What is home birth
Planned Home Birth | ACOG
ABSTRACT: In the United States, approximately 35,000 births (0.9%) per year occur in the home. Approximately one fourth of these births are unplanned or unattended. Although the American College of Obstetricians and Gynecologists believes that hospitals and accredited birth centers are the safest settings for birth, each woman has the right to make a medically informed decision about delivery. Importantly, women should be informed that several factors are critical to reducing perinatal mortality rates and achieving favorable home birth outcomes. These factors include the appropriate selection of candidates for home birth; the availability of a certified nurse–midwife, certified midwife or midwife whose education and licensure meet International Confederation of Midwives’ Global Standards for Midwifery Education, or physician practicing obstetrics within an integrated and regulated health system; ready access to consultation; and access to safe and timely transport to nearby hospitals. The Committee on Obstetric Practice considers fetal malpresentation, multiple gestation, or prior cesarean delivery to be an absolute contraindication to planned home birth.
Recommendations
Women inquiring about planned home birth should be informed of its risks and benefits based on recent evidence. Specifically, they should be informed that although planned home birth is associated with fewer maternal interventions than planned hospital birth, it also is associated with a more than twofold increased risk of perinatal death (1–2 in 1,000) and a threefold increased risk of neonatal seizures or serious neurologic dysfunction (0.4–0.6 in 1,000). These observations may reflect fewer obstetric risk factors among women planning home birth compared with those planning hospital birth. Although the American College of Obstetricians and Gynecologists (the College) believes that hospitals and accredited birth centers are the safest settings for birth, each woman has the right to make a medically informed decision about delivery.
Women should be informed that several factors are critical to reducing perinatal mortality rates and achieving favorable home birth outcomes. These factors include the appropriate selection of candidates for home birth; the availability of a certified nurse–midwife, certified midwife or midwife whose education and licensure meet International Confederation of Midwives’ Global Standards for Midwifery Education, or physician practicing obstetrics within an integrated and regulated health system; ready access to consultation; and access to safe and timely transport to nearby hospitals.
The Committee on Obstetric Practice considers fetal malpresentation, multiple gestation, or prior cesarean delivery to be an absolute contraindication to planned home birth.
In the United States, approximately 35,000 births (0.9%) per year occur in the home 1. Approximately one fourth of these births are unplanned or unattended 2. Among women who originally intend to give birth in a hospital or those who make no provisions for professional care during childbirth, home births are associated with high rates of perinatal and neonatal mortality 3.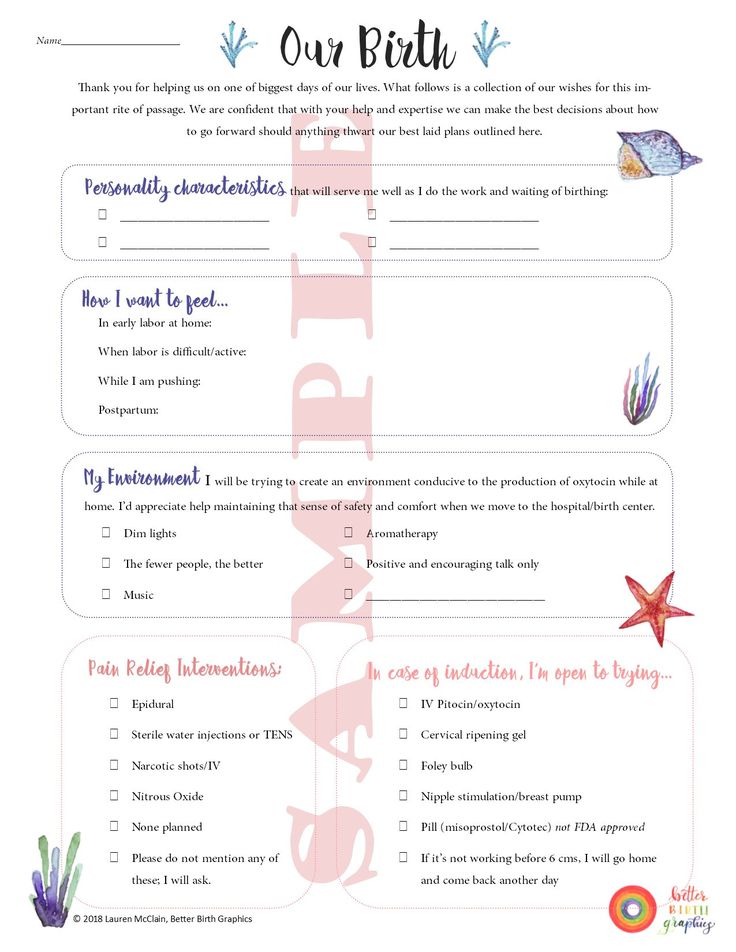 The relative risk versus benefit of a planned home birth, however, remains the subject of debate.
The relative risk versus benefit of a planned home birth, however, remains the subject of debate.
High-quality evidence that can inform this debate is limited. To date, there have been no adequate randomized clinical trials of planned home birth 4. In developed countries where home birth is more common than in the United States, attempts to conduct such studies have been unsuccessful, largely because pregnant women have been reluctant to participate in clinical trials that involve randomization to home or hospital birth 5 6. Consequently, most information on planned home births comes from observational studies. Observational studies of planned home birth often are limited by methodological problems, including small sample sizes 7 8 9 10; lack of an appropriate control group 11 12 13 14 15; reliance on birth certificate data with inherent ascertainment problems 2 16 17 18; reliance on voluntary submission of data or self-reporting 7 12 14 15 19; limited ability to distinguish accurately between planned and unplanned home births 16 20; variation in the skill, training, and certification of the birth attendant 14 15 16 21; and an inability to account for and accurately attribute adverse outcomes associated with antepartum or intrapartum transfers 8 16 22. Some recent observational studies overcome many of these limitations, describing planned home births within tightly regulated and integrated health care systems, attended by highly trained licensed midwives with ready access to consultation and safe, timely transport to nearby hospitals 7 8 10 11 16 19 23 24 25 26 27 28. However, these data may not be generalizable to many birth settings in the United States where such integrated services are lacking. For the same reasons, clinical guidelines for the intrapartum care of women in the United States that are based on these results and are supportive of planned home birth for low-risk term pregnancies also may not currently be generalizable 29. Furthermore, no studies are of sufficient size to compare maternal mortality between planned home and hospital birth and few, when considered alone, are large enough to compare perinatal and neonatal mortality rates. Despite these limitations, when viewed collectively, recent reports clarify a number of important issues regarding the maternal and newborn outcomes of planned home birth when compared with planned hospital births.
Some recent observational studies overcome many of these limitations, describing planned home births within tightly regulated and integrated health care systems, attended by highly trained licensed midwives with ready access to consultation and safe, timely transport to nearby hospitals 7 8 10 11 16 19 23 24 25 26 27 28. However, these data may not be generalizable to many birth settings in the United States where such integrated services are lacking. For the same reasons, clinical guidelines for the intrapartum care of women in the United States that are based on these results and are supportive of planned home birth for low-risk term pregnancies also may not currently be generalizable 29. Furthermore, no studies are of sufficient size to compare maternal mortality between planned home and hospital birth and few, when considered alone, are large enough to compare perinatal and neonatal mortality rates. Despite these limitations, when viewed collectively, recent reports clarify a number of important issues regarding the maternal and newborn outcomes of planned home birth when compared with planned hospital births.
Women planning a home birth may do so for a number of reasons, often out of a desire to avoid medical interventions and the hospital atmosphere 30. Recent studies have found that when compared with planned hospital births, planned home births are associated with fewer maternal interventions, including labor induction or augmentation, regional analgesia, electronic fetal heart rate monitoring, episiotomy, operative vaginal delivery, and cesarean delivery Table 1. Planned home births also are associated with fewer vaginal, perineal, and third-degree or fourth-degree lacerations and less maternal infectious morbidity 18 27 31 32. These observations may reflect fewer obstetric risk factors among women planning home births compared with those planning hospital births. Parous women comprise a larger proportion of those planning out-of-hospital births 27 32. Compared with nulliparous women, parous women collectively experience significantly lower rates of obstetric intervention, maternal morbidity, and neonatal morbidity and mortality, regardless of birth location. Those planning home births also are more likely to deliver in that setting than nulliparous women 15 27 33. For these reasons, recommendations regarding the intrapartum care of healthy nulliparous and parous women may differ outside of the United States 29. Also, proportionately more home births are attended by midwives than planned hospital births, and randomized trials show that midwife-led care is associated with fewer intrapartum interventions 34.
Those planning home births also are more likely to deliver in that setting than nulliparous women 15 27 33. For these reasons, recommendations regarding the intrapartum care of healthy nulliparous and parous women may differ outside of the United States 29. Also, proportionately more home births are attended by midwives than planned hospital births, and randomized trials show that midwife-led care is associated with fewer intrapartum interventions 34.
Strict criteria are necessary to guide selection of appropriate candidates for planned home birth. In the United States, for example, where selection criteria may not be applied broadly, intrapartum (1.3 in 1,000) and neonatal (0.76 in 1,000) deaths among low-risk women planning home birth are more common than expected when compared with rates for low-risk women planning hospital delivery (0.4 in 1,000 and 0.17 in 1,000, respectively), consistent with the findings of an earlier meta-analysis 15 31 33. Additional evidence from the United States shows that planned home birth of a breech-presenting fetus is associated with an intrapartum mortality rate of 13. 5 in 1,000 and neonatal mortality rate of 9.2 in 1,000 15. United States data limited to singleton-term pregnancies demonstrate a higher risk of 5-minute Apgar scores less than 7, less than 4, and 0; perinatal death; and neonatal seizures with planned home birth, although the absolute risks remain low Table 2 17 18 32.
5 in 1,000 and neonatal mortality rate of 9.2 in 1,000 15. United States data limited to singleton-term pregnancies demonstrate a higher risk of 5-minute Apgar scores less than 7, less than 4, and 0; perinatal death; and neonatal seizures with planned home birth, although the absolute risks remain low Table 2 17 18 32.
Although patients with one prior cesarean delivery were considered candidates for home birth in two Canadian studies, details of the outcomes specific to patients attempting home vaginal birth after cesarean delivery were not provided 24 25. In England, women planning a home trial of labor after cesarean delivery (TOLAC) exhibited fewer obstetric risk factors, were more likely to deliver vaginally, and experienced similar maternal and perinatal outcomes compared with those planning an in-hospital TOLAC 35. In contrast, a recent U.S. study showed that planned home TOLAC was associated with an intrapartum fetal death rate of 2.9 in 1,000, which is higher than the reported rate of 0. 13 in 1,000 for planned hospital TOLAC 36 37. This observation is of particular concern in light of the increasing number of home vaginal births after cesarean delivery 38. Because of the risks associated with TOLAC, and specifically considering that uterine rupture and other complications may be unpredictable, the College recommends that TOLAC be undertaken in facilities with trained staff and the ability to begin an emergency cesarean delivery within a time interval that best incorporates maternal and fetal risks and benefits with the provision of emergency care.
13 in 1,000 for planned hospital TOLAC 36 37. This observation is of particular concern in light of the increasing number of home vaginal births after cesarean delivery 38. Because of the risks associated with TOLAC, and specifically considering that uterine rupture and other complications may be unpredictable, the College recommends that TOLAC be undertaken in facilities with trained staff and the ability to begin an emergency cesarean delivery within a time interval that best incorporates maternal and fetal risks and benefits with the provision of emergency care.
The decision to offer and pursue TOLAC in a setting in which the option of immediate cesarean delivery is more limited should be considered carefully by patients and their health care providers. In such situations, the best alternative may be to refer patients to facilities with available resources. Health care providers and insurers should do all they can to facilitate transfer of care or comanagement in support of a desired TOLAC, and such plans should be initiated early in the course of antenatal care 39.
Recent cohort studies reporting comparable perinatal mortality rates among planned home and hospital births describe the use of strict selection criteria for appropriate candidates 23 24 25. These criteria include the absence of any preexisting maternal disease, the absence of significant disease arising during the pregnancy, a singleton fetus, a cephalic presentation, gestational age greater than 36–37 completed weeks and less than 41–42 completed weeks of pregnancy, labor that is spontaneous or induced as an outpatient, and that the patient has not been transferred from another referring hospital. In the absence of such criteria, planned home birth is clearly associated with a higher risk of perinatal death 15 26 40. The Committee on Obstetric Practice considers fetal malpresentation, multiple gestation, or prior cesarean delivery to be an absolute contraindication to planned home birth.
Another factor influencing the safety of planned home birth is the availability of safe and timely intrapartum transfer of the laboring patient. The reported risk of needing an intrapartum transport to a hospital is 23–37% for nulliparous women and 4–9% for multiparous women. Most of these intrapartum transports are for lack of progress in labor, nonreassuring fetal status, need for pain relief, hypertension, bleeding, and fetal malposition 27 41 42. The relatively low perinatal and newborn mortality rates reported for planned home births from Ontario, British Columbia, and the Netherlands were from highly integrated health care systems with established criteria and provisions for emergency intrapartum transport 23 24 25. Cohort studies conducted in areas without such integrated systems and those where the receiving hospital may be remote, with the potential for delayed or prolonged intrapartum transport, generally report higher rates of intrapartum and neonatal death 6 9 11 15 22. Even in regions with integrated care systems, increasing distance from the hospital is associated with longer transfer times and the potential for increased adverse outcomes.
The reported risk of needing an intrapartum transport to a hospital is 23–37% for nulliparous women and 4–9% for multiparous women. Most of these intrapartum transports are for lack of progress in labor, nonreassuring fetal status, need for pain relief, hypertension, bleeding, and fetal malposition 27 41 42. The relatively low perinatal and newborn mortality rates reported for planned home births from Ontario, British Columbia, and the Netherlands were from highly integrated health care systems with established criteria and provisions for emergency intrapartum transport 23 24 25. Cohort studies conducted in areas without such integrated systems and those where the receiving hospital may be remote, with the potential for delayed or prolonged intrapartum transport, generally report higher rates of intrapartum and neonatal death 6 9 11 15 22. Even in regions with integrated care systems, increasing distance from the hospital is associated with longer transfer times and the potential for increased adverse outcomes. However, no specific thresholds for time or distance have been identified 43 44. The College believes that the availability of timely transfer and an existing arrangement with a hospital for such transfers is a requirement for consideration of a home birth. When antepartum, intrapartum, or postpartum transfer of a woman from home to a hospital occurs, the receiving health care provider should maintain a nonjudgmental demeanor with regard to the woman and those individuals accompanying her to the hospital.
However, no specific thresholds for time or distance have been identified 43 44. The College believes that the availability of timely transfer and an existing arrangement with a hospital for such transfers is a requirement for consideration of a home birth. When antepartum, intrapartum, or postpartum transfer of a woman from home to a hospital occurs, the receiving health care provider should maintain a nonjudgmental demeanor with regard to the woman and those individuals accompanying her to the hospital.
A characteristic common to those cohort studies reporting comparable rates of perinatal mortality is the provision of care by uniformly highly educated and trained certified midwives who are well integrated into the health care system 23 24 25 27. In the United States, certified nurse–midwives and certified midwives are certified by the American Midwifery Certification Board. This certification depends on the completion of an accredited educational program and meeting standards set by the American Midwifery Certification Board. In comparison with planned out-of-hospital births attended by American Midwifery Certification Board-certified midwives, planned out-of-hospital births by midwives who do not hold this certification have higher perinatal morbidity and mortality rates 18. At this time, for quality and safety reasons, the College specifically supports the provision of care by midwives who are certified by the American Midwifery Certification Board (or its predecessor organizations) or whose education and licensure meet the International Confederation of Midwives Global Standards for Midwifery Education. The College does not support provision of care by midwives who do not meet these standards.
In comparison with planned out-of-hospital births attended by American Midwifery Certification Board-certified midwives, planned out-of-hospital births by midwives who do not hold this certification have higher perinatal morbidity and mortality rates 18. At this time, for quality and safety reasons, the College specifically supports the provision of care by midwives who are certified by the American Midwifery Certification Board (or its predecessor organizations) or whose education and licensure meet the International Confederation of Midwives Global Standards for Midwifery Education. The College does not support provision of care by midwives who do not meet these standards.
Although the College believes that hospitals and accredited birth centers are the safest settings for birth, each woman has the right to make a medically informed decision about delivery 45. Importantly, women should be informed that several factors are critical to reducing perinatal mortality rates and achieving favorable home birth outcomes. These factors include the appropriate selection of candidates for home birth; the availability of a certified nurse–midwife, certified midwife or midwife whose education and licensure meet International Confederation of Midwives’ Global Standards for Midwifery Education, or physician practicing obstetrics within an integrated and regulated health system; ready access to consultation; and access to safe and timely transport to nearby hospitals.
These factors include the appropriate selection of candidates for home birth; the availability of a certified nurse–midwife, certified midwife or midwife whose education and licensure meet International Confederation of Midwives’ Global Standards for Midwifery Education, or physician practicing obstetrics within an integrated and regulated health system; ready access to consultation; and access to safe and timely transport to nearby hospitals.
For More Information
The American College of Obstetricians and Gynecologists has identified additional resources on topics related to this document that may be helpful for ob-gyns, other health care providers, and patients. You may view these resources at www.acog.org/More-Info/PlannedHomeBirth .
These resources are for information only and are not meant to be comprehensive. Referral to these resources does not imply the American College of Obstetricians and Gynecologists’ endorsement of the organization, the organization’s website, or the content of the resource. The resources may change without notice.
The resources may change without notice.
Midwives Explain What a Home Birth Really Means
The COVID-19 pandemic has presented a unique set of emotionally distressing challenges for pregnant women. From concerns about their health and that of their baby, to the prospect of having to go into labor and birth alone in hospitals, mothers-to-be are facing extreme fear and uncertainty in an already vulnerable time.
With many hospitals operating near or at capacity with limited resources as they take on the flood of Coronavirus patients, many expectant mothers are rethinking their birthing plans—and considering the option of a home birth which, typically, only about one percent of mothers do each year. Midwives are being inundated with home-birth requests. Here, the birthing experts speak on commonly asked questions about home birth, the benefits and potential risks of doing so, and why the decision to have one should be made with careful consideration.
What Is a Home Birth?
"A home birth is exactly what it sounds like—when someone decides to birth their baby in their own home!" explain licensed midwives Robina Khalid and Tanya Wills of New York City's Small Things Grow Midwifery in a shared interview. "People who have a planned home birth, in the absence of complications, will never need to go to the hospital." While someone can birth at home without a midwife, the vast majority of people who choose home birth will work with one. As for who else is present, it varies from family to family; oftentimes it’s just the birthing person, their support person, and a midwife. "In general, home birth is a quiet, intimate experience," explains Sara Howard, a Los Angeles-based midwife and educator at healthcare center LOOM. "Lights can remain dim, music can play in the background, and partners and doulas can provide support no matter where the birthing person wants to be physically, whether that's in a bed, tub, or somewhere else."
"People who have a planned home birth, in the absence of complications, will never need to go to the hospital." While someone can birth at home without a midwife, the vast majority of people who choose home birth will work with one. As for who else is present, it varies from family to family; oftentimes it’s just the birthing person, their support person, and a midwife. "In general, home birth is a quiet, intimate experience," explains Sara Howard, a Los Angeles-based midwife and educator at healthcare center LOOM. "Lights can remain dim, music can play in the background, and partners and doulas can provide support no matter where the birthing person wants to be physically, whether that's in a bed, tub, or somewhere else."
What Role Does a Midwife Play in a Home Birth?
The midwife is there to safeguard the health and safety of the birthing person and the baby. While many midwives vary in credentials in the U.S.—there are licensed midwives, certified professional midwives, certified nurse midwives, and traditional midwives, for example—practices are similar. "I’m licensed by the same medical board that licenses doctors," explains Howard. "I carry a doppler to listen to the baby’s heartbeat in labor, medications to stop bleeding after birth, oxygen, suturing equipment, IVs and antibiotics, and more. I’m certified in neonatal resuscitation and infant CPR, as well as trained in advanced fetal monitoring." A midwife may involve herself during birth by "catching the baby" or, during the immediate postpartum, ensuring the placenta is birthed safely, keeping a watchful eye on bleeding, giving stitches when needed, performing a head-to-toe newborn exam (including weight and measurement), and assisting with breastfeeding. "In the best case scenario a midwife is just there to remind the birthing person of their own strength and to help ensure the birthing person feels safe enough to do what only they can do—birth their baby."
"I’m licensed by the same medical board that licenses doctors," explains Howard. "I carry a doppler to listen to the baby’s heartbeat in labor, medications to stop bleeding after birth, oxygen, suturing equipment, IVs and antibiotics, and more. I’m certified in neonatal resuscitation and infant CPR, as well as trained in advanced fetal monitoring." A midwife may involve herself during birth by "catching the baby" or, during the immediate postpartum, ensuring the placenta is birthed safely, keeping a watchful eye on bleeding, giving stitches when needed, performing a head-to-toe newborn exam (including weight and measurement), and assisting with breastfeeding. "In the best case scenario a midwife is just there to remind the birthing person of their own strength and to help ensure the birthing person feels safe enough to do what only they can do—birth their baby."
What Are Some Benefits of a Home Birth?
"Home birth may be the best chance the average American person has at having a physiologic birth—a birth that occurs without intervention," explain Khalid and Wills. This method has been shown to carry benefits to parent and baby, including a better transition to breathing for the baby, less genital trauma for the birthing person, quicker recovery from birth, increased rates of breastfeeding, improved parent-infant attachment, and decreased incidence of postpartum depression. Planned home births attended by a registered midwife have been associated with reduced rates of obstetric interventions, such as C-sections, and other adverse perinatal outcomes. Plus, there is an inherent bond that's been formed between mother and midwife. "By the time we arrive at the birth, there is a deep understanding of the person, baby, and family we are caring for—there is trust," say Khalid and Wills. "People can birth anywhere they like on their own turf while listening to their bodies and allowing their own innate wisdom to guide them."
This method has been shown to carry benefits to parent and baby, including a better transition to breathing for the baby, less genital trauma for the birthing person, quicker recovery from birth, increased rates of breastfeeding, improved parent-infant attachment, and decreased incidence of postpartum depression. Planned home births attended by a registered midwife have been associated with reduced rates of obstetric interventions, such as C-sections, and other adverse perinatal outcomes. Plus, there is an inherent bond that's been formed between mother and midwife. "By the time we arrive at the birth, there is a deep understanding of the person, baby, and family we are caring for—there is trust," say Khalid and Wills. "People can birth anywhere they like on their own turf while listening to their bodies and allowing their own innate wisdom to guide them."
How Is Labor Pain Managed During a Home Birth?
"Epidurals are an amazing technology that many people choose to use in the U. S., but there are many other people who place value on the experience of labor and birth as it is," explain Khalid and Wills. "We have a belief in our culture that pain is always bad or wrong. And is labor painful? Yes. But pain is different than suffering, and pain is sometimes instructive." For example, the pair believe that having full sensation when pushing helps people know how to push—and when to back off—which helps people tear less than they would during guided pushing. Moreover, birthing at home gives the birthing person the opportunity to move more freely, as well as take advantage of multiple spaces, such as a bed and a pool of water. "Laboring in a big pool of water at body temperature is probably the most soothing tool we have at all to relieve pain at home," explains Howard. "Virtually all people who labor at home will utilize a birth pool for that very reason." Another way to relieve pain naturally is deep, focused breathing. "When you relax and breathe, your muscles get more oxygen, which reduces pain," she explains.
S., but there are many other people who place value on the experience of labor and birth as it is," explain Khalid and Wills. "We have a belief in our culture that pain is always bad or wrong. And is labor painful? Yes. But pain is different than suffering, and pain is sometimes instructive." For example, the pair believe that having full sensation when pushing helps people know how to push—and when to back off—which helps people tear less than they would during guided pushing. Moreover, birthing at home gives the birthing person the opportunity to move more freely, as well as take advantage of multiple spaces, such as a bed and a pool of water. "Laboring in a big pool of water at body temperature is probably the most soothing tool we have at all to relieve pain at home," explains Howard. "Virtually all people who labor at home will utilize a birth pool for that very reason." Another way to relieve pain naturally is deep, focused breathing. "When you relax and breathe, your muscles get more oxygen, which reduces pain," she explains. "Whereas when people are scared and tense, their muscles constrict and they feel more pain."
"Whereas when people are scared and tense, their muscles constrict and they feel more pain."
What Are the Safety Concerns Around Home Birth?
In order to be a good candidate for home birth, a person and a pregnancy need to be “low-risk,” which generally means that there are no major medical problems present either before or during the pregnancy, says Howard. Generally, high-risk factors may include high maternal age or previous C-section delivery. The best way for an expectant mother to know for sure is to talk to their doctor, as well as consult a midwife about their specific history and situation. As for unexpected medical emergencies that could arise during an at-home birth, Howard says the most significant risk is the delay in getting from your home to a hospital, which is why many medical experts recommend that an at-home birth should take place within 15 minutes of a hospital. "The majority of problems that occur during labor and birth present warning signs, and midwives are extensively trained in recognizing these warning signs," explain Khalid and Wills. "Our intimate knowledge of our clients, as well as years of observing people's labor while sitting with them for hours on end, gives us the ability to interpret what’s going on, and decide whether staying at home is still appropriate." The pair also stresses that most transfers are not emergencies, and that the most common reason for going to the hospital during labor is exhaustion or a very long labor that might need some augmentation or pain relief.
"Our intimate knowledge of our clients, as well as years of observing people's labor while sitting with them for hours on end, gives us the ability to interpret what’s going on, and decide whether staying at home is still appropriate." The pair also stresses that most transfers are not emergencies, and that the most common reason for going to the hospital during labor is exhaustion or a very long labor that might need some augmentation or pain relief.
How Can I Decide Between a Home Birth and a Hospital Birth?
In additional to consulting medical professionals, it's important to gauge your personal comfort level with the idea of a home birth. "Home birth can be an incredibly warm, sweet way to bring your baby into the world—but it isn’t for everybody," says Howard. "There are times when epidurals and surgical births are terrific, life-saving things that we can all be grateful for. Deciding where to birth is personal. Take the time to gather the information and resources you need to ensure that you’ve made the best choice for you and your family.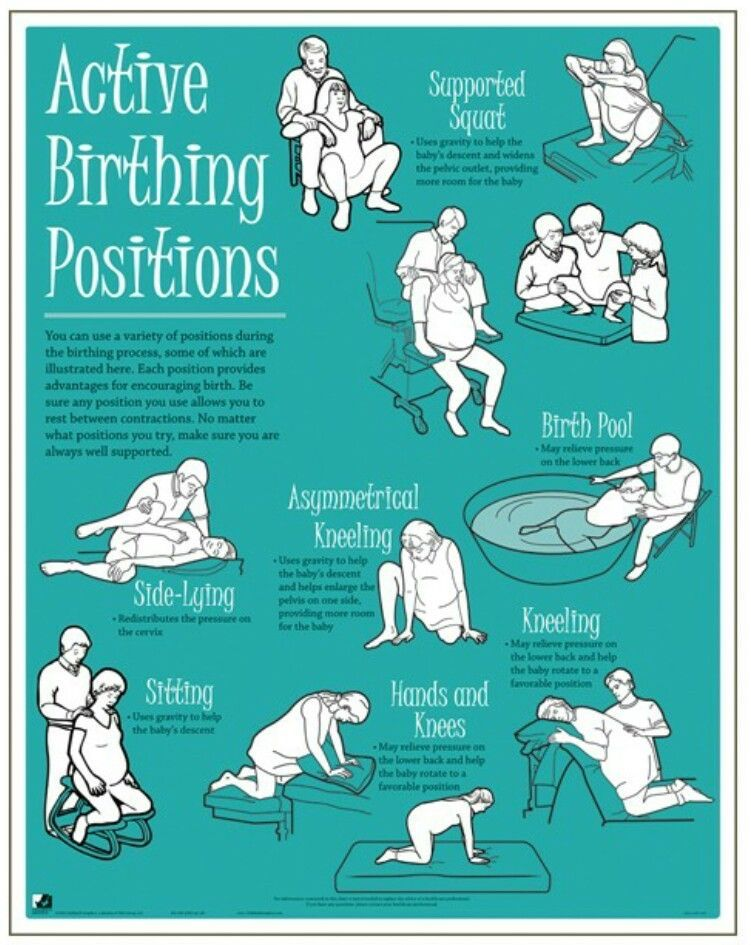 You know best." As far as the timing of a mother-to-be's decision, the earlier the better, especially in the instance of home birthing. "Things get tricky when it’s very late in the pregnancy and folks want to have a home birth, especially because most midwives have small practices that fill up early," explain Khalid and Wills, who released an open letter to address increased interest in home birth during the COVID-19 pandemic. "Moreover, creating trust and familiarity between the midwife and the family over time is key to a safe and healthy experience." Ultimately, the decision to have a home birth is not one to be made out of fear and panic, even in unprecedented times—fundamentally trusting the location of one's birthing is the best way to ensure safety for the mother and child, they stress. "If after diligent and thoughtful research, the autonomy and safety of home birth remains appealing, pregnant people are always welcome to contact individual practices, with the understanding that most practices book up far in advance," Khalid and Wills note in their address.
You know best." As far as the timing of a mother-to-be's decision, the earlier the better, especially in the instance of home birthing. "Things get tricky when it’s very late in the pregnancy and folks want to have a home birth, especially because most midwives have small practices that fill up early," explain Khalid and Wills, who released an open letter to address increased interest in home birth during the COVID-19 pandemic. "Moreover, creating trust and familiarity between the midwife and the family over time is key to a safe and healthy experience." Ultimately, the decision to have a home birth is not one to be made out of fear and panic, even in unprecedented times—fundamentally trusting the location of one's birthing is the best way to ensure safety for the mother and child, they stress. "If after diligent and thoughtful research, the autonomy and safety of home birth remains appealing, pregnant people are always welcome to contact individual practices, with the understanding that most practices book up far in advance," Khalid and Wills note in their address.
We give birth like at home - articles from the specialists of the clinic "Mother and Child"
Zimina Natalya Nikolaevna
Obstetrician-gynecologist
MD GROUP Clinical Hospital
Presentation of home birth
The most typical arguments of supporters of home births:
- A woman's body is designed specifically to give birth to children. By nature, it has all the necessary strengths and capabilities to give birth to a healthy child on its own, which means that the help of a doctor in this process is completely unnecessary.
- The maternity hospital is not needed, because the atmosphere in it is official, hospital, and this does not contribute to relaxation in contractions and the opening of the cervix.
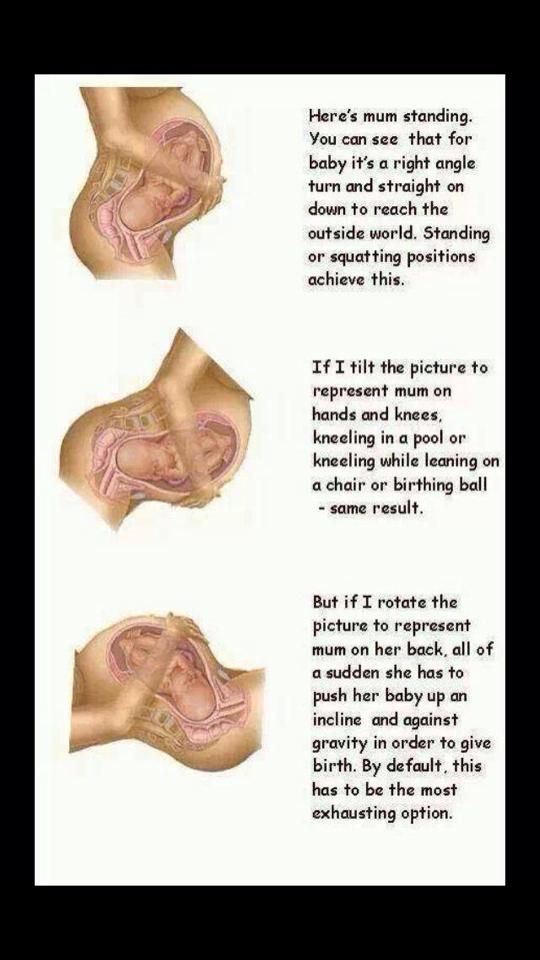
- When giving birth at home, you can take any position that is comfortable for the woman.
- And at home, you can give birth in the water (in the bath), or at least just relieve contractions by immersion in water.

- During home birth, not strangers (doctors, midwives) will be nearby, but the husband, relatives or friends.
- From the first minutes of birth, the child will be constantly next to his mother, he will not be supplemented, he will not be subjected to unnecessary manipulations and examinations.
Well, ideally, supporters of home births present them like this: effective contractions begin at 40 weeks, the first stage of labor lasts no longer than 10-12 hours. At this time, the woman in labor behaves in a way that is convenient for her, takes comfortable postures, uses techniques to anesthetize contractions (massage, breathing, water). Then comes the complete opening of the cervix, water spontaneously pours out, there are attempts, during which a healthy baby is born without much effort. The child is immediately applied to the mother's breast - he sucks it as much as he wants, the umbilical cord is cut only after the end of the pulsation. Mom has no breaks, the child is absolutely healthy. In general, everyone is satisfied and happy.
In general, everyone is satisfied and happy.
Actually
The picture of home birth is presented, of course, idyllically. And how happy ordinary women would be, and doctors too, if every birth went that way. But it’s not always possible to give birth the way you breathe. In childbirth or immediately after them, various unpleasant situations can arise with a woman or a child. We will not list them so as not to upset anyone. Let's just say that often the life and health of a mother and baby depend precisely on how quickly they received medical assistance . But what can be done at home in such a situation? The only thing is to call an ambulance, because it is impossible to help a child with asphyxia or a woman with bleeding or high blood pressure without certain drugs, equipment, and simply medical skills. But after all, one of the specialists will be present at the birth with the expectant mother? Good obstetricians and gynecologists are well aware of the high risk of home births, so they do not accept births at home, and a midwife, even with experience, will only cope with the simplest situation. In addition, many so-called spiritual obstetricians, as a rule, do not even have a higher, often secondary medical education, and, of course, they do not bear any legal responsibility for the outcome of childbirth. And it happens that sometimes in home births there is no midwife at all (did not come or the woman was convinced that she was not needed). Therefore, of course, we can agree that the home environment helps a lot, but will it be possible to give birth in it in the event of some non-standard or difficult situation?
In addition, many so-called spiritual obstetricians, as a rule, do not even have a higher, often secondary medical education, and, of course, they do not bear any legal responsibility for the outcome of childbirth. And it happens that sometimes in home births there is no midwife at all (did not come or the woman was convinced that she was not needed). Therefore, of course, we can agree that the home environment helps a lot, but will it be possible to give birth in it in the event of some non-standard or difficult situation?
Natural childbirth is possible
But how then to ensure naturalness in childbirth and are there such childbirth at all? In fact, today, natural childbirth is widely carried out in most maternity hospitals, and is not only carried out, but also actively promoted . If everything goes well, if the birth proceeds correctly, if the baby’s heart beats evenly, and the mother feels good, the doctors of the maternity hospital do not interfere with the birth, but simply observe their course. A woman gives birth on her own, as nature dictates. But what about the notorious home comfort in childbirth? Turns out today many maternity hospitals provide natural childbirth "at home" :
A woman gives birth on her own, as nature dictates. But what about the notorious home comfort in childbirth? Turns out today many maternity hospitals provide natural childbirth "at home" :
- Almost everywhere now free behavior during childbirth is actively practiced : a woman in labor does not have to lie on the bed all the contractions, but can choose any position.
- In many maternity hospitals there are various devices to facilitate contractions : transforming beds, balls, ropes (with their help you can take different positions in contractions), and in some, in addition to the shower, there is even a jacuzzi in which you can spend the first stage of childbirth.
- Of course, not all, but already many Russian maternity hospitals have either been renovated or built in accordance with modern ideas about beauty and comfort . Even in free maternity hospitals there are cozy double rooms with a private bathroom, fresh renovation and beautiful linens.
 What can we say about childbirth under a contract or in a commercial clinic - the conditions there are more than excellent.
What can we say about childbirth under a contract or in a commercial clinic - the conditions there are more than excellent. - According to the order of the Ministry of Health of the Russian Federation, in any maternity hospital where there are separate maternity boxes, a husband, girlfriend, personal midwife or even a psychologist can be present at the birth, and absolutely free of charge . So, the expectant mother will not be left without support.
- Today, in all maternity hospitals, babies are immediately applied to the mother's breast; it is also possible for mother and baby to stay together in the postpartum department.
- Now you can easily find a maternity hospital where you can live together with your husband after childbirth in a comfortable family room . All this, of course, is not free - but if you really want it, then it is quite feasible.
So do not be afraid of the maternity hospital: it has all the conditions for natural and safe childbirth.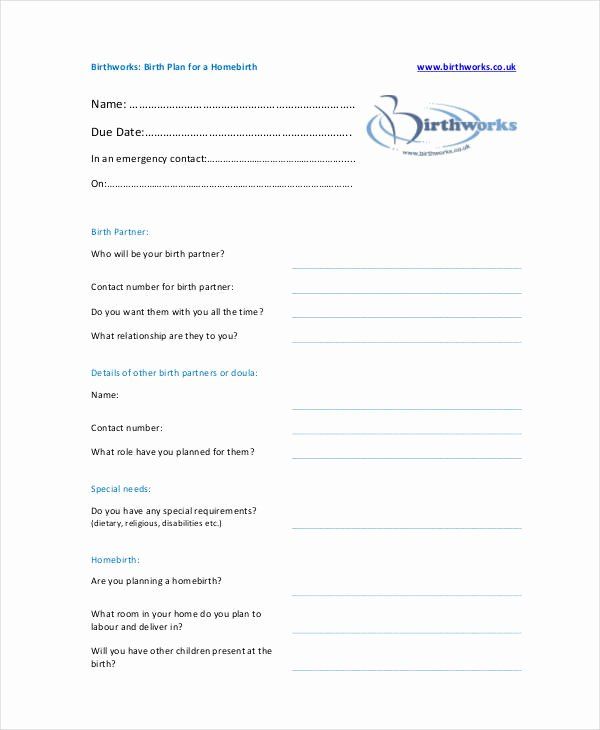 And home birth is an unjustified risk and an unknown result.
And home birth is an unjustified risk and an unknown result.
Have you read at least one story about childbirth at home that ended unsuccessfully? Hardly. And if they read it, it is not enough. And the reason for this, as a rule, is the same: with an unfavorable development of childbirth and problems with the child, a woman is aware of her carelessness and simply keeps silent about it.
“They used to give birth in the field” is one of the popular arguments of supporters of home births. They gave birth, but only the mortality rate in childbirth (both children and mothers) was extremely high.
An individual approach to the future mother and her baby, living together, free behavior during childbirth, the opportunity to choose a doctor and midwife, take a husband to give birth - all this is now available in many Russian maternity hospitals
5 signs that you are having a natural birth in the hospital
- Freedom of movement: in the maternity box there is a multifunctional bed-transformer, balls, ropes.

- Presence of a partner: a future father, girlfriend or psychologist is welcome at the birth.
- Natural Pain Relief: The delivery room has hydromassage baths or showers to ease contractions during the first stage of labour.
- Living together with the child: in the maternity hospital, the constant presence of the baby with the mother and breastfeeding are practiced.
By clicking on the send button, I consent to the processing of personal data
03/15/2018
God loves trinity
Zimina Natalya Nikolaevna Normantovich Tatyana OlegovnaHome births ended with a visit to City Clinical Hospital No. 52
Home births ended with a visit to City Clinical Hospital No. 52
We present two cases of home births with complications that required immediate admission to the hospital of City Clinical Hospital No. 52.
Patient L, 40 years old, was delivered to the maternity hospital along with the SMP with the diagnosis: Pregnancy 37-38 weeks.
 4th urgent delivery (home). Collapse. Bleeding. Tight attachment of the placenta. with a living child.
4th urgent delivery (home). Collapse. Bleeding. Tight attachment of the placenta. with a living child. This pregnancy is the 5th. From the anamnesis, attention was drawn to the 4th pregnancy, which ended in childbirth at home, the postpartum period was complicated by subinvolution of the uterus.
She was registered in the antenatal clinic from 28-29 weeks. I-II trimesters proceeded without complications. III trimester - mild anemia. Edema of the lower extremities. Weight gain 18 kg.
According to her husband, the birth took place at home, in a breech presentation. The husband took delivery. A live girl was born. The placenta did not separate, bleeding developed. At the time of the arrival of the ambulance crew, the patient's condition was grave. Pulse 120 beats / min. BP 40/20 mmHg 2 peripheral veins were catheterized, infusion therapy was started.
In the emergency room, the puerperal was examined by an obstetrician-gynecologist and an anesthesiologist-resuscitator.
 Upon admission to the maternity hospital, the child was examined by a neonatologist on duty, the diagnosis was: The period of early adaptation. High risk group for intrauterine infection, an increase in neurological symptoms. Polycythemia. Cerebral depression with elements of excitation.
Upon admission to the maternity hospital, the child was examined by a neonatologist on duty, the diagnosis was: The period of early adaptation. High risk group for intrauterine infection, an increase in neurological symptoms. Polycythemia. Cerebral depression with elements of excitation. The mother's condition is extremely difficult. Conscious, retarded. The pupils are round, of medium size. Anisocoria is not noted. Photoreaction is normal. Muscle tone is not changed. The skin and visible mucous membranes are pale, clean, cold on the periphery. Foot swelling. Respiration: shortness of breath of mixed type, rhythmic. NPV 24/1 min. Temperature 36.5°C. Vesicular breathing in the lungs. There are no wheezes. Saturation 90% in air. Heart sounds are rhythmic, muffled. Pulse on the main arteries of satisfactory filling, 120/1 min., rhythmic. Pulse in the peripheral arteries of weak filling. AD 90/40 mmHg Art. The abdomen is tense, sharply painful in all departments.
 Symptoms of peritoneal irritation are positive. The uterus is at the level of the umbilicus. Discharge from the genital tract is blood moderate. There is no bleeding.
Symptoms of peritoneal irritation are positive. The uterus is at the level of the umbilicus. Discharge from the genital tract is blood moderate. There is no bleeding. Diagnosis: Home birth. Partial tight attachment of the placenta. Hemorrhagic shock 2-3 degrees.
Given the severity of the patient's condition, signs of hemorrhagic shock of 2-3 degrees, surgical intervention is indicated: manual removal of the placenta and removal of the placenta. Accompanied by an anesthesiologist-resuscitator with ventilation support with an Ambu bag, the patient was taken to a deployed operating room.
Operation performed under endotracheal anesthesia: Manual separation of the placenta and removal of the placenta. Inspection of the birth canal. Sewing up the rupture of the posterior wall of the vagina.
Progress of the operation: under aseptic conditions, the obstetrician's hand, inserted into the uterine cavity, separated the placenta. The placenta is separated with difficulty, fragmentary.
 Selected last. Produced control manual examination of the walls of the postpartum uterus. The walls of the uterus are intact, there is no deformation. The placental platform was located on the back wall. The uterus contracted well, dense. The cervix was examined with the help of mirrors: intact. A rupture of the posterior wall of the vagina of the 2nd degree was found, it was restored with separate catgut sutures. The crotch is intact. Blood loss 700.0 ml. Total blood loss: 2700 ml.
Selected last. Produced control manual examination of the walls of the postpartum uterus. The walls of the uterus are intact, there is no deformation. The placental platform was located on the back wall. The uterus contracted well, dense. The cervix was examined with the help of mirrors: intact. A rupture of the posterior wall of the vagina of the 2nd degree was found, it was restored with separate catgut sutures. The crotch is intact. Blood loss 700.0 ml. Total blood loss: 2700 ml. Diagnosis after surgery: 4th timely home birth. Partial tight attachment of the placenta. Hemorrhagic shock 2-3 degrees. Posthemorrhagic anemia of severe degree. Rupture of the posterior wall of the vagina. Manual separation of the placenta and separation of the placenta. Sewing up the rupture of the posterior wall of the vagina.
Intraoperative Hb 32 g/l, hematocrit 7.8. The patient was transfused with 5 doses of fresh frozen plasma, after laboratory confirmation of the blood type, transfusion of 2 doses of a single-group erythrocyte suspension was performed.
 Consulted by a hemostasiologist: red blood cell transfusion was recommended to reach the target values (Hb not less than 70 g/l).
Consulted by a hemostasiologist: red blood cell transfusion was recommended to reach the target values (Hb not less than 70 g/l). Postoperative period without complications. The postpartum woman was transferred from the operating room to the intensive care unit to continue complex intensive care, a day later she was transferred to the postpartum department and on the 6th day she was discharged home with the child in a satisfactory condition.
Patient K., 31 years old, was delivered to the maternity hospital along with the SMP with a diagnosis of the 3rd stage of the 1st urgent delivery. Home birth with a live baby.
Pregnancy 1st. Registered in the antenatal clinic was from 8-9weeks. I trimester proceeded with the phenomena of early toxicosis, II and III - without complications. Edema of the lower extremities. Weight gain 12 kg.
According to the EMS paramedic, the birth took place at home in the presence of a “spiritual midwife”.
 The placenta did not stand out on its own, bleeding began, SMP was called.
The placenta did not stand out on its own, bleeding began, SMP was called. In the emergency room, the child was examined by a neonatologist: weight 3090 g, height 50 cm. During the examination, a fracture of the left clavicle was found. The puerperal was examined by an obstetrician-gynecologist and an anesthesiologist-resuscitator. Objectively: the condition of the puerperal is severe. Conscious. The skin and visible mucous membranes are pale, clean. Foot swelling. Temperature 36.7 C. Vesicular breathing in the lungs. There are no wheezes. NPV up to 25 in 1 minute. Saturation 90% in air. Heart sounds are rhythmic, muffled. Pulse on the main arteries of satisfactory filling 128 in 1 minute, rhythmic. Blood pressure 60/40 mm Hg. Art. The abdomen is soft, painless in all departments. There are no symptoms of peritoneal irritation. The uterus is at the level of the umbilicus. There are no signs of placental separation. Moderate bloody discharge from the genital tract, it is not possible to establish the exact blood loss.

Diagnosis: 1st timely delivery in cephalic presentation. 3rd stage of childbirth. Partial tight attachment of the placenta. Bleeding. Hemorrhagic shock 2 tbsp. Edema syndrome. Posthemorrhagic anemia. Considering the severity of the patient's condition, signs of hemorrhagic shock of the 2nd degree, surgical intervention is indicated: manual separation of the placenta and removal of the placenta.
Operation performed under intravenous anesthesia: Manual separation of the placenta and removal of the placenta. Inspection of the birth canal.
Progress of the operation: under aseptic conditions, the obstetrician's hand, inserted into the uterine cavity, separated the placenta. The placenta is separated with difficulty, fragmentary. Selected last. Produced control manual examination of the walls of the postpartum uterus. The walls of the uterus are intact, there is no deformation. The placental platform was located on the back wall. The uterus contracted well, dense.