What is an epidural used for
Epidural - NHS
An epidural is an injection in your back to stop you feeling pain in part of your body.
This page covers epidural anaesthesia, a type of epidural commonly given for pain relief in childbirth and in some types of surgery.
When epidurals are used
Epidurals can be used:
- during labour and childbirth, including caesareans
- during some types of surgery
- after some types of surgery
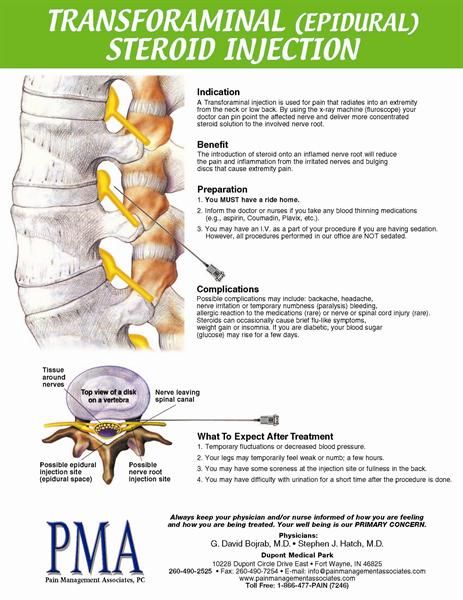
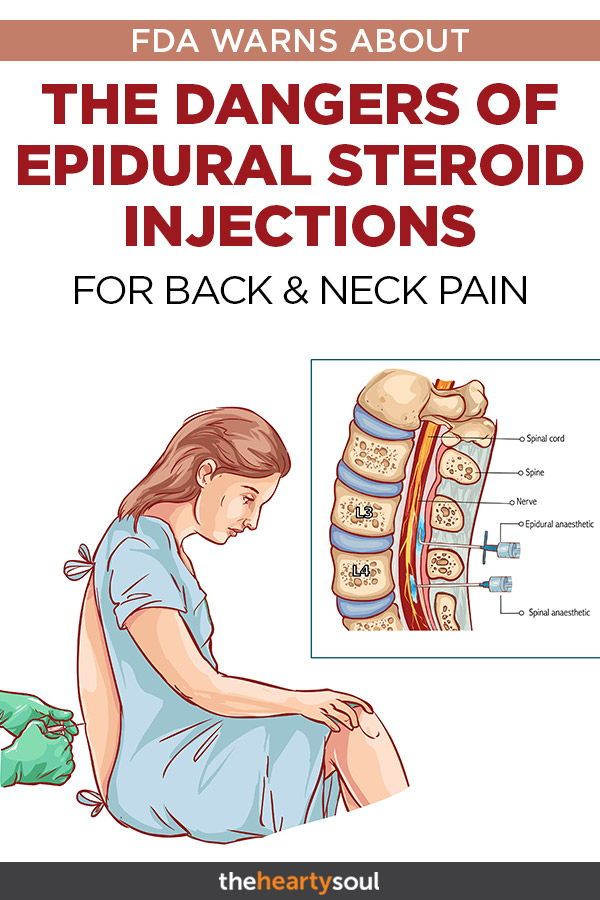
Steroid medicine can also be given with an epidural injection, to treat pain in your back or leg that's caused by sciatica or a slipped (prolapsed) disc.
Preparing for an epidural
If you have any concerns or questions about having an epidural, discuss these with your doctor. Let them know about any medicines you're taking.
You may be given specific advice about eating, drinking and medicines before the epidural.
As you will not be able to drive for 24 hours after having an epidural, so you'll need to arrange for someone to take you home.
How an epidural is given
Epidurals are given by a specialist doctor called an anaesthetist.
You're usually awake during an epidural, but for some types of surgery you may have it while under general anaesthetic.
- A drip will be placed in your arm so you can be given fluids while you're having the epidural.
- You'll be asked to sit down and lean forwards, or lie on your side with your knees up close your chest.
- You'll be given an injection of local anaesthetic to numb the skin where the epidural will be inserted.
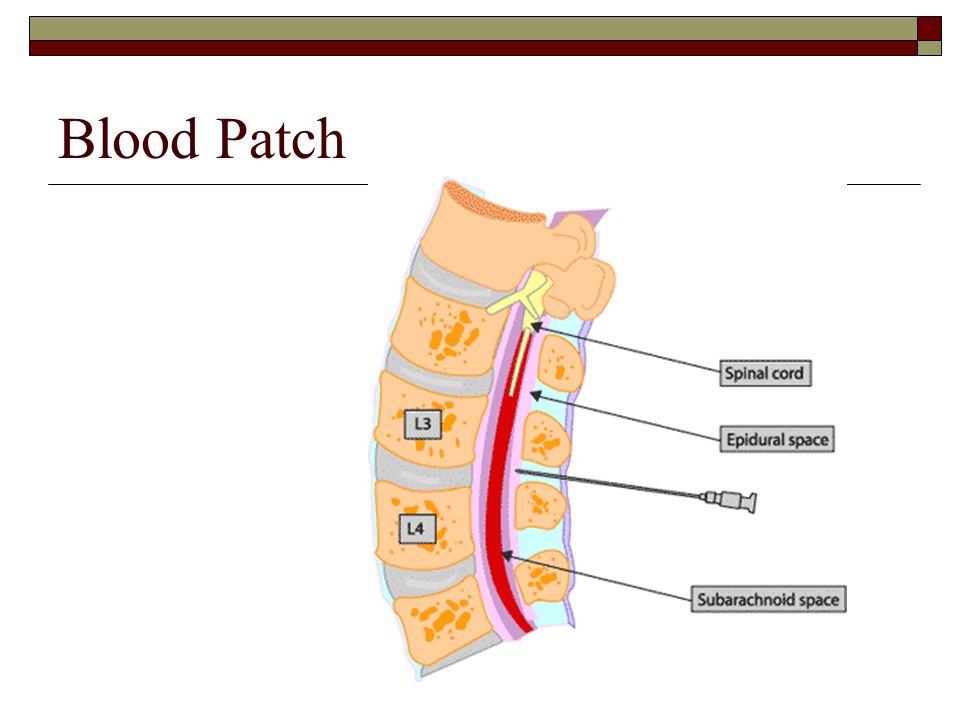
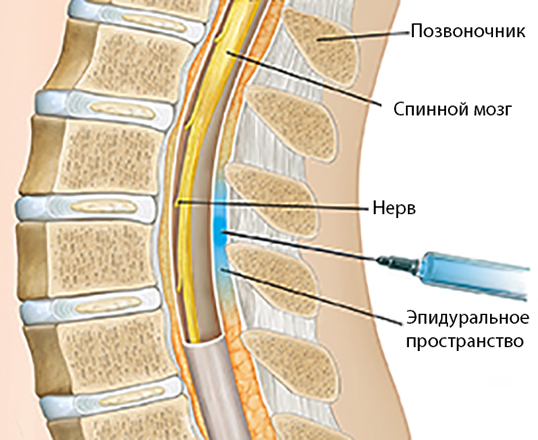
- A needle is used to insert a fine plastic tube called an epidural catheter into your back (spine) near the nerves that carry pain messages to your brain.
- The needle is then removed, leaving just the catheter in your spine.

- You may feel mild discomfort when the epidural needle is positioned and the catheter is inserted.
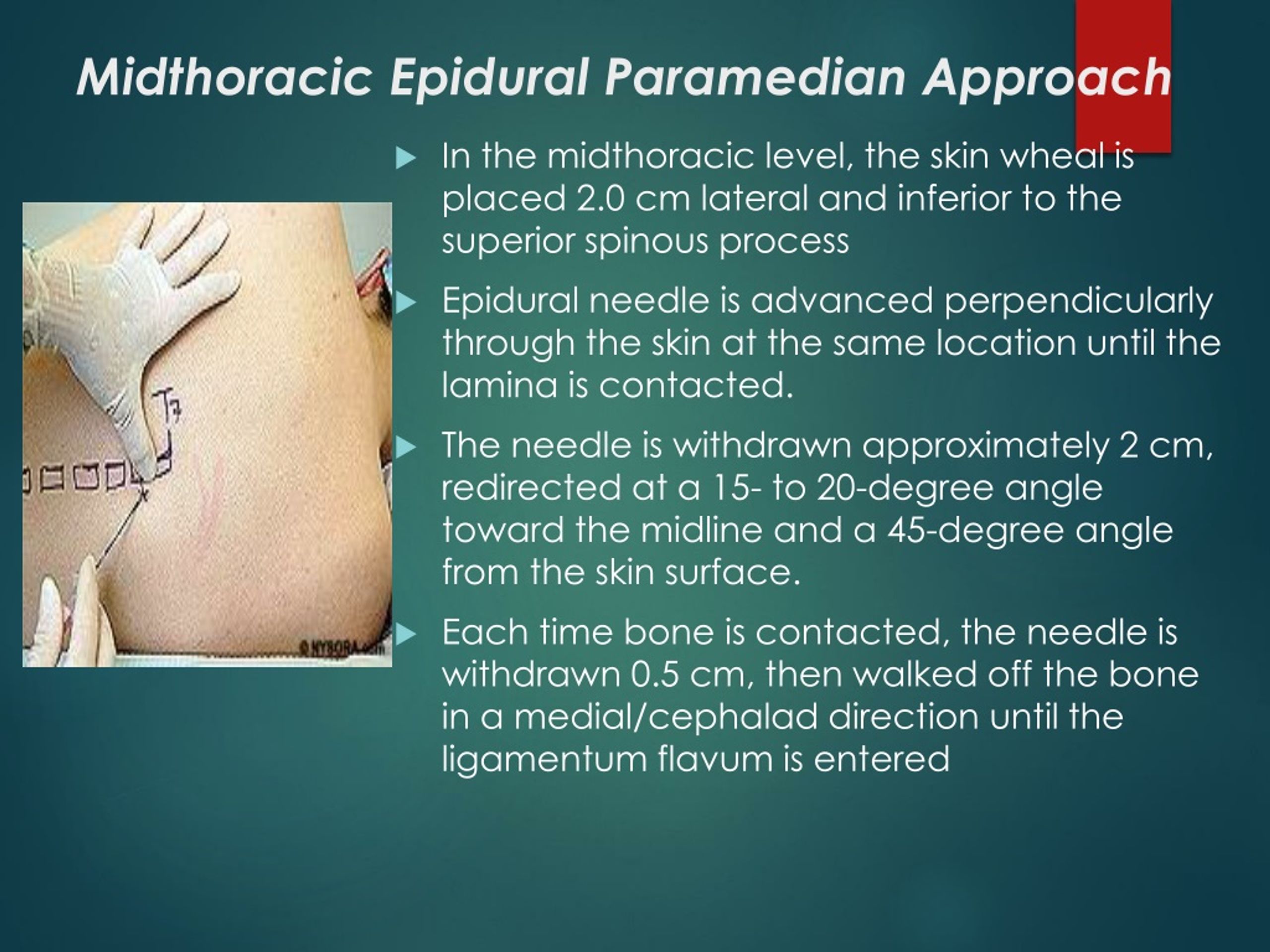
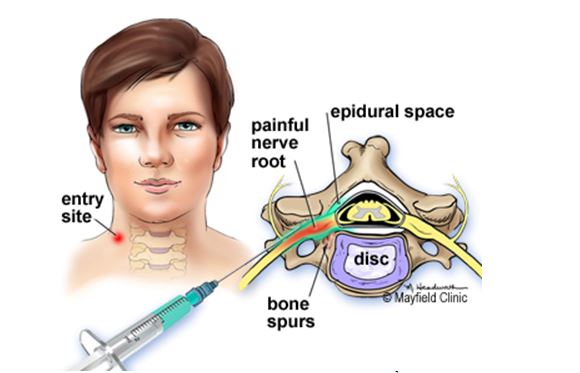
The epidural can be inserted at different levels of your spine, depending on the area of your body that needs pain relief.
Pain relief medicines are then given through the catheter. These take about 20 to 30 minutes to take full effect.
Your chest, tummy and legs may feel numb while the epidural medicines are being used, and your legs may not feel as strong as usual.
While the catheter remains in your back, it can be used to top up your pain relief medicines manually or using an automatic pump.
This can be for several hours (during childbirth) or for a few days (after major surgery).
Mobile epidurals, which use a lower dose of pain relief medicines, are sometimes used in childbirth, allowing you to walk around during labour.
Recovering from an epidural
When the epidural is stopped, the numbness usually lasts for a few hours before its effects begin to wear off.
While the medicine wear off, you'll probably be advised to rest in a lying or sitting position until the feeling in your legs returns.
This can take a couple of hours, and you may feel a slight tingling sensation in your skin.
Tell the doctor or nurse if you feel any pain. They can give you medicines to help control it.
Do not drive, operate machinery or drink alcohol for 24 hours after having an epidural.
Risks and side effects of an epidural
Epidurals are usually safe, but there's a small risk of side effects and complications, including:
- low blood pressure, which can make you feel lightheaded or nauseous
- temporary loss of bladder control
- itchy skin
- feeling sick
- headaches
- nerve damage
Read more about the side effects and complications of an epidural.
Page last reviewed: 11 March 2020
Next review due: 11 March 2023
What It Is, Procedure, Risks & Side Effects
Overview
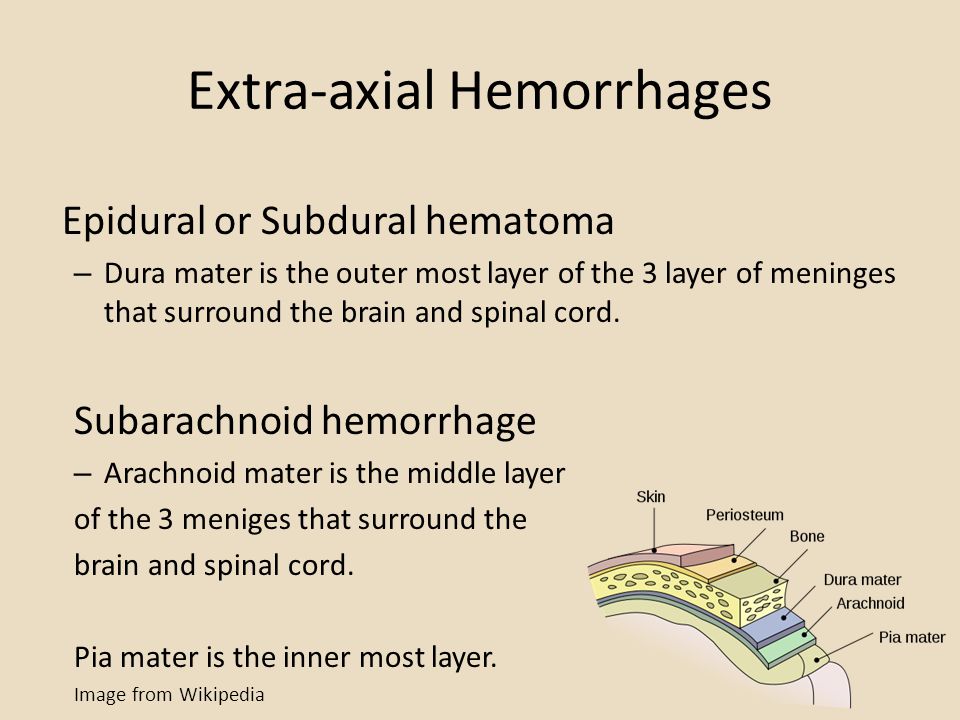
An epidural injects medication into the space around your spinal nerves known as the epidural space.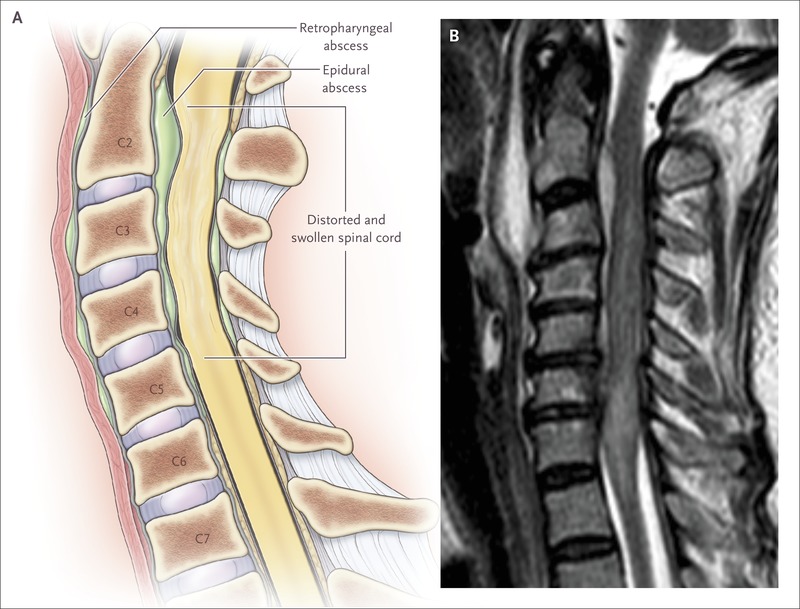
What is an epidural?
An epidural is a procedure that involves injecting a medication — either an anesthetic or a steroid — into the space around your spinal nerves known as the epidural space. The goal of an epidural procedure is to provide pain relief (analgesia) or a complete lack of feeling (anesthesia) for one region of your body, such as your legs or belly.
An epidural is commonly called the following terms:
- Epidural anesthesia.
- Epidural block.
- Epidural steroid injection (ESI).
- Regional anesthesia.
- Neuraxial anesthesia.
How does an epidural work?
An epidural anesthesia injection works by injecting an anesthetic into the epidural space around your spine so that it can stop pain signals from traveling from your spine to your brain. The epidural space is filled with fluid and surrounds your spinal cord. Think of it as a liquid sleeve around your spinal cord.
Your spinal cord acts like a highway that connects the nerves located all over your body to your brain.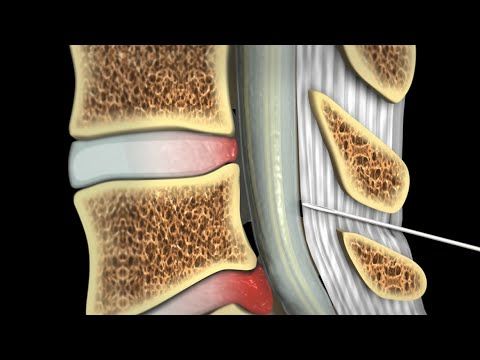 When you get injured, for example, the nerve in that area of your body sends a pain signal that travels through your spinal cord to your brain and back. An epidural anesthetic temporarily numbs the spinal nerves, which then blocks pain signals in a certain region of your body depending on where along your spine your provider injected the epidural.
When you get injured, for example, the nerve in that area of your body sends a pain signal that travels through your spinal cord to your brain and back. An epidural anesthetic temporarily numbs the spinal nerves, which then blocks pain signals in a certain region of your body depending on where along your spine your provider injected the epidural.
Epidural anesthesia can provide temporary pain relief or a temporary total lack of feeling. The following factors contribute to how much feeling you temporarily lose from an epidural:
- The type of anesthetic drug your provider uses.
- The concentration of the drug (how strong it is).
- The dosage of the drug.
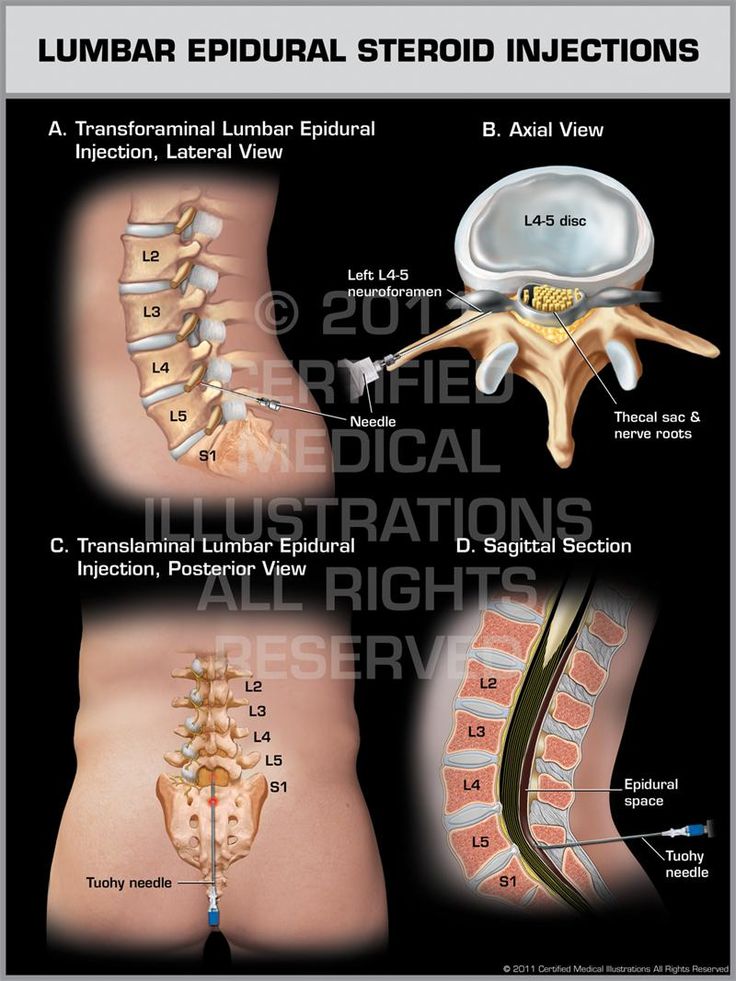
An epidural steroid injection (ESI) works slightly differently and is used for chronic pain management. Instead of anesthetic medication, your provider injects a steroid or corticosteroid medication into the epidural space around your spine. Instead of blocking pain or feeling in a region of your body, the steroid coats the irritated nerve(s) that are causing you pain and works to reduce swelling.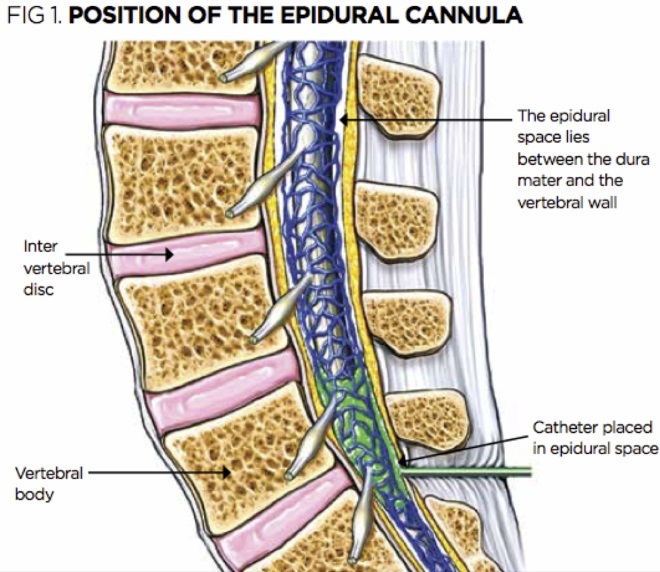 The steroid allows the nerve(s) time to heal. Epidural steroid injections can lead to temporary, long-term or permanent pain relief.
The steroid allows the nerve(s) time to heal. Epidural steroid injections can lead to temporary, long-term or permanent pain relief.
Who performs an epidural?
An anesthesiologist or certified registered nurse anesthetist usually performs an epidural procedure. Anesthesiologists have special training in the field of anesthesiology, which is a medical specialty that involves the care of people before, during and after their surgery or procedure. Anesthesiology covers anesthesia, pain medicine, intensive care medicine and critical emergency medicine.
Healthcare providers of other specialties, such as neurology, may also perform an epidural. Again, they’re specially trained to properly and safely perform an epidural procedure.
For epidural procedures that use a catheter, a supporting healthcare provider is usually present to help as needed.
What’s the difference between epidural analgesia and epidural anesthesia?
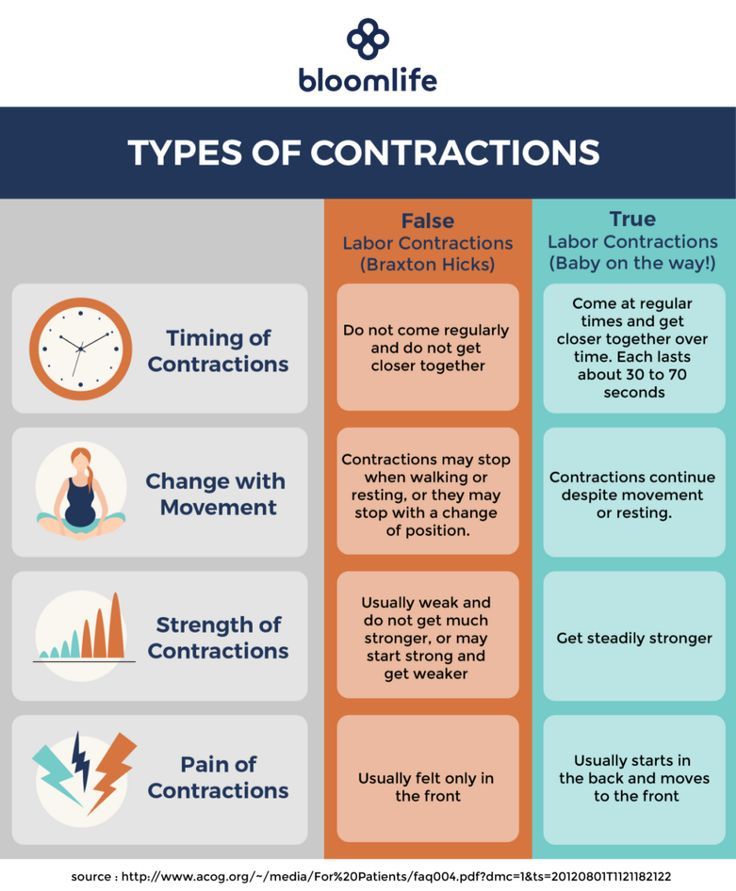
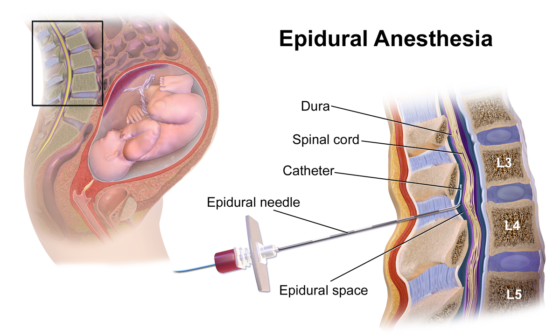
Analgesia is pain relief without losing consciousness (going to sleep) and without complete loss of feeling or movement. Anesthesiologists use epidural analgesia for people who are in labor and are delivering a baby. They inject the epidural into your lower back to provide pain relief for the lower part of your body due to contractions and childbirth.
Anesthesiologists use epidural analgesia for people who are in labor and are delivering a baby. They inject the epidural into your lower back to provide pain relief for the lower part of your body due to contractions and childbirth.
Anesthesia is the loss of physical sensation with or without loss of consciousness. Epidural anesthesia itself won’t cause a loss of consciousness, but if you’re having a certain kind of surgery, your anesthesiologist may give you epidural anesthesia so you don’t feel any pain or don’t move during the surgery and a different medication to make you go to sleep (lose consciousness).
What are epidurals used for?
Your healthcare provider may recommend an epidural procedure for the following situations:
- To provide pain relief (analgesia) for labor and childbirth.
- To provide anesthesia for certain surgeries as an alternative to general anesthesia.
- To provide pain relief after certain surgeries.
- To manage certain causes of back pain and other forms of chronic pain (through epidural steroid injections).
What are the different kinds of epidurals?
There are different variations of epidurals based on certain factors. This section will explain different kinds of epidurals grouped into the following categories:
- How the medication is delivered.
- Labor and childbirth epidurals.
- Epidural steroid injections (ESI).
Epidural medication delivery options
There are a few ways your healthcare provider can deliver medication with an epidural, including:
- Single-injection epidural: This type of epidural involves one injection of a medication (an anesthetic or a steroid) into the epidural space around your spine. If you get a single injection of an anesthesia epidural, the feeling in your affected area usually returns within a few hours. A single injection anesthesia epidural is for short-term pain relief. Most epidural steroid injections are single injections.
- Epidural with a catheter: Most epidural procedures involve the use of a catheter in your epidural space so that your healthcare provider can give you a continuous flow of anesthetic medication, multiple separate doses or both.
 A catheter is a small, flexible tube that’s inserted through a narrow opening into a body cavity. In this case, your provider places a catheter that opens into the epidural space in your spinal area. This way, your provider can administer more than just one injection of medication. Providers usually recommend this type of epidural for longer operations, for providing pain relief over several days and for labor and childbirth.
A catheter is a small, flexible tube that’s inserted through a narrow opening into a body cavity. In this case, your provider places a catheter that opens into the epidural space in your spinal area. This way, your provider can administer more than just one injection of medication. Providers usually recommend this type of epidural for longer operations, for providing pain relief over several days and for labor and childbirth. - Epidural with patient-controlled analgesia (PCA): For recovery from certain kinds of surgery, your healthcare provider may allow you to control the amount of pain relief you’re receiving through your epidural catheter. This is called patient-controlled analgesia (PCA). Your healthcare provider sets controls on the PCA pump, which are programmed for the pain-relieving drug your provider orders based on your age, weight and the type of surgery you had. The PCA pump is safe to use because you receive medication by pressing a button when you feel pain, but the pump won’t give you the medication if it’s not time to receive another dose yet.

Labor and delivery epidurals
There are two general kinds of epidurals that you may choose during labor and childbirth. These include:
- Epidural with a catheter: Your provider will administer medicine through a catheter in your lower back that they insert with an epidural injection. The catheter remains in your epidural space so that your provider can give you more medication if needed.
- Combined spinal-epidural (CSE): A CSE is a combination of two injections: a spinal injection (spinal block) and an epidural. A CSE provides pain relief much faster than just an epidural. Because it involves a lower dose of medication, you’ll have a bit more feeling in your lower half. This allows you to move around more easily and change positions. This type of epidural is often called a “walking” epidural, but most people aren’t able to fully walk with this kind of epidural.
Epidural steroid injections (ESI)
An epidural steroid injection (ESI) involves an injection of a steroid or corticosteroid into your epidural space.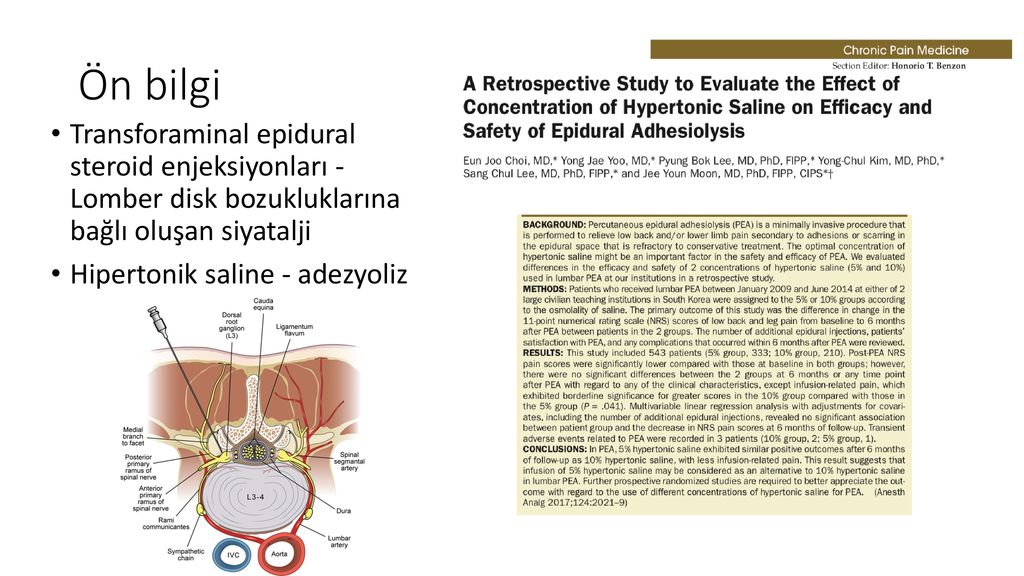 It can help relieve neck, arm, back and leg pain caused by inflamed spinal nerves due to certain conditions or injuries. Pain relief from an ESI may last for several days or even years.
It can help relieve neck, arm, back and leg pain caused by inflamed spinal nerves due to certain conditions or injuries. Pain relief from an ESI may last for several days or even years.
People who have pain in their neck, arm, lower back or leg due to the following conditions may benefit from epidural steroid injections:
- Spinal stenosis.
- Spondylolisthesis.
- Herniated disk (slipped, ruptured or bulging disk).
- Degenerative disk disease.
- Sciatica.
How common are epidurals?
Epidurals are a common procedure. An epidural is the most popular method of pain relief during labor and childbirth. More than 50% of people who give birth at a hospital choose to receive epidural analgesia. Epidural steroid injections (ESI) are one of the most commonly performed pain relief procedures.
Who shouldn’t get an epidural?
Due to certain medical conditions, not everyone can have an epidural. Because of this, it’s important to talk to your healthcare provider about your medical history and any questions you have.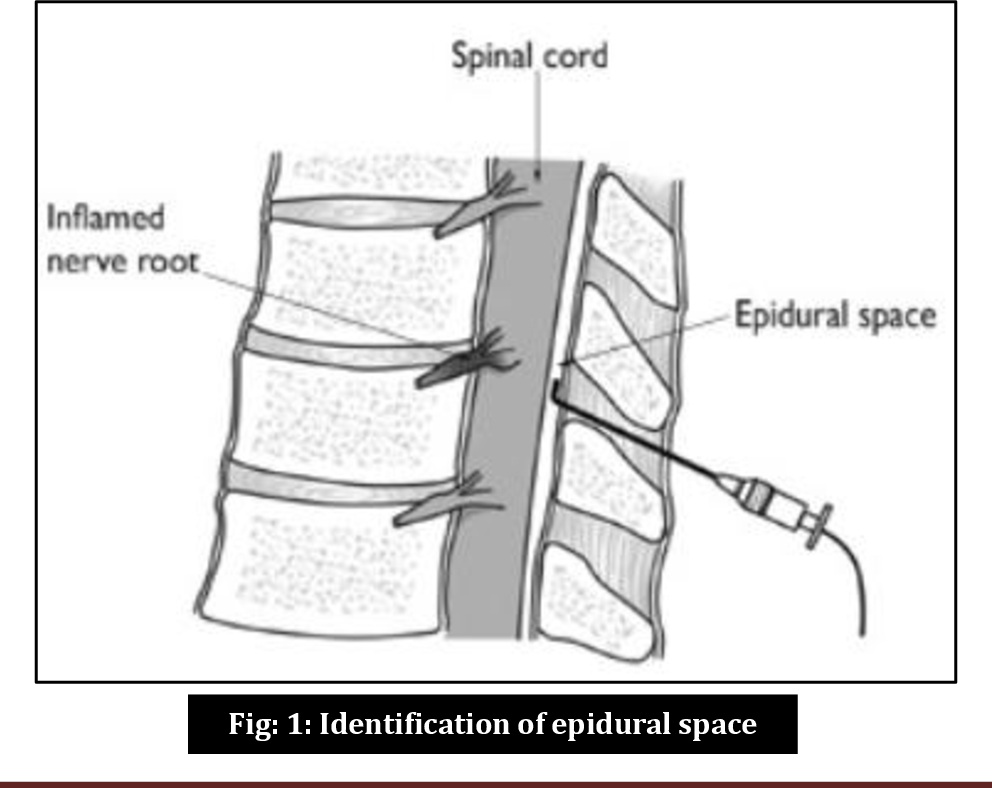 If you have any of the following conditions, you may not be able to get an epidural:
If you have any of the following conditions, you may not be able to get an epidural:
- Anesthetic drug allergies.
- Blood clotting issues.
- An infection.
- Poorly managed diabetes (for epidural steroid injections).
If you’re unable to undergo an epidural procedure, your healthcare provider may recommend another type of pain relief or anesthesia for you, or they may have you wait until a better time to have your surgery, if possible.
Procedure Details
How do I prepare for an epidural?
Your healthcare provider will give you specific instructions about what you need to do to prepare for your epidural. Be sure to follow their instructions. Your provider may:
- Have you not eat or drink for a certain amount of time before your epidural.
- Adjust certain medications you’re taking, especially blood thinner medications.
- Make sure you have someone with you to drive you home after your epidural.
Questions that may be helpful to ask your healthcare provider before you get an epidural include:
- How often do you perform epidurals?
- What do I need to do to prepare for my epidural?
- What are the risks of getting an epidural?
- What will my epidural feel like?
- How long will my epidural last?
- How long will it take to recover from my epidural?
What happens during the epidural procedure?
This section will explain the general procedure for two kinds of epidurals: epidurals that use a catheter and epidural steroid injections.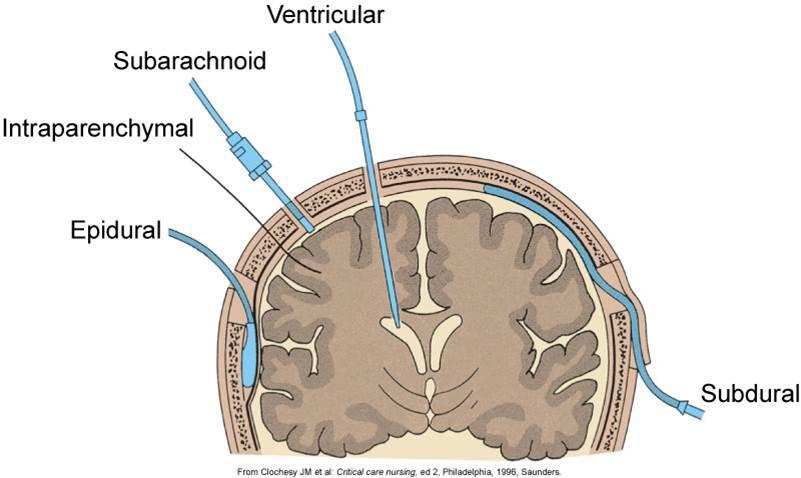
Single-injection epidurals are similar in procedure to epidurals that use a catheter except there’s no catheter placement. Your provider will inject one dose of medication when they insert the needle into your epidural space.
Epidural with a catheter procedure
The steps involved in an epidural procedure that uses a catheter include:
- Before your epidural procedure, a healthcare provider will likely insert a cannula into a vein in your arm so that a medical drip can be attached to it if needed. This is a safety precaution in case your blood pressure drops during the epidural. If this happens, your provider can access the cannula very quickly to give you medication to help stabilize your blood pressure.
- You will likely have to lie on your side or sit up — either way, you’ll need to tuck in your chin to your chest and hunch your back so that your provider can more easily see and access the area where they’ll insert the epidural.
- Your provider will thoroughly clean the area of your back where they’ll insert the epidural to minimize the risk of infection.

- They will then inject local anesthesia with a small needle near the area where they’ll insert the epidural. This is so you won’t feel as much pain when they insert the epidural needle, which is larger than a standard shot needle, such as a vaccine shot needle.
- Your provider will then insert the epidural needle into your back in the epidural space just outside of your spinal cord. If you’re getting an epidural for labor and childbirth, it’ll be in your lower back.
- They’ll then thread a small, soft tube called a catheter through the needle and into your back where the needle went in
- They’ll remove the epidural needle, and the catheter will remain in your back.
- Now your provider can give you anesthetic medicine through the catheter for as long as it’s needed.
- Once you no longer need the epidural, your provider will remove the catheter, clean the area again with an antiseptic and apply a dressing over the site.
Epidural steroid injection procedure
Epidural steroid injections are often used to manage or treat chronic pain. Depending on what’s causing your pain, your healthcare provider will inject the epidural somewhere along your spine. Here are the general steps of an epidural steroid injection procedure:
Depending on what’s causing your pain, your healthcare provider will inject the epidural somewhere along your spine. Here are the general steps of an epidural steroid injection procedure:
- You will lie on a comfortable table on your stomach or side.
- Your healthcare provider will thoroughly clean the area of your back where they’ll insert the epidural to minimize the risk of infection.
- Your provider will inject local anesthesia with a small needle near the area where they’ll insert the epidural. This is so you won’t feel as much pain when they insert the epidural needle, which is larger than a standard shot needle.
- Once the area is numb, your provider will most likely use an imaging machine, such as fluoroscopy equipment or a CT scanner (both are radiology imaging) to help guide the epidural needle to exactly the right position.
- When the epidural needle is in place in the epidural space around your spinal cord, your provider will inject the contrast material.
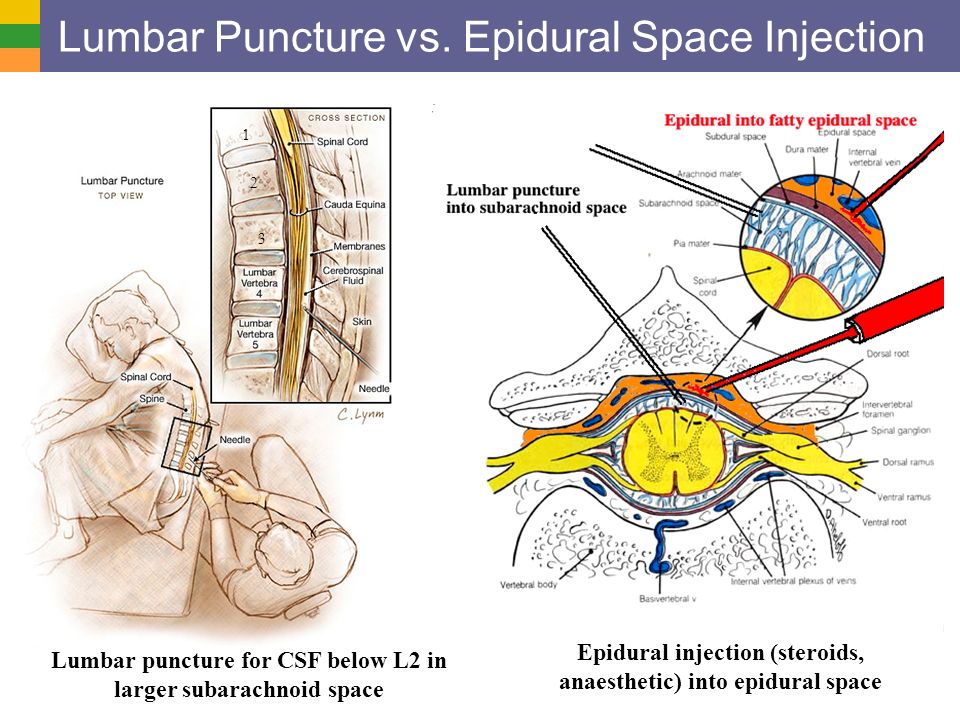 The contrast material will make it easier for your provider to see the area they’re targeting on the screen of the imaging machine. This helps to make sure that the medication will reach the inflamed nerves they are targeting.
The contrast material will make it easier for your provider to see the area they’re targeting on the screen of the imaging machine. This helps to make sure that the medication will reach the inflamed nerves they are targeting. - Your provider will then slowly inject the medication, which is usually an anti-inflammatory medication, such as a steroid or corticosteroid. Some providers may inject a mixture of a corticosteroid and a long-acting anesthetic.
- When your provider is done with the injection they’ll clean the area again and apply a dressing to the site. You’ll move into a chair or bed to rest for a few minutes to an hour. This is so your provider can make sure you don’t have any reactions to the medication before you go home.
What will I experience during my epidural procedure?
You’ll likely experience a minor pinch when your provider injects the local anesthetic to numb the area before the epidural procedure.
You may feel pressure, tingling, a burning sensation or momentary shooting pain when your provider injects the epidural.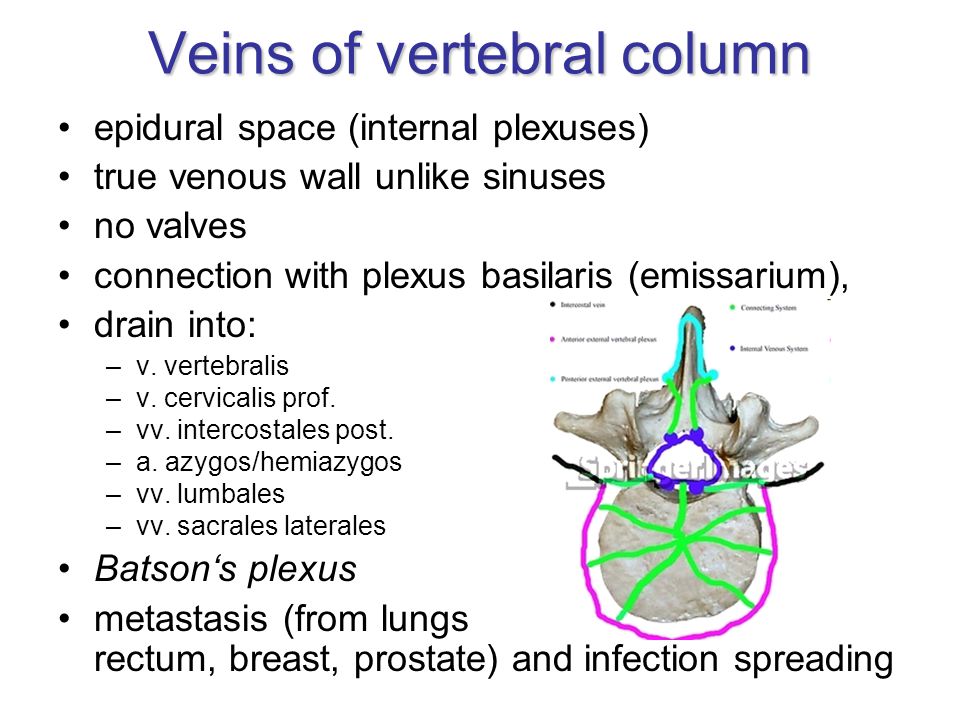 Or you may not feel anything. If you have any discomfort during the injection, it usually disappears once the injection is finished.
Or you may not feel anything. If you have any discomfort during the injection, it usually disappears once the injection is finished.
If you feel intense sharp pain during or after your epidural procedure, tell your provider immediately.
What happens after the epidural procedure?
If you’ve had an epidural with anesthetic medication, it’ll take 20 to 30 minutes for your pain relief and/or loss of feeling to take full effect.
Epidural steroid injections start working within two to seven days, and the pain relief can last several days or longer.
Risks / Benefits
What are the advantages of getting an epidural?
There are different advantages of getting an epidural depending on why you’re getting it.
The advantages of getting epidural analgesia during labor and childbirth include:
- They are usually very effective in minimizing pain felt during labor and delivery.
- They are generally very safe.
- You can often still move around in your bed and push when you need to.
- If you’re experiencing prolonged labor, having an epidural helps you to sleep and recover your strength.
- If you're undergoing a cesarean birth (C-section), you can stay awake during the birth, and your partner can be there as well.
- You can usually get an epidural at any time during your labor.
The advantages of epidural anesthesia injections for surgery include:
- You’ll likely experience less nausea and vomiting than you might with general anesthesia.
- You’ll have a quicker recovery after the surgery than you would with general anesthesia.
- You may have a lower risk of developing a blood clot in one of your leg veins (deep vein thrombosis, or DVT) than you would if you had general anesthesia.
The advantages of epidural steroid injections include:
- You’ll likely experience temporary or long-term pain relief.
- You’ll likely have a better quality of life and an improved ability to do daily activities without the restrictions previously caused by pain.
- Epidural steroid injections may help confirm the origin of your pain. This is often a problem in people who have more than one possible cause of pain.
- Epidural steroid injections may reduce the need for more invasive procedures for pain management.
What are the risks or complications of getting an epidural?
Epidurals are usually safe, but there are risks of certain side effects and complications. Although rare, risks and complications that apply to all types of epidural procedures include:
- Having low blood pressure, which can make you feel lightheaded.
- Experiencing a severe headache caused by spinal fluid leakage. Less than 1% of people experience this side effect.
- Getting an infection from the epidural procedure, such as an epidural abscess, discitis, osteomyelitis or meningitis.
- Having a negative reaction to the medications, such as hot flashes or a rash.
- Experiencing bleeding if a blood vessel is accidentally damaged during the injection, which could cause a hematoma or a blood clot to form.
- Having damage to the nerves at the injection site.
- Temporarily losing control of your bladder and bowels. You might need a catheter (a small tube) in your bladder to help you pee.
Disadvantages and risks that apply to epidural analgesia for labor and delivery specifically include:
- You might lose feeling in your legs for a few hours.
- It might slow down the second stage of labor.
- You might not be able to push and need help to give birth. Your provider may need to use forceps or a vacuum to help deliver your baby.
- Your baby will need to be closely monitored during your labor.
Risks and complications that apply to epidural steroid injections specifically include:
- Experiencing a temporary increase in pain.
- If your provider uses fluoroscopy or a CT scan for imaging guidance, there will be minimal low-level radiation exposure due to the X-rays.
- If you have diabetes, a steroid injection will likely cause high blood sugar (hyperglycemia).
 This could last for several hours or even days.
This could last for several hours or even days.
Can getting an epidural cause back problems?
There’s a common belief that getting an epidural will lead to back pain, but it’s very rare for an epidural to cause long-term or chronic back problems.
It’s normal to experience temporary back pain or tenderness at the site of your epidural. This usually goes away within a few days.
This belief likely stems from the fact that many people who go through childbirth experience back pain after labor and delivery — whether they’ve had an epidural or not. This is because the bones and ligaments in your pelvis are shifting back into their original positions from before your pregnancy, which can cause back pain and discomfort.
Can getting an epidural cause long-term side effects?
While it’s very rare, having an epidural procedure can lead to some long-term complications, including:
- Permanent neurologic deficit due to spinal cord or nerve root damage from the epidural injection.
- Chronic pain due to due to spinal cord or nerve root damage from the epidural injection.
- Permanent paralysis from a hematoma that occurs when there’s a buildup of blood between the dura mater and the spinal cord.
Recovery and Outlook
How long does an epidural last?
How long an epidural lasts depends on what kind of epidural you got and what kind of medicine your healthcare provider injected. Your provider will let you know what to expect. In general, here’s how long certain types of epidurals last:
- Epidural with a catheter: If you have an epidural with a catheter, your provider can give you a continuous flow of anesthetic medicine or multiple separate doses, depending on your situation and pain level. Once your provider has stopped the medication, you’ll likely experience numbness for a few hours before the effect of the medicine begins to wear off. You’ll likely have to rest in a lying or sitting position until you have full feeling in your legs again.
 You may feel a slight tingling sensation while you’re waiting.
You may feel a slight tingling sensation while you’re waiting. - Single-injection epidural: Single injection epidurals usually last a few hours before you begin to regain feeling in the area that was numb.
- Epidural steroid injection: The length of time an epidural steroid injection can provide pain relief varies. Some people experience permanent pain relief if they have a new disk herniation. For people who have chronic pain, epidural steroid injections usually last 3 to 6 months or more.
When can I return to my normal activities after an epidural?
If you’ve had an epidural, do not drive, operate machinery or drink alcohol for at least 24 hours after. Your healthcare provider will give you specific instructions about when you can return to your normal activities depending on your type of epidural and your situation. Be sure to follow them.
When to Call the Doctor
When should I see my healthcare provider?
If you experience any of the following symptoms after you’ve returned home from your epidural procedure, be sure to contact your healthcare provider or go to the nearest hospital as soon as possible:
- Experiencing a severe headache while you’re standing up or sitting that feels better after lying down.
 This could be a sign of a dural puncture.
This could be a sign of a dural puncture. - Having a fever, which could be a sign of an infection.
- Having a reduced or complete loss of bladder or bowel control.
- Feeling numbness and/or weakness in your legs, which could be a sign of nerve injury.
Frequently Asked Questions
What’s the difference between an epidural and a spinal block?
An epidural and a spinal block both provide pain relief through an injection in the area around your spine. The differences are the placement and the effect.
With an epidural, your healthcare provider injects anesthesia into the epidural space around your spinal nerves. With a spinal block, your provider injects the anesthesia into the dural sac around your spinal nerves that contains cerebrospinal fluid. This placement of a spinal block injection means that it gives immediate relief. Epidural injections usually take 20 to 30 minutes before you feel the full effect of pain relief or lack of feeling.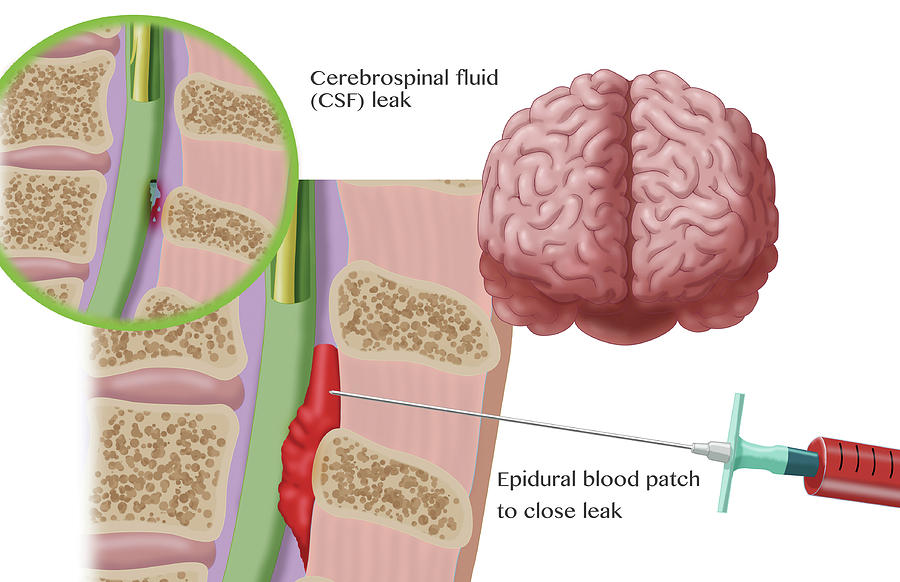
What are the side effects of an epidural after childbirth?
If you get an epidural for labor and childbirth, you may experience the following side effects, which aren’t very common, after delivery:
- Severe headache.
- Temporary difficulty with peeing.
- Temporary difficulty with walking.
- Fever.
You will likely have a small bruise and some tenderness at the site of the epidural after delivery. This should get better in one to two days.
A note from Cleveland Clinic
Epidurals are a common, effective and generally safe procedure to deliver quick pain relief and/or a temporary lack of feeling. If you’re feeling anxious about the possibility of receiving an epidural, don’t be afraid to ask your healthcare provider about it and the procedure. They can answer any questions you may have.
Epidural versus non-epidural or no analgesia for labor pain management
What is the problem?
We set out to evaluate the effectiveness of all types of epidural anesthesia (including combined spinal-epidural anesthesia) for mother and child, compared with non-epidural anesthesia or its absence during childbirth.
Why is this important?
Pain relief is important for women in labour. Pharmacological methods of pain relief include inhaled nitrous oxide, opioid injections, and local analgesia with epidural anesthesia to provide central blockade. Epidural anesthesia is widely used to relieve the pain of childbirth and involves injecting a local anesthetic into the lower back in close proximity to the nerves that transmit pain. Solutions for epidural anesthesia are administered by bolus injection (large, rapid injection), continuous infusion, or using a pump (pump) controlled by the patient. When combined with opiates, lower concentrations of local anesthetic are required, which allows women to maintain the ability to move during childbirth and actively participate in them. Combined spinal-epidural anesthesia involves a single injection of a local anesthetic or opiate into the cerebrospinal fluid for rapid onset of pain relief, and insertion of an epidural catheter for long-term pain relief.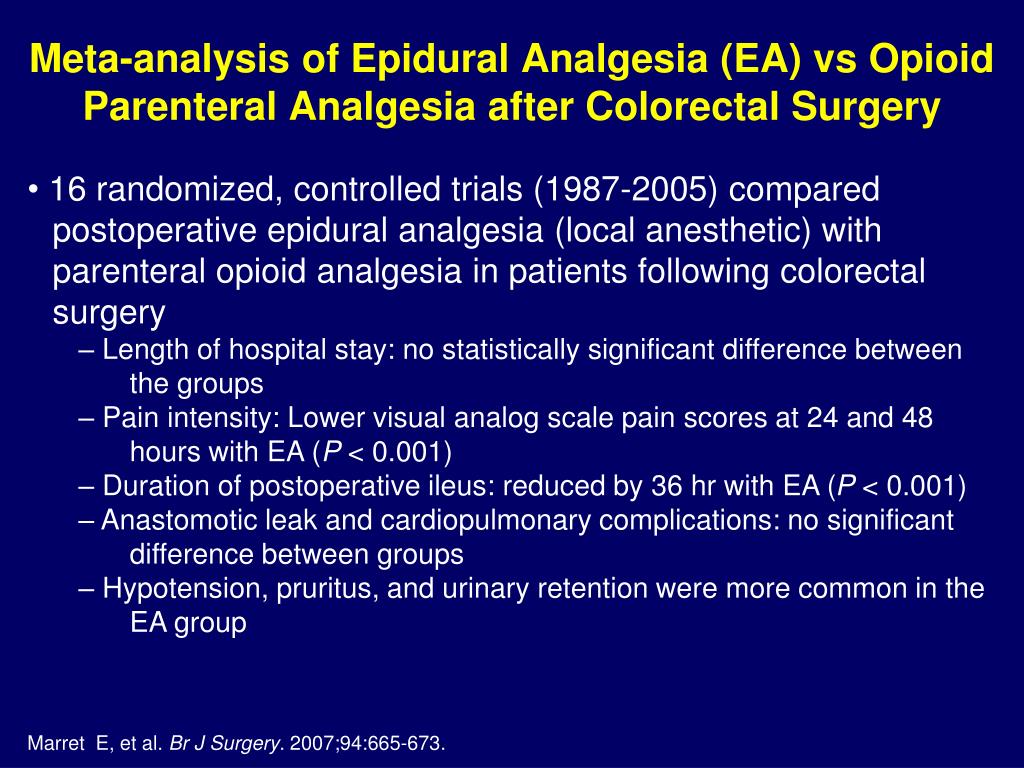 There are reports of side effects such as itching, drowsiness, chills and fever. Rare but potentially serious adverse effects of epidural anesthesia may also occur, such as severe prolonged headache after injection, or nerve damage.
There are reports of side effects such as itching, drowsiness, chills and fever. Rare but potentially serious adverse effects of epidural anesthesia may also occur, such as severe prolonged headache after injection, or nerve damage.
What evidence did we find?
We searched for evidence in April 2017 and identified 40 trials involving over 11,000 women who contributed to this review. Clinical trials have been distinguished by the quality of their methods.
All but six studies compared epidural analgesia with the administration of opioid analgesics. An epidural can relieve labor pain more effectively than opioids, and most women can be satisfied with an epidural. In general, women who have used epidurals are more likely to require forceps or vacuum extraction to assist in labor compared to opioid analgesics. However, we did not see this effect in studies conducted after 2005, which more frequently used lower local anesthetic concentrations and more modern epidural techniques such as patient-controlled epidural analgesia (PCEA).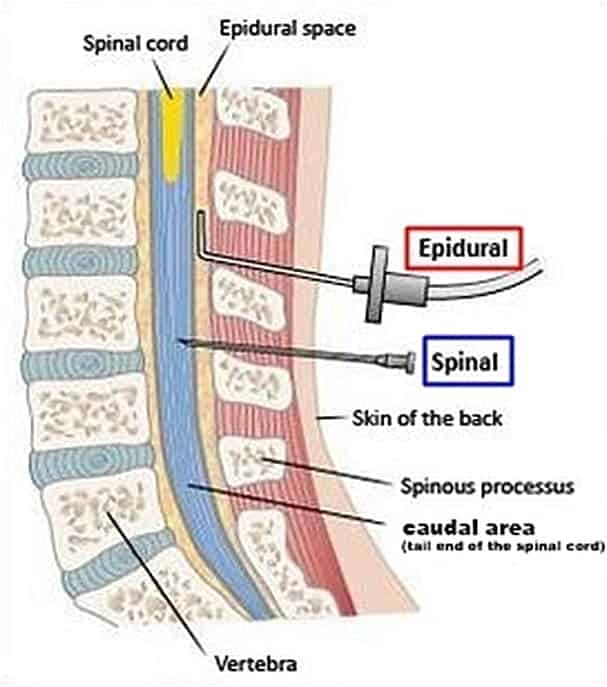 Epidural anesthesia, compared with opioids, may have little or no effect on the rate of caesarean section, prolonged back pain, impact on the baby at birth, or number of infants requiring transfer to the neonatal intensive care unit.
Epidural anesthesia, compared with opioids, may have little or no effect on the rate of caesarean section, prolonged back pain, impact on the baby at birth, or number of infants requiring transfer to the neonatal intensive care unit.
Women who have had an epidural may have trouble urinating and may have a fever. There are highly variable outcomes such as longer labor, very low blood pressure, and inability to move for a period of time after delivery (motor block), likely due to the higher concentration of local anesthetic used in the epidural or due to the use of an epidural. infusions instead of dosed epidural administration of anesthetic at regular intervals. However, women who received opioid analgesics experienced some side effects, such as breathing so slow that they required oxygen masks, and severe nausea and vomiting. More babies whose mothers received opioids received antidotes to counteract the effects of opioids. There was no difference between women who received epidurals or opioid analgesics in terms of postpartum depression, headache, itching, chills, or drowsiness.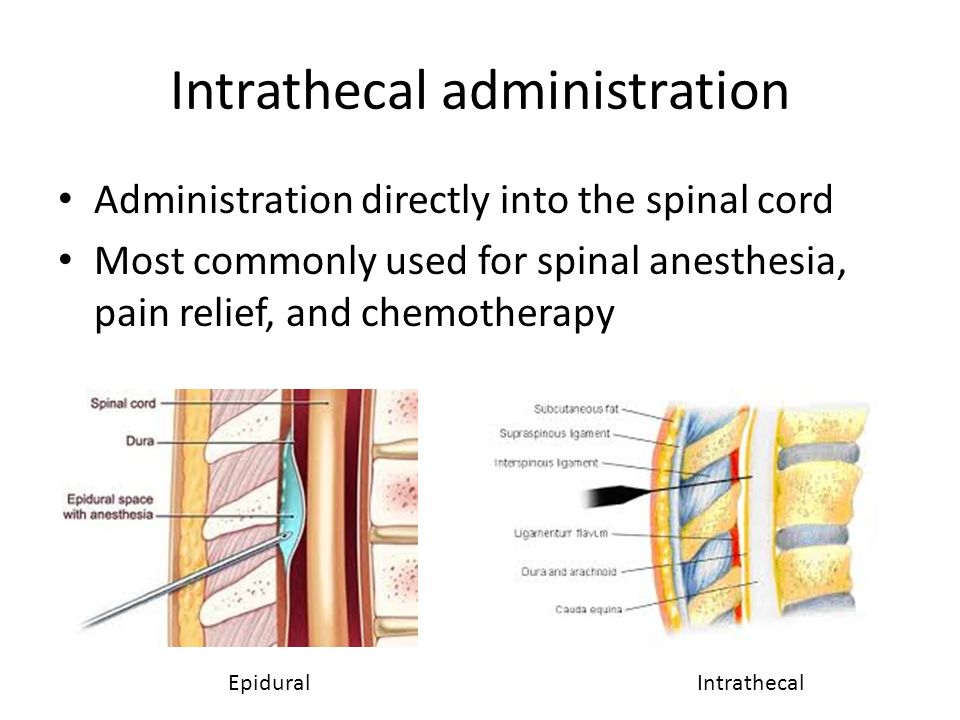
Women who received epidurals reported less pain than women who received placebo or no treatment or acustimulation. There were no reports of pain in trials that compared epidurals with inhaled analgesia or continuous support.
What does this mean?
Epidurals may reduce labor pain more effectively than any other form of pain relief and may increase maternal satisfaction with pain relief. However, some women who received epidurals instead of opioid analgesics were more likely to have assisted vaginal delivery, but this result probably reflects the higher concentrations of local anesthetics used traditionally instead of the low concentrations of modern local anesthetics for epidural anesthesia. Further research will be useful, with more consistent measures to reduce adverse outcomes associated with epidural anesthesia.
Translation notes:
Translation: Tashtanbekova Cholpon Bolotbekovna. Editing: Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University).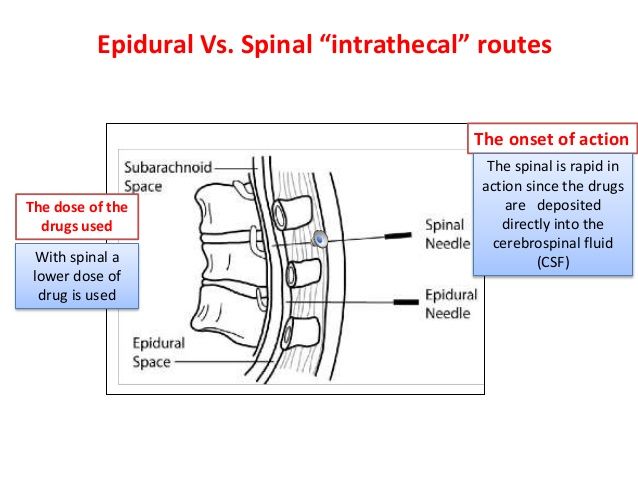 For questions related to this translation, please contact us at: [email protected]; [email protected]
For questions related to this translation, please contact us at: [email protected]; [email protected]
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
You know which doctor you want to book
You know the service you want to book
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.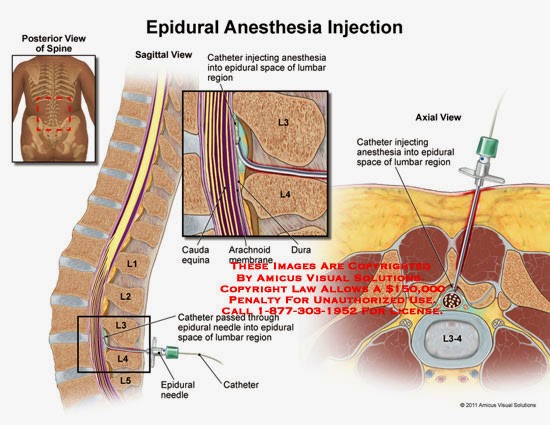
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st.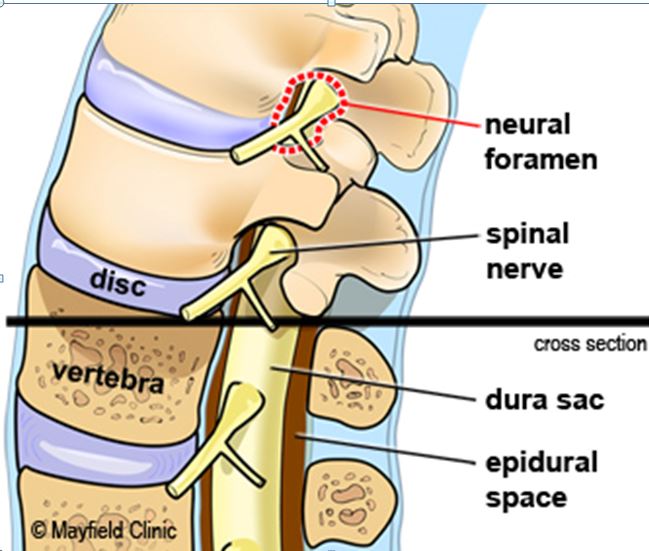 Vikulova, 33, building 2 st. Bolshakova, d. 68
Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022.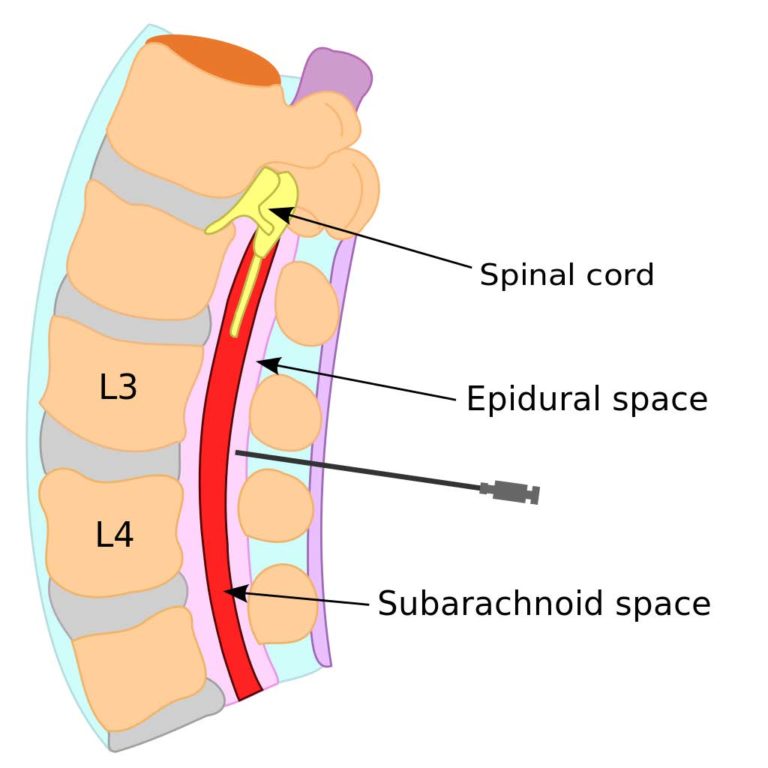 N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia dated July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.