Uti feeling during pregnancy
Urinary tract infections (UTIs) in pregnancy - symptoms, causes
Urinary tract infections (UTIs) in pregnancy - symptoms, causes | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a urinary tract infection?
A urinary tract infection (UTI) is an infection of the urinary system. UTIs are the most common bacterial infection that women develop during pregnancy. They can occur in different parts of the urinary tract, including the bladder (cystitis), urethra (urethritis) or kidneys (pyelonephritis). Sometimes when a UTI develops and bacteria are detected in the urinary tract, you may not have any symptoms of an infection. This is known as asymptomatic bacteriuria.
While anyone can get a UTI, they are much more common in women than men and they are also more likely to occur in the very young and the elderly.
What are the symptoms of UTIs during pregnancy?
Common symptoms of a UTI during pregnancy are similar to those that you might experience at any other time, and include:
- a burning sensation when you pass urine
- feeling the urge to urinate more often than usual
- urinating before you reach the toilet (‘leaking’ or incontinence)
- feeling like your bladder is full, even after you have urinated
- urine that looks cloudy, bloody or is very smelly
- pain above the pubic bone
- fever
Sometimes the first sign of an infection is a faint prickly sensation when you pass urine. If the infection is more advanced and has moved up to the kidneys, you may also experience fever with a particularly high temperature, back pain and vomiting.
What are the common causes of UTIs?
Your urinary tract is normally free of bacteria. If bacteria enter the tract and multiply, they can cause a UTI. There are several factors that increase the risk of developing an infection:
- Infection with common bacteria in your gut, usually from faeces (poo) can contaminate your urinary tract
- Being sexually active increases the risk of bacteria moving around the genital area and entering the urinary tract
- If you have weak pelvic floor muscles your bladder might not empty completely, which can lead to an infection
- Women with diabetes are at increased risk of developing a UTI since the sugar in their urine may cause bacteria to multiply
Are UTIs a risk during pregnancy?
During pregnancy, many changes occur in your body that increase your risk of developing a UTI, including changes to the make-up of your urine and immune system. As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
UTIs can affect women whether they are pregnant or not. However, pregnant women are more likely to develop repeated or more severe infections. Up to 1 in 10 pregnant women will have a UTI but not have any symptoms at all.
Is there a risk to my baby?
Having a UTI during pregnancy can increase your risk of developing high blood pressure, and your baby may be born early and smaller than usual. For this reason, even if you don’t have any symptoms, it is important to treat a UTI as soon as possible.
How are UTIs diagnosed?
UTIs are diagnosed by taking a urine sample which is checked in a laboratory for bacteria. Your doctor may also perform a physical examination if they think you have an infection.
All pregnant women are offered a urine test, usually at their first antenatal visit or soon after. You may need to repeat the urine test if you have a history of UTIs; have symptoms of a UTI; have a contaminated sample or if your doctor thinks you are at high risk of developing a UTI. If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
How are UTIs treated during pregnancy?
When you have a UTI, it is important to drink plenty of water to flush out the urinary tract. UTIs are treated with antibiotics that are safe in pregnancy. Your doctor will select the right antibiotic, based on your infection and the type of bacteria found in your urine sample.
Can I prevent UTIs?
You can lower your risk of developing a UTI during pregnancy by:
- drinking plenty of fluids, especially water
- quickly treating any vaginal infection that may occur, including thrush or a sexually transmitted infection
- avoiding becoming constipated
Some women have also found the following tips helpful:
- urinate immediately after sex
- don’t delay going to the toilet — go as soon as you feel the need
- wipe from the front to the back after going to the toilet
- wear cotton underwear
When should I see my doctor?
See your midwife or doctor if you have any symptoms of a UTI. It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
More information
UTIs are very common during pregnancy, and are best treated early. If you notice the symptoms of an infection, seek medical advice from your doctor, midwife or pharmacist.
For more information on UTIs, visit the Kidney Health Australia page on UTIs.
Sources:
Government of South Australia (Urinary Tract Infection in Pregnancy), Jean Hailes (Urinary Tract Infections), Kidney Health Australia (Factsheet: Urinary Tract Infections), Government of Western Australia North Metropolitan Health Service (Urinary Tract Infection in Pregnant Women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2021
Back To Top
Related pages
- Frequent urination during pregnancy
- Incontinence during pregnancy
Need more information?
Urinary tract infection (UTI) - MyDr.
 com.au
com.au Urinary tract infection occurs when part of the urinary tract becomes infected. UTIs are usually caused by bacteria and generally clear up with a course of antibiotics.
Read more on myDr website
Urinary tract infections (UTIs) explained - NPS MedicineWise
Learn about the causes & treatments for urinary tract infections (UTIs).
Read more on NPS MedicineWise website
Urinary tract infection (UTI) | SA Health
Urinary tract infection (UTI) is an infection of the urinary system. Infection may occur in the kidneys, bladder or urethra.
Read more on SA Health website
Urinary Tract Infections (UTIs) | Jean Hailes
A comprehensive guide to urinary tract infections.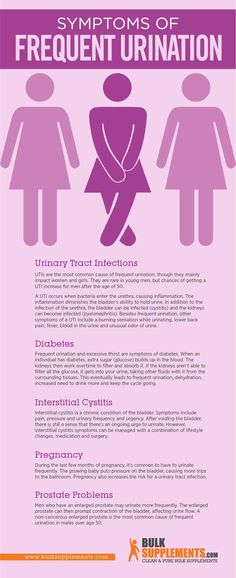 Everything you should know about UTIs including causes, symptoms, management and treatment.
Everything you should know about UTIs including causes, symptoms, management and treatment.
Read more on Jean Hailes for Women's Health website
Incontinence & Bladder Weakness | Jean Hailes
What makes a normal bladder. Types of incontinence. Causes and symptoms. Diagnosis and treatment. Prevention and management.
Read more on Jean Hailes for Women's Health website
Pyelonephritis
Infection of the kidneys.
Read more on Queensland Health website
Check-ups, tests and scans available during your pregnancy
Antenatal care includes several check-ups, tests and scans, some of which are offered to women as a normal part of antenatal care in Australia. Learn more here.
Learn more here.
Read more on Pregnancy, Birth & Baby website
Thrush | SA Health
Thrush or Candidiasis is a common vaginal infection, caused by an overgrowth of yeasts and is not considered to be a sexually transmitted infection
Read more on SA Health website
Pregnancy at week 9
Your baby is now the size of a peanut. You won't be showing just yet, but you may have put on a little weight.
Read more on Pregnancy, Birth & Baby website
Your first antenatal visit
Find out what will happen and what you can learn during your first antenatal care visit with your GP or midwife.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
UTIs During Pregnancy: Symptoms, Treatment, Common Questions
Urinary tract infections (UTIs), also known as bladder infections, are the most common type of bacterial infection diagnosed today, according to research published in the American Journal of Medicine. Roughly 31 percent of pregnant women will have either a symptomatic or an asymptomatic (without symptoms) UTI during pregnancy, research suggests. UTIs occur when bacteria enters into the usually sterile urinary tract and multiplies, causing painful urination and other symptoms. Certain factors during pregnancy make this occurrence more likely to happen.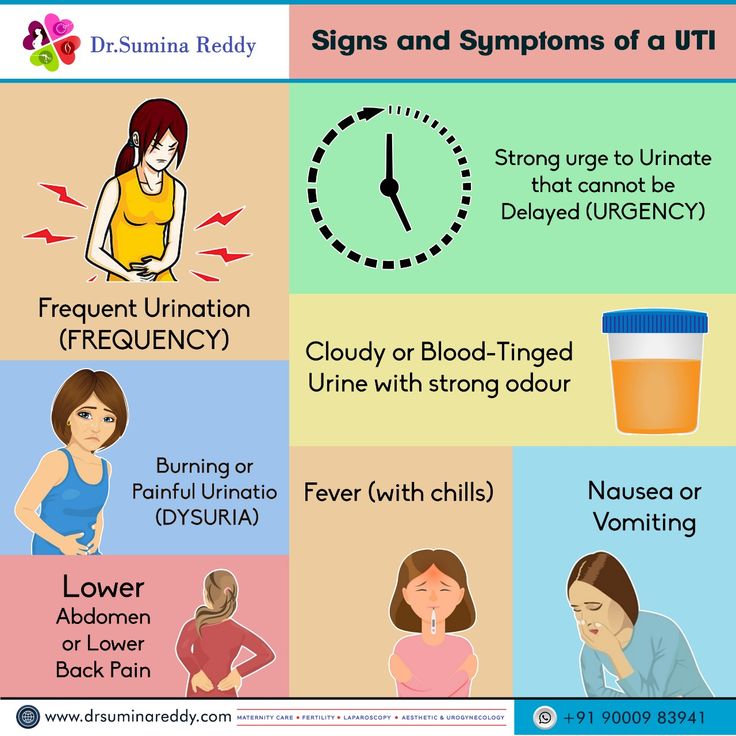 Here’s what you need to know to keep you and your baby healthy.
Here’s what you need to know to keep you and your baby healthy.
RELATED: 8 Home Remedies for Urinary Tract Infection (UTI) Symptoms
Why Are UTIs Common in Pregnant Women?When you’re pregnant, the anatomy of your urinary tract actually changes. For instance, your kidneys become larger and your growing uterus can compress your ureters and bladder. Because of this compression, fully emptying your bladder during pregnancy becomes more difficult. In addition, your progesterone and estrogen levels increase during pregnancy, which can weaken your bladder and ureters. Pregnancy also alters the makeup of your urine, reducing the acidity and increasing the amount of protein, hormones, and sugar in your urine. That excess sugar, for one, can encourage bacterial growth. All of the above contribute to a heightened chance of developing a UTI in pregnancy. And that is why it’s recommended that all pregnant women receive a urinalysis and urine culture at 12 to 16 weeks or during the first prenatal visit.
RELATED: 7 Things an Anesthesiologist Wants You to Know About Pain
UTIs by Pregnancy TrimesterYour risk of UTI goes up beginning at week 6 of your pregnancy; the chances you’ll have a UTI vary by trimester.
First TrimesterAbout 41 percent of UTIs are diagnosed during the first trimester. Because getting a UTI during the first trimester is so common, the U.S. Preventive Services Task Force recommends that your healthcare provider obtain a urinalysis and urine culture at your first prenatal visit. That recommendation holds whether you present with UTI symptoms or not.
Second TrimesterAccording to the Centers for Disease Control and Prevention, about half as many pregnant women are diagnosed with a UTI during their second trimester compared with the first trimester.
Third TrimesterCompared with the second trimester, the number of women who experience a UTI during the third trimester is almost halved. However, 80 to 90 percent of acute kidney infections in pregnancy (many caused by the progression of an untreated UTI) occur in the second and third trimesters, according to research published in the Archives of Medical Science. Thus, it’s recommended to do a repeat urine culture during the third trimester, too.
However, 80 to 90 percent of acute kidney infections in pregnancy (many caused by the progression of an untreated UTI) occur in the second and third trimesters, according to research published in the Archives of Medical Science. Thus, it’s recommended to do a repeat urine culture during the third trimester, too.
“While mildly painful urination during pregnancy can often mean a yeast infection, not a UTI, it’s always best to see your healthcare provider if you experience any symptoms,” says Heather Bartos, MD, an ob-gyn in Cross Roads, Texas. After all, research suggests that about 18 percent of UTIs that occur during pregnancy are symptomatic UTIs, meaning the telltale UTI signs and symptoms are present:
- Strong and frequent urge to use the bathroom
- Burning while urinating
- Regularly passing only small amounts of urine
- Cloudy, red, pink or cola-colored urine
- Foul-smelling urine
- Pelvic pain, usually in the center of the pelvis
In pregnancy, women are also more susceptible to asymptomatic UTIs, meaning you have significant bacteria in your urine but your urinary tract is free of signs and symptoms. Experiencing no symptoms, however, does not mean that asymptomatic UTIs are benign. “An asymptomatic UTI can lead to a symptomatic UTI or even a kidney infection,” says Dr. Bartos. In fact, research shows that if asymptomatic UTIs are left untreated, 30 percent of pregnant women will go on to develop a symptomatic UTI, and half of those women will eventually be diagnosed with acute pyelonephritis (a kidney infection). Up to 23 percent will have a kidney infection recurrence during the same pregnancy. It’s important to note that classic UTI signs, like frequent and painful urination, may or may not occur with a kidney infection. Here, some signs to look out for:
Experiencing no symptoms, however, does not mean that asymptomatic UTIs are benign. “An asymptomatic UTI can lead to a symptomatic UTI or even a kidney infection,” says Dr. Bartos. In fact, research shows that if asymptomatic UTIs are left untreated, 30 percent of pregnant women will go on to develop a symptomatic UTI, and half of those women will eventually be diagnosed with acute pyelonephritis (a kidney infection). Up to 23 percent will have a kidney infection recurrence during the same pregnancy. It’s important to note that classic UTI signs, like frequent and painful urination, may or may not occur with a kidney infection. Here, some signs to look out for:
- High-grade fever
- Chills and rigors (sudden feeling of cold with shivering)
- Headache
- Nausea or vomiting
- Lower back pain
- Flank pain (often right side)
- Possible reduced urine output
“UTIs can rapidly progress to a kidney infection in pregnancy, which can be much more dangerous than a kidney infection in nonpregnant women,” says Bartos. “Severe infections can lead to respiratory problems and sepsis, which can then lead to preterm labor or even the need to urgently deliver the baby.” Beyond a kidney infection, simply having a UTI during pregnancy appears to possibly be a contributing factor to low birth weight. Women who have a UTI in pregnancy also have a 1.31-fold higher risk of developing preeclampsia, a pregnancy complication characterized by high blood pressure, according to a meta-analysis published in September 2018 in the journal Medicine. It’s thought that a UTI may alter a pregnant woman’s inflammatory response, which can spur preeclampsia.
RELATED: National Period Day Is October 19
Can Having a UTI While Pregnant Hurt the Baby?Possibly. “A UTI itself doesn’t hurt the baby directly,” says Bartos. “It’s the failure to treat a UTI that can cause things like preterm birth or, rarely, infection of the amniotic sac. ” For example, research published in American Family Physician shows that treating pregnant women who have asymptomatic UTIs decreases the incidence of preterm birth and low-birth-weight infants. That’s why screening and prompt treatment are important.
Urinary tract infections are not associated with preterm labor, according to research published in the Journal of the Chinese Medical Association. However, if a urinary tract infection is left untreated, it can progress to a kidney infection. And a kidney infection (pyelonephritis) during pregnancy can modestly increase your chances of early contractions and delivery. Research published in the American Journal of Obstetrics & Gynecology notes that women diagnosed with acute pyelonephritis in pregnancy have a 10.3 percent chance of preterm delivery compared with the 7.9 percent chance among women without a kidney infection during pregnancy.
RELATED: Common Types of Vaginal Infections
Do UTIs Differ by Trimester?At week 6, UTI risk starts to go up, with two-fifths of UTIs occurring during the first trimester. Because of the likelihood of getting a UTI during the first trimester, the U.S. Preventive Services Task Force recommends that pregnant women have a urinalysis and urine culture at their first prenatal visit — whether they have UTI symptoms or not. In the second trimester, about half as many pregnant women are diagnosed with a UTI as in the first trimester, according to the Centers for Disease Control and Prevention, and that number is almost halved again for the third trimester. However, 80 to 90 percent of acute kidney infections in pregnancy (many caused by the progression of an untreated UTI) occur in the second and third trimesters, according to data published in the Archives of Medical Science, so pregnant women should have a repeat urine culture during the third trimester.
RELATED: March Is Endometriosis Awareness Month
What Are Pregnancy-Safe UTI Treatment Options?How do you treat a UTI when pregnant? It’s similar to how you treat a UTI when not pregnant — with a few key differences. A short-course of antibiotics is the standard treatment for asymptomatic and symptomatic urinary tract infections that occur during pregnancy. There are, however, two important contrasts in treating UTIs in pregnant women versus nonpregnant women. First, asymptomatic UTIs diagnosed during the first trimester are treated with antibiotics, whereas nonpregnant women’s infections are often not treated in this manner. (Outside of pregnancy, asymptomatic bacteriuria is usually not treated with antibiotics.) Also, the preferred antibiotic drugs used to treat UTI in pregnancy often differ than what would be used while not pregnant. For instance, the following antibiotics have not been associated with any birth defects, thus are likely safe to use at any point during pregnancy:
- Penicillins Amoxicillin, ampicillin, and augmentin are in this group.
- Erythromycin Some of the brand names include Ery-Tab, Akne-Mycin, E.E.S. Eryc, and Pediamycin.
- Cephalosporins Keflex (cephalexin) is a cephalosporin.
UTI history and resistance patterns must be considered before prescribing any of these drugs.
Because certain antibiotics pose a potential risk for birth defects (anencephaly, heart defects, and cleft palate) when taken during the first trimester, they are only considered a first-line treatment for UTIs occurring during the second and third trimesters, according to the American College of Obstetricians and Gynecologists. Prescribing the antibiotics listed below during the first trimester is considered appropriate only when no other suitable alternative treatments are available:
- Nitrofurantoin Macrobid, Furadantin, and Macrodantin are in this category.
- Sulfonamides Bactrim (trimethoprim-sulfamethoxazole) is part of this class.
Be sure to double-check what your healthcare provider is prescribing, since despite the warnings, nitrofurantoin remains the most frequently prescribed antibiotic during the first trimester.
How to Prevent Urinary Tract Infections, or UTIs
Urinary tract infections, or UTIs, are the most common type of bacterial infection diagnosed today, with more than half of all women experiencing at least...
By Holly Pevzner
What Is a Urinary Tract Infection (UTI)? Symptoms, Causes, Diagnosis, Treatment, and Prevention
By Holly PevznerTreatment for Urinary Tract Infections: Antibiotics, Medication, and Home Remedies
By Holly PevznerSigns and Symptoms of Urinary Tract Infections
By Holly PevznerDiagnosing UTI: Tests and Screenings, Early Diagnosis, and Your Doctors
By Holly PevznerCauses and Risk Factors of UTIs
Urinary tract infections occur when harmful bacteria enter the urethra—the tube that carries urine out of the body. Risk factors for UTIs may differ between...
By Lindsey Konkel
Increased tone of the uterus during pregnancy
Nicotine constricts the blood vessels of the expectant mother, as well as the vessels of the placenta and umbilical cord, through which the fetus is nourished. Of course, smoking by itself is unlikely to lead to hypertonicity, but in combination with other factors, it may well
If the work is associated with constant stress, it has harmful effects or it is physically difficult, give it up as soon as possible. If this is not possible, use your rights, which are enshrined in the labor legislation of the Russian Federation
Hypertonicity must be distinguished from Braxton-Hicks contractions: it lasts much longer than these training contractions and usually does not go away on its own (or goes away only after a long time)
what is hypertonicity
, - muscle, and according to the laws of physiology, muscle tissue is reduced under the influence of any factor. Slightly the uterus contracts in women every month during menstruation, much stronger during labor pains. The uterus can also contract during pregnancy, doctors call this condition hypertonicity. What it looks like: suddenly, at some point, a woman feels that her stomach is tense, becomes hard, as if “hardening”. This state lasts for a long time - half an hour, an hour, half a day or even all day. Additionally, discomfort (or pain) in the lower back or sacrum may also appear. It is clear that such tension in the abdomen worries the mother, because since the uterus is contracting, then perhaps there is a threat of termination of pregnancy. But here it all depends on how much and how often the stomach tenses.
Braxton-Hicks contractions
It turns out that the stomach can tense up not only when there is a threat of miscarriage. Starting from the end of the second trimester, the expectant mother can feel the so-called training contractions (Brexton-Hicks contractions) - the stomach also tenses with them for a while, as if “hardening”, - in general, the sensations are the same as with hypertonicity. But the main difference between such contractions and hypertonicity is that they last for a very short time (a few seconds - a couple of minutes) and pass by themselves, as well as if you change the position of the body or take a shower. Braxton-Hicks contractions occur up to about ten times a day, and by the end of pregnancy they appear even more often. These contractions are completely normal during pregnancy, and they do not indicate any threat of interruption. It’s just that with their help, the uterus, as it were, prepares (trains) for childbirth.
where does hypertonicity come from
Hypertonicity can appear in any trimester of pregnancy. In the early stages, it occurs more often due to the fact that there is not enough progesterone, a hormone that is needed for the normal course of pregnancy. Another cause of hypertonicity is some changes in the uterine wall, for example, fibroids (a knot of uterine muscle tissue), endometriosis (growth of the uterine mucosa into the thickness of the wall), and inflammatory diseases. In these situations, the wall of the uterus is not able to stretch as it should. At later dates, hypertonicity can develop, on the contrary, with overstretching of the uterus (with polyhydramnios, large fetuses, multiple pregnancies). Very often, hypertonicity is provoked by some kind of physical activity too strong for a woman, for example, if, in a fit of “nesting”, the mother suddenly began to move and rearrange something in the apartment herself, or she simply moved for a very long time without resting. Someone hypertonicity occurs after psychological overstrain.
how to recognize hypertonicity
Hypertonicity must be distinguished from Braxton-Hicks contractions - as mentioned earlier, it lasts much longer than these training contractions and usually does not go away on its own (or goes away only after some long time). But if the mother cannot understand whether she has hypertension or not, you should consult a doctor. If there is still an increased tone of the uterus, the doctor, simply by placing his hand on his stomach, will feel a seal, tension, up to the feeling of a stone at hand. In addition, you can always do an ultrasound, on which, with hypertonicity, areas of local thickening of the muscular layer of the uterus are visible, and also look at the cervix, by the state of which you can also judge whether there is a threat of abortion or not.
what to do in case of hypertonicity
If it appears, the first thing you need to do is:
1. Calm down and lie down if possible. Do not panic, extra stress will not bring any benefits, especially since without consulting a doctor it is still not clear whether there is hypertonicity and how pronounced it is. Or maybe it's a false alarm? In addition, you can use relaxation techniques (breathing, auto-training, etc.).
2. Call your doctor. Of course, the doctor will not make a diagnosis in absentia, but since he knows the history of the expectant mother, her real or possible problems, he will be able to give the right direction for further action.
3. If it is not possible to contact your doctor, you can contact any clinic or antenatal clinic where pregnant women are treated. If medical institutions are already closed (late evening, at night), you can call an ambulance - she will take you to the nearest hospital or maternity hospital (you can also get there by taxi).
4. Hypertonicity is well eliminated by special medicines that relax the uterus (tocolytics), and if the doctor has prescribed them, then you should not be afraid to take them: they help quickly enough and do not harm the child.
how to prevent hypertonicity
There are simple rules that can prevent hypertonicity or reduce the risk of its occurrence:
1. Quit smoking, watch your weight, do not eat surrogate foods. No matter how trite it may sound, but it is a healthy lifestyle that is the basis of our well-being.
2. Distribute your forces correctly. Laundry, cooking can wait if the expectant mother suddenly feels that she needs a rest. If any activities require physical or psychological stress, cancel them for a while. Do not attend events or places where you may feel uncomfortable, reduce communication with people that are unpleasant for you.
3. Follow your doctor's recommendations: if he recommends any examination or treatment, do not neglect them.
Listen to your body, follow the doctor's advice, tune in to the positive - this is the key to a successful pregnancy. And then no hypertonicity is terrible for you!
Why does the stomach pull in early pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of having an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy may be:
- "obstetrical";
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- missed pregnancy;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- sprains and muscles associated with uterine growth.
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the insertion of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Causes that may cause miscarriage include:
- severe physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- Aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you need to see a doctor, as a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- appeared bloody discharge from the genital tract.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Illegal pregnancy
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes that can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Cystitis due to the anatomical features of a woman can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.
The bladder, located in the lower third of the abdomen, may give false symptoms of threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection.