What is an anembryonic pregnancy
Anembryonic Pregnancy - StatPearls - NCBI Bookshelf
Khalid Chaudhry; Dawood Tafti; Marco A. Siccardi.
Author Information and Affiliations
Last Update: September 19, 2022.
Continuing Education Activity
A blighted ovum, also known as an anembryonic pregnancy, occurs when a fertilized egg implants and a gestational (embryonic) sac forms and grows, but the embryo fails to develop. A blighted ovum is the single leading cause of miscarriage. This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
Objectives:
Outline the risk factors for a blighted ovum.
Describe the clinical presentation of a patient with a blighted ovum.
List the treatment and management options available for a patient with a blighted ovum.
Employ interprofessional team strategies for improving care coordination and communication to enhance fertility rates in patients with a history of miscarriage.
Access free multiple choice questions on this topic.
Introduction
An anembryonic pregnancy is characterized by a gestational sac that forms and grows while an embryo fails to develop. Although the terms anembryonic pregnancy and blighted ovum are synonymous, the latter is falling out of favor for the more descriptive former term. Anembryonic pregnancy constitutes a significant but unknown proportion of miscarriages with the American Pregnancy Association estimating anembryonic pregnancy to constitute half of all first trimester miscarriages. Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
In the first trimester, the terms early pregnancy loss, miscarriage, or spontaneous abortion are often used interchangeably.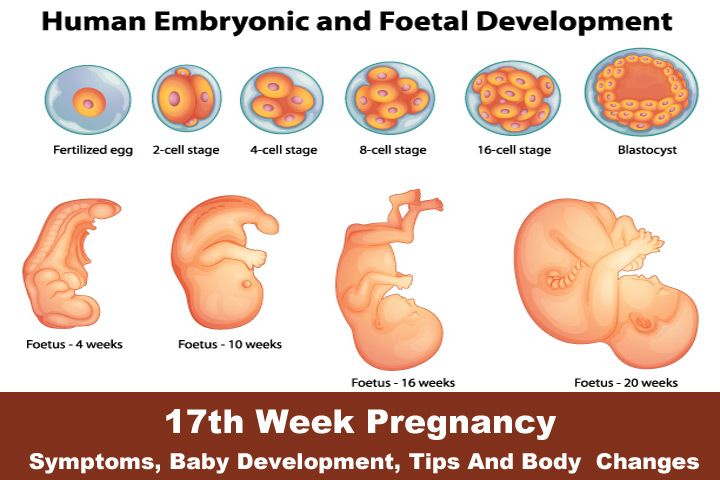 Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
What is a Miscarriage?
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs 500 g or less. This definition is used in the United States; however, it may vary based on State laws.[5]
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification and confirmation.
Clinical miscarriage is when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy. Clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 weeks to 20 weeks).
Etiology
The exact etiology for anembryonic pregnancies is difficult to ascertain. The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
Morphological abnormalities of an embryo that prevents implantation or prevents long term survival of the embryo after implantation. These morphological abnormalities are thought to be related to chromosomal abnormalities. [6]
Chromosomal abnormalities that collectively include autosomal trisomy, polyploidy, sex chromosomal polysomy, and monosomy X likely represent the most common etiologies for EPL. Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.
Other genetic and chromosomal abnormalities include translocations, inversions, single-gene perturbations, and placental mosaicism. [7] Consanguineous marriages resulting in anembryonic pregnancies have also been noted, suggesting a role of single gene determinants. [8] There is a probable link between DNA damage in sperm and miscarriage. [9]]
Obesity and advanced maternal age are well-established factors associated with early pregnancy loss. [10]
Tuberculosis in the developing world as well as reproductive tract infections worldwide can predispose to EPL. [11] The complications of genital tract infections that include intrauterine adhesions can impede implantation and embryo growth.
Malformation of the uterus that includes didelphic, bicornuate, and septate uteri can impede in or prevent the longterm implantation of an embryo.
Immunologic disorders in the mother such as NK Cell Dysfunction, autoantibodies, hereditary, and acquired thrombophilia, among others) can lead to the maternal immunological rejection of the implanting embryo in the uterus resulting in miscarriage.

Hormonal factors (such as low levels of progesterone) and endocrinological disorders(thyroid autoimmunity and thyroid dysfunction) play a complex role in miscarriage. Polycystic ovarian syndrome is also associated with infertility and pregnancy loss.
The role of alcohol consumption and it's associated increased risk in miscarriage has been well established. [12]
Epidemiology
Although difficult to definitively establish, anembryonic pregnancy possibly represents half of all miscarriages in the first trimester of pregnancy. [13][14] The incidence of early pregnancy loss (before 12 weeks) is estimated to be about 15% of clinically evident conceptions with significant variations in incidence based on patient age. The incidence ranges from 10% in women 20 to 24 years of age to 51% in women 40 to 44 years of age. [15] A prior history of early pregnancy loss also predisposes a patient to miscarriage. [16]
History and Physical
The signs and symptoms of an anembryonic pregnancy can potentially mirror those of an ectopic pregnancy.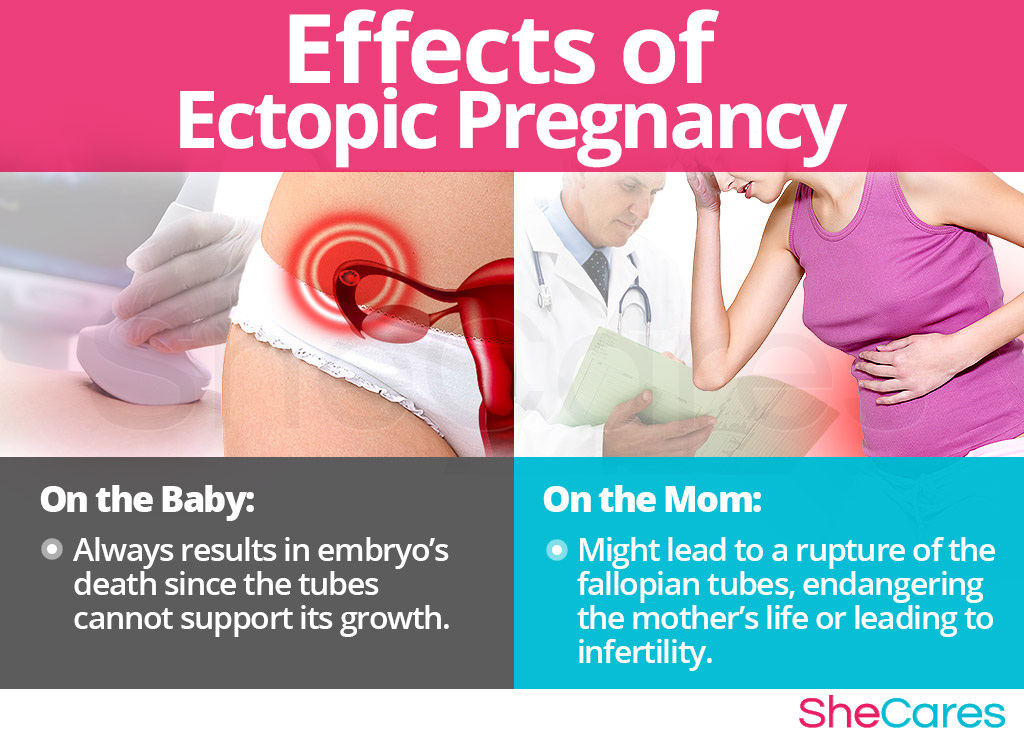 Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Evaluation
Clinical signs and symptoms, a pregnancy test, and an ultrasound exam confirm the diagnosis.
A pregnancy test can be obtained using urine or serum hCG levels.
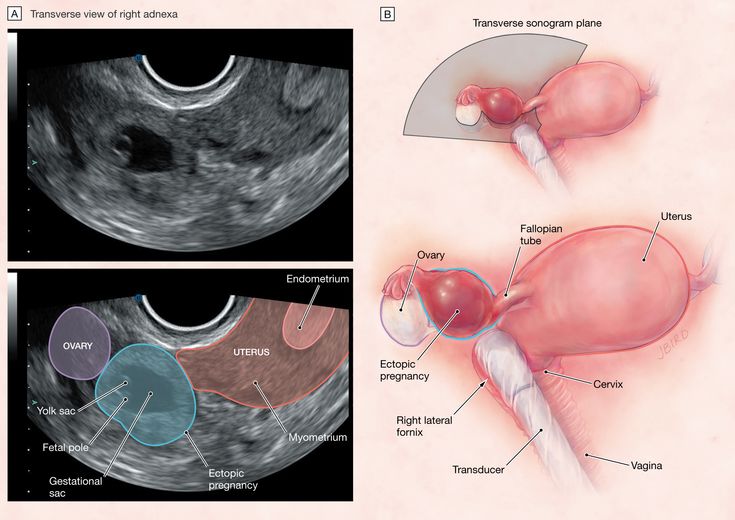
Ultrasound exam (transabdominal or transvaginal) classically demonstrates an empty gestational sac without an embryo.
An anembryonic pregnancy is established on endovaginal ultrasound technique when there is no discernable embryo seen in a gestational sac with a mean sac diameter of ≥25 mm.
Alternatively, an anembryonic pregnancy can be established when there is no embryo on a follow-up endovaginal scan:
≥11 days after a scan demonstrating a gestational sac with a yolk sac, but an absent embryo
≥ 2 weeks (14 days) after a scan demonstrating a gestational sac without an embryo or a yolk sac
Treatment / Management
The three treatment options for early pregnancy loss include expectant management, medical management, and surgical treatment.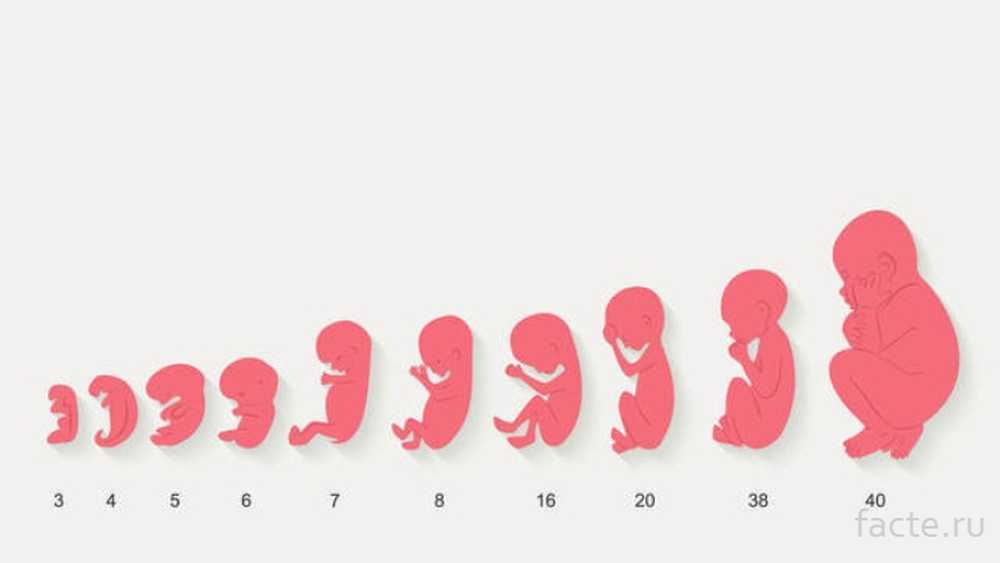 Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Differential Diagnosis
The chief obstetric differential diagnosis for an anembryonic pregnancy includes:
Pseudogestational sac which represents a small amount of intrauterine fluid
Early intrauterine pregnancy
An ectopic pregnancy
Implantation bleeding from an otherwise viable pregnancy
Gestational trophoblastic disease
Complications relating to a viable pregnancy
Prognosis
Prognosis and successful management of early pregnancy loss depends on a variety of factors including gestation age. Prognosis is generally considered good with all three management options.
Expectant management: in a meta-analysis of 20 studies, expectant management and medical management were both determined to be acceptable treatment options for incomplete abortion.
 [17]
[17]Medical management: medical management is more successful with multiple-dose regimens of misoprostol. Patients with incomplete abortion are treated more successfully with medical management than with expectant management.
Surgical Treatment: at least one large randomized control trial determined a higher success rate in surgical treatment than with medical management, with a general conclusion of the general safety of both treatment options. [18]
Complications
Serious complications of treatment are uncommon. Complications can include:
Heavy bleeding/hemorrhage
Uterine perforation(from surgical management)
Infection to include fatal sepsis
Complications from a missed ectopic pregnancy
Consultations
OB/GYN
Primary care provider
Psychologist/psychiatrist
Emergency department physician
Radiologist/sonographer(especially when there is a concern for an ectopic pregnancy)
Deterrence and Patient Education
The following represent key points in patient education:
Patients should be advised to present to their emergency department if they experience heavy vaginal bleeding(two pads per hour for approximately two consecutive hours).

Signs and symptoms of infection should be discussed with patients especially following surgical management.
Treatment with misoprostol can cause a febrile reaction which can be misinterpreted as a sign of infection.
Prophylactic antibiotics are not routinely administered but can be considered in select patients.
Patients should adhere to follow-up sonogram and outpatient appointments especially when additional doses of misoprostol are considered to be clinically necessary.
A miscarriage can be a traumatic experience for a patient. Reassurance and empathy play a key role in helping patients through the grieving process.
Pearls and Other Issues
Pregnancy loss is a common complication in the first trimester of pregnancy
Most losses occur in the first trimester
Early pregnancy loss without embryo development is likely due to chromosomal and genetic abnormalities
There are specific sonographic criteria for determining an anembryonic pregnancy
A pseudogestational sac, an ectopic pregnancy, and an early pregnancy are important differential diagnoses to consider when evaluating an anembryonic pregnancy
Expectant management, medical treatment with misoprostol, and surgical treatment are the three primary options for management
Enhancing Healthcare Team Outcomes
Establishing an anembryonic pregnancy can sometimes b difficult on an ultrasound. Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
References
- 1.
Macklon NS, Geraedts JP, Fauser BC. Conception to ongoing pregnancy: the 'black box' of early pregnancy loss. Hum Reprod Update. 2002 Jul-Aug;8(4):333-43. [PubMed: 12206468]
- 2.
Goldhaber MK, Fireman BH. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology. 1991 Jan;2(1):33-9. [PubMed: 2021664]
- 3.
Serdinšek T, Reljič M, Kovač V. Medical management of first trimester missed miscarriage: the efficacy and complication rate.
 J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]
J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]- 4.
Zeqiri F, Paçarada M, Kongjeli N, Zeqiri V, Kongjeli G. Missed abortion and application of misoprostol. Med Arh. 2010;64(3):151-3. [PubMed: 20645507]
- 5.
Yin Y, Zhang T, Dai Y, Bao Y, Chen X, Lu X. The effect of plasma lead on anembryonic pregnancy. Ann N Y Acad Sci. 2008 Oct;1140:184-9. [PubMed: 18991916]
- 6.
Hertig AT, Rock J. Searching for early fertilized human ova. Gynecol Invest. 1973;4(3):121-39. [PubMed: 4593973]
- 7.
Berglund G. Preparation of antiserum to an antigen of low molecular weight. Nature. 1965 May 01;206(983):523-4. [PubMed: 4953500]
- 8.
Shekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. Int J Mol Cell Med. 2013 Fall;2(4):164-8. [PMC free article: PMC3927383] [PubMed: 24551808]
- 9.
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012 Oct;27(10):2908-17. [PubMed: 22791753]
- 10.
Cavalcante MB, Sarno M, Peixoto AB, Araujo Júnior E, Barini R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. J Obstet Gynaecol Res. 2019 Jan;45(1):30-38. [PubMed: 30156037]
- 11.
Patki A, Chauhan N. An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India. J Obstet Gynaecol India. 2016 Oct;66(5):310-5. [PMC free article: PMC4958068] [PubMed: 27486274]
- 12.
Sundermann AC, Zhao S, Young CL, Lam L, Jones SH, Velez Edwards DR, Hartmann KE. Alcohol Use in Pregnancy and Miscarriage: A Systematic Review and Meta-Analysis. Alcohol Clin Exp Res. 2019 Aug;43(8):1606-1616. [PMC free article: PMC6677630] [PubMed: 31194258]
- 13.
Andersen LB, Dechend R, Karumanchi SA, Nielsen J, Joergensen JS, Jensen TK, Christesen HT. Early pregnancy angiogenic markers and spontaneous abortion: an Odense Child Cohort study. Am J Obstet Gynecol. 2016 Nov;215(5):594.e1-594.e11. [PubMed: 27287686]
- 14.
Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertil Steril. 2000 Feb;73(2):270-4. [PubMed: 10685527]
- 15.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019 Mar 20;364:l869. [PMC free article: PMC6425455] [PubMed: 30894356]
- 16.
Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. BMJ. 1989 Aug 26;299(6698):541-5. [PMC free article: PMC1837397] [PubMed: 2507063]
- 17.
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L.
 Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]
Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]- 18.
Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM., National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005 Aug 25;353(8):761-9. [PubMed: 16120856]
Anembryonic Pregnancy - StatPearls - NCBI Bookshelf
Khalid Chaudhry; Dawood Tafti; Marco A. Siccardi.
Author Information and Affiliations
Last Update: September 19, 2022.
Continuing Education Activity
A blighted ovum, also known as an anembryonic pregnancy, occurs when a fertilized egg implants and a gestational (embryonic) sac forms and grows, but the embryo fails to develop. A blighted ovum is the single leading cause of miscarriage.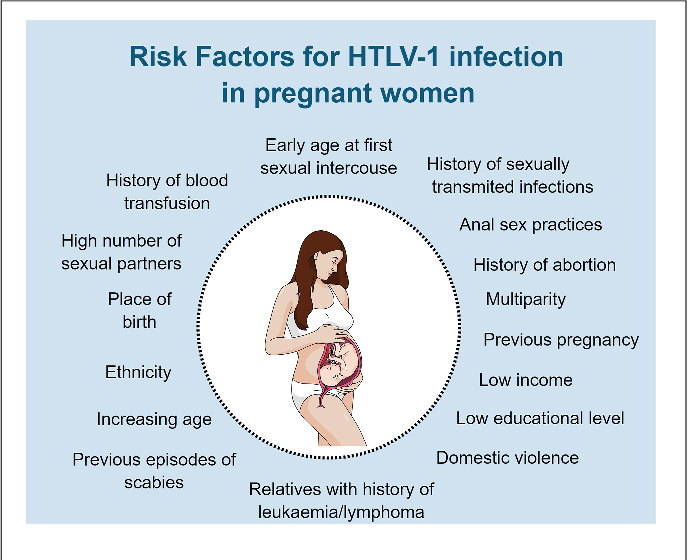 This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
This activity outlines the management of blighted ovum and highlights the role of the interprofessional team in educating the patient on this condition.
Objectives:
Outline the risk factors for a blighted ovum.
Describe the clinical presentation of a patient with a blighted ovum.
List the treatment and management options available for a patient with a blighted ovum.
Employ interprofessional team strategies for improving care coordination and communication to enhance fertility rates in patients with a history of miscarriage.
Access free multiple choice questions on this topic.
Introduction
An anembryonic pregnancy is characterized by a gestational sac that forms and grows while an embryo fails to develop. Although the terms anembryonic pregnancy and blighted ovum are synonymous, the latter is falling out of favor for the more descriptive former term. Anembryonic pregnancy constitutes a significant but unknown proportion of miscarriages with the American Pregnancy Association estimating anembryonic pregnancy to constitute half of all first trimester miscarriages. Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
Approximately 15% of all clinically recognized pregnancies end in first-trimester loss with live birth occurring in only 30% of all pregnancies. [1][2] A significant proportion of patients with early pregnancy loss(that include anembryonic pregnancies) are unaware of their miscarriage particularly when early pregnancy loss occurs in the early stages of pregnancy.
In the first trimester, the terms early pregnancy loss, miscarriage, or spontaneous abortion are often used interchangeably. Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
What is a Miscarriage?
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs 500 g or less. This definition is used in the United States; however, it may vary based on State laws.[5]
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification and confirmation.
Clinical miscarriage is when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy. Clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 weeks to 20 weeks).
Etiology
The exact etiology for anembryonic pregnancies is difficult to ascertain. The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL) which includes both embryonic and anembryonic pregnancies. Etiologies include:
Morphological abnormalities of an embryo that prevents implantation or prevents long term survival of the embryo after implantation. These morphological abnormalities are thought to be related to chromosomal abnormalities. [6]
Chromosomal abnormalities that collectively include autosomal trisomy, polyploidy, sex chromosomal polysomy, and monosomy X likely represent the most common etiologies for EPL.
 Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.
Trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 was found to give rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise. Other genetic and chromosomal abnormalities include translocations, inversions, single-gene perturbations, and placental mosaicism. [7] Consanguineous marriages resulting in anembryonic pregnancies have also been noted, suggesting a role of single gene determinants. [8] There is a probable link between DNA damage in sperm and miscarriage. [9]]
Obesity and advanced maternal age are well-established factors associated with early pregnancy loss.
 [10]
[10] Tuberculosis in the developing world as well as reproductive tract infections worldwide can predispose to EPL. [11] The complications of genital tract infections that include intrauterine adhesions can impede implantation and embryo growth.
Malformation of the uterus that includes didelphic, bicornuate, and septate uteri can impede in or prevent the longterm implantation of an embryo.
Immunologic disorders in the mother such as NK Cell Dysfunction, autoantibodies, hereditary, and acquired thrombophilia, among others) can lead to the maternal immunological rejection of the implanting embryo in the uterus resulting in miscarriage.
Hormonal factors (such as low levels of progesterone) and endocrinological disorders(thyroid autoimmunity and thyroid dysfunction) play a complex role in miscarriage. Polycystic ovarian syndrome is also associated with infertility and pregnancy loss.
The role of alcohol consumption and it's associated increased risk in miscarriage has been well established.
 [12]
[12]
Epidemiology
Although difficult to definitively establish, anembryonic pregnancy possibly represents half of all miscarriages in the first trimester of pregnancy. [13][14] The incidence of early pregnancy loss (before 12 weeks) is estimated to be about 15% of clinically evident conceptions with significant variations in incidence based on patient age. The incidence ranges from 10% in women 20 to 24 years of age to 51% in women 40 to 44 years of age. [15] A prior history of early pregnancy loss also predisposes a patient to miscarriage. [16]
History and Physical
The signs and symptoms of an anembryonic pregnancy can potentially mirror those of an ectopic pregnancy. Anembryonic pregnancy is often incidentally noted on an initial first-trimester pregnancy sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Evaluation
Clinical signs and symptoms, a pregnancy test, and an ultrasound exam confirm the diagnosis.
A pregnancy test can be obtained using urine or serum hCG levels.
Ultrasound exam (transabdominal or transvaginal) classically demonstrates an empty gestational sac without an embryo.
An anembryonic pregnancy is established on endovaginal ultrasound technique when there is no discernable embryo seen in a gestational sac with a mean sac diameter of ≥25 mm.
Alternatively, an anembryonic pregnancy can be established when there is no embryo on a follow-up endovaginal scan:
≥11 days after a scan demonstrating a gestational sac with a yolk sac, but an absent embryo
≥ 2 weeks (14 days) after a scan demonstrating a gestational sac without an embryo or a yolk sac
Treatment / Management
The three treatment options for early pregnancy loss include expectant management, medical management, and surgical treatment. Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Medical management with misoprostol and surgical treatment is considered more effective in the management of anembryonic pregnancy. Ultimately the decision on considering one of these options is based on an informed conversation between a patient and the provider.
Differential Diagnosis
The chief obstetric differential diagnosis for an anembryonic pregnancy includes:
Pseudogestational sac which represents a small amount of intrauterine fluid
Early intrauterine pregnancy
An ectopic pregnancy
Implantation bleeding from an otherwise viable pregnancy
Gestational trophoblastic disease
Complications relating to a viable pregnancy
Prognosis
Prognosis and successful management of early pregnancy loss depends on a variety of factors including gestation age. Prognosis is generally considered good with all three management options.
Expectant management: in a meta-analysis of 20 studies, expectant management and medical management were both determined to be acceptable treatment options for incomplete abortion.
 [17]
[17]Medical management: medical management is more successful with multiple-dose regimens of misoprostol. Patients with incomplete abortion are treated more successfully with medical management than with expectant management.
Surgical Treatment: at least one large randomized control trial determined a higher success rate in surgical treatment than with medical management, with a general conclusion of the general safety of both treatment options. [18]
Complications
Serious complications of treatment are uncommon. Complications can include:
Heavy bleeding/hemorrhage
Uterine perforation(from surgical management)
Infection to include fatal sepsis
Complications from a missed ectopic pregnancy
Consultations
OB/GYN
Primary care provider
Psychologist/psychiatrist
Emergency department physician
Radiologist/sonographer(especially when there is a concern for an ectopic pregnancy)
Deterrence and Patient Education
The following represent key points in patient education:
Patients should be advised to present to their emergency department if they experience heavy vaginal bleeding(two pads per hour for approximately two consecutive hours).

Signs and symptoms of infection should be discussed with patients especially following surgical management.
Treatment with misoprostol can cause a febrile reaction which can be misinterpreted as a sign of infection.
Prophylactic antibiotics are not routinely administered but can be considered in select patients.
Patients should adhere to follow-up sonogram and outpatient appointments especially when additional doses of misoprostol are considered to be clinically necessary.
A miscarriage can be a traumatic experience for a patient. Reassurance and empathy play a key role in helping patients through the grieving process.
Pearls and Other Issues
Pregnancy loss is a common complication in the first trimester of pregnancy
Most losses occur in the first trimester
Early pregnancy loss without embryo development is likely due to chromosomal and genetic abnormalities
There are specific sonographic criteria for determining an anembryonic pregnancy
A pseudogestational sac, an ectopic pregnancy, and an early pregnancy are important differential diagnoses to consider when evaluating an anembryonic pregnancy
Expectant management, medical treatment with misoprostol, and surgical treatment are the three primary options for management
Enhancing Healthcare Team Outcomes
Establishing an anembryonic pregnancy can sometimes b difficult on an ultrasound. Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Communication with the radiologist relaying hCG lab values and patient presentation can be helpful in avoiding a missed diagnosis of an ectopic pregnancy. The sonographer also plays an important role in accurately evaluating a patient to appropriately exclude an ectopic pregnancy. Patients presenting with complications of either initial presentation or from treatment often present to the emergency department. Interprofessional communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough history and physical exam. This especially includes signs of sepsis or hemodynamic instability. The role of a mental health professional in following up with patients is also critical in ensuring the appropriate mental health management of a possibly traumatic experience for a patient.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD
Figure
Single sonographic image demonstrating a gestational sac with a yolk sac. No fetal pole is seen. This is representative of a blighted ovum. Contributed by Dr.Dawood Tafti, MD.
References
- 1.
Macklon NS, Geraedts JP, Fauser BC. Conception to ongoing pregnancy: the 'black box' of early pregnancy loss. Hum Reprod Update. 2002 Jul-Aug;8(4):333-43. [PubMed: 12206468]
- 2.
Goldhaber MK, Fireman BH. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology. 1991 Jan;2(1):33-9. [PubMed: 2021664]
- 3.
Serdinšek T, Reljič M, Kovač V. Medical management of first trimester missed miscarriage: the efficacy and complication rate.
 J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]
J Obstet Gynaecol. 2019 Jul;39(5):647-651. [PubMed: 30917727]- 4.
Zeqiri F, Paçarada M, Kongjeli N, Zeqiri V, Kongjeli G. Missed abortion and application of misoprostol. Med Arh. 2010;64(3):151-3. [PubMed: 20645507]
- 5.
Yin Y, Zhang T, Dai Y, Bao Y, Chen X, Lu X. The effect of plasma lead on anembryonic pregnancy. Ann N Y Acad Sci. 2008 Oct;1140:184-9. [PubMed: 18991916]
- 6.
Hertig AT, Rock J. Searching for early fertilized human ova. Gynecol Invest. 1973;4(3):121-39. [PubMed: 4593973]
- 7.
Berglund G. Preparation of antiserum to an antigen of low molecular weight. Nature. 1965 May 01;206(983):523-4. [PubMed: 4953500]
- 8.
Shekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. Int J Mol Cell Med. 2013 Fall;2(4):164-8. [PMC free article: PMC3927383] [PubMed: 24551808]
- 9.

Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012 Oct;27(10):2908-17. [PubMed: 22791753]
- 10.
Cavalcante MB, Sarno M, Peixoto AB, Araujo Júnior E, Barini R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. J Obstet Gynaecol Res. 2019 Jan;45(1):30-38. [PubMed: 30156037]
- 11.
Patki A, Chauhan N. An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India. J Obstet Gynaecol India. 2016 Oct;66(5):310-5. [PMC free article: PMC4958068] [PubMed: 27486274]
- 12.
Sundermann AC, Zhao S, Young CL, Lam L, Jones SH, Velez Edwards DR, Hartmann KE. Alcohol Use in Pregnancy and Miscarriage: A Systematic Review and Meta-Analysis. Alcohol Clin Exp Res. 2019 Aug;43(8):1606-1616. [PMC free article: PMC6677630] [PubMed: 31194258]
- 13.
Andersen LB, Dechend R, Karumanchi SA, Nielsen J, Joergensen JS, Jensen TK, Christesen HT. Early pregnancy angiogenic markers and spontaneous abortion: an Odense Child Cohort study. Am J Obstet Gynecol. 2016 Nov;215(5):594.e1-594.e11. [PubMed: 27287686]
- 14.
Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertil Steril. 2000 Feb;73(2):270-4. [PubMed: 10685527]
- 15.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019 Mar 20;364:l869. [PMC free article: PMC6425455] [PubMed: 30894356]
- 16.
Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. BMJ. 1989 Aug 26;299(6698):541-5. [PMC free article: PMC1837397] [PubMed: 2507063]
- 17.
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L.
 Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]
Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223. [PMC free article: PMC6464743] [PubMed: 28138973]- 18.
Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM., National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005 Aug 25;353(8):761-9. [PubMed: 16120856]
Anembryony - causes, symptoms | Diamed
Anembryony is a pathology of pregnancy, also known as "premature miscarriage" or "missed pregnancy". This type of miscarriage is one of the most common due to the difficulty of detection. In 60% of cases, this pathology can manifest itself for years without causing discomfort to a woman, especially if during this period of time the woman does not plan pregnancy and does not contact an obstetrician-gynecologist on this issue. Women suffering from disorders of the regularity of the menstrual cycle are more susceptible to this pathology. nine0003
Women suffering from disorders of the regularity of the menstrual cycle are more susceptible to this pathology. nine0003
Anembryony is a type of abnormal pregnancy in which conception occurs but the embryo does not develop.
Obstetrics, as a science, cannot always answer questions about the causes of this pathology. With anembryony, an empty fetal egg is diagnosed. That is, conception occurs, but the embryo in the early stages stops developing and dies for some reason, and ultrasound diagnostics give the impression of the absence of an embryo due to its small size. Most often, this pathology develops between the 5th and 9thth week of pregnancy.
If after this period the pregnancy is not interrupted and the embryo continues to develop, this pathology can no longer develop. If a woman did not go to the doctor or did not detect pregnancy in a timely manner, then in the event of the development of anembryonia, the embryo that stopped developing and died, along with the fetal egg, will leave the uterus naturally during the next menstrual bleeding, without causing inconvenience or discomfort to the woman. Anembryony, regardless of detection, leads to the independent exit of a dead embryo from the body of a woman and does not provoke inflammatory or infectious processes. nine0003
Anembryony, regardless of detection, leads to the independent exit of a dead embryo from the body of a woman and does not provoke inflammatory or infectious processes. nine0003
There is only one way to diagnose this pathology - ultrasound examination of the pelvic organs. If an ultrasound scan detects an empty fetal egg or the absence of embryo development, anembryonia is diagnosed.
Reasons for the development of anembronia
Obstetrics at this stage of development can not always establish the causes of the development of pathology, the most common are:
- Pathology at the genetic level. Currently considered the main cause of anembryos. The pathology of the female or male genetic material (eggs or sperm, respectively) causes anembryony. Even if the genetic material of one of the parents is normal, the pathogenic cell of the second will provoke a stop in the development of the embryo. Thus, in the treatment of this type of miscarriage, both partners should be diagnosed.
 nine0020
nine0020 - Virus, infection, inflammation. Bacterial or viral infection, as well as an inflammatory process in any part of the female body, can stop the development of the embryo. Colds, dental diseases, inflammation of the genital organs, etc. promote the spread of pathogenic bacteria throughout the body. With reduced immunity, the risk of infection and subsequent death of the embryo increases.
- External factors. Ecological conditions, clean air, background radiation and other external factors can also cause anembryony. nine0020
- Hormonal causes. Any disturbances and malfunctions in the work of the endocrine system trigger the mechanisms of destruction of the embryo. If the mother does not suffer from endocrinological disorders, but the father has a hormonal imbalance, fetal death occurs due to sperm pathologies.
Prevention of anembronia
Prevention of pathology consists primarily in a woman's attentive attitude to her health and monitoring changes in her state of health and condition. Since anembryony develops in the earliest stages of pregnancy, in some cases, women will find out that they were pregnant after the death of the fetus or not at all. Such latent miscarriage is fraught with aggravation of the situation in the future, since it is impossible to cure a pathology that has not been detected. nine0003
Since anembryony develops in the earliest stages of pregnancy, in some cases, women will find out that they were pregnant after the death of the fetus or not at all. Such latent miscarriage is fraught with aggravation of the situation in the future, since it is impossible to cure a pathology that has not been detected. nine0003
The main prevention tip is early detection of pregnancy through a blood test, ultrasound or rapid test. If pregnancy is detected, you should immediately register and undergo a full diagnosis. Only a comprehensive study of the mother's health can prevent the development of most pregnancy pathologies in a timely manner.
Unfortunately, if the cause is the genetic material of one or both parents, it is impossible to avoid the death of the embryo even with early detection of pregnancy. However, having fixed this diagnosis, it is possible to carry out treatment, subsequent preparation for pregnancy and, as a result, a normal course of pregnancy without complications. nine0003
nine0003
Come to "Diamed", they will definitely help you!
Anembryony. What is Anembryony?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Anembryony is a type of missed pregnancy in which, after fertilization and implantation, the egg does not develop into an embryo, but an empty fetal egg remains. Pregnancy does not progress, therefore, signs of toxicosis and other early symptoms in the form of drowsiness, pain in the mammary glands, and mood swings gradually disappear. Anembryonia is diagnosed by the results of ultrasound of the pelvic organs at the 5th week of pregnancy, can be confirmed by blood tests for hCG, alpha-fetoprotein. Specific treatment consists in removing the remnants of the embryo medically or with the help of vacuum aspiration. nine0003
nine0003
ICD-10
O02.0 Dead gestational sac and non-vesical mole
- Anembryonic causes
- Pathogenesis
- Classification
- Anembryonic symptoms
- Complications
- Diagnostics
- Treatment of anembryonia
- Medical treatment
- Surgical treatment
- Rehabilitation
- Prognosis and prevention
- Treatment prices
General
Anembryony, or non-vesical drift, may be the result of the initial absence of the embryo in the uterine cavity or its death in up to 5 weeks. In women with a diagnosed pregnancy, on average, one in five ends in spontaneous abortion or stops development. Self-emptying of the uterine cavity occurs in 53% within 2 weeks after diagnosed anembryony. If the remnants of the fetal egg are not removed during this period, then 2.5% experience bleeding or infectious and inflammatory complications that require curettage and subsequent treatment. A fertilized egg with anembryony can linger in the uterus for more than 2 weeks, however, symptoms appear that require surgical care. nine0003
A fertilized egg with anembryony can linger in the uterus for more than 2 weeks, however, symptoms appear that require surgical care. nine0003
Anembryony
Anembryonic causes
The exact causes of this pathology are difficult to establish, they are assumed retrospectively based on additional symptoms and examination of the woman. The cause of anembryony can be maternal diseases, as well as the action of various external and internal pathological factors. The main risk of pregnancy loss occurs at a short time, when the first division of blastomeres occurs, the implantation of the embryo into the uterine mucosa. The causes of anembryony may include the following disorders: nine0003

Anembryony is associated with the death of the embryo and a violation of the inertia of the uterus, which leads to a delay in the cavity of an empty fetal egg. The main causes of myometrial unresponsiveness are as follows:
The main causes of myometrial unresponsiveness are as follows:
- Tight attachment of the embryo. Deep invasion of chorionic villi occurs with structural and functional inferiority of the endometrium. Another reason is the incomplete pregravid transformation in the implantation zone and the high proliferative activity of chorionic villi.
- Immune deficiency. The tissues of the embryo are half alien to the mother's body, therefore, normally, with the participation of progesterone, suppression of immune rejection reactions occurs. The reasons for the preservation of the fetal egg during anembryony are associated with the immunological unreactivity of the myometrium to the products of conception. nine0020
- Impaired contractile function. Rejection of an empty egg does not occur in chronic inflammatory diseases of the uterus due to impaired formation of receptors for uterotonic substances. A common cause is biochemical metabolic defects in the tissues of the uterus.
- Folate deficiency. Folic acid is involved in the division of DNA in cells. With its deficiency in the early stages of pregnancy, there is a violation of the divergence of chromosomes, their incorrect arrangement. Also, with a lack of folate, sensitivity to radiation exposure increases. nine0020
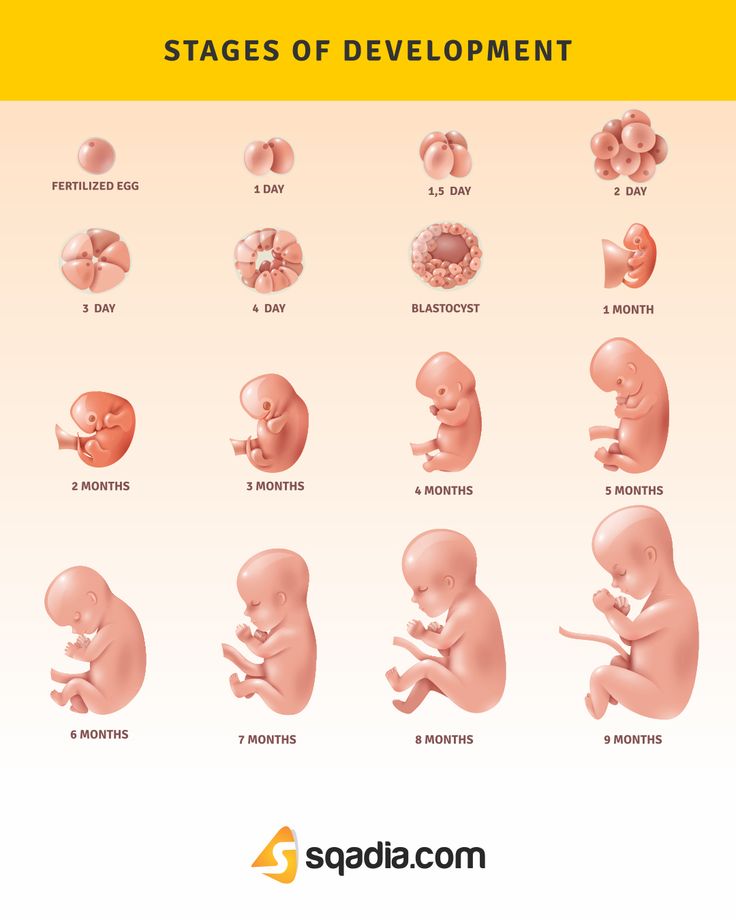
Pathogenesis
On the 7-8th day after fertilization, the embryo implants into the uterine wall, the trophoblast actively produces hCG, which is necessary to maintain pregnancy. By the 3rd week of development, extraembryonic organs are formed in the embryo - the chorion, the yolk sac and the amnion. A little later, the heart begins to beat, but with the help of an ultrasound machine, this can be seen after the 5th week of gestation. If there is a violation of blood flow at the site of implantation, the embryo dies and is gradually reduced. But the fetal vesicle continues to be visualized under the influence of the remaining plume of high pregnancy hormones. In case of violation of uterine contractility, its rejection and expulsion does not occur. nine0003
In case of violation of uterine contractility, its rejection and expulsion does not occur. nine0003
Morphological examination of the endometrium after curettage in anembryonic shows that the decidual layer of cells is dystrophically changed. It often reveals lymphoid infiltration, focal edema of the stroma, dilated glands with flattened epithelial cells. Chorionic villi increase, the epithelium lining them becomes thinner and is located in one layer of synciotrophoblast. Cytotrophoblast is absent in places.
Classification
Anembryony is classified according to the results of an ultrasound examination, which allows you to determine the size of the fetal egg and its contents. The size of the uterus does not affect the type of anembryony, but is taken into account when determining the gestational age. There are two types of the absence of an embryo: nine0003
- 1 typ. The average diameter of the fetal egg is 2-2.5 cm, the embryo is not visualized.
 The size of the uterus corresponds to the 5-7th week of pregnancy, which does not correspond to the period on the first day of the last menstruation. Under dynamic observation, there is no increase in size.
The size of the uterus corresponds to the 5-7th week of pregnancy, which does not correspond to the period on the first day of the last menstruation. Under dynamic observation, there is no increase in size. - 2 typ. The fertilized egg continues to grow, but there is no embryo. Sometimes its remnants are observed in the form of a thin hyperechoic strip. Anembryony of this type can last up to 11 weeks, the egg reaches a size of 4.5-5 cm. nine0033
- Gynecological examination. It is not always possible to notice signs of pathology, sometimes with a two-handed examination, a lag in the size of the uterus, its softening, can be determined. The accession of inflammation is characterized by the appearance of serous-sanitary secretions from the cervix.
- Laboratory studies. HCG in the blood falls 6-8 times lower than normal for gestational age.
 Alpha-fetoprotein increases by 1.5 times or more, but is not a sign of only anembryony, similar changes occur during missed pregnancy. The trophoblastic glycoprotein decreases by 6-18 times, which indicates the death of syncytiotrophoblast cells. The concentration of progesterone may remain at the same level, and estrogens decrease. nine0020
Alpha-fetoprotein increases by 1.5 times or more, but is not a sign of only anembryony, similar changes occur during missed pregnancy. The trophoblastic glycoprotein decreases by 6-18 times, which indicates the death of syncytiotrophoblast cells. The concentration of progesterone may remain at the same level, and estrogens decrease. nine0020 - Instrumental methods. Informative ultrasound with a vaginal probe. Signs of anembryony are a fetal egg of 25 mm or more and the absence of an embryo in it. If after 2 weeks a second ultrasound does not detect a heartbeat, then anembryony is diagnosed.
- Undeveloped pregnancy. Guidelines for MARS (Interdisciplinary Association of Reproductive Medicine Specialists)//StatusPraesens. – 2015.
- Folate cycle and C6777T MTHFR polymorphism – the key to understanding the causes of anembryony/ Veropotvelyan N.P., Kodunov L.O., Pogulyai Yu.S. // Women's health. - 2014 - No. 10 (96).
- Morphological criteria for pathogenetic variants of unspecified abortions / Fedorina T.

Anembryonic symptoms
With a normally developing pregnancy, by 5-6 weeks there are many signs of gestation: symptoms of toxicosis, engorgement of the mammary glands, drowsiness or insomnia, mood swings. During the formation of anembryony, a pregnant woman may notice that at some point she began to feel better, morning sickness disappeared, there is no aversion to odors and hypersalivation. Normal appetite is restored. Then the mammary glands lose soreness and hypersensitivity, become soft. But these signs may not always indicate anembryony. The same symptoms are typical for a missed pregnancy. nine0003
The same symptoms are typical for a missed pregnancy. nine0003
Complications
Women who do not turn to the gynecologist in a timely manner with signs of pregnancy or their disappearance may face serious complications. When an empty fetal vesicle remains in the uterus for up to 2 weeks or more, an inflammatory reaction occurs, symptoms of acute endometritis appear. The temperature rises, serous-mucous discharge appears from the vagina, signs of intoxication are disturbing - weakness, headache. In the absence of treatment or untimely onset, acute inflammation can move to the muscle layer, periuterine tissue, and in severe cases lead to peritonitis. If treatment is not carried out, chronic endometritis develops. nine0003
A sign of rejection of the remains of the embryo from the uterus is the appearance of bloody discharge from the genital tract. But with insufficient contractility of the uterus, violations of hemostasis, bleeding develops. It cannot end on its own, so medical attention is required. The consequence of bleeding is infection of the uterine cavity, anemia. Anembryony is complicated by subsequent habitual miscarriage, secondary infertility.
It cannot end on its own, so medical attention is required. The consequence of bleeding is infection of the uterine cavity, anemia. Anembryony is complicated by subsequent habitual miscarriage, secondary infertility.
Diagnosis
Examination and choice of method of treatment for anembryonia is carried out by an obstetrician-gynecologist. Physical examination does not provide accurate information about the pathology, laboratory methods are also non-specific. The most accurate data can be obtained with vaginal ultrasound of the small pelvis. The survey algorithm includes: nine0003
For a correct assessment of the results, ultrasound is carried out in dynamics. If the fetus does not have a heartbeat at 5 weeks, it cannot be unequivocally said that anembryony has been determined. The absence of a yolk sac is an unfavorable prognostic sign that is consistent with a possible anembryonic pregnancy. nine0003
Anembryonic treatment
Treatment is aimed at evacuating the remains of the fetal egg from the uterine cavity. This can be done medically and surgically. The latter is used more often, but it is associated with an additional risk of infection and complications. WHO recommends medical abortion as the primary treatment for anembryonia.
This can be done medically and surgically. The latter is used more often, but it is associated with an additional risk of infection and complications. WHO recommends medical abortion as the primary treatment for anembryonia.
Medical treatment
Medical interruption of gestation is carried out with symptoms of anembryonia up to 83 days of pregnancy. Mifepristone and misoprostol are used sequentially for the procedure. The dosage of the latter is selected individually and depends on the gestational age for the last menstruation. Bleeding, which means the release of the remains of the embryo, occurs on the second day. A woman should come to the appointment 14 days after taking the last pill to assess the general condition and effectiveness of the procedure. nine0003
Medical abortion has few contraindications. It can be used for infections of the genital tract without prior sanitation. The method is not recommended for bronchial asthma, the presence of pathologies of the cardiovascular system, blood clotting disorders and in women who smoke. Complications of medical abortion may include pain, bleeding, and incomplete abortion, which will require the use of surgical methods.
Complications of medical abortion may include pain, bleeding, and incomplete abortion, which will require the use of surgical methods.
Surgical treatment
Vacuum aspiration is considered the best and least traumatic method among surgical methods. With anembryony, it can be used up to 12 weeks of pregnancy, because. the fertilized egg remains small. Before the procedure, it is necessary to examine the smear for the degree of purity of the vagina. With signs of inflammation, sanitation is carried out with local means. Vacuum aspiration is performed on an outpatient basis, hospitalization in the gynecology department is not required. After the procedure, there is a possibility of infectious complications, bleeding and preservation of the remains of embryonic tissues, which may require curettage. nine0003
For curettage of the uterine cavity, a woman is hospitalized in the gynecological department after a preliminary examination. The procedure is performed under general anesthesia and requires medical supervision for several days after it.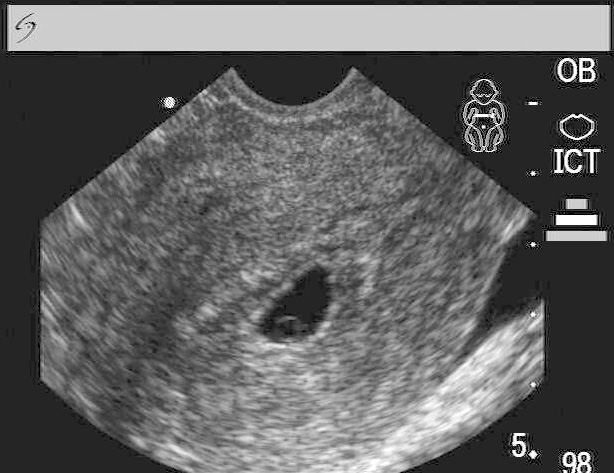 In the postoperative period, antibiotic prophylaxis is mandatory to reduce the risk of infectious complications, uterotonics to improve uterine contractility.
In the postoperative period, antibiotic prophylaxis is mandatory to reduce the risk of infectious complications, uterotonics to improve uterine contractility.
Rehabilitation
A single case of anembryony is not dangerous, but if it is repeated or another type of interruption of gestation for a short period, a thorough examination and rehabilitation is necessary. Most women have severe symptoms of chronic endometritis or its latent course is observed. Therefore, broad-spectrum antibiotics are prescribed. nine0003
To correct metabolic and functional disorders in the endometrium, anti-inflammatory drugs, enzymes, immunomodulators are used, courses of physiotherapy are prescribed. Combined oral contraceptives are used to restore hormonal regulation within 3-6 months. Planning a new pregnancy is carried out after careful preconception preparation.
Prognosis and prevention
For the life of a woman and the subsequent implementation of the reproductive function, the prognosis is favorable. After the restoration of the endometrium and the elimination of possible causes of the pathology, conception can be planned. To prevent anembryonia, it is necessary to beware of the action of external adverse factors, to avoid the use of toxic substances, alcohol, and smoking. If sexually transmitted infections are suspected, they should be treated promptly. Women 2 months before conception should start taking folic acid and continue the course until the end of the first trimester. nine0003
After the restoration of the endometrium and the elimination of possible causes of the pathology, conception can be planned. To prevent anembryonia, it is necessary to beware of the action of external adverse factors, to avoid the use of toxic substances, alcohol, and smoking. If sexually transmitted infections are suspected, they should be treated promptly. Women 2 months before conception should start taking folic acid and continue the course until the end of the first trimester. nine0003
You can share your medical history, what helped you in the treatment of anembryony.
Sources