Pregnancy belly anatomy
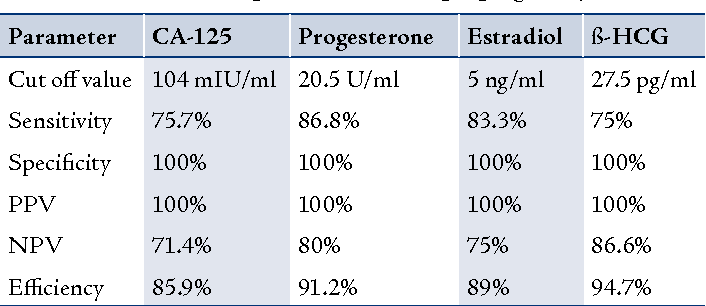
Anatomy of pregnancy and birth - abdominal muscles
Anatomy of pregnancy and birth - abdominal muscles | Pregnancy Birth and Baby beginning of content3-minute read
Listen
The most obvious physical sign that a woman is pregnant is the growing abdomen – or, ‘baby bump’ – which affects the abdominal muscles. Understanding how the abdominal muscles work is helpful for pregnant women. Strengthening your abdominal muscles during and after pregnancy helps these muscles work as they should.
What are abdominal muscles?
The abdominal muscles are those in the front of the torso (also referred to as the trunk), between the ribs and the pelvis. The abdominal muscles in both pregnant and non-pregnant people are designed to support the torso. This allows movement, such as walking and bending. The strength of the abdominal muscles holds the internal organs in place.
There are 4 types of abdominal muscles — the external and internal obliques, and the transversus and rectus abdominis — which come in pairs (one on either side of the torso), and work together to:
- stabilise the torso and keep organs in place
- support movements between the rib cage and the pelvis
- allow the torso to twist
The term 'core muscles' is commonly used to describe the deepest abdominal muscles and the muscles in the back, which attach to the spine or pelvis. The core muscles are responsible for keeping the body stable and balanced, and to protect the spine.
What happens to abdominal muscles during pregnancy and birth?
During pregnancy, the growing baby stretches the abdominal muscles. The mother's abdomen changes shape during the pregnancy because of the growth and movement of the baby, and so her abdominal muscles are also affected.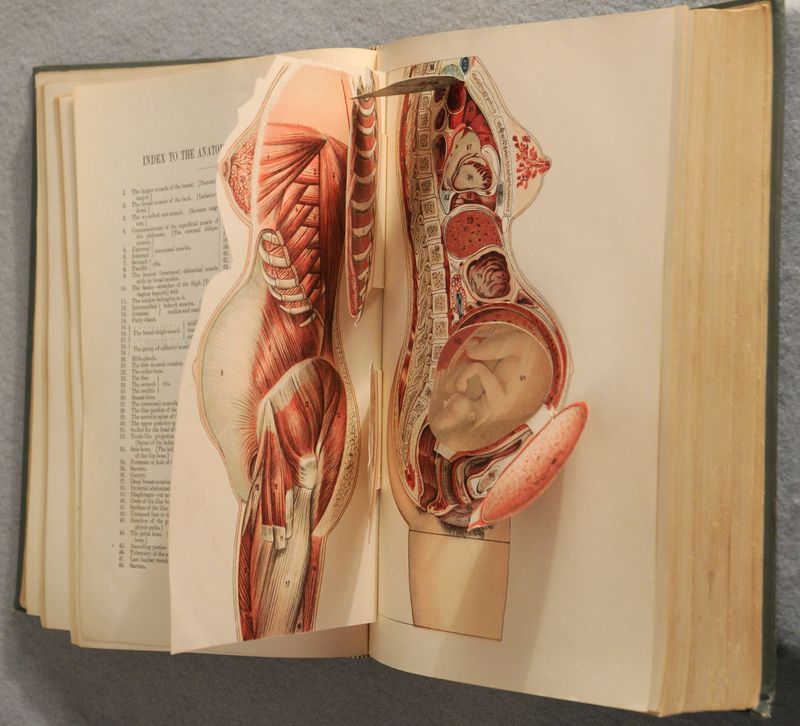 For instance, the abdominal muscles progressively stretch as the pregnancy proceeds as the womb expands.
For instance, the abdominal muscles progressively stretch as the pregnancy proceeds as the womb expands.
During the birth, most of the pushing is done by the uterus, not the abdominal muscles. After the birth, the abdominal muscles will feel weak and stretched, but these muscles should eventually become toned again.
How can abdominal muscles be strengthened during pregnancy?
Abdominal muscles overstretch during the pregnancy since the baby rests forward on them, so it is important that these muscles are exercised. Strengthening the abdominals can help pregnant women stay active and use the abdominal muscles for day-to-day activities, such as support and movement. Exercising abdominal muscles during pregnancy also helps them return to their original length and shape after the baby is born.
Safety tip: Sit-ups and crunches are not recommended during pregnancy. This is because the stretched abdominal muscles in a pregnant woman do not work the same way as when she is not pregnant. These exercises are usually done while lying on your back. This position can cause dizziness in pregnant women because the weight of the baby rests on major blood vessels.
These exercises are usually done while lying on your back. This position can cause dizziness in pregnant women because the weight of the baby rests on major blood vessels.
A safe way to work the abdominal muscles and improve core strength is to draw in the muscles without moving your spine – as though sucking your belly button in, towards the spine.
Pregnancy-specific exercise classes can also help build and maintain core strength, such as yoga and Pilates classes for pregnant women. They tend to focus on low impact exercises and feature movements that help with core strength, breathing and relaxation, strengthening abdominal muscles, the pelvic floor and relieving lower back pain.
What problems can happen to abdominal muscles in pregnancy?
The enlarging uterus causes the abdominal muscles to stretch. It may cause the two bands of muscles that meet in the middle of the abdomen to separate. This condition is called 'diastasis recti'. This muscle separation can sometimes appear as a bulge in the middle of the abdomen.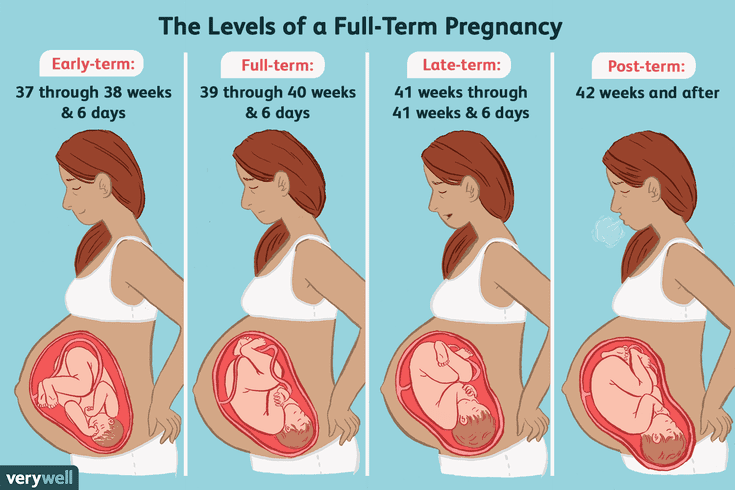 The condition may cause pain in the lower back or it might become hard to lift things or do other physical activities. Abdominal muscle separation is usually managed after childbirth with exercise and physiotherapy. Occasionally surgery is required.
The condition may cause pain in the lower back or it might become hard to lift things or do other physical activities. Abdominal muscle separation is usually managed after childbirth with exercise and physiotherapy. Occasionally surgery is required.
If you think you may have diastasis recti, see your doctor or maternal health service.
Sources:
Royal Women's Hospital (Abdominal muscles), Mayo Clinic (Why do abdominal muscles sometimes separate during pregnancy?), Better Health Channel (Abdominal muscles), Physical Therapy (Structure and Function of the Abdominal Muscles in Primigravid Subjects During Pregnancy and the Immediate Postbirth Period)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - uterus
Need more information?
Abdominal muscles - Better Health Channel
The abdominal muscles support the trunk, allow movement and hold organs in place by regulating internal abdominal pressure.
Read more on Better Health Channel website
Postnatal exercise - sample workout - Better Health Channel
Make sure your abdominal muscles have healed before you do any vigorous tummy exercises, such as crunches.
Read more on Better Health Channel website
Abdominal separation (diastasis recti)
Abdominal separation (‘diastasis recti’) occurs when the stomach muscles weaken and separate during and after pregnancy. Here's how to recognise and treat it.
Read more on Pregnancy, Birth & Baby website
The Abdominal Brace · Core exercises · Pelvic Floor First
The Abdominal Brace. Pelvic floor friendly exercises, Core exercises, The Abdominal Brace. ‘Brace your abs’, ‘Lock on your core’, ‘Switch on your core’. These are all popular phrases used in group exercises classes and by personal trainers.
‘Brace your abs’, ‘Lock on your core’, ‘Switch on your core’. These are all popular phrases used in group exercises classes and by personal trainers.
Read more on Continence Foundation of Australia website
Hernia
A hernia is the protrusion of organs, such as intestines, through a weakened section of the abdominal wall.
Read more on Queensland Health website
Abdominal pain in children - Better Health Channel
Children may feel stomach pain for a range of reasons and may need treatment
Read more on Better Health Channel website
The pelvic floor and core exercises · Pelvic floor friendly exercises · Pelvic Floor First
The pelvic floor muscles form the base of the group of muscles commonly called the ‘core’.
Read more on Continence Foundation of Australia website
The pelvic floor and core · The pelvic floor · Pelvic Floor First
The pelvic floor muscles form the base of the group of muscles commonly called the ‘core’.
Read more on Continence Foundation of Australia website
The pelvic floor · Pelvic Floor First
The pelvic floor is the base of the group of muscles referred to as your ‘core'.
Read more on Continence Foundation of Australia website
Working your pelvic floor · The pelvic floor · Pelvic Floor First
Your pelvic floor muscles can be consciously controlled and therefore trained
Read more on Continence Foundation of Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.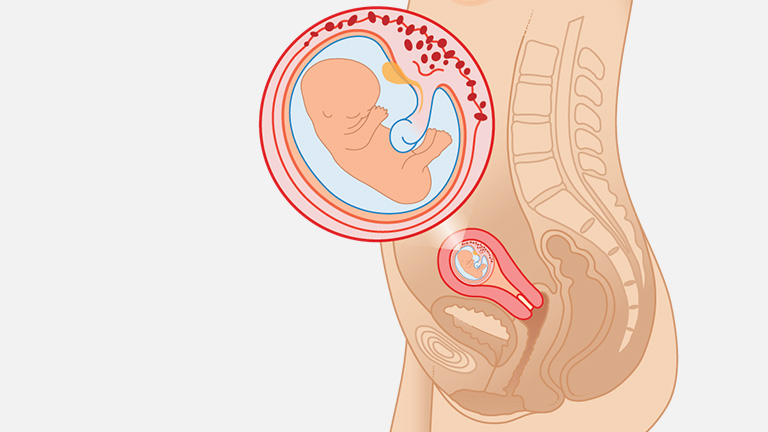
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.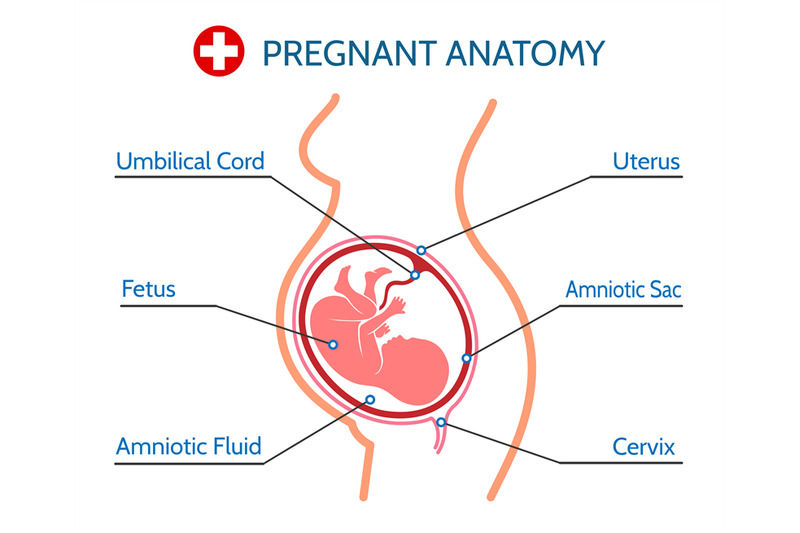
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Your Body throughout Pregnancy
Your Body Before Pregnancy
Next Image
Your Body Before Pregnancy
Before pregnancy, most of the space in your abdomen is taken up by the large and small intestines. There is no real separation between the areas of your pelvis and abdomen.
There is no real separation between the areas of your pelvis and abdomen.
In the picture here, you can see that the vagina is behind the bladder (sac that collects urine) and urethra (tube for moving urine out of bladder and body). In its normal position, your uterus is above and behind the bladder, with the cervix protruding into the vagina. The pelvic colon, rectum and anal canal are behind the vagina and uterus.
Previous | Next
Your Body at 6-7 Weeks of Pregnancy
Next Image
Your Body at 6-7 Weeks of Pregnancy
When you are between 6 and 7 weeks pregnant, you may be experiencing the early signs of pregnancy: your period has stopped and you may have nausea, breast tenderness and swelling, frequent urination and fatigue.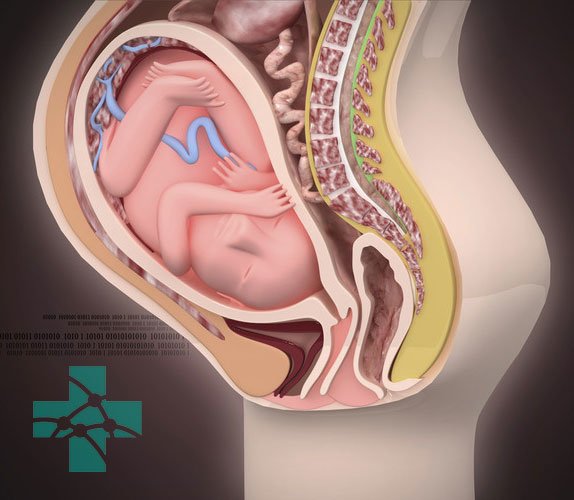
At this point, your uterus has begun to grow and become more egg-shaped. The pressure of the growing uterus on the bladder causes frequent urge to urinate.
In this image, you can see the beginnings of the placenta in the uterus. The embryo is about 1/4 inch to 1/2 inch long and weighs 1/1,000th of an ounce.
The embryo’s head is large in proportion to the rest of the body. The internal organs are forming and the heart has been beating since the end of the 4th week.
The embryo is floating in the amniotic sac. Buds for the arms and legs emerge in the 5th week and, by the 7th week, buds for fingers and toes also appear. The umbilical cord is lengthening and will continue to grow, allowing the fetus freedom to move. The 7th week represents a milestone in development: the embryo is now considered a fetus.
Previous | Next
Your Body at 12 Weeks of Pregnancy
Next Image
Your Body at 12 Weeks of Pregnancy
At the 12th week of pregnancy, the placenta is much larger. It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
The fetus is now about 3 inches long and weighs about 1 ounce. By this week, the fetus has fingernails and toenails and can open and close the fingers. The fetus will start to move, but you will not feel it yet.
Previous | Next
Your Body at 20 Weeks of Pregnancy
Next Image
Your Body at 20 Weeks of Pregnancy
By the 20th week of pregnancy, your uterus can be felt at the level of your belly button (umbilicus). The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
At this point, your uterus is especially enlarged where the placenta attaches to it (usually on the front or back wall). This gives the uterus an uneven bulge. The wall of the uterus, which lengthens and thickens early in pregnancy, stretches as the fetus grows, and becomes thinner now – just 3 to 5 millimeters thick. Your bladder moves up but not as much as your uterus, which straightens as it moves up.
As your uterus moves up, it rests against the lower portion of the front of your abdominal wall, causing it to bulge forward noticeably by your 20th week. The size of the bulge depends on how strong your abdominal muscles are. If they are firm, the uterus may be pressed against the spinal column, and there will be no noticeable bulge; if they are weak, the pressure of the uterus against the inside wall makes a sizeable bulge.
At this point, you should be able to feel light movements of the fetus.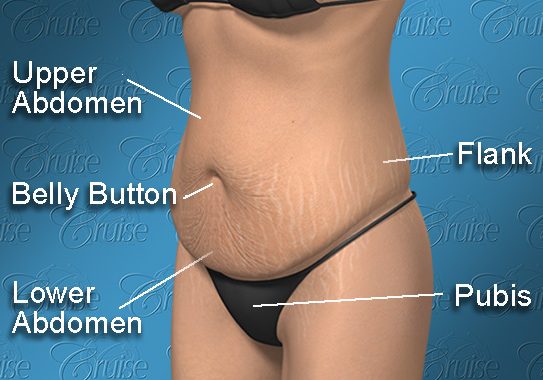 This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
Previous | Next
Next Image
At this point in pregnancy, the top of your uterus is about one-third of the distance between the bellybutton and the xiphoid cartilage at the lower end of your breastbone. Constipation is common because your uterus is pressing on your lower colon and hormones slow down your body’s excretion process. Between the growth of your uterus and general weight gain, you may be feeling fatigued. Some women also experience heartburn as your uterus presses against your stomach.
Your breasts are also changing to get ready for breastfeeding. First colostrum and then milk are produced by the grape-like clusters of tiny sacs (alveoli) deep within the breast tissue. Clusters of alveoli form lobules, which come together to form 15 to 20 lobes. Each lobe connects to a lactiferous duct for conveying milk. As the ducts extend toward the nipple and areola (darker area around the nipple), they widen into the lactiferous sinuses. These sinuses (or milk pools) release the milk through 15 to 20 tiny nipple openings in each breast when the baby nurses.
At week 28, the fetus is about 16 inches long and weighs two to three pounds. The skin is wrinkled but will become less so as more fat builds up under the skin in the next few weeks. Fine, downy hair called lanugo, and a waxy white protective substance covering the skin called vernix, are on the fetus’ body. Its eyes are open, and eyebrows and eyelashes were formed in the fourth month. The fetus sucks its thumb and its taste buds have developed. It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
Fetal organs and systems are quite well developed by the 28th week of pregnancy, but the final two months of gestation are important for further maturation of all body systems and organs.
Previous | Next
Your Body at 36 Weeks of Pregnancy
Next Image
Your Body at 36 Weeks of Pregnancy
By the end of the 36th week of pregnancy, your enlarged uterus almost fills the space within your abdomen. The fetus is inside the membrane sac within the uterus and high within the abdomen. The muscles of your abdomen support much of its weight.
During this week, the top of the uterus is at the tip of the xiphoid cartilage at the lower end of the breastbone, which is pushed forward.
The change in the position of the heart and the upward pressure of the diaphragm may make it hard to breathe at this point. The crowding of your stomach and intestines may contribute to discomfort after eating.
Your cervix is long, thick and filled with the mucous plug. By the 36th week, your vagina and urethra are elongated and all the tissues in the perineum (area between vaginal and anal openings) are enlarged. The swollen perineum projects outward in the last weeks of pregnancy and readily expands during labor.
The brain of the fetus is growing rapidly, but bones in the skull are soft so that he or she will fit through your vagina at birth. The lungs are still forming. You will likely feel the fetus kicking and may be aware of rhythmic movements, which could be hiccups or thumb sucking. Another possible sensation, sudden movement, may be a startle response.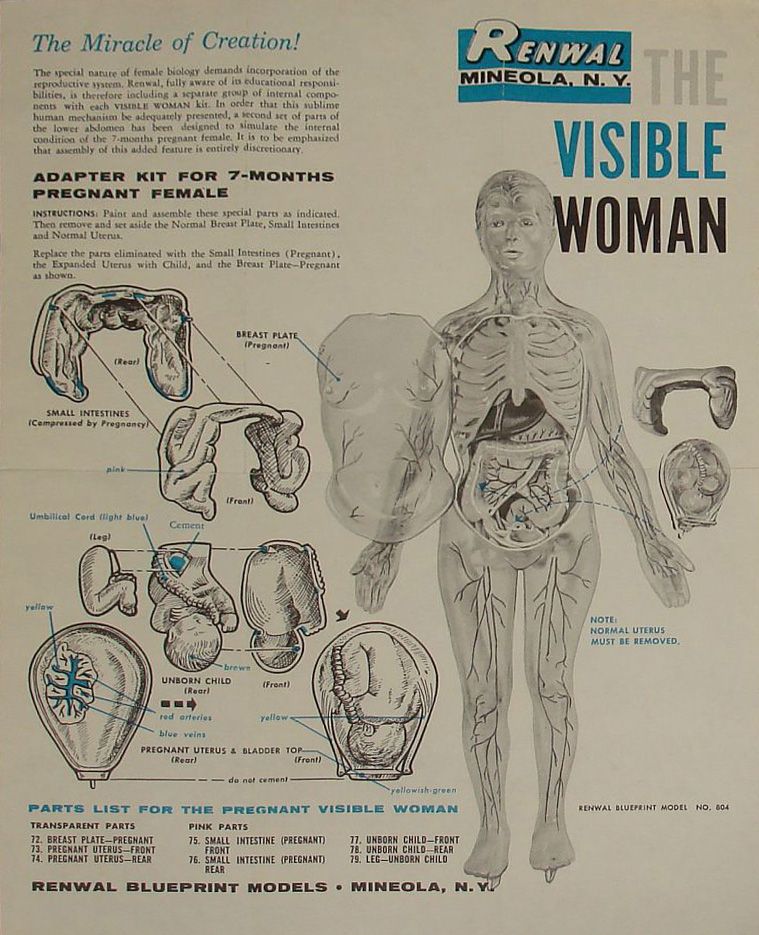
Previous | Next
Your Body at 40 Weeks of Pregnancy (Internal)
Next Image
Your Body at 40 Weeks of Pregnancy (Internal)
At full term, or 40 weeks of pregnancy, the fetus’ head has generally lowered into your pelvis, where it takes up most of the space. This is called “lightening.” In first pregnancies, this may happen a few weeks before labor. In repeat pregnancies, this can happen at the time of labor. The canal of the broad, enlarged cervix is still filled with the plug of mucous. If this is your first pregnancy, the small opening at the bottom of your cervix is usually not dilated, whereas if you have given birth before, it will often be open as wide as two fingers some time before labor begins.
At this point, you may be experiencing frequent urination, increased constipation, edema (water retention) and aching legs or vulva. Varicose veins in the vulva, rectum and legs are also possible. This is because of the position of the uterus, the pressure of the baby's head and a loss of muscle tone as the hormone relaxin loosens your tissues in preparation for birth. Other changes at this time include increased development of blood vessels and increased amount of blood.
Previous | Next
Your Body at 40 Weeks of Pregnancy (External)
Next Image
Your Body at 40 Weeks of Pregnancy (External)
You can see that the round ligament is long and enlarged. It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
Because your uterus dropped a bit, you may be able to breathe and eat more comfortably near the end of your pregnancy.
At this time, the lungs of the fetus are likely fully mature and ready to begin breathing. The fetus gains about a half pound every week at the end of pregnancy, for a birth weight of roughly 7 pounds, and is growing longer for a birth length of about 18 to 21 inches.
Labor starting on its own around week 40 is a sign that your body is ready to give birth and your baby is ready to be born.
Previous | Next
Physiological changes in the body during pregnancy
From the very first days of pregnancy, a woman's body undergoes profound transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body. During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy. nine0003
These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body. During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy. nine0003
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
The mother's circulatory system during pregnancy has to pump more blood to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of blood vessels during pregnancy decreases, which creates favorable conditions for increased supply of tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. nine0003
In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of blood vessels during pregnancy decreases, which creates favorable conditions for increased supply of tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. nine0003
And changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period. nine0003
BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period. nine0003
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), cravings for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur. nine0003
The most significant changes, however, occur in the genitals of pregnant women. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
These changes prepare the woman's reproductive system for childbirth and breastfeeding.
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy. Walls vaginas will loosen and become more elastic. External genitalia (labia minor and major), also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth. nine0003
In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth. nine0003
Skin in the genital area and in the midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released.
Changes in the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This helps to reduce the rigidity of the joints between the bones of the pelvis and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Also, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus. nine0003
This helps to reduce the rigidity of the joints between the bones of the pelvis and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Also, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus. nine0003
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women). nine0003
Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women). nine0003
Changes in the nervous system . In the first months of pregnancy and at the end of it, there is a decrease in the excitability of the cerebral cortex, which reaches its greatest degree by the time of the onset of childbirth. By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.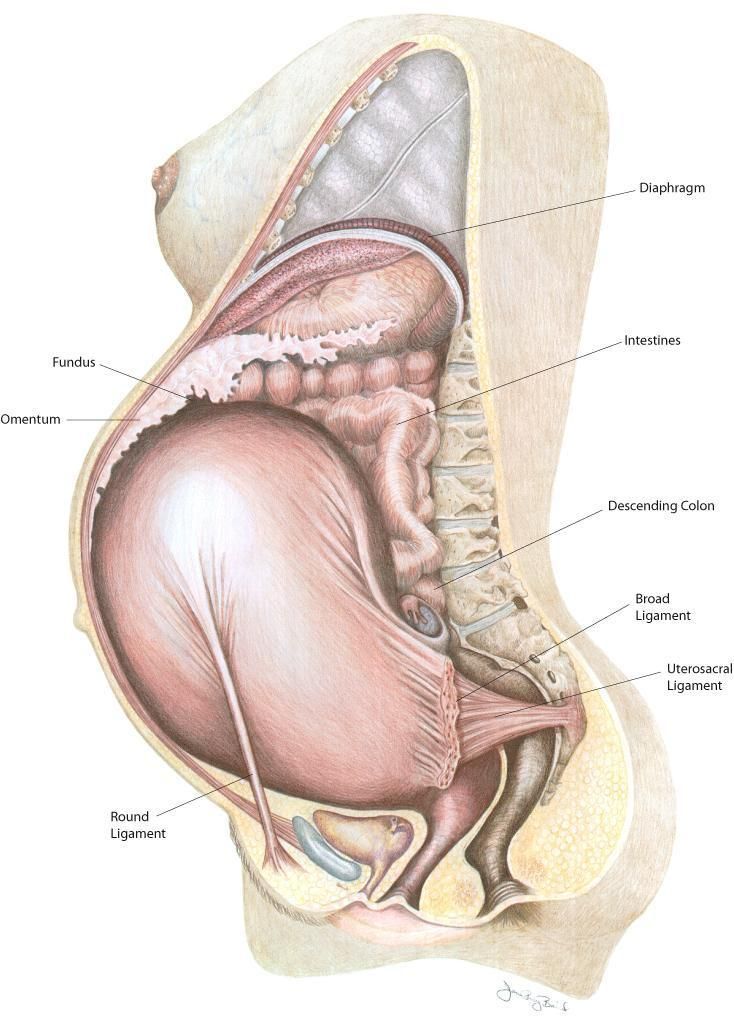
Active endocrine glands there are significant changes that contribute to the proper course of pregnancy and childbirth. Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnyova
— What is muscle diastasis and what is pubic diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy. nine0003
During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy. nine0003
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of collagen in the connective tissue. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin. nine0003
This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin. nine0003
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
— The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act. nine0003
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and cartilage that connect the pubic bones suffer. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain. nine0003
During childbirth, such a patient may have a rupture of the pubic symphysis, may require surgery to restore it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis. nine0003
There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis. nine0003
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis? nine0068
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler. nine0003
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.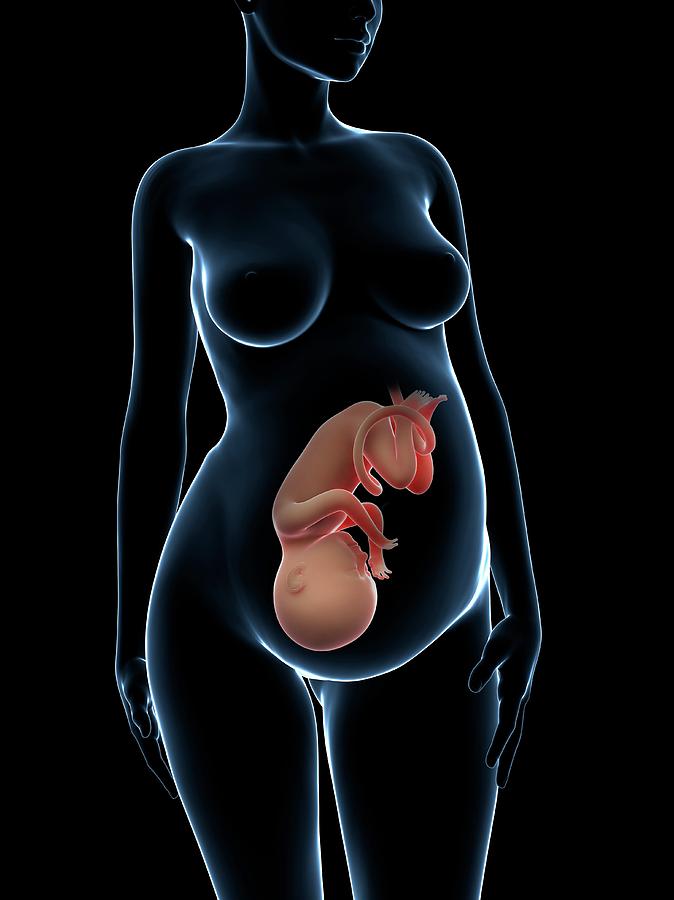
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you). nine0003
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth. nine0003
Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth. nine0003
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced.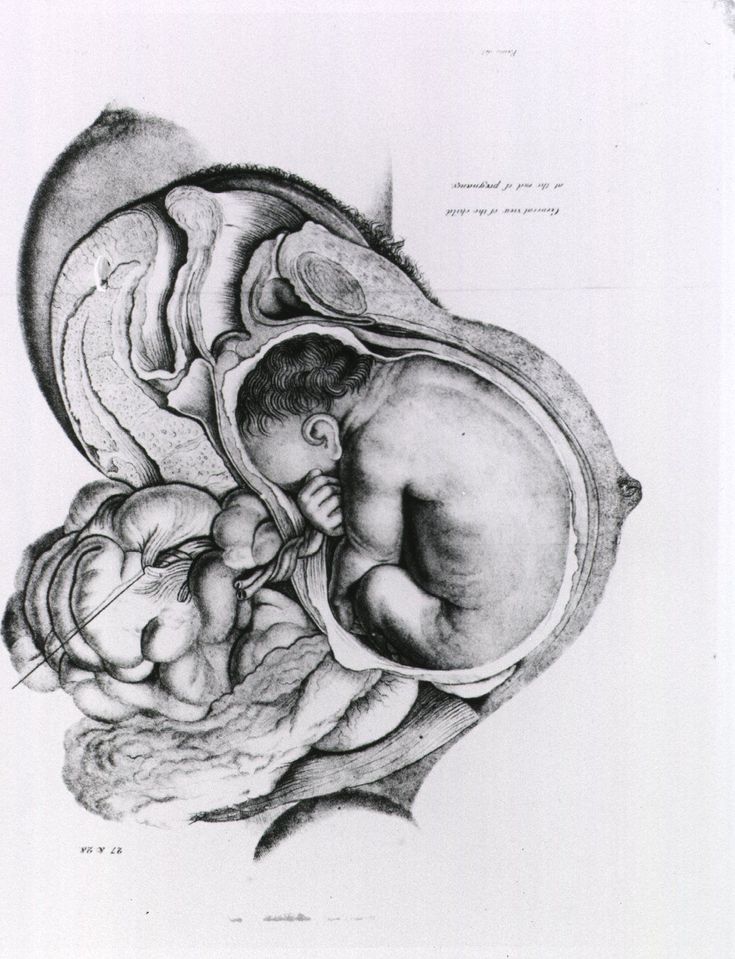 The choice of method depends on the size and localization of the defect. nine0003
The choice of method depends on the size and localization of the defect. nine0003
In case of symphysiopathy, therapeutic exercises reduce back and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment for pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers. nine0003
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence.