How to slow labor down
Preterm labor - Diagnosis and treatment
Diagnosis
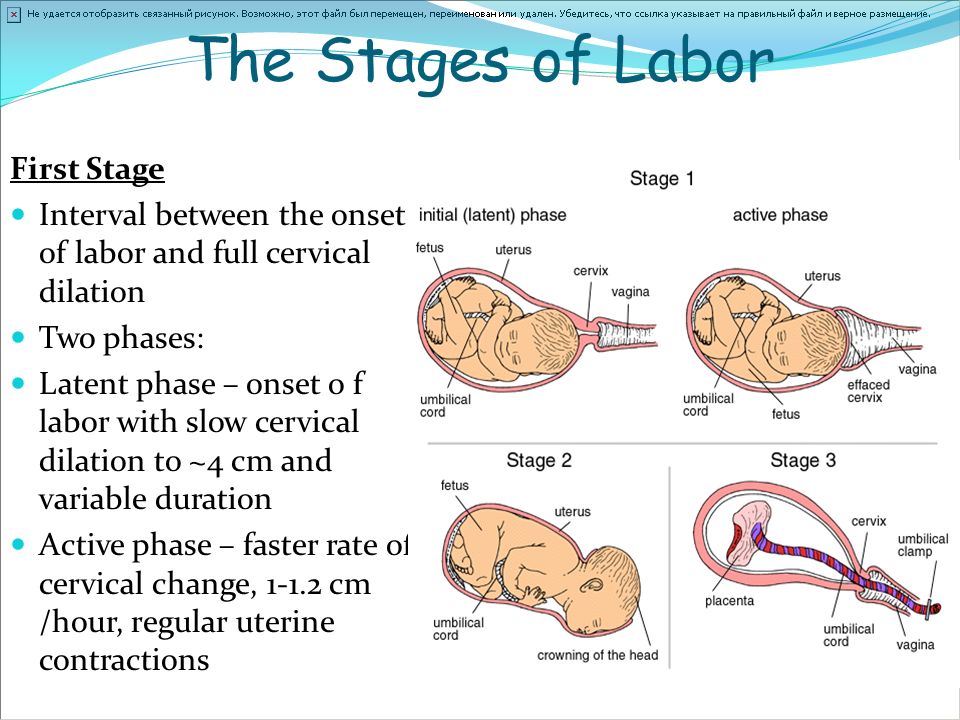
Your health care provider will review your medical history and risk factors for preterm labor and evaluate your signs and symptoms. If you're experiencing regular uterine contractions and your cervix has begun to soften, thin and open (dilate) before 37 weeks of pregnancy, you'll likely be diagnosed with preterm labor.
Tests and procedures to diagnose preterm labor include:
- Pelvic exam. Your health care provider might evaluate the firmness and tenderness of your uterus and the baby's size and position. If your water hasn't broken and there's no concern that the placenta is covering the cervix (placenta previa), he or she might also do a pelvic exam to determine whether your cervix has begun to open. Your health care provider might also check for uterine bleeding.
- Ultrasound. A transvaginal ultrasound might be used to measure the length of your cervix. An ultrasound might also be done to check for problems with the baby or placenta, confirm the baby's position, assess the volume of amniotic fluid, and estimate the baby's weight.
- Uterine monitoring. Your health care provider might use a uterine monitor to measure the duration and spacing of your contractions.
- Lab tests. Your health care provider might take a swab of your vaginal secretions to check for the presence of certain infections and fetal fibronectin — a substance that acts like a glue between the fetal sac and the lining of the uterus and is discharged during labor. These results will be reviewed in combination with other risk factors. You'll also provide a urine sample, which will be tested for the presence of certain bacteria.
More Information
- Pelvic exam
- Ultrasound
Treatment
Medications
Once you're in labor, there are no medications or surgical procedures to stop labor, other than temporarily. However, your doctor might recommend the following medications:
-
Corticosteroids. Corticosteroids can help promote your baby's lung maturity.
 If you are between 23 and 34 weeks, your doctor will likely recommend corticosteroids if you are thought to be at increased risk of delivery in the next one to seven days. Your doctor may also recommend steroids if you are at risk of delivery between 34 weeks and 37 weeks.
If you are between 23 and 34 weeks, your doctor will likely recommend corticosteroids if you are thought to be at increased risk of delivery in the next one to seven days. Your doctor may also recommend steroids if you are at risk of delivery between 34 weeks and 37 weeks.You might be given a repeat course of corticosteroids if you're less than 34 weeks pregnant, at risk of delivering within seven days, and you had a prior course of corticosteroids more than 14 days previously.
- Magnesium sulfate. Your doctor might offer magnesium sulfate if you have a high risk of delivering between weeks 24 and 32 of pregnancy. Some research has shown that it might reduce the risk of a specific type of damage to the brain (cerebral palsy) for babies born before 32 weeks of gestation.
-
Tocolytics. Your health care provider might give you a medication called a tocolytic to temporarily slow your contractions. Tocolytics may be used for 48 hours to delay preterm labor to allow corticosteroids to provide the maximum benefit or, if necessary, for you to be transported to a hospital that can provide specialized care for your premature baby.

Tocolytics don't address the underlying cause of preterm labor and overall have not been shown to improve babies' outcomes. Your health care provider won't recommend a tocolytic if you have certain conditions, such as pregnancy-induced high blood pressure (preeclampsia).
If you're not hospitalized, you might need to schedule weekly or more-frequent visits with your health care provider so that he or she can monitor signs and symptoms of preterm labor.
Surgical procedures
If you are at risk of preterm labor because of a short cervix, your doctor may suggest a surgical procedure known as cervical cerclage. During this procedure, the cervix is stitched closed with strong sutures. Typically, the sutures are removed after 36 completed weeks of pregnancy. If necessary, the sutures can be removed earlier.
Cervical cerclage might be recommended if you're less than 24 weeks pregnant, you have a history of early premature birth, and an ultrasound shows your cervix is opening or your cervical length is less than 25 millimeters.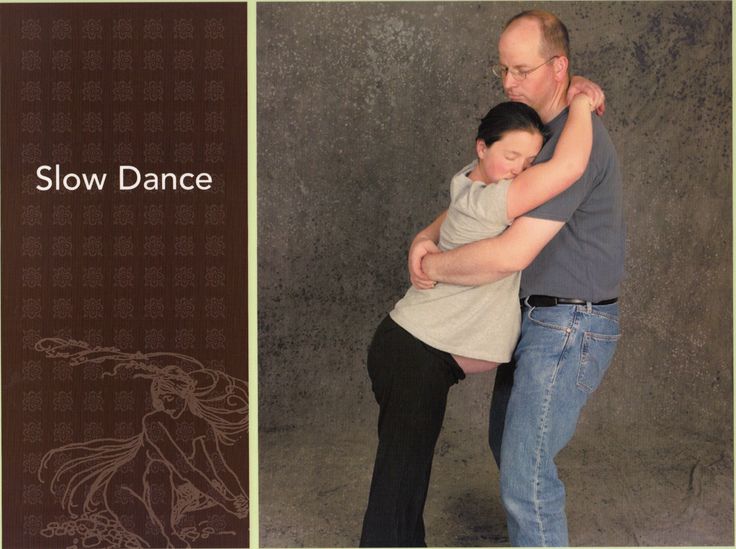
Preventive medication
If you have a history of premature birth, your health care provider might suggest weekly shots of a form of the hormone progesterone called hydroxyprogesterone caproate, starting during your second trimester and continuing until week 37 of pregnancy.
In addition, your health care provider might offer progesterone, which is inserted in the vagina, as a preventive measure against preterm birth. If you are diagnosed with a short cervix before week 24 of pregnancy, your health care provider might also recommend use of progesterone until week 37 of pregnancy.
Recent research suggests that vaginal progesterone is as effective as cervical cerclage in preventing preterm birth for some women who are at risk. The medication has the advantage of not requiring surgery or anesthesia. Your doctor may offer you medication as an alternative to cervical cerclage.
If you have a history of preterm labor or premature birth, you're at risk of a subsequent preterm labor. Work with your health care provider to manage any risk factors and respond to early warning signs and symptoms.
Work with your health care provider to manage any risk factors and respond to early warning signs and symptoms.
Request an Appointment at Mayo Clinic
Lifestyle and home remedies
Preterm contractions might be Braxton Hicks contractions, which are common and don't necessarily mean that your cervix will begin to open. If you're having contractions that you think might be a symptom of preterm labor, try walking, resting or changing positions. This might stop false labor contractions. If you're in true preterm labor, however, your contractions will continue.
Bed rest to manage preterm labor hasn't been shown to reduce the risk of preterm birth. Bed rest can lead to blood clots, emotional distress and muscle weakness.
Coping and support
If you're at risk of preterm labor or premature birth, you might feel scared or anxious about your pregnancy. This might be especially true if you have a history of preterm labor or premature birth. Consult your health care provider about healthy ways to relax and stay calm.
Preparing for your appointment
If you develop any signs or symptoms of preterm labor, contact your health care provider right away. Depending on the circumstances, you might need immediate medical care.
Here's some information to help you get ready for your appointment, as well as what to expect from your health care provider.
What you can do
Before your appointment, you might want to:
- Ask about pre-appointment restrictions. In most cases you'll be seen immediately. If that's not the case, ask whether you should restrict your activity while you wait for your appointment.
- Ask a loved one or friend to join you for your appointment. The fear you might be feeling about the possibility of preterm labor can make it difficult to focus on what your health care provider says. Take someone along who can help remember all the information.
- Write down questions to ask your health care provider.
 That way, you won't forget anything important that you want to ask, and you can make the most of your time with your health care provider.
That way, you won't forget anything important that you want to ask, and you can make the most of your time with your health care provider.
Below are some basic questions to ask your health care provider about preterm labor. If any additional questions occur to you during your visit, don't hesitate to ask.
- Am I in labor?
- Is there anything I can do to help prolong my pregnancy?
- Are there any treatments that could help the baby?
- What signs or symptoms should prompt me to call you?
- What signs or symptoms should prompt me to go to the hospital?
- What are the risks if my baby is born now?
What to expect from your health care provider
Your health care provider is likely to ask you a number of questions, including:
- When did you first notice your signs or symptoms?
- Are you having contractions? If so, how many an hour?
- Have you had any changes in vaginal discharge or bleeding?
- Have you been exposed to an infectious disease? Do you have a fever?
- Have you had any previous pregnancies, miscarriages, or cervical or uterine surgeries that I'm not aware of?
- Do you or did you smoke? How much?
- How far do you live from the hospital?
- How long would it take you to get to the hospital in an emergency, including time to arrange any necessary child care or transportation?
Preterm labor poses serious risks for your baby.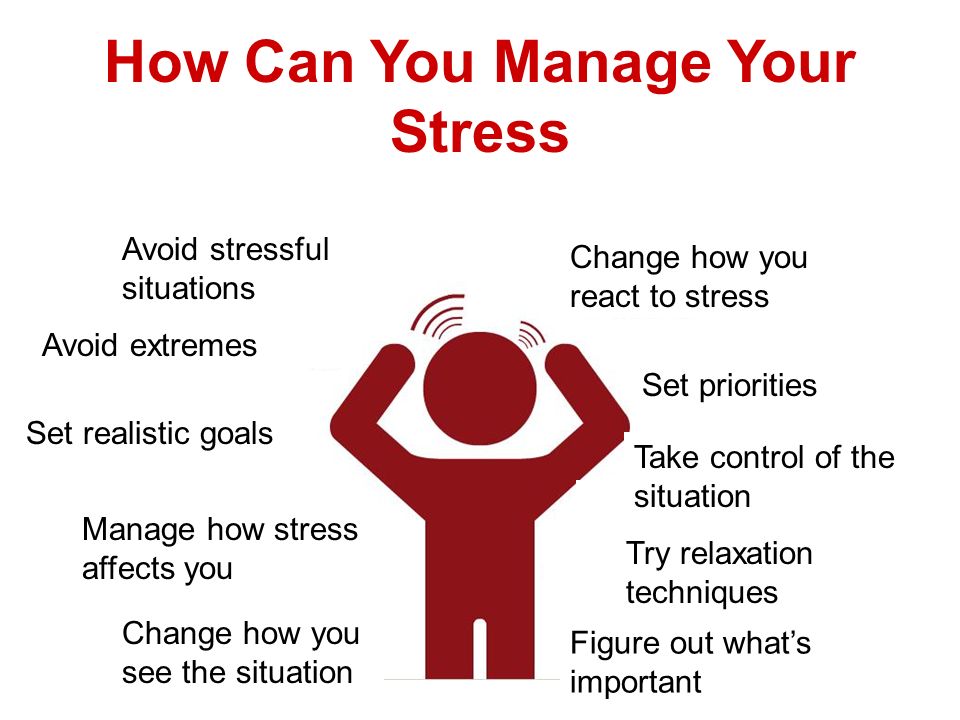 Work with your health care provider to understand your diagnosis and improve your chance of a healthy outcome.
Work with your health care provider to understand your diagnosis and improve your chance of a healthy outcome.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Treatments for preterm labor | March of Dimes
Treatments for preterm labor
Preterm labor is labor that happens too early, before 37 weeks of pregnancy. If you have preterm labor, your health care provider may recommend some treatments that may help stop your contractions and prevent health problems for you and your baby. They aren’t guaranteed, but research shows that they do help some people.
What kinds of medicines are used in preterm labor?
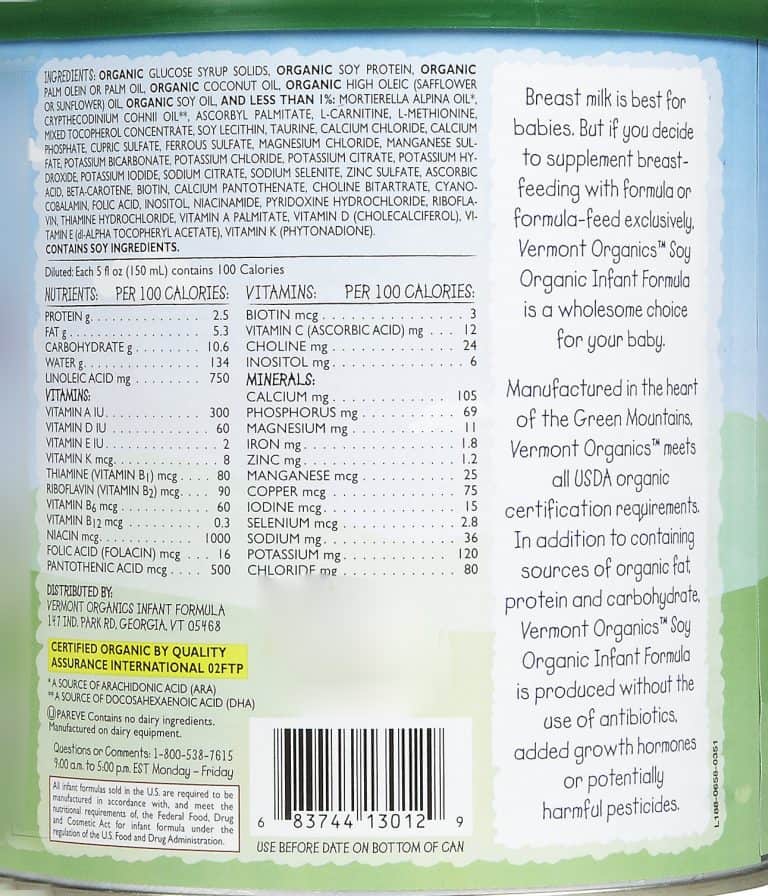
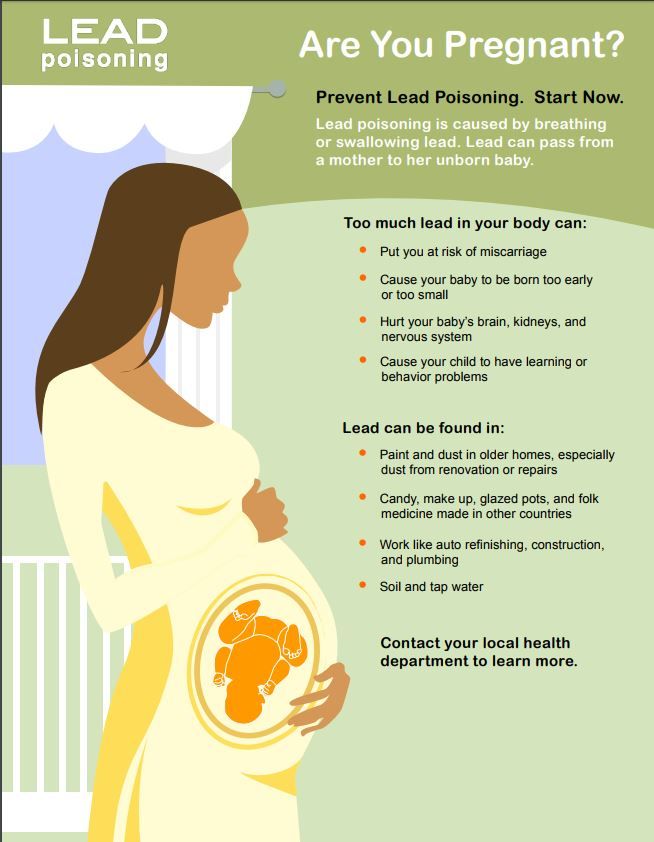
Antenatal corticosteroids (also called ACS). These include medicines such as betamethasone and dexamethasone. These speed up your baby’s lung development. They also help reduce your baby’s chances of having certain health problems after birth, including respiratory distress syndrome (also called RDS), intraventricular hemorrhage (also called IVH) and necrotizing enterocolitis (also called NEC). RDS is a condition that affects a baby's breathing. IVH is bleeding in the brain. NEC is a condition that affects a baby's intestines.
RDS is a condition that affects a baby's breathing. IVH is bleeding in the brain. NEC is a condition that affects a baby's intestines.
Antibiotics. These medicines, which include ceftriaxone, clarithromycin, and metronidazole, kill infections caused by bacteria. If you have a positive Group B strep test, or if you have preterm premature rupture of membranes (also called PPROM), your health care provider may give you antibiotics to help prevent infections in you and your baby. PPROM is when the sac around your baby breaks before 37 weeks of pregnancy.
Tocolytics. These medicines may be used to slow or stop labor contractions. There are several types, including:
- beta-adrenergic receptor agonists,
- calcium channel blockers,
- magnesium sulfate, and
- nonsteroidal anti-inflammatory drugs, or NSAIDs.
Tocolytics may delay labor, often for just a few days. This delay may give you time to get treatment with ACS or to get to a hospital that has a NICU (neonatal intensive care unit).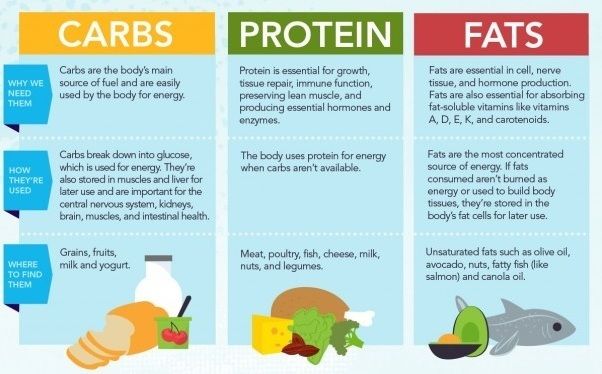 A NICU is a specialized nursery where newborns get medical care. If you have a health condition, such as a heart problem or severe preeclampsia, some tocolytics may not be safe for you. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Some of these signs include having protein in the urine, changes in vision and severe headache.
A NICU is a specialized nursery where newborns get medical care. If you have a health condition, such as a heart problem or severe preeclampsia, some tocolytics may not be safe for you. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Some of these signs include having protein in the urine, changes in vision and severe headache.
Do medicines used during preterm labor have side effects?
Yes. A side effect is an effect of a drug or medicine that is not the intended result. For example, a side effect of some cold medicines is that they make you sleepy. Side effects can be different for everyone
What side effects can antenatal corticosteroids cause?
Antenatal corticosteroids are given as two injections within a 24 to 48-hour period. Possible side effects for you may include elevated blood sugar.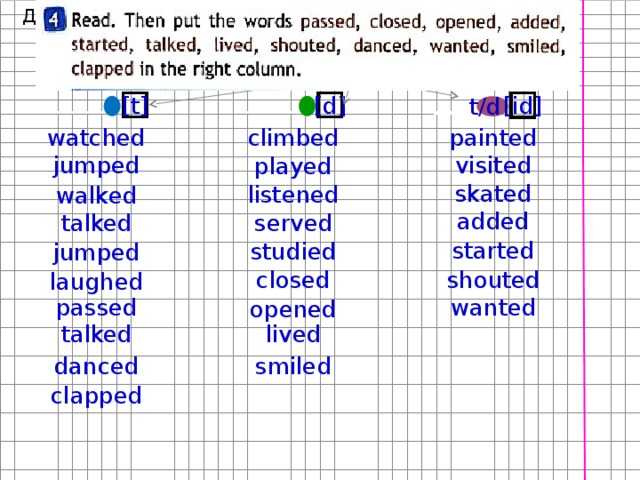 If you take insulin and receive antenatal corticosteroids, your insulin regimen may need to be adjusted.
If you take insulin and receive antenatal corticosteroids, your insulin regimen may need to be adjusted.
What side effects can tocolytics cause?
Beta-adrenergic receptor agonists may cause your baby to have a fast heartbeat. Possible side effects for you may include:
- Chest pain; fast or irregular heartbeat
- Breathing trouble; fluid in the lungs
- Diarrhea, nausea (feeling sick to your stomach), throwing up
- Feeling dizzy; shaking or feeling nervous; seizures
- Fever, headache
- High blood sugar
- Low blood pressure; low blood potassium
Side effects of calcium channel blockers for you may include:
- Constipation, diarrhea, nausea
- Feeling dizzy or faint
- Headache
- Low blood pressure
- Redness of the skin
Magnesium sulfate may cause the following side effects for your baby:
- Being tired and drowsy
- Slowed breathing
- Weak muscles
- Low levels of calcium and bone problems, if the medicine is used for more than 5 to 7 days.
Side effects of magnesium sulfate for you may include:
- Breathing problems, fluid in the lungs
- Dry mouth
- Fatigue (being very tired), weak muscle
- Headache, double vision, slurred speech
- Heart attack
- Nausea or throwing up
- Redness of the skin, heavy sweating
NSAIDs, such as indomethacin. For your baby, these medicines may cause:
- Bleeding in the brain or heart
- Patent ductus arteriosus, also called PDA. This is a heart problem that’s common in premature babies.
- Jaundice. This is a common condition caused by too much bilirubin in the blood. Jaundice refers to the temporary yellow color of the skin and white parts of the eyes.
- Kidney problems, such as making too little urine
- Necrotizing enterocolitis. This is a problem in a baby’s intestines.
- Rising blood pressure in the lungs
Side effects for you might include:
- Feeling dizzy
- Heartburn
- Nausea or throwing up
- Oligohydramnios.
 This is when you have too little amniotic fluid. Amniotic fluid is the fluid that surrounds your baby in the womb.
This is when you have too little amniotic fluid. Amniotic fluid is the fluid that surrounds your baby in the womb. - Swollen stomach lining
- Vaginal bleeding
Talk with your health care provider about the benefits and risks of medicines.
Last reviewed: December 2020
What will help in childbirth - articles from the specialists of the clinic "Mother and Child"
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now, on the contrary, obstetricians recommend that the expectant mother move . For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease. Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals. And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation. nine0003
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
We hang on a rope or wall bars
When the contractions become very strong and painful, you can take poses in which the stomach is, as it were, in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow. In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain. nine0003
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If during childbirth a woman wants not to move, but, on the contrary, to lie down, then, of course, she can lie down. In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
We use everything we have
In any road block, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs. nine0003
In general, it is worth showing imagination and adapting any item in the rodblock to your needs. nine0003
And don't be afraid to look stupid during childbirth. No one in the delivery room cares about how you move or lie down as long as it helps you get through your contractions, so calmly find your comfortable position.
Giving birth in an uncomfortable position is both difficult and inefficient. So memorize and rehearse some poses beforehand, and if there are any fixtures in the rodblock, try using them. Something of this will definitely help you to comfortably and easily survive childbirth.
When we move, take various postures, the blood supply to the uterus improves, as a result, it contracts better, and the cervix opens faster. In addition, uteroplacental blood flow improves, and therefore the baby does not suffer from hypoxia
strength to push
By clicking on the send button, I consent to the processing of personal data
Ways to help pregnant women avoid preterm labor
What is the problem?
Preterm birth, or birth before 37 weeks of gestation, is the leading cause of newborn death and can also lead to long-term disability in surviving infants. There are many ways health professionals try to prevent preterm labor in women. Pregnant women may be asked to take vitamins, limit smoking, take medicines to treat infections, or attend regular checkups with specialists. Our review looks at different ways (or interventions) to prevent preterm birth. We searched the Cochrane Library for relevant documents on November 2, 2017. nine0003
There are many ways health professionals try to prevent preterm labor in women. Pregnant women may be asked to take vitamins, limit smoking, take medicines to treat infections, or attend regular checkups with specialists. Our review looks at different ways (or interventions) to prevent preterm birth. We searched the Cochrane Library for relevant documents on November 2, 2017. nine0003
Why is this important?
Premature births have devastating and costly consequences for women, families and health systems. We wanted to summarize relevant information for pregnant women, healthcare professionals and researchers.
What evidence did we find?
We included 83 systematic reviews of evidence of whether certain interventions reduced the chance of preterm birth or death in children. Seventy reviews contained information on preterm birth. We categorized the evidence we found as follows: clear benefit or harm; no effect; possible benefit or harm; unknown effect.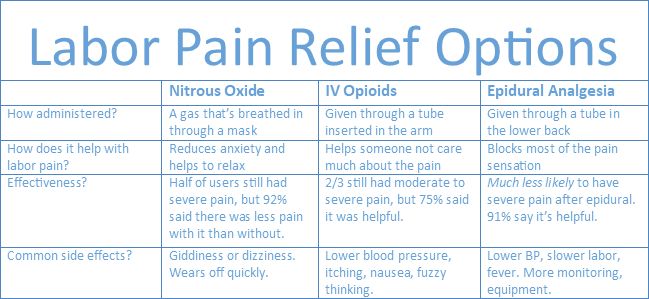 nine0003
nine0003
Outcome: preterm birth
Clear Benefit
We were confident that the following interventions helped specific groups of pregnant women avoid preterm labor: continuous obstetric care models versus other models of care for all women; screening for lower genital tract infections; zinc supplements for pregnant women without systemic diseases. Cervical suturing (cerclage) was only useful for women at high risk of preterm birth and singleton pregnancies. nine0003
Clear harm
We did not find any interventions that increased the chance of preterm birth in women.
Potential benefits
The following interventions may have helped some groups of pregnant women avoid preterm birth, but we are less certain about these results: group antenatal care for all pregnant women; antibiotics for pregnant women with asymptomatic bacteriuria; pharmacological interventions for smoking cessation; vitamin D supplements for women without health problems. nine0003
nine0003
Potential harm
We found two interventions that may make some pregnant women worse: intramuscular progesterone for women at high risk of preterm birth and multiple pregnancies; supplementation of vitamin D, calcium and other minerals by pregnant women without health problems.
Exodus: perinatal death
Clear benefit
We were confident in the evidence for the continuous obstetric monitoring model for all pregnancies and fetal and umbilical cord Doppler for high-risk pregnant women; these interventions appear to reduce a woman's chance of child death. nine0003
Overt harm
We did not find any interventions that increased the woman's risk of child death.
Potential benefits
We have found a possible benefit of cervical sutures (cerclage) for women with singleton pregnancies at high risk of preterm birth.
Possible harms
One review reported possible harms associated with fewer antenatal visits, even for pregnant women at low risk of pregnancy problems. The pregnant women in this review already received limited antenatal care. nine0003
The pregnant women in this review already received limited antenatal care. nine0003
Outcome: preterm birth and perinatal death
Unknown benefit or harm
It is not known whether home monitoring of uterine activity was helpful or harmful for pregnant women at high risk of preterm birth for any reason, including multiple pregnancies. The benefits or harms of the following interventions for high-risk pregnant women with multiple pregnancies have not been established: bed rest, prophylactic oral beta-mimetics, vaginal progesterone, and cervical cerclage. nine0003
What does this mean?
The Cochrane Library contains valuable information for women, clinicians, midwives and researchers interested in preventing preterm birth. We summarized the results of systematic reviews to describe how well different strategies for preventing early birth and death of children work. We have organized the information we found in a clear graphical way to show our confidence in the results and point readers to promising interventions for certain groups of pregnant women.