What is safe to take for headaches while pregnant
Headache and migraine remedies that are safe during pregnancy | Your Pregnancy Matters
Occasional, mild headaches during pregnancy usually are nothing to worry about.Most women deal with headaches at some point in their lives. Data from the Centers for Disease Control and Prevention suggest that one in five women had a severe acute headache or migraine in the previous three months. Additionally, migraines are more common in women than men – approximately 18 percent of women have them compared to 6.5 percent of men.
Because headaches and migraines are so common, it’s probably no surprise that many women deal with them during pregnancy. For the majority of pregnant women, occasional headaches or migraines are no cause for alarm, and most standard treatments are safe. However, suffering a severe headache at key times during or after pregnancy can indicate a serious medical emergency.
Common types of headaches and treatment options
Primary headaches
Primary or acute headaches arise once in a while and typically pass after a few hours. Tension headaches are the most common type and are characterized by muscle tightness and localized pain in the head and neck.
Primary headaches in pregnant women usually can be treated at home. Rest, a neck or scalp massage, hot or cold packs, and over-the-counter anti-inflammatory drugs such as Tylenol, aspirin, or ibuprofen can reduce the pain. However, if you start to have frequent or severe headaches, talk to your doctor to determine the cause.
Migraines
Migraines tend to be episodic (frequent and long-lasting) and typically cause additional neurological symptoms, such as:
● Blurred or tunnel vision
● Hallucinations
● Light sensitivity
● Nausea and vomiting
Studies have shown that migraines can be triggered by hormonal changes, including right before your period or as a result of taking oral contraceptives. Interestingly, some women who have migraines find that the frequency or intensity of their symptoms decreases during pregnancy. Research does not suggest, however, that pregnancy triggers the onset of migraines – if you have your first migraine during pregnancy, it’s likely coincidental.
Interestingly, some women who have migraines find that the frequency or intensity of their symptoms decreases during pregnancy. Research does not suggest, however, that pregnancy triggers the onset of migraines – if you have your first migraine during pregnancy, it’s likely coincidental.
Treatment during pregnancy is fairly similar to standard treatment. Anti-inflammatory drugs are generally safe and effective during pregnancy when used in a limited manner. Midrin is a commonly prescribed headache medication that contains acetaminophen along with a mild sedative. Midrin also has vasoconstrictive properties, which means it narrows the blood vessels, thereby reducing blood flow and pain.
Sumatriptan, commonly known as Imitrex, is another medication that reduces blood flow to the brain. It works best to stop a migraine if it’s taken as soon as symptoms present. Most nausea medications prescribed to women with migraines are safe to use during pregnancy, but I suggest reviewing the medications you take for migraine relief with your obstetrician at your first prenatal visit, just to be safe.
Certain drugs called ergotamines have a stronger vasoconstrictive effect and can adversely affect fetal growth. They also can stimulate uterine activity. Because of this, they absolutely should not be used during pregnancy.
Severe migraines might require hospitalization so you can receive fluids, pain medication, or anti-nausea medication through an IV if you are unable to keep medications down.
"Most women don’t require special care for headaches and migraines during pregnancy, and most standard remedies are safe. However, certain types of headaches require immediate medical attention to avoid potentially harmful health issues."
– Robyn Horsager-Boehrer, M.D.
When headaches are secondary to other problems
Headaches can result from other conditions, some of which are life-threatening:
● Stroke: Sudden and severe headaches might be a sign of a stroke. Women who have strokes during pregnancy or after delivery typically describe the pain as the worst headache of their lives. They also might report other symptoms, such as speech problems, vision issues, or functional problems on one side of the face or body. At the emergency room, the doctor will evaluate you for stroke symptoms, such as visual changes, facial drooping, and arm or leg weakness. If you are having or had a stroke, we will get you emergency treatment at our Advanced Comprehensive Stroke Center.
Women who have strokes during pregnancy or after delivery typically describe the pain as the worst headache of their lives. They also might report other symptoms, such as speech problems, vision issues, or functional problems on one side of the face or body. At the emergency room, the doctor will evaluate you for stroke symptoms, such as visual changes, facial drooping, and arm or leg weakness. If you are having or had a stroke, we will get you emergency treatment at our Advanced Comprehensive Stroke Center.
● Preeclampsia: A headache with preeclampsia (a pregnancy complication characterized by high blood pressure) can indicate a dangerous spike in blood pressure. The doctor will assess you and might admit you to the hospital for management of blood pressure and treatment to prevent seizures.
● Spinal fluid leak: A headache after an epidural or spinal block can indicate a spinal fluid leak, especially if it worsens when you sit or stand up. The most effective treatment is an epidural blood patch, in which the doctor injects a sample of your blood into the leaking area, essentially plugging the hole. This therapy provides dramatic relief right away.
This therapy provides dramatic relief right away.
Occasional mild headaches are common in women. The vast majority are no cause for alarm and can be treated at home, with guidance from your doctor. However, if your symptoms are severe or something just doesn’t seem right, it’s much better to seek care and be safe rather than sorry.
Stay on top of health care news. Subscribe to our blog today.
Migraine & Pregnancy Headache Relief
Headache and migraines commonly affect pregnant women, often during the first trimester. An expert shares treatments to try and when to call your doctor.
Pregnancy is a crucial time of life — a time when the expectant mother wants to make sure that she is taking care of herself and that everything is going well.
SEE ALSO: 3 Reasons Women Are More Likely to Have Insomnia
Unfortunately, frequent or severe headaches can waylay these plans for many mothers-to-be. Here, neurologist and headache specialist Lauren A. Aymen, D.O., shares the medications, supplements, treatments and symptomatic red flags pregnant women should watch for.
Aymen, D.O., shares the medications, supplements, treatments and symptomatic red flags pregnant women should watch for.
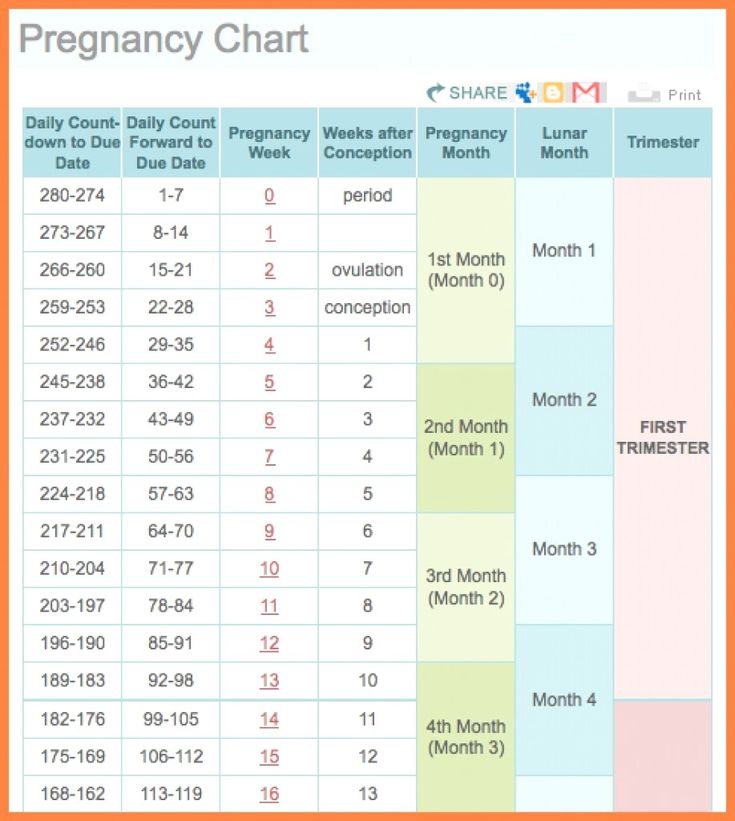
Aymen: Yes. Migraines are usually worse in the first trimester but can improve during the second and third trimester. Unfortunately, in 4 to 8 percent of women, migraines can worsen. Headache frequency typically returns back to the patient’s pre-pregnancy baseline after delivery.
What’s the reason for this?Aymen: Pregnancy usually brings with it hormonal changes, stress, disrupted sleep, nausea and dehydration. And all of these conditions may worsen migraine in pregnancy.
What can be done for pregnant women who have migraines?Aymen: You can’t use most of the over-the-counter (OTC) medications during pregnancy — with the exception of Tylenol (acetaminophen). Magnesium and riboflavin are OTC supplements that are safe and can be effective as well.
Unfortunately, there are few prescription headache medications that are safe to use during pregnancy.
However, there are certain procedures that are safe during pregnancy that can aid in preventing and stopping migraines. For instance, we commonly use nerve blocks to reduce the frequency and severity of headaches. One example is an occipital nerve block, which is very effective at reducing the burden of pain during pregnancy.
SEE ALSO: The Best OTC Meds and Supplements to Treat Headache
There is also a new procedure called a sphenopalatine ganglion nerve block, which involves placing a small rubber tube approximately 4 centimeters (about 1 1/2 inches) into each nostril and delivering medication to the sphenopalatine ganglion, a branch of the facial nerve. This is very effective for patients with frontal or retro-orbital head pain and certain facial pain syndromes. One advantage to this procedure is there are no needles involved, so it’s minimally invasive. In addition, the medication we use in both procedures acts locally and does not have systemic side effects.
In addition, the medication we use in both procedures acts locally and does not have systemic side effects.
If effective, these procedures can be repeated during pregnancy without any known risk to the baby.
Can a headache be a sign of something more serious?Aymen: Yes. A headache with any of the following symptoms — if you’re pregnant or not — could suggest something more serious.
The red flags include:
More Articles About:
Headache
,
Pregnancy
,
Pain Management
,
Neurological (Brain) Conditions
,
90,000 which doctor to contact and how to treat correctly?- Home
- >Pregnancy
Of course, migraine or chronic tension headache is not a contraindication to pregnancy. And almost every woman, regardless of the presence of any chronic diseases, wants to become a mother. However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
- migraine,
- headache,
- panic attacks and anxiety during pregnancy,
- insomnia,
- attacks of vegetovascular dystonia during pregnancy,
- pain in the neck, back, lower back during pregnancy, 9003 diseases during pregnancy.

Pregnancy and breastfeeding has many restrictions in taking medicines. However, some schemes for taking drugs to relieve headaches and migraines during pregnancy still exist. It is better to clarify and select them in advance together with the attending physician, and also to develop a clear algorithm of actions in case of an impending attack. Enduring pain during pregnancy with migraine is still not recommended, with the exception of the first trimester and the last weeks of the third trimester. But most importantly, non-drug methods of relieving headaches come to the aid of pregnant women, such as:
- biofeedback therapy,
- manual therapy,
- massage,
- acupuncture,
- psychotherapy.
botulinum therapy - prevention of migraine and headache during pregnancy
The most interesting and promising method of treating headache during pregnancy and migraine is botulinum therapy. The essence of this method is prevention.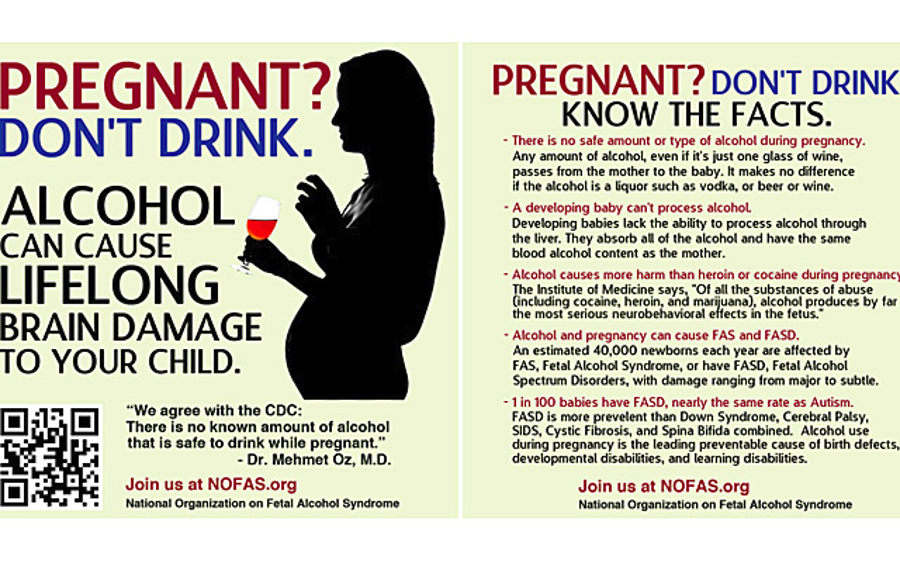 Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Authorized medicines for migraine and headaches
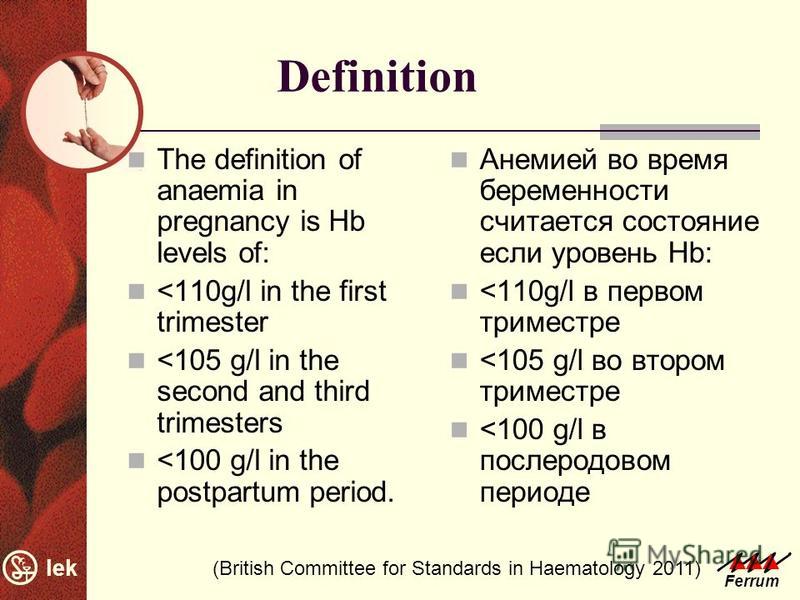
Still, migraines and headaches often take pregnant women by surprise. What painkillers are still allowed for pregnant women? During the entire period of pregnancy, you can take paracetamol at a dose of 325-500 mg up to 4 times a day. Caffeine is also allowed. So, you can drink migraine, panadol extra or solpadein fast. Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
DRUGS FOR MIGRAINES AND HEADACHES IN PREGNANCY
There are drugs that are strictly prohibited during pregnancy. These are painkillers with phenobarbital, codeine, old tranquilizers like phenazepam and ergotamines.
Headache and migraine treatment during pregnancy
Dear expectant mothers! If you suffer from migraines, chronic headaches or other types of pain syndrome, experience a feeling of constant anxiety, panic attacks, we invite you to spend your pregnancy under the supervision of our specialists! Our doctors have harmless, but effective methods of treatment. We are ready to provide specialized medical care in one of the most crucial periods in a woman's life!
We are ready to provide specialized medical care in one of the most crucial periods in a woman's life!
-
Naprienko Margarita Valentinovna
Chief physician, doctor of medical sciences, professor, neurologist of the highest category -
Ekusheva Evgenia Viktorovna
,0004
Neurologist, Doctor of Medical Sciences, Professor -
Latysheva Nina Vladimirovna 9000.
-
Oransky Alexander Vladimirovich
Manual therapist, reflexologist, candidate of medical sciences
- Panic attacks in pregnancy and children
- Migraine with aura
- Migraine in women
- Headache and migraine during lactation
- Panic attacks and VSD during pregnancy
- Pain in the lower back, neck, back during pregnancy Non-drug treatment and migraines ONLINE
- Monoclonal antibodies - preparations Irinex and Ajovi
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, since:
However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, since:
-
drugs approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell you about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman during the entire period of pregnancy and after childbirth too.
How to manage migraines during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink plenty of fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations.
 This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make attacks less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods. Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfering with your life, then under the supervision of a specialist, you can resort to drug therapy.

PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted. However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.