Anatomy of child birth
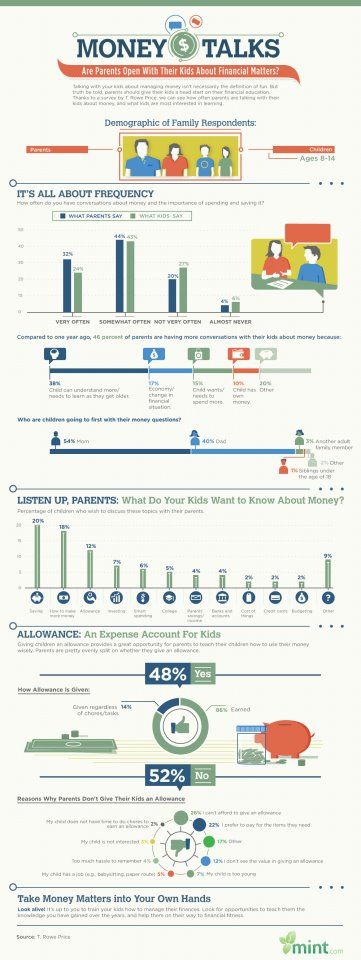
What happens to your body during childbirth
Childbirth is challenging and complications occur, but women's bodies are designed to give birth. The shape of the pelvis, hormones, powerful muscles and more all work together to help you bring your baby into the world - before, during and after childbirth.
How your body prepares for labour
Here are some of the ways your body will prepare both you and your baby for the birth ahead.
Braxton Hicks contractions
In the weeks or days before you start having proper contractions, you may experience Braxton Hicks contractions. This is your uterus tightening then relaxing. These contractions don't usually hurt and are thought to help your uterus and cervix get ready for labour.
Braxton Hicks contractions may become more regular as you get closer to the time of birth, but unlike labour contractions, they don't change the shape of the cervix and are sometimes referred to as 'false labour'. Your midwife can tell you if you're experiencing Braxton Hicks contractions or if you are in labour by doing a vaginal examination to look at your cervix.
Changes to the cervix
As labour gets closer, your cervix softens and becomes thinner, getting ready for the dilation (widening) that will allow the baby to enter the vagina. You may also see a 'show', which is a pinkish plug of mucus, stained with blood.
Engagement
Your baby may move further down your pelvis as the head engages, or sits in place over your cervix, ready for the birth. Some women feel they have more room to breathe after the baby has moved down. This is called 'lightening'.
Rupture of the membranes, or 'waters breaking'
Some women find the sac of amniotic fluid containing the baby breaks before labour, contractions start and the fluid runs (or gushes) out of the vagina. This is referred to as rupture of the membranes, or 'waters breaking'.
Let your maternity team know when your waters have broken and take notice of the colour of the fluid. It is usually light yellow. If it is green or red, tell your maternity team since this could mean the baby is having problems.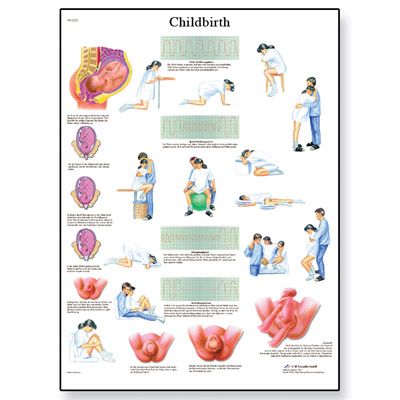
If your waters have broken but you have not started having regular contractions within 24 hours, you may need your labour to be induced because there is a risk of infection. Your midwife or doctor will talk to you about this.
How will you know when labour has started?
Movies often show women suddenly being struck by painful contractions and rushing to hospital. In real life, many women are not sure if they have actually started their labour.
You may feel restless, have back pain or period-like pain, or stomach disturbances such as diarrhoea.
Labour officially begins with contractions, which start working to open up the cervix. You should phone your midwife when your contractions start, although you probably won't be encouraged to come to the hospital or birthing centre until your contractions are closer together.
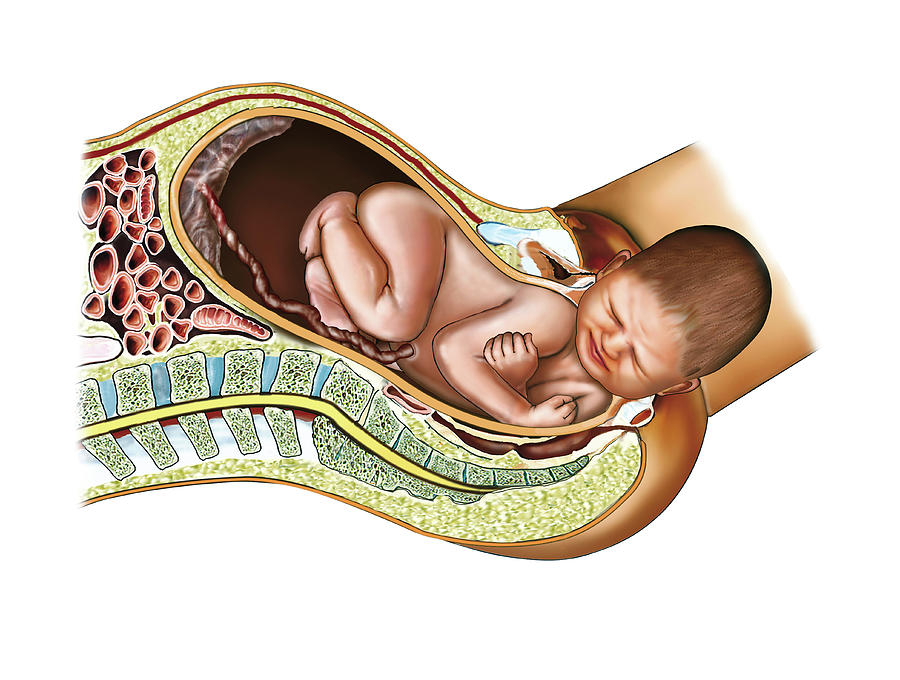
In preparation for labour, your baby may move further down your pelvis as the head engages, or sits in place over your cervix.How the pelvis is designed for childbirth
Your pelvis is located between your hip bones. Women typically have wider, flatter pelvises than men, as well as a wider pelvic cavity (hole) to allow a baby to pass through.
Women typically have wider, flatter pelvises than men, as well as a wider pelvic cavity (hole) to allow a baby to pass through.
The organs sitting in a woman's pelvis include the uterus, cervix and vagina, which are held together by a group of muscles. During childbirth, the muscles at the top of your uterus press down on the baby's bottom. Your baby's head then presses on your cervix which, along with the release of the hormone oxytocin (see 'How hormones help you give birth', below), brings on contractions. Your cervix should dilate so your baby can pass through it.
Your pelvis has bones and ligaments that move or stretch as the baby travels into the vagina. Your baby also has spaces between the skull bones called 'sutures', and the gaps where the sutures meet on the skull are called fontanelles. This allows for the baby's head to mould as the skull bones meet or overlap, allowing it to fit more easily as it travels through your pelvis.
How hormones help you give birth
Your body produces hormones that trigger changes in your body before, during and after childbirth. Here's how they work to help you deliver your baby.
Here's how they work to help you deliver your baby.
- Prostaglandin Before childbirth, a higher level of prostaglandin will help open the cervix and make your body more receptive to another important hormone, oxytocin.
- Oxytocin This hormone causes contractions during labour, as well as the contractions that deliver the placenta after the baby is born. These post-birth contractions, including more that can occur during breastfeeding, help your uterus shrink back to its normal size. Oxytocin and prolactin are the two main hormones that produce and let down breast milk for your baby. Skin-to-skin contact between a mother and baby helps to release more of these hormones.
- Relaxin The hormone relaxin helps soften and stretch the cervix for birth, while helping your waters break and stretching the ligaments in your pelvis to allow the baby to come through.
- Beta-endorphins During childbirth, this type of endorphin helps with pain relief and can cause you to feel joyful or euphoric.
- 'Baby blues' After birth, your hormone balance can change again, and this is believed to cause the ‘baby blues’ in some women. You may feel teary, anxious and irritable and your mood can go up and down.
When childbirth doesn’t go to plan
Sometimes, complications can occur before or during childbirth that mean things don’t go as expected.
Sometimes, labour needs to be induced or started. There are a few ways to induce labour, including the mother being offered synthetic prostaglandin. This is inserted into the vagina to soften the cervix and start contractions.
If contractions slow down or stop during labour, the mother may be offered synthetic oxytocin from a drip to increase the contractions. In both these cases contractions can come on strongly and more pain relief may be needed. Your maternity team should explain the benefits and risks of this with you before you agree to it.
The baby could be in a posterior or breech position, not ideally placed above the cervix before the birth. Your maternity team may need to use forceps or a vacuum to help turn the baby or help the baby travel out of the vagina. Sometimes a caesarean is needed.
Your maternity team may need to use forceps or a vacuum to help turn the baby or help the baby travel out of the vagina. Sometimes a caesarean is needed.
In rare cases, a mother may experience cephalopelvic disproportion (CPD), which is when the baby’s head is too big to fit through the pelvis. A diagnosis of CPD is usually made when labour hasn’t progressed and synthetic oxytocin has not helped. A caesarean is usually the next step.
More information
If you have any questions about childbirth or pregnancy, you can call Pregnancy, Birth and Baby on 1800 882 436, 7 days a week, to speak to a maternal health nurse.
Learn more here about the development and quality assurance of healthdirect content.
Birth Anatomy - A Guide to Mother's Birth Anatomy
A woman’s birthing anatomy includes soft tissues and hard bones.
The bones
Our bones are held together by flexible tendons. In pregnancy, these joints become even more mobile. Waddling is an example of what happens when these joints get softer.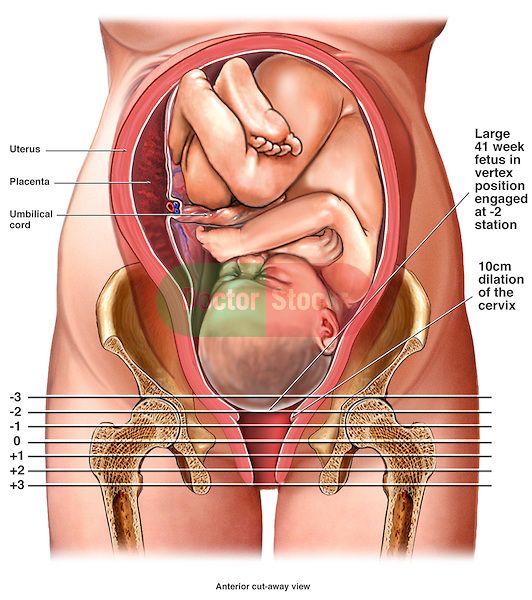 The baby passes through the mobile pelvis.
The baby passes through the mobile pelvis.
The hormone relaxin helps make the pelvis a dynamic, flexible passageway.
The bony pelvis has four joints. In the front of the pelvis is the symphysis pubis joint. Movement here really isn’t that comfortable. Sometimes a pregnancy belt holds this joint stable for walking and rolling over in bed. Symmetry in the symphysis pubis (pubic bone) reduces spasm in the round ligaments and helps the sacrum, around back, to be aligned properly.
On either side of the sacrum are the SI joints (Sacroiliac joints). These are located where the dimples are. Many plastic baby dolls have SI dimples above their bum. The SI joints are a common location for aches when the pelvis is weak or crooked.
Symmetry in the SI joints will help the sacrum be lined up with the pelvic brim. Then the baby can get into a nice, head down position. A chiropractic adjustment helps get the symphysis and the SI joints aligned.
The sacrum, rather than fused, is slightly mobile and in the birth process actually moves to allow the head past.
The tailbone is connected by a joint to the lower end of the sacrum. Sometimes this needs an adjustment, too, especially after birthing a baby. Ligaments connecting to the sacrum and tailbone (coccyx) will become more symmetrical and their tone will be more relaxed and less in spasm after bodywork on the pelvis.
Important Landmarks in the Pelvis
The baby first passes into the brim when engaging in the pelvis. The angle of the baby’s head in relation to the brim of the pelvis plays a role in whether engagement is lengthy or more easy. Some babies engage before labor but when contractions get strong for a while and baby remains high at the brim, it may be because baby’s head is riding up on the brim or pressed against a portion of the inlet at an unfavorable angle.
When the bottom of the pelvis, the outlet, is more narrow than the top, labor can slow down here as well.
The good news is that the body is pliable, and muscles can be released, joints loosened, and fascia smoothed with simple and quick stretches or birth positions – when smartly chosen to match the need of the individuals birth.
Understanding inlet and outlet diameters can help match appropriate techniques and strategies for labor progress.
Kuliukas (2015). looked at 64 women and did not find a clustering of four types but a range throughout.
Lia Betti of the UK offers a dynamic exposure of racist categorization of pelvis shapes and gives a re-interpretation of pelvic difference in Shaping birth: variation in the birth canal and the importance of inclusive obstetric care. For providers, pelvic understanding helps avoid poor technique among the slight differences in pelvic shape when forceps or ventouse are used. For providers and parents, noticing how the labor signals progress or a stall can help redirect care or choice of birth position so that that a position may chosen to optimize all the space available for the baby to move through the pelvis.
Pelvis width associated with bone mass distribution at the proximal femur in children 10–11 years old.
The variety of pelvic shapes, combined with the variety of fetal head presentations, plus size variations, mean that labors vary greatly. Engagement is the phase of labor most affected by pelvic type.
Engagement is the phase of labor most affected by pelvic type.
In the drawing above, we see pelvic inlet shape and the correlating shape of the pubic arch at the outlet.
A pelvis with a roundish brim which allows fetal rotation when the muscles and ligaments in and around the pelvis aren’t tight and twangy.
The pelvic arch in front would allow three fingers to cover the urethra during a “potty dance” – the type of grabbing yourself and try not to pee your pants dance of a child waiting to get to the bathroom. Buttocks are round.
Hip size doesn’t indicate the roomy inside and a petite woman can birth a large baby. When the pelvic floor and other soft tissues aren’t overly tight, the birth tends to go well and a posterior baby can rotate at several various phases of labor.
Narrower in the front
A more triangular pubic arch may hang quite low, giving a fundal height reading higher than the compact bump may seem to justify. Closely-set, small buttock “muscles” of the android make small roundish or triangular cheeks to her “bottom. ” The pelvis with a 2 finger arch, rather than the 3 finger width, means baby fits best with an anterior position and good flexion (chin tucking). Upright positions and more time for pushing and stronger pushing may be part of the story for some with a triangular brim.
” The pelvis with a 2 finger arch, rather than the 3 finger width, means baby fits best with an anterior position and good flexion (chin tucking). Upright positions and more time for pushing and stronger pushing may be part of the story for some with a triangular brim.
Narrow in the front, this pelvis occasionally catches the posterior baby’s forehead. Back it up and let it turn!
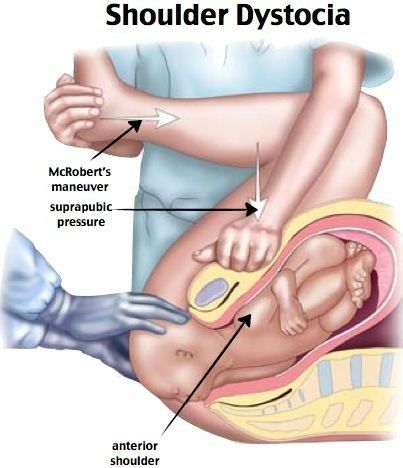
Good fetal positioning, good flexibility in the pelvic joints, and balance in the soft tissues help the natural labor progress. The posterior baby will hope to rotate before engagement or may not be able to rotate until the head fully passes the pelvis rotating on the perineum. Manually rotating the baby’s head may be an option if a skilled doctor or midwife is present. A little help for the shoulders may be needed as the result of those women with low slung pubic bones. They may catch a shoulder.
Tall women with average size babies often birth without an issue even with a triangular pelvis but this shape is in noted in the medical literature for a higher rate of posteriors since they can have a harder time rotating while in between the bones.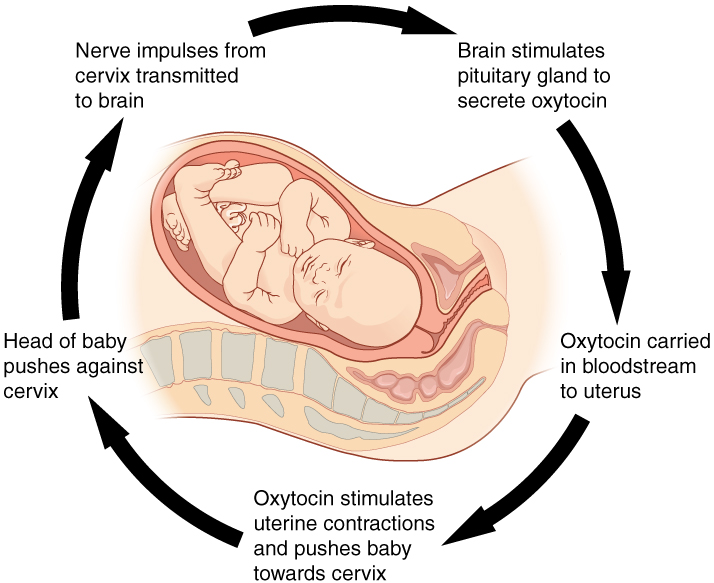 This will be more of an issue for shorter, older, or heavier bodies. An advantage is helping baby through body balancing to rotate to Left Occiput Anterior before engagement.
This will be more of an issue for shorter, older, or heavier bodies. An advantage is helping baby through body balancing to rotate to Left Occiput Anterior before engagement.
Recently a woman told me her doctor felt she may not be able to have a vaginal birth after she previously had a cesarean for birthing her first child. She asked me what I thought. While I acknowledge there are more challenges with a triangular pelvis for some of these labors, most births through an android pelvis are going to be able to finish by the woman’s own efforts -and her baby’s. I said:
Adding body balance and helping baby into position is extremely important when birthing with any smaller pelvis. Body balancing and birth positioning could make a positive solution for many in this situation. If the posterior baby can back up to turn to left occiput anterior and try again, there is much reason to expect a vaginal birth. To help the baby do this, Side-lying Release followed by an inversion of some type during a contraction or two can be necessary.
Releasing the tuberosacral ligaments in the back of the pelvis is a way to allow another portion of the sacrum to have increased mobility and therefore, more space for baby. Our blog has two good descriptions of this release.
Longest space is front-to-back
In this pelvis, the space for baby to enter is longer front-to-back and this spacing is true at the bottom, though baby may rotate a bit for the middle and then return to their starting position. The posterior baby fits more easily in this pelvis but babies are still usually anterior when they start labor. Either way, the Abdominal Lift and Tuck or a belly dance (figure 8 and front to back but not side to side moves) can be a help in helping baby get started into the pelvis (see instructions and what makes this work).
More posterior babies who are born vaginally may have the advantage of this pelvis’ longer front to back opening. Various vertical maternal positions and movements protect fetal engagement.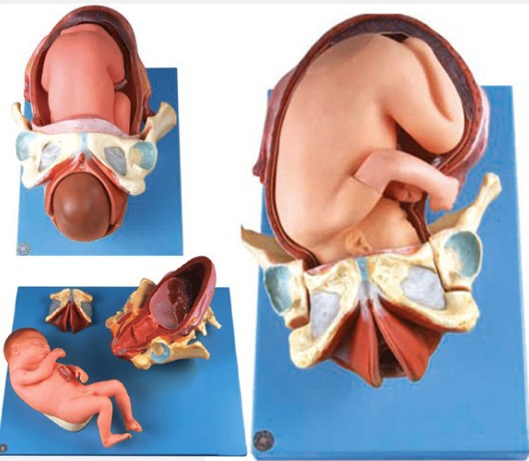 Understanding the unique benefits of this pelvic type help birth finish by the mother’s own efforts.
Understanding the unique benefits of this pelvic type help birth finish by the mother’s own efforts.
Narrow front-to-back
The pubic arch is a wide 4 finger span what has been called the platypelloid pelvis, which is quite wide. Hips may seem wider side-to-side but mainly because the pelvis is flatter front to back. This allows for a flat (non-pregnant) belly look due to the short front-to-back distance of the bones.
At the bottom, the sitz bones are quite wide apart, more than the width of the person’s fist (if she can reach between them while lying down). Very few women have this situation but when a doctor spots it they may presuppose a cesarean is necessary. The best advantage for a vaginal birth is starting labor with baby in the Left Occiput Transverse position where baby is facing sideways. Body balancing can help baby get settled this way, but not simply gravity. Go for an broad and inclusive approach to body preparation, not strength but length in the muscles and more importantly, balance!
Baby really needs to be in the LOT position to get INTO the pelvic brim for engagement. Long early labor is common, but if the baby isn’t LOT, the two days of labor will be all about getting baby rotated and strong contractions and mobility are essential. Once the baby is into the pelvis labor tends to move along, within 5-8 hours of engagement. Pushing may not be very long because the outlet of the pelvis is large. Using Daily Essentials: Activities for Pregnancy Comfort & Easier Childbirth, and Spinning Babies® Parent Class may help your baby get into a LOT or other ideal position.
Long early labor is common, but if the baby isn’t LOT, the two days of labor will be all about getting baby rotated and strong contractions and mobility are essential. Once the baby is into the pelvis labor tends to move along, within 5-8 hours of engagement. Pushing may not be very long because the outlet of the pelvis is large. Using Daily Essentials: Activities for Pregnancy Comfort & Easier Childbirth, and Spinning Babies® Parent Class may help your baby get into a LOT or other ideal position.
Pelvic cavities can have a MIX of opening or closing funnel shapes (narrowest at the bottom) and
How to fit the pelvic shape into a label or category is less important to me than having a set of skills to identify the relationship between the long axis of baby’s head with the short distance of the pelvic level where baby waits during a labor stall.
Knowing what is going on between the baby and the mother at the inlet or other diameters of the pelvis and what we can do to help when help is indeed appropriate.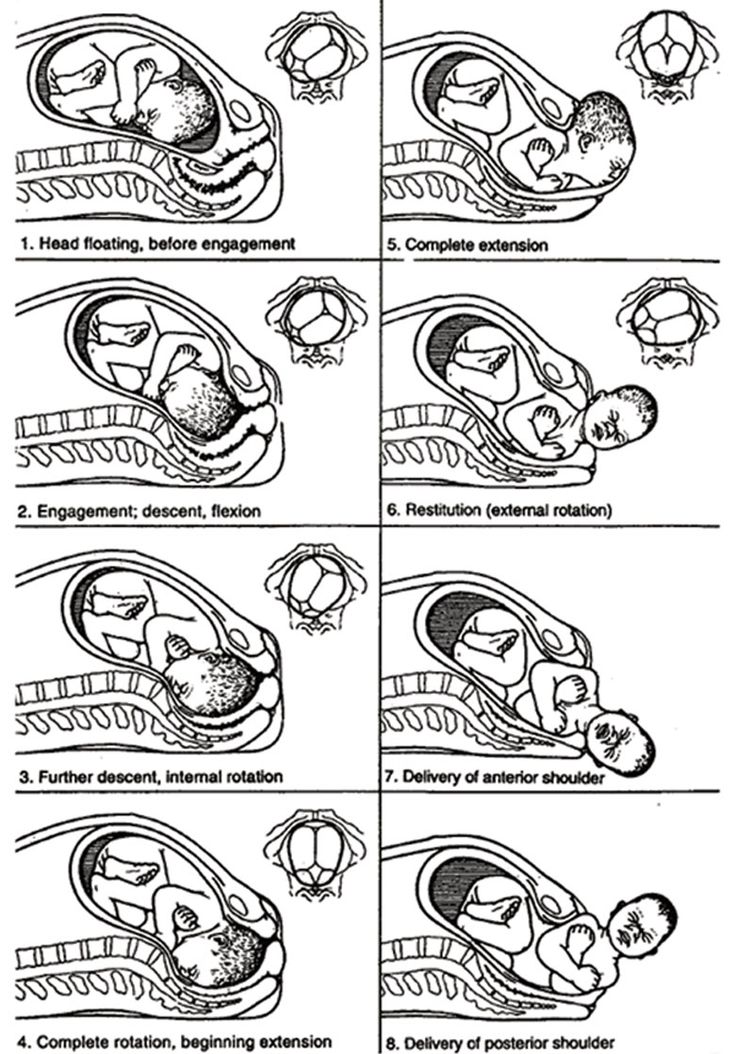 This is explained in the low-cost download, Spinning Babies® Quick Reference.
This is explained in the low-cost download, Spinning Babies® Quick Reference.
Pelvic Inlet diameters and lack of engagement
Occasionally a pelvic shape sets the fetal position. But this, I believe, is secondary to soft tissue “balance.” Some pelvises don’t accommodate posterior presentations. The baby must rotate or will not drop into the pelvis. When the mother can re-angle her pelvis to let the baby in (See steep inlet in Is baby engaged?). A birth stool, posterior pelvic tilt, and standing and leaning over a dresser feels right.
Rarely, a pelvis is too small to let the baby enter the pelvis. When a pelvis is too small its called CephaloPelvic Disproportion (CPD, or baby’s too big). Rickets, injury or an actually too-big-baby may be the cause here. CPD is rare but does exist.
Before we suspect CPD in pregnancy, check to see if the baby is engaged. Until the baby is LOA or LOT and in one of those ideal starting positions, it’s too soon to call it CPD.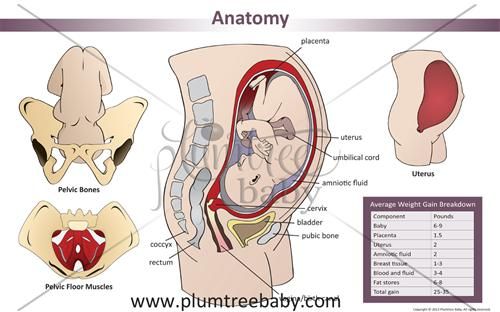 We have an article on this called Will baby fit?
We have an article on this called Will baby fit?
The Soft Tissues
The tone and relative symmetry of a woman’s uterine ligaments and muscles either makes room for baby or reduces room, if tight and twisty or so loose the uterus bends over.
Our ability to stand depends on the psoas muscle pair. The psoas begins at T-12 vertebrae and sweeps around from the center of the sides of the spine over the pelvis to attach at the top of the thigh bone (femur). The muscle pair comes around like supporting arms, pulling up the legs so that our backs don’t fall over.
As the psoas comes across the pelvis, it makes a diagonal support for our organs. The support can be thought of as a shelf. When the uterus is large, at the end of pregnancy, a tight psoas can hold up a baby from descending and engaging in the womb. Many discomforts of the abdomen can stem from psoas tightness, but there are exercises to release the psoas. A great source is Liz Koch’s The Psoas Book.
As the psoas is balanced, so goes the birth!
So as I was saying… The Psoas.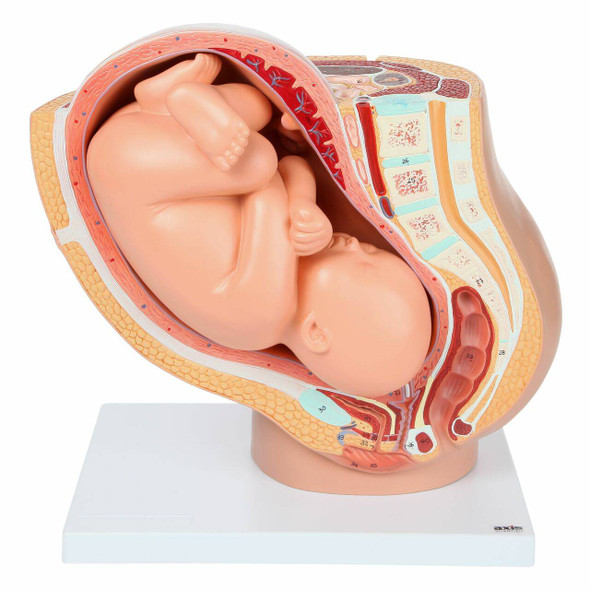
The psoas is the lower triangle (pointing up) of two great muscle pair triangles that give core strength to the human body. The upper triangle (pointing down) is the trapezius, which is more of a diamond shape really, but I say two opposing triangles to help you to visualize of the polarity or pull between them to support our bodies.
The psoas additionally affects our pelvis and uterus because it shares the tendon connecting it to the thigh with another muscle pair, the iliacus. Together they team up to form the iliopsoas muscle group. The tone of the iliacus is dependent in part by the tone of the psoas. So, as the psoas goes, so goes the iliacus. This muscle spans from the top of the thigh (lesser trochanter) back over the pelvic brim to attach at the inside edge of the ilium (behind the hip bone but not as far to the center as the sacrum).
Pelvic floor
The pelvic floor is three layers of several muscles that rise into the lower pelvis to uplift the uterus, bladder, and other abdominal organs. The pelvic floor is open front to back to allow the urinary urethra, vagina, and rectum through to the body’s exterior. The lovely thing about the pelvic floor is the benefits of balance has far reaching benefits from better fetal positioning, easier and less painful birthing, better control and ease in peeing and pooping, walking, thinking, mood, breathing, and sexuality. Some benefits are very direct and others are secondary. A tight pelvic floor is not typically the best functioning, so beware of over kegeling. Combine the ball squeeze and anterior pelvic tilt shown in our daily activities
The pelvic floor is open front to back to allow the urinary urethra, vagina, and rectum through to the body’s exterior. The lovely thing about the pelvic floor is the benefits of balance has far reaching benefits from better fetal positioning, easier and less painful birthing, better control and ease in peeing and pooping, walking, thinking, mood, breathing, and sexuality. Some benefits are very direct and others are secondary. A tight pelvic floor is not typically the best functioning, so beware of over kegeling. Combine the ball squeeze and anterior pelvic tilt shown in our daily activities
The pelvic floor should be considered as one unit since the three compartments work as one entity.
Uterine shape
The uterus is pear shaped before the first birth and apple shaped for future births, Jean Sutton, New Zealand midwife describes. The uterus is shaped to support a baby in a vertical position, and head down is common due to gravity.
Some spiraling and leaning to the right is considered normal for the uterus. But too much lean is not helpful for optimal uterine functioning, including birth. These are called dextrorotation and right obliquity.
But too much lean is not helpful for optimal uterine functioning, including birth. These are called dextrorotation and right obliquity.
The womb is supported by a series of ropes and slings called ligaments and fascia. The ligaments of the womb have a unique mixture of fibrous tissue and muscle cells. The muscle cells allow the ligaments to become longer during pregnancy so that the ligaments can grow with the uterus. Symmetry of the ligaments helps the womb be held upright.
Cervix
The cervix is part of the uterus, the part that opens for baby to be born. The cervix is pulled open by uterine contractions that first soften and thin the uterus. The cervix will be aligned properly, first aiming back in pregnancy and then, during birth, moving forward to line up with the birth canal.
Dilation is less painful when the cervix is not held to the side or back by spasming cervical ligaments. The baby’s head is better positioned with symmetrical ligaments because the lower uterine segment is not in a twist.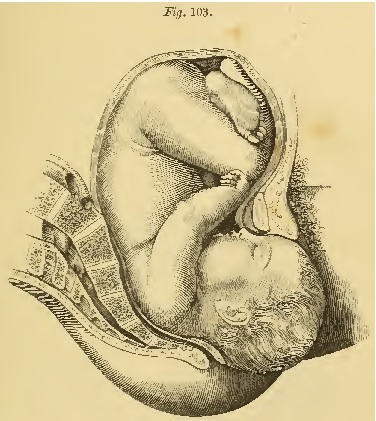 We notice that Side-lying Release and Forward-leaning Inversion are two wonderful techniques (both from Carol Phillips) that help the uterus and baby line up with the cervix so it may open with less time and effort.
We notice that Side-lying Release and Forward-leaning Inversion are two wonderful techniques (both from Carol Phillips) that help the uterus and baby line up with the cervix so it may open with less time and effort.
Fascia
The fascia is a 3D web of fibriles which are in constant movement. This web forms a membranous tissue that wraps every muscle, organ, and bone in the body. The fascia moves with the moving body but also seems to store the “memory” of an abrupt halt. Whether that sudden stop has to do with a trauma or a long-time habit of poor posture, the fascia can thicken and then pull which can, over time, pull organs and bones out of alignment or symmetry. The function of the fascia in balance can be the most important contribution to overall health.
Fortunately, craniosacral therapists, fascial therapists and, to a lesser degree, chiropractic adjustments, can help to release the fascia and so, bring about a greater symmetry of the body. See more at Adrienne Caldwell’s blog. She shares insights and references about the fascia in her post which also talks about scar tissues after cesarean section and how multi-directional massage may reduce obstruction in motion and health.
She shares insights and references about the fascia in her post which also talks about scar tissues after cesarean section and how multi-directional massage may reduce obstruction in motion and health.
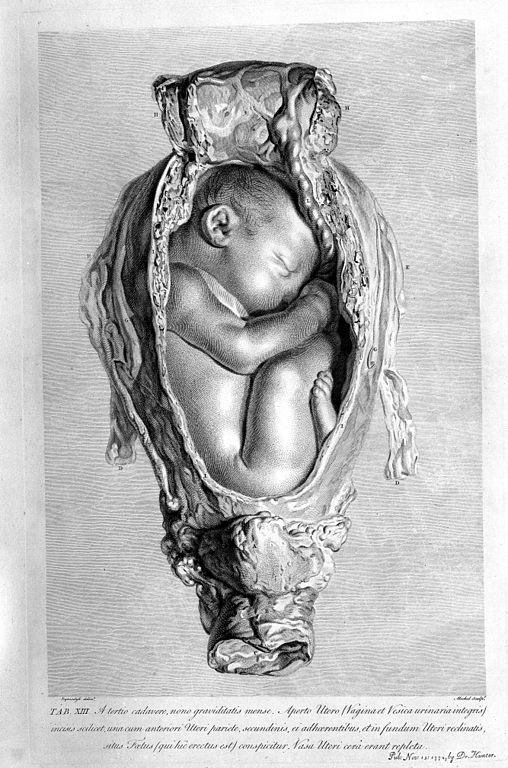
Baby’s birth-related anatomy
The fetal head is heavy in comparison to the rest of the baby’s body. The vertical positions of walking, standing and sitting help the heavy head settle lower than the body during the third trimester, and sometimes in the second trimester.
The fetal skull has not yet hardened and remains somewhat flexible for fitting through the pelvis. There are plates of bone and cartilage that are nearly finished coming together at birth. That nearly finished margin is what allows molding. These margins are called sutures.
The skull plates are held together by a coating for strong fascia. This membrane also wraps down the spine to the pelvis and legs. The fascia also connects to membranes that support the brain, called the tentorium cerebelli.
Which angle the head presses past, or onto, the bony pelvic passageway determines molding. When the crown of the head enters the pelvis first molding is most efficient. When a plate, rather than the margin between, or sutures, aims into the narrow part of pelvis, molding takes a long time and does less to reduce the diameter of the baby’s head. One example of this is the asynclitic baby. Second stage can take a long time and pushing can be quite strenuous when a baby is asynclitic.
The baby’s shoulders can also mold a bit for the birth process. The shoulder girdle is flexible and many times the shoulders are folded towards the chest for the actual emergence. Other times one shoulder comes out just ahead of the other in another natural variation to reduce shoulder breadth.
References:- Holistic Midwifery, Vol. II by Anne Frye
- Hands of Love by Carol Phillips
- The Female Pelvis by Blandine Calais-Germain
- A New Look at a Woman’s Body by Boston Womens’ Health Collective
- Gray’s Anatomy by Henry Gray
- Kuliukas, A.
 , Kuliukas, L., Franklin, D., & Flavel, A. (2015). Female pelvic shape: Distinct types or nebulous cloud?. British Journal of Midwifery, 23(7).
, Kuliukas, L., Franklin, D., & Flavel, A. (2015). Female pelvic shape: Distinct types or nebulous cloud?. British Journal of Midwifery, 23(7). - Cardadeiro, G., Baptista, F., Janz, K. F., Rodrigues, L. A., & Sardinha, L. B. (2014).
- Journal of bone and mineral metabolism, 32(2), 174-183.
- Maccioni, F., & Alt, C. D. (2018). MRI of the Pelvic Floor and MR Defecography. In Diseases of the Abdomen and Pelvis 2018-2021 (pp. 13-20). Springer, Cham.
You may also like to look at Amy Hoyt’s blog posts on Optimal Fetal Positioning with explanations and photos of the pelvis and baby (doll) on her blog: Natural Birth in Kitsap.
The process of childbirth
This event must be approached with self-confidence, one's strengths, capabilities and reliability of information received about childbirth during pregnancy.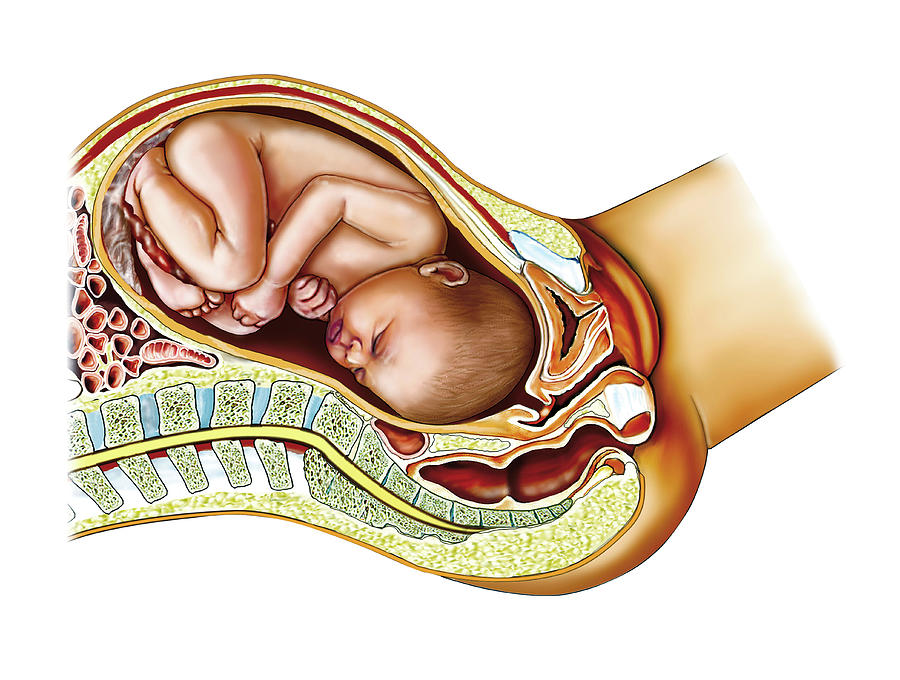 Tuning in the right way and doing everything right, knowledge helps. It is incomparably easier for pregnant women who have a good idea of all the stages of the birth process and are psychologically prepared for the upcoming event than for those expectant mothers who are poorly aware of what will happen to them.
Tuning in the right way and doing everything right, knowledge helps. It is incomparably easier for pregnant women who have a good idea of all the stages of the birth process and are psychologically prepared for the upcoming event than for those expectant mothers who are poorly aware of what will happen to them.
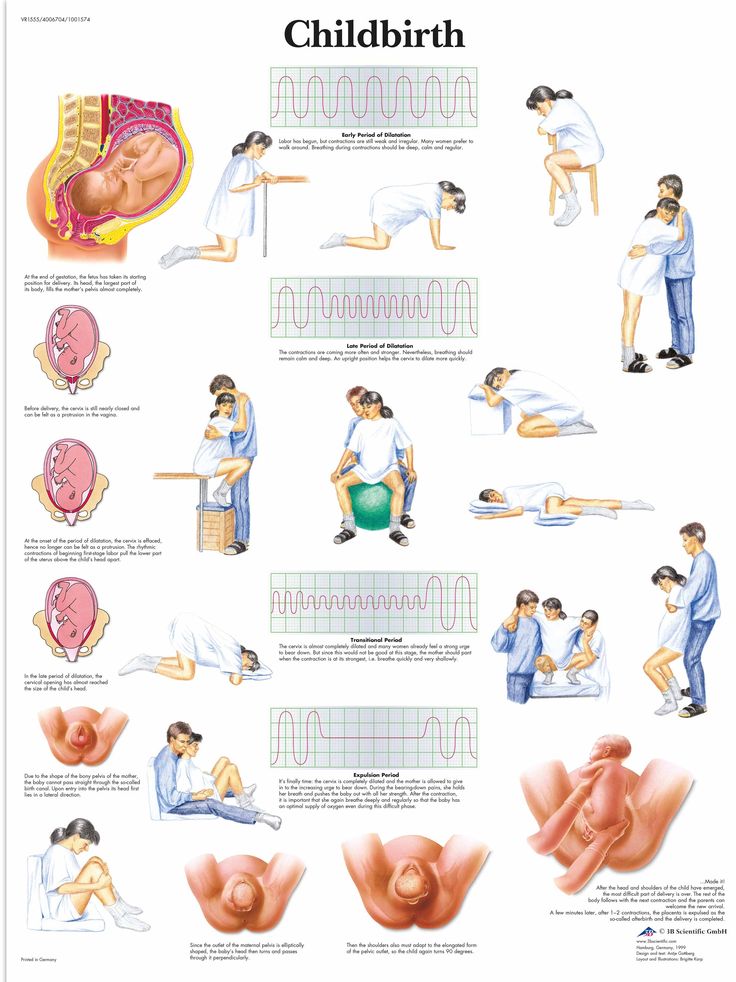
Childbirth is divided into three periods:
- Disclosure period . As a result of regular contractions (involuntary contraction of the muscles of the uterus), the cervix opens.
- The period of expulsion of the fetus from the uterine cavity. Attempts are added to the contractions - arbitrary (that is, controlled by the woman in labor) contractions of the abdominal muscles. The baby moves through the birth canal and is born.
- Follow-up period . The placenta and membranes are born.
First stage of labor
The fact that labor has already begun or is about to begin is indicated by the appearance of regular contractions and / or the outflow of amniotic fluid.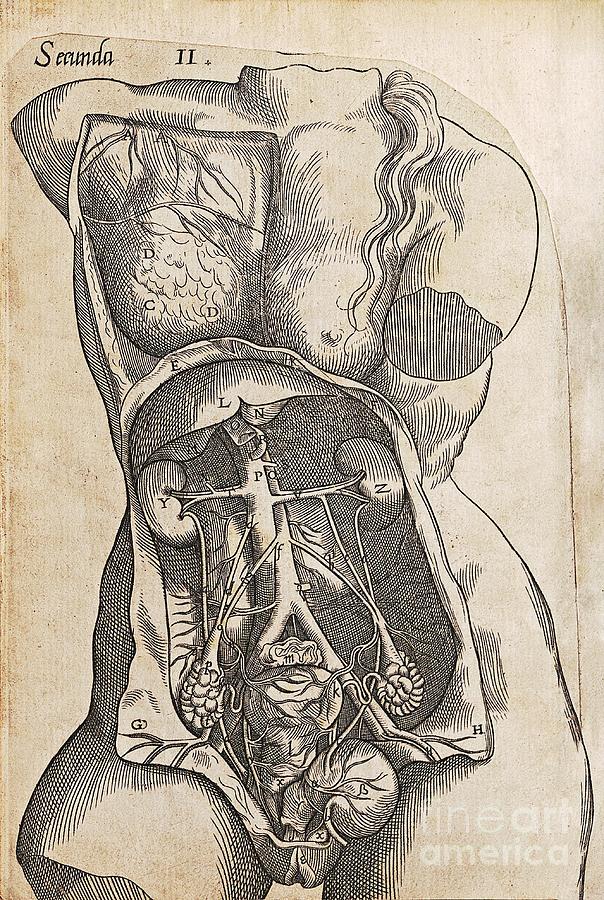 Contractions are involuntary periodic contractions of the muscles of the uterus, aimed at shortening and opening the cervix. Normally, the length of the cervix is 3-5 cm, and the diameter is only a few millimeters. And for the birth of a child, it is necessary that the cervix completely shorten and open up to 9-10 cm.
Contractions are involuntary periodic contractions of the muscles of the uterus, aimed at shortening and opening the cervix. Normally, the length of the cervix is 3-5 cm, and the diameter is only a few millimeters. And for the birth of a child, it is necessary that the cervix completely shorten and open up to 9-10 cm.
The period of dilation is the longest in the process of childbirth. In the natural course of childbirth, this period lasts 10-11 hours for primiparas, 6-7 hours for multiparous ones.
At the beginning of this period there are regular contractions that last 15-20 seconds with an interval of about 15 minutes. As the cervix dilates, the contractions intensify, become longer, and the intervals between them shorten. When the break between contractions is 10 minutes, you need to go to the maternity hospital.
During the opening period, it is recommended to walk, move, breathe properly, take a warm shower or bath. These measures contribute to a faster opening of the cervix, while reducing pain. You can ask your husband or midwife to massage the lumbar region - this will reduce the discomfort from contractions.
You can ask your husband or midwife to massage the lumbar region - this will reduce the discomfort from contractions.
Second stage of labor
Most women agree that the end of the dilation phase, before the onset of the second stage of labor, is the most difficult. Contractions become frequent and painful, anesthesia by this moment usually ceases to act, fatigue accumulates, it is still impossible to push. The state of many women at this moment is described by one single phrase: “That's it! I can not anymore!". The only consolation is that it doesn't last long.
After the cervix is fully dilated, the doctor allows the mother to push. A woman usually herself feels strong urges to "push" the child out of the birth canal. These urges are called pushes.
In order for pushing to be effective, you need to push properly and breathe properly. Before pushing, you need to get more air into the lungs, hold your breath and try to push effectively. It is important not to strain your face and legs during attempts, but on the contrary - to relax as much as possible. Between attempts, you also need to relax and rest.
Between attempts, you also need to relax and rest.
The second stage of labor lasts from 15 minutes to two hours, and in multiparous this stage is shorter than in primiparas. During this period, doctors especially carefully monitor the condition of the mother and fetus (they regularly listen to heartbeats, etc.).
Meanwhile, the baby is moving along the genital tract. At the height of one of the attempts from the genital slit, the lower pole of the head (or buttocks - in breech presentation) is shown, after the end of the attempt, the head is hidden in the genital slit. This process - cutting the head - continues for some time. At a certain moment, the pole of the head remains in the genital gap and in between attempts. Under the influence of continuing attempts, the eruption of the head begins, which continues until its full birth. There is very little left. A few more attempts - and the whole child is born.
The newborn is placed on the mother's belly (ideally) and they get to know each other for a while, resting after the birth.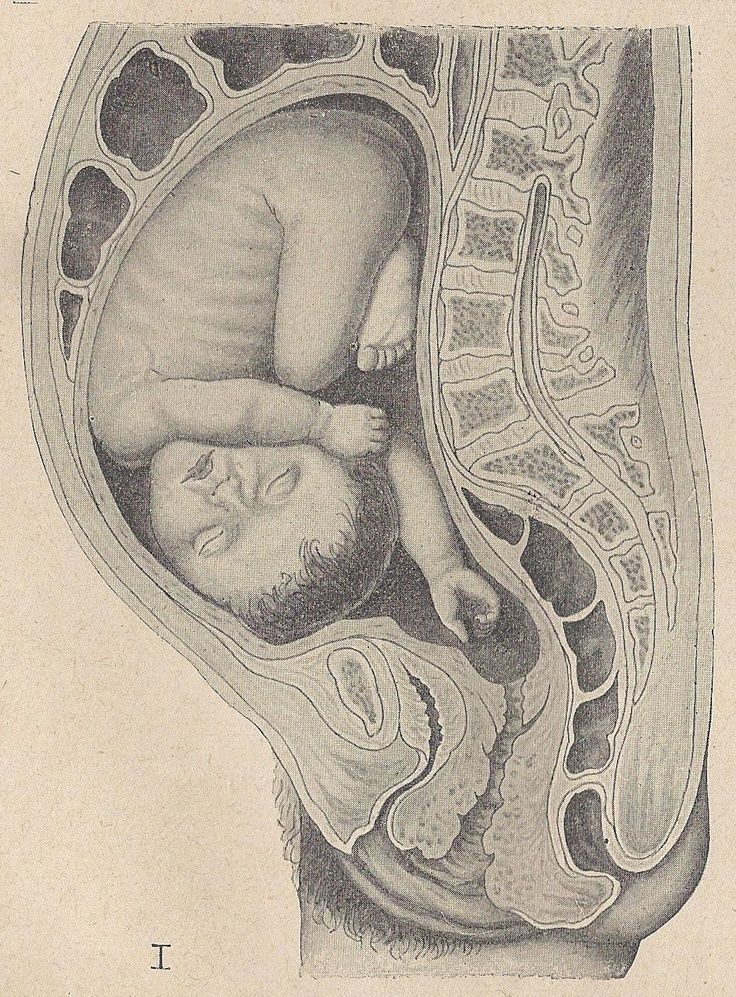 The midwife or doctor then cuts the umbilical cord and takes the baby away for proper treatment, bathing, weighing and examination by a pediatrician.
The midwife or doctor then cuts the umbilical cord and takes the baby away for proper treatment, bathing, weighing and examination by a pediatrician.
10-15 minutes after the birth of the baby can be applied to the breast. This promotes uterine contraction and milk production.
Third stage of labor
The last stage of labor - the birth of the placenta - is the shortest. Usually, the afterbirth is born 10-20 minutes after the birth of the baby. Mom might need to push a little for this.
If the placenta does not separate for more than 30 minutes, doctors diagnose the retention of the placenta in the uterus and begin to take emergency measures.
The delivered placenta is carefully examined for its integrity. If everything is fine, that is, the placenta has separated completely, the woman is sewn up with tears or incisions (if any). After that, a heating pad with ice is placed on her stomach and observed for some time in the delivery room (1.5-2 hours).
This is where the birth process ends and a new life begins for mother and baby.
References
- Florian S., Ichou M., Panico L. Parental migrant status and health inequalities at birth: The role of immigrant educational selectivity. // Soc Sci Med - 2021 - Vol278 - NNULL - p.113915; PMID:33905985
- Naja S., Al Kubaisi N., Singh R., Abdalla H., Bougmiza I. Screening for antenatal depression and its determinants among pregnant women in Qatar: revisiting the biopsychosocial model. // BMC Pregnancy Childbirth - 2021 - Vol21 - N1 - p.330; PMID:33902481
- Shchepin VO., Khabriev RU. [The characteristics of population mortality of the Russian Federation, the Central Federal Okrug and City of Moscow in 2020]. // Probl Sotsialnoi Gig Zdravookhranenniiai Istor Med - 2021 - Vol29 - N2 - p.189-193; PMID:332
- Saavedra LPJ., Prates KV., Gonçalves GD., Piovan S., Matafome P., Mathias PCF. COVID-19 During Development: A Matter of Concern.
 // Front Cell Dev Biol - 2021 - Vol9 - NNULL - p.659032; PMID:33898461
// Front Cell Dev Biol - 2021 - Vol9 - NNULL - p.659032; PMID:33898461 - Caparros-Gonzalez RA., Romero-Gonzalez B., Puertas-Gonzalez JA., Quirós-Fernandez S., Coca-Guzman B., Peralta-Ramirez MI. [Midwives and psychologists as professionals to screen and prevent pregnancy-specific stress.] // Rev Esp Salud Publica - 2021 - Vol95 - NNULL - p.; PMID:33896933
- Burakowska K., Gorka P., Penner GB. Effects of canola meal inclusion rate in starter mixtures for Holstein heifer calves on dry matter intake, average daily gain, ruminal fermentation, plasma metabolites, and total-tract digestibility. // J Dairy Sci - 2021 - Vol - NNULL - p.; PMID:33896627
- Toker E., Aktaş S. The childbirth experiences of Syrian refugee mothers living in Turkey: a qualitative study. // J Reprod Infant Psychol - 2021 - Vol - NNULL - p.1-17; PMID:33896296
- Mérillet L., Pavoine S., Kopp D., Robert M., Mouchet M. Biomass of slow life history species increases as local bottom trawl effort decreases in the Celtic sea.
 // J Environ Manage - 2021 - Vol290 - NNULL - p.112634; PMID:33895454
// J Environ Manage - 2021 - Vol290 - NNULL - p.112634; PMID:33895454 - Patskun E., Yevtushok L., Zymak-Zakutnia N., Lapchenko S., Akhmedzhanova D., Wertelecki W. A teratology information system in vernacular: Closing an information gap. // Birth Defects Res - 2021 - Vol - NNULL - p.; PMID:33893758
- Fu A., Liu C. Is Pregnancy Following a TRAM or DIEP Flap Safe? A Critical Systematic Review and Meta-analysis. // Aesthetic Plast Surg - 2021 - Vol - NNULL - p.; PMID:33893518
What does the child feel during childbirth?
Children, unlike mothers, cannot share their birth stories…maybe it is not in vain that this is provided by nature?
PRESSURE for uterine contractions. The child is not endangered; during normal childbirth, it is protected by amniotic fluid. When passing through the birth canal, the anatomy (bone mobility) helps to compensate for pressure and prevent injuries to the child.
STRESS , in a good way.
SON . The baby can maintain the sleep cycle it is used to in the womb and sleep up to 50 minutes every hour.
DISTRESS fetus. If the pregnancy did not go very smoothly, the condition of the child during childbirth may worsen. For example, oxygen delivery may decrease, and the heartbeat will worsen. Therefore, during childbirth, KTG . If so, the doctors take the necessary measures.
PAIN during the period of exile. With a normal birth, it is not very strong. If, for example, a child is born with a birth tumor, it is logical that he was not well. But the sensations experienced by the child are not comparable with the sensations of the mother.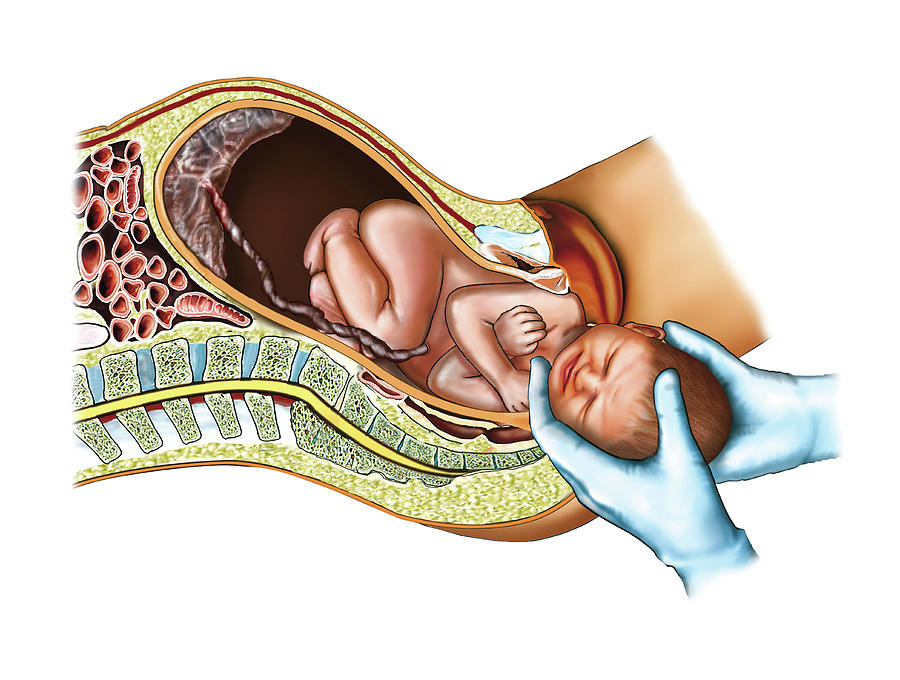 This is due to the fact that the pain receptors in the newborn are not yet fully developed.
This is due to the fact that the pain receptors in the newborn are not yet fully developed.
MOOD mother. It is necessary to remain calm and positive not only during pregnancy, but also during childbirth. It has been proven that the baby's heartbeat slows down, and he calms down when he hears the mother's voice. No matter how the birth goes, the child understands that “something is wrong”, so it is important for him to hear his mother. There are also studies that prove the positive effect of mother's laughter on the child. Women in childbirth don't often laugh, but having a partner help create the right atmosphere would be great!
EFFECTS OF DRUGS . Much that enters the mother's body crosses the placental barrier. With general anesthesia, the child may fall asleep or even stop breathing. Therefore, the preferred method of pain relief is epidural anesthesia. The absorption of its components is minimal, so we can say that it practically does not enter the bloodstream of the fetus and does not have a systemic effect on its body.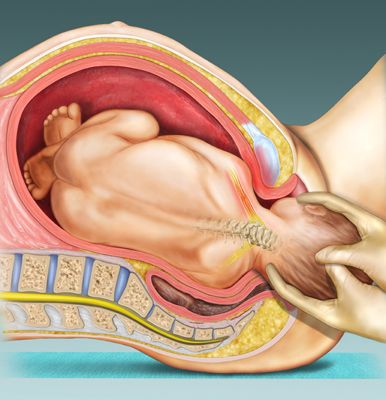
FIRST BREATH . The crying of a baby after birth speaks of the health of his lungs. During the first breath, the lungs begin to expand, and this mechanism is accompanied by a cry. At the same time, the first breath and cry allow you to clear the lungs of amniotic fluid.
SENSOR OVERLOAD . After giving birth, everything around becomes colder, noisier and brighter.
TEMPERATURE CHANGE . Amniotic fluid facilitates the transition from uterine temperature to ambient temperature, and the physiology of the newborn compensates for temperature changes. Moreover, in rodboxes we maintain a comfortable temperature for mother and child, and we put newborns on special heated tables.
CONTACT WITH MOM . It is proved that the first hour after childbirth plays a fundamental role in the further development of the baby. Therefore, the procedures for weighing, washing, etc. are postponed in favor of the soonest establishment of skin-to-skin contact.