When can you see spina bifida in ultrasound
Spina bifida - Diagnosis and treatment
Diagnosis
If you're pregnant, you'll be offered prenatal screening tests to check for spina bifida and other birth defects. The tests aren't perfect. Some mothers who have positive blood tests have babies without spina bifida. Even if the results are negative, there's still a small chance that spina bifida is present. Talk to your doctor about prenatal testing, its risks and how you might handle the results.
Blood tests
Spina bifida can be screened with maternal blood tests, but typically the diagnosis is made with ultrasound.
- Maternal serum alpha-fetoprotein (MSAFP) test. For the MSAFP test, a sample of the mother's blood is drawn and tested for alpha-fetoprotein (AFP) — a protein produced by the baby. It's normal for a small amount of AFP to cross the placenta and enter the mother's bloodstream.
But unusually high levels of AFP suggest that the baby has a neural tube defect, such as spina bifida, though high levels of AFP don't always occur in spina bifida.
- Test to confirm high AFP levels. Varying levels of AFP can be caused by other factors — including a miscalculation in fetal age or multiple babies — so your doctor may order a follow-up blood test for confirmation. If the results are still high, you'll need further evaluation, including an ultrasound exam.
- Other blood tests. Your doctor may perform the MSAFP test with two or three other blood tests. These tests are commonly done with the MSAFP test, but their objective is to screen for other conditions, such as trisomy 21 (Down syndrome), not neural tube defects.
Ultrasound
Fetal ultrasound is the most accurate method to diagnose spina bifida in your baby before delivery. Ultrasound can be performed during the first trimester (11 to 14 weeks) and second trimester (18 to 22 weeks). Spina bifida can be accurately diagnosed during the second trimester ultrasound scan. Therefore, this examination is crucial to identify and rule out congenital anomalies such as spina bifida.
An advanced ultrasound also can detect signs of spina bifida, such as an open spine or particular features in your baby's brain that indicate spina bifida. In expert hands, ultrasound is also effective in assessing severity.
Amniocentesis
If the prenatal ultrasound confirms the diagnosis of spina bifida, your doctor may request amniocentesis. During amniocentesis, your doctor uses a needle to remove a sample of fluid from the amniotic sac that surrounds the baby.
This examination may be important to rule out genetic diseases, despite the fact that spina bifida is rarely associated with genetic diseases.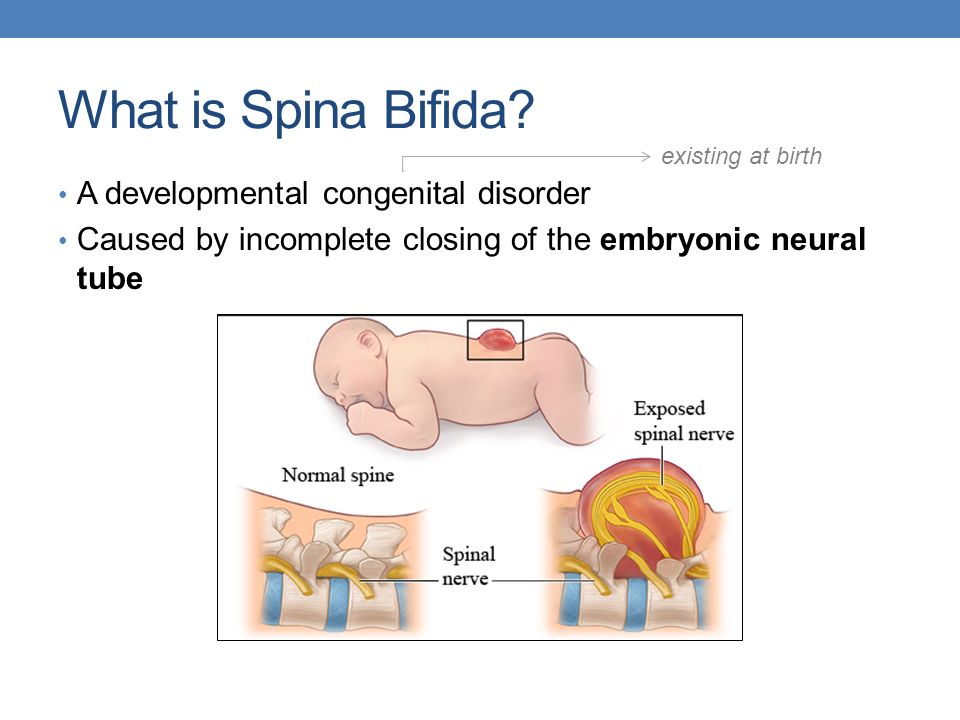
Discuss the risks of amniocentesis, including a slight risk of loss of the pregnancy, with your doctor.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your spina bifida-related health concerns Start Here
More Information
- Spina bifida care at Mayo Clinic
- Amniocentesis
- Ultrasound
Treatment
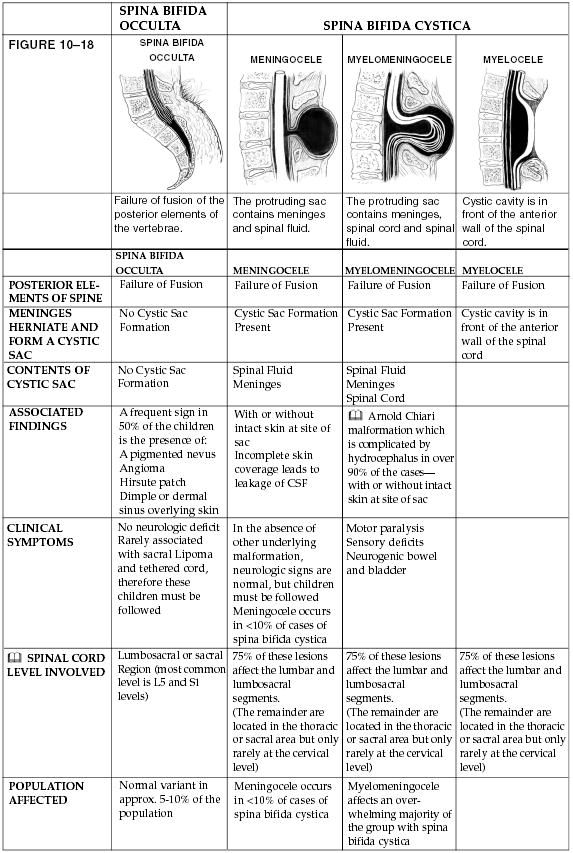
Spina bifida treatment depends on the severity of the condition. Spina bifida occulta often doesn't require any treatment at all, but other types of spina bifida do.
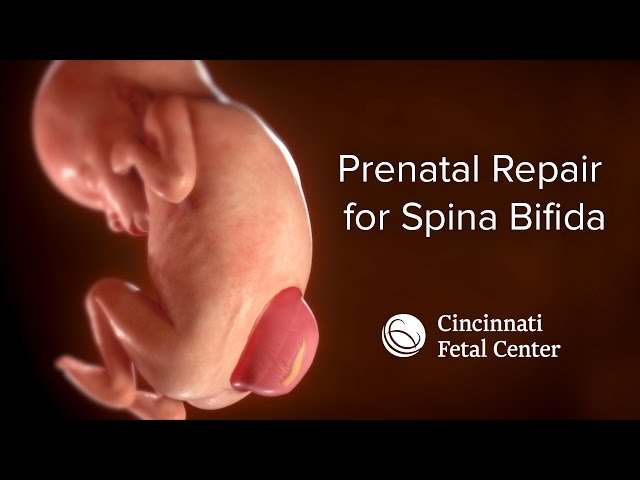
Surgery before birth
Nerve function in babies with spina bifida can worsen after birth if spina bifida isn't treated. Prenatal surgery for spina bifida (fetal surgery) takes place before the 26th week of pregnancy. Surgeons expose the pregnant mother's uterus surgically, open the uterus and repair the baby's spinal cord. In select patients, this procedure can be performed less invasively with a special surgical tool (fetoscope) inserted into the uterus.
Research suggests that children with spina bifida who had fetal surgery may have reduced disability and be less likely to need crutches or other walking devices. Fetal surgery may also reduce the risk of hydrocephalus. Ask your doctor whether this procedure may be appropriate for you. Discuss the potential benefits and risks, such as possible premature delivery and other complications, for you and your baby.
It's important to have a comprehensive evaluation to determine whether fetal surgery is feasible. This specialized surgery should only be done at a health care facility that has experienced fetal surgery experts, a multispecialty team approach and neonatal intensive care. Typically the team includes a fetal surgeon, pediatric neurosurgeon, maternal-fetal medicine specialist, fetal cardiologist and neonatologist.
Cesarean birth
Many babies with myelomeningocele tend to be in a feet-first (breech) position. If your baby is in this position or if your doctor has detected a large cyst or sac, cesarean birth may be a safer way to deliver your baby.
Surgery after birth
Myelomeningocele requires surgery to close the opening in the baby's back within 72 hours of birth. Performing the surgery early can help minimize the risk of infection associated with the exposed nerves. It may also help protect the spinal cord from more trauma.
During the procedure, a neurosurgeon places the spinal cord and exposed tissue inside the baby's body and covers them with muscle and skin. At the same time, the neurosurgeon may place a shunt in the baby's brain to control hydrocephalus.
Treatment for complications
In babies with myelomeningocele, irreparable nerve damage has likely already occurred and ongoing care from a multispecialty team of surgeons, physicians and therapists is usually needed. Babies with myelomeningocele may need more surgery for a variety of complications. Treatment for complications — such as weak legs, bladder and bowel problems, or hydrocephalus — typically begins soon after birth.
Depending on the severity of spina bifida and the complications, treatment options may include:
- Walking and mobility aids.
 Some babies may start exercises to prepare their legs for walking with braces or crutches when they're older. Some children may need walkers or a wheelchair. Mobility aids, along with regular physical therapy, can help a child become independent. Even children who need a wheelchair can learn to function very well and become self-sufficient.
Some babies may start exercises to prepare their legs for walking with braces or crutches when they're older. Some children may need walkers or a wheelchair. Mobility aids, along with regular physical therapy, can help a child become independent. Even children who need a wheelchair can learn to function very well and become self-sufficient. - Bowel and bladder management. Routine bowel and bladder evaluations and management plans help reduce the risk of organ damage and illness. Evaluations include X-rays, kidney scans, ultrasounds, blood tests and bladder function studies. These evaluations will be more frequent in the first few years of life but less often as children grow. A specialist in pediatric urology with experience in evaluating and performing surgery on children with spina bifida may offer the most effective management options.
- Bowel management may include oral medications, suppositories, enemas, surgery or a combination of these approaches.

- Bladder management may include medications, using catheters to empty the bladder, surgery or a combination of treatments.
- Surgery for hydrocephalus. Most babies with myelomeningocele will need a surgically placed tube that allows fluid in the brain to drain into the abdomen (ventricular shunt). This tube might be placed just after birth, during the surgery to close the sac on the lower back or later as fluid accumulates. A less invasive procedure, called endoscopic third ventriculostomy, may be an option. But candidates must be carefully chosen and meet certain criteria. During the procedure, the surgeon uses a small video camera to see inside the brain and makes a hole in the bottom of or between the ventricles so cerebrospinal fluid can flow out of the brain.
- Treatment and management of other complications. Special equipment such as bath chairs, commode chairs and standing frames may help with daily functioning.
 Whatever the issue — orthopedic complications, tethered spinal cord, GI issues, skin problems or others — most spina bifida complications can be treated or at least managed to improve quality of life.
Whatever the issue — orthopedic complications, tethered spinal cord, GI issues, skin problems or others — most spina bifida complications can be treated or at least managed to improve quality of life.
Ongoing care
Children with spina bifida need close follow-up care and observation. Their primary care doctors evaluate growth, the need for vaccinations and general medical issues, and they coordinate medical care.
Children with spina bifida also often need treatment and ongoing care from:
- Physical medicine and rehabilitation
- Neurology
- Neurosurgery
- Urology
- Orthopedics
- Physical therapy
- Occupational therapy
- Special education teachers
- Social workers
- Dietitians
Parents and other caregivers are a key part of the team. They can learn how to help manage a child's condition and how to encourage and support the child emotionally and socially.
More Information
- Spina bifida care at Mayo Clinic
- C-section
- Fetal surgery
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
News that your newborn child has a condition such as spina bifida can naturally cause you to feel grief, anger, frustration, fear and sadness. There's good reason for hope, however, because most people with spina bifida live active, productive and full lives — especially with encouragement and support from loved ones. Children with spina bifida can go on to college, hold jobs and have families.
Special accommodations may be necessary along the way, but encourage your child to be as independent as possible.
Independent mobility is an important and appropriate goal for all children with spina bifida.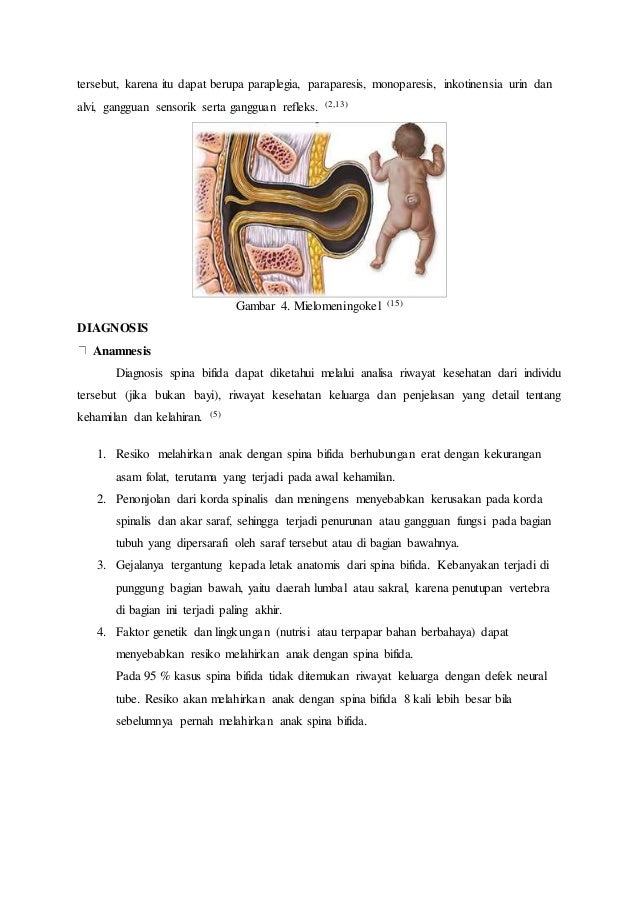 This may mean walking with or without braces, using walking aids (such as canes or crutches), or exclusively using a wheelchair. Encouraging children to participate in activities with their peers can be beneficial, and caregivers can help adjust activities to accommodate physical limitations.
This may mean walking with or without braces, using walking aids (such as canes or crutches), or exclusively using a wheelchair. Encouraging children to participate in activities with their peers can be beneficial, and caregivers can help adjust activities to accommodate physical limitations.
Caregivers of children with spina bifida can help adjust activities to accommodate physical limitations.
Note: This content was created prior to the coronavirus disease 2019 (COVID-19) pandemic and does not demonstrate proper pandemic protocols. Please follow all recommended Centers for Disease Control and Prevention guidelines for masking and social distancing.
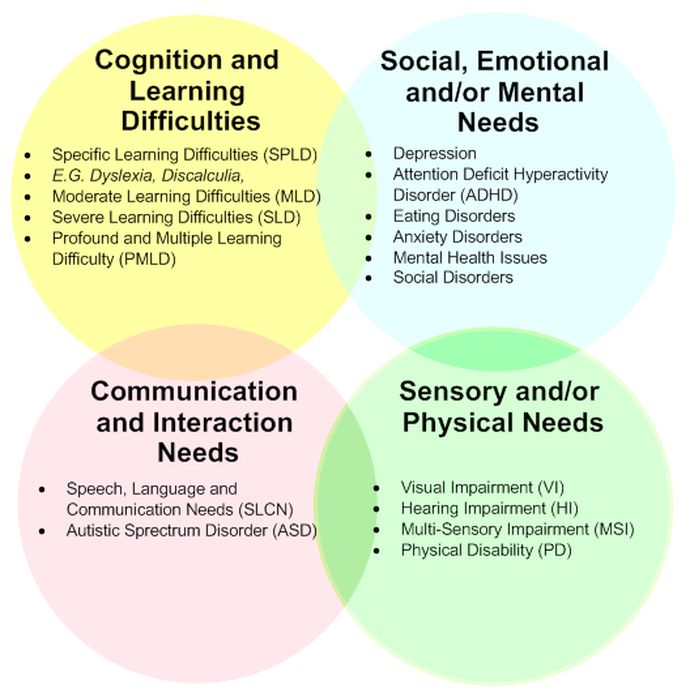
Many children with spina bifida have typical intelligence, but some may need educational intervention for learning problems. Some children experience difficulty with attention, concentration or language that requires treatment from professionals outside of school.
As for any child with a chronic medical condition, children with spina bifida may benefit from meeting with mental health professionals, such as a child psychologist, to assist with adjustment and coping.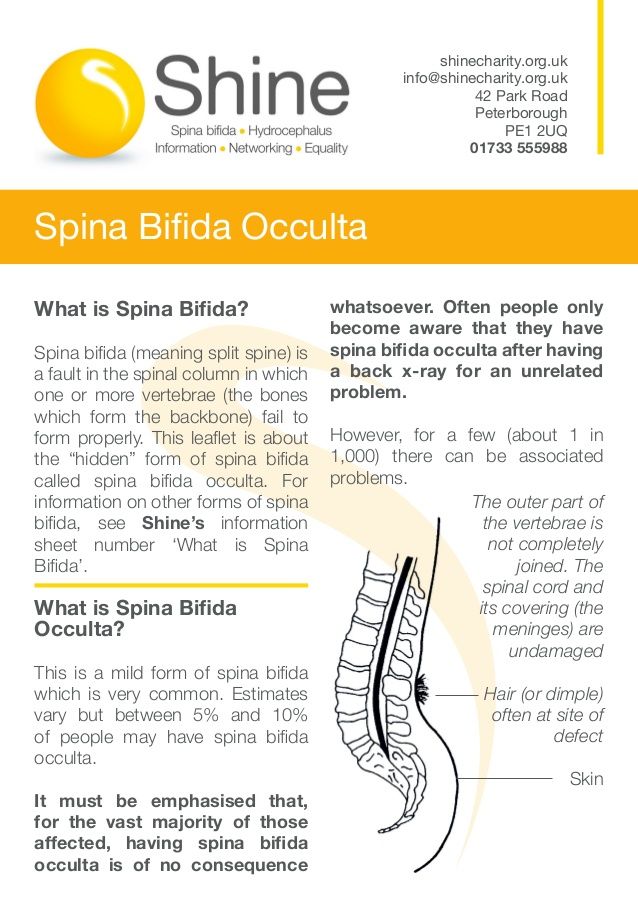 Most children with spina bifida are resilient and adapt to their challenges with support from their parents, teachers and other caregivers.
Most children with spina bifida are resilient and adapt to their challenges with support from their parents, teachers and other caregivers.
If your child has spina bifida, you may benefit from finding a support group of other parents who are dealing with the condition. Talking with others who understand the challenges of living with spina bifida can be helpful.
Preparing for your appointment
Your doctor will likely suspect or diagnose your baby's condition during your pregnancy. If that's the case, you'll likely consult with a multispecialty team of physicians, surgeons and physical therapists at a center that specializes in spina bifida treatment.
Here's some information to help you get ready for your appointment and know what to expect from your health care providers if there are suspicions that your baby may have spina bifida.
What you can do
To prepare for the appointment:
- Be aware of any pre-appointment instructions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as drink extra water before an ultrasound.
- Make a list of all medications, vitamins, herbs and supplements that you took before and during your pregnancy, and the dosages.
- Ask a family member or friend to come with you, if possible. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Create a list of questions to ask your doctor, starting with the most important in case time runs out.
For spina bifida, some basic questions to ask include:
- Is spina bifida present and how severe is it?
- Is there evidence of accumulation of fluid on the brain (hydrocephalus)?
- Can my baby be treated during pregnancy?
- What will be done for my baby immediately after birth?
- Will the treatment cure my child?
- Will there be any lasting effects?
- Who can I contact to find out about community resources that may be able to help my child?
- What is the likelihood of this happening again in future pregnancies?
- How can I keep this from happening again in the future?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Being ready to answer questions from your doctor may reserve time to go over any points you want to focus on. Your doctor may ask, for example:
- Have you ever had a child with spina bifida or other birth defects?
- Is there a family history of spina bifida?
- Did you take folic acid (vitamin B-9) before and during your pregnancy?
- Are you taking any anti-seizure medications, or were you taking them at the beginning of your pregnancy?
- If necessary, are you able to travel to a facility that offers specialized care?
By Mayo Clinic Staff
Spina bifida - Better Health Channel
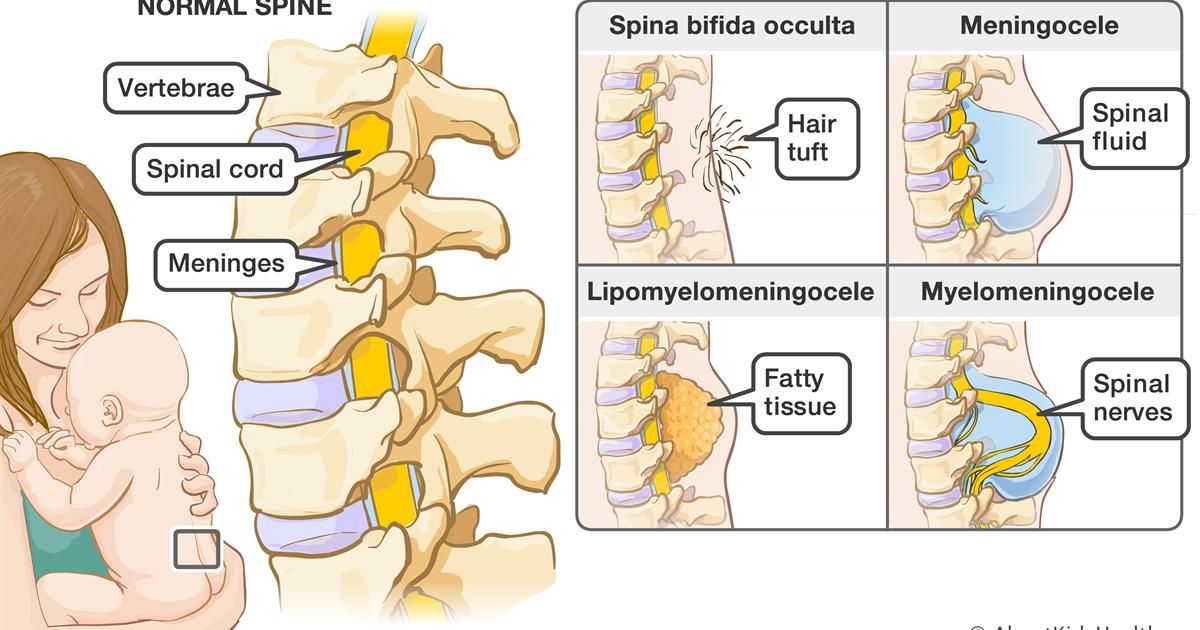
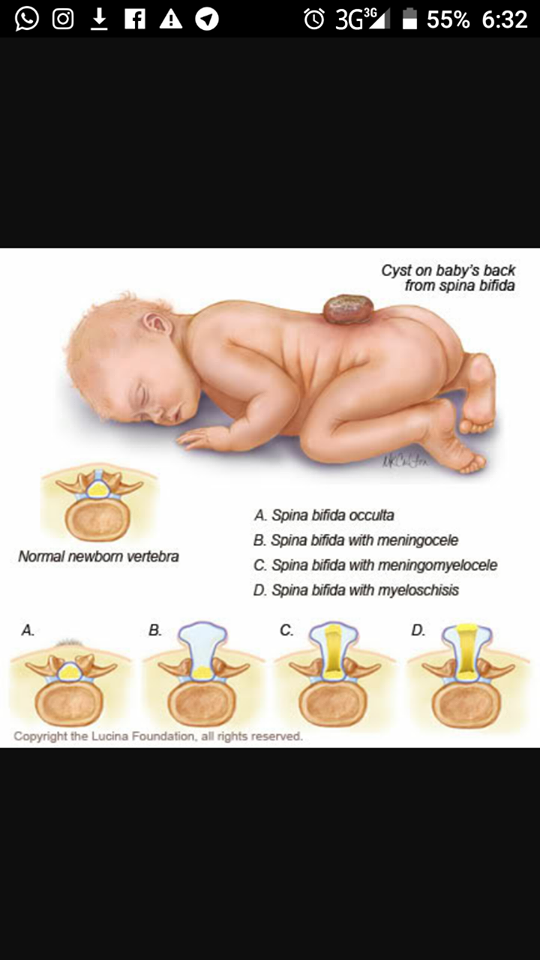
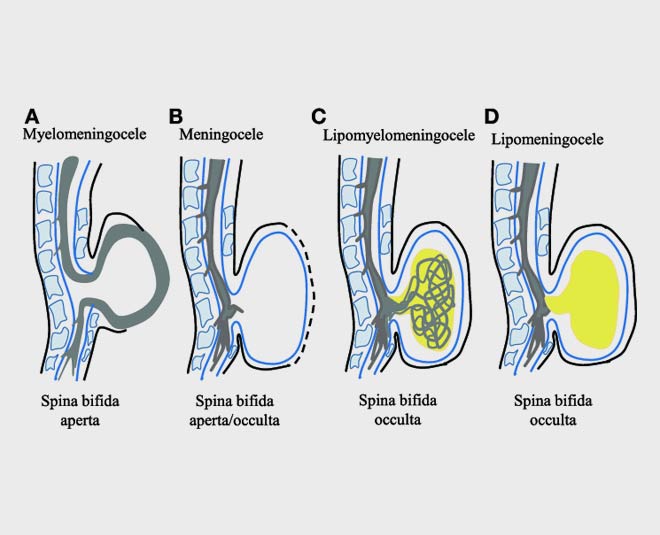
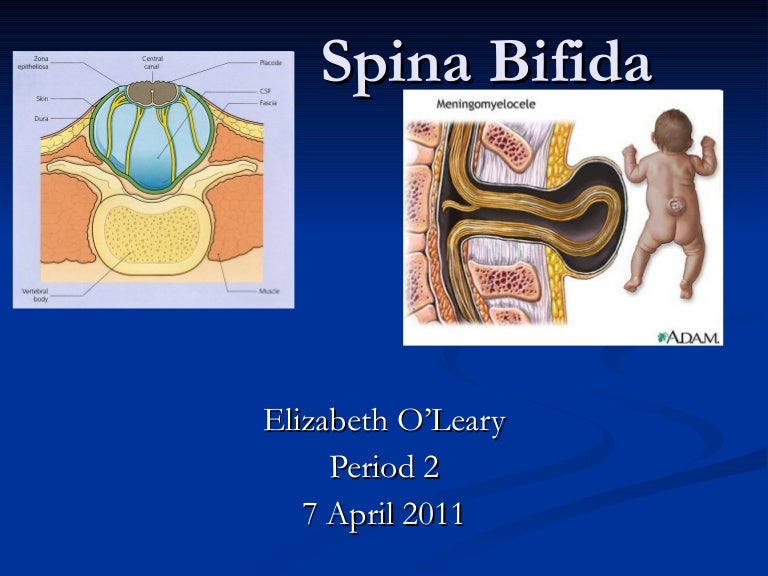
Spina bifida is Latin for ‘split spine’. It is one of a class of serious birth defects called neural tube defects (NTD). It is an abnormality of the folding of the posterior surface of the embryo, which normally forms the vertebral column with its muscles and the spinal cord and the spinal nerves.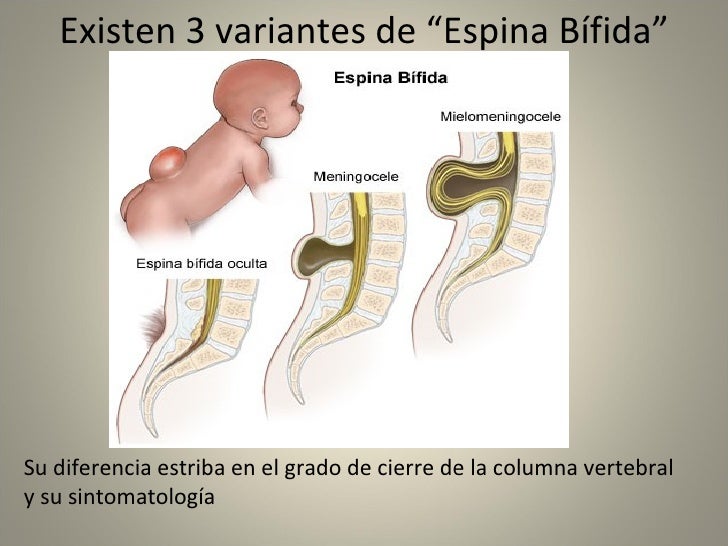
Because of this abnormality, the growing embryo does not develop normally and the spinal cord and nerves are exposed on the surface of the back, instead of being inside a canal of bone surrounded by muscle. This means that the spinal cord and nerves can be easily damaged.
Almost always, the nerves supplying the parts of the body located below the level of the exposed area do not function properly, leading to a range of motor and sensory problems, and disturbance of bodily functions, such as bowel and bladder.
The other main type of NTD is anencephaly in which the brain and upper part of the skull are not developed properly. All babies with anencephaly will either be stillborn or die soon after birth.
Pregnant woman or women planning to become pregnant should take folate regularly to reduce the risk of the fetus developing spina bifida.
Most cases of spina bifida are detected before birth. Spina bifida cannot be cured, but a range of treatments and management options is available.
Diagnosis of spina bifida
Approximately 90 per cent of cases of spina bifida are detected with an ultrasound scan before 18 weeks of pregnancy. Other tests used to diagnose spina bifida are maternal blood tests which measure alpha-fetoprotein (AFP), and magnetic resonance imaging (MRI) scans.
If spina bifida is present, specialist obstetric care and support will be provided. Consultation with an expert paediatrician is available at both the Royal Children’s Hospital and Monash Children’s Hospital.
In open spina bifida where the cord and nerves are exposed (called spina bifida aperta), it is important to close the defect within the first few days of life to avoid infection, excess drainage of cerebrospinal fluid and further damage to the spinal cord and nerves.
Occasionally, spina bifida is not detected until birth when a large soft lump or skin covered lesion on the baby’s back is noticed. This lump contains spinal cord, nerves and often fatty tissue (called a lipomeningocoele). The need for surgery in this situation is not urgent, because the spinal cord and nerves are not exposed.
The need for surgery in this situation is not urgent, because the spinal cord and nerves are not exposed.
Symptoms of spina bifida
The effects of spina bifida vary according to the type, location and severity of the condition. It can be located in the neck, chest or lumbar spinal region. The low thoracic upper lumbar lesions (in the mid-back area) generally produce a greater degree of paralysis and other debilitating complications.
Problems associated with spina bifida include:
- reduced sensation in the lower body, legs and feet, leading to the possibility ofburns and pressure sores
- a degree of paralysis of the lower body and legs, causing walking difficulties or inability to walk
- different degrees and types of urinary incontinence
- different degrees and types of faecal bowel incontinence
- some sexual dysfunction, particularly related to penile erection and ejaculation
- deformities of the spine – commonly scoliosis, where the spine bends into an ‘S’ shape
- cord tethering, where the spinal cord sticks to the area of the original lesion and becomes stretched
- Arnold Chiari malformation – an abnormality of the back of the brain and upper spinal cord which can cause disturbance of breathing, swallowing, eye movement and fluid flow leading to hydrocephalus
- learning difficulties.
Spina bifida and hydrocephalus
The brain and spinal cord are bathed in and nourished by cerebrospinal fluid. Most people with spina bifida have the Arnold Chiari malformation and about 80 per cent have abnormality of cerebrospinal fluid flow causing hydrocephalus (Latin for water on the brain).
Hydrocephalus may be managed early with a shunt if adequate absorption of fluid does not occur. This shunt drains the fluid away from the brain to parts of the body where no damage can be done. The brain looks structurally different in people with spina bifida, but it can function normally. It is not uncommon, however, to have some brain function disability.
Causes of spina bifida
Neural tube defects (both anencephaly and spina bifida) are caused by genetic and environmental factors that are not yet fully understood. The risk of these conditions is approximately one in every 800 pregnancies. Inadequate intake of folate by the mother in early pregnancy is a significant factor in the occurrence of spina bifida.
The number of babies born with spina bifida in Australia has dropped dramatically in recent years due to greater awareness and intake of folate by women prior to and in the early stages of pregnancy.
Improved ultrasound and other tests that detect spina bifida and provide the choice of pregnancy termination have also reduced its occurrence.
High-risk groups
People whose children are at high risk of spina bifida include those who have a:
- previous child with a neural tube defect (NTD)
- family history of NTDs on one or both sides
- close relative with an NTD
- close relative with a child with an NTD.
The children of women taking some anti-epileptic medications (such as valproic acid) also have an increased risk of spina bifida.
Folate can prevent spina bifida
Folate (folic acid) is a B-group vitamin. The recommended dose of folate, taken daily one month before conception and each day during the first three months of pregnancy, can prevent most neural tube defects.
The National Health and Medical Research Council recommends that all women planning a pregnancy or likely to become pregnant should take 0.5 mg of folic acid daily. People in high-risk groups should take a higher dose.
Good sources of folate include:
- folate supplements
- foods naturally rich in folate – asparagus, spinach, oranges, bananas and legumes
- foods fortified with folate, such as some breakfast cereals and bread. Look for the ANZFA Folate Enriched logo on the packet.
Treatment for spina bifida
There is no cure for spina bifida. Treatment options include:
- Surgery – may be used to close the lesion and reduce the risk of infection.
- Shunt insertion – hydrocephalus is treated with the insertion of a tube, called a shunt, into the ventricles in the brain where the spinal fluid is produced, allowing excess cerebrospinal fluid to drain out of the brain via another tube into the abdomen or the heart.
- Orthopaedic surgery – children with spina bifida usually undergo operations on their legs and feet to improve their mobility.
- Mobility aids – walking aids or wheelchairs are commonly used.
- Diet and enemas – are used to manage faecal incontinence.
- Bladder surgery – can increase bladder size and tighten muscles.
- Self-catheterisation and continence pads – may be required to manage urinary incontinence. Sometimes faecal or urinary bags are necessary.
- Regular monitoring of kidney, bladder, shunt and spine functions.
Where to get help
- Your doctor
- Spina Bifida Clinic at the Royal Children’s Hospital Tel. (03) 9345 5898
- Fetal Diagnostic Clinic Monash Health Tel. (03) 9594 2343
- Fetal Management Unit Royal Women’s Hospital Tel. (03) 8345 2000
Things to remember
- Spina bifida refers to a range of birth defects that affect the spinal cord.
- In spina bifida some vertebrae of the spine aren’t closed, leaving the spinal cord nerves exposed and damaged.
- The recommended dose of folate, taken daily one month before conception and during the first three months of pregnancy, will greatly reduce your chances of having a child with a neural tube defect.
Prenatal ultrasonography of fetal craniofacial anomalies
Authors: Annisa Shui Lam Mak, Kwok Yin Leung
Introduction
other, more subtle anomalies, syndromes, chromosomal mutations, or even rarer conditions such as infections or metabolic disorders.
It remains a difficult process, especially in the first trimester. The frequency of detection of craniofacial anomalies (PCA) varies depending on the type of anomaly, its severity, gestational age, associated anomalies, as well as methods and technologies of ultrasound examinations. So the prevalence of cheiloschisis and craniosynostosis is about 0.15% and 0.05%, respectively.
Various professional societies, including the International Society for Ultrasound in Obstetrics and Gynecology (ISUOG), the American Institute of Ultrasound in Medicine, and the Asian Oceania Federation of Obstetrics and Gynecology, have issued recommendations for examination of the face and skull in the second trimester of pregnancy.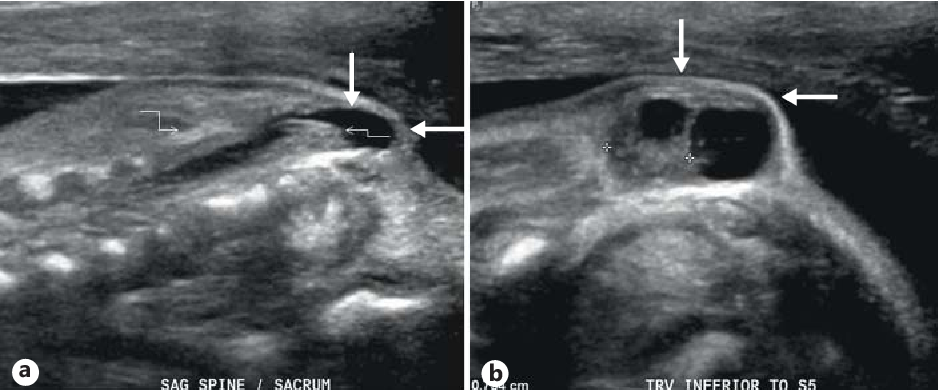 The main purpose of this article is to provide updated information on the prenatal detection of PPA in order to improve the accuracy of diagnosis.
The main purpose of this article is to provide updated information on the prenatal detection of PPA in order to improve the accuracy of diagnosis.
Changes in the brain region of the skull
The size, shape, integrity and density of the skull bone can be assessed when head size is measured and when brain structures are examined. The skull is oval in shape and has a continuous echogenic structure interrupted only by narrow echolucentric sutures. Abnormal features (Fig. 1-3) and associated anomalies are shown in Table 1.
Figure 1: Second trimester fetus with trigonocephaly.
Axial view of the fetal head (H) shows a triangular forehead (arrow).
Figure 2: Second trimester fetus with brachycephaly. Axial view of the fetal head (H) shows that the skull shape is shorter than typical (arrow).
Figure 3: Second trimester fetus with scaphocephaly.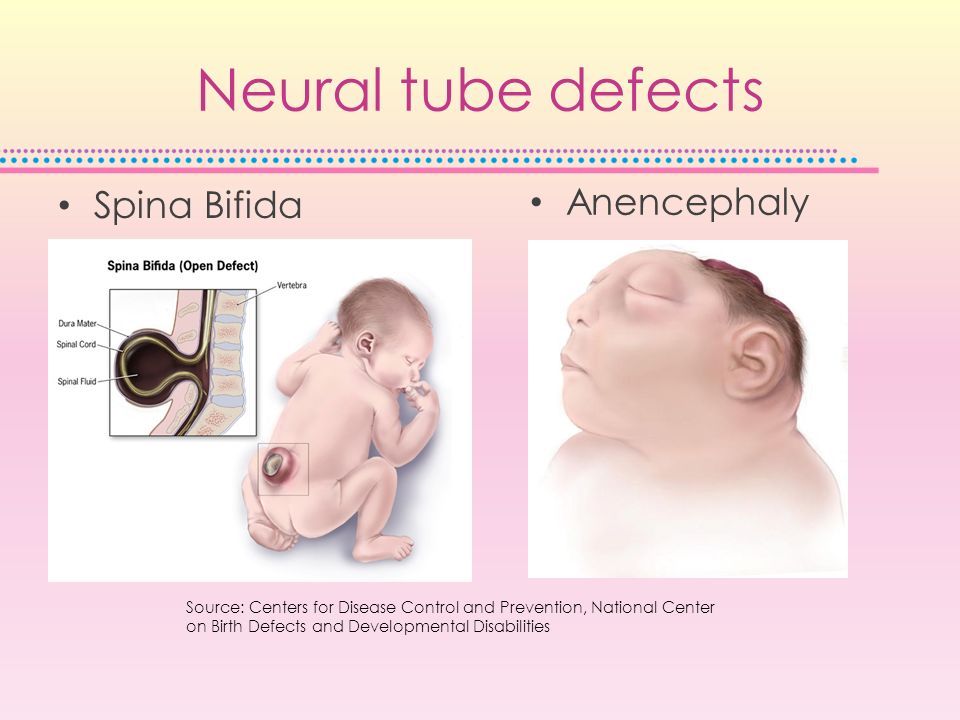
Axial view of the fetal head (H) showing a long (pointer) and narrow fetal head (arrows).
Table 1.
| Criteria | Index | Anomaly |
| Size | Small | Microcephaly |
| Large | Macrocephaly | |
| Form | Not oval, lemon-shaped | Spina bifida, trisomy 18 or skeletal dysplasia |
| Integrity | Defect in the skull bone with protrusion of brain tissue | Encephalocele |
| Density | No echogenicity, skull easily compressed | Weak mineralization, osteogenesis imperfecta or hypophosphatasia |
Diagnosis of craniosynostosis is expressed in the loss of hypoechogenicity in the segment of the main sutures of the skull, along with the expansion of other orthogonal sutures. Indirect signs, including abnormal cephalic index (CI), skull shape (Table 2), and/or facial morphology such as hypotelorism or hypertelorism, may precede suture closure by weeks 4-16. CIs below 70% or above 85% indicate dolichocephaly and brachycephaly, respectively.
Indirect signs, including abnormal cephalic index (CI), skull shape (Table 2), and/or facial morphology such as hypotelorism or hypertelorism, may precede suture closure by weeks 4-16. CIs below 70% or above 85% indicate dolichocephaly and brachycephaly, respectively.
Table 2.
| Shape anomaly | Seam | Associated anomalies |
| Scaphocephaly / Dolichocephaly (long) | Sagittal | – |
| Brachycephaly (short, wide) | Bilateral coronal | Down syndrome Pfeiffer syndrome |
| Plagiocephaly (ipsilateral frontal or occipital flattening) | Single-ended coronal or lambdoid | – |
| Trigonocephaly (forward direction) | Metopic | Jacobsen syndrome or Smith-Lemli-Opitza syndrome |
| Clover (trilobite) | Sagittal, coronal and lambdoid | Thanatophoric dysplasia, Apert syndrome, Crouzon syndrome Carpenter's syndrome |
| Oxycephaly (pointed or conical) | Sagittal and lambdoid | – |
The circumference measurement also has a role. Since a head circumference deviation of more than 3 standard units below or 2 standard units above the mean, depending on gestational age, is a clue to a possible diagnosis of microcephaly or macrocephaly, respectively.
Since a head circumference deviation of more than 3 standard units below or 2 standard units above the mean, depending on gestational age, is a clue to a possible diagnosis of microcephaly or macrocephaly, respectively.
However, the use of these reference values may lead to an overdiagnosis of microcephaly. Other supporting signs should be looked out for, which include forehead deformity, a flat occiput, or intracranial contents that are abnormal or invisible.
DO YOU CARE THE ULTRASONIC MACHINE CORRECTLY?
Download the care guide now
Facial changes
The facial examination should be performed in three planes to assess different facial structures as this facilitates the detection of anomalies (Table 3). According to the ISUOG guidelines, the minimum assessment of the fetal face includes the presence of both orbits, the assessment of the nose/nostrils, the presence of the mouth and, preferably, the assessment of the profile of the face and lips.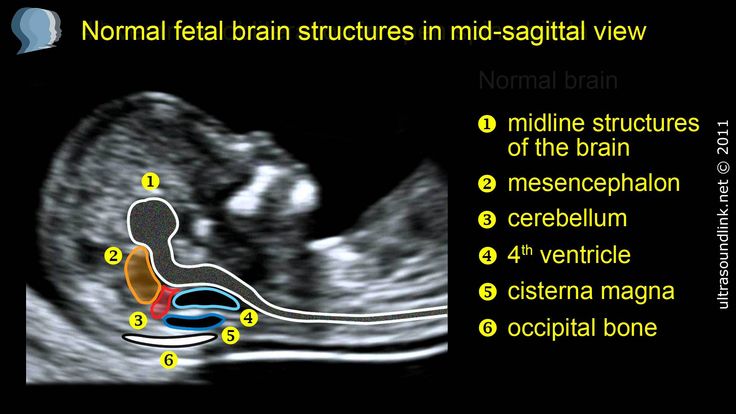
Table 3.
| Flat | Structure | Index | Anomaly |
| Crown | Lips | Integrity violation | Cheiloschisis |
| Roth | Small or continuous, open | Microstomia or syndromes | |
| Nose | Tapered or one nostril available | Hypoplasia or single nostril syndrome | |
| Palpebral groove | Tilt up or down | ||
| Cross | Orbits | Small, absent, abnormal interocular diameter | Microphthalmia / anophthalmia, hypotelorism / hypertelorism |
| Medial cyst | Lacrimal sac cyst | ||
| Crystal lens | Echogenic | Cataract | |
| Dental buds | Cracks, abnormal number | Cleft palate, oligodontia / anodontia | |
| Lower jaw | Small | Micrognathia | |
| Tongue | Missing or double equal sign | Cleft uvula | |
| Ears | Wrong size, shape, location or deployed | Anomaly of ear development | |
| Sagittal | Lob | Convex | Skeletal dysplasia |
| Flattened | Microcephaly | ||
| Hanging | Extension nose | ||
| Nose | Flattened | Syndromes | |
| Absence or shortening of the nasal bone | Aneuploidy | ||
| Upper jaw | Premaxillary protrusion | Bilateral Cleft Facial | |
| Soft sky | No soft palate or "equal sign" | Cleft palate, accessory uvula | |
| philtrum | Long or short | Syndromes | |
| Lower jaw | Small | Micrognathia | |
| Symmetry | Facial asymmetry | ||
| Language | Large, protruding, massively displaced backwards | Macroglossia, tumor glossoptosis | |
| Ears | Abnormal size, shape or location or deployed | Anomaly of ear development |
A cleft is diagnosed when the integrity of the lip is lost on one or both sides on the coronal view (Fig.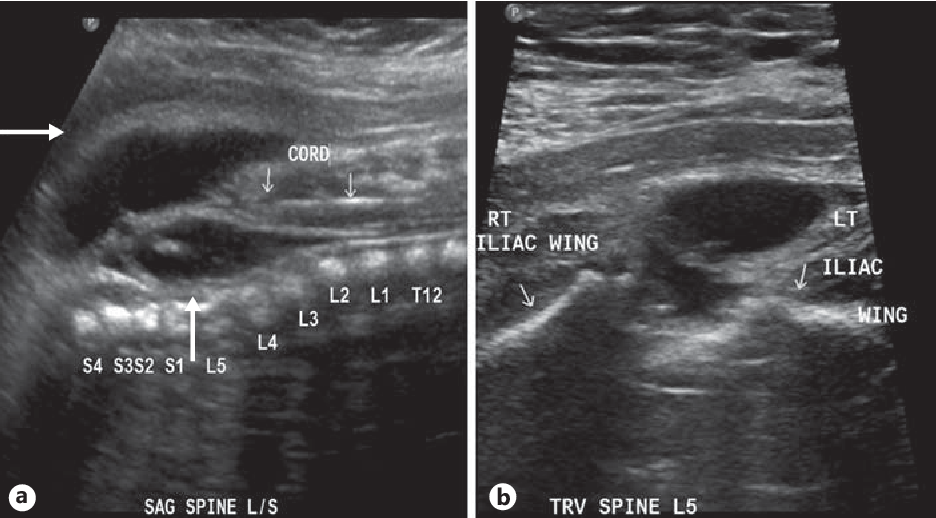 4, 5). Bilateral cleft lip suggests a premaxillary bulge in sagittal view (Fig. 6). It is difficult to diagnose an incomplete cleft lip (Fig. 7), often only a cleft palate is visible. Using color Doppler, one can see the flow of amniotic fluid normally passing through the nostrils during breathing activity, in case of an anomaly through the palate when it has a cleft.
4, 5). Bilateral cleft lip suggests a premaxillary bulge in sagittal view (Fig. 6). It is difficult to diagnose an incomplete cleft lip (Fig. 7), often only a cleft palate is visible. Using color Doppler, one can see the flow of amniotic fluid normally passing through the nostrils during breathing activity, in case of an anomaly through the palate when it has a cleft.
Figure 4: Second trimester fetus with unilateral cleft lip.
Coronal view of the fetal face showing loss of integrity (arrow) of the upper lip (L).
Figure 5: Second trimester fetus with bilateral cleft lip.
Coronal view of the fetal face showing loss of integrity (arrows) of the upper lip (L) on both sides (1 and 2).
Figure 6: Second trimester fetus with premaxillary bulge.
Sagittal view of the fetal face showing a soft tissue mass (arrow) projecting forward under the nose (N).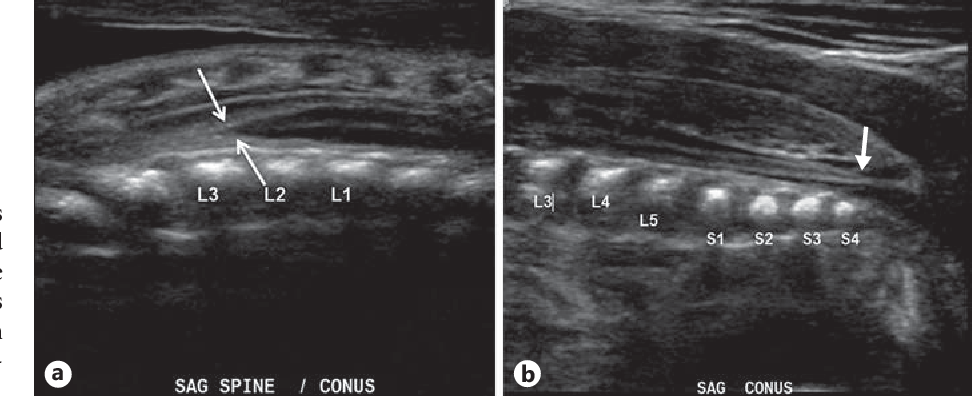
Figure 7: Second trimester fetus with partial unilateral cleft lip. The coronal plane of the fetal face shows partial loss of integrity (arrows) of the upper lip (L).
The face profile can be assessed from the mid-sagittal projection. In particular, frontal bulges (Fig. 8), micrognathia (Fig. 9), or a flat nose (Fig. 10) may be found. From the lateral side, ear anomalies can be assessed (Fig. 11). Both eyes and their anomalies can be assessed in the axial plane (Fig. 12-14).
Figure 8: Second trimester fetus with prominent forehead.
Mid-sagittal view showing a straight bulge (arrow) of the forehead (FH).
Figure 9: Second trimester fetus with micrognathia.
Mid-sagittal view showing a small and receding (arrow) chin (C).
Figure 10: Second trimester fetus with flat nose.
Mid-sagittal view showing a flat (arrow) nose (N).
Figure 11: Second trimester fetus with ear anomaly.
Lateral sagittal view showing a small (arrows) right (R) ear (E) with loss of normal structure.
Figure 12: Second trimester fetus with hypotelorism.
The axial view shows the anomalously reduced distance (arrows) between the two orbits (circle).
Figure 13: Second trimester fetus with bilateral cataract.
Axial view showing echogenicity (arrows) in the lens (L) of both eyes.
Figure 14: Second trimester fetus with protrusion between two orbits. The axial view shows a soft tissue mass (arrows) protruding between two orbits (circles).
It is worth distinguishing between micrognathia (small lower jaw) and retrognathia - displacement of the jaw to the rear. It is differentiated by determining the lower angle of the face in relation to the width of the lower jaw to the width of the upper jaw.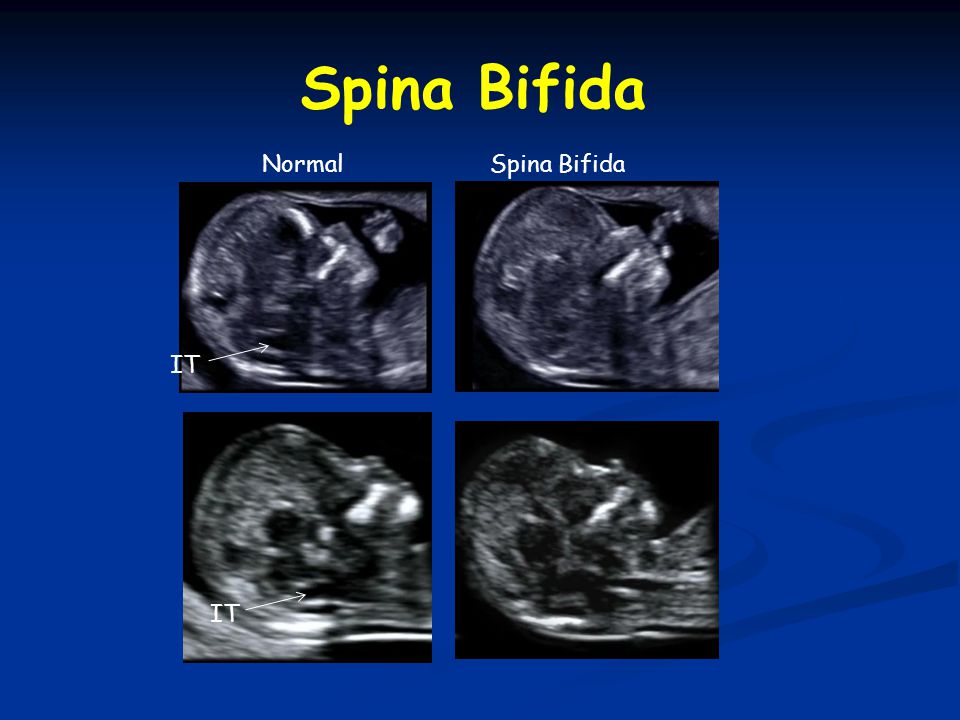 With a confounded family history or if an anomaly is suspected, measurements of fetal structures such as nasal bone length, ear length, maxillary length, and eye and interocular space diameters may be performed.
With a confounded family history or if an anomaly is suspected, measurements of fetal structures such as nasal bone length, ear length, maxillary length, and eye and interocular space diameters may be performed.
3D/4D 3D Imaging
The use of 3D ultrasound, including surface imaging, multiplanar and multilayer imaging, allows accurate assessment of various craniofacial structures and their anomalies, including cleft palate (Figs. 15, 16) and craniosynostosis. Images may be useful for counseling (Figures 17, 18). The use of 3D (Fig. 19) can help differentiate closed and open sutures. The use of 4D can be used to evaluate facial expressions.
Figure 15: Second trimester fetus with bilateral cleft lip and palate. 3D axial view showing loss of integrity (arrows) of the lip (L) and palate (P) on both sides.
Figure 16: Second trimester fetus with midline cleft lip and palate. 3D axial view showing midline loss of integrity (arrows) of the lip (L) and palate (P). The colored boxes on the right show the orientation of the active images on the left: axial view (1), sagittal view (2), and coronal view (3).
The colored boxes on the right show the orientation of the active images on the left: axial view (1), sagittal view (2), and coronal view (3).
Figure 17: Second trimester fetus with unilateral cleft lip.
3D surface view of the fetal face showing a cleft (arrow) on the upper lip (L).
Figure 18: Second trimester fetus with midline cleft.
3D superficial image of the fetal face shows a cleft (arrow) in the midline of the upper lip (L).
Figure 19: Second trimester fetus with craniosynostosis.
3D skeletal superficial, axial view of the skull showing constriction (arrows) of the coronal suture (CS) and part of the anterior fontanelle (AF).
First trimester ultrasound
Between 11 and 13 weeks, during the 6 days of pregnancy, the ISUOG guidelines suggest measuring the biparietal diameter and head circumference, as well as assessing the integrity and echogenicity of the skull. Attempts can be made to evaluate the orbits, interorbital distances, facial profile, ears, and integrity of the mouth and lips. In the first trimester, a flattening of the profile can be detected (Fig. 20). However, some craniofacial anomalies, such as craniosynostosis, cannot be diagnosed in the first trimester, and thus a second trimester scan of the anomaly remains the standard for fetal anatomic evaluation.
Attempts can be made to evaluate the orbits, interorbital distances, facial profile, ears, and integrity of the mouth and lips. In the first trimester, a flattening of the profile can be detected (Fig. 20). However, some craniofacial anomalies, such as craniosynostosis, cannot be diagnosed in the first trimester, and thus a second trimester scan of the anomaly remains the standard for fetal anatomic evaluation.
Figure 20: First trimester fetus with flat facial profile.
Sagittal view showing flat forehead (FH) (arrow), nose (N) (arrow) and drooping chin (C) (curved arrow).
Lateral investigations
When a cleft palate is found, it is important to determine whether it is unilateral, bilateral, or median, and whether there is any cleft plate or amniotic streak, because this varies the prognosis and associated conditions . Combined cleft lip and palate is more common than cleft lip itself, and the associated problems are more serious.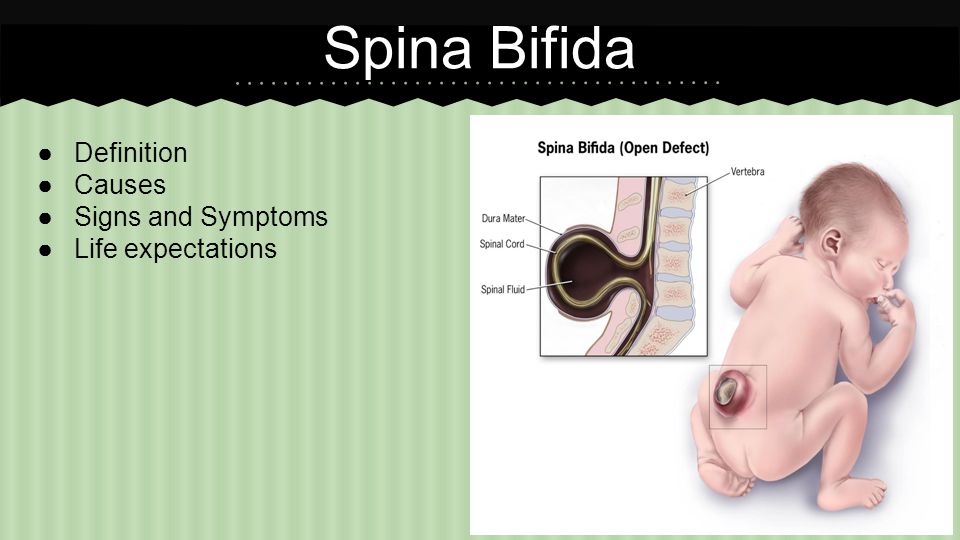 Unilateral/bilateral and median cleft lip are considered different conditions as they have different embryological origins.
Unilateral/bilateral and median cleft lip are considered different conditions as they have different embryological origins.
Whenever a craniofacial anomaly is detected, it is important to perform a detailed scan to look for additional anomalies, especially other potentially subtle malformations of the face, central nervous system, heart, or extremities. Many craniofacial anomalies, including facial clefts, micrognathia, craniosynostosis, hypertelorism/hypothalmia, microphthalmia/anophthalmia, cataracts, and anotia/microtia, are associated with various syndromes and conditions (Table 4).
Overall, 10% of clefts were accompanied by a chromosomal abnormality and 27% had an associated abnormality. Approximately 15% of cases of craniosynostosis are syndromic. Protrusion of the tongue can be a sign of Beckwith-Wiedemann syndrome or Down syndrome.
Table 4.
| Anomaly | Associated defects | Syndromes |
| Cleft face | Upper limbs | Ectrodactyly, ectodermal dysplasia, splitting syndrome, oral-facial syndrome type I |
| Cleft face | Other anomalies of the facial skull and heart | CHARGE syndrome (coloboma, cardiac anomaly, choanal atresia, mental retardation, genital and ear anomalies) |
| Micrognathia | Ears | Goldenhar syndrome |
| Micrognathia | Limbs | Hypogenesis mouth-mandible-limb syndrome, Nager syndrome, splitting syndrome, Roberts syndrome |
| Micrognathia | Other anomalies of the facial skull | Robin Syndrome, Treacher Collins Syndrome |
| Craniosynostosis | Other anomalies of the facial skull and limbs | Apert syndrome, Crouzon syndrome, Carpenter syndrome, thanatophoric dysplasia, Pfeiffer syndrome, Saetre-Chotzen syndrome, Muencke syndrome, Jackson-Weiss syndrome, Antley-Bixtler syndrome, Wolff-Hirshhorn syndrome (4p) |
Prognosis
Prognosis and management depend on the type and severity of craniofacial anomalies, the underlying condition, or chromosomal mutations.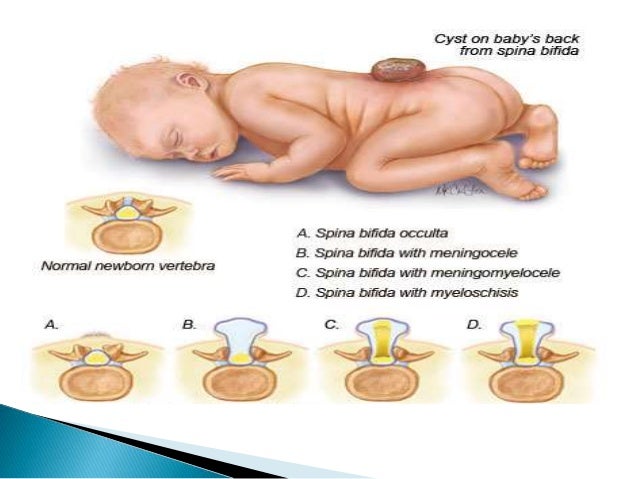 If the prognosis is poor, such as in the case of multiple anomalies or associated aneuploidies, the option of terminating the pregnancy may be offered, depending on gestational age and local norms. Alternatively, continuation of pregnancy with prenatal counseling is appropriate for mild and isolated disorders such as cleft lip.
If the prognosis is poor, such as in the case of multiple anomalies or associated aneuploidies, the option of terminating the pregnancy may be offered, depending on gestational age and local norms. Alternatively, continuation of pregnancy with prenatal counseling is appropriate for mild and isolated disorders such as cleft lip.
Isolated macrocephaly (with a head circumference that is 2-3 standard deviations above the mean for gestational age), dolichocephaly, and brachycephaly usually have a favorable outcome.
In our catalog you can choose devices for examinations in the field of obstetrics and gynecology from leading manufacturers of ultrasound equipment. Contact our manager to clarify the details and choose the model that is best for you.
spina bifida operation using cord blood
02/12/2020
HEMAFUND
Little Emma was born in 2015. Even during pregnancy, the parents found out that the girl has malformations of the spine, when the vertebrae remain not fully developed.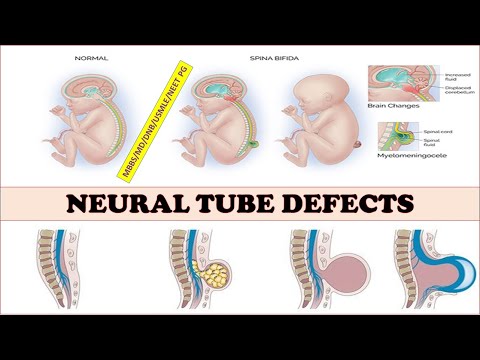 The diagnosis - Spina bifida (spina bifida) finally sounded at the 35th week of pregnancy.
The diagnosis - Spina bifida (spina bifida) finally sounded at the 35th week of pregnancy.
“It was our first wedding anniversary,” says Daria, “my husband and I went for an ultrasound scan to look at our daughter, and learned this terrible news. I had never heard of such a disease before. I didn’t even look for information - I hoped to the last that the doctors were wrong, and my child was healthy.
Subsequently, it turned out that preparing for the birth of a baby with such a diagnosis is quite complicated. “Maternity hospitals one after another refused me,” recalls Emma’s mother,
Only doctors from the 5th maternity hospital in Kyiv agreed to perform a caesarean section if we find a neurosurgeon who will immediately perform the operation on my daughter. This neurosurgeon was Plavsky Pavel Nikolaevich. It was he who said that we need to collect cord blood, because it will help our daughter during the operation.”
Is there at least one thing in the world that can be more important than the health of a child? It is hardly possible to come up with such a thing.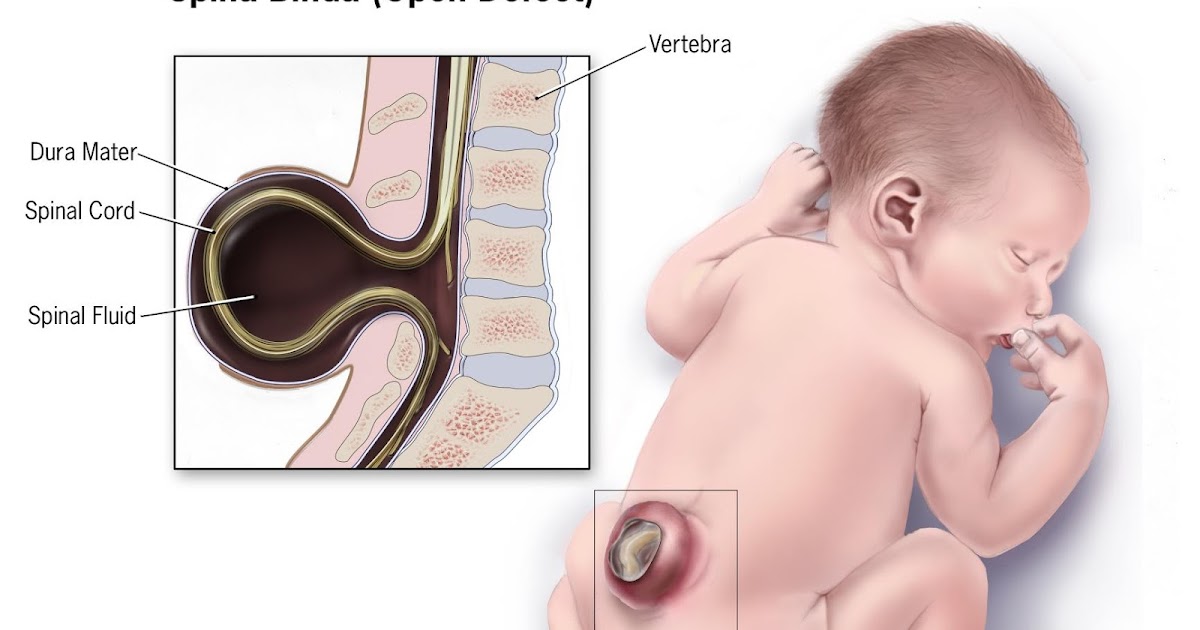 Every pregnant woman thinks only about how to give the baby a happy future. Experiencing unbearable pain and fear during childbirth, she dreams of quickly pressing her newborn baby to her chest. But sometimes these thoughts recede ... When it becomes known during pregnancy that the baby has congenital defects, parents are forced to put aside time for dreams and focus on the existing problem.
Every pregnant woman thinks only about how to give the baby a happy future. Experiencing unbearable pain and fear during childbirth, she dreams of quickly pressing her newborn baby to her chest. But sometimes these thoughts recede ... When it becomes known during pregnancy that the baby has congenital defects, parents are forced to put aside time for dreams and focus on the existing problem.
Darya says that during the birth she was constantly thinking about the “red bag with a heart” that would help save the life of her newborn daughter:
“When I was in intensive care before the caesarean section, HEMAPHOD couriers brought a container for cord blood sampling. I constantly kept this red bag in my field of vision, and I was very scared when I forgot to take it with me to the “caesarean”. The pregnant woman didn't even let the nurse go for the container. I went for the bag myself, despite the needle from the dropper, which was inserted into a vein in my arm. “I then constantly tried to find this bag during the operation with my eyes. Even when my daughter saw her, she only thought that the doctors would not forget to collect cord blood. I calmed down only when the container with my daughter's umbilical cord blood was handed over to the HEMAFUND specialists, ”admits Daria.
Even when my daughter saw her, she only thought that the doctors would not forget to collect cord blood. I calmed down only when the container with my daughter's umbilical cord blood was handed over to the HEMAFUND specialists, ”admits Daria.
Just a few hours after her birth, Emma ended up in the neurosurgical department of Okhmatdet, where cord blood was delivered in a timely manner by a HEMAFUND vehicle.
“The operation was very difficult. Emma had a hernia on her back, into which the roots of the spinal cord had sprouted, - says Daria, - the surgeon had to fill these roots into place and remove the hernial sac. Recovery after the operation was quite fast and encouraging. A month later we were discharged from the hospital and the worst was left behind. I am sure that everything went so well thanks to the use of umbilical cord blood.”
Neurosurgeon Dr. Plavsky conducted a study in which 39 children with spina bifida received intravenous infusions of their autologous cord blood.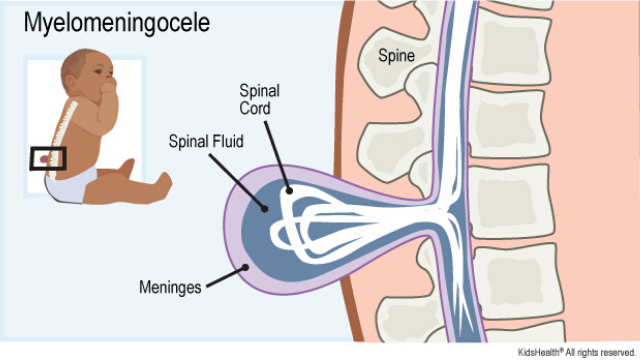 This type of surgery is performed almost immediately after birth, and cord blood was injected immediately after collection. The motivation for using cord blood during surgery was to replace blood loss and stimulate stem cell-mediated repair. The children were followed up for 16 months after surgery and showed improvement in both movement and function of the pelvic organs.
This type of surgery is performed almost immediately after birth, and cord blood was injected immediately after collection. The motivation for using cord blood during surgery was to replace blood loss and stimulate stem cell-mediated repair. The children were followed up for 16 months after surgery and showed improvement in both movement and function of the pelvic organs.
Today, Emma's illness is only a reminder of regular medical examinations and problems with her legs. The girl's parents admit that the difficulties in treatment are now associated only with the lack of comprehensive information about the disease and a comprehensive treatment program in medical institutions. Doctors tell little about the developmental features of children with spina bifida, so you have to look for information on your own, or learn from personal experience - which often becomes “painful”.
Spina bifida is a birth defect in which, during early pregnancy, there is incomplete closure of the vertebrae in the spine and the membranes around the spinal cord.