Small rashes on face of baby
Rash on a baby's face: Pictures, causes, and treatments
In babies, most facial rashes are harmless and tend to clear up without treatment. Causes can include eczema, acne, and infection.
Sometimes, however, a rash on a baby’s face can indicate a more serious condition.
Being able to distinguish between different rashes can help a parent or caregiver know when to seek professional advice.
In this article, we describe common facial rashes in babies, treatments, and when to see a doctor.
Eczema refers to a group of conditions that cause the skin to become rough, irritated, itchy, and inflamed.
These conditions are common in young children, often appearing between the ages of 6 months and 5 years. Many children grow out of their eczema.
According to the National Eczema Association in the United States, if eczema develops within the first 6 months of life, it tends to appear on the cheeks, chin, forehead, or scalp. The rash will be dry, red, and itchy.
Between the ages of 6 and 12 months, eczema may develop in other parts of the body. The elbows and knees are particularly susceptible when babies start to crawl.
Treatment
Although the exact cause of eczema is unknown, experts believe that both genetic and environmental factors can play a role.
Certain environmental triggers may over-activate the immune system, causing inflammation and skin irritation.
When trying to establish the cause of a child’s eczema, it may help to keep a diary of symptoms and potential triggers. By avoiding these triggers, it may be possible to prevent flare-ups of symptoms.
Below are some common triggers of eczema in babies:
- heat and sweating
- dry skin
- irritants, such as soaps, washing detergents, and cigarette smoke
- allergens, such as dust mites, pollen, and pet dander
- certain fabrics, such as wool and nylon
Treatments for eczema include:
- over-the-counter (OTC) moisturizers
- prescription creams and ointments, such as steroid creams
- immunosuppressant drugs
- phototherapy
A doctor can consult with a pediatric dermatologist and recommend a course of treatment. They can also advise about triggers and how to avoid them.
They can also advise about triggers and how to avoid them.
Check that over-the-counter treatments are suitable for infants.
Seborrheic dermatitis causes a rash to develop on areas of skin that contain many oil-producing glands.
In babies, the rash mainly appears on the scalp, and people commonly refer to it as cradle cap. However, cradle cap can also affect the cheeks, particularly around the eyes and nose.
The rash may have the following characteristics:
- redness and inflammation
- an oily or greasy appearance
- white or yellow scaly or crusty patches
Treatment
Cradle cap is generally harmless and usually disappears between 6 and 12 months of age.
If the child is not experiencing any discomfort, treatment may not be necessary.
For mild symptoms, OTC medications, such as antifungal creams and medicated shampoos, may help to relieve discomfort and speed healing. However, talk to a doctor before using these products on an infant.
If the rash is scaly, applying mineral oil or petroleum jelly to the baby’s scalp 1 hour before using an anti-dandruff shampoo can help loosen and remove the scales.
For babies with more severe symptoms, a doctor may prescribe topical steroids to reduce inflammation.
Particularly severe cradle cap can increase the risk of infection. See a doctor immediately, if the baby’s skin:
- feels hot
- oozes fluid
- gives off an unpleasant odor
Around 40–50 percent of healthy newborns develop milia, which are tiny white or yellow bumps about 1–3 mm in size.
Milia result from blocked pores and typically develop on the face, often around the eye and nose. The bumps can appear in large numbers, and usually a roughly equal number form on each side of the face.
In babies, milia can also develop in the mouth. In this case, the medical name is Epstein pearls.
Treatment
Milia tends to clear up on their own within a few weeks, once the pores open up.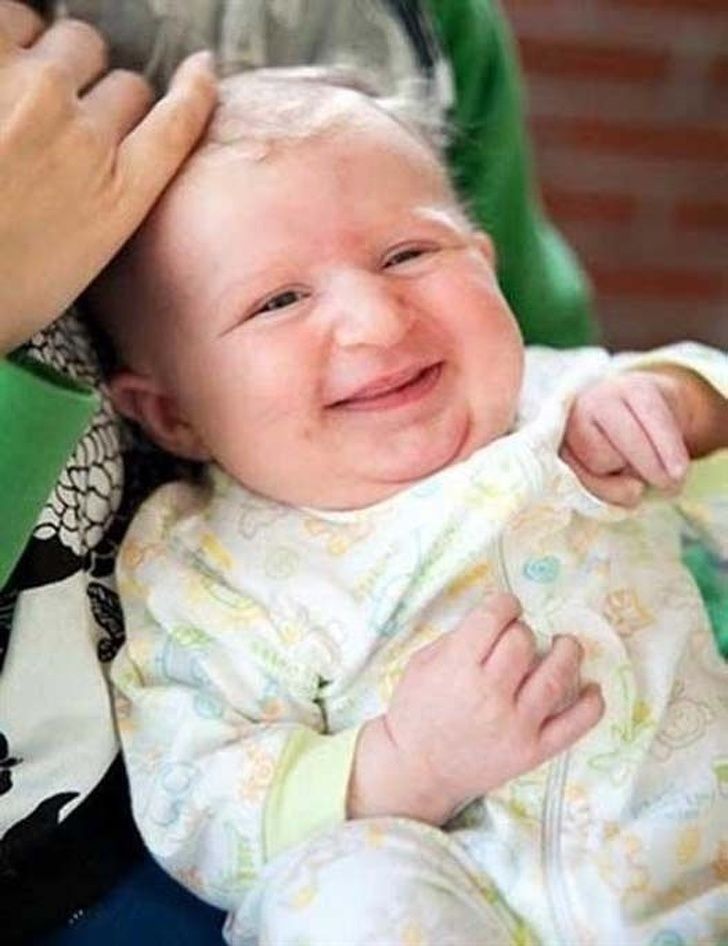
No treatment is usually necessary. Avoid using creams and ointments on the baby’s skin, as these can further clog the pores and lead to more milia.
Newborn, or neonatal, acne causes small, red pimples to develop, usually around 2–6 weeks of age. However, some babies are born with them.
The medical term for acne that develops between 6 weeks and 6 months of age infantile acne, and we discuss this below.
Neonatal acne affects around 20 percent of newborns, according to the American Academy of Dermatology.
The pimples tend to develop on the baby’s cheeks and nose, but breakouts can also appear on the:
- forehead
- chin
- scalp
- neck
- chest
- upper back
Treatment
Generally, newborn acne is not a cause for concern. It is unlikely to cause scarring and tends to clear up without treatment after a few weeks or months.
Parents and caregivers should:
- gently wash the baby’s skin with lukewarm water
- avoid scrubbing affected areas
- avoid oily or greasy skincare products
- seek advice from the child’s doctor before using acne medicines or cleansing products
Infantile acne develops in babies older than 6 weeks. It typically appears between 3 and 6 months of age.
It typically appears between 3 and 6 months of age.
Infantile acne is less common than newborn acne. Symptoms can be more severe and may require treatment.
Before treating infantile acne, it is important to rule out other conditions, such as such as eczema and infections, which are more common in this age group.
Treatment
Infantile acne usually clears up within 6–12 months after it first appears.
After diagnosis, a dermatologist can advise about treating the acne and preventing scarring. If they suspect that the acne results from an underlying medical condition, they may consult a specialist.
A doctor can diagnose the cause of a rash.
Slapped cheek syndrome is a viral infection. Anyone can get it, but it most commonly develops in school-aged children.
Other names for the syndrome include fifth disease and erythema infectiosum. It results from infection with the B19 parvovirus.
The defining characteristic is a bright red rash on one or both cheeks. The rash is not usually painful. It typically appears within 4–14 days of infection.
The rash is not usually painful. It typically appears within 4–14 days of infection.
The cheek rash often disappears in a few days, but another rash may develop on areas such as the chest, arms, and legs. This rash usually lasts for 7–10 days, but it may come and go.
The rash on the body is usually blotchy and light in color. It can be itchy, but it is not typically painful.
Slapped cheek syndrome can also cause the following symptoms:
- a fever of 38°C or higher
- a headache
- a runny nose
- a sore throat
Children can initially pass the infection to other children, but it usually stops being contagious once the rash appears.
Treatment
The symptoms of slapped cheek syndrome are usually mild, and the underlying infection typically clears up without treatment.
OTC medications, such as acetaminophen and ibuprofen, can help relieve any discomfort. However, speak to a doctor before giving these drugs to babies or young children.
Never give a child aspirin, as it may increase the risk of a serious condition called Reye’s syndrome.
Most rashes on babies’ faces are harmless. They usually clear up on their own.
However, a rash in this area can indicate an infection or an underlying health condition.
See a doctor if the rash is severe, or if the baby has:
- fluid-filled blisters
- a fever
- a loss of appetite
- red streaks extending from the rash
- tiny red or purple spots that do not fade when someone applies pressure
- swollen lymph nodes
- lethargy
- a cough
Facial rashes are common in babies and young children. The many possible causes include eczema, acne, and infection.
Most rashes clear up without treatment. However, see a doctor if a rash is severe or persistent, or if it accompanies other symptoms.
Read the article in Spanish.
Is It Baby Acne, a Rash, or Something Else?
Even adults can find it difficult to identify their skin issues. Everyone’s skin is different, and the way rashes and acne flare up can vary. Babies can’t tell you what they’re feeling, so you’ll have to go on looks alone.
Everyone’s skin is different, and the way rashes and acne flare up can vary. Babies can’t tell you what they’re feeling, so you’ll have to go on looks alone.
Read on to learn about some of the most common skin issues that babies face and how you can treat them at home.
Baby acne usually develops about 2 to 4 weeks after birth. Tiny red or white bumps appear on the baby’s cheeks, nose, and forehead. The cause is unknown. It typically clears up on its own in about 3 to 4 months without leaving marks.
To treat baby acne, don’t use any of the over-the-counter acne products you’d use on yourself. These can damage your baby’s delicate skin.
Regular home care should be enough to treat baby acne:
- Wash your baby’s face daily with warm water. You may also try a gentle, unscented soap.
- Do not scrub hard or pinch irritated areas.
- Avoid lotions and oily face products.
If you’re concerned that your baby’s acne isn’t going away, their doctor can recommend or prescribe safe treatments.
Eczema is a skin condition that causes a dry, red, itchy, and sometimes painful rash. It’s more common in children and often develops in the first 6 months of life. The condition can continue as the child gets older, or they may grow out of it.
In babies up to 6 months old, eczema often appears on the cheeks or forehead. As the baby gets older, the rash may move to the elbows, knees, and skin creases.
Eczema flares up when the skin is dry or when the skin comes into contact with an allergen or irritant, such as:
- pet dander
- dust mites
- detergent
- household cleaner
Drooling can also irritate eczema around the chin or mouth.
There’s no cure for eczema, but there are ways to manage your baby’s symptoms:
- Give your baby short, lukewarm baths (between 5 and 10 minutes) and use an unscented or gentle soap on the affected areas.
- Use a thick, unscented cream or ointment as a moisturizer twice a day.
- Use fragrance-free laundry detergent designed for sensitive skin.

Your baby’s pediatrician may be able to prescribe a steroid ointment to help reduce inflammation. Use this as directed by their doctor.
Milia are tiny white bumps on a newborn’s nose, chin, or cheeks that look similar to acne. They can also appear on the baby’s arms and legs. The bumps are caused by dead skin flakes becoming trapped near the skin’s surface. Like baby acne, milia go away without treatment.
However, you can use the same at-home care:
- Wash your baby’s face daily with plain water or if needed, an unscented or gentle soap.
- Do not scrub hard or pinch the irritated areas.
- Avoid lotions or oily face products.
Cradle cap looks like scaly, yellowish, crusty patches on the baby’s head. Depending on your baby’s skin tone, the patches may appear yellowish, brown, purple, or grey.
Cradle cap usually develops when a baby is 2 or 3 months old. There may also be redness surrounding the patches. This rash may also appear on the baby’s:
- face
- eyebrows
- neck
- ears
- armpits
Cradle cap is not harmful to your baby. It’s not itchy like eczema. It’ll go away on its own in a few weeks or months without treatment.
It’s not itchy like eczema. It’ll go away on its own in a few weeks or months without treatment.
Some things you can do at home to manage cradle cap are:
- Wash your baby’s hair and scalp with a gentle shampoo.
- Brush scales out with a soft-bristled hairbrush.
- Avoid washing hair too often, as it’ll dry out the scalp.
- Use baby oil to soften the scales so they’re easier to brush out.
Heat rash is caused when sweat gets trapped under the skin because of blocked pores. It’s usually caused by exposure to hot or humid weather. When a baby gets heat rash, they develop tiny, red, fluid-filled blisters. These can appear on the:
- neck
- shoulders
- chest
- armpits
- elbow creases
- groin
The rash generally goes away within a few days without treatment. However, see your baby’s doctor if they develop a fever or if the rash:
- does not go away
- looks worse
- gets infected
To avoid overheating, dress your baby in loose-fitting cotton clothing during hot summer months. Take off extra layers if they get too hot in cooler weather.
Take off extra layers if they get too hot in cooler weather.
Hand, foot, and mouth disease (HFMD) is a highly contagious viral infection. HFMD commonly causes blisters or sores to appear in or around the mouth or on the hands or feet. The rash may be seen in one or more of these locations.
The rash looks like red blisters or bumps. As the disease progresses, the sores may crust over. The spots may be harder to identify on darker skin tones.
While it can occur in anyone, it’s more commonly seen in children under 5 years old.
Additional symptoms may include:
- fever
- decreased appetite
- general malaise
- drooling
- irritability
- sore throat
- headache
Because HFMD is a viral infection, there is no treatment. People typically recover within 7 to 10 days.
Talk with your baby’s pediatrician to determine if you can offer baby acetaminophen (Tylenol) to help make your child more comfortable while they recover. Your pediatrician may also recommend ibuprofen (Motrin) in babies 6 months and older.
Your pediatrician may also recommend ibuprofen (Motrin) in babies 6 months and older.
A pediatrician may also be able to recommend over-the-counter or prescription topical ointments to help relieve pain from the sores.
Limit acidic or spicy foods, such as citrus, as these can irritate the sores. Instead, offer cold foods, like popsicles, to help soothe sores in the mouth. It’s also important to keep your child isolated and out of care settings until the sores have healed. HFMD is extremely contagious.
These skin conditions are generally harmless and usually go away on their own with little or no treatment. You can help your baby avoid irritating the area by keeping their nails short and putting soft cotton gloves or socks on them at night.
If you’re concerned or feel that your child may require medical intervention, talk with their pediatrician.
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the website
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
Causes of a rash in children
Naturally, only a pediatrician, dermatologist or allergist can correctly determine the cause of the rash , diagnose and prescribe treatment for a child. But provide initial assistance, relieve itching and the parents themselves can help the baby, knowing the main signs and causes of rash . At the first stage, it is important to determine the nature of the rash - infectious , allergic or none of the above.
But provide initial assistance, relieve itching and the parents themselves can help the baby, knowing the main signs and causes of rash . At the first stage, it is important to determine the nature of the rash - infectious , allergic or none of the above.
Causes of rashes in children:
1. Newborn acne . For the first time may occur in newborns at the age of 1 - 2 months. As a rule, such rashes are hormonal in nature, are not contagious and are not allergic . A rash in the form of pimples, sometimes with a white dot in the middle, appears on the head, body of the baby. If there are no purulent compartments, then the rash goes away on its own and does not require treatment. Acne can also occur in teenagers. They most often appear on the face in the form of black dots and are associated with hormonal changes in the body of a teenager and an increased work of the sebaceous glands. To prevent acne, there are cosmetic lotions, washing gels and other products. In case of inflammation, it is better to seek advice from a pediatric dermatologist or cosmetologist, because. antibiotic treatment may be needed;
To prevent acne, there are cosmetic lotions, washing gels and other products. In case of inflammation, it is better to seek advice from a pediatric dermatologist or cosmetologist, because. antibiotic treatment may be needed;
2. Urticaria is an allergic reaction on the child's skin, accompanied by itching and the appearance of blisters on various parts of the body, in some cases the temperature may rise and the child's stool is disturbed. The blisters appear suddenly and can disappear just as quickly, but sometimes they disappear only after a few days. The causes of urticaria can be various factors: hormonal disorders, malfunctions of the liver, kidneys, consumption of foods that caused an allergic reaction (fish, eggs, citrus fruits, etc.), insect bites, reaction to sunlight, temperature changes, emotional stress etc. Urticaria can be chronic does not go away for a long time, and acute disappears after a few hours. For the treatment of urticaria, it is important to identify the underlying cause that caused it;
For the treatment of urticaria, it is important to identify the underlying cause that caused it;
3. Food allergy manifests as pinkish-red spots. It is slightly convex, edematous in places of scratching and is accompanied by itching. It is localized, as a rule, on the baby's cheeks, but can also appear on other parts of the body. It can occur in both infants and adolescents. If the baby is breastfed, then the allergy that has arisen is associated with the products consumed by the mother. If the newborn is artificially fed, then an allergic reaction may appear on the mixture. In older children, food allergies can be caused by fish, eggs, nuts, chocolate, strawberries, and other foods;
Allergy, as a rule, is accompanied by edema, which in turn, if not properly treated and provided with untimely assistance, cause suffocation . If an allergy of any nature occurs, a pediatrician's consultation is required to help in choosing the optimal mixture for the baby, or a pediatric dermatologist - allergist for referral to laboratory tests of older children ;
4. Household allergies . It can occur in both newborns and older children. It usually appears as pimples all over the body and is accompanied by lachrymation, sneezing. The causes of such a reaction of the body can be washing powder and other detergents, dust, plants, animal hair, etc. An allergic rash differs from an infectious rash in that the child does not have a temperature with it, he does not have general ailments, there is no loss of appetite, drowsiness;
Household allergies . It can occur in both newborns and older children. It usually appears as pimples all over the body and is accompanied by lachrymation, sneezing. The causes of such a reaction of the body can be washing powder and other detergents, dust, plants, animal hair, etc. An allergic rash differs from an infectious rash in that the child does not have a temperature with it, he does not have general ailments, there is no loss of appetite, drowsiness;
5. Prickly heat . It occurs mainly in infants. It manifests itself in the form of red pimples all over the body, especially in the inguinal zone. The affected areas must be smeared with a special baby cream, air baths more often for the baby and a diaper change;
6. Roseola (erythema infectiosum) is an acute childhood viral disease affecting only children under 2 years of age. Very often, roseola is confused with SARS or rubella . At the beginning of the illness, the baby's temperature rises sharply, which lasts 3-5 days, and after that the child becomes covered with a red-pink rash that disappears in 5-7 days. This is not a dangerous disease, it does not require treatment, and if it occurs, the child should be given only antipyretic drugs;
At the beginning of the illness, the baby's temperature rises sharply, which lasts 3-5 days, and after that the child becomes covered with a red-pink rash that disappears in 5-7 days. This is not a dangerous disease, it does not require treatment, and if it occurs, the child should be given only antipyretic drugs;
7. Windmill . This is a common childhood infectious disease that requires treatment. The incubation period of this disease can last from 11 to 21 days. Occurs at any age. It is accompanied by a rash on the skin and mucous membranes in the form of red spots, in the center of which blisters with a yellowish liquid are localized. Accompanied by itching. As the disease progresses, the blisters burst, crusts form, leaving scars if the child has scratched the blister and brought the infection. The disease can also cause fever and headache;
8. Measles is an acute infectious disease that is quite rare due to the use of vaccinations. In addition, this virus is rarely activated in babies under 8 months old, because. they are protected by their mother's immunity. The disease begins with symptoms of a common cold - coughing, lacrimation, sneezing and fever up to 40 C. Then the child develops white spots on the mucous surface of the cheeks, nasal discharge, severe headache, photophobia. Then, within a few days, red spots of various shapes appear on the face, neck, near the head and further throughout the body. The disease is contagious within a week of the onset of the first symptoms. The virus is dangerous with complications such as: meningitis , pneumonia , development of deafness, brain damage and even death;
In addition, this virus is rarely activated in babies under 8 months old, because. they are protected by their mother's immunity. The disease begins with symptoms of a common cold - coughing, lacrimation, sneezing and fever up to 40 C. Then the child develops white spots on the mucous surface of the cheeks, nasal discharge, severe headache, photophobia. Then, within a few days, red spots of various shapes appear on the face, neck, near the head and further throughout the body. The disease is contagious within a week of the onset of the first symptoms. The virus is dangerous with complications such as: meningitis , pneumonia , development of deafness, brain damage and even death;
9. Scarlet fever is an acute infectious streptococcal disease. Begins with sore throat, high temperature, enlarged tonsils , in some cases with plaque. Then a small dotted rash appears on the back, chest, knees, armpits, groin and quickly spreads throughout the body and face. Only the area around the mouth remains white. Throat and tongue become very red. By the end of the disease, peeling of the skin on the toes and hands begins;
Only the area around the mouth remains white. Throat and tongue become very red. By the end of the disease, peeling of the skin on the toes and hands begins;
10. Rubella is an acute infectious disease . The disease begins with a slight increase in temperature and enlargement of the lymph nodes in the parotid and cervical region. A small rash also appears on the face and behind the ears, and then all over the body. Rubella is very dangerous for pregnant women, and complications can occur in older children and adolescents. In children, the disease proceeds in a fairly mild form;
11. Meningitis is an inflammation of the membranes of the brain and spinal cord. Rash in meningitis is not the main symptom. However, with this disease, rashes appear on the back of the throat, as well as on the hips, back, buttocks in the form of a red rash of various shapes. Symptoms of meningitis include very high fever, severe headache, vomiting, photophobia, and neck muscle tension. At the slightest suspicion of meningitis, parents should immediately consult a doctor. Timely help with this disease will save the child's life;
At the slightest suspicion of meningitis, parents should immediately consult a doctor. Timely help with this disease will save the child's life;
12. Streptoderma is a skin infection caused by Staphylococcus aureus. The disease affects, as a rule, the paranasal and perioral region. In the beginning, redness appears around the nose and mouth, then small bubbles with liquid. When they burst, yellow crusts remain. The disease may be accompanied by fever;
13. Herpes is an infectious disease accompanied by the appearance of blisters on the skin and mucous membranes, in children it is most often located on the lips. This disease is extremely rare in newborns, because. they are given maternal immunity. It affects children from 3 to 4 years of age. In addition to a rash, the disease may be accompanied by a sore throat, fever.
There are a lot of skin rashes and diseases in children, they can be very similar, but some are completely harmless to your child's health, while others pose a threat not only to the general condition, but also to the child's life! Do not take risks, and if you have any doubts, if any spots, rashes and other symptoms appear, contact your pediatrician, who, if necessary, will refer you and your child to a pediatric dermatologist, allergist, neurologist or other highly specialized specialist, depending on the nature of the rash and the severity of the skin disease.