Baby cycle pregnancy
Fetal development: Month-By-Month Stages of Pregnancy
When does a pregnancy start?
The start of pregnancy is actually the first day of your last menstrual period. This is called the gestational age, or menstrual age. It’s about two weeks ahead of when conception actually occurs. Though it may seem strange, the date of the first day of your last period will be an important date when determining your due date. Your healthcare provider will ask you about this date and will use it to figure out how far along you are in your pregnancy.
How does conception work?
Each month, your body goes through a reproductive cycle that can end in one of two ways. You will either have a menstrual period or become pregnant. This cycle is continuously happening during your reproductive years — from puberty in your teen years to menopause around age 50.
In a cycle that ends with pregnancy, there are several steps. First, a group of eggs (called oocytes) gets ready to leave the ovary for ovulation (release of the egg). The eggs develop in small, fluid-filled cysts called follicles. Think of these follicles as small containers for each immature egg. Out of this group of eggs, one will become mature and continue on through the cycle. This follicle then suppresses all the other follicles in the group. The other follicles stop growing at this point.
The mature follicle now opens and releases the egg from the ovary. This is ovulation. Ovulation generally happens about two weeks before your next menstrual period begins. It’s generally in the middle of your cycle.
After ovulation, the opened (ruptured) follicle develops into a structure called the corpus luteum. This secretes (releases) the hormones progesterone and estrogen. Progesterone helps prepare the endometrium (lining of the uterus). This lining is the place where a fertilized egg settles to develop. If you don’t become pregnant during a cycle, this lining is what is shed during your period.
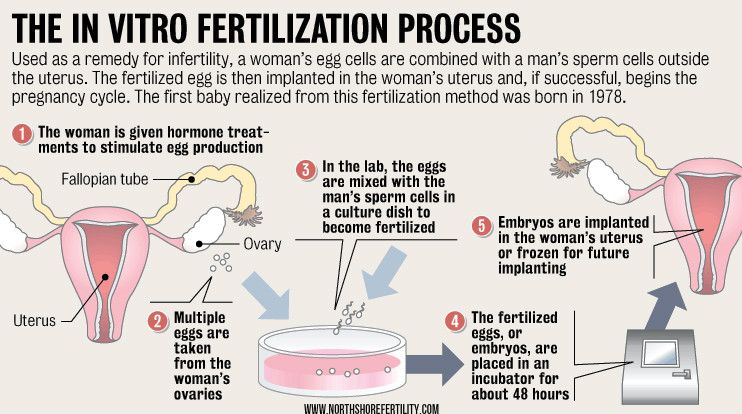
On average, fertilization happens about two weeks after your last menstrual period. When the sperm penetrates the egg, changes occur in the protein coating of the egg to prevent other sperm from entering.
When the sperm penetrates the egg, changes occur in the protein coating of the egg to prevent other sperm from entering.
At the moment of fertilization, your baby’s genetic make-up is complete, including its sex. The sex of your baby depends on what sperm fertilizes the egg at the moment of conception. Generally, women have a genetic combination of XX and men have XY. Women provide each egg with an X. Each sperm can be either an X or a Y. If the fertilized egg and sperm is a combination of an X and Y, it’s a boy. If there are two Xs, it’s a girl.
What happens right after conception?
Within 24 hours after fertilization, the egg begins rapidly dividing into many cells. It remains in the fallopian tube for about three days after conception. Then the fertilized egg (now called a blastocyte) continues to divide as it passes slowly through the fallopian tube to the uterus. Once there, its next job is to attach to the endometrium. This is called implantation.
Before implantation though, the blastocyte breaks out of its protective covering.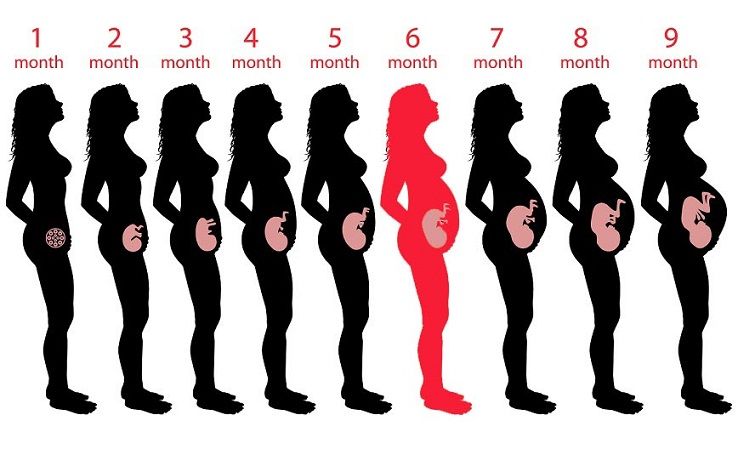 When the blastocyte makes contact with the endometrium, the two exchange hormones to help the blastocyte attach. Some women notice spotting (slight bleeding) during the one or two days when implantation happens. This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
When the blastocyte makes contact with the endometrium, the two exchange hormones to help the blastocyte attach. Some women notice spotting (slight bleeding) during the one or two days when implantation happens. This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
Within three weeks, the blastocyte cells ultimately form a little ball, or an embryo. By this time, the first nerve cells have formed.
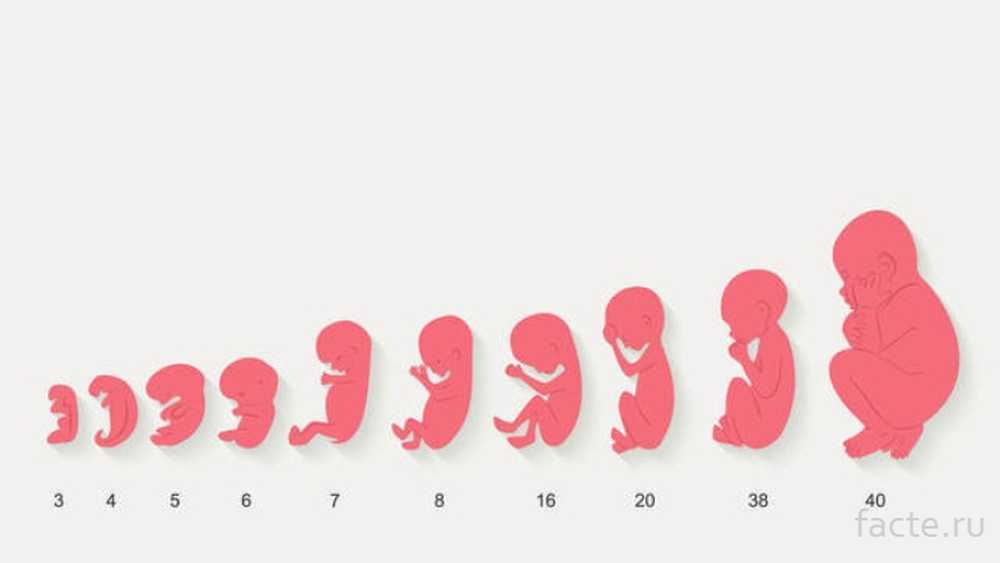
Your developing fetus has already gone through a few name changes in the first few weeks of pregnancy. Generally, it's called an embryo from conception until the eighth week of development. After the eighth week, it's called a fetus until it’s born.
How early can I know I’m pregnant?
From the moment of conception, the hormone human chorionic gonadotrophin (hCG) will be present in your blood. This hormone is created by the cells that form the placenta (food source for the growing fetus). It’s also the hormone detected in a pregnancy test. Even though this hormone is there from the beginning, it takes time for it to build within your body. It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
It’s also the hormone detected in a pregnancy test. Even though this hormone is there from the beginning, it takes time for it to build within your body. It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
When should I reach out to my healthcare provider about a new pregnancy?
Most healthcare providers will have you wait to come in for an appointment until you have had a positive home pregnancy test. These tests are very accurate once you have enough hCG circulating throughout your body. This can be a few weeks after conception. It’s best to call your healthcare provider once you have a positive pregnancy test to schedule your first appointment.
When you call, your healthcare provider may ask you if you are taking a prenatal vitamin. These supplements contain folic acid. It’s important that you get at least 400mcg of folic acid each day during a pregnancy to make sure the fetus's neural tube (beginning of the brain and spine) develops correctly.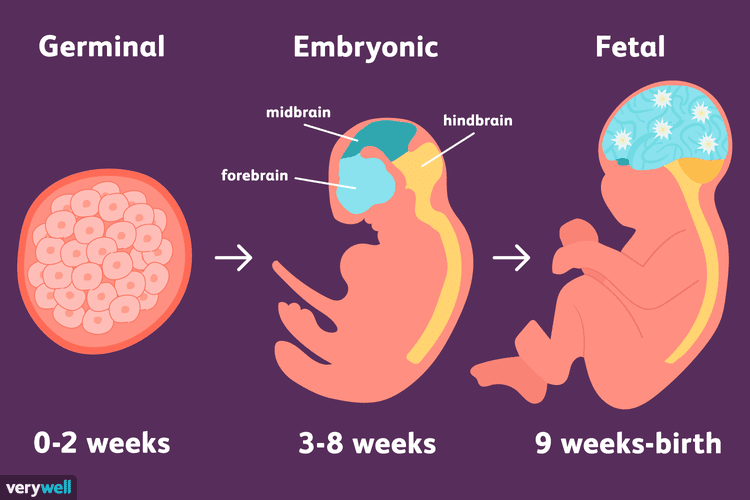 Many healthcare providers suggest that you take prenatal vitamins with folic acid even when you aren’t pregnant. If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
Many healthcare providers suggest that you take prenatal vitamins with folic acid even when you aren’t pregnant. If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
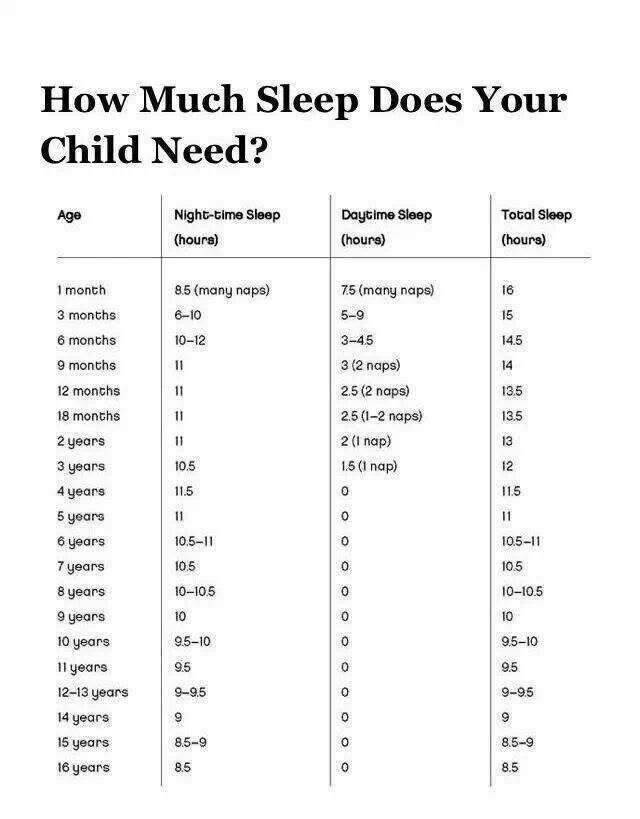
What’s the timeline for fetal development?
The fetus will change a lot throughout a typical pregnancy. This time is divided into three stages, called trimesters. Each trimester is a set of about three months. Your healthcare provider will probably talk to you about fetal development in terms of weeks. So, if you are three months pregnancy, you are about 12 weeks.
You will see distinct changes in the fetus, and yourself, during each trimester.
Traditionally, we think of a pregnancy as a nine-month process. However, this isn’t always the case. A full-term pregnancy is 40 weeks, or 280 days. Depending on what months you are pregnant during (some are shorter and some longer) and what week you deliver, you could be pregnant for either nine months or 10 months. This is completely normal and healthy.
This is completely normal and healthy.
Once you get close to the end of your pregnancy, there are several category names you might hear regarding when you go into labor. These labels divide up the last few weeks of pregnancy. They’re also used to look out for certain complications in newborns. Babies that are born in the early term period or before may have a higher risk of breathing, hearing or learning issues than babies born a few weeks later in the full term time frame. When you’re looking at these labels, it’s important to know how they’re written. You may see the week first (38) and then you’ll see two numbers separated by a slash mark (6/7). This stands for how many days you currently are in the gestational week. So, if you see 38 6/7, it means that you are on day 6 of your 38th week.
The last few weeks of pregnancy are divided into the following groups:
- Early term: 37 0/7 weeks through 38 6/7 weeks.
- Full term: 39 0/7 weeks through 40 6/7 weeks.

- Late term: 41 0/7 weeks through 41 6/7 weeks.
- Post term: 42 0/7 weeks and on.
Talk to your healthcare provider about any questions you may have about gestational age and due date.
Stages of Growth Month-by-Month in Pregnancy
First trimester
The first trimester will span from conception to 12 weeks. This is generally the first three months of pregnancy. During this trimester, the fertilized egg will change from a small grouping of cells to a fetus that is starting to have a baby’s features.
Month 1 (weeks 1 through 4)
As the fertilized egg grows, a water-tight sac forms around it, gradually filling with fluid. This is called the amniotic sac, and it helps cushion the growing embryo.
During this time, the placenta also develops. The placenta is a round, flat organ that transfers nutrients from the mother to the fetus, and transfers wastes from the fetus. Think of the placenta as a food source for the fetus throughout your pregnancy.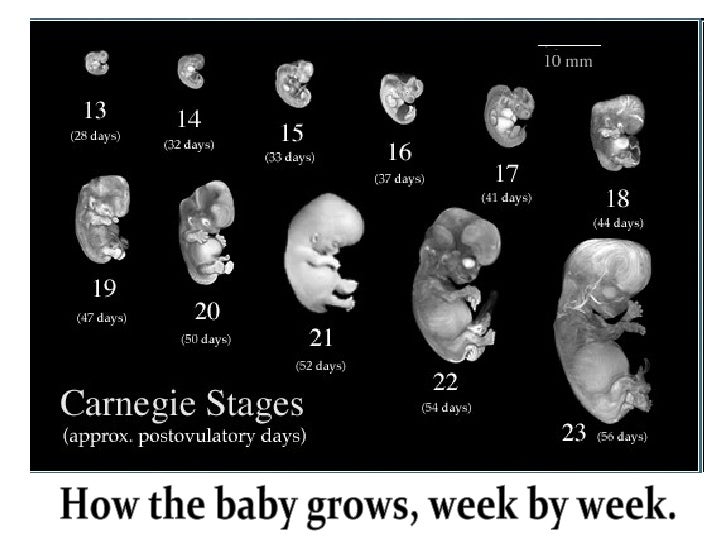
In these first few weeks, a primitive face will take form with large dark circles for eyes. The mouth, lower jaw and throat are developing. Blood cells are taking shape, and circulation will begin. The tiny "heart" tube will beat 65 times a minute by the end of the fourth week.
By the end of the first month, the fetus is about 1/4 inch long – smaller than a grain of rice.
Month 2 (weeks 5 through 8)
Facial features continue to develop. Each ear begins as a little fold of skin at the side of the head. Tiny buds that eventually grow into arms and legs are forming. Fingers, toes and eyes are also forming.
The neural tube (brain, spinal cord and other neural tissue of the central nervous system) is well formed now. The digestive tract and sensory organs begin to develop too. Bone starts to replace cartilage.
The head is large in proportion to the rest of the body at this point. At about 6 weeks, a heartbeat can usually be detected.
After the 8th week, healthcare providers refer to it as a fetus instead of an embryo.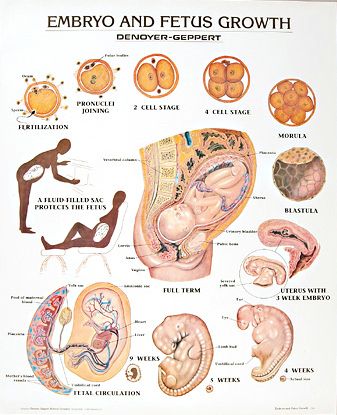
By the end of the second month, the fetus is about 1 inch long and weighs about 1/30 of an ounce.
Month 3 (weeks 9 through 12)
The arms, hands, fingers, feet and toes are fully formed. At this stage, the fetus is starting to explore a bit by doing things like opening and closing its fists and mouth. Fingernails and toenails are beginning to develop and the external ears are formed. The beginnings of teeth are forming under the gums. The reproductive organs also develop, but sex is still difficult to distinguish on ultrasound.
By the end of the third month, the fetus is fully formed. All the organs and limbs (extremities) are present and will continue to develop in order to become functional. The circulatory and urinary systems are also working and the liver produces bile.
At the end of the third month, the fetus is about 4 inches long and weighs about 1 ounce.
Since the most critical development has taken place, your chance of miscarriage drops considerably after three months.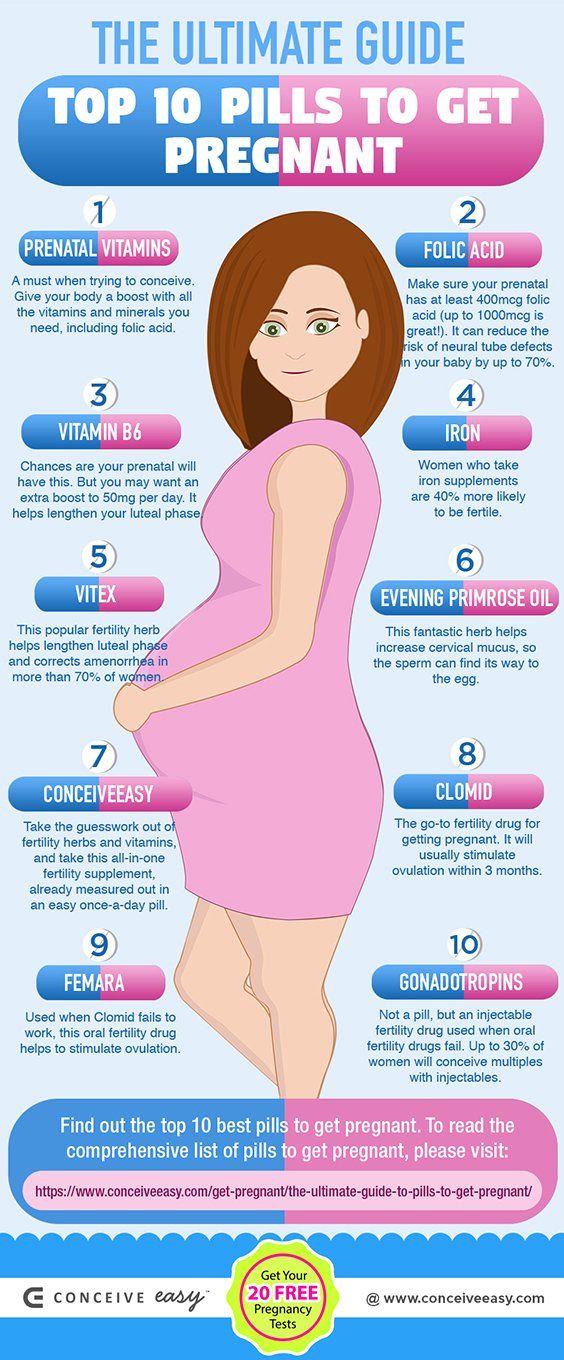
Second trimester
This middle section of pregnancy is often thought of as the best part of the experience. By this time, any morning sickness is probably gone and the discomfort of early pregnancy has faded. The fetus will start to develop facial features during this month. You may also start to feel movement as the fetus flips and turns in the uterus. During this trimester, many people find out whether their baby will be designated male or female at birth. This is typically done during an anatomy scan (an ultrasound that checks physical development) around 20 weeks.
Month 4 (weeks 13 through 16)
The fetal heartbeat may now be audible through an instrument called a doppler. The fingers and toes are well-defined. Eyelids, eyebrows, eyelashes, nails and hair are formed. Teeth and bones become denser. The fetus can even suck his or her thumb, yawn, stretch and make faces.
The nervous system is starting to function. The reproductive organs and genitalia are now fully developed, and your doctor can see on ultrasound if the fetus will be designated male or female at birth.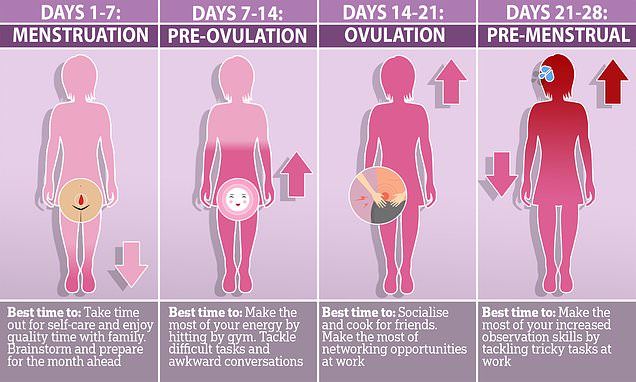
By the end of the fourth month, the fetus is about 6 inches long and weighs about 4 ounces.
Month 5 (weeks 17 through 20)
At this stage, you may begin to feel the fetus moving around. The fetus is developing muscles and exercising them. This first movement is called quickening and can feel like a flutter.
Hair begins to grow on the head. The shoulders, back and temples are covered by a soft fine hair called lanugo. This hair protects the fetus and is usually shed at the end of your baby's first week of life.
The skin is covered with a whitish coating called vernix caseosa. This "cheesy" substance is thought to protect fetal skin from the long exposure to the amniotic fluid. This coating is shed just before birth.
By the end of the fifth month, the fetus is about 10 inches long and weighs from 1/2 to 1 pound.
Month 6 (weeks 21 through 24)
If you could look inside the uterus right now, you would see that the fetus's skin is reddish in color, wrinkled and veins are visible through translucent skin. The finger and toe prints are visible. In this stage, the eyelids begin to part and the eyes open.
The finger and toe prints are visible. In this stage, the eyelids begin to part and the eyes open.
The fetus responds to sounds by moving or increasing the pulse. You may notice jerking motions if the fetus hiccups.
If born prematurely, your baby may survive after the 23rd week with intensive care.
By the end of the sixth month, the fetus is about 12 inches long and weighs about 2 pounds.
Month 7 (weeks 25 through 28)
The fetus continues to mature and develop reserves of body fat. At this point, hearing is fully developed. The fetus changes position frequently and responds to stimuli, including sound, pain and light. The amniotic fluid begins to diminish.
If born prematurely, your baby would be likely to survive after the seventh month.
At the end of the seventh month, the fetus is about 14 inches long and weighs from 2 to 4 pounds.
Third trimester
This is the final part of your pregnancy. You may be tempted to start the countdown till your due date and hope that it would come early, but each week of this final stage of development helps the fetus prepare for birth.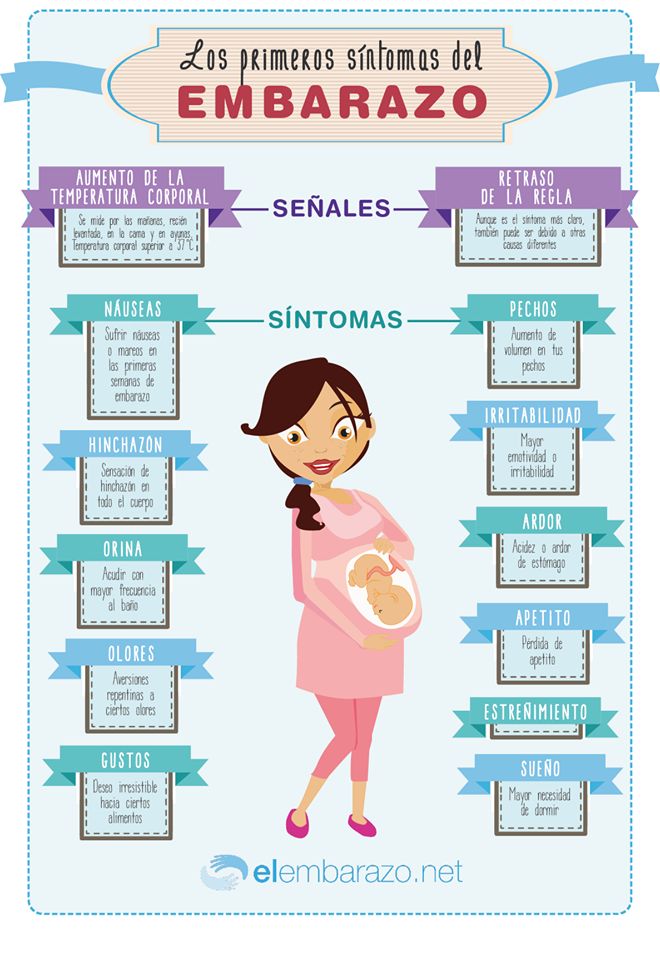 Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Remember, even though popular culture only mentions nine months of pregnancy, you may actually be pregnant for 10 months. The typical, full-term pregnancy is 40 weeks, which can take you into a tenth month. It’s also possible that you can go past your due date by a week or two (41 or 42 weeks). Your healthcare provider will monitor you closely as you approach your due date. If you pass your due date, and don’t go into spontaneous labor, your provider may induce you. This means that medications will be used to make you go into labor and have the baby. Make sure to talk to your healthcare provider during this trimester about your birth plan.
Month 8 (weeks 29 through 32)
The fetus continues to mature and develop reserves of body fat. You may notice more kicking. The brain developing rapidly at this time, and the fetus can see and hear. Most internal systems are well developed, but the lungs may still be immature.
The fetus is about 18 inches long and weighs as much as 5 pounds.
Month 9 (weeks 33 through 36)
During this stage, the fetus continues to grow and mature. The lungs are close to being fully developed at this point.
The fetus has coordinated reflexes and can blink, close the eyes, turn the head, grasp firmly, and respond to sounds, light and touch.
The fetus is about 17 to 19 inches long and weighs from 5 ½ pounds to 6 ½ pounds.
Month 10 (Weeks 37 through 40)
In this final month, you could go into labor at any time. You may notice that less movement because space is tight. At this point, The fetus's position may have changed to prepare for birth. Ideally, it's head down in your uterus. You may feel very uncomfortable in this final stretch of time as the fetus drops down into your pelvis and prepares for birth.
Your baby is ready to meet the world at this point. They are about 18 to 20 inches long and weigh about 7 pounds.
Pregnancy - week by week
The unborn baby spends around 38 weeks in the womb, but the average length of pregnancy (gestation) is counted as 40 weeks. This is because pregnancy is counted from the first day of the woman’s last period, not the date of conception, which generally occurs two weeks later.
Pregnancy is divided into three trimesters:
- First trimester – conception to 12 weeks
- Second trimester – 12 to 24 weeks
- Third trimester – 24 to 40 weeks.
Conception
The moment of conception is when the woman’s ovum (egg) is fertilised by the man’s sperm. The gender and inherited characteristics are decided in that instant.
Week 1
This first week is actually your menstrual period. Because your expected birth date (EDD or EDB) is calculated from the first day of your last period, this week counts as part of your 40-week pregnancy, even though your baby hasn’t been conceived yet.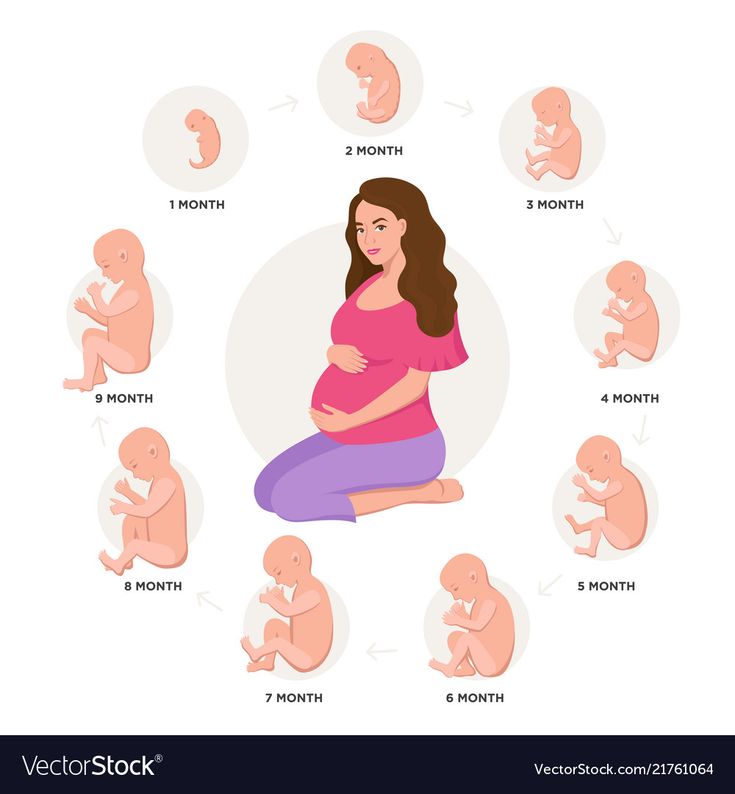
Week 2
Fertilisation of your egg by the sperm will take place near the end of this week.
Week 3
Thirty hours after conception, the cell splits into two. Three days later, the cell (zygote) has divided into 16 cells. After two more days, the zygote has migrated from the fallopian tube to the uterus (womb). Seven days after conception, the zygote burrows itself into the plump uterine lining (endometrium). The zygote is now known as a blastocyst.
Week 4
The developing baby is tinier than a grain of rice. The rapidly dividing cells are in the process of forming the various body systems, including the digestive system.
Week 5
The evolving neural tube will eventually become the central nervous system (brain and spinal cord).
Week 6
The baby is now known as an embryo. It is around 3 mm in length. By this stage, it is secreting special hormones that prevent the mother from having a menstrual period.
It is around 3 mm in length. By this stage, it is secreting special hormones that prevent the mother from having a menstrual period.
Week 7
The heart is beating. The embryo has developed its placenta and amniotic sac. The placenta is burrowing into the uterine wall to access oxygen and nutrients from the mother’s bloodstream.
Week 8
The embryo is now around 1.3 cm in length. The rapidly growing spinal cord looks like a tail. The head is disproportionately large.
Week 9
The eyes, mouth and tongue are forming. The tiny muscles allow the embryo to start moving about. Blood cells are being made by the embryo’s liver.
Week 10
The embryo is now known as a fetus and is about 2.5 cm in length. All of the bodily organs are formed. The hands and feet, which previously looked like nubs or paddles, are now evolving fingers and toes. The brain is active and has brain waves.
The brain is active and has brain waves.
Week 11
Teeth are budding inside the gums. The tiny heart is developing further.
Week 12
The fingers and toes are recognisable, but still stuck together with webs of skin. The first trimester combined screening test (maternal blood test + ultrasound of baby) can be done around this time. This test checks for trisomy 18 (Edward syndrome) and trisomy 21 (Down syndrome).
Week 13
The fetus can swim about quite vigorously. It is now more than 7 cm in length.
Week 14
The eyelids are fused over the fully developed eyes. The baby can now mutely cry, since it has vocal cords. It may even start sucking its thumb. The fingers and toes are growing nails.
Week 16
The fetus is around 14 cm in length. Eyelashes and eyebrows have appeared, and the tongue has tastebuds. The second trimester maternal serum screening will be offered at this time if the first trimester test was not done (see week 12).
The second trimester maternal serum screening will be offered at this time if the first trimester test was not done (see week 12).
Week 18-20
An ultrasound will be offered. This fetal morphology scan is to check for structural abnormalities, position of placenta and multiple pregnancies. Interestingly, hiccoughs in the fetus can often be observed.
Week 20
The fetus is around 21 cm in length. The ears are fully functioning and can hear muffled sounds from the outside world. The fingertips have prints. The genitals can now be distinguished with an ultrasound scan.
Week 24
The fetus is around 33 cm in length. The fused eyelids now separate into upper and lower lids, enabling the baby to open and shut its eyes. The skin is covered in fine hair (lanugo) and protected by a layer of waxy secretion (vernix). The baby makes breathing movements with its lungs.
Week 28
Your baby now weighs about 1 kg (1,000 g) or 2 lb 2oz (two pounds, two ounces) and measures about 25 cm (10 inches) from crown to rump. The crown-to-toe length is around 37 cm. The growing body has caught up with the large head and the baby now seems more in proportion.
Week 32
The baby spends most of its time asleep. Its movements are strong and coordinated. It has probably assumed the ‘head down’ position by now, in preparation for birth.
Week 36
The baby is around 46 cm in length. It has probably nestled its head into its mother’s pelvis, ready for birth. If it is born now, its chances for survival are excellent. Development of the lungs is rapid over the next few weeks.
Week 40
The baby is around 51 cm in length and ready to be born. It is unknown exactly what causes the onset of labour. It is most likely a combination of physical, hormonal and emotional factors between the mother and baby.
Where to get help
- Your doctor
- Obstetrician
- Midwife
Things to remember
- Pregnancy is counted as 40 weeks, starting from the first day of the mother’s last menstrual period. Your estimated date to birth is only to give you a guide. Babies come when they are ready and you need to be patient.
- The gender and inherited characteristics of the baby are decided at the moment of conception.
Pregravid preparation
Sign up for a consultation on pregravid preparation
The concept of the term "pregravid preparation"
The term "pregravid preparation" is heard by women for the first time, having visited a consultation with a gynecologist about a future pregnancy. At first, it causes a double feeling: on the one hand, it frightens a woman, and on the other hand, it inspires hope that she will be able to give birth to a healthy child.
The word "pregravid" comes from lat. Gravida (pregnant) and prefixes (before something). And pregravid preparation is the scrupulous preparation for a successful pregnancy.
And pregravid preparation is the scrupulous preparation for a successful pregnancy.
The question of preconception preparation arises among couples with a responsible approach to the birth of common children, as well as among women who can no longer become a mother on their own. In most cases, infections, hormonal disorders, and previously terminated pregnancies prevent pregnancy. And this is not strange, because by the age of 27-30, women often become owners of many diseases that are sexually transmitted or various physiological pathologies after an abortion.
Important to know! Pregnancy planning is not only for women, but also for men. They can also be carriers of infections or genetic diseases. In addition, it is men who create the optimal psychological and social atmosphere for a successful pregnancy.
Preconception milestones
Most couples think that pregnancy planning is about taking vitamins and quitting smoking 1-2 months in advance. This is only appropriate for young and completely healthy spouses. Pregravid preparation for the desired pregnancy begins 6-10 months before the "work" on the pregnancy. This is a troublesome process with a certain list of procedures. It is possible that this will take a lot of effort and finances, but you will expect the birth of a baby with confidence and a clear conscience.
This is only appropriate for young and completely healthy spouses. Pregravid preparation for the desired pregnancy begins 6-10 months before the "work" on the pregnancy. This is a troublesome process with a certain list of procedures. It is possible that this will take a lot of effort and finances, but you will expect the birth of a baby with confidence and a clear conscience.
It is indicated in the following cases:
- spontaneous miscarriage;
- missed previous pregnancy;
- fetal malformations in the past;
- history of surgery and abortion;
- chronic diseases.
Preconception preparation for pregnancy takes place in several stages:
- Medical examination of spouses: collection of anamnesis of diseases in the past, passing the necessary tests and diagnostic procedures, consultations of a number of specialists.
- Preparing a couple for conception and a woman for carrying a pregnancy.
- Calculation of favorable days for conception.
Comprehensive examination of a married couple
So that the stages of preconception preparation do not frighten you, let's study them in more detail and find out what exactly the preconception examination includes. To begin with, the therapist will examine the couple and determine which tests will need to be passed. Then the woman will go for further examination to the gynecologist, and the man to the andrologist.
General examination of the couple
- Family doctor examination.
- Collection of general analyzes (blood/urine) and blood for biochemistry.
- Diagnosis of chronic diseases and consultation with specialists (endocrinologist, pulmonologist, cardiologist, dentist, etc.).
- Identification of the blood group for the prevention of Rh conflict in a pregnant woman and her baby after birth.
- Pregravid preparation of the endometrium. It is carried out with chronic endometritis or with endometrial hypoplasia.

- Testing for HIV, syphilis, hepatitis.
- Test for torch infection.
- Consultation at the genetic center.
This is done at the request of future parents. But there are cases when the help of a geneticist is simply necessary:
- a woman is over 35 years old, a man is over 50 years old;
- stillbirth or anomalies in the development of the embryo in the past;
- genetic diseases in the family;
- blood ties between spouses.
Interesting! Examination for infections includes: a smear from the cervical canal and vagina in women, as well as from the urethra in men, for further microscopic and PCR diagnostics. This method determines the presence of mycoplasma, ureaplasma, chlamydia, gonococcal infection and sexually transmitted diseases.
Examination of a man by an andrologist
The stages of preconception preparation are obligatory for a man, even if he feels completely healthy.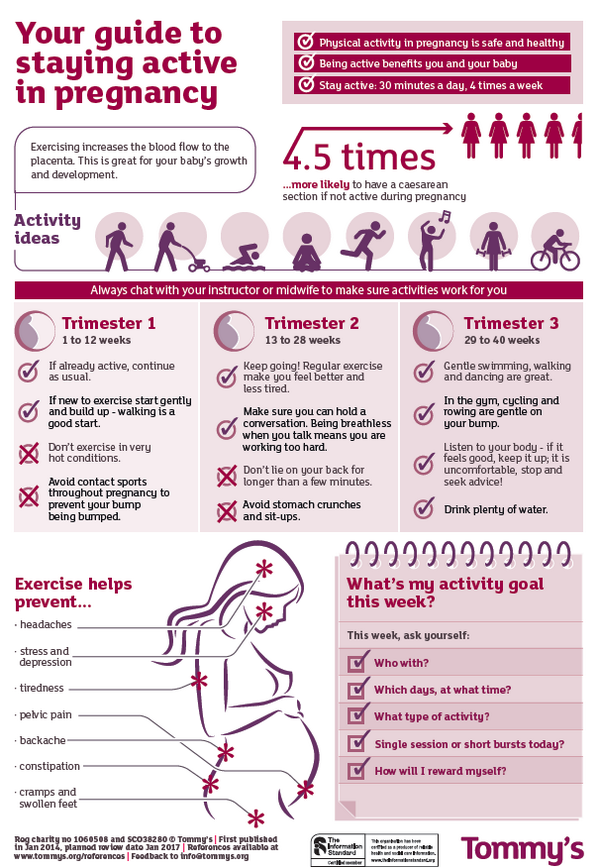 In addition to the procedures listed above, men are recommended to take a spermogram to assess the activity and quality of spermatozoa. Reproductive health is strongly affected by stress, smoking, alcohol and a sedentary lifestyle. If the examination is carried out for "infertility", the hormonal status is also determined.
In addition to the procedures listed above, men are recommended to take a spermogram to assess the activity and quality of spermatozoa. Reproductive health is strongly affected by stress, smoking, alcohol and a sedentary lifestyle. If the examination is carried out for "infertility", the hormonal status is also determined.
Did you know...
The body temperature in the scrotum is slightly lower than in the rest of the body, so sauna and heated seat lovers run the risk of significantly degrading the quality of the genetic material.
Examination in women
It is not surprising that the preconception preparation of women is more thorough and longer. After all, the period of gestation and birth depends on the state of health of the mother.
In addition, a number of examinations are carried out for the woman:
- Complete gynecological examination, including colposcopy and taking smears for the presence of atypical cells.
- Bridle of internal organs to exclude neoplasms, endometriosis, malformations of the uterus
- Examination of the hormonal panel, if there are signs of disorders: irregular cycle, excessive hair growth, acne.
- Coagulogram - blood clotting test.
- Comprehensive examination of the thyroid gland under the supervision of an endocrinologist: T4 homones, TSH and ultrasound diagnostics. The latent form of hypothyroidism can cause spontaneous miscarriage or mental retardation in a child (cretinism).
- Histological examination of fluid from the uterine cavity, if chronic inflammation of unexplained etiology is present.
- Diagnosis of autoimmune disorders.
And what does the statistics say?
85% of couples conceive within 6-24 months. And this is considered the norm. If after a couple of years the result has not appeared, it is worth looking for the cause.
What to do before conception and pregnancy
When the test results are ready, the couple is allowed to conceive if everything is in good health. In case of any deviations, the doctor prescribes an individual treatment algorithm (drug, surgical, complex). Treatment delays pregnancy by 3-6 months, depending on the complexity of the disease.
Treatment delays pregnancy by 3-6 months, depending on the complexity of the disease.
At the stage of preparing a couple for conception and a woman for carrying a pregnancy, the following recommendations are given:
- Refusal of alcohol and cigarettes.
- Active lifestyle.
- Folic acid 400 mcg for the woman and vitamin E for both partners.
- Calm atmosphere and no stress.
- Prevention of ODS and influenza.
- Optimistic mood.
- A balanced diet with enough vegetables and fats.
- Taboo on products with preservatives, dyes and all kinds of dietary supplements.
Determine the possible days of conception
Endless tests and visits to doctors are over. The diet and the correct mode of the day are ideal. There is very little left - to help our body cope with the task as soon as possible. To do this, you just need to determine when ovulation occurs in order to catch on at the right time and in the right place.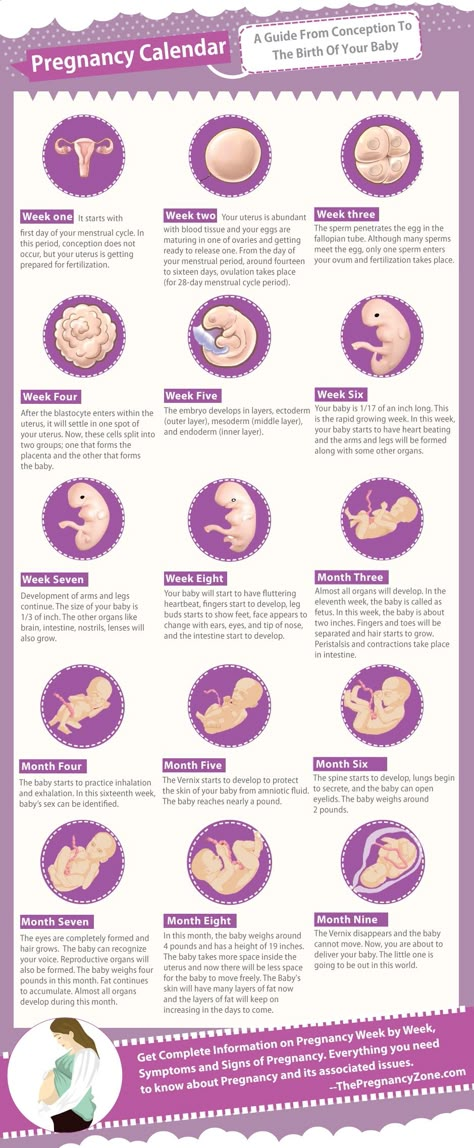
Ovulation is a favorable moment for conception. During this period, a mature egg leaves the ovary and goes into the fallopian tube. Ovulation occurs approximately on the 12th-14th day of the cycle, if it is, of course, regular. In women under 30 years old, there are about 8-10 ovulatory cycles per year. Then their number gradually fades away.
Every woman has many methods in her arsenal to solve this problem. Each has its own advantages and disadvantages, but there are plenty to choose from:
- Determination of ovulation by the nature of cervical mucus.
- Basal temperature measurement.
- Calendar method.
- Ovulation tests.
- Ultrasound monitoring.
Determination of ovulation by the nature of the cervical mucus
Normal discharge should not occur after menstruation. As the egg travels down the fallopian tube, the woman may notice some moisture as the cervical mucus thins. At the time of ovulation, it begins to stretch like an egg white.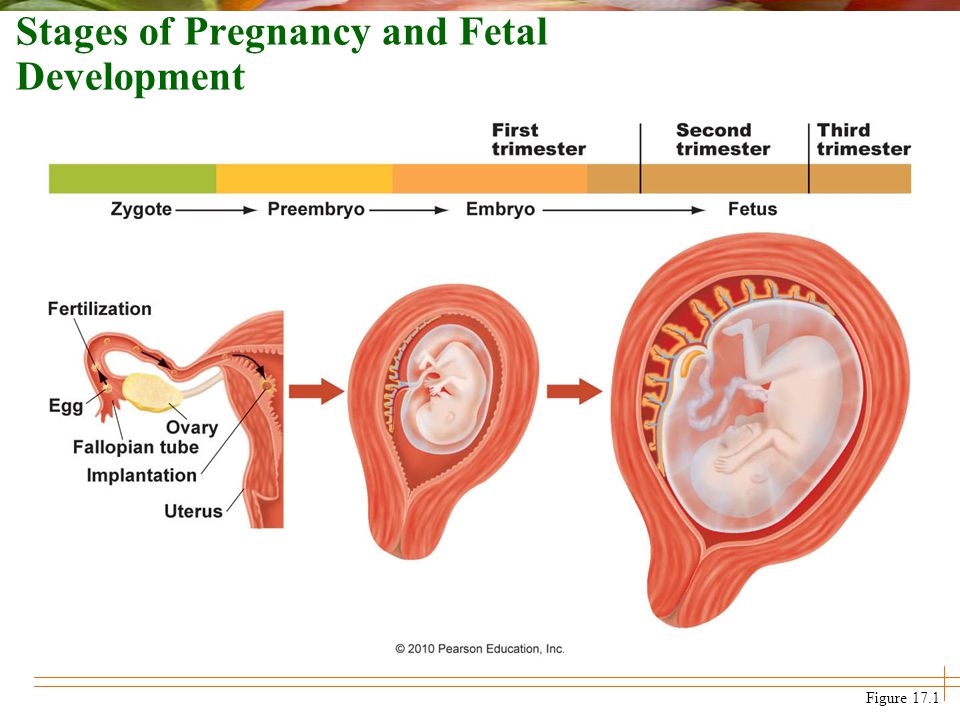
Advantages of this method:
- it does not require time and money
- it is safe and easy
Cons
- does not give 100% certainty, therefore it is not suitable for preventing pregnancy
- gives a false picture in inflammatory processes
Basal temperature measurement
Basal or rectal temperature should be measured strictly in the morning after waking up. This method is quite accurate only in combination with ultrasound. The temperature is kept within 35-36⁰С, and during the period of ovulation there is a sharp jump to 37⁰С. These figures are relative and each woman may be different.
Pros:
- allows you to objectively assess the picture of the phases of the menstrual cycle
- suggest a possible day of ovulation
- suspect anovulatory cycle
- determine pregnancy in the first week of conception
Cons:
- laborious process
- daily monitoring
- the presence of many factors that affect basal temperature (stress, poor sleep, alcohol)
Tip! To measure temperature, it is better to use an electronic thermometer - it is safer and faster.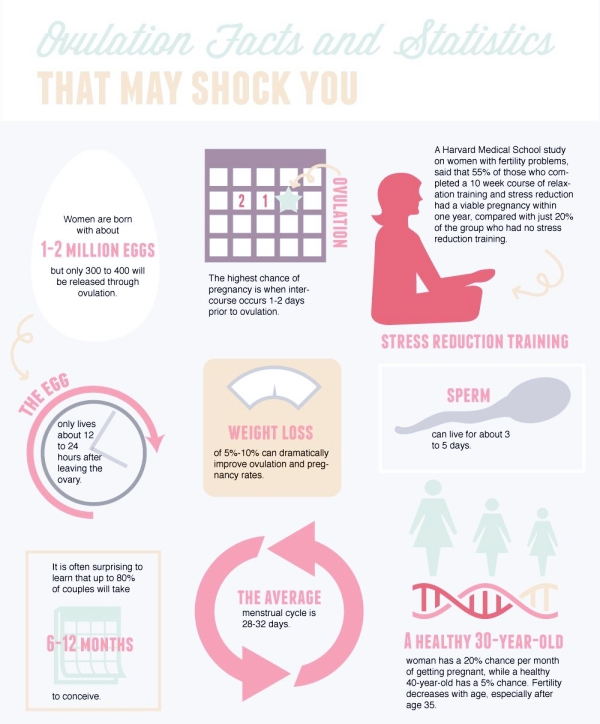
Calendar method (Claus-Ogino method)
This method was developed back in 1876 by Dr. Maria Putnam. It is suitable only for women with a regular 26-32 day cycle. The fertile (favorable) period is indicated from the 10th to the 17th day of the cycle.
Pros:
- low cost and availability
- ease of use
Cons:
- relative accuracy
- you can miss early ovulation due to hormonal failure
Ovulation Tests
Ovulation Tests are quite accurate. They are inexpensive and are sold in every pharmacy. It takes 5 minutes to get the result. As a rule, you need five test strips per month to monitor ovulation. Their principle of action is the same as that of pregnancy tests, only in this case the luteinizing hormone is determined.
These tests are very easy to use. For example, you have a 28-day cycle: 28-17=11. This means that testing should be carried out from the 11th day of the cycle.
Pros:
- minimal time investment
- 99% confidence
- safety and ease of use
Cons:
- additional financial costs.
Ultrasound monitoring
This is the most accurate way to confirm ovulation. Ultrasound control is carried out 3-5 times in the first half of the cycle to measure the size of the follicles - folliculometry. And after the rupture of the dominant follicle - to determine the ovulatory fluid and corpus luteum, which confirms ovulation.
Pros:
- the ability to predict ovulation with an accuracy of 6-12 hours
- confirm that the follicle has ovulated.
Cons:
- expensive
- you need to visit the diagnostic center several times
- waste of time.
Successful completion of preconception preparation
Preconception preparation is considered successful if you hold a positive pregnancy test in your hands.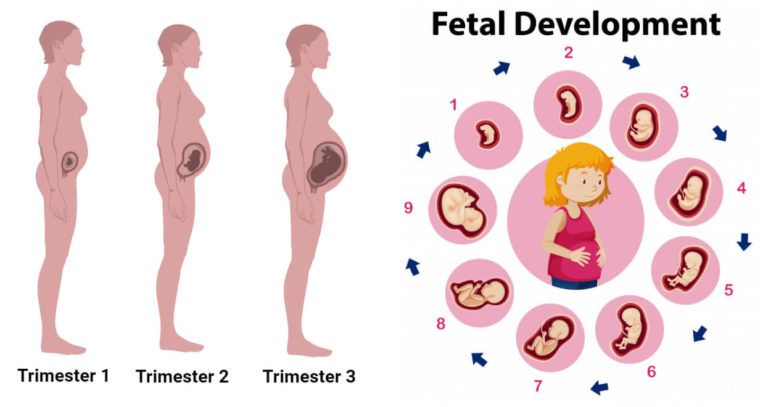 Now it remains to bring everything to its logical conclusion. The final stage is early confirmation of pregnancy, screening tests, biochemical diagnostics and ultrasound monitoring. This will help to save the long-awaited pregnancy and give birth to a wonderful baby.
Now it remains to bring everything to its logical conclusion. The final stage is early confirmation of pregnancy, screening tests, biochemical diagnostics and ultrasound monitoring. This will help to save the long-awaited pregnancy and give birth to a wonderful baby.
Sign up for a consultation on preconception preparation
Pregnancy and drugs / Obstetrics and gynecology, reproductive medicine / Articles about health / Articles and encyclopedia / madez.ru
We have been actively planning for a baby for a long time, but we never think about the dangers of drugs during pregnancy!
Gynecologist, gynecologist endocrinologist Popova Natalya Vladimirovna will tell you which medicines can be taken during pregnancy, and which are categorically not recommended.
One of the most important periods in a woman's life is the period of bearing a child. And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby.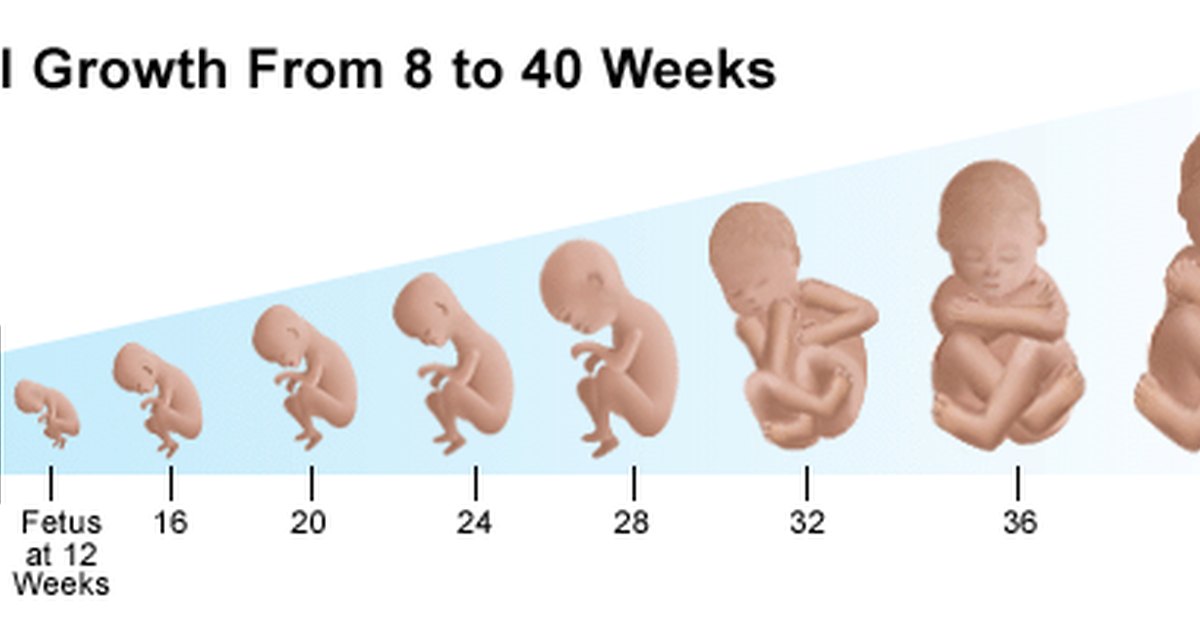 But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
If it is necessary to use any drug during pregnancy, the mother-to-be should remember:
- Any drug during pregnancy (at any stage) can be used only in accordance with the indications and only as prescribed by the attending physician;
- When choosing a medicinal product, preference should be given only to those medicinal products that have proven efficacy;
- Prefer monotherapy, i.e. treatment with only one drug if possible; combined treatment during this period is undesirable;
- Topical treatment is more desirable than systemic (oral, intravenous, intramuscular) administration of the drug.
- A pregnant woman should remember that completely safe and absolutely harmless drugs do not exist.
The most dangerous period for the use of any drugs, both of chemical and natural origin, is the first trimester of pregnancy (the first 12 gestational weeks), when all organs and systems are laid in the fetus, which will only develop and form the placenta in the future. It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
Pronounced mutagenic hazard:
1. in industry - asbestos, acetaldehyde, vinyl chloride, dimethyl sulfate; factors of metallurgical and rubber industries;
Metals: copper, nickel, lead, zinc, cadmium, mercury, chromium, arsenic, styrene, formaldehyde, chloroprene, epichlorohydrin, ethylene oxide.
2. agriculture - a mixture of defoliants, pesticides, insectiosides, repellents, fungicides, pesticides, methylpartion, phthalaphos, chlorophos, gardona, DDT, contan.
If you work in a hazardous industry and come into contact with these chemicals, from early pregnancy, switch to "light work".
Global trends in early pregnancy from the point of view of evidence-based medicine are unambiguous: the need for rational diet therapy , taking folic acid at least 400 mcg / day and potassium iodide 200 mg / day is recognized.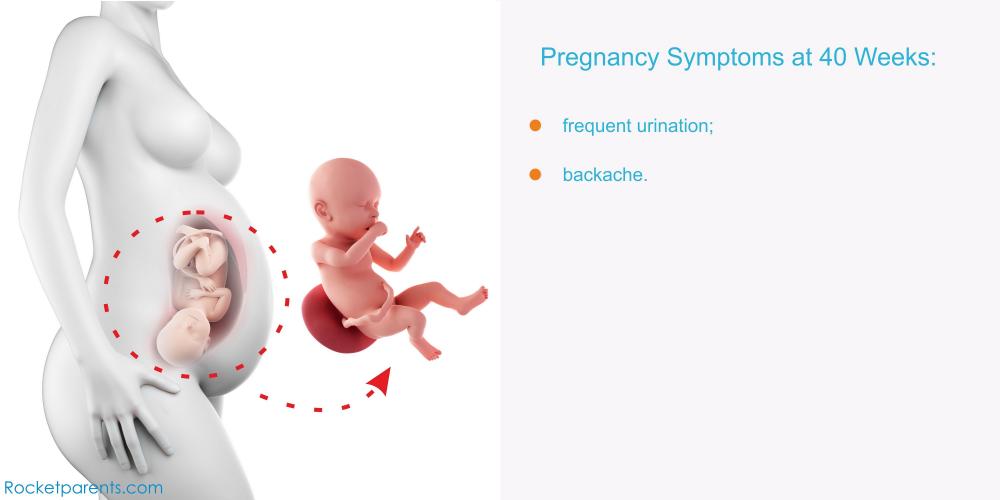
After 12-14 weeks of pregnancy, with an inadequate diet, the use of vitamin preparations during pregnancy and lactation is recommended as a way to improve the health of the mother and fetus . Vitamin complexes intended for other groups of the population (including children) are contraindicated for pregnant women!
Medicines during pregnancy
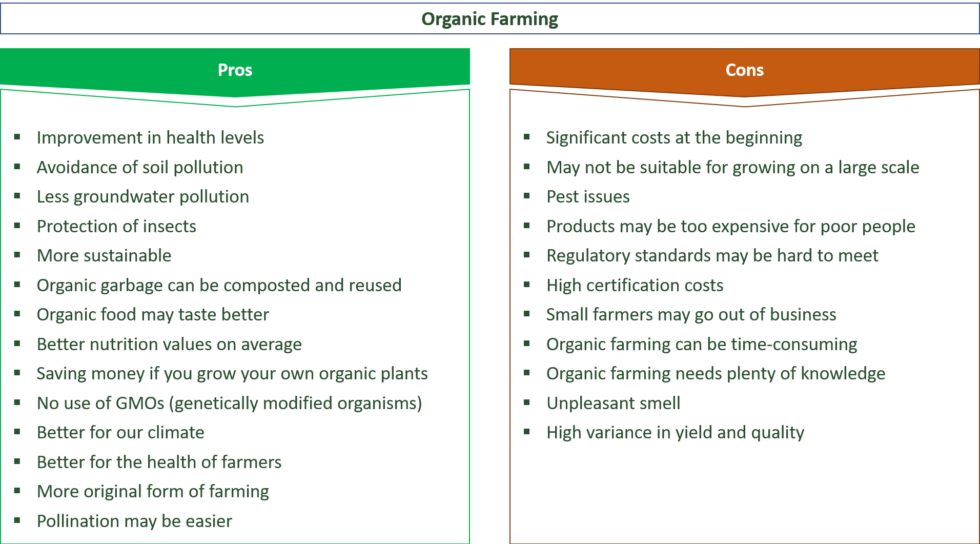
In existing classifications, it is customary to subdivide drugs during pregnancy into groups - safe, relatively safe, relatively unsafe and dangerous. Moreover, the list of drugs is periodically updated.
- Category A - safe drugs. Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate.

- Category B - relatively safe drugs. Experimental studies have generally not shown their teratogenic effects in animals and children whose mothers took such drugs. These are amoxicillin, heparin, insulin, aspirin, metronidazole (except first trimester)
- Category C - relatively unsafe drugs. When testing these drugs on animals, their teratogenic or embryotoxic effects were revealed. Controlled trials have not been conducted or the effect of the drug has not been studied (isoniazid, fluoroquinolones, gentamicin, antidepressants, antiparkinsonian drugs). These drugs should only be used if the potential benefit outweighs the potential risk.
- Caregory D - dangerous drugs. The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac).
- Category X - dangerous drugs that are contraindicated for use.
The teratogenic effect of drugs in this group has been proven, their use is contraindicated during pregnancy, as well as when planning a pregnancy.
Although nearly 1,000 chemicals are known to be teratogenic in animals, only a few chemicals have been proven to be permanently teratogenic in humans. These include a number of narcotic analgesics, chemotherapeutic drugs (antimetabolites, alkylating agents), anticonvulsants (trimethadione, valproic acid, fenithione, carbamazepine), androgens, warfarin, danazol, lithium, retinoids, thalidomide.
The safest drugs
(Larimore W.L., Petrie K.A., 2000)
| Drug groups | The safest drugs |
| Analgesics | Paracetamol, narcotic analgesics (short courses), NSAIDs (except due date) |
| Antibiotics | Aminopenicillins, macrolides (Vilprafen), azithromycin, cephalosporins, clindamycin, erythromycin, metronidazole (except 1st trimester), penicillins, trimethoprim (except 1st trimester) |
| Antidepressants | Venlafaxine, fluoxetine, trazodone |
| Antidiarrheals | Loperamide |
| Antiemetics | Andacids, doxylamine, prochlorperazine, promethazine, vitamin B |
| Antihypertensives | B-blockers, hydralazine, methyldopa, prazosin |
| Antiparasitics | Permethrin |
| Antituberculous drugs | Ethambutol, isoniazid |
| Antivirals | Amantadine, acyclovir |
| Antihistamines | Cetirizine, loratadine |
| Anti-asthma/anti-allergy products | Epinephrine, inhaled bronchodilators, theophylline |
| Cardiovascular medicines | B-blockers, calcium channel blockers, digoxin, nitroglycerin |
| Constipation products | Bisacodyl, methylcellulose |
| Antidiabetics | Insulin |
| Gastrointestinal medicines | Sucralfate, metoclopramide |
| Thyroid hormones | Levothyroxine, liothyronine |
Terminals
It is very important that every pregnant woman remember that any drug during pregnancy can bring not only benefits, but also considerable harm, therefore, any self-administration during this period is not permissible, since their consequences are unpredictable and in many cases can cause irreparable harm to the developing fetus.