What is mastitis in the breast
Mastitis - NHS
Mastitis is when your breast becomes swollen, hot and painful.
It's most common in breastfeeding women, but women who are not breastfeeding and men can also get it.
Check if you have mastitis
Mastitis usually only affects 1 breast, and symptoms often come on quickly. They include:
- a swollen area on your breast that may feel hot and painful to touch – the area may become red but this can be harder to see if you have darker skin
- a wedge-shaped breast lump or a hard area on your breast
- a burning pain in your breast that might be constant or only when you breastfeed
- nipple discharge, which may be white or contain streaks of blood
You may also get flu-like symptoms, such as aches, a high temperature, chills and tiredness.
Things you can do
Do
-
soak a cloth in warm water and place it on your breast to help relieve the pain – a warm shower or bath may also help
-
rest and drink lots of fluids
-
take paracetamol or ibuprofen to reduce any pain or fever
-
if you are breastfeeding, continue to breastfeed
-
start feeds with the sore breast first
-
express milk from your breast in between feeds
-
massage your breast to clear any blockages – stroke from the lumpy or sore area towards your nipple to help the milk flow
Non-urgent advice: See a GP if:
- you do not feel better within 24 hours despite continuing to breastfeed
- you get mastitis and you are not breastfeeding
- your symptoms do not get any better 48 hours after taking antibiotics
Treatment for mastitis from a GP
A GP will usually prescribe antibiotics.
If you're breastfeeding a very small amount of the antibiotic may go into your breast milk. There is no risk to your baby, but it might make them irritable and restless.
What to do if mastitis comes back
If you are breastfeeding and keep getting mastitis, it might be due to problems with positioning and attaching.
If you have any breastfeeding problems, it's important to ask for help from a midwife, health visitor or a breastfeeding specialist as soon as possible.
Information:
You can also call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm, daily)
Causes of mastitis
Mastitis is common in breastfeeding women as it can be caused by a build-up of milk.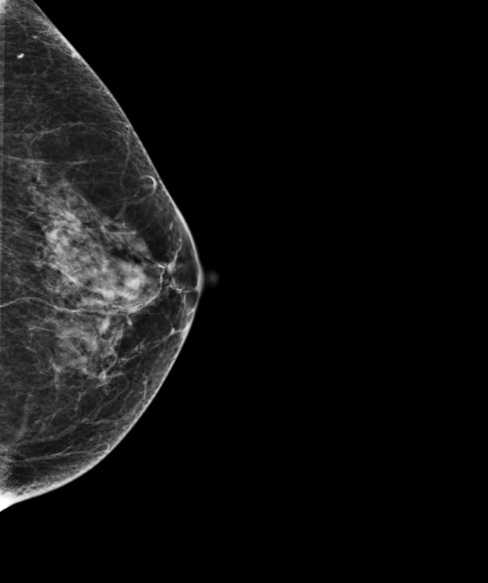
Women who are not breastfeeding can also get mastitis, as can men. This can happen due to:
- smoking – toxins found in tobacco can damage breast tissue
- damage to the nipple, such as a piercing or skin condition like eczema
- you have a breast implant
- having a weak immune system due to a health condition like diabetes
- shaving or plucking hairs from around your nipples
Page last reviewed: 29 October 2019
Next review due: 29 October 2022
Breast Infection (Mastitis): Symptoms, Causes, Treatments
Written by WebMD Editorial Contributors
In this Article
- How the Breast Is Built
- Breast Infection Causes
- Breast Infection Symptoms
- When to Seek Medical Care
- Breast Infection Exams and Tests
- Breast Infection Treatment
- Breast Infection Home Remedies
- Medications for Mastitis
- Surgery for an Abscess
- Next Steps
- Follow-Up Care After a Breast Infection
- Mastitis Prevention
- Outlook for Breast Infections
How the Breast Is Built
The breast is composed of several glands and ducts that lead to the nipple and the surrounding colored area called the areola. The milk-carrying ducts extend from the nipple into the underlying breast tissue like the spokes of a wheel. Under the areola are lactiferous ducts. These fill with milk during lactation after a woman has a baby. When a girl reaches puberty, changing hormones cause the ducts to grow and cause fat deposits in the breast tissue to increase. The glands that produce milk (mammary glands) that are connected to the surface of the breast by the lactiferous ducts may extend to the armpit area.
The milk-carrying ducts extend from the nipple into the underlying breast tissue like the spokes of a wheel. Under the areola are lactiferous ducts. These fill with milk during lactation after a woman has a baby. When a girl reaches puberty, changing hormones cause the ducts to grow and cause fat deposits in the breast tissue to increase. The glands that produce milk (mammary glands) that are connected to the surface of the breast by the lactiferous ducts may extend to the armpit area.
Breast Infection Causes
Mastitis is an infection of the tissue of the breast that occurs most frequently during the time of breastfeeding. It can occur when bacteria, often from the baby's mouth, enter a milk duct through a crack in the nipple.
Breast infections most commonly occur one to three months after the delivery of a baby, but they can occur in women who have not recently delivered and in women after menopause. Other causes of infection include chronic mastitis and a rare form of cancer called inflammatory carcinoma.
In healthy women, mastitis is rare. However, women with diabetes, chronic illness, AIDS, or an impaired immune system may be more susceptible.
About 1%-3% of breastfeeding mothers develop mastitis. Engorgement and incomplete breast emptying can contribute to the problem and make the symptoms worse.
Chronic mastitis occurs in women who are not breastfeeding. In postmenopausal women, breast infections may be associated with chronic inflammation of the ducts below the nipple. Hormonal changes in the body can cause the milk ducts to become clogged with dead skin cells and debris. These clogged ducts make the breast more open to bacterial infection. Infection tends to come back after treatment with antibiotics.
Breast Infection Symptoms
Breast infections may cause pain, redness, and warmth of the breast along with the following symptoms:
- Tenderness and swelling
- Body aches
- Fatigue
- Breast engorgement
- Fever and chills
- Abscess: A breast abscess can be a complication of mastitis.
 Noncancerous masses such as abscesses are more often tender and frequently feel mobile beneath the skin. The edge of the mass is usually regular and well defined. Indications that this more serious infection has occurred include the following:
Noncancerous masses such as abscesses are more often tender and frequently feel mobile beneath the skin. The edge of the mass is usually regular and well defined. Indications that this more serious infection has occurred include the following:- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.)
- Pus draining from the nipple
- Persistent fever and no improvement of symptoms within 48-72 hours of treatment
When to Seek Medical Care
Call your health care provider as soon as you feel any suspicious lump, whether you are breastfeeding or not. Call for an appointment if:
- You have any abnormal discharge from your nipples.
- Breast pain is making it difficult for you to function each day.
- You have prolonged, unexplained breast pain.
- You have any other associated symptoms such as redness, swelling, pain that interferes with breastfeeding, a mass or tender lump in the breast that does not disappear after breastfeeding.

- If you are breastfeeding, call your doctor if you develop any symptoms of breast infection so that treatment may be started promptly.
You may need to be evaluated in a hospital's emergency department if the breast pain is associated with other signs of an infection (such as a fever, swelling, or redness to the breast) and if your health care provider cannot see you promptly. The below symptoms require emergency treatment:
- A persistent high fever greater than 101.5°F
- Nausea or vomiting that is preventing you from taking the antibiotics as prescribed
- Pus draining from the breast
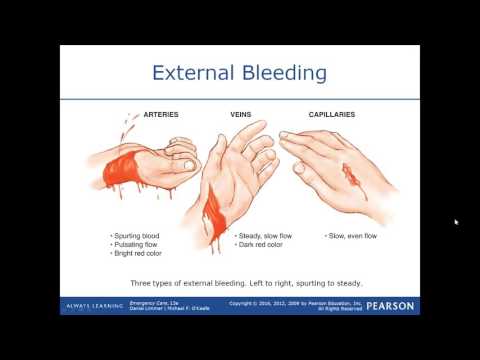
- Red streaks extending toward your arm or chest
- Dizziness, fainting, or confusion
Breast Infection Exams and Tests
The diagnosis of mastitis and a breast abscess can usually be made based on a physical exam.
- If it is unclear whether a mass is due to a fluid-filled abscess or to a solid mass such as a tumor, a test such as an ultrasound may be done.
 An ultrasound may also be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. This noninvasive test allows your doctor to directly visualize the abscess by placing an ultrasound probe over your breast. If an abscess is confirmed, aspiration or surgical drainage, and IV antibiotics, are often required.
An ultrasound may also be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. This noninvasive test allows your doctor to directly visualize the abscess by placing an ultrasound probe over your breast. If an abscess is confirmed, aspiration or surgical drainage, and IV antibiotics, are often required. - Cultures may be taken, either of breast milk or of material taken out of an abscess through a syringe, to determine the type of organism causing the infection. This information can help your doctor decide what kind of antibiotic to use.
- Nonbreastfeeding women with mastitis, or those who do not respond to treatment, may have a mammogram or breast biopsy. This is a precautionary measure because a rare type of breast cancer can produce symptoms of mastitis.
Breast Infection Treatment
Breast infections require treatment by a health care provider.
Breast Infection Home Remedies
After you see a doctor, try the following to help your breast infection heal.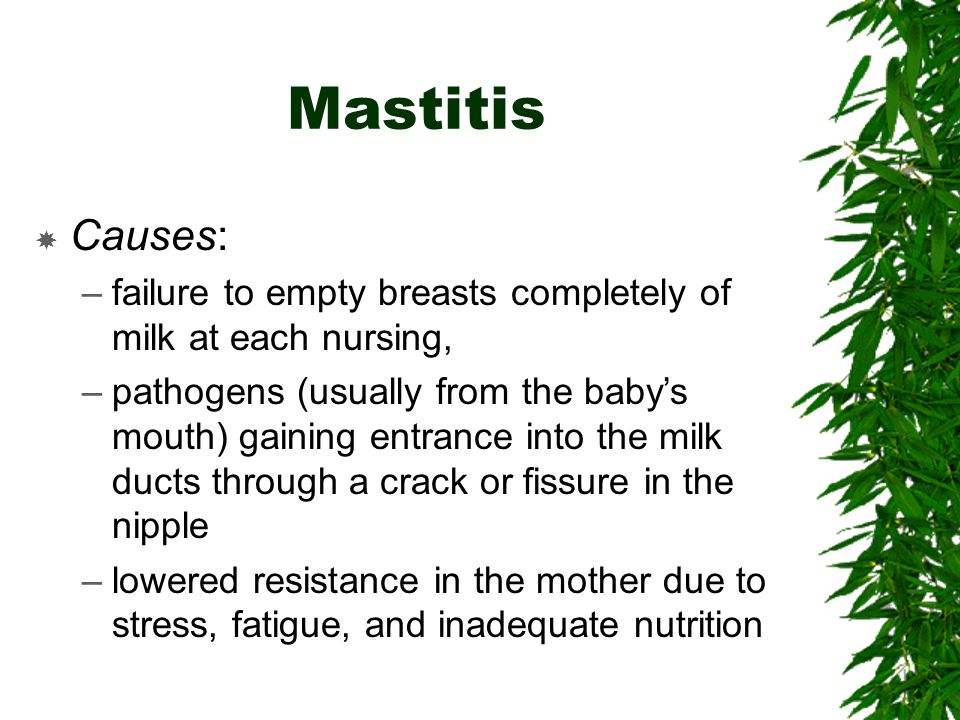
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (such as Advil) for pain. These drugs are safe while breastfeeding and will not harm your baby. Your doctor may prescribe a prescription strength pain reliever if your pain is severe and not relieved with over-the-counter medication.
- In mild cases of mastitis, antibiotics may not be prescribed at all. If you are prescribed antibiotics, finishing the prescription even if you feel better in a few days is very important.
- Frequent feedings: Do not stop breastfeeding from the affected breast, even though it will be painful and you may be taking antibiotics. Frequent emptying of the breast prevents engorgement and clogged ducts that can only make mastitis worse.
- If needed, use a breast pump to relieve pressure and completely empty the breast.
- You can also breastfeed from the unaffected side and supplement with infant formula as needed.
- The infection will not harm the baby because the germs that caused the infection probably came from the baby’s mouth in the first place.

- Breastfeeding should be avoided in the infected breast when an abscess is present.
- Pain relief: A warm compress applied before and after feedings can often provide some relief. A warm bath may work as well.
- If heat is ineffective, ice packs applied after feedings may provide some comfort and relief.
- Avoid using ice packs just before breastfeeding because it can slow down milk flow.
- Drink plenty of water -- at least 10 glasses a day. Eat well-balanced meals and add 500 extra calories a day while breastfeeding. Dehydration and poor nutrition can decrease milk supply and make you feel worse.
Medications for Mastitis
For simple mastitis without an abscess, oral antibiotics are prescribed. Cephalexin (Keflex) and dicloxacillin (Dycill) are two of the most common antibiotics chosen, but a number of others are available. The antibiotic prescribed will depend on your specific situation, your doctor’s preference, and any drug allergies you may have. This medicine is safe to use while breastfeeding and will not harm the baby.
This medicine is safe to use while breastfeeding and will not harm the baby.
Chronic mastitis in nonbreastfeeding women can be complicated. Recurrent episodes of mastitis are common. Occasionally, this type of infection responds poorly to antibiotics. Therefore, close follow-up with your doctor is mandatory.
If the infection worsens in spite of oral antibiotics or if you have a deep abscess requiring surgical treatment, you may be admitted to the hospital for IV antibiotics.
Surgery for an Abscess
If an abscess is present, it must be drained. After injection of a local anesthetic, the doctor may drain an abscess near the surface of the skin either by aspiration with a needle and syringe or by using a small incision. This can be done in the doctor’s office or emergency department.
If the abscess is deep in the breast, however, it may require surgical drainage in the operating room. This procedure is usually done under general anesthesia to minimize pain and completely drain the abscess.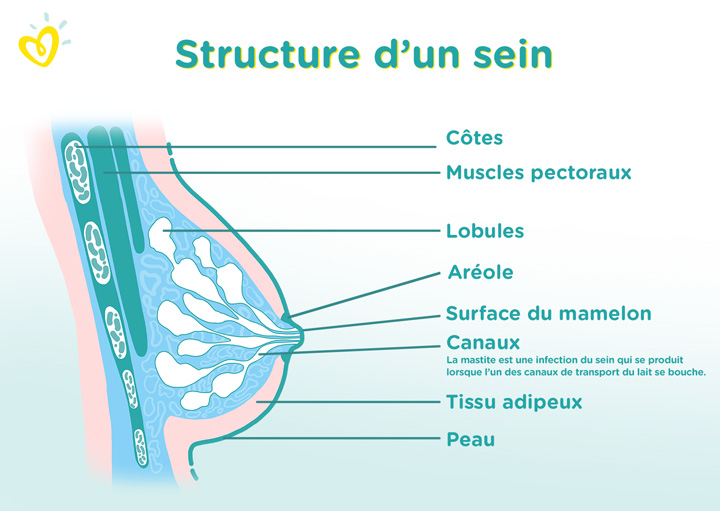 Antibiotics and heat on the area are also used to treat abscesses.
Antibiotics and heat on the area are also used to treat abscesses.
Next Steps
Mastitis does not cause cancer, but cancer can mimic mastitis in appearance. If a breast infection is slow to go away, your health care provider may recommend a mammogram or other tests to rule out cancer.
Follow-Up Care After a Breast Infection
If you have a breast infection, you may be seen for a recheck in 24-48 hours.
- Take all antibiotics as prescribed.
- Take your temperature three times a day for the first 48 hours after treatment begins. Watch for fever.
- Call your doctor if you develop a high fever, vomiting, or increasing redness, swelling, or pain in the breast.
- Follow up with your doctor in one to two weeks to make sure that the infection has gone away. If the infection spreads or an abscess develops, you may require IV antibiotics or surgical treatment.
Mastitis Prevention
Sometimes mastitis is unavoidable. Some women are more susceptible than others, especially those who are breastfeeding for the first time.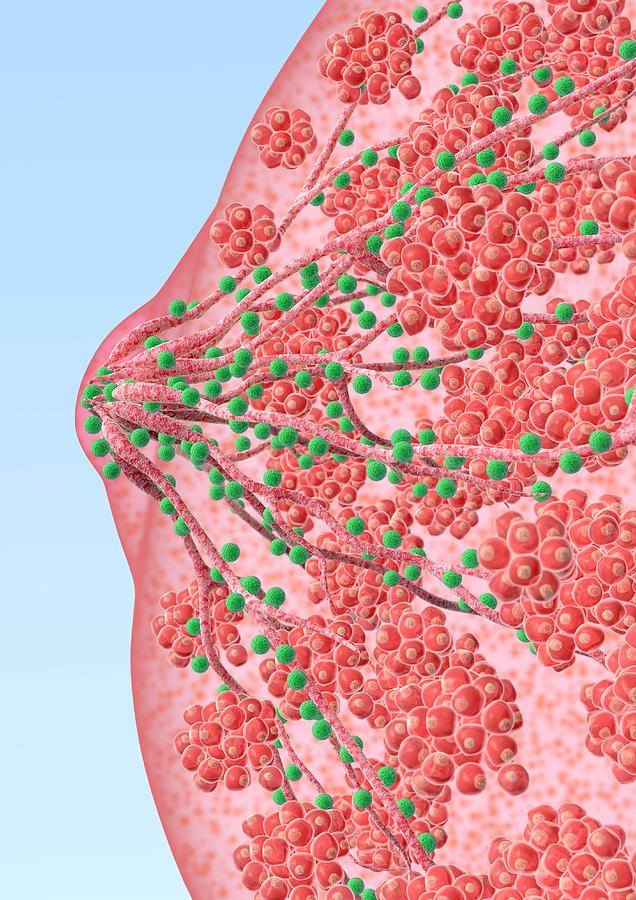 In general, good habits to prevent mastitis include the following:
In general, good habits to prevent mastitis include the following:
- Breastfeed equally from both breasts.
- Empty breasts completely to prevent engorgement and blocked ducts.
- Use good breastfeeding techniques to prevent sore, cracked nipples.
- Allow sore or cracked nipples to air dry.
- Prevent moisture from accumulating in breast pads or bras.
- Avoid dehydration by drinking plenty of fluids.
- Practice careful hygiene: Handwashing, cleaning the nipples, keeping your baby clean.
Outlook for Breast Infections
When treated promptly, the majority of breast infections go away quickly and without serious complications. Most women can and should continue to breastfeed despite an episode of uncomplicated mastitis. With proper treatment, symptoms should begin to resolve within one to two days.
A breast abscess may require surgical drainage, IV antibiotics, and a short hospital stay. A small incision is made and usually heals quite well.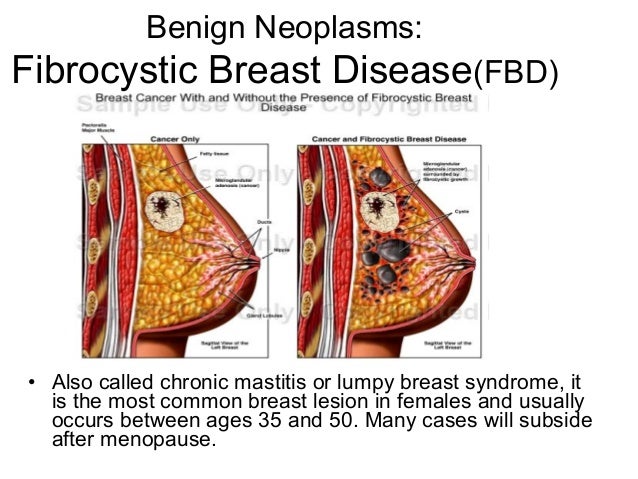 Prognosis for complete recovery is also good.
Prognosis for complete recovery is also good.
Postmenopausal women with breast abscesses have a high rate of return after simple drainage and frequently need to follow up with a surgeon for more definitive treatment. Chronic infection can result if an abscess is not completely drained, and this can result in a poor cosmetic outcome.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
Causes, symptoms, diagnostics and treatment — Doctor Bogolyubov MC Network
Mastitis is an inflammation of the mammary glands that develops when an infection, after a mechanical injury or other negative factors. The disease often develops in lactating women as a result of lactostasis. A mammologist is engaged in the diagnosis and treatment of mastitis - with the timely start of therapy, it is possible to quickly achieve recovery.
When symptoms of inflammation appear, an ultrasound of the mammary glands is done to clarify the diagnosis. The tactics of treatment are selected depending on the severity of the pathological process.
Symptoms of mastitis
The disease begins suddenly. Symptoms of lactational and non-lactational mastitis are similar:
- mammary gland edema;
- the appearance of a dense painful knot;
- redness of the skin over the area of inflammation;
- local increase in skin temperature in the area of induration;
- arching pain and burning in the mammary gland;
- fever;
- deterioration of health - chills, weakness, headache;
- enlarged axillary lymph nodes.
Types of mastitis
-
Serous.
The initial stage of mastitis, in which the first signs of inflammation appear - areas of tissue compaction with clear boundaries. A woman feels weakness and deterioration of health, body temperature rises.
-
Infiltrative.
The focus of inflammation is well palpated, but has no clear boundaries. The gland increases in size, when pressed, severe pain appears. If left untreated, body temperature rises to high values and severe edema develops. -
Destructive.
It is accompanied by severe intoxication of the body - chills, nausea, weakness and high fever appear. Purulent foci are determined in the chest, the mammary gland is hyperemic and hot.
Classification of mastitis by clinical types includes 3 forms of the disease:
-
Postpartum.
It is a consequence of lactostasis in women who are breastfeeding. -
Plasma cell.
Non-lactational mastitis is diagnosed in older women and is accompanied by infiltration of the areolar region with plasma cells. -
Neonatal mastitis.
It develops in both boys and girls under the influence of mother's hormones. Mastitis in children usually resolves on its own.
Mastitis in children usually resolves on its own.
Causes of mastitis
In most cases, inflammation occurs as a result of penetration of pathogenic bacteria into the mammary gland. They can get into the ducts in several ways:
- through cracked nipples and enlarged milk ducts during lactation;
- for mechanical chest trauma;
- from other organs in the presence of foci of inflammation in them.
There are provoking factors that increase the likelihood of developing mastitis:
- mastopathy;
- chronic inflammatory diseases, eg tonsillitis or sinusitis or latent infections;
- previous operations on the mammary glands;
- chest injury, including piercing;
- improperly fitted underwear, such as a tight bra that compresses the mammary glands;
- lactostasis, narrow or blocked milk ducts during breastfeeding.
Complications of mastitis
In case of untimely treatment, mastitis of the breast can lead to serious consequences:
- purulent inflammation of breast tissue;
- necrosis with death of part of the mammary gland;
- change in the shape of the breast due to necrosis;
- sepsis - infection of the blood;
- formation of fistulas on the surface of the chest;
- lymphadenitis - inflammation of the lymph nodes.

Methods for diagnosing mastitis
It is possible to assume the diagnosis already during the examination - the doctor finds out the symptoms and palpates the mammary gland. To assess the condition of the mammary gland, an ultrasound examination is performed, during which the localization of the inflammatory focus, its size and shape are determined. In addition, ultrasound helps to exclude or confirm the presence of a purulent abscess.
In case of lactational mastitis, a bacteriological examination of milk is carried out to identify the bacteria that caused the inflammation. The sensitivity of microorganisms to antibiotics is determined in order to select an effective antibacterial drug.
Treatments for mastitis
Mastitis requires immediate treatment as the disease develops rapidly. In the initial stages, with a serous and infiltrative form, conservative therapy is used: antibacterial drugs, therapeutic compresses are prescribed, electrolyte solutions are infused to relieve symptoms of intoxication. As a rule, with the timely start of treatment, complete recovery occurs in 4-7 days.
As a rule, with the timely start of treatment, complete recovery occurs in 4-7 days.
Acute purulent mastitis requires antibiotics. With an increase in purulent foci, emergency surgical treatment is indicated. The lesion site is opened and the purulent contents are removed, the tissues are treated with antibacterial solutions and sutures are applied.
How to treat mastitis while breastfeeding?
Treatment of mastitis during feeding depends on the severity of the disease. Antibacterial drugs are prescribed and purulent foci are washed. It is recommended to temporarily stop breastfeeding until complete recovery, while it is important to express milk 4-5 times a day to prevent lactostasis. The decision to completely stop lactation is made individually, women may be prescribed drugs to suppress milk production.
Prevention of mastitis
A few simple recommendations will help prevent inflammation:
- wearing comfortable underwear;
- daily breast hygiene;
- timely treatment of diseases of the mammary glands;
- treatment of cracked nipples in the postpartum period;
- correct attachment of the infant to the breast;
- compliance with the feeding regimen for the prevention of milk stagnation;
- regular breast self-examination.

Where to go if you have mastitis?
- The multidisciplinary medical center "Doctor Bogolyubov" employs experienced mammologists who are proficient in various methods of treating mastitis.
- High-precision equipment for the diagnosis of breast diseases.
- Possibility to make an appointment by phone or on the site at a convenient time, without queues.
- Recording availability for the coming days.
How does mastitis start?
The disease begins with a feeling of heaviness in the chest, which gradually increases and turns into pain. An area of compaction appears in the chest, which hurts when pressed. If left untreated, this seal increases, the skin over it turns red and becomes hot, and the body temperature rises.
Why is mastitis dangerous?
The disease can lead to breast suppuration, abscess formation, phlegmon and tissue death. With the progression of purulent mastitis, there is a risk of developing sepsis - blood poisoning. After necrosis, the breast may remain deformed, increasing the risk of developing mastopathy and cancer.
After necrosis, the breast may remain deformed, increasing the risk of developing mastopathy and cancer.
What to do with mastitis?
At the first symptoms of inflammation in the mammary gland, you should seek medical help as soon as possible, since with timely treatment, the disease is treated with medication. If mastitis occurs in breastfeeding women, you should express milk or give a light massage to ensure the flow of milk, and consult a doctor.
Mastitis: symptoms and treatment | Philips Avent
search support iconSearch keywords
Home ›› Mastitis in a nursing mother: symptoms and treatment
Home ›› Mastitis in a nursing mother: symptoms and treatment
↑ Top
doesn't always go easy. Along with the individual aspects of breastfeeding, there are some general problems that new breastfeeding mothers may face.
One of these is mastitis, an inflammatory disease that causes tenderness and tenderness in the breast tissue.
The frequency of lactational mastitis among women in different countries ranges from 2% to 33% and averages about 10%*.
Mastitis in breastfeeding women is caused by a bacterial infection of the milk ducts that enters through cracks, irritation of the nipple, or a nipple piercing.
Lactational mastitis is dangerous because it can cause pain while breastfeeding, interfere with the bonding process between mother and baby, or even interfere with milk production.
To protect the health and comfort of mother and child, and the mother's milk supply, this issue must be addressed urgently.
So, here are the answers to the most frequently asked questions about mastitis and the fight against it: “How does mastitis occur?”, “What are the symptoms of mastitis?” and "Is it possible to breastfeed with mastitis?".
Ask your doctor for more information.
Signs of mastitis
What does mastitis feel like? In addition to pain and discomfort, symptoms of mastitis can also include fatigue and a feeling of exhaustion.
How mastitis manifests:
- fever (>38.5°C) and/or flu-like symptoms;
- nausea;
- vomiting;
- yellowish discharge from the nipple;
- chest warm or hot to the touch;
- pink or red breasts.
These symptoms of mastitis are similar to the symptoms of breast engorgement, but there is a fundamental difference between these conditions. Mastitis differs from engorgement in that it usually only affects one breast, not both.
Causes of mastitis
Mastitis can develop in a new mother at any time, but it usually occurs within the first two to three weeks after childbirth. A common cause of this disease is long breaks between feedings - for example, when the baby begins to sleep through the night.
Other possible causes of mastitis are:
- incorrect breastfeeding;
- incomplete outflow of milk from the mammary glands, for example, due to blockage of the milk duct;
- unattended breast engorgement;
- regular pressure on some part of the breast, wearing tight clothing;
- chest injury caused by injury or impact.
In short: mastitis usually develops as a result of too much milk in the breast, known as milk stasis. Stagnation of milk provokes the growth of bacteria, which causes mastitis and symptoms of pain and fever. Therefore, to prevent mastitis and stagnation of milk, it is important to make sure that it is removed from the breast properly.
Blockage of the milk ducts can also be the cause. Mastitis is indeed caused by milk stagnation or too long milk in the breast, but this condition and the subsequent symptoms of mastitis - fever and pain - are precisely due to the rapid multiplication of bacteria due to milk stagnation.
Prevention of mastitis while breastfeeding
The good news is that there are many ways to prevent mastitis. Below you will find some tips on how to avoid mastitis.
1. Care for your breasts to prevent nipple irritation. Proper breast care can help prevent mastitis by gently massaging and keeping your nipples dry with soft bra pads.
Find out more about breast care in our article here.
2. Feed your baby often. For complete emptying of the breast, it is important to feed regularly and on time. Even if the baby is sleeping, it should be woken up when it's time for feeding. If the mother cannot be with the baby during feeding, she should express milk from the breast using a breast pump.
Choose an easy-to-use breast pump, such as a single electric breast pump. It allows you to express gently and naturally thanks to its special Natural Motion technology. Many of the complications of breastfeeding can be avoided if the baby latch on properly. Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
4. Wean your baby gradually. To minimize the chance of complications, it is necessary to reduce milk production by gradually reducing the number of breastfeeds.
If you are interested in the topic of stopping breastfeeding, check out our tips for weaning your baby in the article at the link.
Treatment of mastitis in women
One of the most common questions that breastfeeding mothers face with mastitis is: "Can I continue to breastfeed?" Answer: yes. What's more, breastfeeding for mastitis can help clear the infection without causing harm or side effects.
An important point: if you have symptoms of mastitis, contact your doctor immediately. Doctors usually prescribe antibiotics (eg, acetaminophen or ibuprofen) to relieve symptoms of mastitis after making sure the prescribed drug is safe for breastfeeding.
Mastitis can be uncomfortable, but there is no reason to panic or despair. This is a common problem that many new mothers experience when breastfeeding for the first time. By following the advice in this article, you can reduce the likelihood of developing mastitis, but if something bothers you, you should seek the help of a specialist.