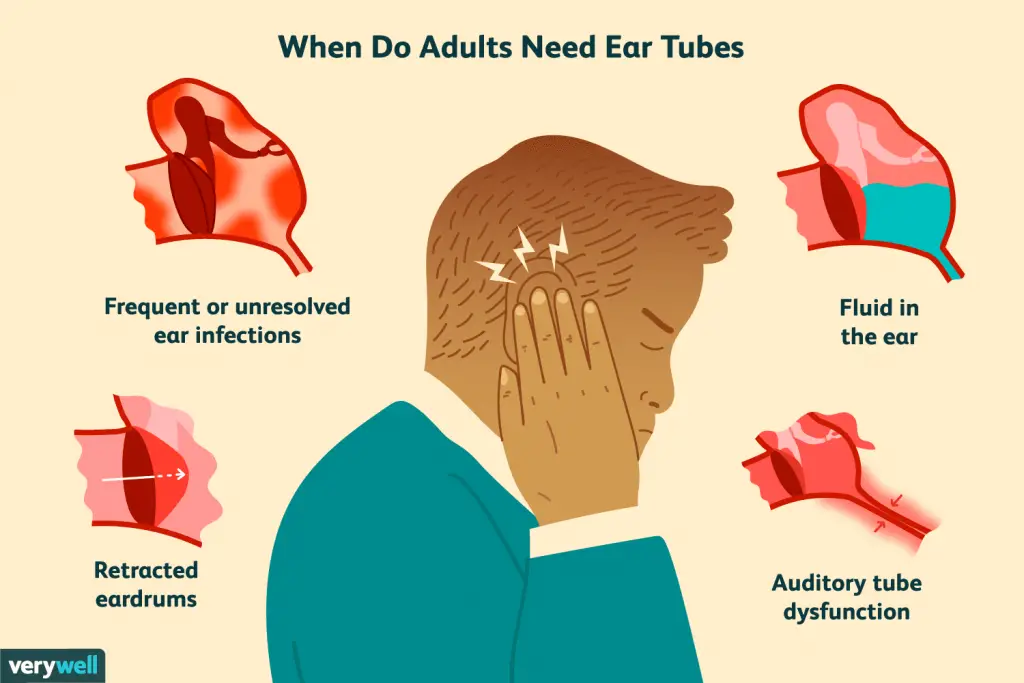 Fluid (pus or serous effusion) accumulates in the middle ear cavity, which leads to increased pressure inside the ear cavity and pain. Otitis media with effusion usually resolves in 3 months. Treatment uses acetaminophen or ibuprofen to reduce inflammation and pain. Warm compresses may also be used. Important: do not use compresses without a doctor's prescription, because. with some types of purulent inflammation, they are contraindicated. nine0003
Fluid (pus or serous effusion) accumulates in the middle ear cavity, which leads to increased pressure inside the ear cavity and pain. Otitis media with effusion usually resolves in 3 months. Treatment uses acetaminophen or ibuprofen to reduce inflammation and pain. Warm compresses may also be used. Important: do not use compresses without a doctor's prescription, because. with some types of purulent inflammation, they are contraindicated. nine0003
In children older than 6 months, if there are no signs of purulent bacterial otitis, antibiotics are not used.
Children with otitis media may experience temporary mild hearing loss. If the disorder persists for more than 3 months, or if the hearing loss is found in more than just the ear where the otitis media was present, the child should be examined by an ENT doctor to decide whether a tympanostomy tube should be placed to drain fluid from the middle ear.
How do ears hurt with an ear infection? nine0085
When the Eustachian tube, which connects the middle ear to the back of the nose, becomes blocked and fluid builds up in the middle ear, viruses or bacteria can multiply in the fluid, and not only the increased pressure in the middle ear, but also the waste products of these micro-organisms (pus) can cause pain. ). This disease is called acute otitis media. Ear infections usually occur as a complication after or during a child's infection with a viral upper respiratory tract infection. Otitis media is more common in winter in children attending kindergarten or school. If otitis media is bacterial in nature, antibiotics are used to treat it. Antibacterial agents are not used to treat viral otitis media. nine0003
). This disease is called acute otitis media. Ear infections usually occur as a complication after or during a child's infection with a viral upper respiratory tract infection. Otitis media is more common in winter in children attending kindergarten or school. If otitis media is bacterial in nature, antibiotics are used to treat it. Antibacterial agents are not used to treat viral otitis media. nine0003
Swimmer's ear.
Ears can be sore from inflammation caused by contaminated water entering the ear canals. This is most often observed in children visiting the pool, if ear hygiene is not given enough attention. This can happen if the skin in the passage is damaged (for example, scratches from nails). Antibiotic drops (such as Otipax) are used to treat this disease, and ear pain is reduced with the use of anti-inflammatory drugs. nine0003
How do the ears hurt with Eustachian tube dysfunctions ?
Pain during inflammation of the Eustachian tube is accompanied by a feeling of fullness in the ear, "transfusion" of fluid inside the ear, hearing loss, tinnitus. Therapy includes treatment of the root cause of Eustachian tube dysfunction: allergic rhinitis, rhinosinusitis, laryngeal-pharyngeal reflux.
Therapy includes treatment of the root cause of Eustachian tube dysfunction: allergic rhinitis, rhinosinusitis, laryngeal-pharyngeal reflux.
Ear pain from other causes: most often caused by trauma to the ears or ear canals, foreign objects in them or the formation of sulfuric plugs. nine0003
Other disorders that can cause ear pain include teething, parotitis, sinusitis, throat infections, lymphadenitis, and cervical spine injuries.
When should I contact a pediatric ENT?
It is necessary to show the child to a pediatrician or an otorhinolaryngologist if:
- Ear pain worsens or does not improve with treatment
- Blood or pus leaks from ears
- The area around the ear begins to swell or become red
- An unpleasant or putrid odor comes from the ear
- The child has a fever
- Pain in ears worse when lying down
- Pain in the ear appeared at the time of aftercare of acute respiratory infections or SARS
Ear pain is classified as one of the most severe, worse than ear pain - only toothache.