Blighted ovum statistics
Anembryonic Pregnancy - StatPearls - NCBI Bookshelf
Khalid Chaudhry; Dawood Tafti; Marco A. Siccardi.
Author Information
Last Update: September 19, 2022.
Continuing Education Activity
A blighted ovum, also known as an anembryonic pregnancy, occurs when a fertilized egg implants and a gestational (embryonic) sac forms and grows, but the embryo fails to develop. A blighted ovum is the single leading cause of miscarriage. This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
Objectives:
Outline the risk factors for a blighted ovum.
Describe the clinical presentation of a patient with a blighted ovum.
List the treatment and management options available for a patient with a blighted ovum.
Employ interprofessional team strategies for improving care coordination and communication to enhance fertility rates in patients with a history of miscarriage.
Access free multiple choice questions on this topic.
Introduction
An anembryonic pregnancy is characterized by a gestational sac that forms and grows while an embryo fails to develop. Although the terms anembryonic pregnancy and blighted ovum are synonymous, the latter is falling out of favor for the more descriptive former term. Anembryonic pregnancy constitutes a significant but unknown proportion of miscarriages with the American Pregnancy Association estimating anembryonic pregnancy to constitute half of all first trimester miscarriages. Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
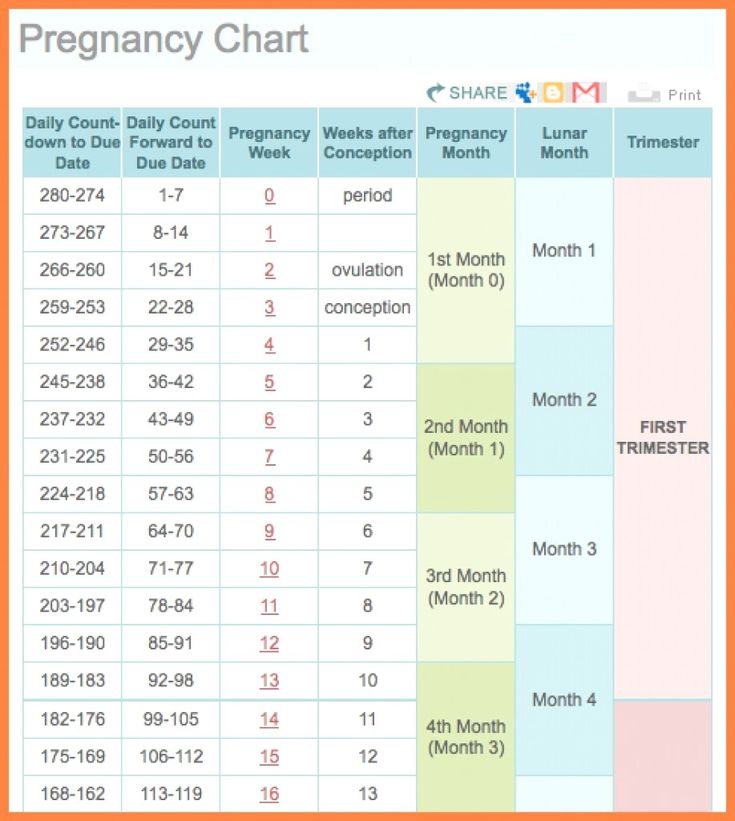
In the first trimester, the terms early pregnancy loss, miscarriage, or spontaneous abortion are often used interchangeably. Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
What is a Miscarriage?
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs 500 g or less. This definition is used in the United States; however, it may vary based on State laws.[5]
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification and confirmation.
Clinical miscarriage is when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy. Clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 weeks to 20 weeks).
Etiology
The exact etiology for anembryonic pregnancies is difficult to ascertain. The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
Morphological abnormalities of an embryo that prevents implantation or prevents long term survival of the embryo after implantation. These morphological abnormalities are thought to be related to chromosomal abnormalities. [6]
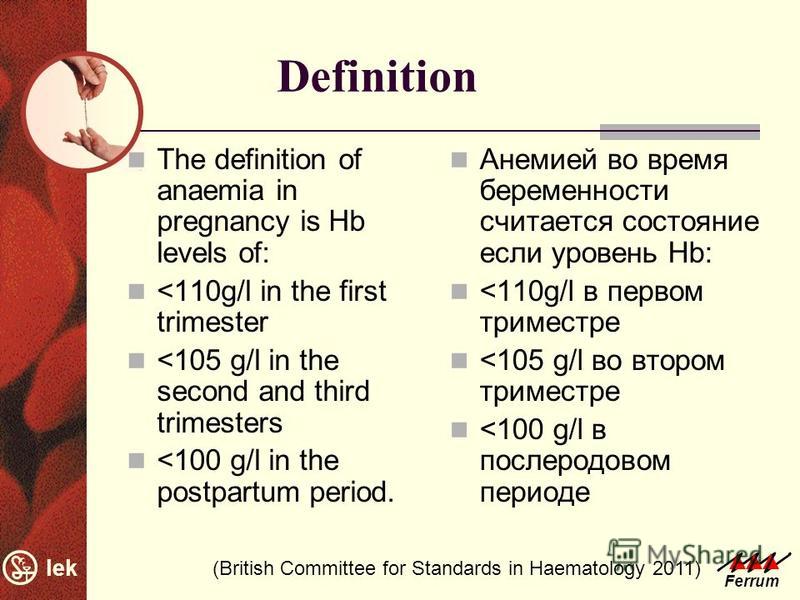
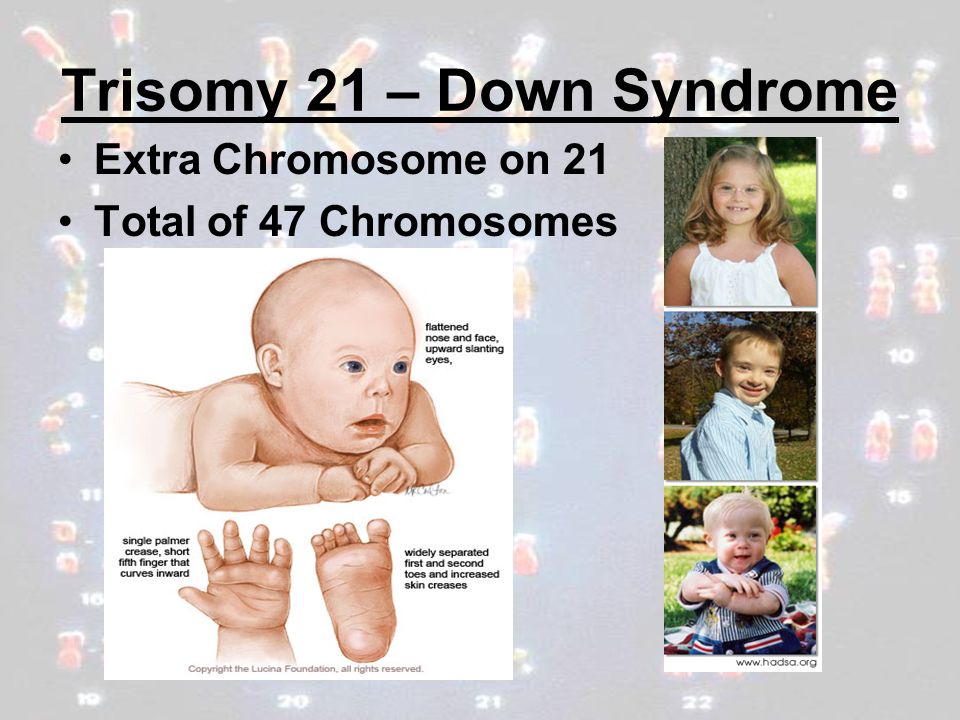
Chromosomal abnormalities that collectively include autosomal trisomy, polyploidy, sex chromosomal polysomy, and monosomy X likely represent the most common etiologies for EPL. Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.

Other genetic and chromosomal abnormalities include translocations, inversions, single-gene perturbations, and placental mosaicism. [7] Consanguineous marriages resulting in anembryonic pregnancies have also been noted, suggesting a role of single gene determinants. [8] There is a probable link between DNA damage in sperm and miscarriage. [9]]
Obesity and advanced maternal age are well-established factors associated with early pregnancy loss. [10]
Tuberculosis in the developing world as well as reproductive tract infections worldwide can predispose to EPL. [11] The complications of genital tract infections that include intrauterine adhesions can impede implantation and embryo growth.
Malformation of the uterus that includes didelphic, bicornuate, and septate uteri can impede in or prevent the longterm implantation of an embryo.
Immunologic disorders in the mother such as NK Cell Dysfunction, autoantibodies, hereditary, and acquired thrombophilia, among others) can lead to the maternal immunological rejection of the implanting embryo in the uterus resulting in miscarriage.
Hormonal factors (such as low levels of progesterone) and endocrinological disorders(thyroid autoimmunity and thyroid dysfunction) play a complex role in miscarriage. Polycystic ovarian syndrome is also associated with infertility and pregnancy loss.
The role of alcohol consumption and it's associated increased risk in miscarriage has been well established. [12]
Epidemiology
Although difficult to definitively establish, anembryonic pregnancy possibly represents half of all miscarriages in the first trimester of pregnancy. [13][14] The incidence of early pregnancy loss (before 12 weeks) is estimated to be about 15% of clinically evident conceptions with significant variations in incidence based on patient age. The incidence ranges from 10% in women 20 to 24 years of age to 51% in women 40 to 44 years of age. [15] A prior history of early pregnancy loss also predisposes a patient to miscarriage. [16]
History and Physical
The signs and symptoms of an anembryonic pregnancy can potentially mirror those of an ectopic pregnancy. Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Evaluation
Clinical signs and symptoms, a pregnancy test, and an ultrasound exam confirm the diagnosis.
A pregnancy test can be obtained using urine or serum hCG levels.
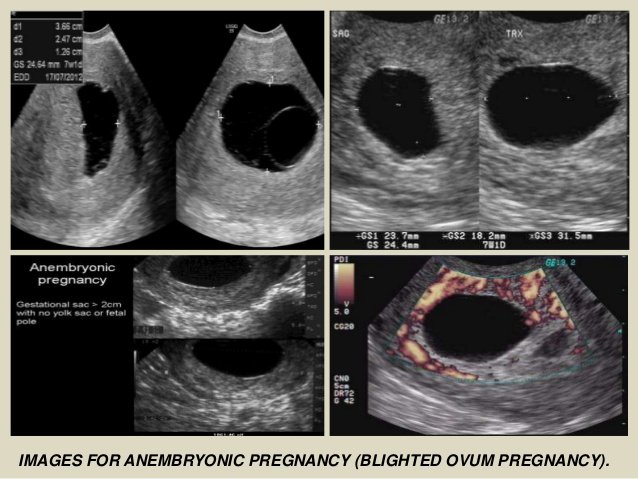
Ultrasound exam (transabdominal or transvaginal) classically demonstrates an empty gestational sac without an embryo.
An anembryonic pregnancy is established on endovaginal ultrasound technique when there is no discernable embryo seen in a gestational sac with a mean sac diameter of ≥25 mm.
Alternatively, an anembryonic pregnancy can be established when there is no embryo on a follow-up endovaginal scan:
≥11 days after a scan demonstrating a gestational sac with a yolk sac, but an absent embryo
≥ 2 weeks (14 days) after a scan demonstrating a gestational sac without an embryo or a yolk sac
Treatment / Management
The three treatment options for early pregnancy loss include expectant management, medical management, and surgical treatment.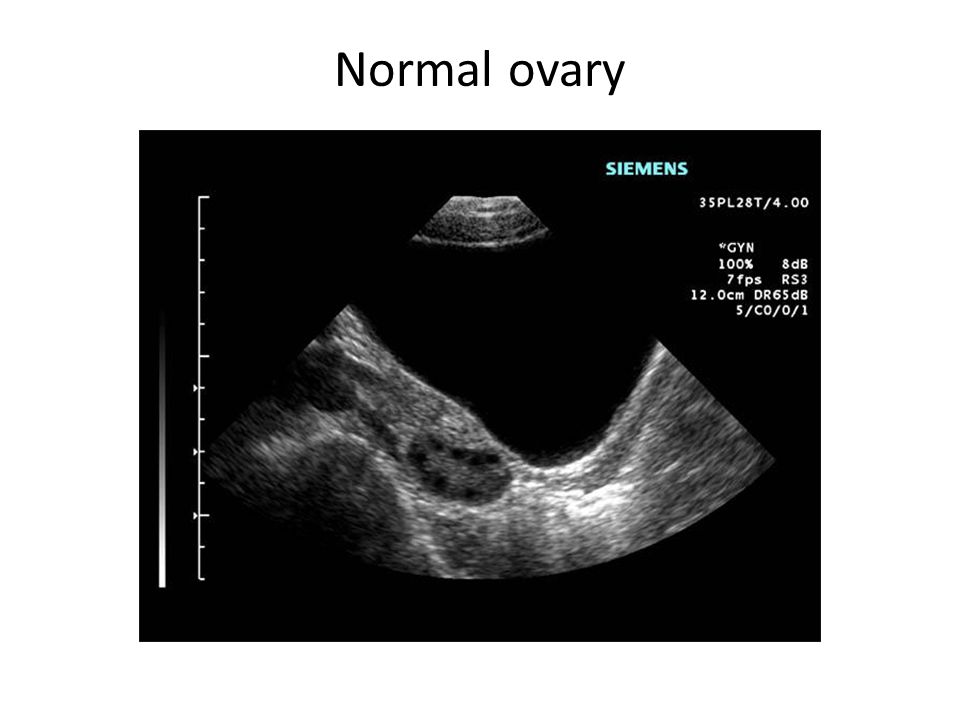 Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Differential Diagnosis
The chief obstetric differential diagnosis for an anembryonic pregnancy includes:
Pseudogestational sac which represents a small amount of intrauterine fluid
Early intrauterine pregnancy
An ectopic pregnancy
Implantation bleeding from an otherwise viable pregnancy
Gestational trophoblastic disease
Complications relating to a viable pregnancy
Prognosis
Prognosis and successful management of early pregnancy loss depends on a variety of factors including gestation age. Prognosis is generally considered good with all three management options.
Expectant management: in a meta-analysis of 20 studies, expectant management and medical management were both determined to be acceptable treatment options for incomplete abortion.
 [17]
[17]Medical management: medical management is more successful with multiple-dose regimens of misoprostol. Patients with incomplete abortion are treated more successfully with medical management than with expectant management.
Surgical Treatment: at least one large randomized control trial determined a higher success rate in surgical treatment than with medical management, with a general conclusion of the general safety of both treatment options. [18]
Complications
Serious complications of treatment are uncommon. Complications can include:
Heavy bleeding/hemorrhage
Uterine perforation(from surgical management)
Infection to include fatal sepsis
Complications from a missed ectopic pregnancy
Consultations
OB/GYN
Primary care provider
Psychologist/psychiatrist
Emergency department physician
Radiologist/sonographer(especially when there is a concern for an ectopic pregnancy)
Deterrence and Patient Education
The following represent key points in patient education:
Patients should be advised to present to their emergency department if they experience heavy vaginal bleeding(two pads per hour for approximately two consecutive hours).

Signs and symptoms of infection should be discussed with patients especially following surgical management.
Treatment with misoprostol can cause a febrile reaction which can be misinterpreted as a sign of infection.
Prophylactic antibiotics are not routinely administered but can be considered in select patients.
Patients should adhere to follow-up sonogram and outpatient appointments especially when additional doses of misoprostol are considered to be clinically necessary.
A miscarriage can be a traumatic experience for a patient. Reassurance and empathy play a key role in helping patients through the grieving process.
Pearls and Other Issues
Pregnancy loss is a common complication in the first trimester of pregnancy
Most losses occur in the first trimester
Early pregnancy loss without embryo development is likely due to chromosomal and genetic abnormalities
There are specific sonographic criteria for determining an anembryonic pregnancy
A pseudogestational sac, an ectopic pregnancy, and an early pregnancy are important differential diagnoses to consider when evaluating an anembryonic pregnancy
Expectant management, medical treatment with misoprostol, and surgical treatment are the three primary options for management
Enhancing Healthcare Team Outcomes
Establishing an anembryonic pregnancy can sometimes b difficult on an ultrasound. Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
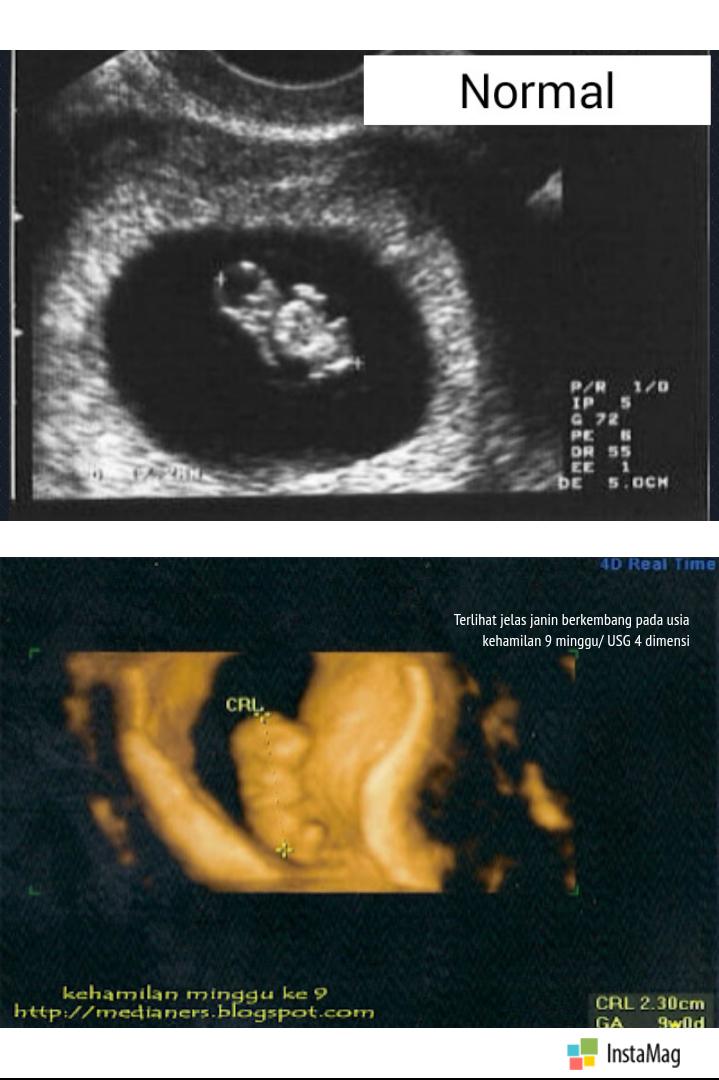
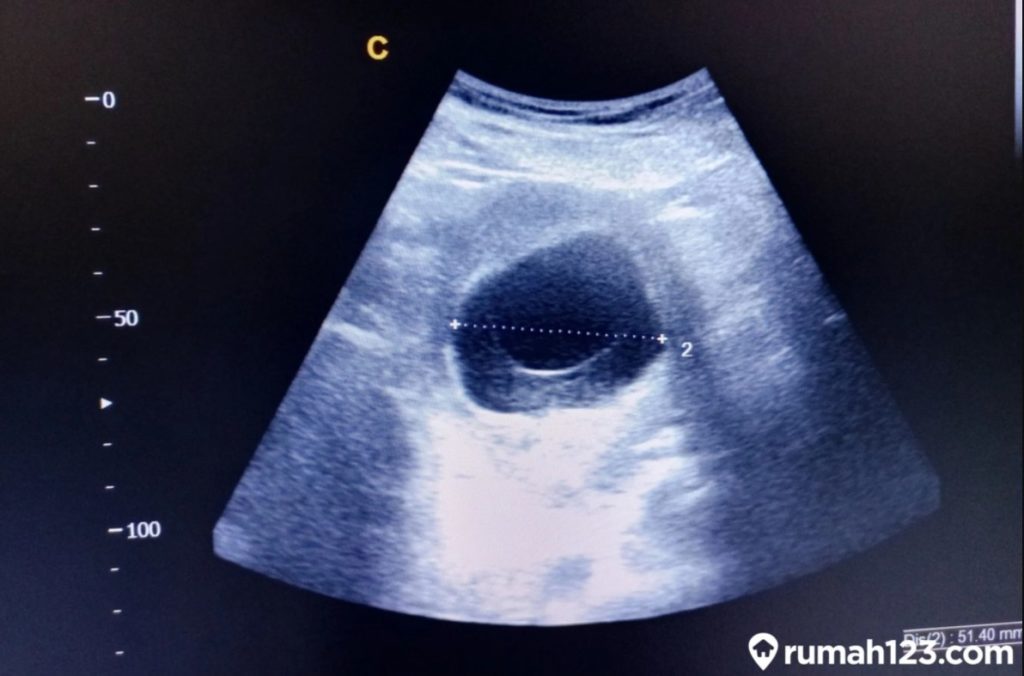
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac.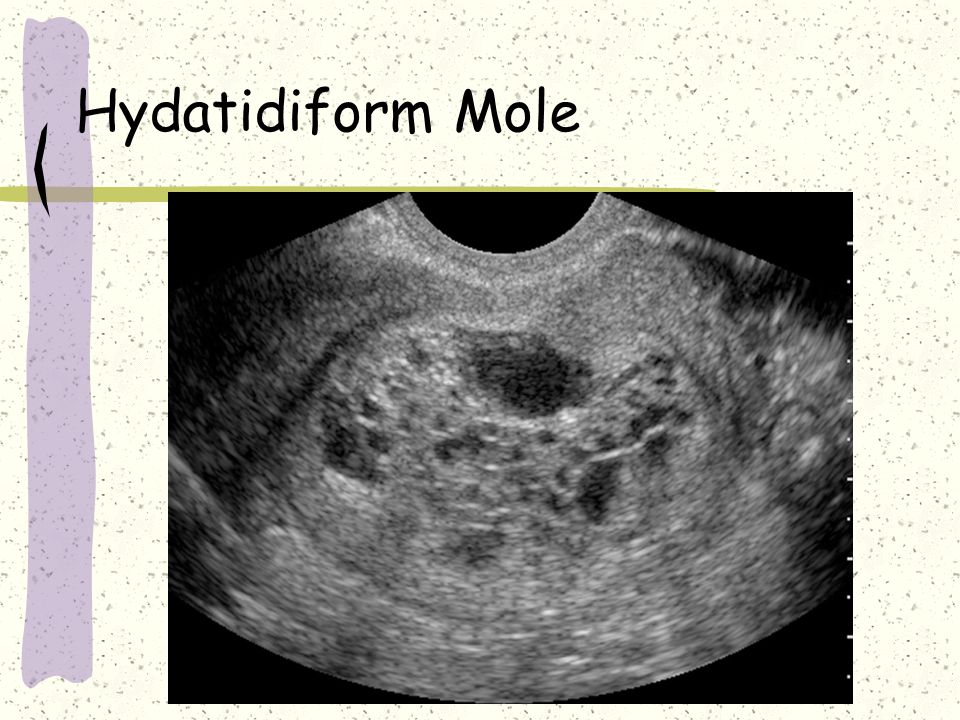 No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
References
- 1.
Macklon NS, Geraedts JP, Fauser BC. Conception to ongoing pregnancy: the 'black box' of early pregnancy loss. Hum Reprod Update. 2002 Jul-Aug;8(4):333-43. [PubMed: 12206468]
- 2.
Goldhaber MK, Fireman BH. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology. 1991 Jan;2(1):33-9. [PubMed: 2021664]
- 3.
Serdinšek T, Reljič M, Kovač V. Medical management of first trimester missed miscarriage: the efficacy and complication rate.
 J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]
J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]- 4.
Zeqiri F, Paçarada M, Kongjeli N, Zeqiri V, Kongjeli G. Missed abortion and application of misoprostol. Med Arh. 2010;64(3):151-3. [PubMed: 20645507]
- 5.
Yin Y, Zhang T, Dai Y, Bao Y, Chen X, Lu X. The effect of plasma lead on anembryonic pregnancy. Ann N Y Acad Sci. 2008 Oct;1140:184-9. [PubMed: 18991916]
- 6.
Hertig AT, Rock J. Searching for early fertilized human ova. Gynecol Invest. 1973;4(3):121-39. [PubMed: 4593973]
- 7.
Berglund G. Preparation of antiserum to an antigen of low molecular weight. Nature. 1965 May 01;206(983):523-4. [PubMed: 4953500]
- 8.
Shekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. Int J Mol Cell Med. 2013 Fall;2(4):164-8. [PMC free article: PMC3927383] [PubMed: 24551808]
- 9.

Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012 Oct;27(10):2908-17. [PubMed: 22791753]
- 10.
Cavalcante MB, Sarno M, Peixoto AB, Araujo Júnior E, Barini R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. J Obstet Gynaecol Res. 2019 Jan;45(1):30-38. [PubMed: 30156037]
- 11.
Patki A, Chauhan N. An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India. J Obstet Gynaecol India. 2016 Oct;66(5):310-5. [PMC free article: PMC4958068] [PubMed: 27486274]
- 12.
Sundermann AC, Zhao S, Young CL, Lam L, Jones SH, Velez Edwards DR, Hartmann KE. Alcohol Use in Pregnancy and Miscarriage: A Systematic Review and Meta-Analysis. Alcohol Clin Exp Res. 2019 Aug;43(8):1606-1616. [PMC free article: PMC6677630] [PubMed: 31194258]
- 13.

Andersen LB, Dechend R, Karumanchi SA, Nielsen J, Joergensen JS, Jensen TK, Christesen HT. Early pregnancy angiogenic markers and spontaneous abortion: an Odense Child Cohort study. Am J Obstet Gynecol. 2016 Nov;215(5):594.e1-594.e11. [PubMed: 27287686]
- 14.
Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertil Steril. 2000 Feb;73(2):270-4. [PubMed: 10685527]
- 15.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019 Mar 20;364:l869. [PMC free article: PMC6425455] [PubMed: 30894356]
- 16.
Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. BMJ. 1989 Aug 26;299(6698):541-5. [PMC free article: PMC1837397] [PubMed: 2507063]
- 17.
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L.
 Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1:CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]
Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1:CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]- 18.
Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM., National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005 Aug 25;353(8):761-9. [PubMed: 16120856]
Anembryonic Pregnancy - StatPearls - NCBI Bookshelf
Khalid Chaudhry; Dawood Tafti; Marco A. Siccardi.
Author Information
Last Update: September 19, 2022.
Continuing Education Activity
A blighted ovum, also known as an anembryonic pregnancy, occurs when a fertilized egg implants and a gestational (embryonic) sac forms and grows, but the embryo fails to develop. A blighted ovum is the single leading cause of miscarriage. This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
Objectives:
Outline the risk factors for a blighted ovum.
Describe the clinical presentation of a patient with a blighted ovum.
List the treatment and management options available for a patient with a blighted ovum.
Employ interprofessional team strategies for improving care coordination and communication to enhance fertility rates in patients with a history of miscarriage.
Access free multiple choice questions on this topic.
Introduction
An anembryonic pregnancy is characterized by a gestational sac that forms and grows while an embryo fails to develop. Although the terms anembryonic pregnancy and blighted ovum are synonymous, the latter is falling out of favor for the more descriptive former term. Anembryonic pregnancy constitutes a significant but unknown proportion of miscarriages with the American Pregnancy Association estimating anembryonic pregnancy to constitute half of all first trimester miscarriages. Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
In the first trimester, the terms early pregnancy loss, miscarriage, or spontaneous abortion are often used interchangeably. Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
What is a Miscarriage?
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs 500 g or less. This definition is used in the United States; however, it may vary based on State laws.[5]
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification and confirmation.
Clinical miscarriage is when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy. Clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 weeks to 20 weeks).
Etiology
The exact etiology for anembryonic pregnancies is difficult to ascertain. The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
Morphological abnormalities of an embryo that prevents implantation or prevents long term survival of the embryo after implantation. These morphological abnormalities are thought to be related to chromosomal abnormalities. [6]
Chromosomal abnormalities that collectively include autosomal trisomy, polyploidy, sex chromosomal polysomy, and monosomy X likely represent the most common etiologies for EPL.
 Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.
Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise. Other genetic and chromosomal abnormalities include translocations, inversions, single-gene perturbations, and placental mosaicism. [7] Consanguineous marriages resulting in anembryonic pregnancies have also been noted, suggesting a role of single gene determinants. [8] There is a probable link between DNA damage in sperm and miscarriage. [9]]
Obesity and advanced maternal age are well-established factors associated with early pregnancy loss.
 [10]
[10] Tuberculosis in the developing world as well as reproductive tract infections worldwide can predispose to EPL. [11] The complications of genital tract infections that include intrauterine adhesions can impede implantation and embryo growth.
Malformation of the uterus that includes didelphic, bicornuate, and septate uteri can impede in or prevent the longterm implantation of an embryo.
Immunologic disorders in the mother such as NK Cell Dysfunction, autoantibodies, hereditary, and acquired thrombophilia, among others) can lead to the maternal immunological rejection of the implanting embryo in the uterus resulting in miscarriage.
Hormonal factors (such as low levels of progesterone) and endocrinological disorders(thyroid autoimmunity and thyroid dysfunction) play a complex role in miscarriage. Polycystic ovarian syndrome is also associated with infertility and pregnancy loss.
The role of alcohol consumption and it's associated increased risk in miscarriage has been well established.
 [12]
[12]
Epidemiology
Although difficult to definitively establish, anembryonic pregnancy possibly represents half of all miscarriages in the first trimester of pregnancy. [13][14] The incidence of early pregnancy loss (before 12 weeks) is estimated to be about 15% of clinically evident conceptions with significant variations in incidence based on patient age. The incidence ranges from 10% in women 20 to 24 years of age to 51% in women 40 to 44 years of age. [15] A prior history of early pregnancy loss also predisposes a patient to miscarriage. [16]
History and Physical
The signs and symptoms of an anembryonic pregnancy can potentially mirror those of an ectopic pregnancy. Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Evaluation
Clinical signs and symptoms, a pregnancy test, and an ultrasound exam confirm the diagnosis.
A pregnancy test can be obtained using urine or serum hCG levels.
Ultrasound exam (transabdominal or transvaginal) classically demonstrates an empty gestational sac without an embryo.
An anembryonic pregnancy is established on endovaginal ultrasound technique when there is no discernable embryo seen in a gestational sac with a mean sac diameter of ≥25 mm.
Alternatively, an anembryonic pregnancy can be established when there is no embryo on a follow-up endovaginal scan:
≥11 days after a scan demonstrating a gestational sac with a yolk sac, but an absent embryo
≥ 2 weeks (14 days) after a scan demonstrating a gestational sac without an embryo or a yolk sac
Treatment / Management
The three treatment options for early pregnancy loss include expectant management, medical management, and surgical treatment.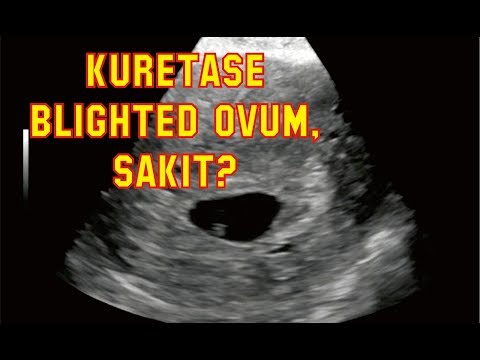 Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Differential Diagnosis
The chief obstetric differential diagnosis for an anembryonic pregnancy includes:
Pseudogestational sac which represents a small amount of intrauterine fluid
Early intrauterine pregnancy
An ectopic pregnancy
Implantation bleeding from an otherwise viable pregnancy
Gestational trophoblastic disease
Complications relating to a viable pregnancy
Prognosis
Prognosis and successful management of early pregnancy loss depends on a variety of factors including gestation age. Prognosis is generally considered good with all three management options.
Expectant management: in a meta-analysis of 20 studies, expectant management and medical management were both determined to be acceptable treatment options for incomplete abortion.
 [17]
[17]Medical management: medical management is more successful with multiple-dose regimens of misoprostol. Patients with incomplete abortion are treated more successfully with medical management than with expectant management.
Surgical Treatment: at least one large randomized control trial determined a higher success rate in surgical treatment than with medical management, with a general conclusion of the general safety of both treatment options. [18]
Complications
Serious complications of treatment are uncommon. Complications can include:
Heavy bleeding/hemorrhage
Uterine perforation(from surgical management)
Infection to include fatal sepsis
Complications from a missed ectopic pregnancy
Consultations
OB/GYN
Primary care provider
Psychologist/psychiatrist
Emergency department physician
Radiologist/sonographer(especially when there is a concern for an ectopic pregnancy)
Deterrence and Patient Education
The following represent key points in patient education:
Patients should be advised to present to their emergency department if they experience heavy vaginal bleeding(two pads per hour for approximately two consecutive hours).

Signs and symptoms of infection should be discussed with patients especially following surgical management.
Treatment with misoprostol can cause a febrile reaction which can be misinterpreted as a sign of infection.
Prophylactic antibiotics are not routinely administered but can be considered in select patients.
Patients should adhere to follow-up sonogram and outpatient appointments especially when additional doses of misoprostol are considered to be clinically necessary.
A miscarriage can be a traumatic experience for a patient. Reassurance and empathy play a key role in helping patients through the grieving process.
Pearls and Other Issues
Pregnancy loss is a common complication in the first trimester of pregnancy
Most losses occur in the first trimester
Early pregnancy loss without embryo development is likely due to chromosomal and genetic abnormalities
There are specific sonographic criteria for determining an anembryonic pregnancy
A pseudogestational sac, an ectopic pregnancy, and an early pregnancy are important differential diagnoses to consider when evaluating an anembryonic pregnancy
Expectant management, medical treatment with misoprostol, and surgical treatment are the three primary options for management
Enhancing Healthcare Team Outcomes
Establishing an anembryonic pregnancy can sometimes b difficult on an ultrasound. Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
References
- 1.
Macklon NS, Geraedts JP, Fauser BC. Conception to ongoing pregnancy: the 'black box' of early pregnancy loss. Hum Reprod Update. 2002 Jul-Aug;8(4):333-43. [PubMed: 12206468]
- 2.
Goldhaber MK, Fireman BH. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology. 1991 Jan;2(1):33-9. [PubMed: 2021664]
- 3.
Serdinšek T, Reljič M, Kovač V. Medical management of first trimester missed miscarriage: the efficacy and complication rate.
 J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]
J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]- 4.
Zeqiri F, Paçarada M, Kongjeli N, Zeqiri V, Kongjeli G. Missed abortion and application of misoprostol. Med Arh. 2010;64(3):151-3. [PubMed: 20645507]
- 5.
Yin Y, Zhang T, Dai Y, Bao Y, Chen X, Lu X. The effect of plasma lead on anembryonic pregnancy. Ann N Y Acad Sci. 2008 Oct;1140:184-9. [PubMed: 18991916]
- 6.
Hertig AT, Rock J. Searching for early fertilized human ova. Gynecol Invest. 1973;4(3):121-39. [PubMed: 4593973]
- 7.
Berglund G. Preparation of antiserum to an antigen of low molecular weight. Nature. 1965 May 01;206(983):523-4. [PubMed: 4953500]
- 8.
Shekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. Int J Mol Cell Med. 2013 Fall;2(4):164-8. [PMC free article: PMC3927383] [PubMed: 24551808]
- 9.
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012 Oct;27(10):2908-17. [PubMed: 22791753]
- 10.
Cavalcante MB, Sarno M, Peixoto AB, Araujo Júnior E, Barini R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. J Obstet Gynaecol Res. 2019 Jan;45(1):30-38. [PubMed: 30156037]
- 11.
Patki A, Chauhan N. An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India. J Obstet Gynaecol India. 2016 Oct;66(5):310-5. [PMC free article: PMC4958068] [PubMed: 27486274]
- 12.
Sundermann AC, Zhao S, Young CL, Lam L, Jones SH, Velez Edwards DR, Hartmann KE. Alcohol Use in Pregnancy and Miscarriage: A Systematic Review and Meta-Analysis. Alcohol Clin Exp Res. 2019 Aug;43(8):1606-1616. [PMC free article: PMC6677630] [PubMed: 31194258]
- 13.
Andersen LB, Dechend R, Karumanchi SA, Nielsen J, Joergensen JS, Jensen TK, Christesen HT. Early pregnancy angiogenic markers and spontaneous abortion: an Odense Child Cohort study. Am J Obstet Gynecol. 2016 Nov;215(5):594.e1-594.e11. [PubMed: 27287686]
- 14.
Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertil Steril. 2000 Feb;73(2):270-4. [PubMed: 10685527]
- 15.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019 Mar 20;364:l869. [PMC free article: PMC6425455] [PubMed: 30894356]
- 16.
Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. BMJ. 1989 Aug 26;299(6698):541-5. [PMC free article: PMC1837397] [PubMed: 2507063]
- 17.
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L.
 Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1:CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]
Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1:CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]- 18.
Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM., National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005 Aug 25;353(8):761-9. [PubMed: 16120856]
Medicine - Ogonyok No. 6 (5502) dated February 19, 2018
Gerontology
Get old, not get sick
Photo: Science Source / Getty Images
Scientists have discovered a mechanism in bats that prevents cells from aging. If it can be applied to humans, we can extend years of disease-free life. Compared to people, bats do not live long - 20 years. But for such small animals, this is a record age. Scientists decided to investigate what happens to their chromosomes. More precisely, with special sections at their ends - telomeres. Throughout life, telomeres in humans decrease. And when they become very short, the cells stop dividing and begin to age. Scientists studied almost five hundred bats of four species from 6 to 25 years. And they found out that in animals of the genus bat, telomeres do not shorten. This is due to the SETX and ATM genes, which are associated with the repair of damaged DNA sections. "Bats will help us find the molecular mechanisms of healthy aging," says lead author Emma Teeling of University College Dublin, Ireland.
Scientists decided to investigate what happens to their chromosomes. More precisely, with special sections at their ends - telomeres. Throughout life, telomeres in humans decrease. And when they become very short, the cells stop dividing and begin to age. Scientists studied almost five hundred bats of four species from 6 to 25 years. And they found out that in animals of the genus bat, telomeres do not shorten. This is due to the SETX and ATM genes, which are associated with the repair of damaged DNA sections. "Bats will help us find the molecular mechanisms of healthy aging," says lead author Emma Teeling of University College Dublin, Ireland.
Reproductology
Cells mature
Photo: BSIP / UIG via Getty Images
Biologists from the University of Edinburgh (UK) have grown in vitro mature human eggs - the same as those that are released from the ovaries during ovulation. For this, progenitor cells from the ovaries of female volunteers were used. As well as "cocktails" of signal proteins and nutrients. These four "cocktails" are necessary for cells to sequentially go through the stages of maturation. Development in the test tube took about 20 days, twice as long as in the body. Now scientists plan to speed up the process. "We have learned to manage all stages of egg growth in the laboratory, this expands our ability to combat infertility," says researcher Evelyn Telfer. "If the regulatory authorities allow the experiment, we will try to fertilize the cells."
As well as "cocktails" of signal proteins and nutrients. These four "cocktails" are necessary for cells to sequentially go through the stages of maturation. Development in the test tube took about 20 days, twice as long as in the body. Now scientists plan to speed up the process. "We have learned to manage all stages of egg growth in the laboratory, this expands our ability to combat infertility," says researcher Evelyn Telfer. "If the regulatory authorities allow the experiment, we will try to fertilize the cells."
Immunology
Wedge wedge
Photo: Depositphotos / PhotoXPress.ru
Cow's milk can cope with an allergy to cow's milk. This paradoxical conclusion was made by scientists from the Messerli Research Center (Italy). They studied the effect of allergen proteins from milk on patients with gastric upset, dermatitis and inflammation of the mucous membranes. It turns out that this can be avoided if the cow eats a lot of green grass. Together with the grass, the cow gets a lot of vitamin A. The body breaks down this vitamin and produces retinoic acid. This acid combines with one of the main allergen proteins in milk, beta-lactoglobulin. And in this form, for some reason, it does not cause an allergic reaction in people. This discovery can reduce the allergic reaction or even get rid of it not only for children, but also for adults who have not allowed themselves cow's milk products for decades.
Together with the grass, the cow gets a lot of vitamin A. The body breaks down this vitamin and produces retinoic acid. This acid combines with one of the main allergen proteins in milk, beta-lactoglobulin. And in this form, for some reason, it does not cause an allergic reaction in people. This discovery can reduce the allergic reaction or even get rid of it not only for children, but also for adults who have not allowed themselves cow's milk products for decades.
Epidemiology
Antivirus lamp
Physicists from Columbia University (USA) have created a harmless ultraviolet lamp. It can be turned on in any crowded place and will kill flu viruses and other germs without affecting people. Typically, germicidal lamps are used to treat empty spaces (people can only be in protective glasses, since such lamps usually operate at a wavelength of 254 nanometers, which can damage the eyes). The new lamps operate at a wavelength of 222 nanometers, which cannot penetrate into living human cells.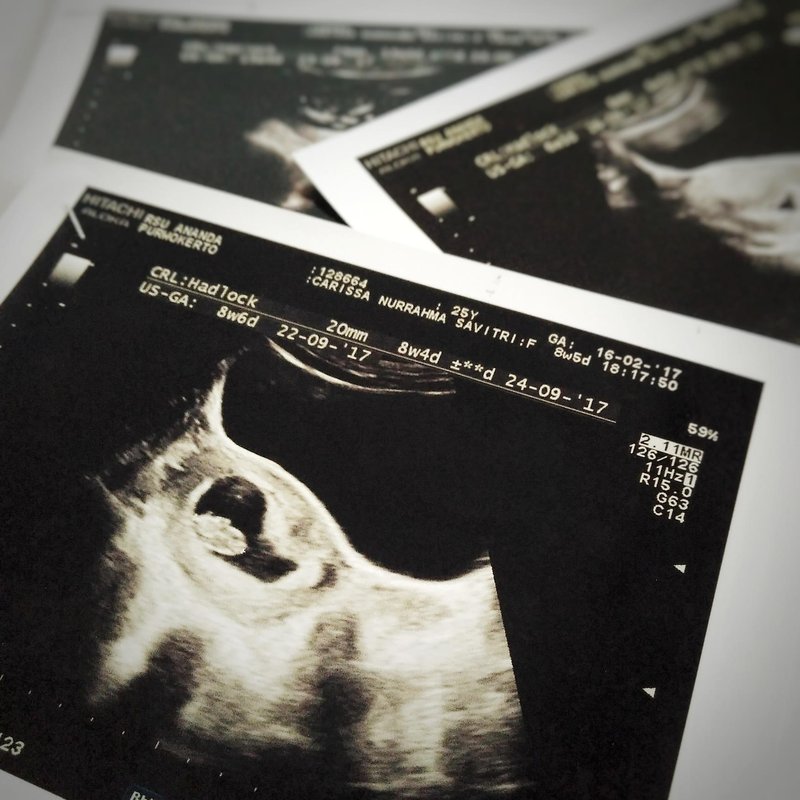 "Viruses and bacteria are much smaller, so this kind of ultraviolet light can reach and destroy their DNA," explains co-author David Brenner. Experience has shown: such lamps kill 99 percent viruses.
"Viruses and bacteria are much smaller, so this kind of ultraviolet light can reach and destroy their DNA," explains co-author David Brenner. Experience has shown: such lamps kill 99 percent viruses.
Psychology
Dusk dulls
Dim light impairs memory, researchers at Michigan State University (USA) believe after an experiment with mice. They kept one group of rodents for four weeks under 1000 lux lighting (corresponding to a cloudy day). The other is at 50 (similar to dim lights in a bathroom or toilet). As a result, the hippocampus, one of the main centers of memory and orientation, began to work poorly in rodents from the second group. In it, the formation of new neural connections necessary for memorization slowed down by 30 percent, mice began to orient themselves worse. Scientists suggest that the changes are due to a lack of a protein called neurotrophic growth factor. Lack of light slows down protein synthesis, and the brain loses its ability to remember and learn. Interestingly, under normal light, mice eventually began to navigate normally again in space.
Technology
Without scars
Medical "bandages" for burns were created by employees of NUST MISIS (Russia). They do not need to be removed: they dissolve themselves. But most importantly, they help skin regeneration without scarring. The new material is based on polycaprolactone nanofibers. This biodegradable polymer is used in medicine, for example as a suture material. For an antibacterial effect, silver particles and antibiotics were applied to the fibers, and to restore the skin, blood plasma with an increased content of platelets was added to the tissue (they secrete substances that stimulate cell growth). As a result, new skin cells should appear at the site of the burns, and not scar tissue, as is usually the case. “With the help of chemical bonds, it was possible to create a stable layer containing blood plasma components,” says researcher Elizaveta Permyakova. Experiments with cell cultures showed that therapeutic dressings doubled the growth of cells.
Experiments with cell cultures showed that therapeutic dressings doubled the growth of cells.
Statistics
Influenza attacks
By mid-February, Rospotrebnadzor noted outbreaks of influenza and SARS in 11 regions. Of the 5,200 people who were examined on February 7-14, over 500 are influenza carriers. Children are most often ill: the weekly epidemiological threshold among schoolchildren aged 7-14 has been exceeded in 11 regions of the Russian Federation. Outbreaks among adults were detected only in three subjects of the Federation.
Here are the viruses that were detected in patients from the surveyed group:
influenza-29.4%
Paragrippe viruses-8%
Adenovirus-11%
Respiratory-syncitial viruses-28%
Other viures of Negroppoose etiology-23.6% 9000
Source: Rospotranszor supervisor
ᐈ Preservation of reproductive health - Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
More details
More about hormones or the list of must-haves for week
Read more
Visit to the urologist. For or Against?
For or Against?
Read more
Preservation of reproductive health
Read more
Pregnancy with uterine fibroids
more
Read more
Varicocele and impaired spermatogenesis
More details
Secretory and obstructive infertility in men
More details
Protocols for controlled ovarian stimulation (COS)
More details
Miscarriage. What is the reason?
Read more
Hysteroscopy and its role in the treatment of infertility
Read more
Why you can’t get pregnant
Read more
How to calculate the sex of a child before conception
Read more
Obtainability of the fallopian tubes
Read more
ovarian hypermostation syndrome: a modern view of the problem
more
Pregnancy with endometriosis - modern view
Read more
Immunological infertility and the role of anti -permal antibodies in it 9000,
Details
9000 9000 9000 9000 9000 9000 9000 9000 9000 uterus?Read more
Natural cycle IVF: pros and cons
Read more
Practical skills in examining infertile couples
Read more
Artificial insemination
Read more
Laser removal of scars and scars, skin whitening.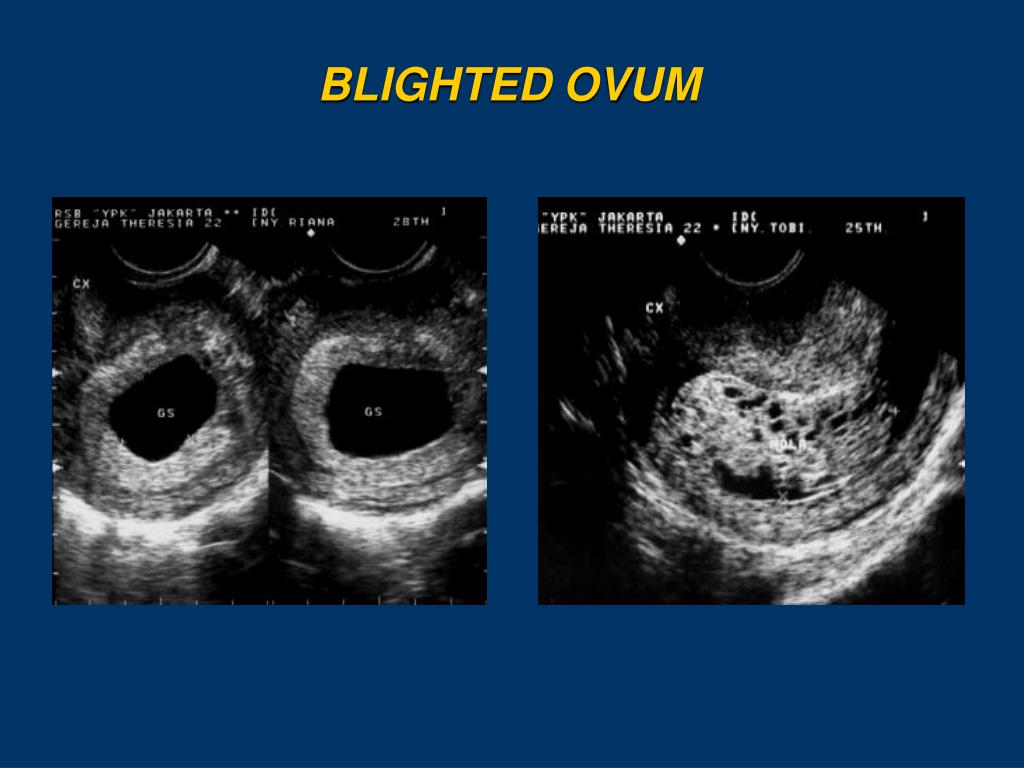
Read more
Unable to get pregnant. Where to run? Where to begin?
Read more
What future parents need to know (most popular questions)
Read more
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
More
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
More details
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
More details
Infertility and cancer: why men should definitely visit a reproductive specialist
More details
Sex, children, rock-roll about what can increase the chances of IVF
More
Portrait of a female doctor: 5 signs of a good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never. Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
More details
How to plan health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
Read more
Threatened miscarriage
Read more
Reproductive health of teenage girls: what children and their parents need to know
Read more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth - pledge of happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More
Maxim Gapchuk in "Mother and Child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
IVF: modern methods and approaches in the treatment of female infertility
Read more
ICSI: male infertility is not a sentence
Read more
Laparoscopy: Advantages over traditional surgery
Read more
Office of the uterus: What do you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: The essence of the method, stages and results of
Read more
Details in men
Details reasons for a man to visit an andrologist
More details
Cryotechnologies as a way of family planning
More details
How to become a mother: psychological and physical preparation
More details
Monalisa Touch — what is this technology
More details
Premature menopause in men: how to recognize and what is dangerous
More details
Why go to a gynecologist07
Read more
Laser therapy in gynecology: without anesthesia and pain
Learn more
Outpatient gynecology - timely access to qualified help
7
Read more
Pregnancy after 35: why additional tests and examinations are needed
Read more
Causes and prevention of female infertility
Read more
One-day surgery: a modern approach to treatment
Keeping a child healthy and healthy
Read more well-being of the motherRead more
Pregnancy after IVF: what future parents need to remember
Read more
Anomalies of the uterus and their influence on the onset and bearing of pregnancy.