Can newborns get colds
What to Expect, Treatment, When to See a Doctor
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Colds in newborns are common. However, while most colds are not cause for concern, it’s important to monitor symptoms closely and know when to seek treatment.
All babies are born with some immunity to illness. Even so, it takes time for their brand new immune systems to fully mature. This makes babies susceptible to viral infections, which cause colds.
There are over 200 types of viruses that can cause colds. Luckily, most of the colds your baby gets will help increase their immunity. Even so, their very first cold can be scary for parents.
A baby can catch a cold at any age or time of year. In fact, they may get as many as 8 to 10 a year in their first 2 years. If your little one is around older children, their chances of getting colds may increase.
Common colds in newborns aren’t dangerous, but they can quickly escalate into conditions that are, such as pneumonia or croup. Any illness in a baby under 3 months old is a reason to call their pediatrician, especially if they’re running a fever.
A stuffed or runny nose may be your first clue that your newborn has caught a cold. Their nasal discharge may start out as thin and clear, but turn thicker and yellowish-green in color over several days. This is normal, and doesn’t mean your baby’s cold is getting worse.
Other symptoms include:
- fussiness
- fever
- coughing, especially at night
- sneezing
- reduced appetite
- difficulty breastfeeding or taking a bottle due to nasal congestion
- trouble falling or staying asleep
Colds in newborns have some of the same symptoms as other illnesses, such as the flu, croup, and pneumonia. This can make diagnosis at home more stressful for parents.
Flu
If your newborn has the flu, they may have chills, vomiting, and diarrhea in addition to common cold symptoms. They may also have symptoms you can’t see and that they can’t tell you about, including headache, muscle or body aches, or sore throat.
Getting a flu shot every year can help keep you from getting sick and protect others around you, including your newborn.
Pneumonia
A cold can advance to pneumonia quickly. Symptoms may include:
- chills
- flushed skin
- sweating
- high fever
- vomiting
- worsening cough
- rapid breathing or difficulty breathing
Your baby may also develop a bluish tint to the lips or finger beds. This means your baby isn’t getting enough oxygen and should be taken to a hospital immediately.
Croup
If your baby’s cold escalates to croup, they may have difficulty breathing, hoarseness, and a barking cough. They may also have stridor, a type of high-pitched sound that occurs due to obstructed airflow.
RSV
Respiratory syncytial virus (RSV) is a serious cause of respiratory infection that can affect people of all ages. But it is particularly serious for babies, because their airways are smaller.
Learn more about RSV in babies.
Bronchiolitis
Babies are frequently hospitalized with bronchiolitis, an inflammatory respiratory condition that affects the smallest air passages in the lungs (bronchioles). It’s the most common cause of hospitalization in preterm infants. Viral bronchiolitis is often caused by RSV.
It’s the most common cause of hospitalization in preterm infants. Viral bronchiolitis is often caused by RSV.
Whooping cough
Pertussis, also known as whooping cough, is a type of respiratory infection that causes congestion, sneezing, and a severe cough. Though it can affect people of all ages, it can be very serious for babies under one year of age.
Getting vaccinated can help prevent caregivers from passing whooping cough to their newborn. Babies should also be vaccinated against whooping cough according to the routine vaccine schedule.
Another name for a common cold is a viral, upper respiratory infection. They aren’t caused by bacterial infections and don’t respond to antibiotics.
Your baby’s pediatrician may take a nasal swab to determine the cause of your baby’s symptoms. Blood tests may also be used to help rule out a bacterial infection.
Bacterial infections sometimes develop as complications from viral infections. They can also cause illnesses, such as pneumonia or ear infections.
Colds in newborns aren’t unusual. The viruses which cause them can live in the air and on hard surfaces for short periods of time. That makes it possible for transmission to occur with or without direct contact to someone who’s sick.
Babies who are around older children may be more likely to get colds. But even a trip to the pediatrician’s office, a cuddle with a loving adult, or a stroll to the store can expose your baby to germs.
Breastfed babies have more immunity than babies exclusively fed formula. This is because breastfeeding supplies antibodies, white blood cells, and enzymes to your baby, which help safeguard them from infection.
Breastfed babies have all, or part, of their mother’s immunity to the illnesses she has had or been exposed to. This doesn’t, however, mean breastfed babies are completely immune from colds.
A baby under 3 months old should be seen by a doctor if they have a cold. This will help rule out more serious conditions, and will also put your mind at ease.
Fever is one way your baby’s body works to fight off colds. Even so, a fever of 100.4°F (38°C) or higher in a baby who’s under 3 months old warrants a call to the doctor.
You should also call your doctor if your older baby has a persistent fever or other symptoms.
No matter their age, a fever that persists for more than 5 days warrants a call to the doctor and likely a visit.
Keep an eye on all of your baby’s symptoms. They should see a doctor if they have any of the following symptoms:
- rash
- vomiting
- diarrhea
- persistent or croupy cough
- odd, unusual-sounding cry
- trouble breathing
- retractions — when the areas below and between the ribs and in the neck sink in with each attempt to inhale
- thick or bloody mucus from the nose or mouth
- fever for more than 5 days
- rubbing their ear, or other sign of physical discomfort or pain anywhere in their body
- signs of dehydration, such as not wetting as many diapers as they usually do
- refusal to nurse or take a bottle
- bluish tinge around nail pads or lips
You know your little one best. If they just don’t seem like themselves, call their pediatrician so you can rule out anything more serious than a cold. That’s what the doctor is there for.
If they just don’t seem like themselves, call their pediatrician so you can rule out anything more serious than a cold. That’s what the doctor is there for.
In many cases, treatment for a cold involves taking steps to help ease symptoms and keep your baby comfortable.
This may include helping them stay hydrated, using a humidifier, or suctioning nasal mucus to clear up a stuffy nose.
Over-the-counter medications, including fever reducers and cold medications, should not be used unless directed by a doctor.
Treating a newborn cold at home
Home treatment for a newborn’s cold consists of helping them feel comfortable. Do’s and don’ts include:
Do’s
- Give plenty of liquids, including breast milk or formula (if your baby doesn’t take breast milk). A small amount of water may be offered to your baby if they’re over 6 months old.
- Suction out nasal mucus using saline drops and a suction bulb.
- Moisturize the air with a cool-mist humidifier.
 Keep in mind that hot-water humidifiers are not recommended and may pose a burning risk, especially to older, curious children.
Keep in mind that hot-water humidifiers are not recommended and may pose a burning risk, especially to older, curious children.
Don’ts
- Antibiotics don’t work on viruses and shouldn’t be given as treatment for a cold.
- Over-the-counter (OTC) fever reducers, including Infants’ Tylenol, aren’t recommended for babies under 3 months unless directed by your baby’s doctor. Check with your pediatrician before giving any type of OTC medication to a baby under 1 year. These medications may also not be recommended for a baby who’s vomiting.
- Aspirin should never be given to a baby or child.
- Cough and cold medications aren’t recommended for children under 4 years.
- Vapor rubs, even those formulated for babies, can be irritating to airways. Don’t use these either on the skin or in a vaporizer for children under 2.
- Don’t let your baby sleep on their stomach, even if they have congestion.
Other treatments for colds
There are no other treatments for an infant’s cold except the passage of time. The best thing you can do is make sure that you or another caring adult stays close by to provide comfort. This will help your baby relax and get the rest they need.
The best thing you can do is make sure that you or another caring adult stays close by to provide comfort. This will help your baby relax and get the rest they need.
Shop for saline drops and humidifiers online.
The average cold may last as long as 10 to 14 days. This includes the period of time when babies don’t display many symptoms but are contagious, as well as the period of time when they’re starting to act normally but still have crusty noses and nasal discharge.
Breastfeeding your baby can help boost their immunity. Even small amounts of breast milk supplemented with formula can help. This is especially true of antibody-rich colostrum, the first type of breast milk you produce when your baby is born.
You can’t keep your baby in a hermetically sealed environment. But you can help avoid exposure to some germs using the following guidelines:
- Wash your hands often and ask visitors to do the same.
- Avoid contact with people who are ill, and wipe down surfaces that have been touched by people who are coughing or sneezing.

- Ask people who come into contact with your baby to cough or sneeze into their elbows, rather than into their hands.
- If possible, limit your baby’s contact with older children.
- Make sure the adults and children around your newborn are current on their pertussis vaccine and have received the flu shot.
Colds are caused by viruses and are common in newborns. Even breastfed babies get colds, although their immunity is greater than babies who aren’t breastfed.
Colds aren’t serious, but they can turn into more serious illnesses. It’s important to have your pediatrician look at your baby if they have a cold and are under 3 months old — especially if they’re running a fever or have other symptoms.
Don’t hesitate to make this phone call! Your baby’s doctor will be happy to help rule out more serious conditions and put your mind at ease.
Does Breast Milk Change When Your Baby Is Sick?
You may have heard that breastfeeding is one of the best ways to boost your baby’s immune system and prevent them from getting sick. That doesn’t mean that your baby won’t ever catch a virus. Babies tend to be little germ factories, whether they’re nursing or not.
That doesn’t mean that your baby won’t ever catch a virus. Babies tend to be little germ factories, whether they’re nursing or not.
If your nursing baby has caught a bug, you might be wondering in what way your milk will protect them. Does breast milk change in some way when your baby is sick? Should you continue nursing your little one when they’re sick? What about when you’re feeling unwell? (Hint: yes, yes, and yes!)
Even when your baby isn’t fighting a virus, your breast milk has a baseline of elements that help protect your baby from illnesses and infections. First, breast milk is full of antibodies. These antibodies are highest in colostrum, the milk your baby receives at birth and during the first few days afterward. The antibodies also continue to be present in your milk the WHOLE time you’re nursing your baby, even if you nurse well into toddlerhood or beyond.
Your milk also contains a blend of proteins, fats, sugars, and white blood cells that work to fight infections. Other immune-boosting elements include lactoferrin, lactadherin, antiproteases, and osteopontin — antivirals and anti-inflammatories that help keep your baby’s immune system strong.
Other immune-boosting elements include lactoferrin, lactadherin, antiproteases, and osteopontin — antivirals and anti-inflammatories that help keep your baby’s immune system strong.
According to the Academy of Breastfeeding Medicine (ABM), there is strong evidence, too, that breast milk changes when you’re sick. When a nursing parent is under the weather, antibodies against that infection begin to be produced immediately and are found in breast milk.
What about when it’s your baby who catches the bug first? ABM notes that disease-fighting elements start to increase in breast milk in this case as well. So the answer to “Does your breast milk change when your baby is sick” is, “Yes!”
Tips for nursing a sick baby
Nursing can be more challenging when your baby is sick. Your baby may be fussier than usual. They may want to nurse more or less frequently. They may also be too congested to nurse. Here are some tips for getting through this tough time.
- If your baby is too stuffed up to nurse, consider saline spray or using a bulb syringe to clear the mucus before nursing.

- Keep the humidifier running to loosen mucus; you can also nurse your baby in a steamy bathroom.
- Nursing in a more upright position can also help with a congested baby.
- Often, sick babies will want to nurse more frequently; try to go with the flow, knowing that you can get back into a routine once your baby is better.
- If your baby is sleeping more than usual and nursing less, offer the breast right when they wake up, or even in the middle of a nap.
- If your baby seems too lethargic to nurse, you should call their pediatrician: it’s very important that your baby stays hydrated while sick.
More research needs to be done to get a fuller picture, but there is evidence that breast milk changes in response to a baby’s illness.
First, a study from 2012 found that when a baby has an active infection, the white blood cell content (macrophages) of their parent’s breast milk increases, as do other protective factors. This supports the idea that the immune defense provided by your nursing sick infants is active and responsive.
Next, a study in 2013 looked at what happened to the baseline amounts of leukocytes (a type of white blood cells) in breast milk during times of illness for the nursing parent or their nursed baby. The researchers found that leukocytes increased “significantly” when either the nursing parent or their baby was ill.
Once the illness passed, the level of leukocytes returned to normal baseline levels, suggesting a relationship between illness and leukocyte levels in breast milk. The study researchers concluded that there’s likely a strong association between the health of the nursing parent and infant and leukocyte levels of their breast milk.
Questions for your doctor or healthcare professional
It’s understandable that you might have concerns about nursing while your baby is sick. Here are some questions you might want to ask a healthcare professional to put your mind at ease:
- Do I need to change the frequency of nursing while my baby is sick?
- What should I do if my baby is too tired or congested to nurse?
- What are some signs that I should be taking my baby to the pediatrician?
- Is it OK if my baby seems to want to nurse “all the time” while they are sick?
You may have seen some viral social media posts depicting color changes in breast milk during times of illness. While these are certainly fascinating, there is no published evidence as of yet showing that these color changes are a direct result of breast milk changing in reaction to an infection from a nursed baby or nursing parent.
While these are certainly fascinating, there is no published evidence as of yet showing that these color changes are a direct result of breast milk changing in reaction to an infection from a nursed baby or nursing parent.
That doesn’t mean this isn’t possible — just that there’s no research to support it as of now. However, there is evidence that breast milk changes color for other reasons, including in reaction to something a nursing parent ate, a vitamin they took, or other external changes that may affect their milk’s color.
One example is this case report from 2012 of a nursing mother whose breast milk turned green as a result of a multivitamin she was taking. Breast milk is known to turn a rusty brown at times as a result of something called “rusty pipe” syndrome, which is where a little blood is found in milk during early breastfeeding, but soon resolves.
Other known causes of breast milk color changes include the fact that milk changes from the yellowish/gold color of colostrum when your baby is first born to the whitish color of mature milk. Even mature milk changes color throughout the day and from feed to feed. The more watery “foremilk” that comes at the beginning of a feed or when your breasts are very full has a more bluish hue. The fattier “hindmilk” that comes as your breasts empty usually appears more creamy and yellowish.
Even mature milk changes color throughout the day and from feed to feed. The more watery “foremilk” that comes at the beginning of a feed or when your breasts are very full has a more bluish hue. The fattier “hindmilk” that comes as your breasts empty usually appears more creamy and yellowish.
If you notice any changes in your milk that can’t easily be explained, you should reach out to a healthcare professional or lactation consultant for clarification.
These days, the illness parents of little ones are probably worried about most is COVID-19. Thankfully, there is research suggesting that it’s safe to breastfeed if you have COVID-19, and the World Health Organization (WHO) recommends that lactating parents with COVID-19 continue to nurse their infants.
There is even some research to suggest that nursing may protect babies against serious SARS-CoV-2 (the infection that causes COVID-19). An observational study found that babies who were nursed were less likely to test positive for COVID-19 than babies who didn’t receive any breast milk.
Additionally, antibodies for COVID-19 have been found in the breast milk of parents who have COVID-19 and parents who have been vaccinated against COVID-19. This means that a breastfed baby can likely have some immunity against COVID-19 even without getting sick or being vaccinated themselves.
Moreover, there’s no evidence that the SARS-CoV-2 virus itself can be passed to a baby via breast milk. In other words, if you have COVID-19, you can’t give it to your baby through your milk. All of these reasons are why experts urge parents to continue breastfeeding when either they or their babies are ill with COVID-19.
Breastfeeding has been found to prevent babies from getting sick in the first place, and protects against common childhood ailments such as ear infections, diarrhea and vomiting, pneumonia, and urinary tract infections. Even when your baby does get sick, breastfeeding has many benefits for your baby:
- Breastfeeding has been found to lower the illness course and severity
- Breastfeeding keeps your baby hydrated, and it’s often the one thing that babies can keep down when they’re vomiting or ill
- Breastfeeding comforts babies, and keeps them close and bonded with their parents
- Breastfeeding is good for parents too: it offers you a chance to sit and rest with your baby, and fills you with “feel good” hormones like prolactin and oxytocin that keep you emotionally balanced during stressful times, such as when your baby is sick
Researchers have just begun to scratch the surface of the ways that breast milk changes when your baby is sick. There is emerging evidence that breast milk increases its protections and immune-boosting properties when your baby is sick. What’s more, there is evidence that breast milk changes when a breastfeeding parent is sick.
There is emerging evidence that breast milk increases its protections and immune-boosting properties when your baby is sick. What’s more, there is evidence that breast milk changes when a breastfeeding parent is sick.
Let’s not forget all the data out there showing the many protective elements found in breast milk, whether your baby is currently sick or not. The bottom line is that if your baby is sick, breast milk is one of the best ways to help them fight their illness.
If you have any questions about breastfeeding during times of illness, don’t hesitate to reach out to your healthcare professional.
Colds in newborns - signs, prevention and treatment
A newborn due to unformed immunity is very susceptible to various kinds of viruses. To protect the baby from ARI, parents need to follow a number of simple but important rules.
Dry initial milk formula adapted by Valio Baby 1 NutriValio for feeding children from birth to 6 months More
Follow-up dry milk formula adapted by Valio Baby 2 NutriValio for feeding children from 6 to 12 months Read more
Dry milk drink "Baby milk" Valio Baby 3 NutriValio for feeding children over 12 months Read more
Most often, the baby gets sick when one of the parents or other adults in the house catches a cold. First of all, you need to take measures so that the child does not catch a virus that is dangerous for him. In children under 1 year old, even the simplest cold can lead to rather serious complications.
First of all, you need to take measures so that the child does not catch a virus that is dangerous for him. In children under 1 year old, even the simplest cold can lead to rather serious complications.
How not to infect a child with a cold?
-
If possible, move the sick family member to a separate room. The patient needs to move around the apartment only in a medical mask.
-
The baby should sleep in the nursery or at least in a separate bed. Do not take an infant to an adult bed, even if you practice co-sleeping.
-
Ventilate the room more often. At least twice a day, no less than 10 minutes. Take the child to another room, but rather go for a walk with him in the fresh air.
-
Every day (and preferably twice a day) spend in the apartment or at least the room where the baby spends most of the time, wet cleaning. You can use a weak dose of disinfectant detergent.
-
Try to adjust the air temperature in the apartment - the rooms should not be hot.
 This encourages the growth of microbes in the air.
This encourages the growth of microbes in the air.
Signs of a cold in a baby
A small child cannot explain that he is unwell, however, attentive parents, of course, will notice the symptoms of an incipient cold:
-
The baby has a fever.
-
The baby becomes capricious, whiny, sleeps poorly, refuses to breast or bottle with a mixture.
-
The child has a runny nose, wheezing, coughing may appear.
- Quite often, ARVI and acute respiratory infections in crumbs are accompanied by stool disorder.
How to treat a cold in a baby?
It is impossible to treat newborns on their own in any case. With the symptoms listed above, be sure to call the doctor to the baby. Only he will professionally diagnose and prescribe treatment. Fulfilling his prescriptions, create favorable conditions for the recovery of the crumbs - do not wrap him up (this will only increase the fever) and let's drink more (especially if the baby's cold is accompanied by diarrhea). Do not force your baby to eat if he refuses milk or formula. However, offer him a breast or a bottle more often so that he eats at least a little. If the baby is already receiving complementary foods, suspend acquaintance with new foods during the illness.
Do not force your baby to eat if he refuses milk or formula. However, offer him a breast or a bottle more often so that he eats at least a little. If the baby is already receiving complementary foods, suspend acquaintance with new foods during the illness.
#PROMO_BLOCK#
Prevention of colds in the newborn
The disease, of course, is better to prevent than to cure. Therefore, parents should definitely take measures to prevent colds, especially during the epidemic season. Refrain from receiving guests and visiting public places with the baby. If a nursing mother is sick, it is far from always necessary to stop breastfeeding - after all, breast milk contains the necessary antibodies and helps strengthen the baby's immunity. In what cases it is still worth switching to a mixture, read in our article *.
To make the baby less susceptible to disease, temper it. Walk outdoors more often and practice baby sleep while walking. Do not bathe the baby in hot water (start water procedures at 33-34 ° C and make the water cooler so that the baby is in good shape in it). When changing your baby, leave him to lie down undressed, air baths are very useful for strengthening children's health.
When changing your baby, leave him to lie down undressed, air baths are very useful for strengthening children's health.
3.26 19
Care and developmentShare:
Author: Reetta Tikanmäki
Palm oil in baby food
Infant milk formulas are made from cow's milk. However, in terms of fat composition, it differs significantly from that of the mother.
Read
Author: Ivargizova Oksana
How to choose milk formula for a baby
Breast milk is the best food for a newborn baby. It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development.
It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development.
Read
Show all
Colds in infants
How to understand that a newborn baby has a cold
To begin with, it is important to determine the prerequisites for the onset of the disease. The disease that many people know as a cold is SARS - a common infectious disease. The cause of the occurrence is viruses that infect the mucous membrane of the respiratory tract and cause inflammation with the subsequent manifestation of characteristic symptoms. The disease develops due to hypothermia, weakening the general, local immunity. The respiratory system is freely attacked by dangerous viruses.
If a newborn baby sneezes like a cold, has a fever or a runny nose, you should immediately contact your pediatrician. After the examination, the doctor will, if necessary, prescribe medicines for infants for colds. Parents are required to carefully follow the instructions of the physician who will monitor the dynamics of recovery.
Parents are required to carefully follow the instructions of the physician who will monitor the dynamics of recovery.
Treatment of a cold in a newborn child: features
Parents ask: if a baby has a cold, what should I do? Treatment of colds in infants begins with proper care. First you need to provide ideal conditions in the room. Viruses thrive in stagnant, dry air. For this reason, it is recommended to ventilate the children's room frequently and use a humidifier. When it is cold or frosty outside, when airing, you need to take the newborn to another room. If the weather is warm, the child can be left in the nursery if he has a normal temperature. The main thing is that there is no draft in the room.
If there is a cold in an infant 4 months old or older, hypothermia should be avoided. Overheating is also not allowed, especially at elevated body temperature. The child should be dressed in such a way that he is comfortable.
Colds and newborn feeding: what you need to know?
Pediatricians give specific recommendations regarding feeding. The best medicine for babies from colds is mother's breast milk, because it contains immunoglobulins, which give every small organism protective properties. Often sick babies have a reduced appetite. It is important to note that children should not be force-fed. You can apply the newborn to the breast often, but for a short time.
The best medicine for babies from colds is mother's breast milk, because it contains immunoglobulins, which give every small organism protective properties. Often sick babies have a reduced appetite. It is important to note that children should not be force-fed. You can apply the newborn to the breast often, but for a short time.
How to treat a cold in a 2 month old baby? It is advisable not to self-medicate. The best option is to contact a pediatrician, who, after examination and examination, will prescribe a therapy that does not harm the baby.
In addition, parents are wondering: how to quickly cure a newborn from a cold? The duration of treatment depends on:
1. Symptoms;
2. The prescribed therapy;
3. The presence or absence of complications.
Even simple forms of the common cold in infants can lead to severe, life-threatening consequences.
Features of symptoms
The symptoms of a cold differ among themselves depending on the level of severity, which depends on the age of the baby, the presence of concomitant diseases, the strength of the immune system, and prematurity at birth. In infants, a cold is manifested by the following symptoms:
In infants, a cold is manifested by the following symptoms:
1. Nose stuffed up - a huge amount of mucus accumulates in the nasal passages, due to which the child's breathing through the nose is disturbed. Such a phenomenon can be easily seen when the baby begins to breathe through the mouth;
2. A runny nose appears, which has a mucous structure - sometimes it is strong, and in some cases debilitating;
3. Cough - most often appears along with rhinitis, but in some situations only 1-2 days after the onset of dry cough. After the infection joins, it is wet, and sputum is also released;
4. Redness of the throat, which is bright red. The cause is the development of inflammation. A red throat causes the baby to have difficulty swallowing;
5. Diarrhea - often manifested in SARS and other viral infections;
6. High temperature - inflammation develops in the body. The temperature can reach 39o.
Cold medicine for newborns can only be prescribed by a pediatrician.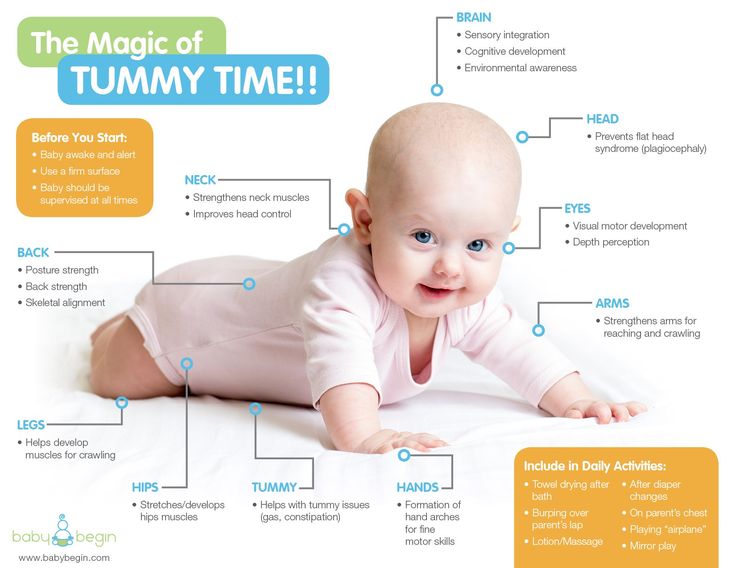 It is strongly not recommended to self-medicate with an illness of infants.
It is strongly not recommended to self-medicate with an illness of infants.
Traditional medicine
In addition to the main therapy prescribed by the doctor, some parents make a decoction of chamomile for newborns with a cold. It has a beneficial effect on babies:
1. Fights colds, coughs, sore throats;
2. Makes sleep sound;
3. Eliminates colic, indigestion, bloating;
4. Removes inflammation, irritation and diaper rash on the epidermis.
For kids with a cold, a special infusion is made. In 1 st. boiling water is brewed 1 tsp. pharmaceutical dry chamomile. The mixture is infused for 25 minutes, then filtered. Chamomile for a newborn with a cold, how to give? Preferably after feeding a maximum of six times a day.
Can a mother infect a newborn with a cold?
A child who is breastfed, of course, can catch a virus from a sick mother, because she is in dark contact with her. Mom spends most of her time with her baby, although SARS is not a reason to stop breastfeeding. In some cases, each member of the family is sick at the same time, while the newborn is not exposed to the disease. If the disease still does not bypass the kids, they often endure it in a mild form. Symptoms are not as pronounced as in other family members, so children recover quickly.
In some cases, each member of the family is sick at the same time, while the newborn is not exposed to the disease. If the disease still does not bypass the kids, they often endure it in a mild form. Symptoms are not as pronounced as in other family members, so children recover quickly.
Can a newborn get a cold from a mother? It all depends on the home environment, the immunity of the child and other factors. It is only important to know how not to infect a baby with a cold. Parents are advised to maintain personal hygiene, wash their hands often, especially after a woman or man has touched their face. You can’t sneeze or cough on a newborn. You also need to cover your mouth. It is necessary to stop using shared towels. It is best to buy paper napkins.
An equally important question: is it possible to walk with a newborn with a cold? In the fresh air, blood circulation improves, immunity increases, and the body is saturated with oxygen. Pediatricians allow walks, during which you should follow simple tips to eliminate the risks of negative consequences:
1.