Can type 1 diabetes go away
Type 1 Diabetes Cure - DRIF
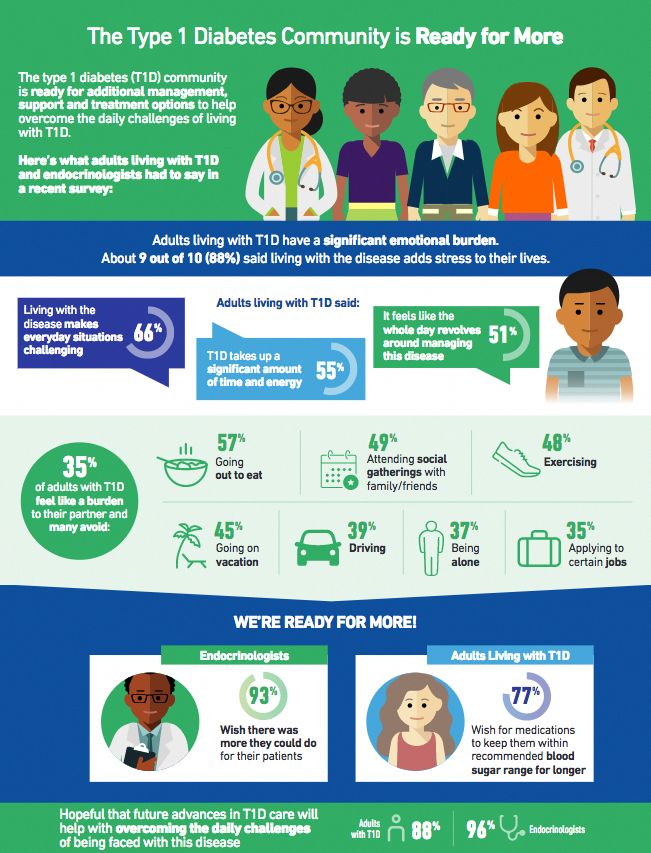
One of the first things people ask when they’ve been diagnosed with type 1 diabetes is: is there a cure? The truth is, while type 1 diabetes can be managed with insulin, diet and exercise, there is currently no cure. However, researchers with the Diabetes Research Institute are now working on treatments to reverse the disease, so that people with type 1 diabetes can live healthy lives without medication.
What is type 1 diabetes?
With type 1 diabetes, your pancreas stops making insulin, a hormone that helps the body convert blood sugar into energy. Without insulin, sugar builds up in the blood and can damage your internal organs, including your heart, kidneys, eyes, nervous system, and other parts of the body. This can lead to serious or life-threatening complications over time.
Type 1 diabetes is not caused by a person’s diet or lifestyle. It is an autoimmune disorder, where the body’s immune system mistakenly attacks and destroys healthy cells in the pancreas. While it’s most commonly diagnosed in children and young adults, people can develop type 1 diabetes at any age.
How close are we to a cure?
For a century, treatment for type 1 diabetes has focused on managing the disease. Thanks to past advancements in medicine, patients are able to control their blood glucose levels with regular insulin injections or an insulin pump.
Now clinical trials are underway for treatments to reverse type 1 diabetes and restore the body’s ability to produce insulin naturally. These trials are already allowing some patients to live insulin-free, significantly improving their quality of life.
What is a biological cure?
DRI researchers are working toward a biological cure for type 1 diabetes. A biological cure means treatment that would help the body start producing its own insulin again, restoring blood sugars to normal levels without introducing other risks.
This research focuses on a process called islet transplantation. Islets are clusters of cells found in the pancreas that work together to regulate blood sugar. In an islet transplant, doctors take healthy islets from the pancreas of an organ donor, and inject them into someone with type 1 diabetes. In studies, some patients who had this procedure have been able to reduce the need for insulin injections, or stop injecting insulin altogether.
Islets are clusters of cells found in the pancreas that work together to regulate blood sugar. In an islet transplant, doctors take healthy islets from the pancreas of an organ donor, and inject them into someone with type 1 diabetes. In studies, some patients who had this procedure have been able to reduce the need for insulin injections, or stop injecting insulin altogether.
DRI scientists have already shown that islet transplantation can eliminate the need for insulin injections. Now they are working to improve the science so that more people can benefit from this treatment.
The BioHub Strategy
DRI’s BioHub strategy is a three-step approach to overcoming the current limitations of islet transplantation.
First, scientists focus on the transplant site. While the liver is the traditional site for islet transplantation, this location is not ideal. Scientists are investigating other possible transplant sites and options, including a bio-engineered platform that acts as an artificial pancreas.
Second, they are looking for ways to sustain the islets’ long-term survival and protecting them from the autoimmune attack that caused the type 1 diabetes in the first place. Some options include creating barriers to protect the cells, or adding oxygen or other agents to the transplant site.
Finally, researchers are investigating how to increase the supply of islets available for transplant. This could include finding a method to regenerate a patient’s own pancreatic cells, so cells don’t have to be taken from a donor.
Research Progress
Research has come a long way since the first islet transplant in a human was performed in 1985. Recent work by DRI scientists has included the discovery of pancreatic stem cells that can be stimulated to create insulin-producing beta cells, and a study that demonstrated that abdominal tissue called the omentum could work as a transplant site. And in 2019, a study by DRI scientists showed that a small group of patients who received islet transplants had been able to live without insulin injections for 10 years, while maintaining blood sugar levels that were in the same range as people who had never had type 1 diabetes.
Clinical Trials
A clinical trial is a study that takes treatments that have been developed in lab and pre-clinical research, and tests them in human patients. DRI scientists have a number of clinical trials currently underway, including an islet transplant study that is testing the omentum as an alternative transplant site to the liver. Other ongoing clinical trials include the POSEIDON Trial, which tests whether high doses of vitamin D and Omega-3 fatty acids can help slow or stop the progression of type 1 diabetes in newly diagnosed children and adults.
While past studies have shown that islet transplantation can reduce or eliminate the need for patients to inject insulin, so far this treatment has only been available to people with the most severe cases of type 1 diabetes. At the Diabetes Research Institute, we have one goal: a cure. With more research, our goal is to effectively reverse type 1 diabetes, restoring the body’s ability to normalize blood sugar levels naturally.
What Is Type 1 Diabetes? (for Parents)
If your child has been diagnosed with type 1 diabetes, you probably have questions. Here are the basics.
What Is Type 1 Diabetes?
People who have type 1 diabetes can’t use glucose (the body’s main type of sugar) for energy. That’s because their body stopped making the hormone insulin. Normally, after we eat, the amount of glucose in the blood (blood sugar) goes up. When it does, the pancreas sends insulin into the blood. Insulin works like a key that opens the doors of the body’s cells to let the glucose in, giving the cells the energy they need.
In type 1 diabetes, the pancreas doesn’t make insulin. Without insulin, glucose can't get into the cells. It stays in the blood, which leads to high blood sugar. Having too much sugar in the blood isn’t healthy and can cause problems. Some problems happen quickly and need treatment right away, while others develop over time and show up later in life.
What Happens in Type 1 Diabetes?
In type 1 diabetes, the body's immune system attacks and destroys the cells in the pancreas that make insulin. So the body can’t make insulin anymore.
So the body can’t make insulin anymore.
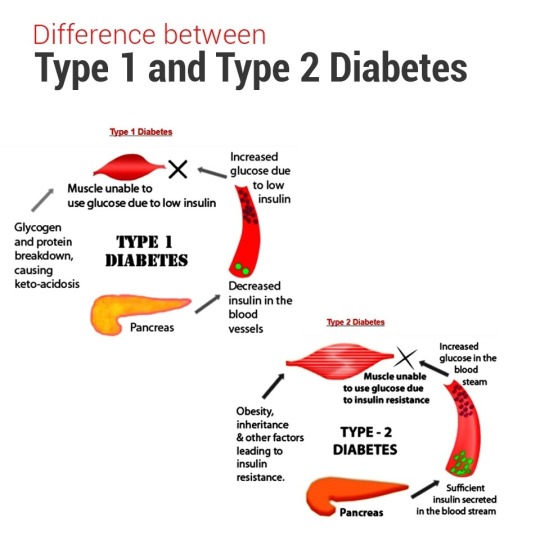
This is different from type 2 diabetes, where the body still makes insulin, but the insulin doesn’t work as it should.
Why Do Some People Get Type 1 Diabetes?
No one knows for sure why some people get type 1 diabetes. Doctors and scientists think a person’s genes make them more likely to get it. But just having the genes for diabetes probably isn't enough. It’s likely that something else needs to happen. Scientists are studying if other things — like some viral infections, a person’s birth weight, or their diet — might make someone who already has the genes for type 1 diabetes more likely to get it.
Type 1 diabetes can’t be prevented, and can happen in people of any age.
What Are the Signs & Symptoms of Type 1 Diabetes?
Type 1 diabetes can come on over time or suddenly. Sometimes, kids don’t have diabetes symptoms yet and the condition is discovered when blood or urine tests are done for another reason.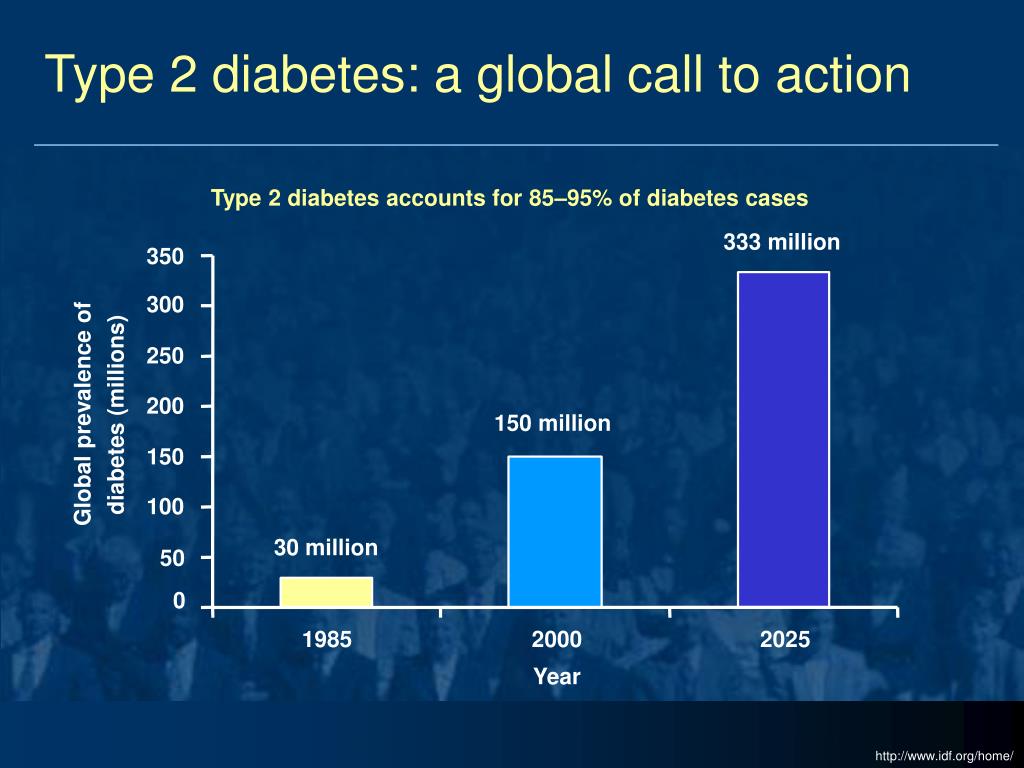 Kids who show symptoms may:
Kids who show symptoms may:
- need to pee a lot
- start to wet the bed after having been dry at night
- be thirstier and drink more than usual
- feel tired often
- lose weight
How Is Type 1 Diabetes Diagnosed?
Doctors use a blood test that measures the amount of sugar (glucose) in the blood. High blood sugars show that a child has diabetes. Then, the doctor will do more blood tests to find out what type it is.
Kids with type 1 diabetes often go to a pediatric endocrinologist. This kind of doctor finds and treats problems affecting hormones, like diabetes.
How Is Type 1 Diabetes Treated?
Type 1 diabetes needs lifelong treatment because there is no cure yet. Doctors treat type 1 diabetes using a diabetes care plan. The care plan tells you and your child the things to do every day to help keep blood sugar levels in a healthy range.
Each child’s diabetes care plan is made just for them. But all plans have the same 4 basic parts:
- take insulin (by injection or an insulin pump)
- eat a healthy, balanced diet that includes counting carbohydrates
- check blood sugar levels at least 4 times a day
- get regular physical activity
Following the diabetes care plan helps kids stay healthy, now and into the future.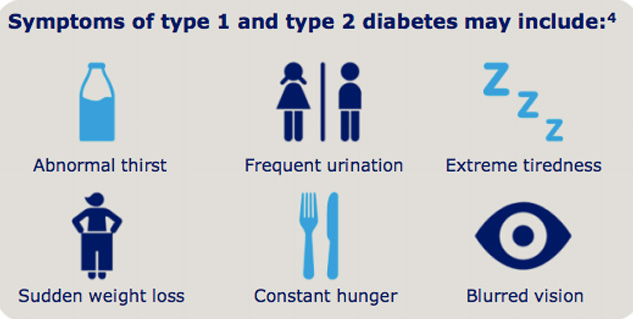
What Problems Can Happen With Type 1 Diabetes?
Not having the right amount of sugar in the blood can lead to:
- hyperglycemia: This is when blood sugars are too high. Kids with hyperglycemia may be extra thirsty, pee more than usual, and lose weight. High blood sugars can be treated. If they aren’t, kids can develop health issues later in life.
- diabetic ketoacidosis (DKA): This serious condition needs treatment right away. When there’s not enough insulin in the body to let the glucose into the cells, the body starts to break down fat instead of sugar. Symptoms of DKA can include nausea, vomiting, belly pain, fast breathing, and, in severe cases, unconsciousness.
- hypoglycemia: This is when blood sugars are too low and can sometime happen when people are being treated for diabetes. Symptoms can include headache, weakness, shakiness, anxiety, and sweating.
- growth and development problems: Some kids might grow slower than their peers or start puberty (when kids start growing into adults) later than usual.
How Can Parents Help?
Now is the perfect time to help your child to create healthy habits for life. Here’s how:
- Get involved with daily care. Help your child put their care plan into action every day. From counting carbs, to calculating insulin doses, and giving injections, there’s a lot to learn at first. Share the responsibilities with your child. Over time, they’ll be able to take on more on their own. Turn to your child’s care team with any questions about the care plan or daily care.
- Learn all you can about diabetes. The more you know about type 1 diabetes, the more confident you’ll feel about helping your child manage it day to day. And a solid understanding of diabetes lets you advocate for your child. You can share your knowledge with important people in your child’s life, like grandparents, teachers, coaches, and babysitters. Doing so helps you build a community of support for your child.
- Encourage your child.
 It can take a while to adjust to the new responsibilities that come with type 1 diabetes. Remind your child that many kids their age have type 1 diabetes, and they follow a similar care plan. If your child has concerns that you’re not sure how to handle, ask the care team. They’ll connect you with the right resources.
It can take a while to adjust to the new responsibilities that come with type 1 diabetes. Remind your child that many kids their age have type 1 diabetes, and they follow a similar care plan. If your child has concerns that you’re not sure how to handle, ask the care team. They’ll connect you with the right resources.
Having a child with type 1 diabetes may seem overwhelming at times, but you're not alone. If you have questions or problems, reach out to your child’s diabetes care team — they can help with all kinds of issues, and will guide your family through this journey.
You also can learn more about type 1 diabetes online:
- The Juvenile Diabetes Research Foundation (JDRF)
- CDC: Type 1 Diabetes
- BeyondType1
Reviewed by: Cheryl Patterson, RD, CDE
Date reviewed: September 2021
treatment and diagnostics in Moscow
What is it
Diabetes mellitus is an extremely common chronic disease, ranking third among the leading causes of death: after cardiovascular disease and cancer.
Sugar (it is more correct to call it "glucose") is necessary for our body as a source of energy. Glucose enters the body with food and is absorbed in the intestines, and is also produced by the liver on an empty stomach. Insulin is an important hormone produced by the pancreas and is responsible for transporting glucose from the blood into cells. Cells, in turn, convert glucose into energy. Insulin also regulates the production of glucose by the liver.
The disease is divided into the first and second types.
In type 2 diabetes mellitus the cells of the body are less sensitive to insulin, so they do not take in the glucose they can tolerate and it remains in excess in the blood. Or, due to some reason, insulin ceases to effectively regulate the production of glucose by the liver, so blood sugar levels increase.
In insulin dependent type 1 diabetes own immunity destroys the cells of the pancreas responsible for the production of insulin.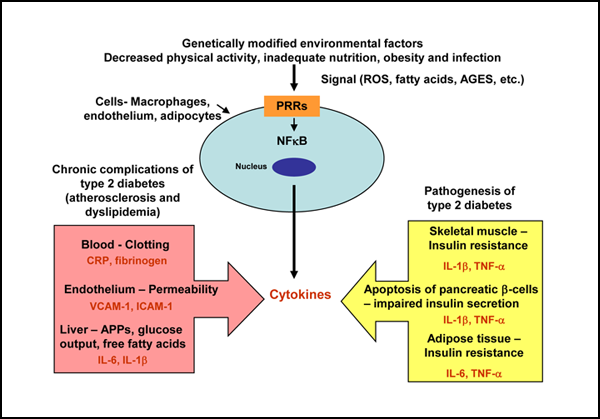 Thus, insulin does not enter the bloodstream and does not transfer glucose into the cells, which remains in the blood. This condition requires the introduction of insulin into the body by injection, which is why the first type is called insulin-dependent diabetes mellitus.
Thus, insulin does not enter the bloodstream and does not transfer glucose into the cells, which remains in the blood. This condition requires the introduction of insulin into the body by injection, which is why the first type is called insulin-dependent diabetes mellitus.
Causes of type 1 diabetes
Insulin-dependent type 1 diabetes refers to autoimmune diseases, i.e. to those caused by an aggressive reaction of the immune system in relation to the body's own cells. Unfortunately, the reasons for this reaction are still unknown.
Most scientists tend to genetic predisposition and transmission of the disease by inheritance. There is also an assumption about the viral component: at risk are people who have had serious viral infections against the background of a genetic predisposition to diabetes.
Most often, insulin-dependent type 1 diabetes manifests itself already in childhood or adolescence, less often in adulthood. Diabetic coma is an extreme manifestation of an untreated disease, because about half of patients do not know about their disease until the first serious complications appear.
Type 1 diabetes symptoms
Late diagnoses and complications are a consequence of the fact that the first symptoms are often overlooked.
Among the main first symptoms can be listed:
- feeling of dry mouth,
- constant thirst,
- frequent urination,
- sleep disorders due to frequent urge to urinate,
- general weakness, lethargy, fatigue,
- weight loss,
- blurred vision.
One of the frequent complications of insulin-dependent type 1 diabetes - ketoacytosis - is an attempt by the body to make up for the lack of energy (after all, glucose is not absorbed) by burning fat, which releases ketone bodies.
The presence of a large amount of ketone bodies in the blood is toxic and manifests itself with the following symptoms:
- smell of acetone from the mouth,
- dizziness,
- vomiting,
- abdominal pain,
- palpitations,
- loss of consciousness,
- coma.

Often, a doctor is consulted only after the first symptoms of ketoacytosis appear, and this complication is life-threatening. Therefore, it is important to know and monitor the appearance of the primary symptoms of type 1 diabetes in yourself or your loved ones, especially children.
Diagnostics
To make a diagnosis, an endocrinologist will first need a blood and urine test, which will show the level of glucose. In addition, additional tests may be ordered. For example, analysis for HBA1C (glycosylated hemoglobin) is a rather complex study that can only be carried out in well-equipped laboratories.
The analysis will show how much glucose was in the body in the last 12 days, based on the amount of glycosylated hemoglobin in red blood cells: hemoglobin has the property of combining with glucose, becoming glycosylated. In some cases (most often for pregnant women), the doctor may recommend a glucose tolerance test, i.e.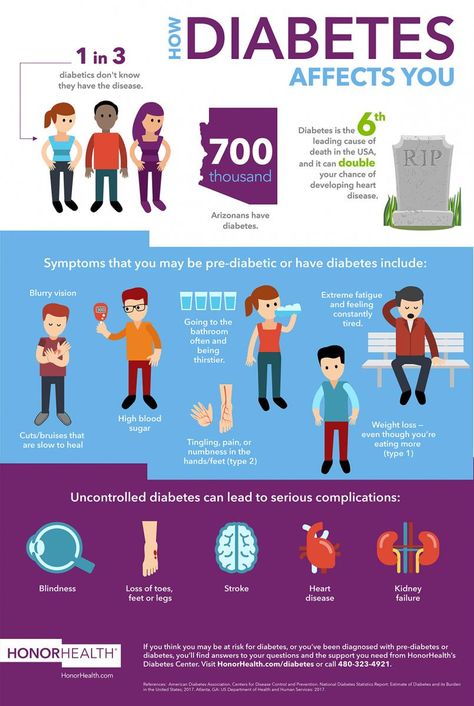 resistance of body cells to insulin.
resistance of body cells to insulin.
Thus, the diagnosis of type 1 diabetes is not difficult and is carried out in a short time. Therefore, it is extremely important for the patient to pay attention to his health and monitor the first symptoms of diabetes, to prevent serious complications due to the timely visit to a specialist.
Treatment of type 1 diabetes mellitus
Despite the fact that type 1 diabetes is a chronic disease (it is impossible to completely cure the patient), it is quite possible to turn the course of the disease into a controlled channel.
With diagnosed type 1 diabetes, in the vast majority of cases, insulin therapy is prescribed - hormone administration by injection. The injected hormone is used by the body to process the incoming glucose.
In addition to insulin therapy, depending on the patient's condition, drugs that lower blood sugar levels may be prescribed. And a diet will definitely be prescribed, because the treatment of type 1 diabetes largely depends on following the recommendations for eating habits:
- frequent, moderate meals,
- a large number of vegetables in the diet,
- refusal of fast carbohydrates,
- restriction of sweet, starchy foods.
There are many myths surrounding type 1 and type 2 diabetes. But even with such a serious illness, with a proper responsible approach, people restore the quality of their lives. It should be noted that the success of treatment also depends on the experience and qualifications of the attending physician.
It is important for the patient to learn to live with his disease, and for this the doctor must choose the most effective therapy, answer all the patient's questions, and help understand the treatment plan. This applies to diet, allowable physical activity, the correct doses of insulin, the way it is administered, as well as taking additional drugs if necessary.
At the FSCC FMBA, the management of patients with type 1 and type 2 diabetes mellitus is built on a long-term basis from early diagnosis to a stable course of the disease. Our doctors stay in touch, ready to answer all the patient's possible questions about their condition and the disease in general.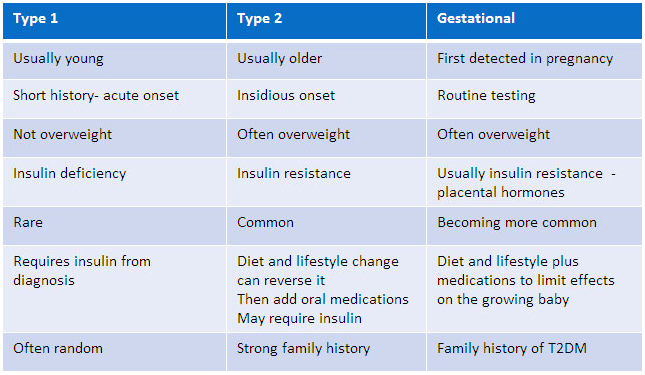
We do not insist on regular consultations, we stand for maximum trust between the patient and the attending physician for prompt correction of the treatment regimen, if necessary. In addition, the specialists of our center have developed a special program for the early diagnosis of type 1 and type 2 diabetes - Diabetes under control.
This program is recommended for anyone who has noticed mild symptoms of diabetes, or who already has close relatives. The program includes the necessary tests and consultations with specialists who will give a professional opinion on the risk of developing type 1 and type 2 diabetes. After all, like any other disease, diabetes is much more effectively controlled when detected in the early stages.
Thanks to the versatility of the center, our endocrinologists, with the help of colleagues from other departments, successfully cope with the complications and consequences of type 1 diabetes. Earlier we touched on ketoacinosis, but in addition to it, there are often cardiovascular complications associated with a change in blood density against the background of high sugar content in it: the risk of developing atherosclerosis, vision problems (due to insufficient blood supply to the organs of vision), problems with the legs (with insufficient blood supply affects the nerve endings of the lower extremities, especially the feet, up to diabetic neuropathy), kidney damage, periodontitis.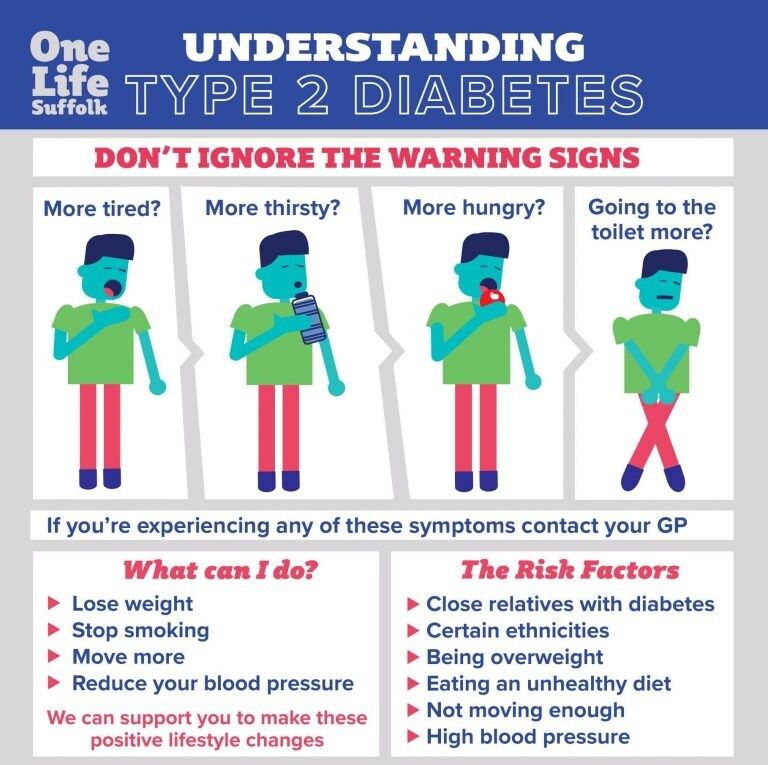
Such a wide range of complications requires complex management of the patient by several specialists, and often by several departments. But it is precisely this multifunctional approach to treatment that is bearing fruit - we offer our patients qualified medical care in one place at a convenient time for them.
You can sign up for a consultation with an endocrinologist through the form on the website or by phone.
Assess your risk of developing diabetes
Assess your risk of developing diabetes Diabetes mellitus (DM) is a chronic disease that develops when the body does not produce enough insulin or cannot use it effectively. Insulin is a hormone that regulates blood sugar levels. A common result of uncontrolled diabetes mellitus is hyperglycemia, or elevated levels of glucose (sugar) in the blood. Over time this leads to serious damage to many organs: heart, blood vessels, eyes, kidneys and nervous system. The development of type 2 diabetes is usually preceded by changes in the body, referred to as prediabetes.
The development of type 2 diabetes is usually preceded by changes in the body, referred to as prediabetes.
Signs of diabetes mellitus
5 myths
about diabetes
one
I don't like sweets, I can't have diabetes.
Reality:
The sweet name of the disease was not at all due to excessive addiction to sweets.
Diabetes mellitus is chronic disease that occurs when the pancreas produces insufficient amounts of the hormone insulin, or when the body cannot fully utilize the insulin he produces for his needs.
Precisely insulin maintains a normal level of glucose (sugar) in the blood. because of insulin deficiency, blood sugar levels rise, hyperglycemia develops.
2
If you feel well, you may not need to measure your blood glucose.
Reality:
It is necessary to regularly monitor the level of glucose in the blood, regardless of how you feel. The fact, that moderate hyperglycemia may not be felt by the patient himself, but contributes to the development of complications diabetes mellitus. Therefore, only regular measurement of glucose levels will help in a timely manner. diagnose the disease, select the required dosage of drugs, evaluate their effectiveness and monitor the diet. It is also necessary to evaluate other indicators of blood and urine.
The fact, that moderate hyperglycemia may not be felt by the patient himself, but contributes to the development of complications diabetes mellitus. Therefore, only regular measurement of glucose levels will help in a timely manner. diagnose the disease, select the required dosage of drugs, evaluate their effectiveness and monitor the diet. It is also necessary to evaluate other indicators of blood and urine.
3
Diabetes mellitus is a disease of the elderly. Young people don't get sick.
Reality:
You can get diabetes at any age, both in the young and in the more mature. Type 1 diabetes develops due to the destruction of special cells pancreas (Langerhans cells) that produce insulin. A decrease in insulin leads to an increase in the concentration of glucose in the blood. It is for this type of diabetes mellitus that the onset is characteristic diseases in childhood and adolescence.
Type 2 diabetes is more common among older adults age.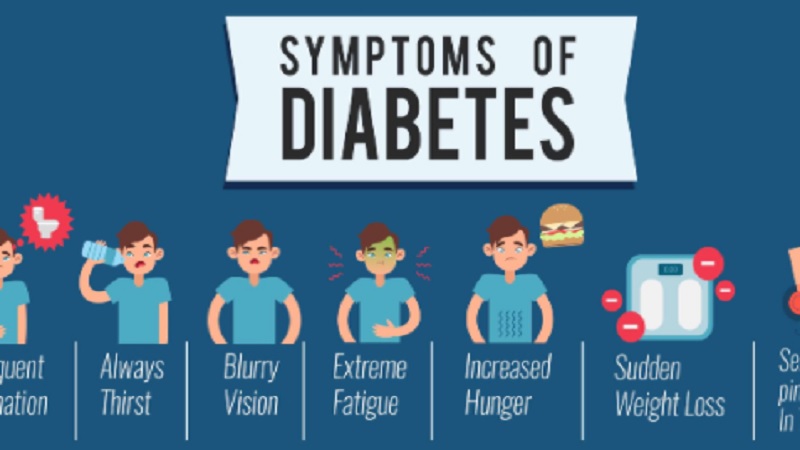 This form of the disease most often develops when there is enough insulin, but the cells of the body lose their sensitivity to its effects. And also in other conditions, most often associated with dysfunction of the pancreas and liver.
This form of the disease most often develops when there is enough insulin, but the cells of the body lose their sensitivity to its effects. And also in other conditions, most often associated with dysfunction of the pancreas and liver.
four
I was prescribed a diet and pills. If I don't need insulin injections, then I have no diabetes?
Reality:
Not always used to treat diabetes only insulin injections. For example, in type 2 diabetes mellitus, treatment may be initiated with specific diets and antidiabetic drugs in the form of tablets. But this does not mean that there is no disease or that it does not need to be controlled. In any case, it is necessary to visit a doctor, check the level of glucose and other indicators of carbohydrate metabolism. Blood sugar control will help to avoid the development of complications.
5
Diabetes is a sentence.
Reality:
If you have been diagnosed with diabetes, do not despair. On the contrary, early diagnosis of the disease and timely treatment is an important starting point. for a prosperous life. Regular administration of insulin or taking hypoglycemic drugs, timely control of glucose and other blood and urine parameters, adherence to a rational diet with restriction of simple carbohydrates, moderate physical activity and observation by an endocrinologist - all this will keep glucose levels under control, and therefore prevent and delay the onset fatal complications.
Risk assessment
for type 2 diabetes mellitus
19
Enter your gender.
- Woman
- The male
2 / 9
How old are you?
- Up to 45
- 45 to 54
- 55 to 64
- Over 65
3 / 9
What is your waist circumference (cm)?
- Up to 94
- 94 to 102
- Over 102
3 / 9
What is your waist circumference (cm)?
- Up to 80
- 80 to 88
- Over 88
4 / 9
Do you regularly exercise for more than 30 minutes a day?
- Yes
- Not
5 / 9
How often do you eat vegetables, fruits, or whole grains?
- Every day
- Not every day
6 / 9
Have you ever taken drugs to lower your blood pressure? pressure?
- Yes
- Not
7 / 9
Have you ever had high glucose (sugar) in blood?
- Yes
- Not
8 / 9
Did any of your relatives suffer from diabetes?
- Not
- Yes (grandparents, aunts/uncles, cousins)
- Yes (parents, siblings or own children)
9 / 9
Calculation of body mass index.
- Your weight, kg:
- Your height, cm:
Your risk of developing type 2 diabetes in the next 10 years is LOW
You do not need any special prophylaxis. You should continue to watch your diet and lead an active lifestyle. The likelihood of developing diabetes is 1% (only 1 person in 100 can get sick).
5
The risk of developing type 2 diabetes is SLIGHTLY INCREASED
However, if you want to be safe, you should be active, exercise daily, limit your intake of fatty and fried foods, your daily diet must include vegetables , fruits, whole grains. The likelihood of developing diabetes is 4% (4 people out of 100 can get sick).
5
Type 2 diabetes risk MODERATE
If you fall into this group, then you need to consult a specialist (your doctor or dietitian) for a more thorough assessment of risk factors for developing diabetes, receive recommendations on lifestyle changes, nutrition, etc. The probability of developing diabetes is 17 % (17 people out of 100 may get sick).
The probability of developing diabetes is 17 % (17 people out of 100 may get sick).
5
Type 2 diabetes risk HIGH
You should seek specialist advice for testing, advice on lifestyle changes, nutrition, risk factors and possibly treatment. The probability of developing diabetes is 33% (every third person can get sick).
5
The risk of developing type 2 diabetes is HIGH
You should seek the advice of a specialist for an examination, advice on lifestyle changes, nutrition, risk factors, and possibly treatment. The probability of developing diabetes is 33% (every third person can get sick).
5
Type 2 diabetes risk is VERY HIGH
You probably have type 2 diabetes. Seek help from a specialist (your doctor, dietitian, or endocrinologist) right away for an examination, advice on lifestyle changes, nutrition, risk factors, and possibly treatment.