What to expect with a planned c section
Elective caesarean birth: what to expect
About elective caesarean birth
A caesarean section is an operation to give birth to your baby. A caesarean section is also called a caesarean, a c-section or a caesar.
Sometimes health problems or pregnancy complications mean that a caesarean birth is a safer option than vaginal birth.
You might have a planned or elective caesarean birth for medical reasons or because there are signs late in your pregnancy that you or your baby might have problems with a vaginal birth.
If you feel worried or there’s something you want to know about caesarean birth, talk with your doctor or midwife before you go to hospital. You can also let them know beforehand about any special preferences you have for the birth so they can try their best to support you.
Before you go to hospital: getting ready for your elective caesarean
A caesarean can be done only if you give your written permission. Before your hospital admission, your doctor will explain the benefits, risks and complications of your elective caesarean. Then you’ll need to sign a consent form.
You’ll need to fast before an elective caesarean birth. This usually means having no food or drink, including water, for 6 hours before the surgery. The length of fasting before surgery varies from hospital to hospital, so make sure to ask your hospital about their fasting requirements.
Most hospitals give you a list of what to bring, like clothing for yourself and your baby. Before you leave home it’s a good idea to check that you have everything you need.
You might like to ask your support person to bring a camera or phone, but remember to check with hospital staff that it’s OK to take photos or videos of your baby being born. You’ll also need permission to take photos of hospital staff or equipment.
In the maternity ward before your elective caesarean
At hospital, you’ll usually be admitted to the maternity ward. You might have to arrive at the hospital very early in the morning.
Being pregnant and having an operation can increase your risk of developing blood clots. To help prevent this, you’ll be given compression stockings to wear during the surgery.
The top few centimetres of your pubic hair and your lower tummy might be clipped. This is so the area is clean and clear for the cut. It might also make it less likely you’ll get an infection.
Before you have a caesarean section, medical staff will want to talk with you about whether you have any health problems, allergies, and bleeding or bruising problems and whether you take any medications.
Caesarean section surgery usually takes 30-60 minutes. But the entire process can take a few hours, from going to the operating theatre, preparing for surgery, having the surgery, and then returning to your room in the maternity ward.
In the operating theatre: anaesthetics and other preparations
You’ll be taken to an operating theatre for your elective caesarean. Your theatre team will prepare you for surgery, which can take some time.
Your theatre team will prepare you for surgery, which can take some time.
You’ll be prepared for your anaesthetic so that you don’t feel any pain during the surgery. A spinal anaesthetic is most common for planned caesarean births. An epidural is more likely to be used for an unplanned (emergency) caesarean birth.
With spinal anaesthetic and epidurals, you’re awake and can breathe normally.
You might have a general anaesthetic if you can’t have a spinal or epidural anaesthetic. You might also have a general anaesthetic if your baby needs to be born very quickly. In this case, you’ll be asleep during your baby’s birth.
You’ll have a small plastic tube inserted in the back of your hand or the crook of your elbow for your fluid drip.
Your tummy will be cleaned with antiseptic by the theatre team and covered with sterile cloths to lessen the chance of infection. A plastic tube (a catheter) will be put into your urethra (where urine comes out) to keep your bladder empty.
Operating theatres can be quite cold, so ask for some extra blankets if you feel cold.
It’s normal to feel anxious and sometimes teary as you go into surgery.
During preparation and surgery, you can probably have a support person with you, unless you need a general anaesthetic or there are serious medical problems. Your support person can sit next to you, hold your hand and be there to welcome your baby.
Your caesarean section operation
There’ll be many people in the operating theatre with you, including the obstetrician, an assistant surgeon, an anaesthetist, theatre nurses, a midwife and sometimes a paediatrician. Each person in the room has an important role in keeping you and your baby safe.
You’ll have a drape or curtain over your chest area so that you and your support person can’t see the surgery.
Once the anaesthetic is working properly, the doctor will make cuts in your tummy and your uterus. Both cuts will be about 10 cm long.
Your baby will be lifted out through the cuts. You might feel a tugging or pulling sensation, but there won’t be any pain. Sometimes the doctor might use forceps to help with lifting out your baby’s head. If everything is OK, you can ask the doctor to hold your baby up so you can get a first look.
The umbilical cord will be cut and your placenta removed. Then the doctors or midwives will check your baby very carefully.
Your doctor will recommend an injection or medicine through an intravenous drip to make your uterus contract and to reduce bleeding. You’ll be given antibiotics through your drip to reduce the risk of infection.
The doctor will stitch the layers of the uterus, muscle, fat and skin in your tummy back together and put a dressing over your wound.
Early skin-to-skin contact helps your baby to stay warm and feel secure. It also lets you and baby bond physically and helps with breastfeeding. If everything is OK with your baby, it’s good to have skin-to-skin contact as soon as possible. You should be able to have it in the operating theatre. If you can’t, your support person will probably be able to hold your baby instead.
You should be able to have it in the operating theatre. If you can’t, your support person will probably be able to hold your baby instead.
After your caesarean birth
Midwives and nurses will look after you in the recovery room until you’re ready to go back to the maternity ward. You’ll most likely have your baby stay with you. You can ask a midwife to go with you to the recovery room to help you breastfeed your baby. If the medical staff are worried about your health or your baby’s, this might not be possible at first.
After a general anaesthetic, the midwife or nurses will look after you in the recovery room until you wake up. Once you’re awake and stable you should be able to see your baby.
It’s normal to feel pain and discomfort after a caesarean, especially when you move. Let the midwives know how you’re feeling. It’s best to keep on top of pain, because this will help you recover faster.
The midwives will regularly check your blood pressure, your wound and how much vaginal bleeding you have. You’ll probably have a drip and a urinary catheter for the first 12-24 hours. After the first 12 hours, a midwife will help you get up so that you can shower.
You’ll probably have a drip and a urinary catheter for the first 12-24 hours. After the first 12 hours, a midwife will help you get up so that you can shower.
Getting up and moving around as soon as possible after the surgery will help reduce your risk of blood clots. And you might be asked to keep wearing compression stockings or be fitted with another compression device over your lower legs to reduce your risk. Some birthing mothers are also given daily injections of blood thinning medicine.
Breastfeeding after caesarean
Breastmilk is the best possible food to help your baby grow healthy and strong.
After a caesarean, starting to breastfeed can take a while. It’s a good idea to ask for support from midwives and a lactation consultant, if the hospital has one. The midwives can help you find the most comfortable ways to hold your baby while breastfeeding.
The sooner you start with breastfeeding, the easier it is for you and your baby. The hospital should help you breastfeed as soon as possible after birth. This is usually in the recovery room but sometimes you can do this in the operating theatre.
This is usually in the recovery room but sometimes you can do this in the operating theatre.
It’s good to ask for practical help, especially in the first 6 weeks after caesarean. For example, you can ask friends to help with housework or with driving your other children while you recover.
What to Expect from a (Planned) C-section
Submitted by Shannon Roberts, BSN, RN, RNC-OB on November 22, 2021
It's hard to prepare for something you didn't plan for at all.
A cesarean section (c-section) may not be the way you envisioned your birth, but this kind of birth-day is just as special. Knowing what to expect can help you shift your mindset and get ready for the big day.
What is a planned c-section?C-sections are pre-scheduled when a health care provider feels it's the best choice for both mom and baby. This is different than an urgent or emergency cesarean, which takes place after mom has gone into labor and complications necessitate the surgery. C-sections are most often planned because:
C-sections are most often planned because:
- Baby is breech (facing the wrong way)
- Mom is pregnant with multiples
- A previous cesarean or abdominal surgery determines the need for one
- There is a medical concern for either mom or baby
Other pregnancy or health complications may also require a scheduled c-section. Your OB/GYN can talk you through all of your options for your particular situation.
C-sections are considered major abdominal surgeries, but they are generally safe and somewhat common. Like other surgical procedures, risks can include infection at the surgical site, swelling, excessive bleeding and blood clots, among others. Risks to baby can include an accidental cut on the skin or breathing difficulties, which most often affects babies born before 39 weeks.
Women who have had a previous cesarean section are at a slightly higher risk for future pregnancy complications than those who have had a vaginal birth. However, most women go on to have healthy future pregnancies and many go on to have a vaginal births after their primary c-section--this is called a VBAC.
The best part about a scheduled c-section is the chance to get prepared. You'll want to pack your bags and ready your home accordingly for your return. Most planned c-sections are scheduled for around 39 weeks, but you'll still want to have a bag packed by 37 weeks--just in case you go into labor early on your own.
- Your hospital bag should include most of the regular essentials for mom and baby, but your homecoming outfit should be loose fitting, like a dress, so it will not irritate your incision.
- Many moms choose to pre-purchase a belly binder to aid in supporting their abdomen after surgery.
- It is beneficial to pack two separate bags, one small bag with all your necessities for pre-surgery, like your glasses, lip balm and a phone charger (it is recommended to leave all valuables at home). You can keep a separate bag full of postpartum items with a family member until after baby arrives.
- Before leaving home, consider also setting up a nursing/feeding station in a comfortable chair with a few must-haves in easy reach--including diapers, wipes, burp cloths, extra clothes, a water bottle, phone charger and healthy snacks.

- Stock up on loose-fitting clothes to wear for a few weeks after delivery.
- You'll also want to have pads and over-the-counter pain medication, like acetamenophen, on hand.
Pre-surgical instructions
Just like any surgery, your doctor's office will provide you with some ahead-of-time instructions to carefully follow to ensure a healthy delivery. They will likely include:
- Information on pre-surgical bloodwork. It is important to complete this at the required location, date and time.
- Instructions about eating and drinking. Typically moms are asked to discontinue food and liquids up to 12 hours before surgery. At our hospital, clear liquids are approved up to two hours before c-section.
- A special soap for use at home before your surgery. Chlorhexidine Gluconate (CHG) helps remove germs from your skin and thereby reduces the risk of infection. Be sure to follow the instructions on the label.
- Paperwork that includes surgery arrival time, as well as the the time of your c-section.
 Be sure to be on the Labor and Delivery Unit at your arrival time.
Be sure to be on the Labor and Delivery Unit at your arrival time.
To find out more about what will happen on the day of your c-section, check out: What a c-section entails.
Featured Image
Shannon Roberts, BSN, RN, RNC-OB, is the Director of Women's Services. She previously served as Unit Director on Chesapeake Regional Medical Center’s Labor & Delivery unit, where she worked for more than 20 years. She received her Bachelor of Science in Nursing degree at Old Dominion University in Norfolk and also is certified in inpatient obstetrics. She began her tenure at CRH as a candy striper at age 14.
Sign up for our newsletter
We're committed to your privacy. Chesapeake Regional uses the information you provide to contact you about content. You may unsubscribe from these communications at any time.
Planned caesarean section: what you need to know
On-demand caesarean section? Not necessary. Elective caesarean section is primarily intended to make the operation of maternity hospitals more predictable and reliable, when it can be foreseen that natural childbirth is impossible or complicated.
Share this information
What to expect during a planned caesarean section
Few pregnant women want to think about the process of caesarean section, since most are set for a natural birth. However, the number of caesarean sections in the world increased by 20 percent from 2006 to 2017. One of the reasons for this is the increase in the number of elective caesarean sections, which are performed as a precautionary measure to avoid emergency caesarean sections and complications during childbirth. We answer the most frequently asked questions about "caesarean section at will" and medically necessary birth interventions.
If I want to have a caesarean, can I decide whether to have a baby naturally or by caesarean?
First of all: Elective caesarean section is not the same as voluntary caesarean section, which is also a misleading term. Every mother can decide for herself which birth she needs. However, you should discuss the pros and cons of natural birth, vaginal delivery, and caesarean section with your doctor or midwife.
However, you should discuss the pros and cons of natural birth, vaginal delivery, and caesarean section with your doctor or midwife.
It is important to remember that there are strong indications for a planned caesarean section. If there is a foreseeable risk to the mother or baby during childbirth, the gynecologist will advise a caesarean section by prior arrangement. For example, if the placenta overlaps the cervix - the so-called placenta praevia - a planned caesarean section will avoid damage to the placenta and life-threatening bleeding.
How is the preparation for a caesarean section carried out?
During your birth planning consultation at the clinic, you will talk to your attending physicians about preparing for a planned caesarean section. Since the consultation is usually done well in advance, there is still a lot that can happen before delivery. If your gynecologist recommends that you have a caesarean section, he or she will make a note in the referral to hospital for a consultation.
This appointment will have ultrasound to reassess the size and weight of the baby , the cervix was examined and CTG was done . If a caesarean section is to be performed due to a transverse or breech presentation, then at the 37th or 38th week of pregnancy, a recheck will likely be performed to see if the position of the baby in the womb has changed. An elective caesarean section does not have to remain an elective one: if a mother decides to have a normal birth after her baby turns in the womb again, the decision can be changed.
How is a planned caesarean section performed?
Together with your doctor, you will decide whether you need general anesthesia or regional (local) anesthesia for your operation. Regional anesthesia for caesarean section has the advantage that after caesarean section you can immediately take the baby in your arms and breastfeed.
Once the anesthesia has worn off, the bladder catheter is inserted and the operation begins. Doctors usually open the abdominal wall using the Misgava-Ladakh method. The top layer of the skin is cut off and the deeper layers of tissue are carefully opened by hand, which ensures a slight loss of blood. The baby is then removed from the uterus, and the wound on the uterus and abdominal tissues is carefully closed.
Doctors usually open the abdominal wall using the Misgava-Ladakh method. The top layer of the skin is cut off and the deeper layers of tissue are carefully opened by hand, which ensures a slight loss of blood. The baby is then removed from the uterus, and the wound on the uterus and abdominal tissues is carefully closed.
When is the right time for a planned caesarean section at what time?
The timing of the caesarean section affects the outcome for the baby, as does the timing of a natural birth. "People are now trying to have caesarean section as close as possible to the estimated due date of , that is, from the end of the 39th week of gestation," explains Prof. MD Dimpfl. At this stage, the development of the child is completed, and he is ready to be born - by caesarean section or by natural means. If there is no medical reason for an earlier delivery, your doctor will advise you to have a planned caesarean section from the beginning of the 40th week.
Elective caesarean section - Raduga Family Birth Center
Preparation:
Any birth is a journey of your body, mind and spirit to meet your baby.
Preparation includes all these aspects that will help you to go through any childbirth as smoothly and comfortably as possible, as well as significantly reduce the number of complications in the postpartum period, during the period of breastfeeding, as well as during the recovery period after childbirth.
Main recommendations during the period of preparation for surgery:
First of all, before the operation, just like before childbirth, you should have a good rest, quality sleep and proper rest are important. Putting various pillows under your arms, legs, stomach and neck helps to significantly improve the quality of sleep in order to relax the body well. To sleep well: it is useful to drink several glasses of clean water in the morning to avoid dehydration by the evening; a walk in the park or in the forest before going to bed helps; fresh cool air in the bedroom. All this will help to create good external conditions for recreation.
All this will help to create good external conditions for recreation.
Secondly, any internal tension and excitement increase physical discomfort and tension in the body. Use relaxation techniques to help yourself: reading, warm bath, watching a good movie, talking with loved ones, practicing self-hypnosis, breathing techniques/breathing, aromatherapy, visualization/guided meditation, music, self-massage of the head, arms, legs and shoulders, massage and light stretching of the muscles of the body, support for loved ones, relatives and friends, spiritual practices, prayer, etc.
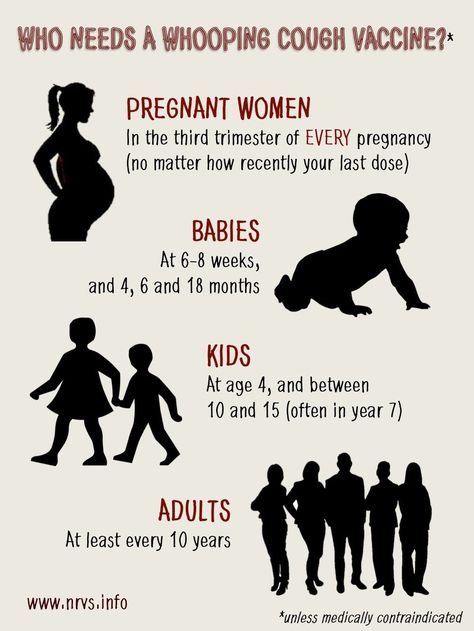
Third, it is important to discuss any fears with people you trust. When knowledge and understanding of the experience coming to you comes, fear dissolves and leaves. Your midwife will tell you in detail what will happen and how, the obstetrician-gynecologist will prescribe medications and laboratory diagnostics necessary before the operation (usually a clinical blood test for hemoglobin and platelet levels). You may be advised to purchase compression stockings to prevent blood clots. The anesthesiologist will discuss with you the type of anesthesia and the necessary preparation for the operation. You can discuss all the details of the operation with the doctors and midwife and ask all your questions so that everything becomes clear and understandable, this will psychologically add peace and joy to your child's birthday.
You may be advised to purchase compression stockings to prevent blood clots. The anesthesiologist will discuss with you the type of anesthesia and the necessary preparation for the operation. You can discuss all the details of the operation with the doctors and midwife and ask all your questions so that everything becomes clear and understandable, this will psychologically add peace and joy to your child's birthday.
Fourth, pay attention to the body, on the day of surgery in the morning, do not eat, you can drink a little, take a shower, it is recommended not to apply any cream and makeup on the skin, do not wear jewelry, except when it is very important for you. Do not wear lenses or glasses. Put on compression stockings. Bring music if you wish and a camera if you decide to take a photo.
You will be required to sign an informed consent form for medical intervention. The operation time may vary slightly, due to various unforeseen situations that may arise in the maternity hospital.
In the operating room, you will be introduced to all participants in the process, a team of doctors and nurses with whom you are not familiar, your data in the birth history will be checked again, a cuff for continuous monitoring of blood pressure will be installed, an venous catheter will be inserted to inject you with saline / fluid and drugs substances, if necessary, and will also place a urinary catheter to control urine output.
If you are having SEA (spinal epidural anesthesia):
First, they will be asked to take a position with a rounded back. There are two provisions. First: lying on your side, with your chin pressed and your knees pressed as much as possible. Second: sitting on the edge of the table, pressing the chin to the chest as much as possible, rounding the back and relaxing the shoulders. This is necessary to increase the maximum distance between the lumbar vertebrae, for a safer introduction of the catheter. You will need to remain still in this position until the anesthesiologist places the catheter. Therefore, if you need to move, sneeze, etc., it is very important to first warn the doctor loudly with your voice and try to remain still until he allows it. This is necessary for the safety of manipulations in the epidural space around the spine. The injection site will be treated with alcohol, then anesthetized by injecting an anesthetic through a syringe. Then, when the catheter insertion site becomes insensitive, the anesthetist will proceed to place the catheter. During this procedure, the mother usually feels only a touch of the skin, a slight pushing of the body, if the sensations are very unpleasant or painful, be sure to inform the doctor about this. After the introduction of anesthesia through the catheter, you will feel warmth in your legs, they may tingle slightly, these are normal sensations.
Therefore, if you need to move, sneeze, etc., it is very important to first warn the doctor loudly with your voice and try to remain still until he allows it. This is necessary for the safety of manipulations in the epidural space around the spine. The injection site will be treated with alcohol, then anesthetized by injecting an anesthetic through a syringe. Then, when the catheter insertion site becomes insensitive, the anesthetist will proceed to place the catheter. During this procedure, the mother usually feels only a touch of the skin, a slight pushing of the body, if the sensations are very unpleasant or painful, be sure to inform the doctor about this. After the introduction of anesthesia through the catheter, you will feel warmth in your legs, they may tingle slightly, these are normal sensations.
Next you will be asked to lie on your back to free up your stomach area as much as possible, this may be unusual or not very comfortable, don't worry, these are standard sensations and will not last long.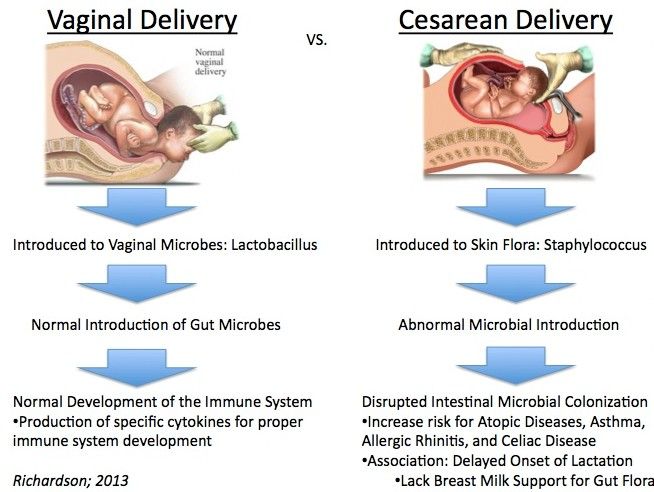
The doctors test the effect of the anesthesia again, then the abdomen is cleaned for the operation with a special solution, and you are covered with a special sterile sheet.
During the operation, you may feel nausea, tell your doctor about it, this is a common reaction to a decrease in pressure due to anesthesia. You may feel a little uncomfortable from having difficulty making a deep entry or coughing, this is a normal reaction as the anesthesia can affect the sensitivity of the chest ribs. Don't worry, the anesthesiologist monitors your breathing with the help of instruments. If you have any other discomfort, dizziness, etc. let the anesthetist know so they can help you feel more comfortable.
An anesthetist and midwife will be at your head during the operation to support you, answer questions and comment on the steps of the operation.
Doctors will proceed with the operation and when they enter the uterus and the baby is due to be born, they will need to push and press a little on the abdomen to gently take the baby out. In these 1-2 minutes you can feel some unusual state, this is the moment of the birth of the child. If you want the baby to be shown to you right away so that you can be the first to see him and/or find out his gender yourself, tell the midwife and/or doctor about this in advance.
In these 1-2 minutes you can feel some unusual state, this is the moment of the birth of the child. If you want the baby to be shown to you right away so that you can be the first to see him and/or find out his gender yourself, tell the midwife and/or doctor about this in advance.
Almost all babies are usually somewhat surprised by such a quick birth, so don't worry if they don't cry right away. If the baby and mother are fine, then usually the neonatologist (children's doctor) makes sure that the umbilical cord does not cross until all the blood returns to the baby from the placenta, this usually takes about 1-2 minutes.
In less than a minute, when the baby receives additional internal oxygen support through the umbilical cord and external stimulation by the doctor's hands with a gentle massage and rubbing his body with a diaper, he will definitely raise his voice.
After cutting the umbilical cord, the midwife receives the baby and transfers him to a heated table with warm prepared linen. The baby is washed and dried. Children's doctor, neonatologist examines a newborn. Contact with the mother, including skin to skin, helps the baby to keep warm and stimulates his adaptation mechanisms and respiratory system, supporting his breathing.
The baby is washed and dried. Children's doctor, neonatologist examines a newborn. Contact with the mother, including skin to skin, helps the baby to keep warm and stimulates his adaptation mechanisms and respiratory system, supporting his breathing.
In the meantime, the OB/GYNs will clean up the uterus and administer special medications that help the uterus contract, at which point you may feel hot or feel unusual sensations, but they are not painful.
The baby is usually returned to the mother immediately after the examination and dressing. The midwife will help you hold it, attach it to your breast, and at this time, you can take photos or record a short video greeting for the family.
The operation usually takes about 30 minutes. All this time, until the end of the operation, the devices will record your condition so that the doctors can make sure that everything is fine with you. At this time, the neonatologist will tell you about the baby’s condition and offer to sign an agreement / refusal to vaccinate and administer vitamin K.
At the end of the operation, the skin will be closed with a cosmetic suture, which is usually a self-absorbable suture and does not need to be removed. Then the suture is processed and a sterile adhesive bandage is applied to the skin around the suture.
You will then be disconnected from all monitors and transported to the ICU. Your baby will be waiting for you at the children's department under the supervision of a nurse. Or in the family room with dad. If you have an agreement, then your midwife will be able to bring him to feed every three hours.
In the intensive care unit, you will be put back on continuous monitoring for several hours to make sure you are stable after surgery. You will be offered pain relief after surgery that is compatible with breastfeeding. Please report pain, any complaints and discomfort to the staff so that the doctor can adjust your treatment in time.
The sooner you can move, sit, stand and walk, drink and eat on your own, the better your recovery after surgery will be, and the chance of possible complications will decrease. If everything goes well, after 6-8 hours, the mother is transferred to the postpartum department with the child.
If everything goes well, after 6-8 hours, the mother is transferred to the postpartum department with the child.
Gentle C-Section Principles:
- Preparation
- Informing
- Birthing Plan
- Finding an institution and experienced professionals that inspire confidence and peace of mind staff.
- Competent anesthesia and comfort during the operation
- Ability to pulse the umbilical cord 1-2 minutes after removing the baby
- Ability to ensure contact with the mother, including skin to skin
- Ability to breastfeed and start breastfeeding within the first hour after birth.
- The ability to feed the baby in the intensive care unit.
- Early transfer to a shared ward with a baby.
- Ability to move, start drinking and eating as soon as possible after surgery
- Special gymnastics from the second day after childbirth for better recovery after surgery.
Vaginal delivery after CS:
80-90% of successful cases, if the cause of the previous CS was not related to the absolute impossibility of vaginal delivery in principle.