What week is your 2nd trimester
What To Expect, Development & Tests
What is the second trimester of pregnancy?
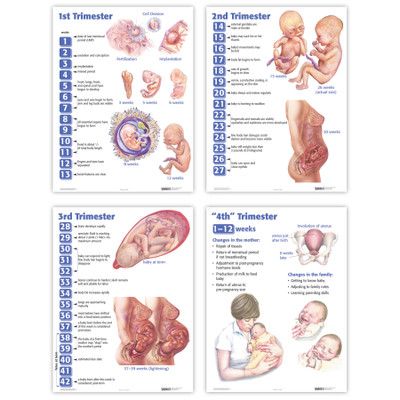
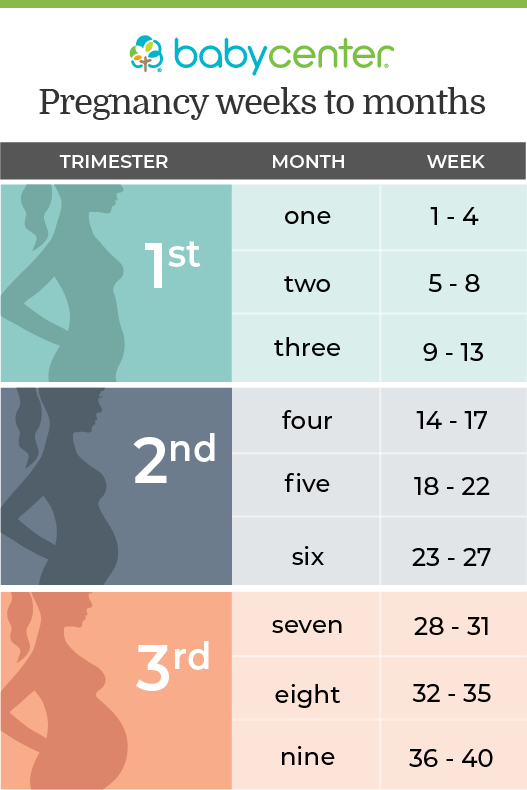
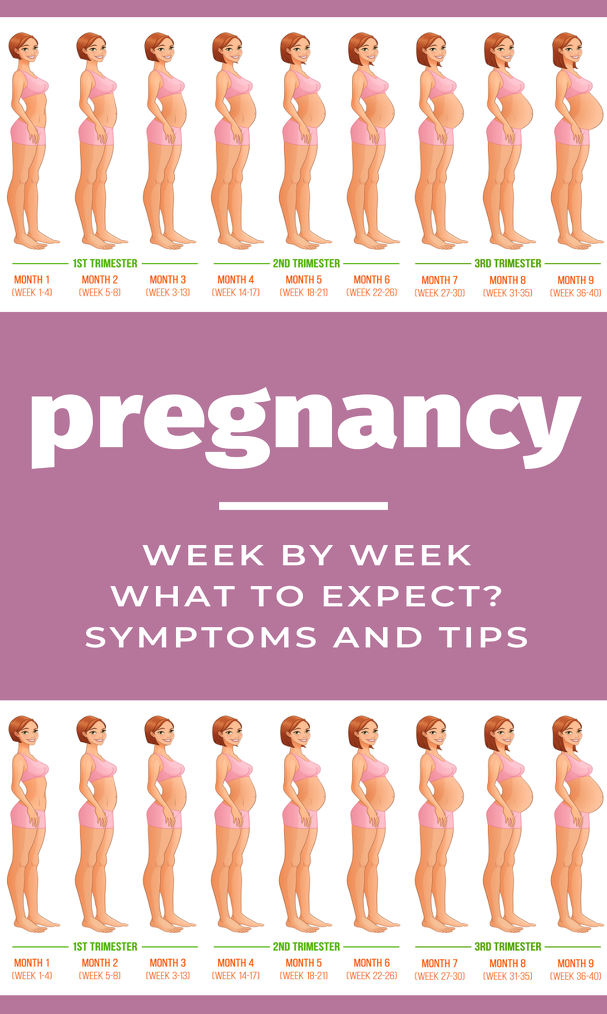
The typical pregnancy lasts about 40 weeks. It’s divided into three periods of time — the first, second and third trimester. Each trimester is roughly 14 weeks long. When you enter your second trimester, you are around 14 weeks pregnant. This middle trimester will last from week 14 to the end of week 27.
During your second trimester of pregnancy, you’ll start looking and feeling more pregnant. For many people, this is the best part of pregnancy because the morning sickness and fatigue of their first trimester fade into the past. Often, any anxiety that went with your first trimester also starts to diminish at this point. You’ll start to feel your fetus move by the end of this trimester, and you might begin to settle into your pregnancy and enjoy it more. Of course, it’s important to remember that pregnancy is different for everyone. Some people never experience negative symptoms like morning sickness in their first trimester. Others might continue to feel sick well into their second trimester of pregnancy.
How does my baby develop during the second trimester of pregnancy?
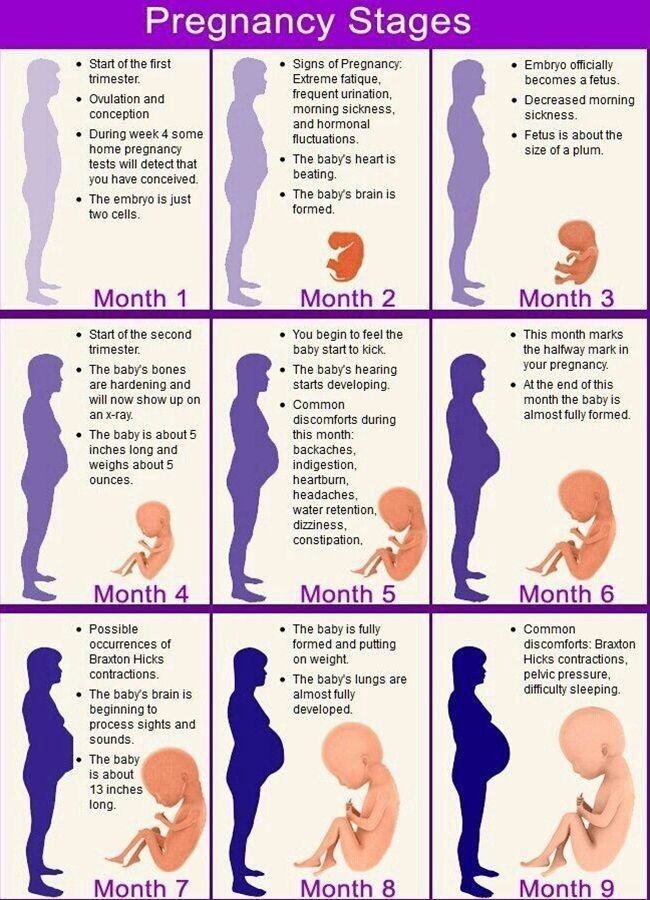
Your fetus will go through many changes during your second trimester of pregnancy. During this trimester, the fetus starts to look more like a child — with its facial features aligning, and its fingers and toes becoming well-defined. By month four, the fetus will actually have eyelids, eyebrows, eyelashes, nails and hair. The fetus will also be able to stretch, make faces and even suck on its thumb. You’ll soon be able to determine the sex of the fetus on an ultrasound — often around 20 weeks.
At this point, you might also start feeling the fetus move. The movement is often described as a flutter or similar to the feeling of having butterflies in your stomach. The fetus will be doing flips and movements throughout your second trimester. This first movement is called the quickening. If this isn’t your first pregnancy, you might feel the fetus move sooner.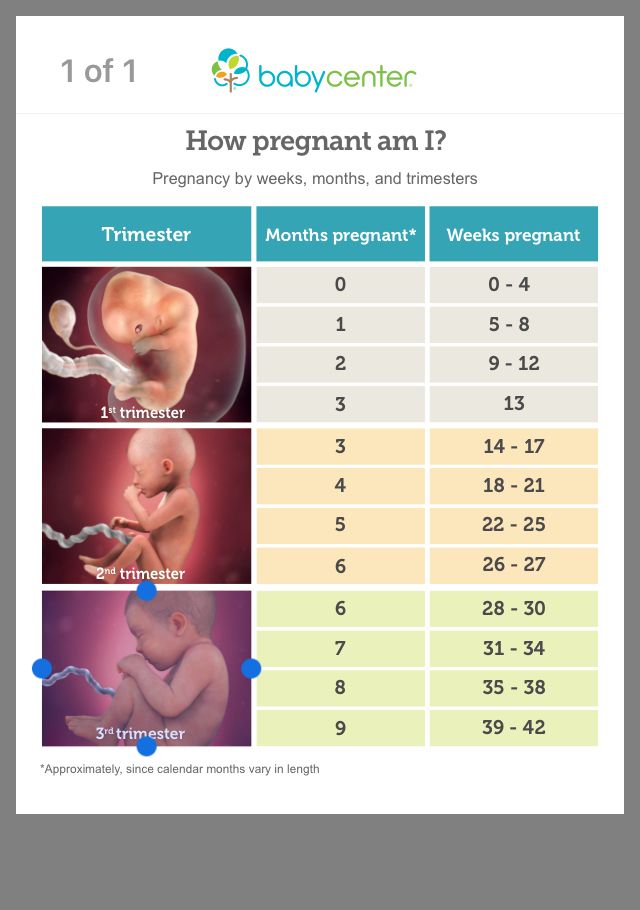
In the last few weeks of the second trimester, the fetus can also hear you. If you talk to your growing belly, you might notice movement in response.
If your baby was born at the end of your second trimester (premature birth), they would be likely to survive with intensive care.
What happens to my body during the second trimester of pregnancy?
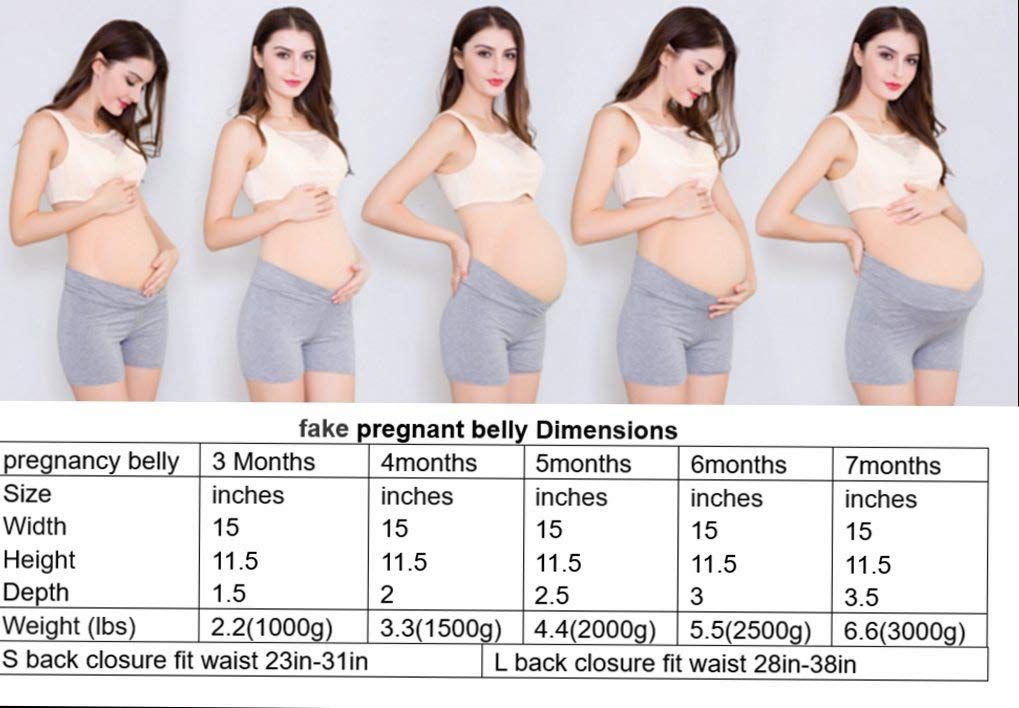
The fetus isn’t the only one growing and changing during your second trimester. You'll notice several changes in your own body during this time. Your uterus — the place where the fetus grows during pregnancy — continues to stretch. This organ will expand throughout your pregnancy as the fetus gets larger. After pregnancy, your uterus will return to its pre-pregnancy size (picture an upside-down pear).
However, your uterus isn’t the only thing growing during the second trimester either. You’ll start gaining weight and might start developing the tell-tale enlarged belly of a pregnant person. Don’t worry if this takes time to develop.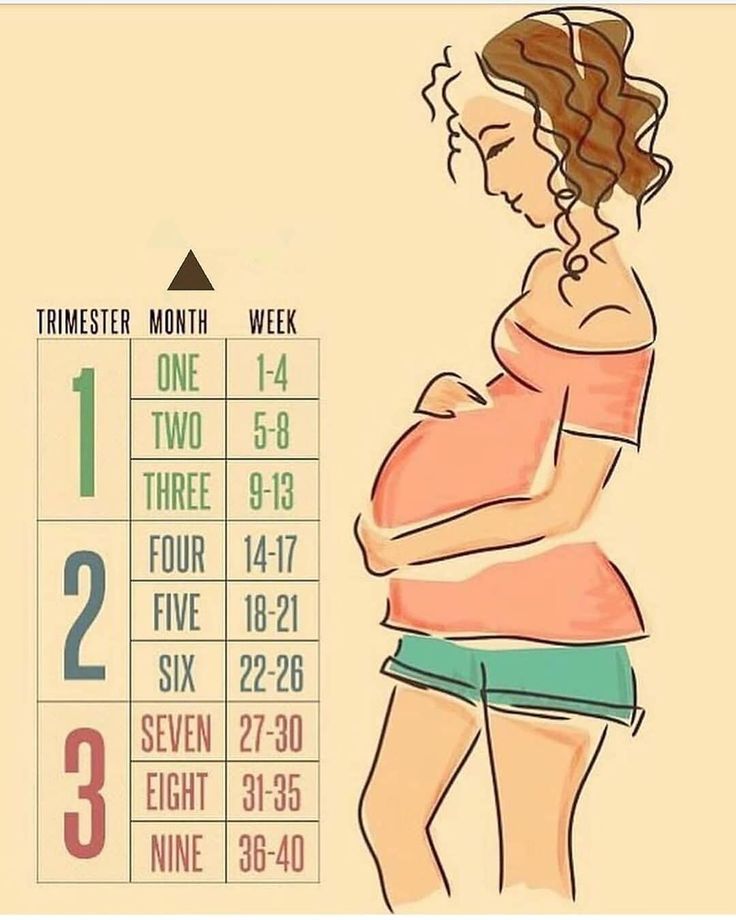 Everyone is different, and no two bodies will look exactly the same during pregnancy.
Everyone is different, and no two bodies will look exactly the same during pregnancy.
You might also feel or develop a few new symptoms of pregnancy during your second trimester, including:
- An increased appetite.
- An achy body.
- Some swelling in your hands, feet and ankles.
- Some stretch marks.
If you experienced morning sickness during your first trimester, it’s likely fading away now. The uncomfortable symptoms of early pregnancy (nausea and extreme fatigue, for example) don’t typically continue into your second trimester. This is one reason why many people consider their second trimester of pregnancy to be the best part of pregnancy.
What tests will I have during the second trimester of pregnancy?
Throughout your pregnancy, your healthcare provider will order various tests to check on your health and the health of your developing fetus. During your second trimester, you’ll typically be screened for a few different things, including the Rh factor of your blood and the condition gestational diabetes. You'll also have an ultrasound during your second trimester. This ultrasound is probably best known for telling new parents the sex of the fetus, but it’s mainly used to look at their anatomy.
You'll also have an ultrasound during your second trimester. This ultrasound is probably best known for telling new parents the sex of the fetus, but it’s mainly used to look at their anatomy.
One thing your provider will test for during your second trimester is your Rh factor. Rh factor is an antigen protein found on most people’s red blood cells. If you don’t have the protein, then you are Rh- (negative). You’ll be given an injection of Rh immune globulin (called Rhogam®) during the 28th week of your pregnancy to prevent the development of antibodies that could be harmful to the fetus. You’ll also be given an injection of Rhogam® after delivery if your fetus has Rh+ (positive) blood.
If you are Rh-, you may also receive this injection if you:
- Are having an invasive procedure (such as amniocentesis).
- Had an abdominal trauma.
- Had any significant bleeding during pregnancy.
- Need to have the fetus turned in your uterus (due to breech presentation).
Your provider will also order a test called the oral glucose screening test. This is usually done at the end of your second trimester — often between weeks 24 and 28. The purpose of the glucose screening test is to see if you are developing gestational diabetes. During the test, you’ll be given a syrup-like drink. The healthcare provider administering this test will give you a set amount of time to drink the entire bottle, then you'll be asked to wait nearby for one hour. After the hour is over, you’ll have your blood drawn. Your healthcare provider will then go over your test results with you.
What do I need to prepare or plan for during the second trimester of pregnancy?
There are many things you can start thinking about during your second trimester of pregnancy to prepare for your new family member. Many of these things will center around conversations that you should start having at this point in your pregnancy. It’s good to discuss the type of birth you hope to have and learn about the different ways your child might be born.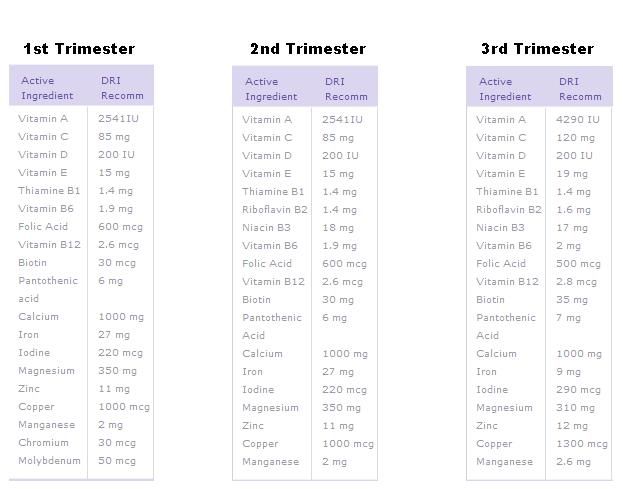
A few ways your baby could be born can include:
- Vaginal birth (this could be medicated so that your pain is decreased, or unmedicated).
- Assisted birth (you might need tools like forceps or a vacuum to help with your delivery).
- Cesarean section (C-section).
You can learn more about these types of birth through your own research or in a birth class. This is the time for you to look into educational classes about birth, breastfeeding and parenting of your newborn. These classes can help prepare you for your new role as a parent. Ask your healthcare provider for more information on classes and groups you can join at this point in your pregnancy.
This might also be a good time to take a tour of the hospital where you’ll give birth. A hospital tour is a great way to get familiar with the place where your baby will be born. During the tour, you’ll learn where you should go when you first get to the hospital during labor and what will happen afterward.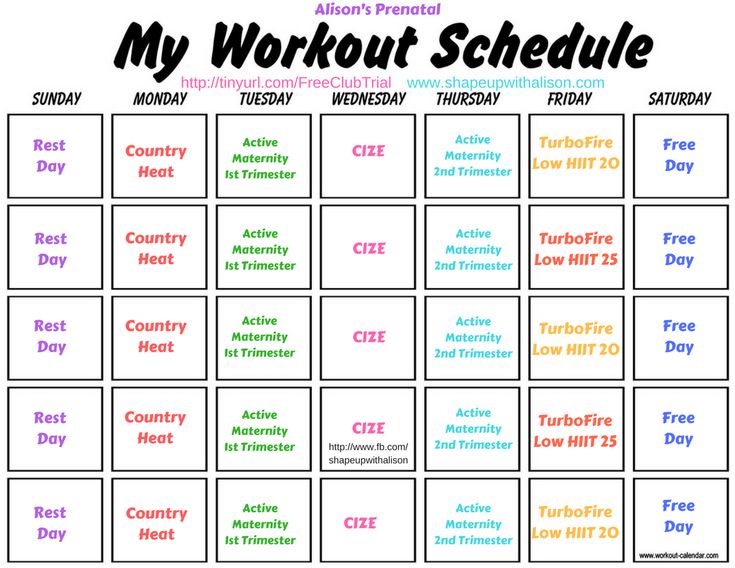 You’ll typically get to see hospital rooms and learn more about the hospital staff, as well.
You’ll typically get to see hospital rooms and learn more about the hospital staff, as well.
What should I be doing during the second trimester of pregnancy to stay healthy?
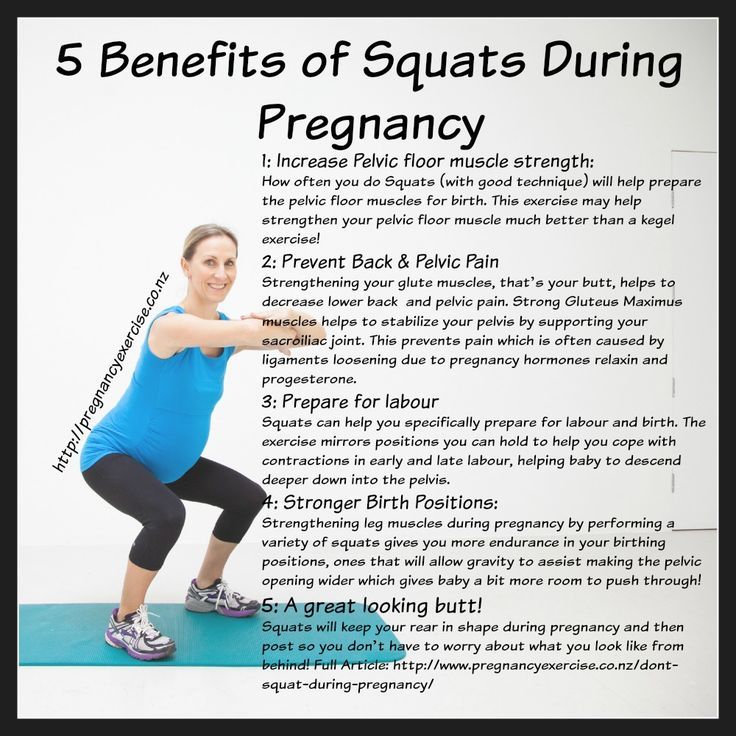
Throughout your second trimester, you should continue maintaining a healthy lifestyle. Try to exercise for about 20 minutes a day. Regular exercise is good for you and your developing fetus. Some of the safest types of exercise include walking and swimming; though, there are many other options you can try. Talk to your healthcare provider about the type of exercise you'd like to do beforehand just to be safe. You’ll want to avoid contact sports and activities where you could fall, as these could endanger your pregnancy.
It’s also a good idea to do kegel exercises throughout your entire pregnancy. These exercises will help strengthen your pelvic floor muscles.
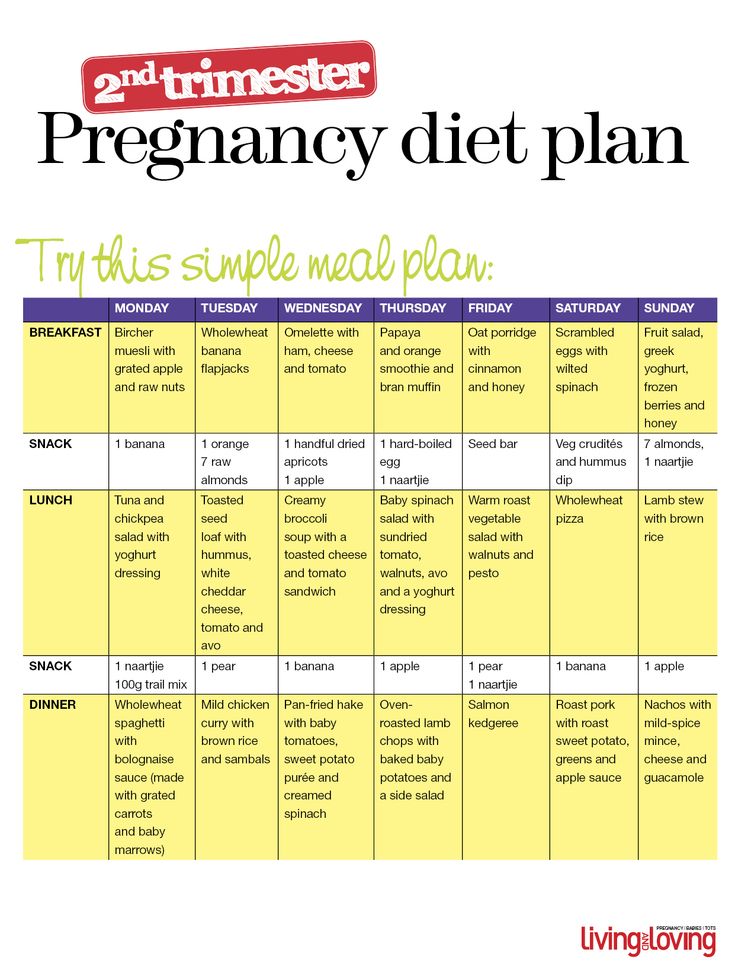
Apart from exercise, you should continue eating a healthy diet, taking your prenatal vitamins and attending each of your appointments.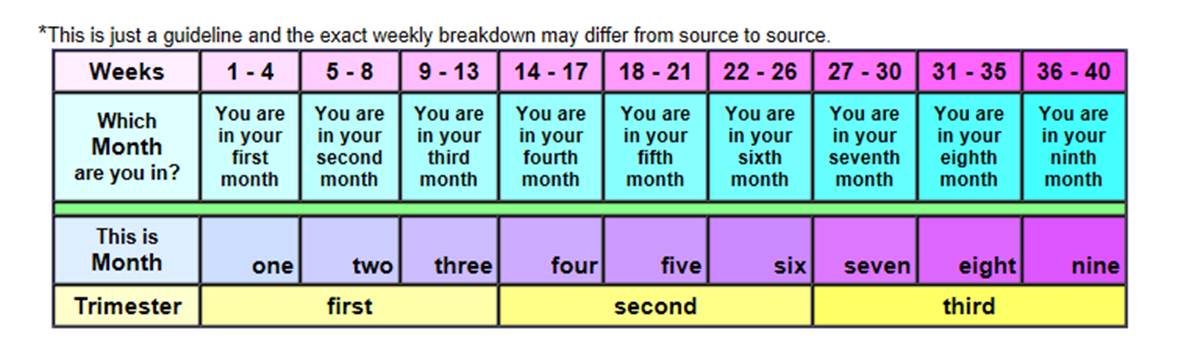
When should I call my doctor during the second trimester of pregnancy?
You’re the person who knows your body the best. If you ever feel like something is wrong, it’s completely OK to reach out to your healthcare provider. It’s also a good idea to call your healthcare provider right away if you have:
- Unusual or severe cramping or abdominal pain.
- Noticeable changes in how much the fetus moves (after 28 weeks of gestation). If you don’t count six to 10 movements in one hour or less, call your provider.
- Difficulty breathing or shortness of breath that seems to be getting worse over time.
You should also reach out to your provider right away if you start having any signs of premature labor. Talk with your provider if you have any of the following signs of premature labor:
- Regular tightening or pain in your lower abdomen or back that occurs more than four times in an hour.
- Any bleeding in your second or third trimester of pregnancy.

- Any fluid leakage. Vaginal discharge often increases as part of the hormonal changes in pregnancy.
- Pressure in your pelvis or vagina.
13 Weeks Pregnant | Pregnancy
You are now a 3rd of the way through your pregnancy and you're hopefully through the worst of your symptoms.
What's happening in my body?
A small baby bump may now be visible as your uterus (womb) grows upwards and outwards. If you've been feeling the urge to pee more often, that should stop as the womb moves away from your bladder.
Meanwhile, there's a lot more blood pumping around your pelvic area and some women find that it increases their sex drive. It could also make you feel more thirsty, so drink lots of fluids.
Sex during pregnancy is perfectly safe, unless your midwife or doctor has advised you otherwise.
Infection alert
There are ways you can protect yourself and the baby from many harmful viruses and bacteria:
- Try to avoid contact with anyone who has chickenpox or rubella – talk to your doctor or midwife straight away if you think you could be infected.
- If you have a cat, get someone else to empty the cat litter tray, as the faeces could contain a bug called toxoplasma gondii. This can cause an infection called toxoplasmosis that could damage your unborn baby.
- You can also get toxoplasmosis from certain foods. Foods to avoid during pregnancy include undercooked meats, cured meats like salami, and unpasteurised goats' milk and cheese.
- Seek advice before travelling to any area affected by the Zika virus, as the virus can cause birth defects.
Read more about infections in pregnancy on the NHS website.
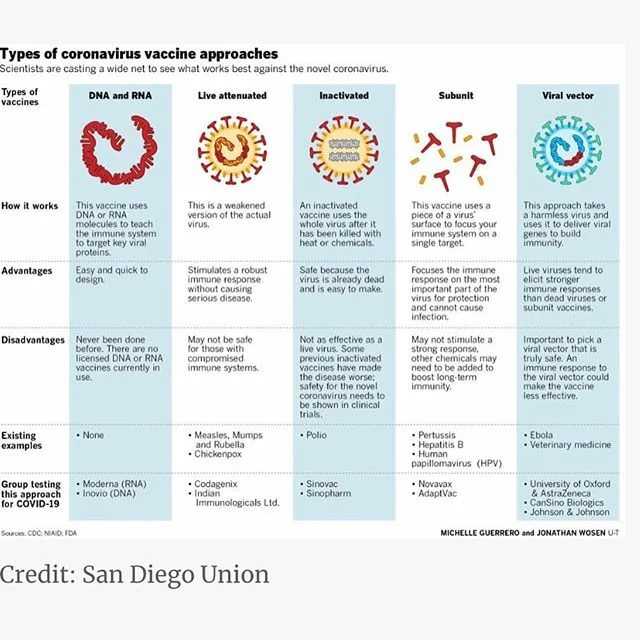
Coronavirus (COVID-19)
You and your family should follow the government and NHS guidance on coronavirus (COVID-19):
- read government guidance on how to stay safe from COVID-19
- get NHS advice about COVID-19
- use the NHS COVID-19 app for England and Wales - it's the fastest way of knowing when you've been exposed to COVID-19
Teeth troubles
Swollen, painful and bleeding gums are common during pregnancy.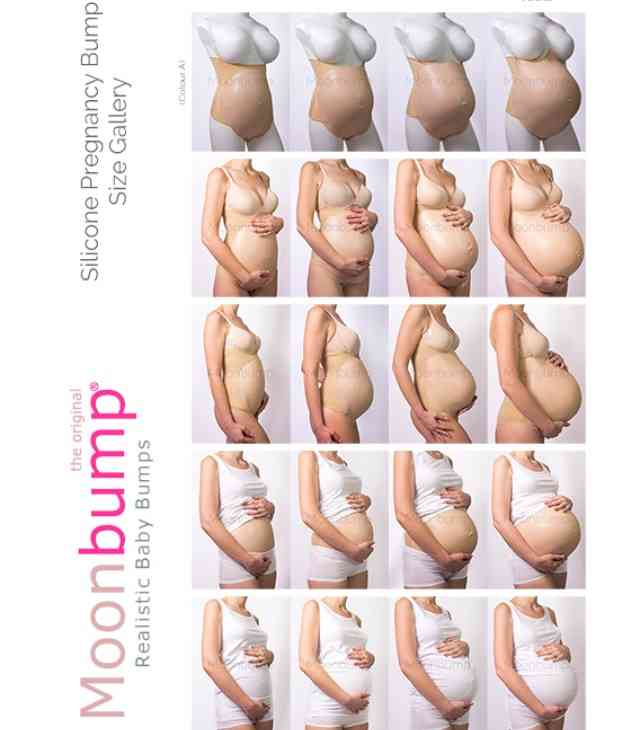 Read about keeping teeth and gums healthy in pregnancy on the NHS website.
Read about keeping teeth and gums healthy in pregnancy on the NHS website.
You are entitled to free NHS dental care during pregnancy and for a year after your baby is born. Ask your doctor or midwife for a maternity exemption certificate.
You already know the basics – clean your teeth twice a day, avoid sugary snacks and drinks, and don't smoke as it can make gum disease worse. But did you also know that:
- a soft toothbrush is best for sensitive gums
- you should brush in gentle circles, up and down
- if you're sick, protect your teeth by rinsing your mouth out with water, to flush away harmful acid in your vomit
- you should stick to alcohol-free mouthwashes to reduce plaque
2nd trimester pregnancy symptoms (at 13 weeks)
Your signs of pregnancy could include:
- swollen and bleeding gums
- pains on the side of your belly caused by your expanding womb (known as "round ligament pains")
- headaches
- nosebleeds
- bloating (read ways to cope with bloating on week 10's page)
- constipation (read about how to treat constipation on week 16's page)
- indigestion and heartburn (read ways to cope with indigestion and heartburn on week 25's page)
- sore breasts
- leg cramps
- feeling hot
- dizziness
- swollen hands and feet
- urine infections
- vaginal infection (read about how to treat vaginal infections on week 15's page)
- darkened skin on your face or brown patches – this is known as chloasma or the "mask of pregnancy"
- greasier, spotty skin
- thicker and shinier hair
You may also still experience symptoms from earlier weeks, including:
- morning sickness
- unusual pregnancy cravings
- heightened sense of smell
- mood swings
- white milky pregnancy discharge from your vagina
- light spotting (seek medical advice for any bleeding)
Read Tommy's guide to common pregnancy symptoms.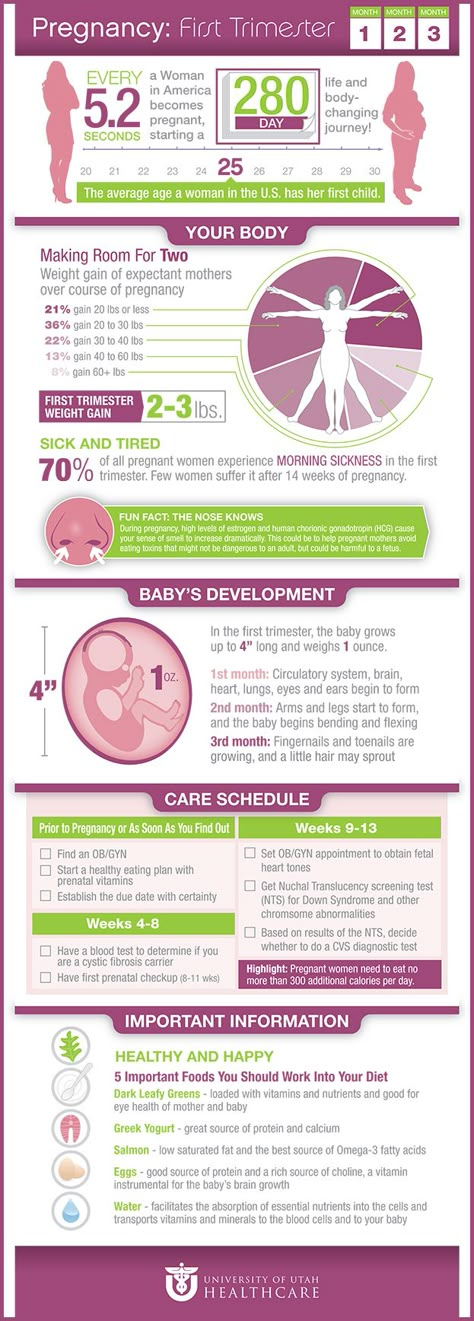
What does my baby look like?
Your baby, or foetus, is around 7.4cm long, which is about the size of a peach. The weight is about 25g, which is as heavy as a toothbrush with toothpaste on it.
Your baby's ovaries or testes are fully developed inside and final tweaks are being made on the outside. The baby is moving around. At first the movements are very jerky and random but then they start to look more deliberate.
You may not feel any movement until around week 17. Some babies suck their thumb in the womb. This actually serves a purpose as it helps to develop their sucking reflex. They'll need this when it comes to feeding.
Action stations
Many women will tell their employer after they've had their first pregnancy scan at around 12 weeks. Once you tell your employer, you have maternity rights and can attend antenatal appointments during paid work time. You can also ask for a risk assessment of your workplace to ensure that you're working in a safe environment.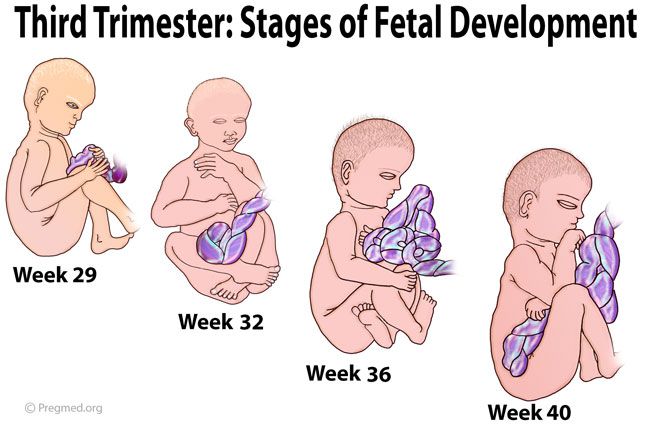
It's a good time to tone up your pelvic floor muscles. Gentle exercises can help to prevent leakage when you laugh, sneeze or cough. Get the muscles going by pretending that you're having a pee and then stopping midflow. Visit Tommy's for more information on pelvic floor exercises.
Ask your midwife or doctor about online antenatal classes – they may be able to recommend one. The charity Tommy's has lots of useful information on antenatal classes and preparing you for birth.
Even if you've had children before, antenatal classes are still worth going to as you can meet other parents-to-be. The NCT offers online antenatal classes with small groups of people that live locally to you.
To keep bones and muscles healthy, we need vitamin D. From late March/early April to the end of September, most people make enough vitamin D from sunlight on their skin. However, between October and early March, you should consider taking a daily vitamin D supplement because we cannot make enough from sunlight.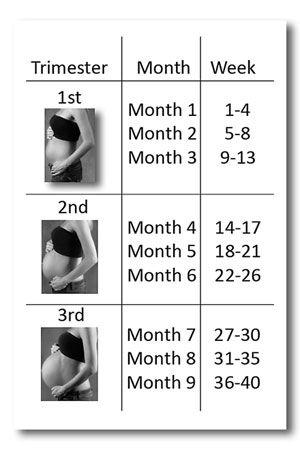
Some people should take a vitamin D supplement all year round, find out if this applies to you on the NHS website. You just need 10 micrograms (it's the same for grown-ups and kids). Check if you're entitled to free vitamins.
It's recommended that you do 150 minutes of exercise a week while pregnant. You could start off with just 10 minutes of daily exercise - perhaps take a brisk walk outside. Check out Sport England's #StayInWorkOut online exercises (scroll to the pregnancy section). Listen to your body and do what feels right for you.
There's no need to eat for 2. You don't need any extra calories until the 3rd trimester, which starts in week 28. Try to eat healthily, with plenty of fresh fruit and veg, and avoid processed, fatty and salty foods. You may be able to get free milk, fruit and veg through the Healthy Start scheme.
You and your family should follow the government and NHS guidance on coronavirus (COVID-19):
To find out about about COVID-19 and pregnancy, childbirth and breastfeeding, have a look at advice on the:
Second trimester of pregnancy (from 13 to 28 weeks)
The beginning of the second trimester is traditionally considered one of the calmest. Walk more. Walking is very helpful. Sit down to rest only when you are tired. Movement in the fresh air improves the supply of oxygen to the fetus, which is very necessary for its normal development.
Walk more. Walking is very helpful. Sit down to rest only when you are tired. Movement in the fresh air improves the supply of oxygen to the fetus, which is very necessary for its normal development.
Nausea disappears, appetite improves. Do not eat a lot of salty, refuse marinades, smoked meats, if you have not done this before. The increased need of the child's body for proteins and vitamins begins. The daily diet should include meat or fish (boiled or stewed), dairy products, especially cottage cheese, eggs. Do not forget about vegetables, fruits, greens. An excellent source of vitamin C is sauerkraut (rather than salted) cabbage. Salads from carrots, cabbage, beets, apples, green radish should be on your table every day.
At 17-20 weeks you will feel your baby's first kicks. From them you can determine how comfortable the baby feels. Intense tremors are a signal of lack of oxygen. Maybe you haven’t walked for a long time or, on the contrary, you are engaged in hard physical labor.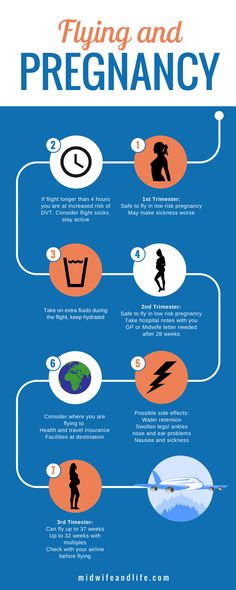 Get out into the fresh air or lie down to rest and you will immediately feel how the child has calmed down.
Get out into the fresh air or lie down to rest and you will immediately feel how the child has calmed down.
But the lack of movement is an alarm. See a doctor immediately!
The fetal need for calcium sharply increases - intensive growth of the skeleton has begun. If you don't have enough free calcium in your body right now, you could lose your teeth. To prevent this from happening, start taking calcium supplements in consultation with your doctor.
At this time, toxicosis of the second half of pregnancy may occur, the child suffers greatly from it. Therefore, if the doctor suggests hospitalization, do not refuse. Toxicosis can, if not be avoided, then at least reduce its manifestations. Be sure to follow your diet. Completely exclude salty, smoked, fried, spicy, canned food, chocolate. Do not eat a lot of grapes and drink fresh milk. Limit flour and rich products. As before, your diet should include boiled meat and fish, oatmeal and buckwheat porridge, vegetables and fruits
Periodically, once a week, check for fluid retention in the body. It is allowed to release liquid 200-300 ml less than what was drunk. If little urine is released, this is a signal of latent edema and the onset of toxicosis.
It is allowed to release liquid 200-300 ml less than what was drunk. If little urine is released, this is a signal of latent edema and the onset of toxicosis.
It is very good if you can measure your blood pressure at home. Show the results of measurements at the next visit to the doctor. Both high and too low pressure should alert. With low pressure, blood sluggishly crosses the placenta, and the baby does not receive enough nutrients.
Do not neglect blood tests - it is important not to miss the development of anemia. In this case, you will be prescribed iron supplements and multivitamins. The diet should include beef liver, tomato juice, buckwheat porridge, apples, preferably Antonovskie (they contain more iron than other varieties).
Women who are at risk of giving birth to a child with a genetic pathology (those who have severe hereditary ailments in their families), as well as women over 35 years old (they have an increased likelihood of having a child with Down syndrome) are referred for a consultation by a geneticist.
In case of a normal pregnancy at 20-22 weeks of pregnancy, a second scheduled ultrasound examination is prescribed.
Tests in the second trimester of pregnancy with a discount of up to 50%
Description of analysis
The second trimester (14-28 weeks of pregnancy) is characterized by the final formation of the placenta, the completion of the laying of all organs and systems of the fetus. After the 20th week, the fetus is already considered fully formed.
If you have not yet registered with the antenatal clinic, take the Tests in the 1st trimester of pregnancy (1-13 weeks) and the Coagulogram for pregnant women.
In the second trimester, it is recommended to take this complex once a month to monitor the woman's health and identify early laboratory signs of pregnancy complications.
Test material — Venous blood with EDTA, Blood serum, Plasma EDTA + glucose stabilizer
includes 9 studies
-
Carbohydrate - the main source of energy in the body
-
A mineral that provides oxygen transfer to cells, the work of enzymes
-
All blood calcium, bound to proteins and free
-
Mineral involved in energy metabolism, functioning of the nervous system and cell enzymes
-
Blood cells are responsible for oxygen transport, blood clotting and immune defense
-
ESR increases if the number of erythrocytes is reduced or there are many proteins in the blood, for example, inflammatory
-
Blood protein that binds iron ions
-
Index of thyroid stimulation affecting metabolism, energy, weight and body temperature
-
Protein storing iron in the liver
How to prepare
In advance
It is recommended to take blood in the morning from 8.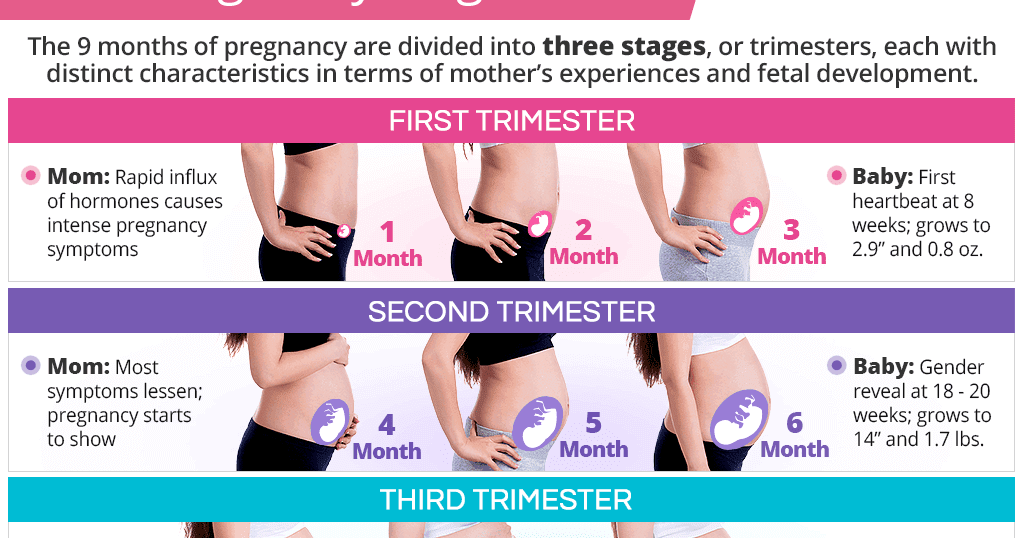 00 to 11.00. To check the dynamics of the indicator each time, select the same intervals for the delivery of the analysis.
00 to 11.00. To check the dynamics of the indicator each time, select the same intervals for the delivery of the analysis.
Talk to your doctor about taking your medications the day before and on the day of your blood test, and any additional preparations you might need.
Do not take a blood test immediately after X-ray, fluorography, ultrasound, physiotherapy.
Taking drugs containing thyroid hormones affects the results of tests for these hormones. Discuss with your doctor whether you need to take tests while taking medications or stop them 7 days before the test. Thyroid hormones are recommended to be taken 3 days after taking medications containing iodine.
The day before
24 hours before blood sampling:
- Limit fatty and fried foods, do not take alcohol.
- Avoid sports and emotional stress.
From 8 to 14 hours before donating blood, do not eat, drink only clean still water.
On the day of donation
Before blood sampling
- 60 minutes without smoking,
- 15-30 minutes to be in a calm state.
Result
-
Electronic result
At the post office and in your personal account when ready
View example
-
References and their meaning
The range within which the result of the analysis is considered normal. However, the indicator a particular analysis should be evaluated in conjunction with others.
View reference
-
Medical consultation
Online consultation based on test results and a questionnaire that you fill out in advance.
 It will be available to order in 2023.
It will be available to order in 2023. See example
2nd trimester tests 14-28 weeks
Pregnancy management is regulated by the Order of the Ministry of Health of the Russian Federation dated November 1, 2012 N 572n "On approval of the Procedure for the provision of medical care in the profile" obstetrics and gynecology (with the exception of the use of assisted reproductive technologies) ".
When the first basic tests were passed, on the basis of an order for monthly monitoring of the course of pregnancy, we developed this complex.
Complete blood count, platelets, leukocyte formula and ESR help to control hemoglobin levels, inflammatory processes in a woman's body, the first signs of pathology of the blood coagulation system and pregnancy complications.
In the second trimester, iron is heavily consumed, and anemia is said to occur when hemoglobin falls below 105 g/L. However, iron stores can be depleted before anemia develops. This will be reflected in a decrease in the level of ferritin (this is the depot of iron in the body) and saturation of transferrin with iron (deficiency in iron transport).
However, iron stores can be depleted before anemia develops. This will be reflected in a decrease in the level of ferritin (this is the depot of iron in the body) and saturation of transferrin with iron (deficiency in iron transport).
During pregnancy, tissue sensitivity to insulin decreases. In this regard, in pregnant women, an increase in plasma glucose levels and the occurrence of transient gestational diabetes mellitus (diabetes mellitus of pregnant women) is possible.
Thyroid hormones are involved in the formation of the membranes of the fetus, its organs and systems, including the brain. Determination of TSH allows you to evaluate the secretion of thyroid hormones by the thyroid gland of a pregnant woman. With the development of preeclampsia (a complication of pregnancy that manifests itself in the second trimester), the level of TSH may increase.
Calcium and magnesium deficiencies also increase the risk of preeclampsia. A pregnant woman should consume enough calcium and magnesium rich foods.