When are you clear of miscarriage
Miscarriage
What is miscarriage?
Miscarriage (also called early pregnancy loss) is when a baby dies in the womb (uterus) before 20 weeks of pregnancy. For women who know they’re pregnant, about 10 to 15 in 100 pregnancies (10 to 15 percent) end in miscarriage. Most miscarriages happen in the first trimester before the 12th week of pregnancy. Miscarriage in the second trimester (between 13 and 19 weeks) happens in 1 to 5 in 100 (1 to 5 percent) pregnancies.
As many as half of all pregnancies may end in miscarriage. We don’t know the exact number because a miscarriage may happen before a woman knows she’s pregnant. Most women who miscarry go on to have a healthy pregnancy later.
What are repeat miscarriages?
If you have repeat miscarriages (also called recurrent pregnancy loss), you have two or more miscarriages in a row. About 1 in 100 women (1 percent) have repeat miscarriages. Most women who have repeat miscarriages (50 to 75 in 100 or 75 percent) have an unknown cause. And most women with repeat miscarriages with an unknown cause (65 in 100 women or 65 percent) go on to have a successful pregnancy.
What causes miscarriage and repeat miscarriages?
We don’t know what causes every miscarriage. But some miscarriages and repeat miscarriages can be caused by:
Problems with chromosomes
About half of all miscarriages are caused when an embryo (fertilized egg) gets the wrong number of chromosomes. This usually happens by chance and not from a problem passed from parent to child through genes. Chromosomes are the structures in cells that holds genes. Each person has 23 pairs of chromosomes, or 46 in all. For each pair, you get one chromosome from your mother and one from your father. Examples of chromosome problems that can cause miscarriage include:
- Blighted ovum. This is when an embryo implants in the uterus but doesn’t develop into a baby. If you have a blighted ovum, you may have dark-brown bleeding from the vagina early in pregnancy.
 If you’ve had signs or symptoms of pregnancy, like sore breasts or nausea (feeling sick to your stomach), you may stop having them.
If you’ve had signs or symptoms of pregnancy, like sore breasts or nausea (feeling sick to your stomach), you may stop having them. - Intrauterine fetal demise. This is when an embryo stops developing and dies.
- Molar pregnancy. This is when tissue in the uterus forms into a tumor at the beginning of pregnancy.
- Translocation. This is when part of a chromosome moves to another chromosome. Translocation causes a small number of repeat miscarriages.
Problems with the uterus or cervix.
The cervix is the opening to the uterus that sits at the top of the vagina. Problems with the uterus and cervix that can cause miscarriage include:
- Septate uterus. This is when a band of muscle or tissue (called a septum) divides the uterus in two sections. If you have a septate uterus, your provider may recommend surgery before you try to get pregnant to repair the uterus to help reduce your risk of miscarriage.
 Septate uterus the most common kind of congenital uterine abnormality. This means it’s a condition that you’re born with that affects the size, shape or structure of the uterus. Septate uterus is a common cause of repeat miscarriages.
Septate uterus the most common kind of congenital uterine abnormality. This means it’s a condition that you’re born with that affects the size, shape or structure of the uterus. Septate uterus is a common cause of repeat miscarriages. - Asherman syndrome. If you have this condition, you have scars or scar tissue in the uterus that can damage the endometrium (the lining of the uterus). Before you get pregnant, your provider may use a procedure called hysteroscopy to find and remove scar tissue. Asherman syndrome may often cause repeat miscarriages that happen before you know you’re pregnant.
- Fibroids (growths) in the uterus or scars from surgery on the uterus. Fibroids and scars can limit space for your baby or interfere with your baby’s blood supply. Before you try to get pregnant, you may need a surgery called myomectomy to remove them.
- Cervical insufficiency (also called incompetent cervix). This is when your cervix opens (dilates) too early during pregnancy, usually without pain or contractions.
 Contractions are when the muscles of your uterus get tight and then relax to help push your baby out during labor and birth. Cervical insufficiency may lead to miscarriage, usually in the second trimester. To help prevent this, your provider may recommend cerclage. This is a stitch your provider puts in your cervix to help keep it closed.
Contractions are when the muscles of your uterus get tight and then relax to help push your baby out during labor and birth. Cervical insufficiency may lead to miscarriage, usually in the second trimester. To help prevent this, your provider may recommend cerclage. This is a stitch your provider puts in your cervix to help keep it closed.
Infections
Infections, like sexually transmitted infections (also called STIs) and listeriosis, can cause miscarriage. An STI, like genital herpes and syphilis, is an infection you can get from having sex with someone who is infected. If you think you may have an STI, tell your health care provider right away. Early testing and treatment can help protect you and your baby. Listeriosis is a kind of food poisoning. If you think you have listeriosis, call your provider right away. Your provider may treat you with antibiotics to help keep you and your baby safe. Having certain infections may cause miscarriage, but they’re not likely to cause repeat miscarriages.
Are you at risk for a miscarriage?
Some things may make you more likely than other woman to have a miscarriage. These are called risk factors. Risk factors for miscarriage include:
- Having two or more previous miscarriages
- Being 35 or older. As you get older, your risk of having a miscarriage increases.
- Smoking, drinking alcohol or using harmful drugs. If you’re pregnant or thinking about getting pregnant and need help to quit, tell your provider.
- Being exposed to harmful chemicals. You or your partner having contact with harmful chemicals, like solvents, may increase your risk of miscarriage. A solvent is a chemical that dissolves other substances, like paint thinner. Talk to your provider about what you can do to protect yourself and your baby.
Some health conditions may increase your risk for miscarriage. Treatment of these conditions before and during pregnancy can sometimes help prevent miscarriage and repeat miscarriages. If you have any of these health conditions, tell your health care provider before you get pregnant or as soon as you know you’re pregnant:
If you have any of these health conditions, tell your health care provider before you get pregnant or as soon as you know you’re pregnant:
- Autoimmune disorders. These are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake. Autoimmune disorders that may increase your risk of miscarriage include antiphospholipid syndrome (also called APS) and lupus (also called systemic lupus erythematosus or SLE). If you have APS, your body makes antibodies that attack certain fats that line the blood vessels; this can sometimes cause blood clots. If you have APS and have had repeat miscarriages, your provider may give you low-dose aspirin and a medicine called heparin during pregnancy and for a few weeks after you give birth to help prevent another miscarriage. Lupus can cause swelling, pain and sometimes organ damage. It can affect your joints, skin, kidneys, lungs and blood vessels. If you have lupus, your provider may treat you with low-dose aspirin and heparin during pregnancy.
- Obesity. This means you have too much body fat and your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. If you’re obese, your chances of having a miscarriage may increase. To find out your BMI, go to cdc.gov/bmi.
- Hormone problems, like polycystic ovary syndrome (also called PCOS) and luteal phase defect. Hormones are chemicals made by the body. PCOS happens when you have hormone problems and cysts on the ovaries. A cyst is a closed pocket of that contains air, fluid or semi-solid substances. If you’re trying to get pregnant, your provider may give you medicine to help you ovulate (release an egg from your ovary into the fallopian tubes). Luteal phase defect can cause repeat miscarriages. It’s when you have low levels of progesterone over several menstrual cycles. Progesterone is a hormone that helps regulate your periods and gets your body ready for pregnancy. If you have luteal phase defect, your provider may recommend treatment with progesterone before and during pregnancy to help prevent repeat miscarriages.
- Preexisting diabetes (also called type 1 or type 2 diabetes). Diabetes is when you have too much sugar (also called glucose) in your blood. Preexisting diabetes means you have diabetes before you get pregnant.
- Thyroid problems, including hypothyroidism and hyperthyroidism. They thyroid is a butterfly-shaped gland in your neck. Hypothyroidism is when the thyroid gland doesn’t make enough thyroid hormones. Hyperthyroidism is when the thyroid gland makes too many thyroid hormones.
- Having certain prenatal tests, like amniocentesis and chorionic villus sampling. These tests have a slight risk of miscarriage. Your provider may recommend them if your baby is at risk for certain genetic conditions, like Down syndrome.
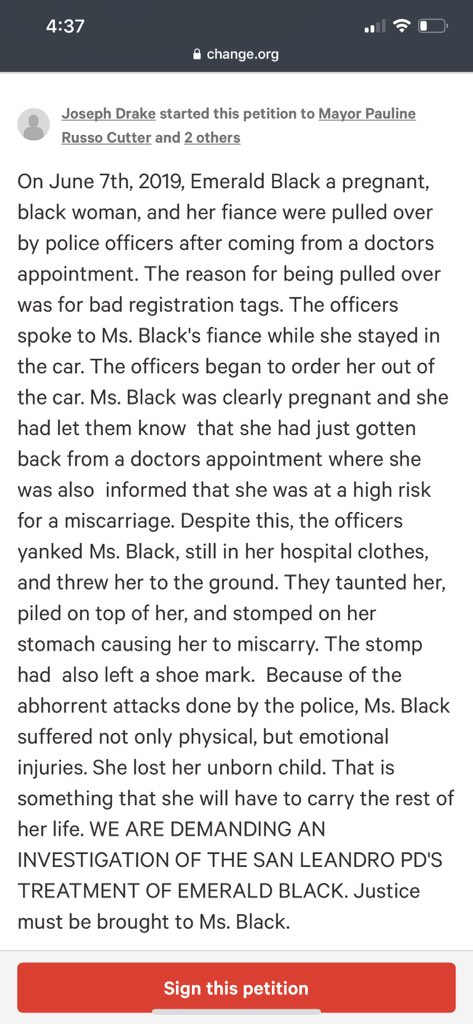
Having an injury to your belly, like from falling down or getting hit, isn’t a high risk for miscarriage. Your body does a good job of protecting your baby in the early weeks of pregnancy.
You may have heard that getting too much caffeine during pregnancy can increase your risk for miscarriage. Caffeine is a drug found in foods, drinks, chocolate and some medicine. It’s a stimulant, which means it can help keep you awake. Some studies say caffeine may cause miscarriage, and some say it doesn’t. Until we know more about how caffeine can affect pregnancy, it’s best to limit the amount you get to 200 milligrams each day. This is what’s in about one 12-ounce cup of coffee.
What are the signs and symptoms of miscarriage?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Signs and symptoms of miscarriage include:
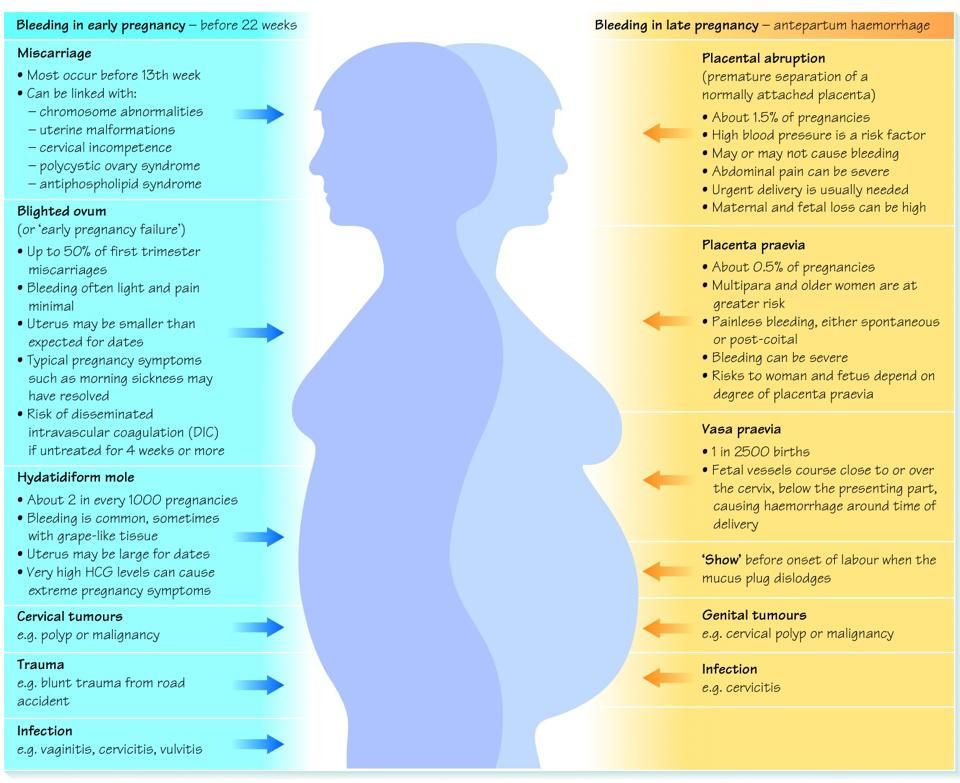
- Bleeding from the vagina or spotting
- Cramps like you feel with your period
- Severe belly pain
If you have any of these signs or symptoms, call your provider. Your provider may want to do some tests to make sure everything’s OK. These tests can include blood tests, a pelvic exam and an ultrasound. An ultrasound is a test that uses sound waves and a computer screen to show a picture of your baby inside the womb.
Your provider may want to do some tests to make sure everything’s OK. These tests can include blood tests, a pelvic exam and an ultrasound. An ultrasound is a test that uses sound waves and a computer screen to show a picture of your baby inside the womb.
Many women have these signs and symptoms in early pregnancy and don’t miscarry.
What treatment do you get after a miscarriage or repeat miscarriages?
If you’ve had a miscarriage, your provider may recommend:
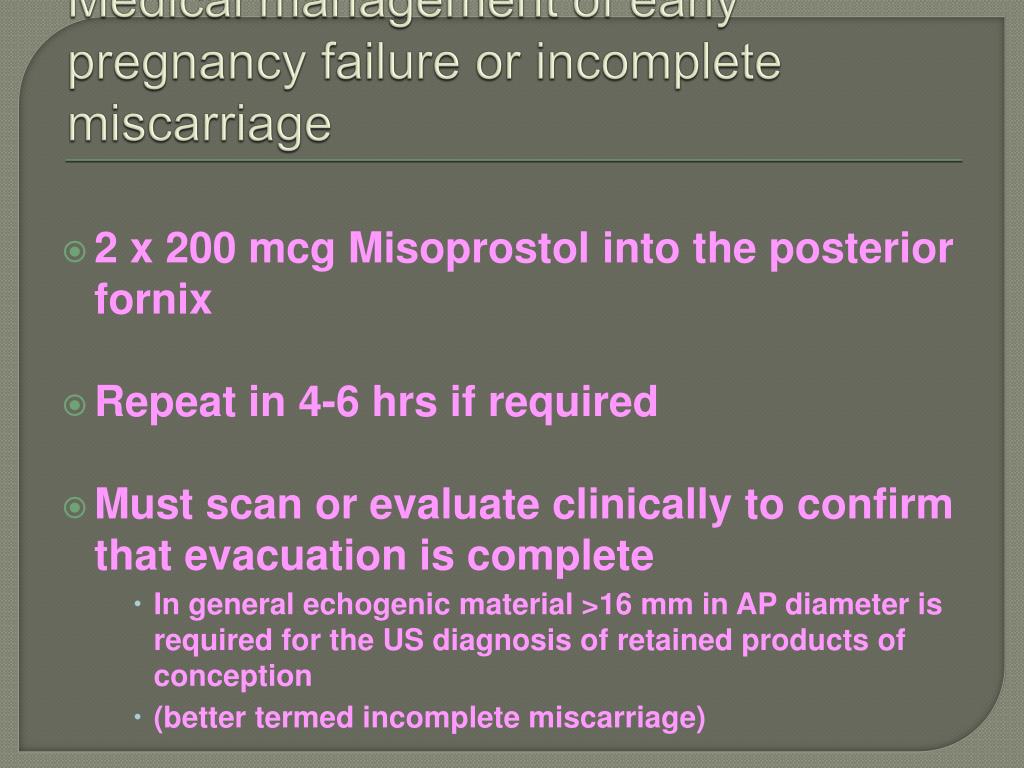
- Dilation and curettage (also called D&C). This is a procedure to remove any remaining tissue from the uterus. Your provider dilates (widens) your cervix and removes the tissue with suction or with an instrument called a curette.
- Medicine. Your provider may recommend medicine that can help your body pass tissue that’s still in the uterus.
Do you need any medical tests after a miscarriage or repeat miscarriages?
If you miscarry in your first trimester, you probably don’t need any medical tests. Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
If you have repeat miscarriages in the first trimester, or if you have a miscarriage in the second trimester, your provider usually recommends tests to help find out the cause. Tests can include:
- Chromosome tests. You and your partner can have blood tests, like karyotyping, to check for chromosome problems. Karyotyping can count how many chromosomes there are and check to see if any chromosomes have changed. If tissue from the miscarriage is available, your provider can test it for chromosomal conditions.
- Hormone tests. You may have your blood tested to check for problems with hormones. Or you may have a procedure called endometrial biopsy that removes a small piece of the lining of the uterus to check for hormones.
- Blood tests to check your immune system. Your provider may test you for autoimmune disorders like, APS and lupus.
- Looking at the uterus. You may have an ultrasound, a hysteroscopy (when your provider inserts a special scope through the cervix to see your uterus) or a hysterosalpingography (an X-ray of the uterus).
How long does it take to recover from a miscarriage?
It can take a few weeks to a month or more for your body to recover from a miscarriage. Depending on how long you were pregnant, you may have pregnancy hormones in your blood for 1 to 2 months after you miscarry. Most women get their period again 4 to 6 weeks after a miscarriage.
It may take longer to recover emotionally from a miscarriage. You may have strong feelings of grief about the death of your baby. Grief is all the feelings you have when someone close to you dies. Grief can make you feel sad, angry, confused or alone. It’s OK to take time to grieve after a miscarriage. Ask your friends and family for support, and find special ways to remember your baby. For example, if you already have baby things, like clothes and blankets, you may want to keep them in a special place. Or you may have religious or cultural traditions that you’d like to do for your baby. Do what’s right for you.
Or you may have religious or cultural traditions that you’d like to do for your baby. Do what’s right for you.
Certain things, like hearing names you were thinking of for your baby or seeing other babies, can be painful reminders of your loss. You may need help learning how to deal with these situations and the feelings they create. Tell your provider if you need help to deal with your grief. And visit Share Your Story, the March of Dimes online community where you can talk with other parents who have had a miscarriage. We also offer the free booklet From hurt to healing that has information and resources for grieving parents.
If you miscarry, when can you try to get pregnant again?
This is a decision for you to make with your partner and your provider. It’s probably OK to get pregnant again after you’ve had at least one normal period. If you’re having medical tests to try to find out more about why you miscarried, you may need to wait until after you’ve had these tests to try to get pregnant again.
You may not be emotionally ready to try again so soon. Miscarriage can be hard to handle, and you may need time to grieve. It’s OK if you want to wait a while before trying to get pregnant again.
More information
- From hurt to healing (free booklet from the March of Dimes for grieving parents)
- Share Your Story (March of Dimes online community for families to share experiences with prematurity, birth defects or loss)
- Centering Corporation (grief information and resources)
- Compassionate Friends (resources for families after the death of a child)
- Journey Program of Seattle Children’s Hospital (resources for families after the death of a child)
- Lupus Research Alliance: Pregnancy and family planning
- Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
Last reviewed: November, 2017
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and RisksMedically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
Overview
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past. Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities. This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage. Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity. If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester.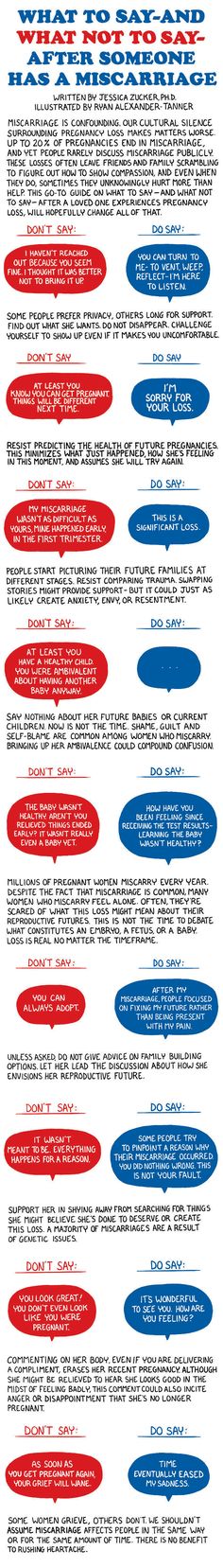 Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent. According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent.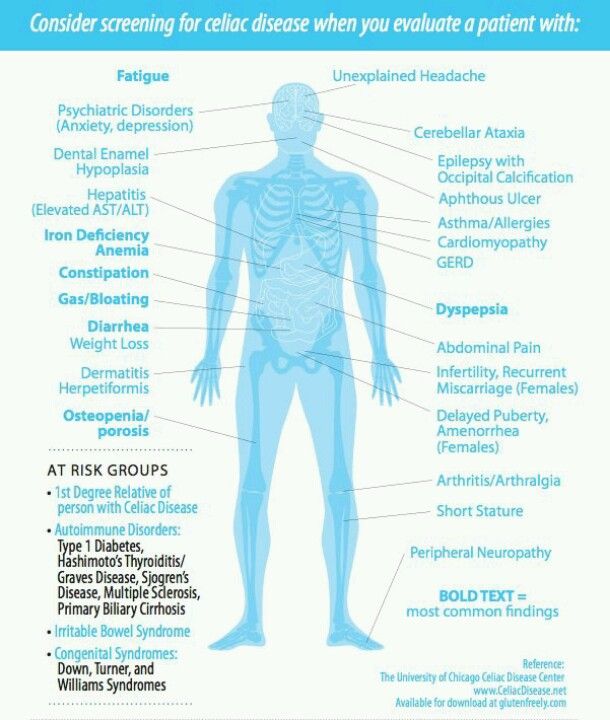 But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble. But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy. Here are some tips to staying healthy during pregnancy:
Here are some tips to staying healthy during pregnancy:
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive. A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
Last medically reviewed on October 3, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
Medically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.

READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.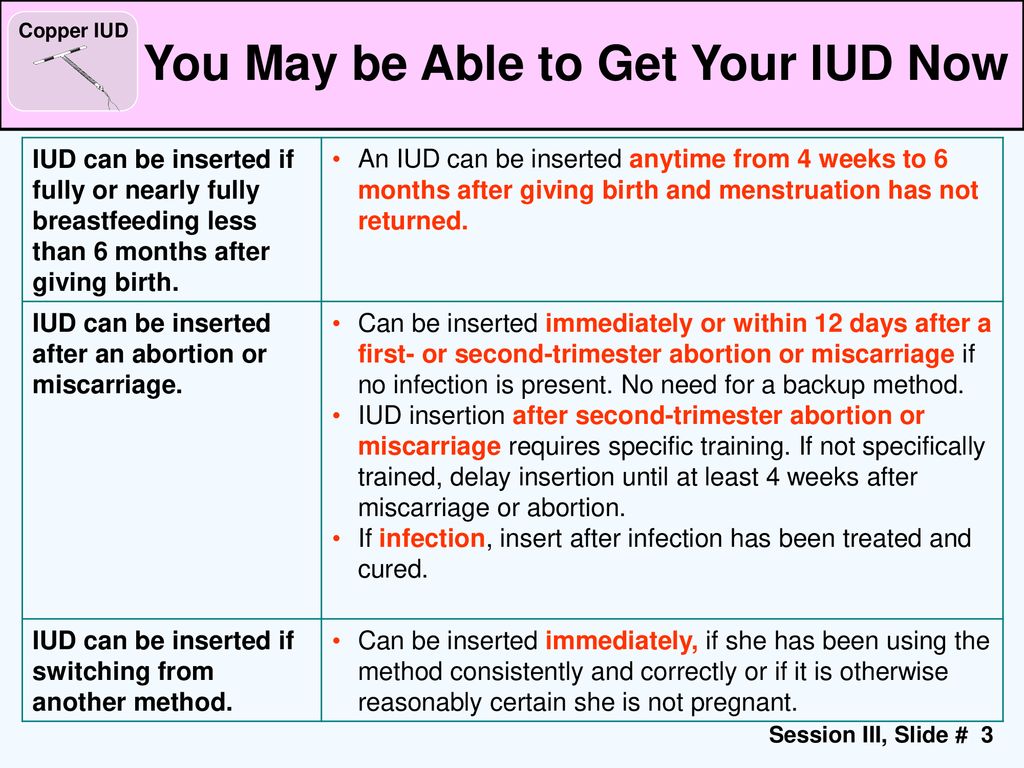
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be initiated.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Threat of miscarriage – OSTEOMED Clinics Network
Threat of miscarriage may occur at any stage of pregnancy.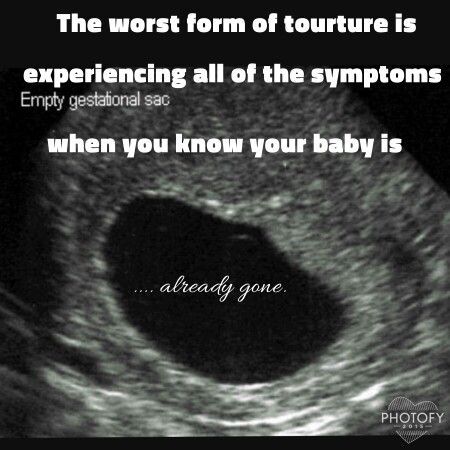 If this condition occurs before the 28th week of pregnancy, then they talk about the threat of termination of pregnancy, if after 28 weeks - then about the threat of premature birth. Recently, this diagnosis is quite common in expectant mothers, the reason for this is the intense rhythm of life of pregnant women, the environmental situation, the spread of infections, as well as an increase in the number of pregnancies after 35 years. Spontaneous abortion occurs in 10-20% of all pregnancies, with the bulk of miscarriages occurring in the first trimester. If the pregnancy is interrupted after 28 weeks, then they talk about premature birth.
If this condition occurs before the 28th week of pregnancy, then they talk about the threat of termination of pregnancy, if after 28 weeks - then about the threat of premature birth. Recently, this diagnosis is quite common in expectant mothers, the reason for this is the intense rhythm of life of pregnant women, the environmental situation, the spread of infections, as well as an increase in the number of pregnancies after 35 years. Spontaneous abortion occurs in 10-20% of all pregnancies, with the bulk of miscarriages occurring in the first trimester. If the pregnancy is interrupted after 28 weeks, then they talk about premature birth.
Symptoms:
- Drawing and aching pains in the lower abdomen and lower back;
- Uterine hypertonicity;
- Bloody discharge from the genital tract; moreover, the discharge can be both blood-red and brown (traces of "old" blood).
Causes:
- Threat pains in the abdomen are usually located in the center above the womb, and may resemble the pains of menstruation.
 Pain in the lateral parts of the abdomen is associated with stretching of the ligamentous apparatus of the uterus and is not related to the threat of interruption.
Pain in the lateral parts of the abdomen is associated with stretching of the ligamentous apparatus of the uterus and is not related to the threat of interruption. - Uterine hypertonicity can be localized (usually not felt by the woman), is most often detected by ultrasound and affects only a small segment of the uterus (usually the anterior or posterior wall). In the first trimester of pregnancy, it may occur due to a reaction to ultrasound. If hypertonicity is noted at a later date, then this indicates an increased excitability of the muscles of the uterus, and the woman is at risk for the threat of interruption. In order to prevent this condition, she may be prescribed drugs that reduce the tone of the uterus (magnesium preparations (Magnesium B6, magnesia), papaverine in suppositories, no-shpa).
- Total hypertonicity is characterized by the fact that the entire uterus "hardens". It may be accompanied by pain. Usually, total hypertonicity occurs in the second half of pregnancy and can be observed right up to the very birth.
 The occurrence of such hypertonicity is regarded as a threat of abortion, the pregnant woman is shown treatment and examination in a hospital. Separately, we note that after the 32nd week of pregnancy, Braxton-Hicks training contractions appear, but they are not accompanied by pain, and their duration is short.
The occurrence of such hypertonicity is regarded as a threat of abortion, the pregnant woman is shown treatment and examination in a hospital. Separately, we note that after the 32nd week of pregnancy, Braxton-Hicks training contractions appear, but they are not accompanied by pain, and their duration is short. - The appearance of bloody discharge at any stage of pregnancy is a formidable symptom, even if the discharge is very slight. The appearance of such a symptom indicates a violation of the connection between the fetal egg (in the early stages of pregnancy) or the placenta (at a later stage) with the uterine wall. Bloody discharge can be a symptom of a complication such as placenta previa or placental abruption. With partial placental abruption, a retroplacental hematoma occurs, which can be detected by ultrasound. Bloody discharge in a pregnant woman requires urgent hospitalization and ultrasound examination. Ultrasound is necessary to assess the condition of the fetus (presence of heartbeat and heart rate), assess uteroplacental blood flow, and the presence of retroplacental hematoma.
There are many reasons for the threat of termination of pregnancy. In the first trimester, most often the threat of interruption is caused by hormonal deficiency, infections, genetic defects of the fetus, pathology of the blood coagulation system.
In the second half of pregnancy, infections, hormonal imbalances, pathology of the blood coagulation system, immunological problems (Rhesus conflict), preeclampsia, polyhydramnios, and isthmic-cervical insufficiency most often cause a threat.
In order to identify the cause of the threat of interruption, an examination in a hospital is required.
Diagnosis:
- Clinical blood test, urinalysis
- Coagulogram (extended) + homocysteine + D-dimer
- Cervical swab for microflora and its sensitivity to antibacterial drugs (vaginal smear is not good!) Urinalysis quantitative for hCG (human chorionic gonadotropin), performed in the first trimester
- Tests for TORCH infection (in the first trimester of pregnancy)
- Ultrasound examination and examination by a competent obstetrician-gynecologist are mandatory
Treatment
Treatment of this condition should begin with the elimination of the cause of the threat of interruption.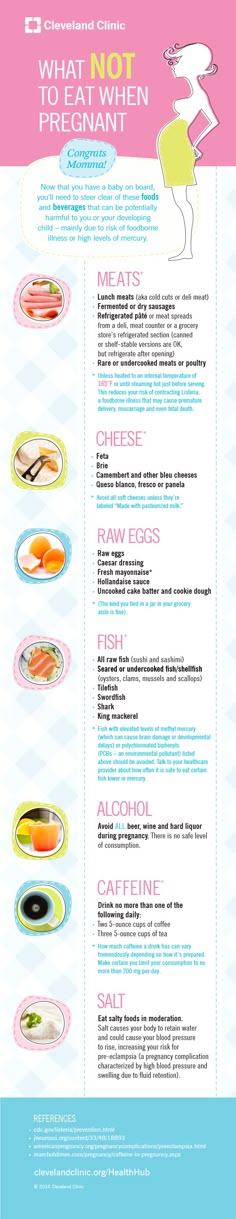 All other means to relax the muscles of the uterus are only symptomatic treatment. Sexual rest and bed rest are required.
All other means to relax the muscles of the uterus are only symptomatic treatment. Sexual rest and bed rest are required.
The threat of abortion in her first trimester is always accompanied by hormonal deficiency. Therefore, it is necessary to prescribe hormonal preparations of progesterone to compensate for the deficiency. Duphaston preparations (in the form of tablets) or Utrozhestan (vaginal suppositories) are used. Also, injections of progesterone or 17-OPG are additionally prescribed. Progesterone dosages are prescribed by a doctor. Obstetrician-gynecologists even have a saying: "There is no such thing as too much progesterone." Progesterone preparations can be used up to 20-22 weeks of pregnancy.
If the threat of interruption is associated with the pathology of the blood coagulation system (thrombophilia), then the pregnant woman is prescribed blood-thinning drugs (anticoagulants). Their use avoids the occurrence of microthrombi in the placenta, which leads to a threat. The most commonly used are Fraxiparine (subcutaneous injections) and Curantil (tablets).
The most commonly used are Fraxiparine (subcutaneous injections) and Curantil (tablets).
If the reasons for the threat of termination of pregnancy are infections (if microflora is found in a smear from the cervical canal), then the appointment of antibacterial drugs is mandatory. If treatment is not carried out in time, then it will be almost impossible to get rid of total hypertonicity later.
After 12 weeks of pregnancy, magnesia is administered intravenously (rarely intramuscularly). Magnesia improves placental blood flow, relaxes the muscles of the uterus. After the end of the course of magnesia, further administration of magnesium preparations (Magnesium B6) is indicated.
Taking sedatives is mandatory, but not the main method of treatment. The woman's anxiety about the threat that has arisen only increases the likelihood of progression of the pathology, therefore, preparations of valerian and motherwort are prescribed.
OSTEOPATHICS AND THREATS OF PREGNANCY
To date, the prevention and treatment of the threat of miscarriage is based on medication.












