What is the cause of leaking urine
Urinary Incontinence in Older Adults
Urinary incontinence means a person leaks urine by accident. While it can happen to anyone, urinary incontinence, also known as overactive bladder, is more common in older people, especially women. Bladder control issues can be embarrassing and cause people to avoid their normal activities. But incontinence can often be stopped or controlled.
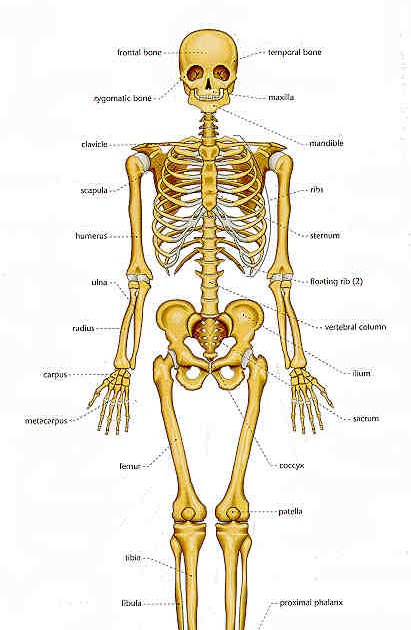
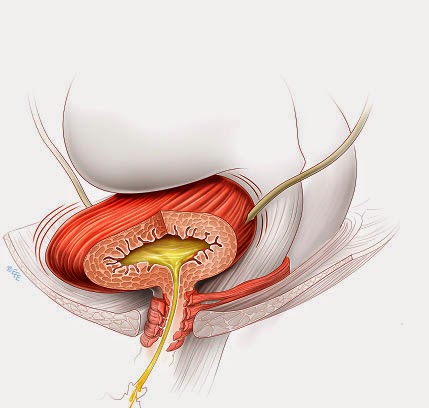
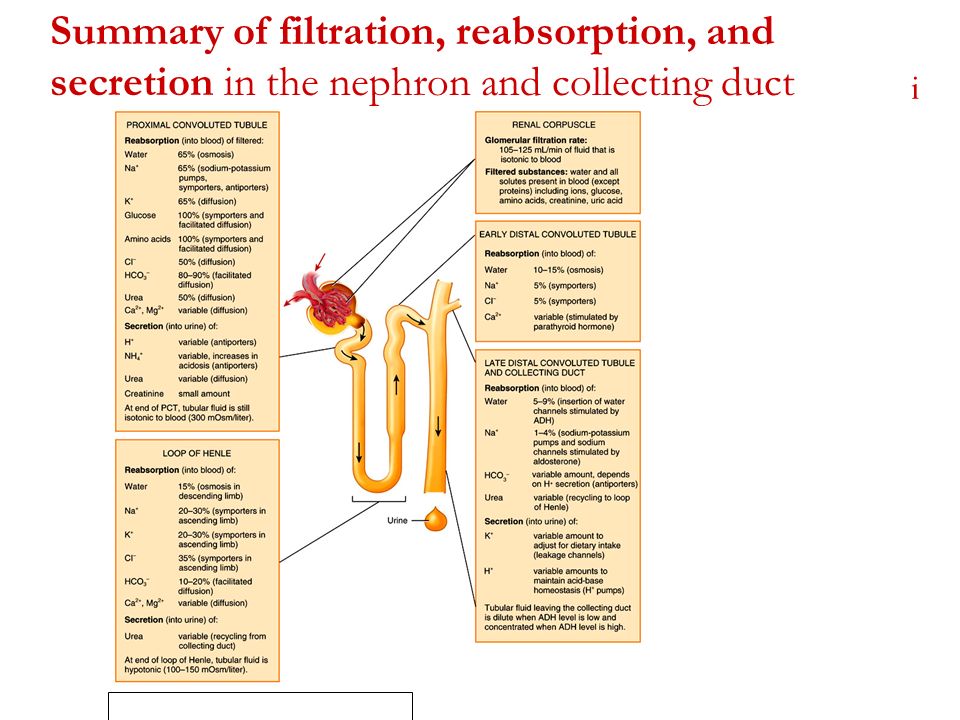
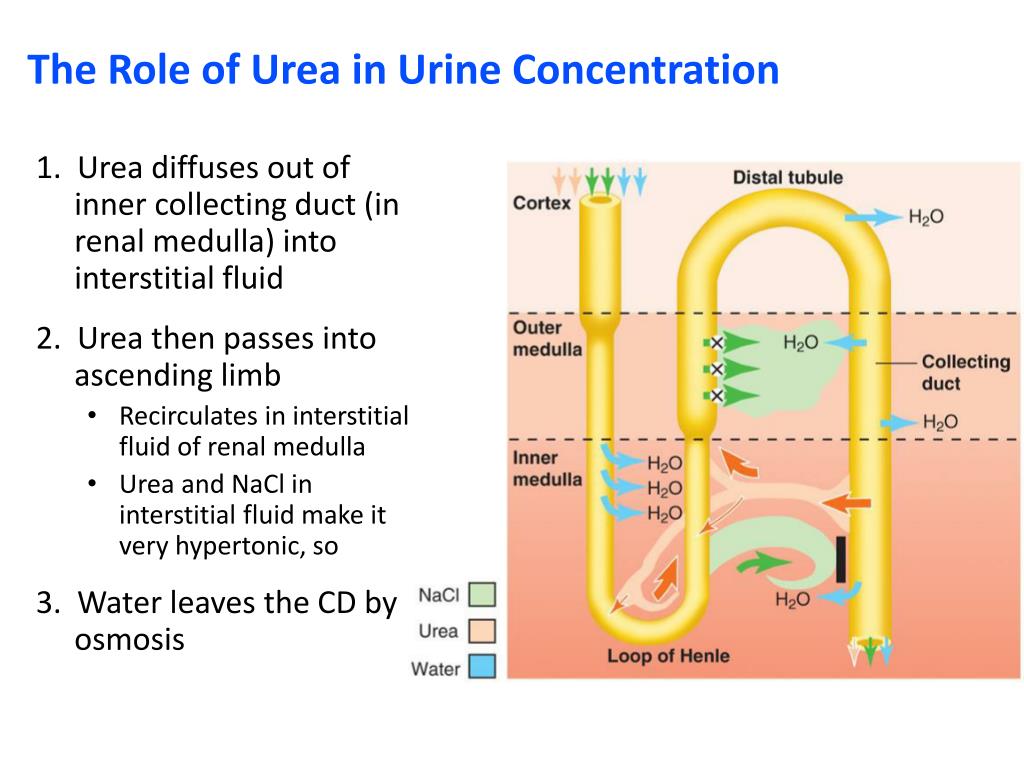
What happens in the body to cause bladder control problems? Located in the lower abdomen, the bladder is a hollow organ that is part of the urinary system, which also includes the kidneys, ureters, and urethra. During urination, muscles in the bladder tighten to move urine into the tube-shaped urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder don’t work the way they should, urine can leak, resulting in urinary incontinence.
Incontinence can happen for many reasons, including urinary tract infections, vaginal infection or irritation, or constipation. Some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
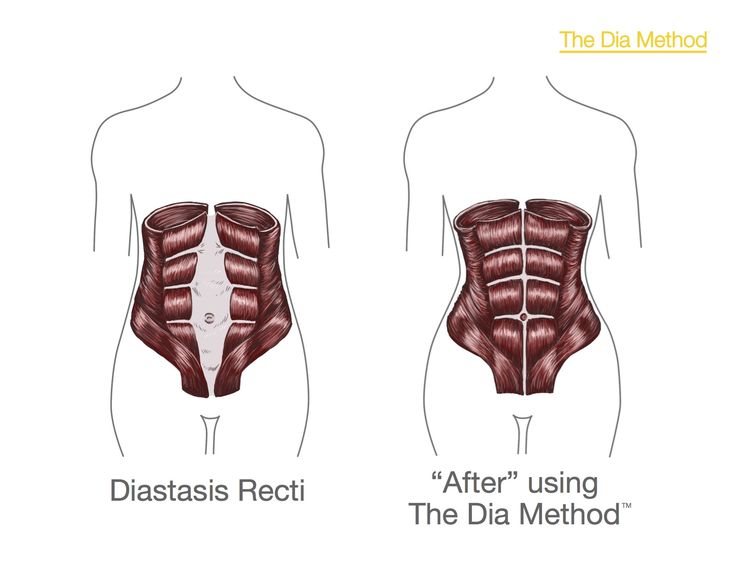
- Weak bladder or pelvic floor muscles
- Overactive bladder muscles
- Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinson’s disease
- Diseases such as arthritis that may make it difficult to get to the bathroom in time
- Pelvic organ prolapse, which is when pelvic organs (such as the bladder, rectum, or uterus) shift out of their normal place into the vagina or anus. When pelvic organs are out of place, the bladder and urethra are not able to work normally, which may cause urine to leak.
Most incontinence in men is related to the prostate gland. Male incontinence may be caused by:
- Prostatitis, a painful inflammation of the prostate gland
- Injury or damage to nerves or muscles from surgery
- An enlarged prostate gland, which can lead to benign prostate hyperplasia, a condition in which the prostate grows as men age
Types of urinary incontinence
There are different types of incontinence:
- Stress incontinence occurs when urine leaks as pressure is put on the bladder, such as during exercise, coughing, sneezing, laughing, or lifting heavy objects.
 It’s the most common type of bladder control problem in younger and middle-aged women. It also may begin later, around the time of menopause.
It’s the most common type of bladder control problem in younger and middle-aged women. It also may begin later, around the time of menopause. - Urge incontinence happens when people have a sudden need to urinate and cannot hold their urine long enough to get to the toilet. It may be a problem for people who have diabetes, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, or stroke.
- Overflow incontinence happens when small amounts of urine leak from a bladder that is always full. A man can have trouble emptying his bladder if an enlarged prostate is blocking the urethra. Diabetes and spinal cord injuries can also cause this type of incontinence.
- Functional incontinence occurs in many older people who have normal bladder control. They just have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly.
Treating and managing urinary incontinence
Today, there are more treatments and ways to manage urinary incontinence than ever before. The choice of treatment depends on the type of bladder control problem you have, how serious it is, and what best fits your lifestyle. As a general rule, the simplest and safest treatments should be tried first.
A combination of treatments may help you get better control of your bladder. Your doctor may suggest you try the following:
Bladder control training
- Pelvic muscle exercises (also known as Kegel exercises) strengthen the muscles that support the bladder, which can help you hold urine in your bladder and avoid leaks. Learn more about pelvic floor exercises and how to do them.
- Urgency suppression helps control strong urges to urinate so you can make it to a toilet on time. For example, you can try distracting yourself to help keep your mind off needing to urinate, taking long relaxing breaths, holding still, and squeezing the pelvic floor muscles.
- Timed voiding is used to help control your bladder through scheduling time to urinate. For example, you can set a plan to urinate every hour. As time goes on, you can slowly extend the time between toilet breaks.
Medical treatments
- Medications that come in a pill, liquid, or patch may be prescribed to help with bladder control problems. However, some medications for overactive bladder have been associated with a higher risk of cognitive decline in adults over age 65. Talk with your doctor about what medications, if any, would work best for you.
- Vaginal estrogen cream may help relieve urge or stress incontinence. A low dose of estrogen cream is applied directly to the vaginal walls and urethral tissue.
- Bulking agents can be used to help close the bladder opening. Doctors can inject a bulking gel or paste that thickens the area around the urethra. This can reduce stress incontinence but may need to be repeated.
- Medical devices may also be used to manage urinary incontinence, such as a catheter that drains urine from your bladder; a urethral insert that helps prevent leakage; and a vaginal pessary ring that provides pressure to lessen leakage.
- Biofeedback uses sensors to make you aware of signals from your body. This may help you regain control over the muscles in your bladder and urethra.
- Electrical nerve stimulation sends mild electric currents to the nerves around the bladder that help control urination and your bladder’s reflexes.
- Surgery can sometimes improve or cure incontinence if it is caused by a change in the position of the bladder or blockage due to an enlarged prostate.
Behavioral and lifestyle changes
Changing your lifestyle may help with bladder problems. Losing weight, quitting smoking, saying “no” to alcohol, choosing water instead of other drinks, and limiting drinks before bedtime can help with some bladder problems. Preventing constipation and avoiding lifting heavy objects may also help with incontinence. Even after treatment, some people still leak urine from time to time. There are bladder control products and other solutions, including disposable briefs or underwear, furniture pads, and urine deodorizing pills that may help.
Preventing constipation and avoiding lifting heavy objects may also help with incontinence. Even after treatment, some people still leak urine from time to time. There are bladder control products and other solutions, including disposable briefs or underwear, furniture pads, and urine deodorizing pills that may help.
Visit the National Institute of Diabetes and Digestive and Kidney Diseases for more information on urinary incontinence in men and urinary incontinence in women.
When to see a health care provider and what to expect
Talk to your health care provider if you have urinary incontinence or any signs of a bladder problem, such as:
- Needing to urinate more frequently or suddenly
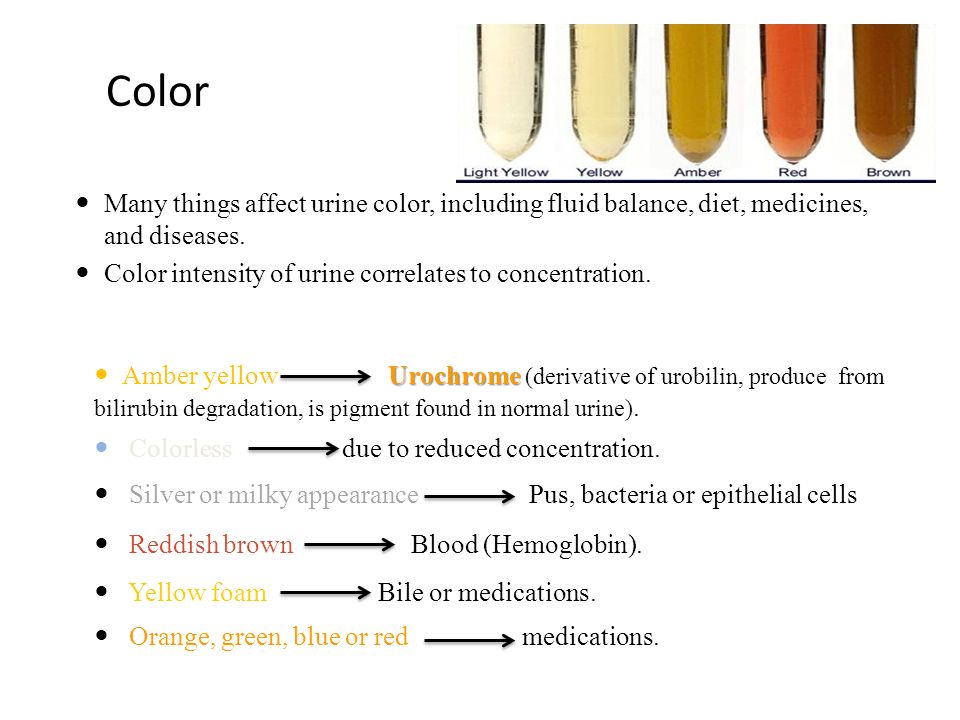
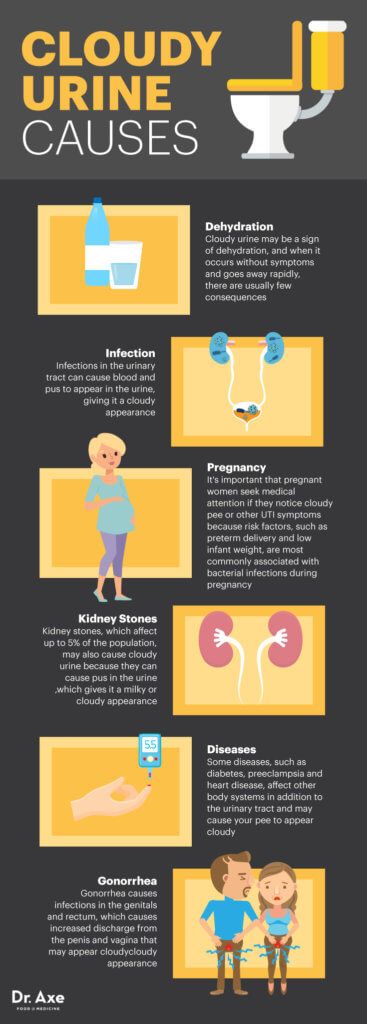
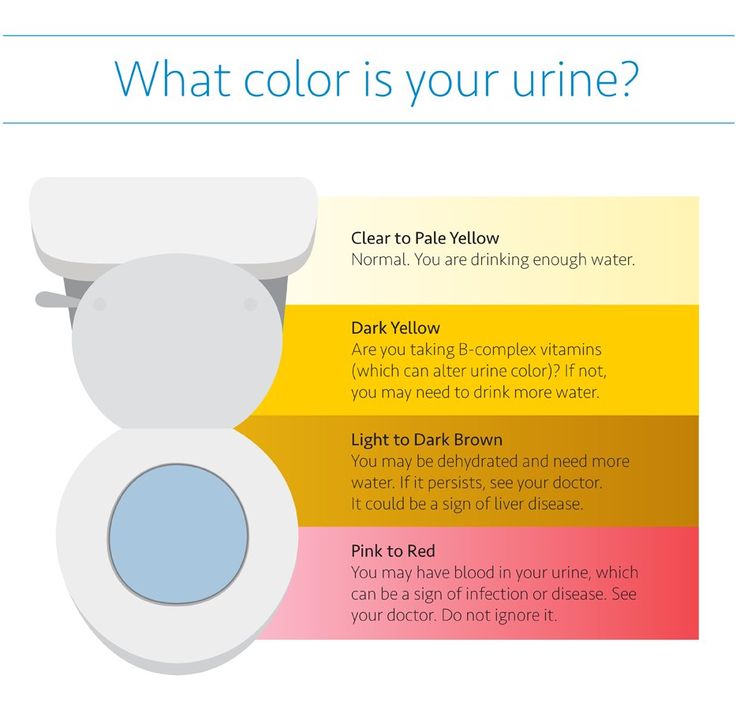
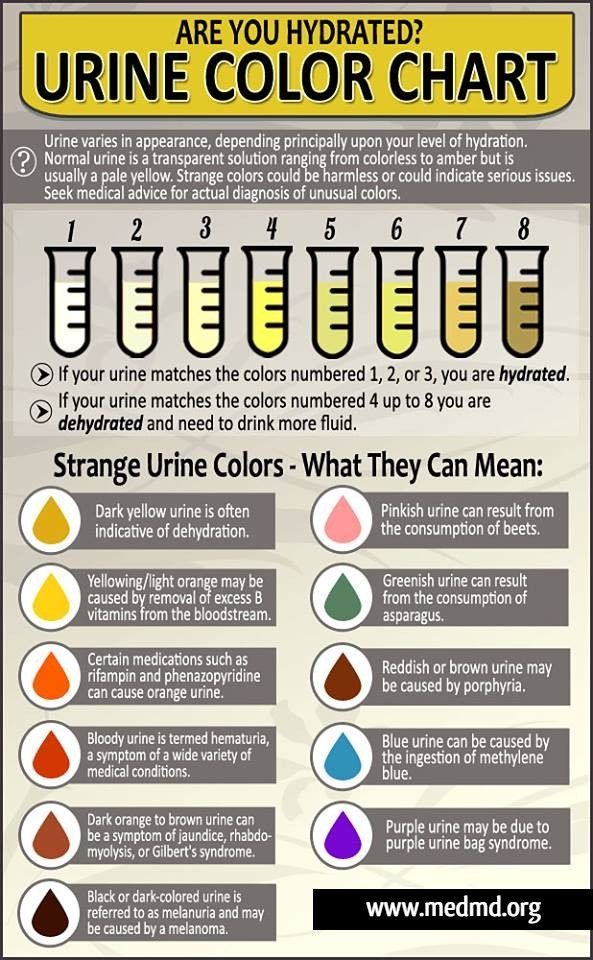
- Cloudy urine
- Blood in the urine
- Pain while urinating
- Urinating eight or more times in one day
- Passing only small amounts of urine after strong urges to urinate
- Trouble starting or having a weak stream while urinating
Get tips on talking to your doctor about sensitive subjects.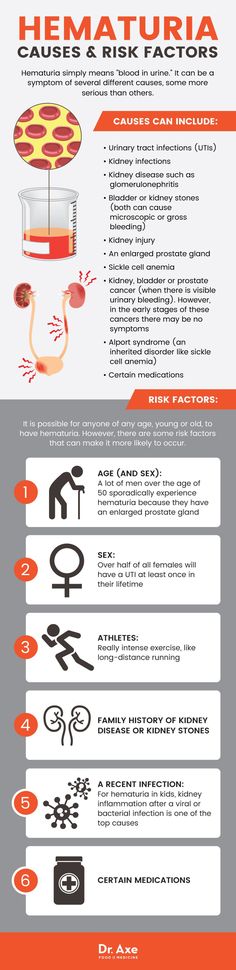
Your doctor may recommend urodynamic testing and perform the following to try to figure out what might be causing your bladder problem:
- Give you a physical exam and take your medical history.
- Ask about your symptoms and the medications you take.
- Take urine and blood samples.
- Examine the inside of your bladder using a cystoscope — a long, thin tube that slides up into the bladder through the urethra. This is usually done by a urinary specialist.
- Fill the bladder with warm fluid and use a cystoscope to check how much fluid your bladder can hold before leaking.
- Order or perform a bladder ultrasound to see if you are fully emptying your bladder with each void.
- Ask you to keep a daily diary of when you urinate and when you leak urine. Your primary care doctor may also send you to a urologist, a doctor who specializes in urinary tract problems.
For more tips to keep your bladder healthy, visit 15 Tips to Keep Your Bladder Healthy.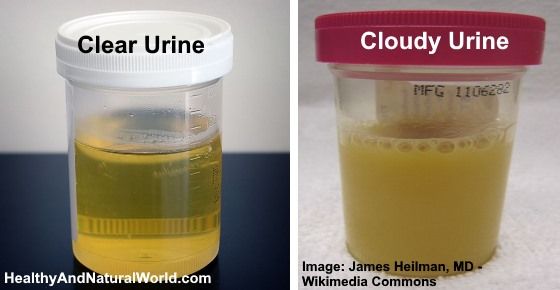
Read about this topic in Spanish. Lea sobre este tema en español.
For more information on urinary incontinence and bladder health
National Association for Continence
800-252-3337
[email protected]
www.nafc.org
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
800-860-8747
866-569-1162 (TTY)
[email protected]
www.niddk.nih.gov
MedlinePlus
National Library of Medicine
www.medlineplus.gov
Simon Foundation for Continence
800-237-4666
[email protected]
www.simonfoundation.org
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed: January 24, 2022
Related Articles
Urinary incontinence - Diagnosis and treatment
Diagnosis
It's important to determine the type of urinary incontinence that you have, and your symptoms often tell your doctor which type you have. That information will guide treatment decisions.
That information will guide treatment decisions.
Your doctor is likely to start with a thorough history and physical exam. You may then be asked to do a simple maneuver that can demonstrate incontinence, such as coughing.
After that, your doctor will likely recommend:
- Urinalysis. A sample of your urine is checked for signs of infection, traces of blood or other abnormalities.
- Bladder diary. For several days you record how much you drink, when you urinate, the amount of urine you produce, whether you had an urge to urinate and the number of incontinence episodes.
- Postvoid residual measurement. You're asked to urinate (void) into a container that measures urine output. Then your doctor checks the amount of leftover urine in your bladder using a catheter or ultrasound test. A large amount of leftover urine in your bladder may mean that you have an obstruction in your urinary tract or a problem with your bladder nerves or muscles.
If further information is needed, your doctor may recommend more-involved tests, such as urodynamic testing and pelvic ultrasound. These tests are usually done if you're considering surgery.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your urinary incontinence-related health concerns Start Here
More Information
- Urinary incontinence care at Mayo Clinic
- Cystoscopy
- Ultrasound
- Urinalysis
Treatment
Treatment for urinary incontinence depends on the type of incontinence, its severity and the underlying cause. A combination of treatments may be needed. If an underlying condition is causing your symptoms, your doctor will first treat that condition.
Your doctor may recommend less invasive treatments to start with and move on to other options if these techniques fail to help you.
Behavioral techniques
Your doctor may recommend:
- Bladder training, to delay urination after you get the urge to go.
 You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you're urinating only every 2.5 to 3.5 hours.
You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you're urinating only every 2.5 to 3.5 hours. - Double voiding, to help you learn to empty your bladder more completely to avoid overflow incontinence. Double voiding means urinating, then waiting a few minutes and trying again.
- Scheduled toilet trips, to urinate every two to four hours rather than waiting for the need to go.
- Fluid and diet management, to regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine or acidic foods. Reducing liquid consumption, losing weight or increasing physical activity also can ease the problem.
Pelvic floor muscle exercises
Female pelvic floor muscles
Female pelvic floor muscles
A woman's pelvic floor muscles work like a hammock to support the pelvic organs, including the uterus, bladder and rectum.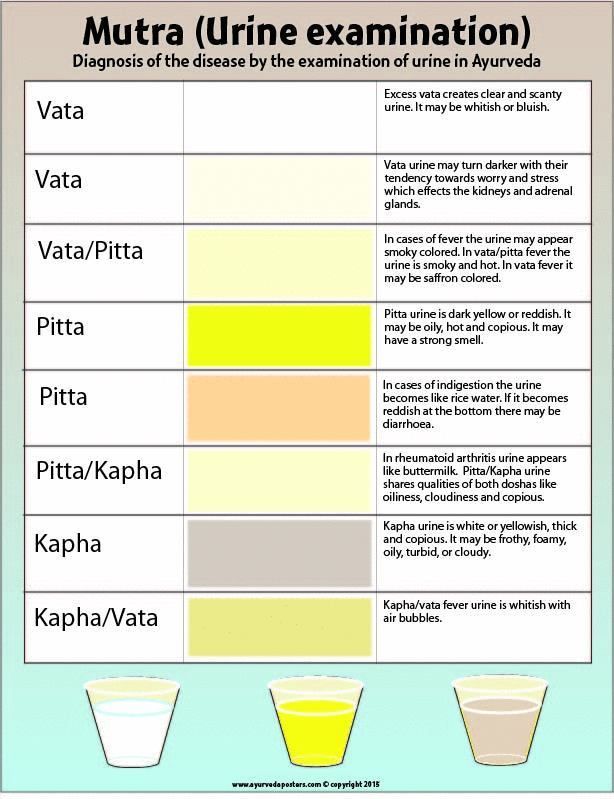 Kegel exercises can help strengthen these muscles.
Kegel exercises can help strengthen these muscles.
Male pelvic floor muscles
Male pelvic floor muscles
The pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
Your doctor may recommend that you do these exercises frequently to strengthen the muscles that help control urination. Also known as Kegel exercises, these techniques are especially effective for stress incontinence but may also help urge incontinence.
To do pelvic floor muscle exercises, imagine that you're trying to stop your urine flow. Then:
- Tighten (contract) the muscles you would use to stop urinating and hold for five seconds, and then relax for five seconds. (If this is too difficult, start by holding for two seconds and relaxing for three seconds.)
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
To help you identify and contract the right muscles, your doctor may suggest that you work with a pelvic floor physical therapist or try biofeedback techniques.
Medications
Medications commonly used to treat incontinence include:
- Anticholinergics. These medications can calm an overactive bladder and may be helpful for urge incontinence. Examples include oxybutynin (Ditropan XL), tolterodine (Detrol), darifenacin (Enablex), fesoterodine (Toviaz), solifenacin (Vesicare) and trospium chloride.
- Mirabegron (Myrbetriq). Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It may also increase the amount you are able to urinate at one time, helping to empty your bladder more completely.
- Alpha blockers. In men who have urge incontinence or overflow incontinence, these medications relax bladder neck muscles and muscle fibers in the prostate and make it easier to empty the bladder.
 Examples include tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo), and doxazosin (Cardura).
Examples include tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo), and doxazosin (Cardura). - Topical estrogen. Applying low-dose, topical estrogen in the form of a vaginal cream, ring or patch may help tone and rejuvenate tissues in the urethra and vaginal areas.
Electrical stimulation
Electrodes are temporarily inserted into your rectum or vagina to stimulate and strengthen pelvic floor muscles. Gentle electrical stimulation can be effective for stress incontinence and urge incontinence, but you may need multiple treatments over several months.
Medical devices
Types of pessaries
Types of pessaries
Pessaries come in many shapes and sizes. The device fits into the vagina and provides support to vaginal tissues displaced by pelvic organ prolapse. A health care provider can fit a pessary and help provide information about which type would work best.
Devices designed to treat women with incontinence include:
- Urethral insert, a small, tampon-like disposable device inserted into the urethra before a specific activity, such as tennis, that can trigger incontinence.
 The insert acts as a plug to prevent leakage and is removed before urination.
The insert acts as a plug to prevent leakage and is removed before urination. - Pessary, a flexible silicone ring that you insert into your vagina and wear all day. The device is also used in women with vaginal prolapse. The pessary helps support the urethra, to prevent urine leakage.
Interventional therapies
Sacral nerve stimulation device
Sacral nerve stimulation device
During sacral nerve stimulation, a surgically implanted device delivers electrical impulses to the nerves that regulate bladder activity. These are called the sacral nerves. The unit is placed under the skin in the lower back, about where the back pocket is on a pair of pants. In this image, the device is shown out of place to allow a better view of the unit.
Interventional therapies that may help with incontinence include:
- Bulking material injections. A synthetic material is injected into tissue surrounding the urethra.
 The bulking material helps keep the urethra closed and reduce urine leakage. This procedure is for the treatment of stress incontinence and is generally less effective than more-invasive treatments such as surgery. It may need to be repeated more than once.
The bulking material helps keep the urethra closed and reduce urine leakage. This procedure is for the treatment of stress incontinence and is generally less effective than more-invasive treatments such as surgery. It may need to be repeated more than once. - OnabotulinumtoxinA (Botox). Injections of Botox into the bladder muscle may benefit people who have an overactive bladder and urge incontinence. Botox is generally prescribed to people only if other treatments haven't been successful.
- Nerve stimulators. There are two types of devices that use painless electrical pulses to stimulate the nerves involved in bladder control (sacral nerves). One type is implanted under your skin in your buttock and connected to wires on the lower back. The other type is a removable plug that is inserted into the vagina. Stimulating the sacral nerves can control overactive bladder and urge incontinence if other therapies haven't worked.
Surgery
Bladder neck suspension
Bladder neck suspension
The Burch procedure, the most common suspension surgery, adds support to the bladder neck and urethra, reducing the risk of stress incontinence. In this version of the procedure, surgery involves placing sutures in vaginal tissue near the neck of the bladder — where the bladder and urethra meet — and attaching them to ligaments near the pubic bone.
In this version of the procedure, surgery involves placing sutures in vaginal tissue near the neck of the bladder — where the bladder and urethra meet — and attaching them to ligaments near the pubic bone.
If other treatments aren't working, several surgical procedures can treat the problems that cause urinary incontinence:
- Sling procedures. Synthetic material (mesh) or strips of your body's tissue are used to create a pelvic sling underneath your urethra and the area of thickened muscle where the bladder connects to the urethra (bladder neck). The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is used to treat stress incontinence.
- Bladder neck suspension. This procedure is designed to provide support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision, so it's done during general or spinal anesthesia.
- Prolapse surgery. In women who have pelvic organ prolapse and mixed incontinence, surgery may include a combination of a sling procedure and prolapse surgery. Repair of pelvic organ prolapse alone does not routinely improve urinary incontinence symptoms.
- Artificial urinary sphincter. A small, fluid-filled ring is implanted around the bladder neck to keep the urinary sphincter shut until there's a need to urinate. To urinate, you press a valve implanted under your skin that causes the ring to deflate and allows urine from your bladder to flow.
Absorbent pads and catheters
If medical treatments can't eliminate your incontinence, you can try products that help ease the discomfort and inconvenience of leaking urine:
- Pads and protective garments. Most products are no more bulky than normal underwear and can be easily worn under everyday clothing. Men who have problems with dribbles of urine can use a drip collector — a small pocket of absorbent padding that's worn over the penis and held in place by close-fitting underwear.
- Catheter. If you're incontinent because your bladder doesn't empty properly, your doctor may recommend that you learn to insert a soft tube (catheter) into your urethra several times a day to drain your bladder. You'll be instructed on how to clean these catheters for safe reuse.
More Information
- Urinary incontinence care at Mayo Clinic
- Bladder control problems in women: Seek treatment
- Bladder control problems: Medications
- Surgery for stress urinary incontinence in women
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Problems with urine leakage may require you to take extra care to prevent skin irritation:
- Use a washcloth to clean yourself.
- Allow your skin to air-dry.

- Avoid frequent washing and douching because these can overwhelm your body's natural defenses against bladder infections.
- Consider using a barrier cream, such as petroleum jelly or cocoa butter, to protect your skin from urine.
- Ask your doctor about special cleansers made to remove urine that may be less drying than other products.
If you have urge incontinence or nighttime incontinence, make the toilet more convenient:
- Move any rugs or furniture you might trip over or collide with on the way to the toilet.
- Use a night light to illuminate your path and reduce your risk of falling.
If you have functional incontinence, you might:
- Keep a bedside commode in your bedroom
- Install an elevated toilet seat
- Widen an existing bathroom doorway
More Information
- Urinary incontinence care at Mayo Clinic
- Bladder control: Lifestyle strategies
Alternative medicine
There are no alternative medicine therapies that have been proved to cure urinary incontinence. Early studies have shown that acupuncture can provide some benefit. Yoga also may provide some benefit for urinary incontinence, but more study is needed.
Early studies have shown that acupuncture can provide some benefit. Yoga also may provide some benefit for urinary incontinence, but more study is needed.
Coping and support
If you're embarrassed about a bladder control problem, you may try to cope on your own by wearing absorbent pads, carrying extra clothes or even avoiding going out.
But effective treatments are available for urinary incontinence. It's important to ask your doctor about treatment. Once you do, you'll be on your way to regaining an active and confident life.
Preparing for your appointment
If you have urinary incontinence, you're likely to start by seeing your primary care doctor. You may be referred to a doctor who specializes in urinary tract disorders (urologist) or a gynecologist with special training in female bladder problems and urinary function (urogynecologist).
What you can do
To get ready for your appointment, it helps to:
- Be aware of any pre-appointment restrictions, such as restricting your diet
- Write down your symptoms, including how often you urinate, nighttime bladder activity and episodes of incontinence
- Make a list of all your medications, vitamins and supplements, including doses and how often you take the medication
- Write down key medical information, including other conditions you may have
- Ask a relative or friend to accompany you, to help you remember what the doctor says
- Take a notebook or electronic device with you, and use it to note important information during your visit
- Write down questions to ask your doctor
For urinary incontinence, some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What kinds of tests do I need? Do these tests require any special preparation?
- Is my urinary incontinence temporary?
- What treatments are available?
- Should I anticipate any side effects of the treatment?
- Is there a generic alternative to the medicine you're prescribing for me?
- I have other health conditions.
 How can I best manage these conditions together?
How can I best manage these conditions together?
Don't hesitate to ask other questions during your appointment as they occur to you.
What to expect from your doctor
Your doctor is likely to ask you a few questions, such as:
- When did you first begin experiencing symptoms, and how severe are they?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve or worsen your symptoms?
- How often do you need to urinate?
- When do you leak urine?
- Do you have trouble emptying your bladder?
- Have you noticed blood in your urine?
- Do you smoke?
- How often do you drink alcohol and caffeinated beverages?
- How often do you eat spicy, sugary or acidic foods?
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Urinary incontinence in women | City Clinical Hospital.
 VM Buyanova
VM Buyanova Urinary incontinence is manifested in women after the implementation of everyday activities for life: prolonged laughter, coughing, prolonged physical exertion, changing body position during sleep, lifting heavy objects, sexual contact.
Almost every fifth woman in the world has experienced this problem. However, not everyone seeks treatment. In Moscow, only 1.5% of women make an appointment with a doctor with urinary incontinence. In America and Europe, the statistics are much worse - 30-40%.
The most common cases are:
- stress urinary incontinence in women. It can occur anywhere, depending on the complexity of the surrounding situation, its psychological, emotional side. It is considered the most common problem in urology;
- urinary incontinence in women when coughing. There is a sharp jump in pressure inside the abdominal cavity, the muscles of the bladder are in great tension. If the sphincters are weak, then urine begins to leak. The same situation is observed with urinary incontinence when sneezing in women. The reasons for the rejection are exactly the same.
The same situation is observed with urinary incontinence when sneezing in women. The reasons for the rejection are exactly the same.
- Bedwetting in women. Uncontrolled urination. As a rule, children suffer from "enuresis";
- urinary incontinence in women after childbirth. Occurs due to a violation, weakening of the muscles of the pelvic floor;
Urinary incontinence in young women. May occur due to all of the above reasons;
- urinary incontinence in elderly women. It is divided into three types: stressful (due to pressure on the abdominal cavity), forced (with any sudden urge), total (uncontrolled, occurs constantly).
Spontaneous loss of urine does not harm a woman's life in any way. At the same time, it brings serious physical and moral inconvenience, affects various aspects of activity.
Most women hesitate to tell their doctor about their problem. This is due to her deepest intimacy, as well as ignorance of a quick way to eliminate urinary incontinence.
Symptoms of urinary incontinence in women
The main symptom of urinary incontinence in women is the spontaneous flow of urine during various daily activities, physical exertion and other situations. Also, the symptoms of the disease include sudden urges, a feeling of incomplete emptying of the bladder, sensations of the presence of a foreign object in the vagina.
Causes of urinary incontinence
Urinary incontinence in women can have different causes. The main ones are:
- pregnancy, difficult childbirth;
- strong physical activity;
- operations;
- genetic predisposition.
Age also influences the development of this disease and is a common cause of urinary incontinence in women over 50 years of age. If the manifestations are minor, conservative treatment with special preparations is used. If the situation is difficult, there are pronounced changes in the anatomy, surgical intervention is prescribed.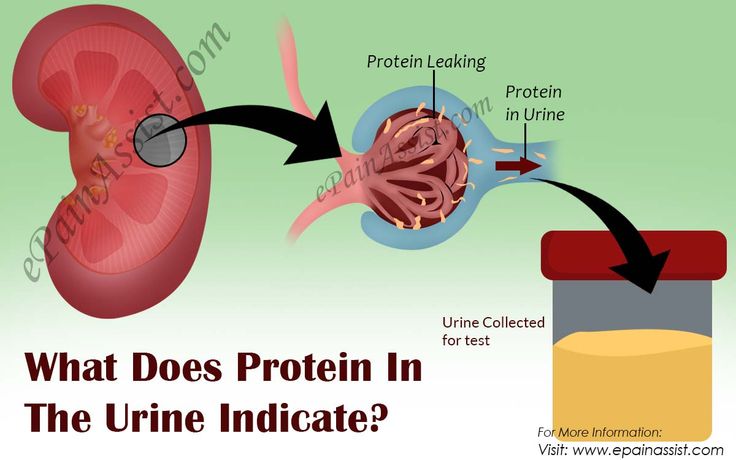
Bedwetting in women is caused by lack of muscle control. At this point, they are relaxed. In addition, infectious diseases and disorders of the nervous system can also affect urine leakage.
Why is urinary incontinence dangerous for women?
In essence, the disease does not harm a woman's health in any way. But with its seemingly minimal danger, urinary incontinence can completely ruin life, limit it, make it constrained. A woman will lose her mobile, will experience constant discomfort. This can also affect your career and professional growth.
Prevention, diagnosis and treatment of urinary incontinence
The first step in the diagnosis of urinary incontinence in women is a consultation with a specialist. The doctor prescribes a complete examination, which helps to identify the causes of the disease. In the future, the most appropriate method of treatment is selected.
Successful surgery requires specific, clear indications.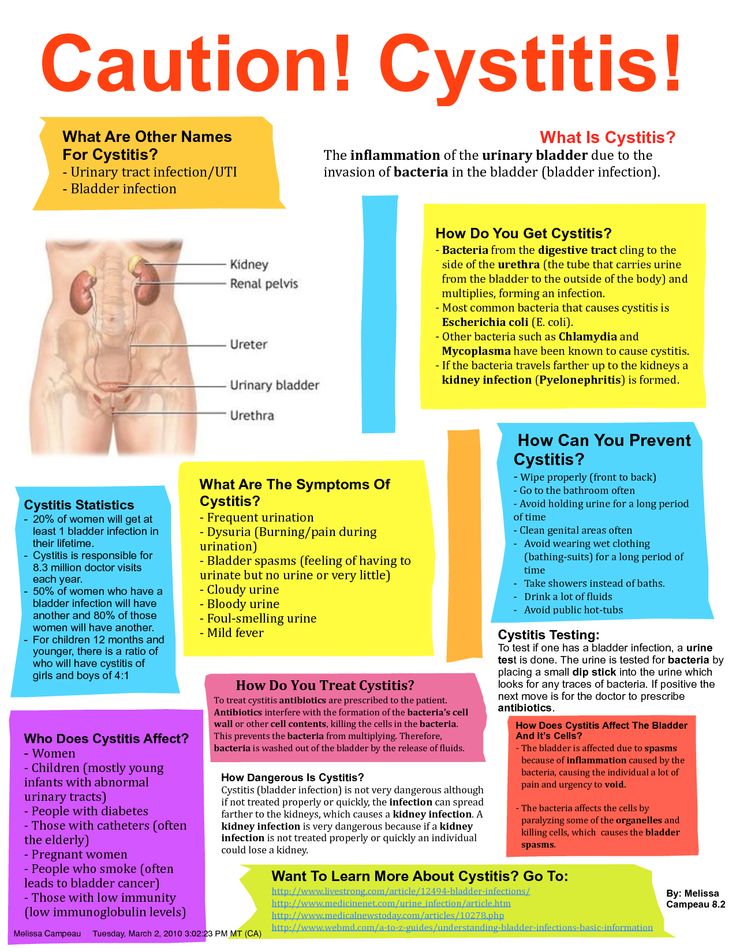 Without them, intervention cannot be carried out, it can only exacerbate the problem.
Without them, intervention cannot be carried out, it can only exacerbate the problem.
Urinary incontinence in women is treated with minimally invasive surgery using the most advanced instruments and equipment.
A special synthetic implant is placed under the middle of the urethra - a mesh that reliably supports the organ, adjacent tissues, and prevents urine leakage. The prosthesis is made of the most modern materials - polypropylene, which has been used in medicine for several years. Its structure freely passes blood cells, thereby preventing the occurrence of inflammatory processes. The implant is installed through a small incision in the vagina 1 cm long. Incisions 2-3 mm long are also made on the inside of the thighs. The operation lasts 20 - 30 minutes.
Bedwetting in women can also be treated with implants. depending on the complexity of the case.
The patient is discharged after the operation every other day. Over the next month, it is necessary to adhere to sexual rest, as well as limit physical activity.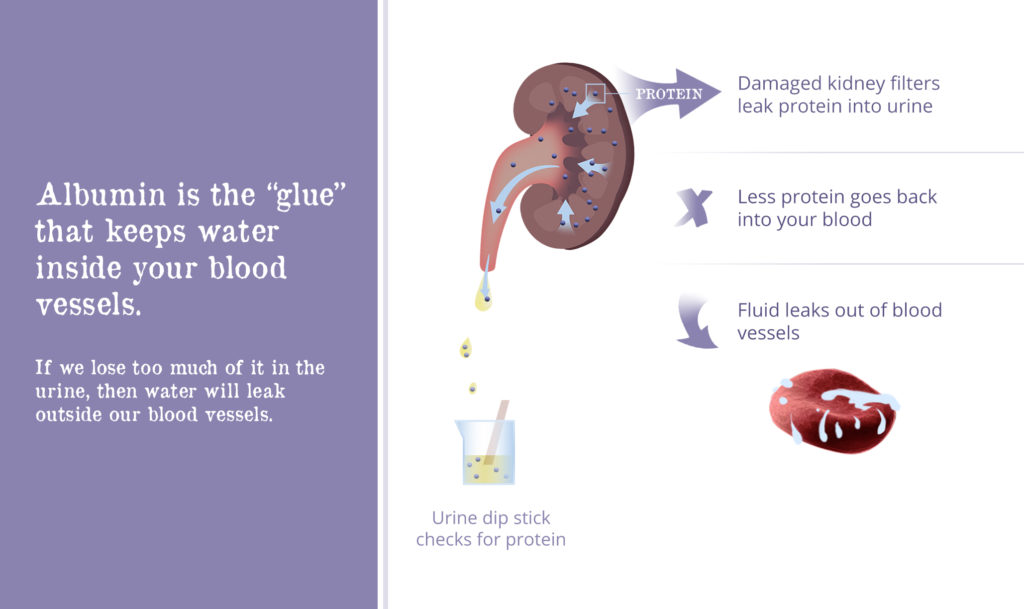
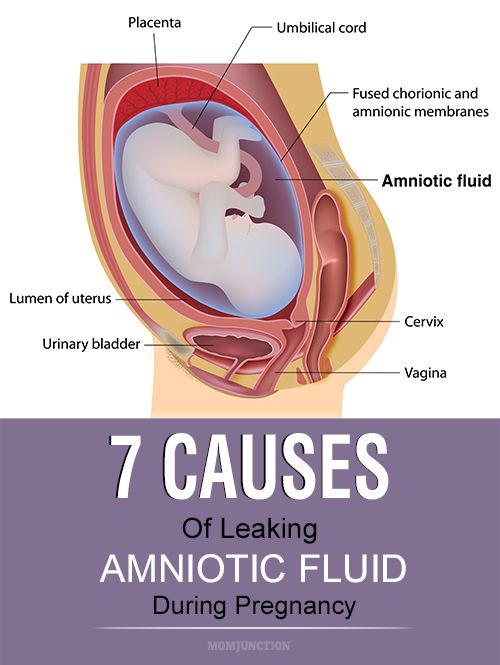
Urinary incontinence and pregnancy
Urinary incontinence is considered to be common during pregnancy. The longer the period, the stronger the disease becomes. It can also persist after childbirth.
Causes of involuntary leakage of urine during pregnancy:
- pelvic floor muscles weaken. This happens due to changes in the hormonal background of the woman's body;
- changes in the size of the uterus. The organ increases, thereby squeezing the bladder;
- movements of the child. When the pregnancy is in the later stages, the fetus is actively moving. Blows of the arms and legs of the child may fall on the bladder.
Despite the safety of the disease for the health of the body, it brings significant discomfort to a woman's life. And only timely treatment will normalize the situation. The main thing is not to be shy about it and immediately consult a doctor!
Demina Olga Alekseevna
obstetrician-gynecologist
Head of the Department of Gynecology
Candidate of Medical Sciences
Appointment for a paid appointment
Parsadanyan Sophia Araratovna
obstetrician-gynecologist
candidate of medical sciences
Appointment for a paid appointment
Phone for inquiries and appointments: +7 (495) 321-57-40 (department of paid medical services).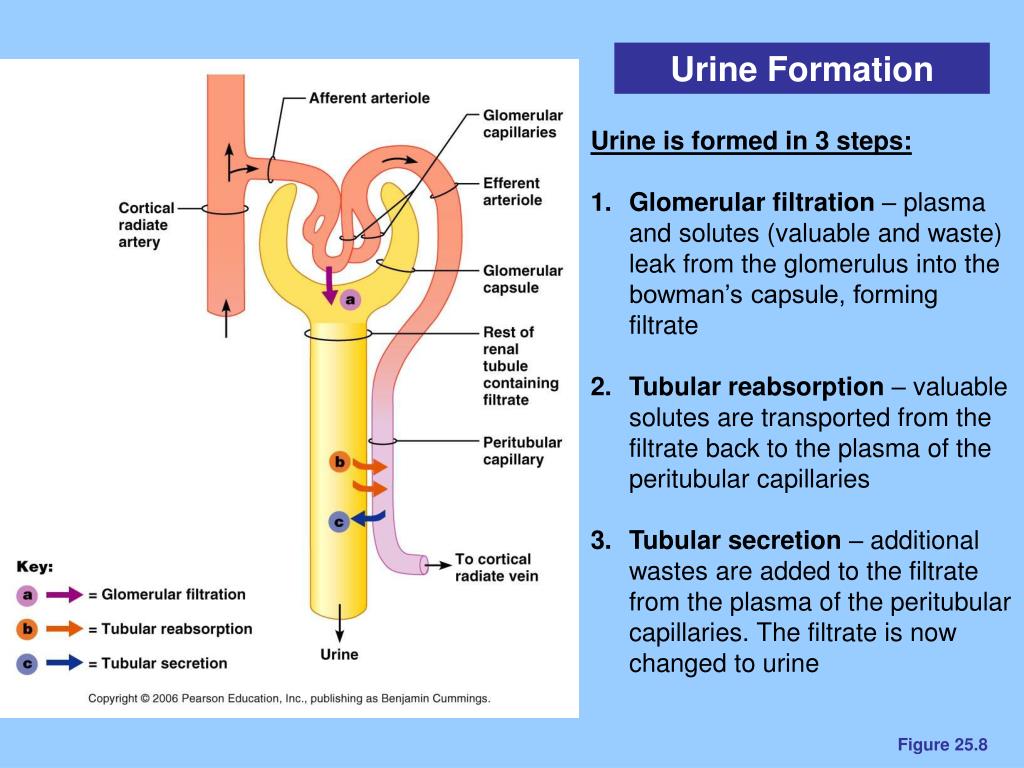
Urinary incontinence: an open conversation with a doctor
Photo from the archive of the Center
“Jumping with a child on a trampoline, I felt that an “accident” had happened,” the obstetrician-gynecologist of the Medical Center for Diagnostics and Treatment Irena Kirilova, with whom we are talking today about delicate problem of urinary incontinence.
- The issue of incontinence is getting louder. The story of a young woman is far from a particular case, when patients of this age category complain of urinary incontinence. Is this another female "epidemic" caused by the modern lifestyle?
- Urinary incontinence or incontinence has always tormented both women and men. We are used to talking only about female incontinence. This is probably due to the fact that a myth has taken root in our minds that all women who have given birth naturally will face this problem to some extent with age, and, alas, nothing can be done about it. We, gynecologists, today confidently declare that this condition can be effectively treated and a woman can return to a full life at any age.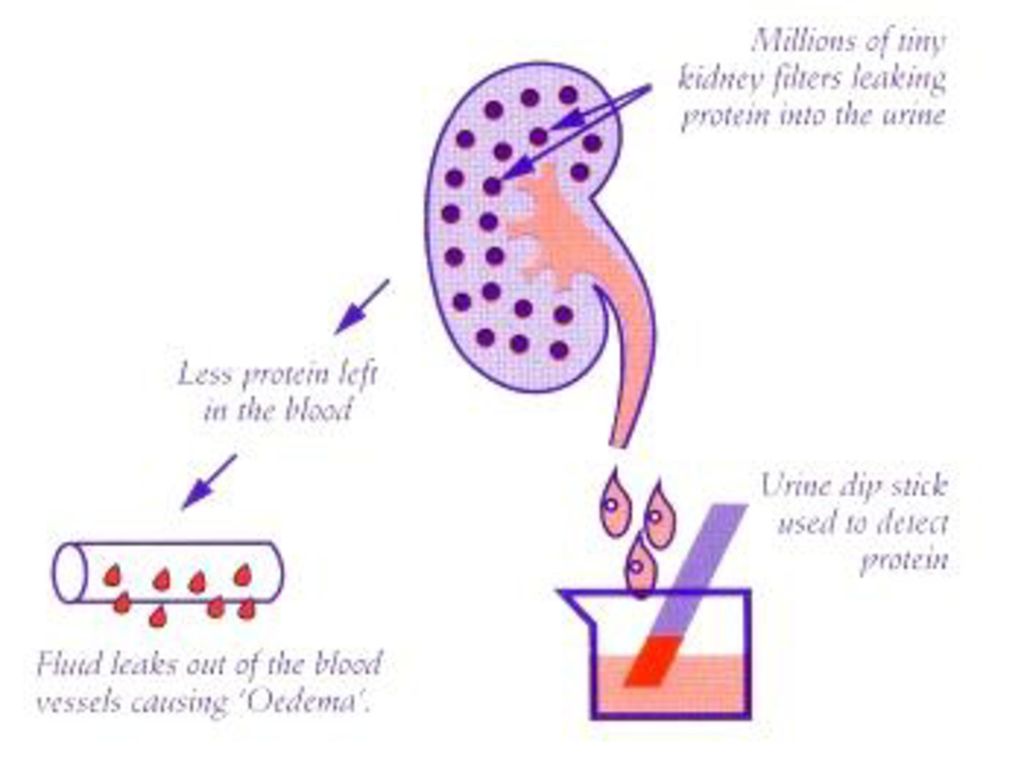 Whether you are thirty or eighty-five years old - if you suffer from urinary incontinence, seek help. Older people, of course, are much more likely to encounter such a problem due to the changes that the whole body undergoes as a whole, but one should not think that young people bypass this problem, and even episodic “accidents” should lead a woman to a doctor.
Whether you are thirty or eighty-five years old - if you suffer from urinary incontinence, seek help. Older people, of course, are much more likely to encounter such a problem due to the changes that the whole body undergoes as a whole, but one should not think that young people bypass this problem, and even episodic “accidents” should lead a woman to a doctor.
- If only a drop of urine comes out when you sneeze, is it worth worrying?
- Any involuntary leakage of urine, no matter how much, is already a signal that the system is leaking.
People sometimes treat incontinence lightly, as a variation of the norm, which, however, they are ashamed to talk about. Yes, indeed, because incontinence does not lead to death, does not affect the state of health, so patients often try to “solve” this problem on their own. Nowadays, there is a great variety of items for proper personal hygiene. Unfortunately, over time, the disease, progressing, makes a person who does not want to suddenly find himself in an awkward position, lead a reclusive lifestyle, give up traveling, meetings, going to the theater, playing sports.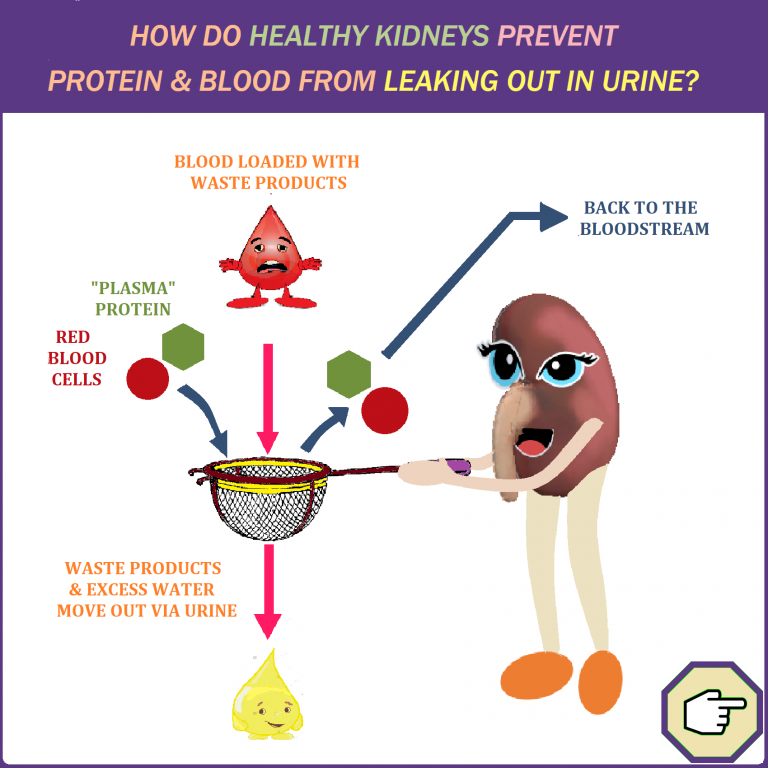 This can affect the psyche, causing a feeling of inferiority and even lead to depression. If coughing, sneezing, vomiting, urine is involuntarily released, the urge to urinate becomes frequent, you have to get up at night, and when urinating you experience pain, burning, cloudy sediment or blood impurities appear in the urine, be sure to consult a doctor. Only a doctor will be able to assess whether you have, among other things, more formidable diseases of the genitourinary system and prescribe an effective treatment.
This can affect the psyche, causing a feeling of inferiority and even lead to depression. If coughing, sneezing, vomiting, urine is involuntarily released, the urge to urinate becomes frequent, you have to get up at night, and when urinating you experience pain, burning, cloudy sediment or blood impurities appear in the urine, be sure to consult a doctor. Only a doctor will be able to assess whether you have, among other things, more formidable diseases of the genitourinary system and prescribe an effective treatment.
- What causes urinary incontinence?
- Urinary incontinence is more common among the elderly, and due to anatomical features, women more often than men. Dementia, multiple sclerosis, Parkinson's disease, stroke, endocrine disorders, and sometimes the use of certain medications can also trigger the development of this disease.
In young and middle-aged women, after childbirth, especially after complicated ones, or if the child was large, there are stretching and ruptures of the muscles of the pelvic floor, perineum and urogenital diaphragm, which in turn can provoke the problem that we are talking about today.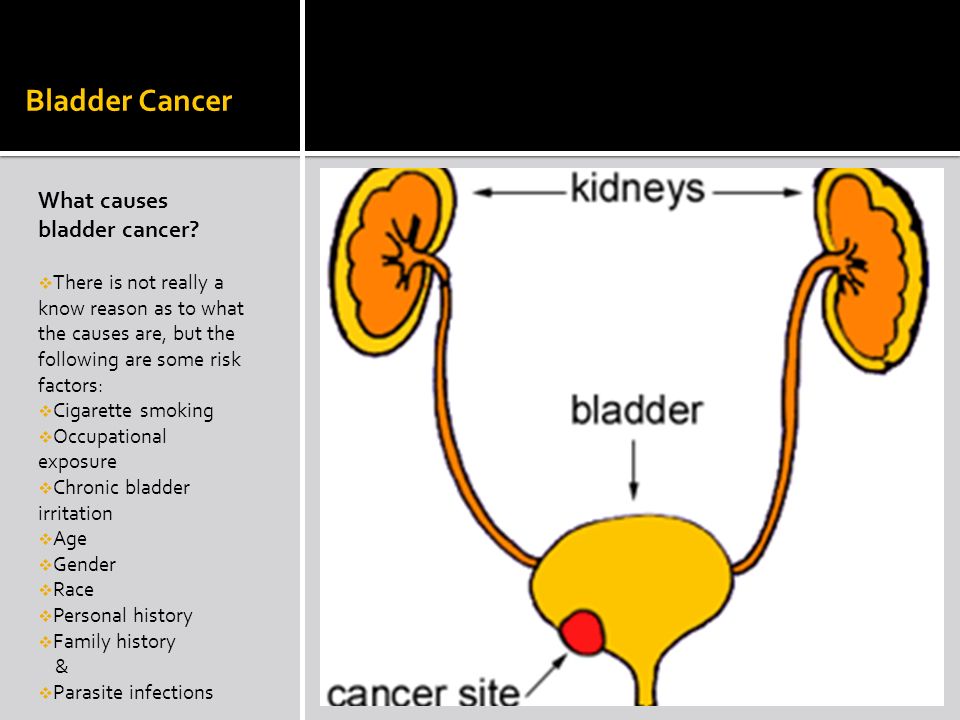 All expectant mothers before and after childbirth are advised to strengthen their pelvic floor muscles daily with Kegel exercises. This gymnastics is very simple, but very effective. Training the muscles of the vagina and the pubococcygeal muscle, among other things, protects against prolapse of organs, and also gives intimate life a new color.
All expectant mothers before and after childbirth are advised to strengthen their pelvic floor muscles daily with Kegel exercises. This gymnastics is very simple, but very effective. Training the muscles of the vagina and the pubococcygeal muscle, among other things, protects against prolapse of organs, and also gives intimate life a new color.
The causes of this disease can be various, and, therefore, a detailed examination should be carried out to identify them, and the correct treatment tactics should be chosen - drug therapy, surgery, or a simple change in lifestyle - diet, gymnastics to strengthen the muscles of the pelvic floor especially in younger patients. Such a restructuring is not easy to perform, but it is so necessary to return to a full life without drastic measures.
- Do different causes of incontinence lead to the same result?
- Basically, three types of urinary incontinence are distinguished: stress (with tension, for example, when coughing), imperative (irritable bladder syndrome), associated with an uncontrollable urge to urinate, and mixed.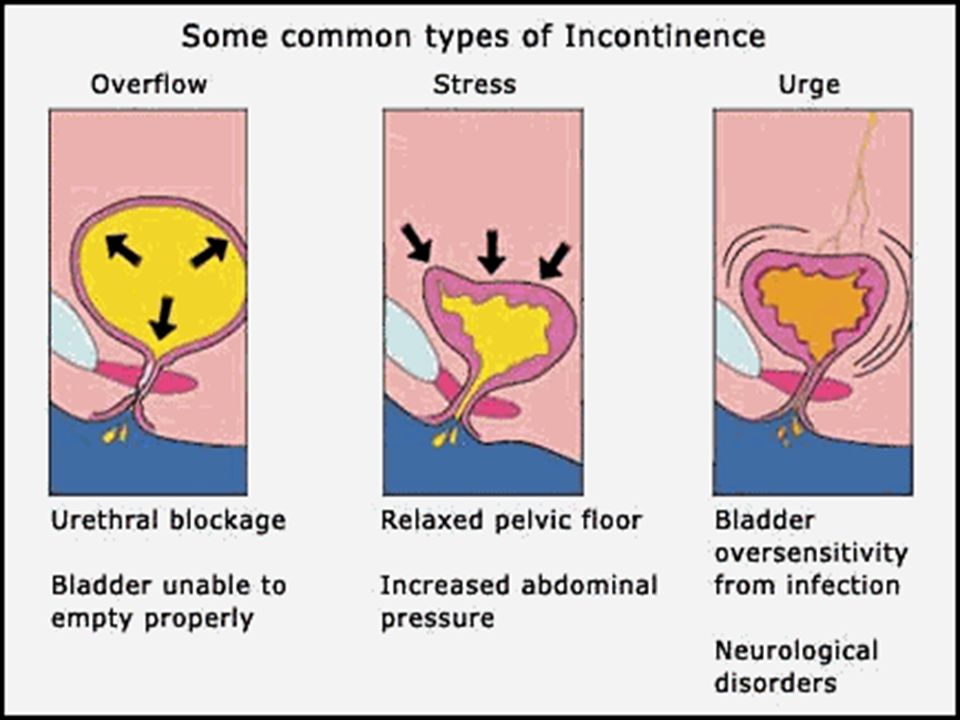 The result is the same - the bladder "does not obey", but the mechanism of "disobedience" is different.
The result is the same - the bladder "does not obey", but the mechanism of "disobedience" is different.
Stress urinary incontinence - involuntary leakage of urine during coughing, laughing, running and other physical activities, leading to an increase in intra-abdominal and, therefore, intravesical pressure. A characteristic feature of stress urinary incontinence is the lack of an urge to urinate.
The main reason for the development of stress urinary incontinence in women is a decrease in the tone of the pelvic floor, leading to prolapse of the pelvic organs (uterus, vagina, bladder, urethra), damage to the connective tissue structures of the pelvic floor, impaired coordination of various muscle groups. Emotional stress can also serve as a trigger.
Women who suffer from irritable bladder syndrome complain that they do not have time to run to the toilet when an overwhelming urge occurs. Such an urge is called "imperative" or "imperative." External stimuli can provoke incontinence in this condition: pouring water, bright light, or something else.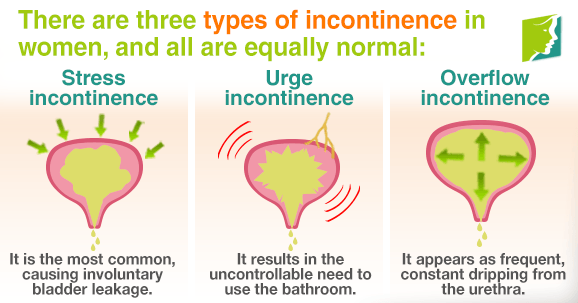 Its main cause is an overactive bladder, which instantly responds to even a slight irritation.
Its main cause is an overactive bladder, which instantly responds to even a slight irritation.
- How to treat urinary incontinence?
- Today, incontinence is perfectly cured. First of all, the doctor determines the cause of urinary incontinence - checks for organ prolapse, conducts diagnostic tests and determines the type of incontinence. Sometimes it is difficult to immediately establish the cause, research and observation are necessary, which take some time, consultation of other specialists, for example, a urologist. The patient should come to the gynecologist's appointment with a full bladder.
If the diagnosis is irritable bladder syndrome, medication is most commonly prescribed to desensitize bladder receptors. Patients should also follow a specific diet to reduce excess weight and strengthen the pelvic floor muscles.
Stress urinary incontinence is effectively treated with minimally invasive surgery through the vagina. During the operation, which lasts about 10 minutes under full anesthesia, a supporting synthetic loop is laid around the middle part of the urethra.