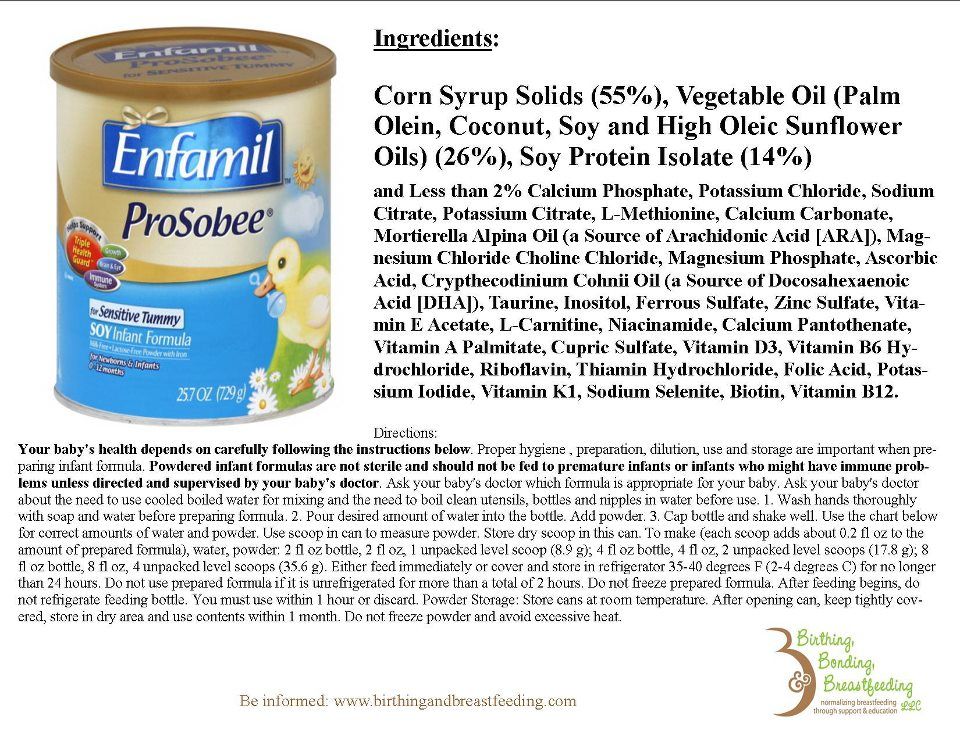
What is baby formula made out of
Types of formula milk - NHS
Formula milk, also known as baby formula or infant formula, is usually made from cows' milk that has been treated to make it more suitable for babies.
There's a wide range of brands and types of formula available in pharmacies and shops. Always check labels carefully to make sure you're buying a suitable milk for your baby.
Formula comes in 2 different forms: a dry powder you make up with water, or a ready-to-feed liquid formula. While ready-to-feed liquid formula can be convenient, it tends to be more expensive and, once opened, needs to be used more quickly.
Formula milk provides babies with the nutrients they need to grow and develop. However, it does not have the same health benefits as breast milk for you and your baby. For example, it cannot protect your baby from infections.
First infant formula (first milk)
Suitable from birth
First infant formula (first milk) should always be the first formula you give to your baby.
The cows' milk in formula contains 2 types of proteins – whey and casein. First infant formula is based on whey protein which is thought to be easier to digest than other types of formula.
Unless a midwife, health visitor or GP suggests otherwise, first infant formula is the only formula your baby needs. Your baby can stay on it when you start to introduce solid foods at around 6 months and drink it throughout their 1st year.
There's no evidence that switching to a different formula does any good or harm. However, if you think a particular brand of formula disagrees with your baby, talk to a midwife or health visitor. They can help you decide whether to try a different type.
When your baby is 1 year old, they can start to drink whole cows' milk or sheep's or goats' milk (as long as it's pasteurised).
Find out more about drinks to give your baby.
Goats' milk formula
Suitable from birth
Different kinds of goats' milk formula are available in pharmacies and shops. They are produced to the same nutritional standards as cow's milk-based formula.
They are produced to the same nutritional standards as cow's milk-based formula.
Goats' milk formula is not less likely to cause allergies in babies than cows' milk formula.
Goats' milk formulas are not suitable for infants with cows' milk allergy (also known as cows' milk protein allergy), as the proteins they contain are very similar.
Hungrier baby formula (hungry milk)
Suitable from birth (but ask a midwife or health visitor for advice first).
This type of formula contains more casein than whey, and casein is harder for babies to digest.
Although it's often described as suitable for "hungrier babies", there's no evidence that babies settle better or sleep longer when fed this type of formula.
Anti-reflux (staydown) formula
Suitable from birth (but only under medical supervision).
This type of formula is thickened with the aim of preventing reflux in babies (when babies bring up milk during or after a feed).
Although it's available in pharmacies and supermarkets, it's recommended you only use it on the advice of a health professional.
The instructions for making up anti-reflux formulas may be different to standard formula. The usual guidelines for making up formula recommend using boiled water that has stood for no more than 30 minutes, so that the temperature is still above 70C.
Some manufacturers of anti-reflux formula recommend making it up at lower temperatures than are usually recommended. Otherwise it may get lumpy. Follow the instructions on the pack or speak to a health professional for advice.
It's important to take extra care when making up and storing these products as powdered formula is not sterile and making it up at lower temperatures will not kill any harmful bacteria it may contain.
Speak to a midwife, health visitor or GP if you have any concerns.
Comfort formula
Suitable from birth (but ask a midwife or health visitor for advice first).
This type of formula contains cows' milk proteins that have already been partly broken down (partially hydrolysed). This is supposed to make it easier to digest and help prevent digestive problems such as colic and constipation. However, there's no evidence for this.
Partially hydrolysed formulas are not suitable for babies who have cows' milk allergy.
Lactose-free formula
Suitable from birth (but only under medical supervision).
This formula is suitable for babies who are lactose intolerant. This means they cannot absorb lactose, which is a sugar that's naturally in milk and dairy products.
Lactose intolerance is rare in babies. Symptoms include diarrhoea, abdominal pain, wind and bloating.
Lactose-free formula is available in pharmacies and shops, but if you think your baby may be lactose intolerant, it's important to speak to a midwife, health visitor or GP.
Hypoallergenic formula
Suitable from birth (but only under medical supervision).
If your baby is diagnosed as being allergic to cows' milk, a GP will prescribe an appropriate infant formula with fully hydrolysed (broken down) proteins.
Formula with partially hydrolysed proteins (comfort formula) is available in pharmacies and shops, but it's not suitable for babies with cows' milk allergy.
Follow-on formula
Suitable from 6 months (but ask a health visitor for advice first).
Follow-on formula should never be fed to babies under 6 months old.
Research shows that switching to follow-on formula at 6 months has no benefits for your baby. Your baby can continue to have first infant formula as their main drink until they are 1 year old.
The labels on follow-on formula can look very similar to those on first infant formula. Read the label carefully to avoid making a mistake.
Good night milk
Suitable from 6 months (but ask a health visitor for advice first).
Some follow-on formula has cereal added to it and is sold as a special formula for babies to have at bedtime.
This type of formula is not needed, and there's no evidence that babies settle better or sleep longer after having it.
Good night formula should never be given to babies under 6 months old.
Soya formula
Suitable from 6 months (but only under medical supervision).
Soya formula is made from soya beans, not cows' milk. It's occasionally used as an alternative to cows' milk formula for babies who have cows' milk allergy.
There are some concerns about the fact that soya contains phytoestrogens. These are found naturally in some plants.
The chemical structure of phytoestrogens is similar to the female hormone oestrogen. Because of this, there are concerns that they could affect a baby's reproductive development, especially in babies who drink only soya-based infant formula.
Babies' low body weight means they take in much higher amounts of phytoestrogens than older children or adults who eat soya products as part of a varied and balanced diet.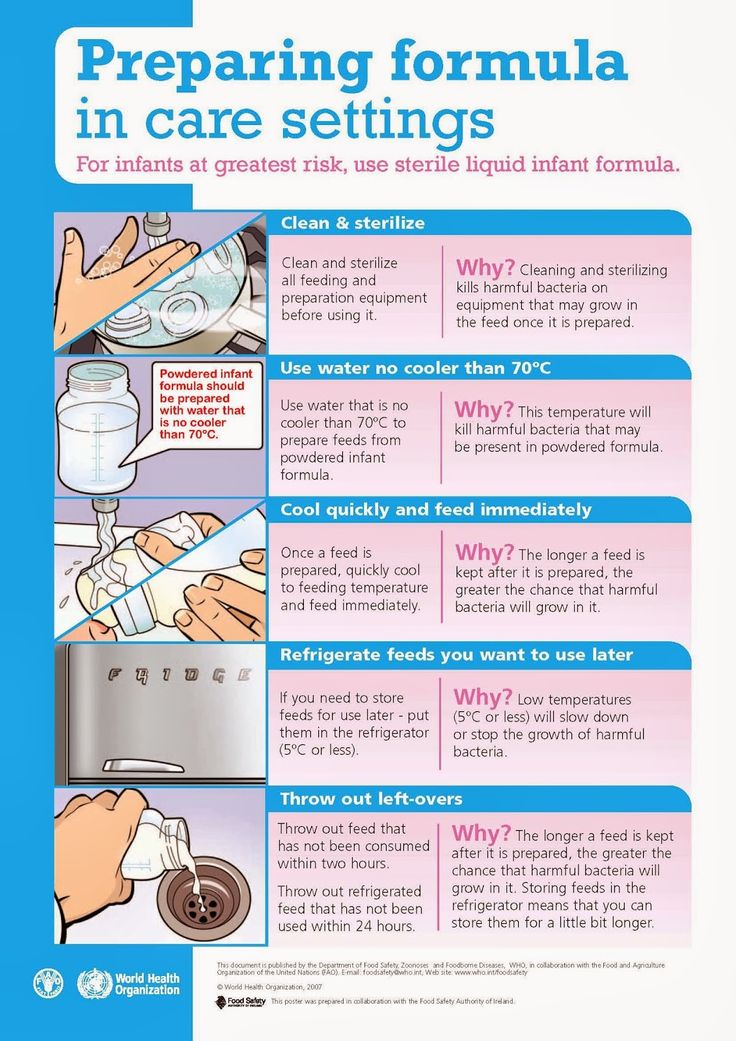
Also, because soya formula contains glucose, so it is more likely to harm a baby's teeth.
Only use soya formula if it has been recommended or prescribed by a health visitor or GP.
Growing-up milk (toddler milk)
Suitable from 1 year (but ask a health visitor for advice first).
Growing-up and toddler milks are marketed as an alternative to whole cows' milk for toddlers and children over 1 year old. There's no evidence to suggest that these products provide extra nutritional benefits for young children.
Whole cows' milk is a suitable choice as a main drink for your child from age 1. Semi-skimmed cows' milk is a suitable main drink for children over 2 who are eating a balanced diet.
It's recommended that all children aged 6 months to 5 years have vitamin drops containing vitamins A, C and D every day.
See more about vitamins for children.
Types of milk to avoid
Not all milk is suitable for feeding babies. You should never give the following types of milk to a baby under 1 year:
You should never give the following types of milk to a baby under 1 year:
- condensed milk
- evaporated milk
- dried milk
- goats' or sheep's milk (but it's fine to use them when cooking for your baby, as long as they are pasteurised)
- other types of drinks known as "milks", such as soya, rice, oat or almond drinks
- cows' milk as a drink (but it's fine to use it in cooking)
Further information
- combining breast and bottle feeding
- what if my child is intolerant to cows' milk?
Feeding your baby with formula
Feeding your baby with formula | Pregnancy Birth and Baby beginning of content10-minute read
Listen
Key facts
- Formula is a safe alternative to breast milk
- Formula can be given to your baby in their first 12 months
- Not all mothers can breastfeed, while others choose not to breastfeed
- Babies who receive formula grow and thrive if the formula is prepared correctly and they drink enough of it
What is formula?
Formula is a breast milk substitute made from a special dried-milk powder. Most infant formula is made from cow’s milk, vitamins and minerals. Formula is mixed with cooled boiled water and fed to babies in a bottle or cup.
Most infant formula is made from cow’s milk, vitamins and minerals. Formula is mixed with cooled boiled water and fed to babies in a bottle or cup.
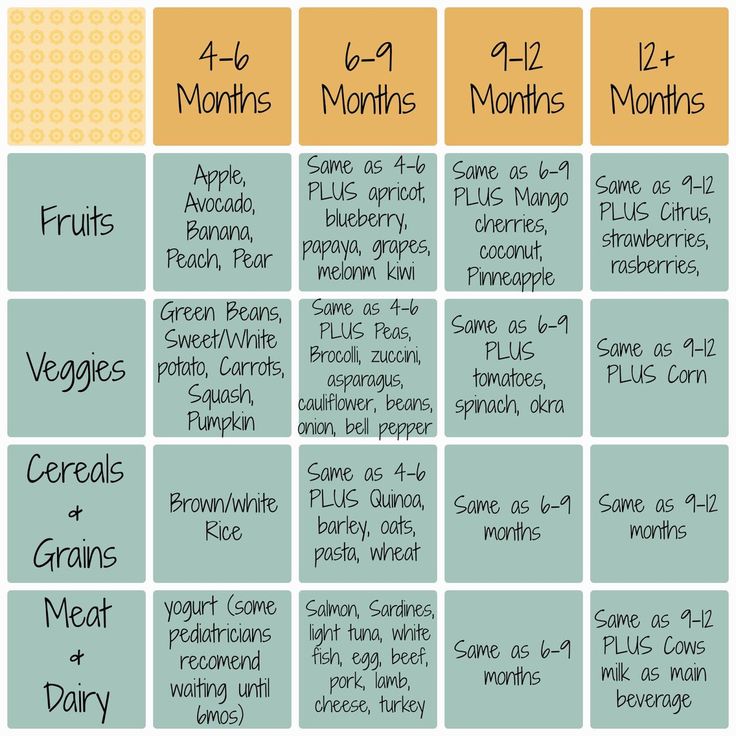
The nutrients in formula support a baby’s growth during their first 6 months. Once they reach 6 months, they can start eating solids as well, but a baby should not drink regular cow’s milk until they are at least 12 months old.
The main sources of protein in formula come from cow’s milk. Formula also includes fat from vegetable oils to support a baby’s growth.
Some formulas have sources other than cow’s milk, such as soybeans or rice. These specialty formulas have been altered so they are easier to digest or are suitable for babies who cannot tolerate cow’s-milk protein or lactose. Specialty formulas should only be used under the guidance of a healthcare professional.
How is formula different from breast milk?
Formula is a nutritionally complete food for babies. Many formula products contain extra ingredients so that they more closely match breast milk.
One of the main differences between formula and breast milk is that breast milk contains antibodies, which help protect the baby against a range of illnesses. The nutrition in breast milk adapts over the baby’s lifespan, unlike formula whose nutritional content stays the same.
Breast milk also has less protein than formula. Choosing a formula with less protein will reduce your baby’s risk of becoming overweight or obese as they get older.
Why might I give my baby formula?
There are many reasons why formula might be the best option for you and your baby. Not all women can breastfeed: some may be unable to produce enough milk for their baby’s needs while others may have a health condition or take medication that prevents them from breastfeeding.
Breastfeeding problems can be challenging and may even mean it’s unrealistic some women to continue.
Other women choose not to breastfeed, or they may not always be with their baby, such as when they are returning to work.
Many parents do not have the option to breastfeed, such as dads in same-sex relationships, adoptive and foster parents, and kinship carers.
Some women may not breastfeed if they have experienced sexual abuse that involved their breasts since this can trigger trauma. Understandably, mothers may not share this as the reason why they feed their baby formula.
What are the different types of baby formula?
All formula sold in Australia needs to meet stringent nutritional and hygiene standards. Most baby formulas are made from dried cow's milk with vitamins, minerals and vegetable oils added. Straight cow's milk is not suitable for a baby's digestion, unless it has been altered to make it easy to digest and so the nutrients can be absorbed.
There are 3 types of formula:
- Milk-based formulas are made from cow's milk, with added vegetable oils, iron, vitamins and minerals.
- Soy-based formulas are made from soybeans and have added vegetable oils and nutrients.
- Specialty formulas are made from cow's milk which has been 'predigested' and the protein removed or reduced. There is also a range of hypoallergenic formulas available. Most specialty formulas are designed for babies who have a milk intolerance or who are allergic to cow's milk. Formula might also be the best choice for babies who have a food protein allergy or other form of digestive, malabsorption or gut problem. Specialty formulas can be used for specific cultural or religious reasons too.
Other types of formula include:
- Stage 1 or starter formulas: These are suitable for babies aged up to 6 months. After this age, Stage 2 or follow-on formulas are recommended since they often have a higher iron content. However, there is no significant benefit in changing to these later-stage formulas.
- Anti-reflux or AR formulas: These have a thickener added that helps to keep the milk in the baby's stomach and reduce the likelihood of reflux.
- Some formulas have added compounds: Manufacturers claim these make the formula more like breast milk. But this doesn't mean the baby's body can digest or absorb these compounds in the same way as they would if they were breastfed. Prebiotics, probiotics and antioxidants are common examples or additives, as are long chain polyunsaturated (LCP) acids.
Tips for choosing a baby formula
- Healthy babies, who are born full-term and who are not breastfeeding, should always be fed with a cow's milk-based formula before trying any other type.
- The price of a formula is not a sign of its quality. Words like "Superior" or "Gold" are used by marketing people to persuade parents to buy their product.
- Check the price of the formula against the ratio of formula scoops to water. This will give you a good idea of how long a tin of formula may last.
- Read the label and make sure you're choosing the right formula for your baby's age.
- Look for a formula with a lower concentration of protein. Excess protein can increase the risk of your baby becoming overweight or obese later in life.
- Give your baby a few days to become accustomed to a new type of formula. Avoid switching multiple times to different brands and formula types.
Can babies be allergic to formula?
Some babies are particularly sensitive or allergic to cow’s milk-based formula. Generally, the protein in cow’s milk causes them to react. Hydrolysed formula is often recommended as an alternative. Hydrolysed formula contains cow’s milk protein that has been broken down into smaller particles.
There are a range of specialised formulas that suit babies with a cow’s milk allergy or soy formula allergy. These alternatives can be expensive, though. Speak with your GP or baby’s paediatrician about getting a prescription for a specialty formula since this can significantly reduce its cost.
How to tell when your baby is hungry?
It can be hard to know for sure when a baby is hungry or if there is something else causing them to fuss. Sometimes you won't know for sure that they're hungry until they're offered a bottle.
Sometimes you won't know for sure that they're hungry until they're offered a bottle.
Most babies usually cry when they are hungry. Placing the teat of the bottle in their mouth will calm them and they will start sucking.
Try to position your baby in your arms as you would if you were breastfeeding. Hold them close, look into their eyes and be sensitive to their cues or signals.
They suck and swallow in a coordinated way. They may look as if they're concentrating on feeding, their hands are clenched and their whole body looks like it's focused on sucking. As they fill up, their hands relax and their body becomes more relaxed.
Breastfed babies regulate their own milk intake. They suck when they're hungry and stop sucking when they're full. In comparison, formula-fed babies aren't as much in control of how much milk they drink — this is managed by the person offering the bottle.
When your baby has had enough, they will usually pull away from the teat to let you know they are full.
Sometimes you may notice that their sucking slows down and they have longer pauses between sucks.
Other ways your baby might show you they have had enough could be milk starting to pool in their mouth or they may vomit or 'spill' some milk.
Some babies might fuss after having a feed or might go to sleep.
Step-by-step guide to preparing formula
- Read the information on the container the formula comes in to make sure you understand how much water and how many scoops you need to combine.
- Wash and dry your hands well.
- Make sure you have a clean surface and area where you can prepare the formula.
- Boil fresh tap water in a kettle or on the stove. Let the water cool to room temperature or until it’s lukewarm. Fresh, plain and unopened bottled water, (not natural or sparkling mineral or soda water) can be used to prepare formula.
- Pour the water into already-sterilised bottles. Make sure you’re using the correct amount of water for your baby’s needs.

- You can store the sealed bottles of water in the main part of the fridge for up to 24 hours. Just before your baby’s feed you can add the correct number of formula scoops.
- Only use the scoop that came with the formula’s container and follow the manufacturer’s instructions.
- Fill the scoop so it’s loose and level. Don’t over or under-fill the scoop. Fill each scoop from the centre of the tin and level it off with the lid edge or a clean, sterilised knife.
- Tap the bottle on the bench so the formula powder settles into the water.
- Seal the bottle with the teat and screw cap. Shake well until all the formula is well dissolved in the water.
- Test the temperature of the formula on your wrist before offering it to your baby.
Preparation and hygiene
Make up each bottle as your baby needs to be fed. If you do need to store formula, place it towards the back of the refrigerator where the temperature is coldest.
Only use bottles and feeding equipment that have been washed and sterilised.
Throw away any formula that has been warmed but not finished within one hour. Don’t store partially empty bottles of formula. Formula and bottles become contaminated once the baby has had a feed from them.
Always make up formula according to the instructions on the tin. If the formula is made too weak, it can cause poor growth and the baby will be hungry. If it is too strong it can lead to constipation and the baby becoming overweight.
If you’re going out, transport the cooled, boiled water and formula powder separately. Mix the two just before feeding. Otherwise, keep the prepared formula cold in an ‘esky’ (cold storage container), baby bottle pack or cold bag.
Never warm formula in a microwave. This can cause the milk to heat unevenly and lead to burns. Instead, warm up each bottle in a jug of hot water. Bottle warmers are a safe option as long as they have a thermostat control and the bottle isn’t left in the warmer for longer than 10 minutes.
Every baby has their own unique feeding needs, so if you’re unsure about how much formula to offer your baby, check with your child health nurse. They will guide you on the correct amount for your baby’s age and weight.
They will guide you on the correct amount for your baby’s age and weight.
Call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Sources:
Raising Children Network (Infant formula: making, storing and transporting it), Raising Children Network (Mixed feeding: Supplementing breastfeeding with formula), Australasian Society of Clinical Immunology and Allergy (Guide for Milk Substitutes in Cow’s Milk Allergy), Pregnancy, Birth and Baby (Milk intolerance in babies and children), World Health Organization (How to Prepare Formula for Bottle-Feeding at Home), Department of Health (Infant formula)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2021
Back To Top
Related pages
- Balancing introducing solids with milk feeds
- Introducing solid food
- Weaning
- Cleaning and sterilising baby bottles
Need more information?
Baby formula & bottle-feeding for babies | Raising Children Network
Baby formula is the only safe alternative to breastmilk for the first 12 months. All Australian cow’s milk-based formulas meet strict standards. Read more.
All Australian cow’s milk-based formulas meet strict standards. Read more.
Read more on raisingchildren.net.au website
Formula feeding - Ngala
Infant formula is the safe alternative to breast milk for the first 12 months
Read more on Ngala website
Making formula – dos and don'ts
Use this handy guide on the dos and don't of making up formula for your baby.
Read more on Pregnancy, Birth & Baby website
Newborn nutrition: bottle-feeding | Raising Children Network
Get reliable information and tips on bottle-feeding newborn babies with articles on preparing formula, giving bottles, cleaning bottles and supplementing.
Read more on raisingchildren.net.au website
Mixed feeding: supplementing with formula | Raising Children Network
Worried your baby isn’t getting enough breastmilk? Mixed feeding, or supplementing with formula, might help. Start by talking with your midwife, nurse or GP.
Read more on raisingchildren.net.au website
Bottle-feeding: cleaning & sterilising | Raising Children Network
Bottle-feeding your baby? Find out what equipment you need – bottles, teats, rings and caps – plus how to clean and sterilise it all.
Read more on raisingchildren.net.au website
Introducing solid food
By the time your baby is about 6 months of age, breast milk or formula will no longer provide all the nutrition they need for healthy growth.
Read more on Pregnancy, Birth & Baby website
Donor Milk - Miracle Babies
The World Health Organisation recommends that donated breast milk is a better alternative to infant formula when mothers own milk (your babys optimum food) is not available
Read more on Miracle Babies Foundation website
When can babies drink water?
You may wonder when it is safe to start giving your baby water. Whether you are breastfeeding or formula feeding, learn how and at what age to get started.
Read more on Pregnancy, Birth & Baby website
Mixed feeding
Mixed feeding is when a baby is fed formula as well as breastmilk. Learn about why some women use mixed feeding, how to manage it, and where to get help.
Learn about why some women use mixed feeding, how to manage it, and where to get help.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia..jpg)
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What is infant formula made of?
The World Health Organization recommends that healthy full-term babies be exclusively breastfed for the first 6 months of life because breast milk is the best food for optimal growth and development of the baby. However, the situations may be different. The key to proper growth and development of the child is the full intake of essential nutrients into the body. Especially those that support the development of the brain and organ of vision. Children's bodies are very sensitive to nutritional deficiencies. Follow the recommendations of the pediatrician, follow a clear feeding schedule - and the baby will develop correctly! nine0003
Especially those that support the development of the brain and organ of vision. Children's bodies are very sensitive to nutritional deficiencies. Follow the recommendations of the pediatrician, follow a clear feeding schedule - and the baby will develop correctly! nine0003
For any occasion there are different options for infant formula .
• Initial and subsequent. The first are intended for feeding a child up to 6 months, the second - after six months. There are also special meals for premature babies and those born with low birth weight.
• Fresh and sour milk. Cow's milk is taken as the basis in fresh milk, in fermented milk it is fermented with special bacteria. The latter are less allergenic, but can cause some problems in children of the first months of life, so they are recommended to be given to the baby, alternating with fresh ones. nine0003
• Medical. If your baby has minor digestive problems or a mild allergy, the doctor will prescribe a preventive formula.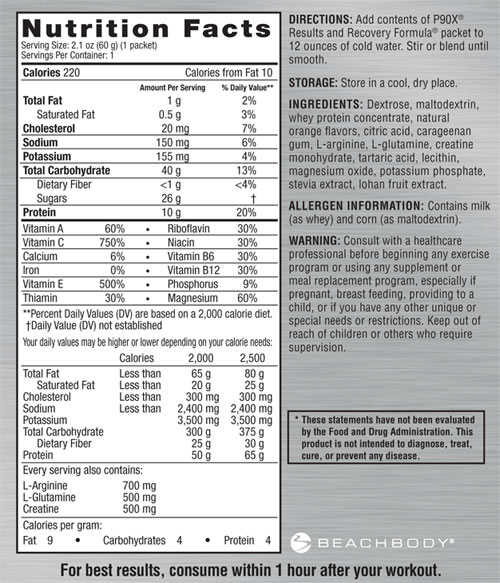 But with more serious ailments, such as lactase deficiency or intolerance to cow's milk protein, the baby needs therapeutic mixtures.
But with more serious ailments, such as lactase deficiency or intolerance to cow's milk protein, the baby needs therapeutic mixtures.
Declassified composition
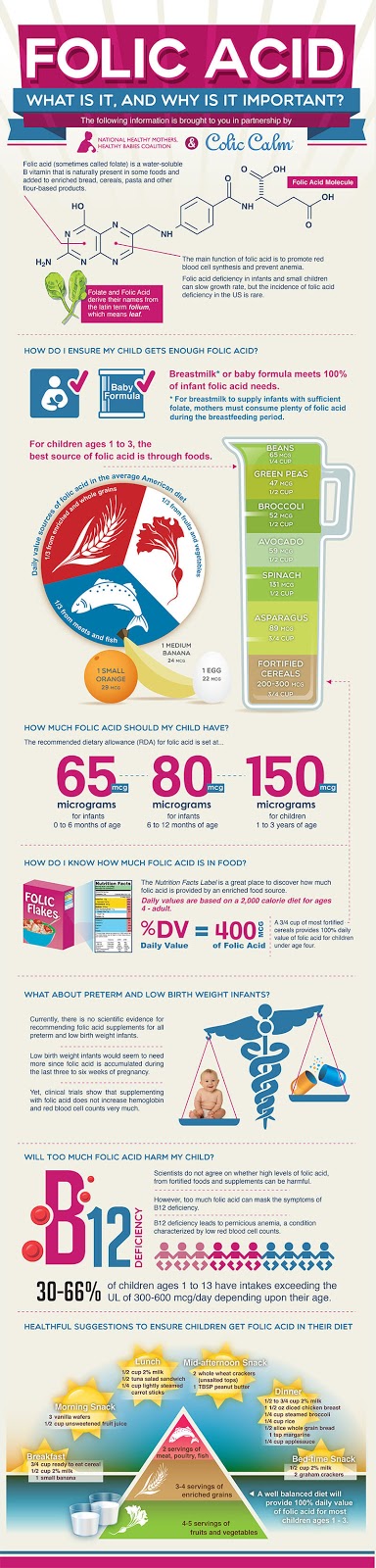
The formula of infant formula is gradually improving, more and more approaching the composition of breast milk. One of the last stages in their improvement was addition of lutein , a natural antioxidant found in breast milk, and probiotic bacteria Bifidobacteriumlactis. The galactooligosaccharides previously present in the composition of natural prebiotics together with the probiotic Bifidobacteriumlactis form a complex of symbiotics. Its components have been shown to reduce the frequency of diarrhea, they are involved in strengthening the immune system and microflora, and improve digestion in infants.
What is the mixture made of? nine0021
• Whey protein and casein are the main proteins in cow's or goat's milk. These substances are the main building material for a growing organism. Mixtures with a predominance of whey proteins are intended for babies from birth to 6 months, with casein - after six months.
Mixtures with a predominance of whey proteins are intended for babies from birth to 6 months, with casein - after six months.
• Lactose (milk sugar) improves digestion, provides a growing body with energy, creates a favorable environment for physiological microflora. In addition, lactose promotes the absorption of iron and calcium. nine0003
• Taurine is a free amino acid essential for the development of the central nervous system and vision.
• Linoleic acid plays an important role in the formation of the brain and retina.
• Dextrinmaltose promotes the growth of bifidobacteria in the intestines.
• probiotics suppress harmful microflora in the intestines and help the beneficial microflora multiply, forming immunity.
• Prebiotic fibers stimulate the growth of beneficial microflora, increase the protective properties of the body and regulate digestion.
• Starch or gum is needed if the baby vomits frequently. These components increase the viscosity of the mixture in the stomach.
• Modern adapted mixtures also include trace elements important for child development – zinc, copper, manganese, selenium and iodine.
• In addition, they are enriched with vitamins , depending on the age category or purpose. From breast milk, vitamins are absorbed better than from a mixture, so there are more of them in dry food. nine0003
• Lutein is an innovative component of the formula, along with a similar substance zeaxanthin, it is an essential component of breast milk. Lutein is not synthesized in the body, the baby before the introduction of complementary foods receives it only from breast milk. Lutein selectively absorbs the harmful blue part of the spectrum of the light flux, performing a protective function, and neutralizes the destructive effect if some part of the rays still penetrates the delicate structures of the retina. Lutein deficiency leads to irreversible visual impairment. nine0003
Lutein deficiency leads to irreversible visual impairment. nine0003
When choosing a milk formula for your baby, remember that the formula must be balanced in its composition and contain the ingredients necessary for the full development of the baby. After all, how a small child eats depends on his intellectual abilities and the development of vision.
Important! Breast milk is the best food for the baby, breastfeeding should be maintained as long as possible. If breastfeeding is not possible, your doctor will help you choose formula. nine0003
Published as an advertisement.
what infant formula manufacturers are silent about
Mankind has been breastfeeding its children for almost half a million years. And only in the last 60 years we began to give babies semi-finished products resulting from the deep processing of raw materials, called "artificial infant formula." The health consequences of this way of eating are simply amazing - 5 times the risk of gastroenteritis, 2 times the risk of diabetes, up to 8 times the risk of cancer of the lymphatic system. Manufacturers of infant formula in the UK spend about £20 per child to promote artificial milk substitutes. Compare that to the measly 14p per child the government in the UK spends to support breastfeeding, and what can we do to stop artificial feeding being rampant? nine0003
Manufacturers of infant formula in the UK spend about £20 per child to promote artificial milk substitutes. Compare that to the measly 14p per child the government in the UK spends to support breastfeeding, and what can we do to stop artificial feeding being rampant? nine0003
All mammals suckle their young, and the human race has breastfed babies for at least 400,000 years. All these many centuries, if a woman could not breastfeed her child herself, another nursing woman or “nurse” came to her aid. It's only in the last half century that we've almost completely abandoned our mammalian instinct, and instead created a fashion for bottle-feeding our babies. This new fad doesn't just encourage mothers to give their babies formula from birth, it also reassures them that these breast milk substitutes are just as good, if not better, than natural breast milk. nine0003
infant formula was never intended to be as widely consumed as it is today. It was invented in the late 1800s to save foundlings and orphans from starvation and provide them with the necessary food. In this narrow context - when no other food is available - the mixture has been a lifesaver.
In this narrow context - when no other food is available - the mixture has been a lifesaver.
However, over time, as human nutrition in general, and infant formula in particular, became more and more "scientific", manufacturers began to present artificial milk substitutes to the general public as some kind of technological innovation in breastfeeding. nine0003
“If someone asks: “What is the best mixture to use?” or “Which formula is more like breastmilk?” the answer should be “no one knows,” as no one has ever provided any unbiased source of information on this,” says Mary Smile, breastfeeding advisor. breastfeeding in the National Background for Child Health (NCT, UK) for 28 years. “Only the mix manufacturers know the exact composition of their product, and they don't disclose it. They may advertise special "healthy" ingredients in the blend, such as oligosaccharides, polyunsaturated fats, or beta-carotene, but they will never tell you what the basis of the product is made from or where the ingredients come from. " nine0003
" nine0003
That is, the components of breast milk, which have already been identified, have been and are still used as a reference for formulating infant formula. But to this day, there is no hard and fast recipe or formula for infant formula. In fact, infant formula is still created, as it was in its early days, through trial and error.
In their own commercial interests, manufacturers may add whatever they see fit to infant formula. The recipe for the same mixture may vary from batch to batch if the manufacturer needs to optimize the price, the cost of the product, or some ingredients become less available. It seems to us that the composition of the mixture is rigidly set and controlled, but in fact, no one requires such transparency from baby food manufacturers: for example, they are not required to use any specific ingredients for a specific batch or brand. nine0003
Most infant formula on the market is based on cow's milk. But before a baby can eat cow's milk as his main food, he needs to change a lot. It is necessary to reduce the content of protein and minerals, and increase the amount of carbohydrates, which is usually done by adding sugar. Milk fat, which is difficult to digest by the human body, especially with the immature digestive system of newborns, is removed and replaced with other vegetable, animal or mineral fats. nine0003
It is necessary to reduce the content of protein and minerals, and increase the amount of carbohydrates, which is usually done by adding sugar. Milk fat, which is difficult to digest by the human body, especially with the immature digestive system of newborns, is removed and replaced with other vegetable, animal or mineral fats. nine0003
Vitamins and trace elements are added to the mixture, but not always in their most easily digestible form. (This means that attempts to present artificial infant formula as "complete nutrition" can only be considered valid if infant formula is viewed very roughly as a complete set of vitamins and minerals to provide nutrition at the lowest level.)
Many infant formulas are also very heavily sweetened. While most infant formulas do not contain the sugar in the form of sucrose, they can contain large amounts of other sugars such as lactose (milk sugar), fructose (fruit sugar), glucose (also known as dextrose, a simple sugar derived from plants), and maltodextrin (malt sugar). Due to the imperfection of the legislation, all these mixtures can be advertised as “sugar-free” mixtures. Infant formula may also contain accidental contamination from the manufacturing process. It may also contain traces of genetically modified soy and corn. nine0003
Due to the imperfection of the legislation, all these mixtures can be advertised as “sugar-free” mixtures. Infant formula may also contain accidental contamination from the manufacturing process. It may also contain traces of genetically modified soy and corn. nine0003
In infant formulas sold in ordinary stores, potent toxic, carcinogenic, mutagenic substances are regularly found - Salmonella bacteria and aflatoxins produced by the fungus Aspergillus; or Enterobacter sakazakii, a devastating foodborne illness that can cause sepsis (a bacterial infection entering the bloodstream), meningitis (inflammation of the meninges), and neonatal necrotizing enterocolitis (a severe infectious disease that affects the small and large intestines). nine0003
Special attention should be paid to soy mixtures, as they contain plant estrogens (phytoestrogens) in very high concentrations. In fact, the concentration of phytoestrogens in the blood of children fed soy formula can be increased from 13,000 to 22,000 times compared to the normal concentration of natural human estrogen. Estrogen in doses exceeding the natural level, which should be maintained in the body, can provoke cancer.
Estrogen in doses exceeding the natural level, which should be maintained in the body, can provoke cancer.
Artificial feeding is dangerous for children's health
For many years it has been thought that the risks of getting sick and dying from bottle feeding are mainly related to babies in developing countries, where there may be problems with the clean water needed to prepare formula, and where poor mothers may be forced to skimp on formula and add it less than it should be in order to stretch one jar for a longer time. A shortage of clean water creates a risk of spreading water-borne diseases such as diarrhea or cholera, and a highly diluted mixture leads to malnutrition. But new data from the West clearly demonstrates that babies in developed countries are also at risk of getting sick and dying due to an early transition to a diet of processed foods. nine0003
Formula cannot be a complete food because it does not contain breast milk immunostimulants and because, as a product for ever growing babies, it does not take into account their constantly changing nutritional needs. As a result, it can be detrimental to the health of children who are forced to eat formula day after day early in their lives, both in the short and long term.
As a result, it can be detrimental to the health of children who are forced to eat formula day after day early in their lives, both in the short and long term.
Living food versus powdered food
Breast milk is a "living" food that contains living cells, hormones, active enzymes, antibodies and at least 400 other unique components. It is a dynamic substance, the composition of which is constantly changing from the very beginning to the end of breastfeeding, depending on the age and needs of the child. Since breast milk also provides the formation of immunity, every time the baby is applied to the breast, he receives protection from the disease. nine0003
Compared to this wonderful substance, artificial milk substitutes sold as infant formula are little better than the lowest quality food. It is also the only food industry product that is offered as the only source of food for several months, although we know that health and well-being cannot be expected from the human body if it is put on a monotonous diet of processed foods.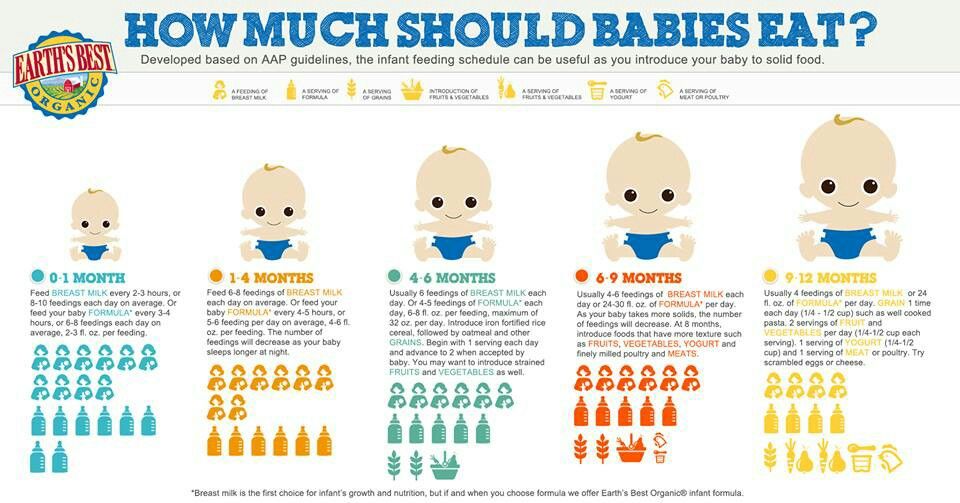
Breast milk - fats
- Plenty of omega-3s essential for brain development, namely docosahexaenoic acid and alpha-linolenic acid.
- Automatically adjusts to baby's needs - levels decrease as baby gets older.
- A lot of cholesterol, which is almost completely absorbed.
- Contains the enzyme lipase, which aids in the absorption of fats by the body.
Infant formula - fats
- No docosahexaenoic acid. nine0128
- Unable to accommodate infant's needs.
- No cholesterol.
- Not fully absorbed by the body.
- No lipase.
Fat is the most important nutrient in breast milk; the absence of cholesterol and DHA can provoke heart disease and damage to the central nervous system in a child. Undigested fat residues are the cause of the unpleasant odor of the stool of formula-fed babies.
Proteins - breast milk
- Gentle, easily absorbed serum
- Better digestion, higher content in the milk of mothers who give birth prematurely
- Lactoferrin for intestinal health
- Lysozyme - antimicrobial ingredient
- Plenty of protein components needed to build the brain and muscles
- Many “growth factors”
- Contains sleep-promoting proteins
Proteins - infant formula
- Hard-to-digest casein clots
- Not completely absorbed, so more is wasted, harder on the kidneys
- Little or no lactoferrin
- No lysozyme
- Some proteins needed for brain and muscle development are deficient or deficient
- Inadequate content of “growth factors”
- Almost free of sleep-promoting proteins
Please note that breast milk proteins do not cause allergies in babies
Carbohydrates - breast milk
Carbohydrates - infant formula
- No lactose in some formula formulations
- Oligosaccharide deficiency
Note
Lactose is very important for brain development.
Immunostimulants - breast milk
- Millions of live leukocytes per feed
- Many immunoglobulins
Immunostimulants - infant formula
- No live leukocytes and no others at all nine0127 No benefit to immunity
Breastfeeding provides active and dynamic protection against infections of all kinds. Breast milk can be used to relieve a number of mild conditions such as diaper rash and conjunctivitis.
Vitamins and minerals - breast milk
- Better absorbed by the gastrointestinal tract
- 50-75% iron absorbed
- Contains more selenium (antioxidant)
Vitamins and minerals - infant formula
- Not absorbed as well
- 5-10% iron absorbed
- Low in selenium (antioxidant)
Nutrients in infant formula are poorly absorbed. To compensate for this, manufacturers add more nutrients to the mixture, making it even more difficult to digest.
To compensate for this, manufacturers add more nutrients to the mixture, making it even more difficult to digest.
Enzymes and hormones - breast milk
- Many digestive enzymes such as lipase and amylase
- Many different hormones such as thyroxine, prolactin and oxytocin. Their composition depends on the mother's diet, thereby helping the child get used to the food culture of the region where his family lives
Enzymes & Hormones - Infant Formula
- Milk Processing Kills Digestive Enzymes
- Milk processing kills hormones that are not intended for humans
- Composition is always the same, no help with fitting
Digestive enzymes provide the foundation for digestive health; hormones ensure the biochemical balance and well-being of the child.
Cost - breast milk
-
Approximately £350/year for extra food for the mother if she was previously very poor
Cost - infant formula
- Approximately £650/year
- Up to £1,300/year for hypoallergenic formula (RUB 105,221.
 22 as of 12/27/2014)
22 as of 12/27/2014) - Additional costs for bottles and related accessories
In the UK, the National Health Service spends £35m (2,832,879,000 as of 12/27/2014) a year on treatment of gastroenteritis in artificial babies. In the United States, insurance companies pay out $3.6 billion each (291,381,840,000 rubles as of December 27, 2014) for the treatment of formula-fed children annually.
Side effects of bottle-feeding
In the first 6 weeks of life, bottle-fed babies have a 2-fold higher risk of dying in any situation compared to breast-fed babies. In particular, formula feeding increases the risk of SIDS (Sudden Infant Death Syndrome) by 2-5 times. Click here to read Dr. Sears' article on the link between breastfeeding and a lower risk of SIDS (Sudden Infant Death Syndrome). Formula-fed babies are also significantly more likely to end up in the hospital with various infections. For example, the probability of getting into the hospital with gastroenteritis for artificers increases by 5 or more times. nine0003
nine0003
Even in developed countries, formula-fed infants are twice as likely to have diarrhea as infants. They are 2 times more likely (20% vs 10%) to have otitis (inflammation of the middle ear), 2 times more likely to develop eczema or shortness of breath if there are prerequisites for this in a family history, 5 times more likely to develop a urinary tract infection. In the first 6 months of life, artificial babies have a 6 to 10-fold increased risk of necrotizing enterocolitis, a serious intestinal infection that kills intestinal tissue, and this figure rises to 30-fold at older ages. nine0003
Even more serious illnesses have been linked to artificial feeding. Compared to newborns who have been breastfed for at least 3-4 months, a child fed artificial milk substitutes is 2 times more likely to join the ranks of juvenile insulin-dependent diabetics (type 1 diabetes). Formula-fed children and those who have been breastfed for less than 6 months have a 5- to 8-fold increased risk of developing lymphoma before age 15.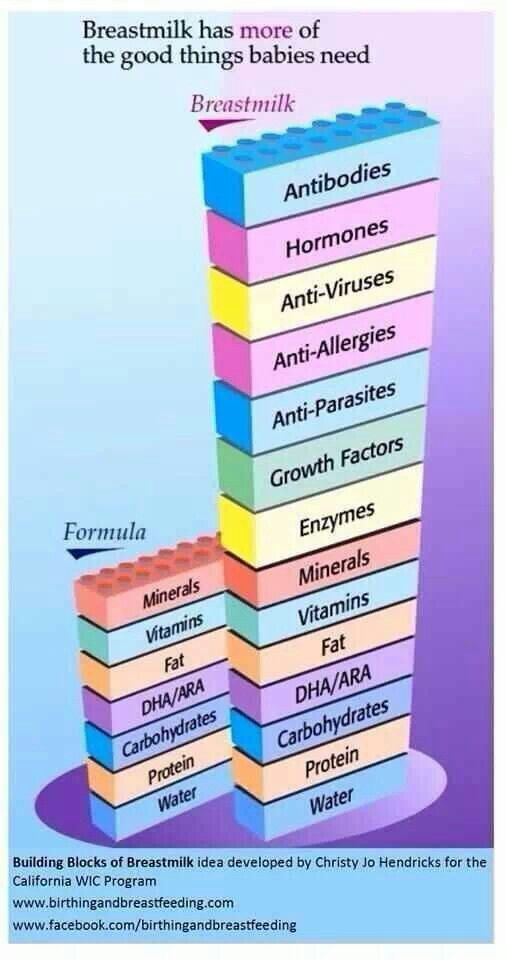 nine0003
nine0003
Studies have shown that later in life artificial children are much more prone to childhood inflammatory bowel disease, multiple sclerosis, malocclusion, coronary heart disease, diabetes mellitus, hyperactivity, autoimmune thyroid disease, and celiac disease.
Knowing the above, infant formula cannot even be called a “second choice” product after breast milk. Officially, the World Health Organization (WHO) suggests choosing formula last for feeding your baby. In the first place is mother's breast milk, in second place is mother's own milk, but already expressed, in third place is donor breast milk from a milk bank or a nurse's milk. And finally, in fourth place is the milk mixture. nine0003
And yet, there are fewer and fewer breastfed babies every year. In the UK, their numbers are catastrophically low and have remained so for decades. According to current statistics, only 62% of women are trying to start breastfeeding (usually immediately after giving birth in a hospital). By six weeks, the number of breastfeeding is reduced to 42%. By four months, only 29% of mothers are still breastfeeding their babies, dropping to 22% by six months.
By six weeks, the number of breastfeeding is reduced to 42%. By four months, only 29% of mothers are still breastfeeding their babies, dropping to 22% by six months.
These figures can be applied to almost any developed country in the world, and it should be noted that we are not talking about exclusive breastfeeding. Many current mothers practice mixed feeding - a combination of breastfeeding and feeding artificial infant formula milk and baby food. Globally, WHO estimates that only 35% of infants at 4 months of age receive no food other than breast milk, and only 1% of infants are exclusively breastfed at 6 months of age. But no one can vouch for these numbers, as studies on exclusive breastfeeding are few and far between. nine0003
The younger the woman, the less likely she is to breastfeed. More than 40% of mothers under the age of 24 do not even try to start breastfeeding. Of greatest importance, however, is the socio-economic position of women in society. Women living in low-income families with little education are many times less likely to breastfeed, despite the fact that this can be critical to the health of the child.
Women living in low-income families with little education are many times less likely to breastfeed, despite the fact that this can be critical to the health of the child.
For disadvantaged children, exclusive breastfeeding for the first 6 months of life bridges the health gap between those born poor and those born wealthy. In essence, breastfeeding protects the child from poverty during the first decisive months of life and gives him a worthy start in life. nine0003
So why don't women breastfeed?
Before bottles were ubiquitous, breastfeeding was part of a daily routine based on emulation of other women and learning from family and kin. Through trial and error, women have accumulated vast experience and become real experts. But today, what should happen more or less naturally has become extremely complex. Breastfeeding has become the focus of marketing strategies of transnational corporations and politics, lawmaking, the interests of lobbyists, various activists and figures acting in good faith and not always effectively, a cult of professionals is being created. nine0003
nine0003
As Mary Smile says, confidence in success and expectation of support from others differ greatly among women belonging to different social strata. “The concept of self-efficacy, or the belief that you can accomplish what you set out to do, is very important. You can tell a woman that breastfeeding is indeed a very good idea, but she will continue to believe in a thousand different things that must come together to make it work. First of all, in order to be imbued with the idea of the importance of breastfeeding, she must understand that it will be good for her and for her baby. Secondly, she must be sure that she will succeed. Thirdly, but perhaps the most important point, a woman must know that if she encounters difficulties, she will be able to find support and overcome them. nine0003
Research shows, for example, that low-income women often believe that breastfeeding is painful, and they also tend to believe that formula is just as good. Thus, initially there is simply no motivation to breastfeed. They are sure that if there are any problems with breastfeeding, then nothing can be done about it, for example, if it hurts, then it’s just bad luck. This type of thinking is very different from middle-class mothers who, when needed, seek help over the phone or in conversation with a midwife or health visitor: “I want you to help me with this…”
They are sure that if there are any problems with breastfeeding, then nothing can be done about it, for example, if it hurts, then it’s just bad luck. This type of thinking is very different from middle-class mothers who, when needed, seek help over the phone or in conversation with a midwife or health visitor: “I want you to help me with this…”
Almost all women - about 99% - can breastfeed and produce enough milk for the growth and development of their children. With encouragement, support and help, almost all women are ready to start breastfeeding, and 90% of women who stop breastfeeding within the first six weeks would like to continue breastfeeding. It is likely that long-term exclusive breastfeeding would be more common if it were provided with more consistent support in the family and in society, if breastfeeding itself became habitual and ubiquitous. nine0003
But at the moment there is no social support, and it can be assumed that medical, socio-economic, cultural and political stereotypes of modern society play a significant role in the global picture of “breastfeeding versus artificial feeding”. They regularly undermine women's self-confidence, move the issue of feeding children from the plane of health to the plane of lifestyle, and convince that the body of a modern woman simply cannot cope with the task of producing enough milk for her descendants. nine0003
They regularly undermine women's self-confidence, move the issue of feeding children from the plane of health to the plane of lifestyle, and convince that the body of a modern woman simply cannot cope with the task of producing enough milk for her descendants. nine0003
"Breastfeeding is a natural way for mother and child to communicate and it is dangerous to interfere with it," says Professor Mary Renfrew, director of the Maternal and Child Research Center at York University. “But in the early years of the last century, people were very concerned about intervening in it. If we consider breastfeeding as an ecological system, then the natural habitat has been disturbed. This was not only due to the appearance of one big predator - the invention of artificial milk replacer, although this is also very important. The key was that the habitat was already weakened by other forces that made it so vulnerable to the catastrophe. nine0003
If you look at the medical textbooks of the early 20th century, you will find many quotes presenting breastfeeding as scientific and measurable, and this is where the system started to fall apart. “It's falling apart,” says Renfrew, largely out of fear and distrust of the natural order of things, and an attempt to prioritize science. In particular, it turned out that the fact that the mother can put the baby on the breast and do something else during breastfeeding, and that the baby himself will let go of the breast when he wants, is all messy and unscientific, and therefore was replaced with an artificial situation. accurate measurements. For example, control weighing as a way to determine how many milliliters of milk a child receives during feeding could only arise due to a bias from the natural balanced system of mother and child to a bottle as a biological norm. nine0003
“It's falling apart,” says Renfrew, largely out of fear and distrust of the natural order of things, and an attempt to prioritize science. In particular, it turned out that the fact that the mother can put the baby on the breast and do something else during breastfeeding, and that the baby himself will let go of the breast when he wants, is all messy and unscientific, and therefore was replaced with an artificial situation. accurate measurements. For example, control weighing as a way to determine how many milliliters of milk a child receives during feeding could only arise due to a bias from the natural balanced system of mother and child to a bottle as a biological norm. nine0003
The value of breastfeeding also began to decline due to changes in women's lifestyles after the First World War, as more women left their children for work as women's emancipation spread and the huge loss of men in the killing fields, and continued to decline even more with the onset of the Second World War. world war, when even more women were employed outside the home.
world war, when even more women were employed outside the home.
"The first wave of feminism also played its part," says Renfrew, who left her mark on everyone in the 60s and encouraged women to leave their children and start living their own lives. So, helping in one thing - women began to support each other - in fact, she created a situation where even intellectual, socially active, conscious women who could think about the importance of breastfeeding, missed it from the spotlight. nine0003
As a result, widespread breastfeeding has ended, confidence in breastfeeding has declined, awareness of its importance has fallen, and health professionals have been unable to support breastfeeding mothers. And in parallel with this, there was a technological progress in the production of milk substitutes and the distribution of infant formula in the public domain.”
Medicalization of childbirth and its role
Before the Second World War, pregnancy, childbirth and breastfeeding as their natural continuation were integral parts of everyday life. Women gave birth at home with the help and support of experienced midwives, who themselves were part of the society in which the woman lived. After giving birth, women breastfed and were encouraged and supported by family and friends. nine0003
Women gave birth at home with the help and support of experienced midwives, who themselves were part of the society in which the woman lived. After giving birth, women breastfed and were encouraged and supported by family and friends. nine0003
By tearing childbirth out of social life and transferring it to the hospital, we have come to the medicalization of this aspect of women's life. Life events have turned into medical problems, and generational experience has been replaced by scientific and technological solutions. This medicalization has led to a growing wave of interventions in the natural process that undermine a woman's confidence in her ability to conceive, carry, give birth, and then feed a healthy child. The chain of deterioration looks something like this: Hospitals are institutions, they are impersonal and forced to work according to instructions and procedures. For a hospital to run smoothly, the ideal patient would need to be immobilized and unconscious (or sedated).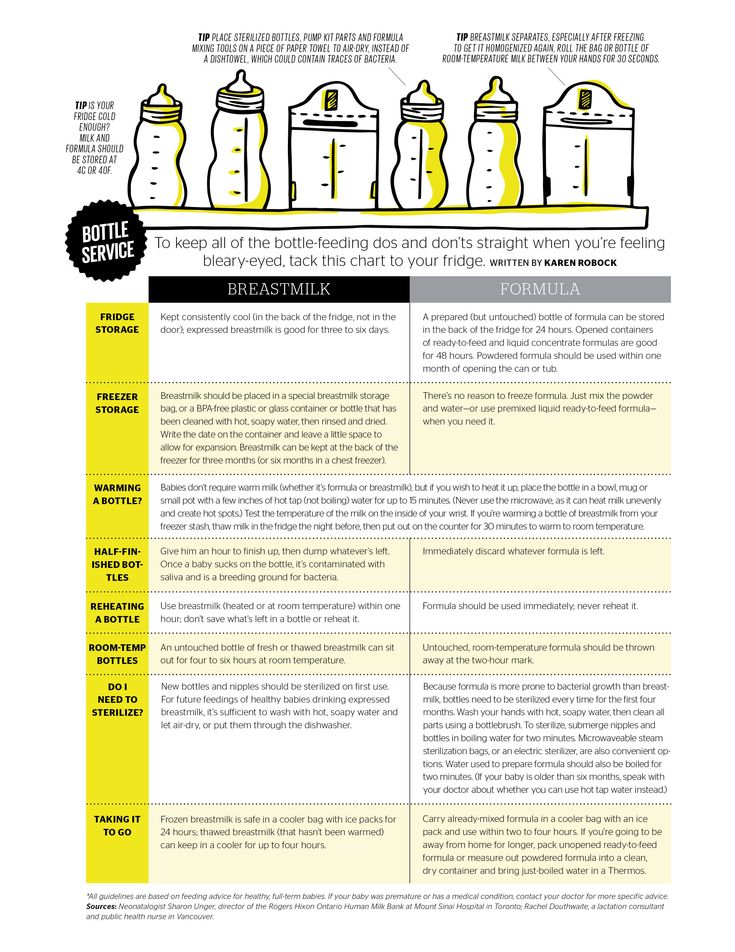 For a woman in labor, this means lying on her back in bed, in an unnatural position that slows down labor, makes it less productive and much more painful. nine0003
For a woman in labor, this means lying on her back in bed, in an unnatural position that slows down labor, makes it less productive and much more painful. nine0003
To "correct" these iatrogenic prenatal births, physicians have developed a range of drugs (mostly synthetic hormones such as prostaglandin and synthetic oxytocin), technologies (such as forceps and vacuum extraction), and procedures (such as episiotomy) to speed up the process. Artificially speeding up labor made it even more painful, and this, in turn, boosted the pain medication industry. Many of them turned out to be so powerful that the mother was unconscious or inhibited at the very moment of birth and was not able to put the newborn baby to her breast. All pain medication crosses the placenta, so even if the mother is conscious, the baby may be unconscious or so drugged that her natural instincts to find the nipple won't work, and the muscles to properly latch onto the breast won't be able to coordinate. nine0003
While mother and child are recovering from the ordeal of medical delivery, they are usually separated from each other, especially in the 1970s and 1980s. Often the baby was not allowed to breastfeed until he was bottle fed first, especially if something was wrong with his gastrointestinal tract. Breastfeeding, if it came at all, had to follow a strict schedule. This feeding schedule - usually with 3 or 4 hour breaks - is completely unnatural for human newborns who need 12 or more feeds a day. Children who inevitably became hungry between feedings were routinely supplemented with water and/or formula. nine0003
Often the baby was not allowed to breastfeed until he was bottle fed first, especially if something was wrong with his gastrointestinal tract. Breastfeeding, if it came at all, had to follow a strict schedule. This feeding schedule - usually with 3 or 4 hour breaks - is completely unnatural for human newborns who need 12 or more feeds a day. Children who inevitably became hungry between feedings were routinely supplemented with water and/or formula. nine0003
“There were a lot of supplements,” says Professor Renfrew. “The spread of this ‘scientific’ breastfeeding in hospitals has resulted in the baby being given only two minutes on each breast per feed on the first day, four minutes on each breast on the second day, seven minutes on the third, and so on. . This led to increased anxiety in mothers who stopped looking at their children and started looking at their watches. Infants were supplemented after each feed, then supplemented throughout the night instead of breastfeeding during this time. And everyone was crying - babies were crying in the children's ward, mothers were crying in the postnatal ward. And that was considered normal throughout the 60s and 70s of the last century.” nine0003
And everyone was crying - babies were crying in the children's ward, mothers were crying in the postnatal ward. And that was considered normal throughout the 60s and 70s of the last century.” nine0003
Breast milk is produced by the mother's body on the basis of a supply-demand system, and routine supplementary feeding alleviated infant hunger and thereby reduced the demand for mother's milk, and there was less milk. As a result, women at the mercy of the system were frustrated by the unsuccessful and painful struggle to breastfeed. And at the same time, in these unbearable conditions, when it was “not possible” to breastfeed, the formula was presented as a “complete food”, which was also more “modern”, “cleaner” and “socially acceptable”. nine0003
At least two generations of women have experienced these harmful medical interventions, which is why many mothers today look at breastfeeding as something strange and unaccustomed. Breastfeeding has been undeservedly given the image that “sometimes it can be”, but often “it doesn’t work out”, that it would be nice to breastfeed, but if it didn’t work out, then you don’t have to feel guilty about it, and nothing terrible happened.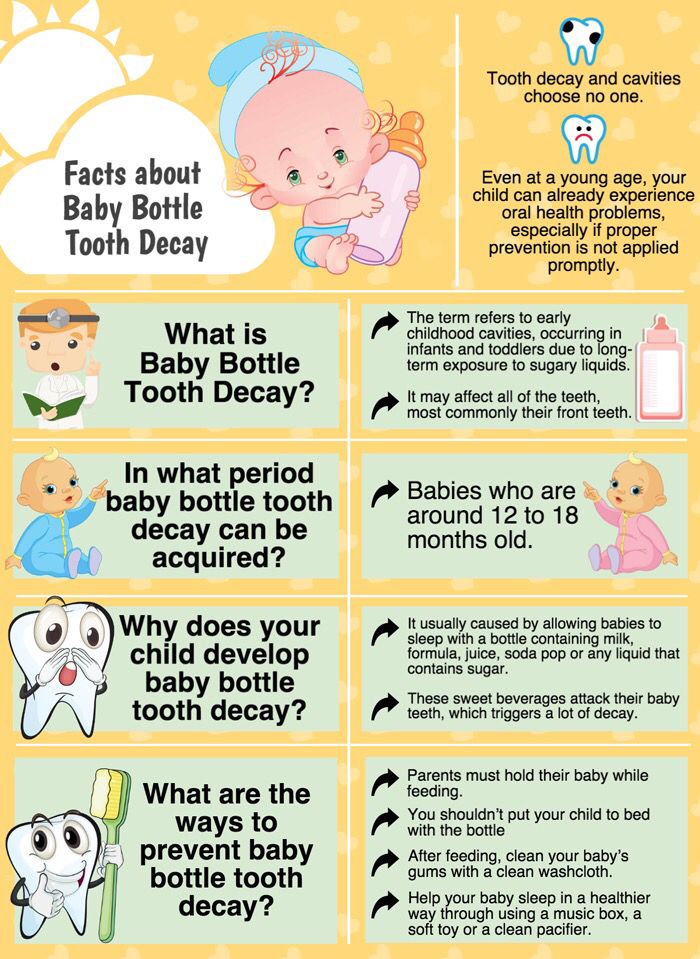
Medical professional failures
Former young doctors, nurses and midwives who pioneered the medical model of childbirth are now working in medicine. Therefore, it should not be surprising to anyone that modern hospitals are essentially no different from their predecessors. They have televisions, CD players, beautiful wallpapers, more sophisticated medicines, but the basic aims and principles of medical birth have changed little in the past 40 years, and breastfeeding is having a devastating effect. nine0003
In many cases, medical professionals' opinions about breastfeeding are based on their own subjective experiences. Surveys show, for example, that a determining factor in how effective and accurate breastfeeding advice from a mother's doctor will be is the doctor's own experience with breastfeeding if it is a woman, or whether the doctor's wife has breastfed her children if it is a man. Similarly, if a midwife, nurse or health visitor does not have breastfeeding experience themselves, they are unlikely to advocate for it and be able to help. nine0003
nine0003
It is bad that these professionals contribute to the spread and perpetuation of myths about breastfeeding, which provoke rejection. Some hospitals continue to advise women to limit the amount of time their baby spends at the breast, on the grounds that the nipples can become hard. Or mothers are told that the baby “should” suck out all the milk in the first 10 minutes and there is no longer any need to keep it at the breast. Some places still recommend a 4-hour feeding schedule. nine0003
British statistics show that there are still too many children in the UK being unnecessarily supplemented. In 2002, 30% of newborns in UK hospitals received a bottle of formula from the hands of hospital staff and nearly 20% of these were separated from their mothers at some point during their stay in the hospital.
The flood of unskilled breastfeeding advice from health professionals was one of the reasons 19In 1991, UNICEF organized a certification system for hospitals "Baby Friendly Hospital" - "BDR". Hospitals that have received this certification must meet certain criteria to promote breastfeeding:
Hospitals that have received this certification must meet certain criteria to promote breastfeeding:
- training for all health care workers on how to help women breastfeed,
- helping mothers start breastfeeding within the first hour after birth,
- not giving newborns no other food or drink than breast milk, unless otherwise prescribed by medical indications,
- The hospital does not accept free or heavily discounted infant formula or supplies.
In principle, such an initiative is an important step in the spread of breastfeeding, and studies show that women who give birth in baby-friendly hospitals breastfeed for longer (in Russia, even in baby-friendly maternity hospitals, the staff does not always know and in practice fulfills the provisions of this initiative - at. per.). In Scotland, for example, where about 50% of hospitals are BDR certified, the number of women starting to breastfeed has increased dramatically in recent years.