What is a vba2c
The Facts & Statistics on Birth After 2 Cesareans
We receive a lot of questions about VBA2C, like this email from a follower:
“I am contemplating having one more child [after two C-sections]. I have moved to Utah, where I know I can easily find a doula or birthing center that would support a VBAC. After 2 though, I don’t really know all the risks. I have friends that say don’t try it, it’s too dangerous. I’m not pregnant yet. I just want to have some dialogue about it. I want to know what’s possible.”
This mother’s story is one of frustration and struggle. VBA2C and VBAMC can be a confusing and a very misunderstood topic, leaving parents with a lot of questions and doubt. I can personally say that I had a lot of those questions and doubt when I was going for my VBA2C.
What are the risks and how can you find a VBAC-friendly provider to support you? How long should you wait to get pregnant after a C-section? What are the benefits of a natural birth, as opposed to a third Cesarean?
What are the FACTS about VBA2C?
This article will answer your questions, providing facts and VBA2C statistics to help you make informed decisions with your provider about your next birth.
What is a VBA2C?
VBA2C stands for Vaginal Birth After Two Cesareans. If you have given birth via C-Section twice, your provider will consider your next birth a Vaginal Birth after 2 C-sections, even if you’ve also had previous vaginal births.
What are the risks of having a natural birth after 2 C-Sections?
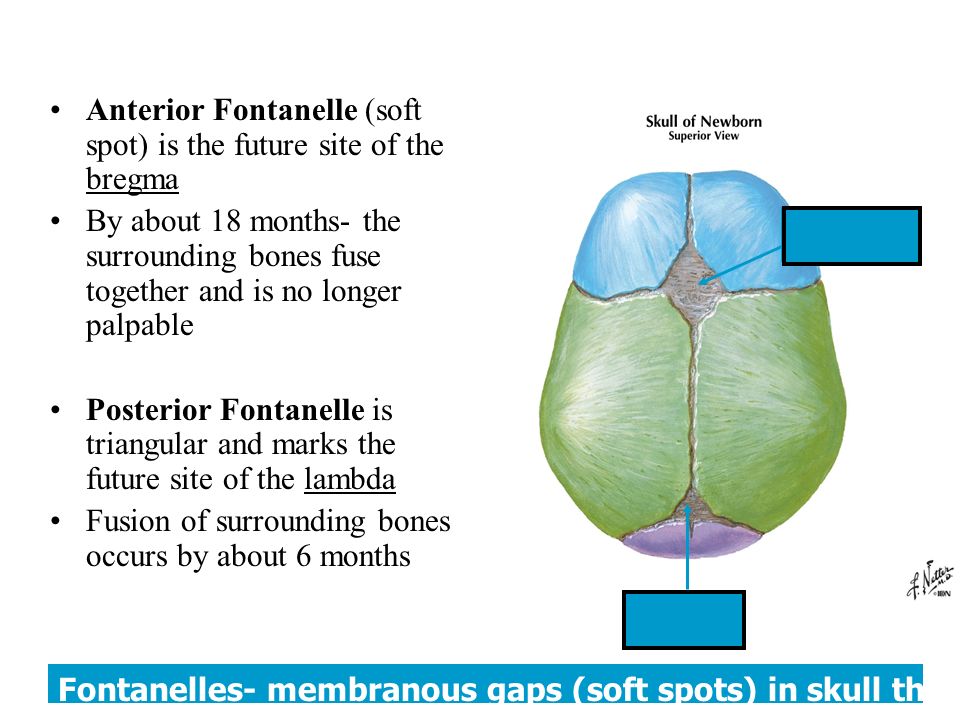
Uterine rupture is the main risk discussed by healthcare providers with parents who want to have a vaginal birth after two C-sections. Uterine rupture occurs when there is a small or large tear in the uterine wall, usually at the initial Cesarean scar location.
Although the chances are very low, there is a slight increase in rates of uterine rupture for VBA2C, with a rate of approximately 1.4%. ACOG suggests that VBA2C is still a very reasonable option and not a contraindication.
When it comes to VBAC, there are risks that people should be aware of. However, there are also risks that come with a repeat C-Section. It is very important to learn the risks of VBA2C and repeat Cesarean before deciding on your birth plan.
What is the VBA2C success rate?
Many providers discourage their patients from trying for a VBA2C, when in fact, the chances of having a successful vaginal birth after two C-sections is pretty high. Research shows that people who decide to have a VBA2C will have a 71.1% success rate.
One of the biggest hurdles for people who want to go forward with delivering vaginally after two C-sections is that it can be hard to find a provider who is up to date with the VBA2C facts and statistics and will truly support them.
5 VBA2C facts you should know
Now that we’ve covered some of the most common questions about VBA2C, here are five more facts about VBA2C to help guide your journey!
P.S. Did you know, my business partner, Meagan, had a VBA2C? You can read her story here.
Look at this picture of Meagan and her VBA2C baby, aren’t they just gorgeous?!
1. Your chances of a successful VBA2C are similar to those of VBAC after just one Cesarean.
In ACOG Practice Bulletin 184, two large studies are referenced. These studies had sample sizes large enough to account for small variances that might influence the results.
It is significant for ACOG (American College of Obstetrics and Gynecology) to recognize studies like this as credible. In other words, the fact that they are even cited there is AWESOME!
The two studies referenced in the bulletin concluded that the success rate of vaginal birth after one Cesarean and two Cesareans varies by 2% or less, depending on which study you look at. They also state that having a midwife, doula support, and going into spontaneous labor increase the likelihood of a vaginal birth.
2. ACOG recommends VBA2C as a safe option.
Speaking of ACOG, since 2010, their stance on VBA2C is that it is reasonable to consider:
“…reasonable to consider women with two previous low-transverse cesarean deliveries to be candidates for TOLAC and to counsel them based on the combination of other factors that affect their probability of achieving a successful VBAC.
ACOG Practice Bulletin Number 205”
More important to note is that there is no mention of a requirement to have had a prior vaginal delivery to be considered. If you are going for VBA2C, this bulletin is very important to have in your back pocket as you work with your provider to determine your care.
3. Choosing a repeat Cesarean does NOT eliminate your chance of rupture.
We often only talk about uterine rupture during TOLAC (Trial of Labor After Cesarean, which simply means attempting VBAC), and by choosing elective repeat Cesarean, you can eliminate any chance of uterine rupture.
Although focus is usually on uterine rupture during labor, it is possible for uterine ruptures to occur before labor begins. These types of uterine rupture are usually more devastating, and can cause serious health complications or worse in mother and baby.
It is NOT true that deciding against a VBAC means that you won’t have any risk of uterine rupture. In fact, occasional studies have even found a higher rate of rupture in the elective repeat Cesarean groups! So keep in mind that it is the PREVIOUS CESAREAN that puts you at risk for uterine rupture.
In fact, occasional studies have even found a higher rate of rupture in the elective repeat Cesarean groups! So keep in mind that it is the PREVIOUS CESAREAN that puts you at risk for uterine rupture.
4. There are things you can do to minimize uterine rupture risks.
There are many things you can do to help minimize the risk of uterine rupture, while encouraging labor to progress at your body’s pace. While induction and stimulation of labor are sometimes necessary, studies show they may be factors in uterine rupture risk.
Learning about these factors and discussing them with your provider before the birth will improve your chances of having a successful VBAC, too.
- Stay away from induction for VBAC unless absolutely necessary.
- Avoid augmentation of labor (using something to stimulate contractions, usually Pitocin)
- Avoid excessive Pitocin, and increasing the dose too fast.
- Avoid Cytotec (misoprostol) COMPLETELY.
- Avoid providers who aggressively intervene with and manage labor.
- Stay mobile. Walk, change position and posture when in active labor.
- In early labor and if labor stalls, rest or sleep.
- Do EVERYTHING you can to encourage an optimal fetal position BEFORE labor begins.
- IF your baby is not in a great position and labor stalls, or you have back labor, try optimal fetal positioning exercises like Spinning Babies, MILES circuit, abdominal lifting, side lying, or getting on your hands and knees to try and help baby settle into a better position.
- Avoid rupturing membranes if the baby is not in optimal position if possible.
- Avoid or delay getting an epidural for VBAC if possible.
- Have attentive labor support from a VBAC doula or labor coach ALL THE TIME
- Be aware of typical labor patterns. Any stall in labor is usually indicative that something needs to change (mindfulness or relaxation for birth, baby position, rest/sleep, and even Pitocin in some instances). Figure out what needs to change and fix it if you can.
 A long stall combined with high doses of Pitocin is a prime scenario for uterine rupture.
A long stall combined with high doses of Pitocin is a prime scenario for uterine rupture. - HONOR YOUR INTUITION!!! If you feel that something is not quite right or if the baby’s movement is significantly decreased, insist that your provider or their staff pay attention to you. In many instances, uterine rupture occurs when a mother knows something is wrong intuitively before providers pay sufficient attention.
5. The risk for rupture is still incredibly low, maybe even the same as VBAC.
The limit of most VBA2+C research is that almost no studies have controls for Pitocin or other pharmaceutical interventions, and this may be a significant factor.
Although there is still some debate, uterine rupture rates may be somewhat higher in VBA2C when Pitocin or multiple induction agents are used. Nearly all VBA2C studies analyzed stated Pitocin or other drugs to stimulate labor were used with 50% or more of participants.
So, it is impossible to know for sure the true rate of rupture in VBA2C.
Although hard data is lacking, it seems likely that the average VBA2C rupture rate of 1.4% found in the ACOG bulletin could be reduced by inducing less, inducing only when the cervix is ripe, when induction is truly necessary, and using drugs and interventions a lot less (and much more judiciously when they are used).
So, with all this information, should I attempt (TOLAC) a VBA2C?
This is a decision that each family must make for themselves. Take a look at your desires and fears and what motivates YOU. Weigh the benefits and risks based on your specific needs and circumstances.
Listen to the advice of your providers, but remember that each provider differs, sometimes drastically, in their support, knowledge, and how they approach VBA2C. They may not be up to date with current recommendations and guidelines.
Moving forward, seek out the current recommendations and research, talk to several providers and get their opinions until you find one whose knowledge and philosophy align with yours. Weigh the potential risks and benefits and check your own intuition to decide what is best for YOU and YOUR family.
Weigh the potential risks and benefits and check your own intuition to decide what is best for YOU and YOUR family.
Where to find even more info about VBA2C
Learn more about not only VBA2C but Vaginal Birth after Multiple C-sections (VBAMC) on our blog.
Check out Episode 2 of our podcast, all about Meagan’s VBA2C journey. Then find more VBA2C birth stories as you continue to listen.
Want to learn everything you can before your VBAC? Register today for our Ultimate VBAC Course for Parents.
Vaginal Birth After Cesarean Delivery (VBAC)
-
If you have had a previous cesarean delivery, you have two choices about how to give birth again:
-
You can have a scheduled cesarean delivery.
-
You can give birth vaginally. This is called a VBAC.
-
-
A TOLAC is the attempt to have a VBAC.
 If it is successful, TOLAC results in a vaginal birth. If it is not successful, you will need another cesarean delivery.
If it is successful, TOLAC results in a vaginal birth. If it is not successful, you will need another cesarean delivery. -
A successful VBAC has the following benefits:
-
No abdominal surgery
-
Shorter recovery period
-
Lower risk of infection
-
Less blood loss
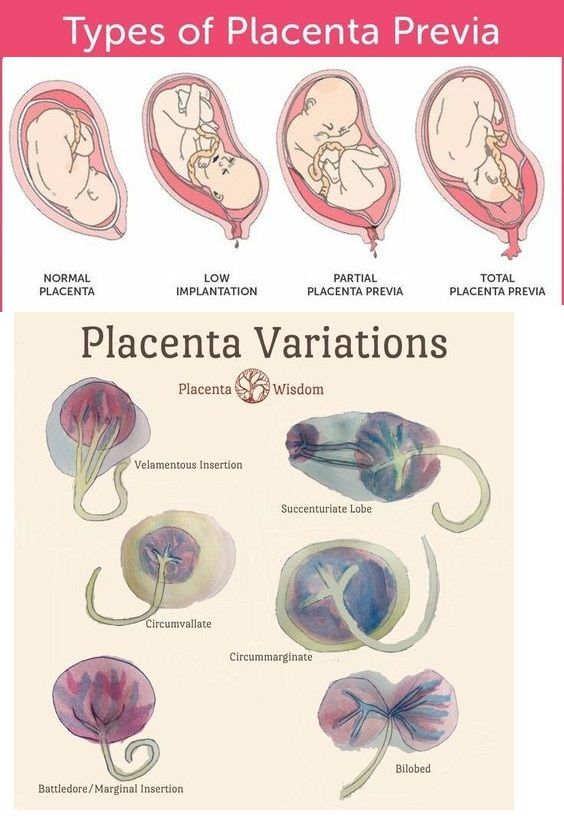
Many women would like to have the experience of vaginal birth, and when successful, VBAC allows this to happen. For women planning to have more children, VBAC may help them avoid certain health problems linked to multiple cesarean deliveries. These problems can include bowel or bladder injury, hysterectomy, and problems with the placenta in future pregnancies. If you know that you want more children, this may figure into your decision.
-
-
Some risks of a VBAC are infection, blood loss, and other complications.
 One rare but serious risk with VBAC is that the cesarean scar on the uterus may rupture (break open). Although a rupture of the uterus is rare, it is very serious and may harm both you and your fetus. If you are at high risk of rupture of the uterus, VBAC should not be tried.
One rare but serious risk with VBAC is that the cesarean scar on the uterus may rupture (break open). Although a rupture of the uterus is rare, it is very serious and may harm both you and your fetus. If you are at high risk of rupture of the uterus, VBAC should not be tried. -
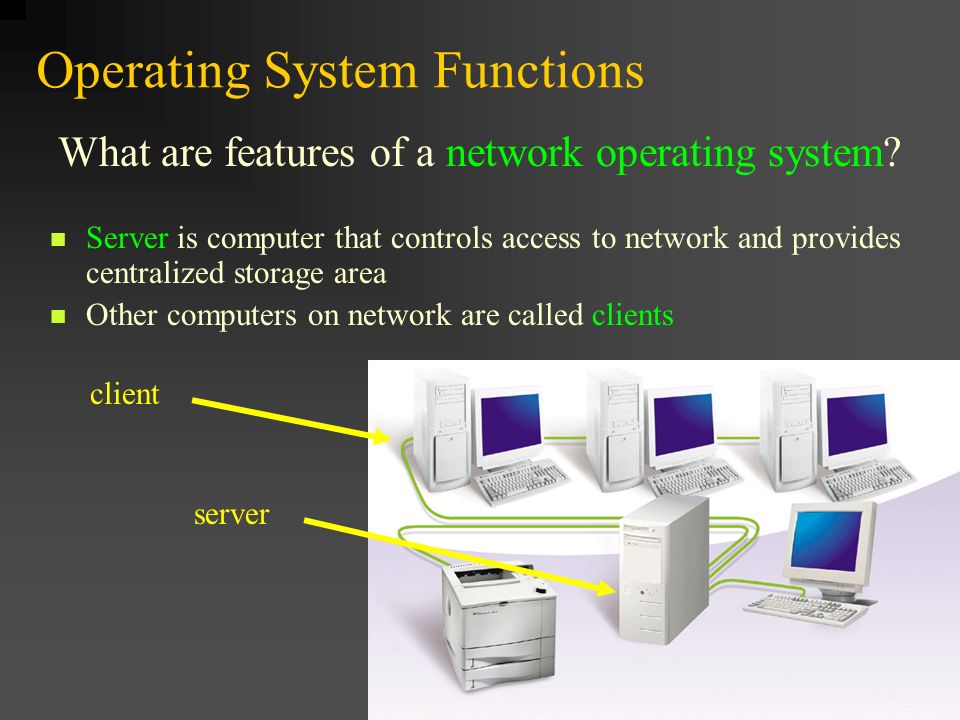
After cesarean delivery, you will have a scar on your skin and a scar on your uterus. Some uterine scars are more likely than others to cause a rupture during VBAC. The type of scar depends on the type of cut in the uterus:
-
Low transverse—A side-to-side cut made across the lower, thinner part of the uterus. This is the most common type of incision and carries the least chance of future rupture.
-
Low vertical—An up-and-down cut made in the lower, thinner part of the uterus. This type of incision carries a higher risk of rupture than a low transverse incision.

-
High vertical (also called “classical”)—An up-and-down cut made in the upper part of the uterus. This is sometimes done for very preterm cesarean deliveries. It has the highest risk of rupture.
-
-
You cannot tell what kind of cut was made in the uterus by looking at the scar on the skin. Medical records from the previous delivery should include this information. It is a good idea to get your medical records of your prior cesarean delivery so your obstetrician-gynecologist (ob-gyn) or other health care professional can review them.
-
VBAC should take place in a hospital that can manage situations that threaten the life of the woman or her fetus. Some hospitals may not offer VBAC because hospital staff do not feel they can provide this type of emergency care.
 You and your ob-gyn or other health care professional should consider the resources available at the hospital you have chosen.
You and your ob-gyn or other health care professional should consider the resources available at the hospital you have chosen. -
If you have chosen to try a VBAC, things can happen that alter the balance of risks and benefits. For example, you may need to have your labor induced (started with drugs or other methods). This can reduce the chances of a successful vaginal delivery. Labor induction also may increase the chance of complications during labor. If circumstances change, you and your ob-gyn or other health care professional may want to reconsider your decision.
The reverse also may be true. For example, if you have planned a cesarean delivery but go into labor before your scheduled surgery, it may be best to consider VBAC if you are far enough along in your labor and your fetus is healthy.
-
Cesarean Delivery: Delivery of a baby through surgical incisions made in the woman’s abdomen and uterus.
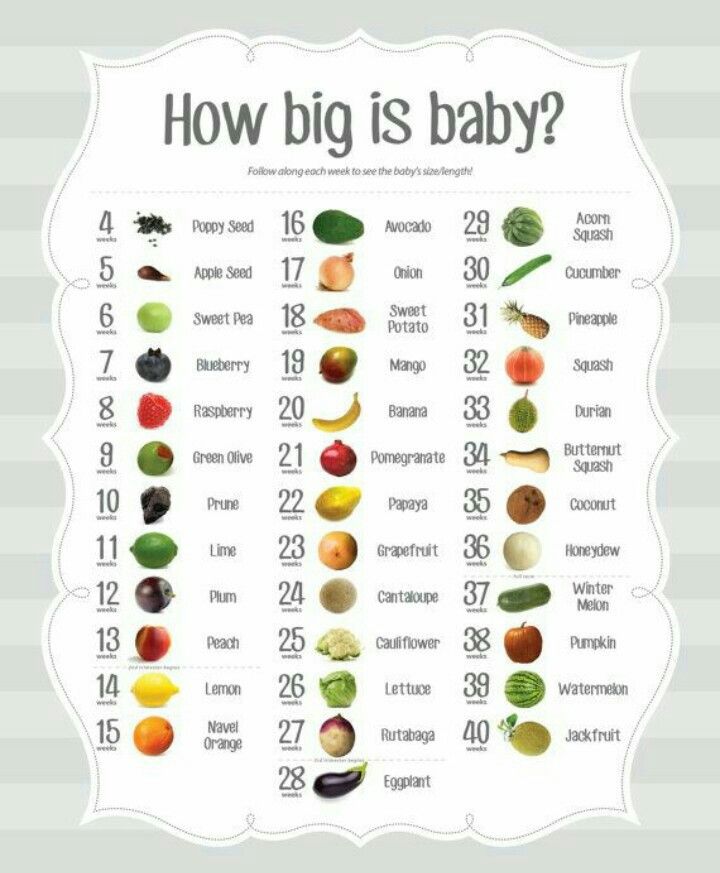
Fetus: The stage of prenatal development that starts 8 weeks after fertilization and lasts until the end of pregnancy.
Hysterectomy: Removal of the uterus.
Obstetrician–Gynecologist (Ob-Gyn): A physician who specializes in caring for women during pregnancy, labor, and the postpartum period.
Placenta: Tissue that provides nourishment to and takes waste away from the fetus.
Uterus: A muscular organ located in the female pelvis that contains and nourishes the developing fetus during pregnancy.
Don't have an ob-gyn? Search for doctors near you.
FAQ070
Published: December 2017
Last reviewed: August 2022
Copyright 2022 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public.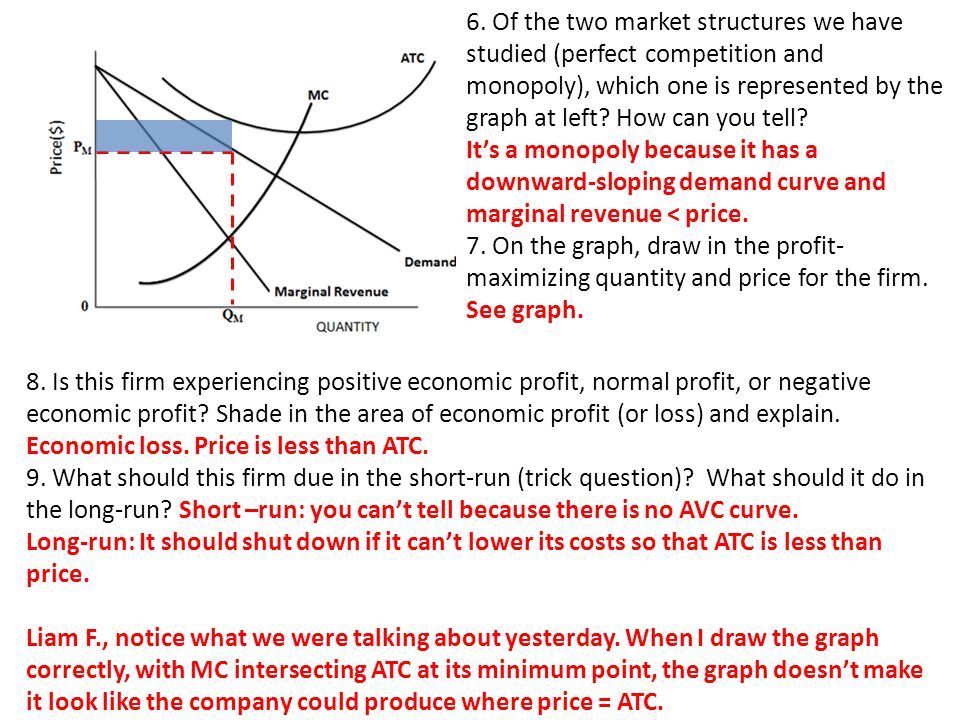 It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
Medical Techniques to Replace Conventional Vaginal Births
Your body, your baby, your obstetrician or midwife all have an influence (some more pronounced than others) that makes every birth almost entirely unique. While childbirth is often portrayed in a fairly similar fashion in the popular media, there are actually many medical techniques that can be used to aid or replace conventional childbirth.
Which birth option is right for you depends on your health, the health of your baby, and the possible complications that may arise. As a result, the best way for you to give birth may change from moment to moment. A normal birth may suddenly turn into a caesarean section or an operative vaginal delivery due to your urgent medical needs. nine0003
nine0003
What does it all mean?
When you're pregnant, you hear a lot of abbreviations and jargon! So it's helpful to have a brief definition of what it all means:
- Caesarean section: In a caesarean section, the baby is delivered through a surgical incision in the abdomen and uterus.
- Single apex caesarean section: This is a caesarean section performed on a single baby (not twins, triplets or more) whose head is pointing down into the birth canal. In other words, Singleton-Vertex caesarean delivery tends to be less predictable or selective. nine0012
- Operative vaginal delivery: When your obstetrician or midwife uses forceps, a special vacuum, or other instruments, this is commonly referred to as an operative vaginal delivery.
- VBAC: Also known as vaginal delivery after caesarean section, that's exactly what it sounds like. A woman who gives birth vaginally after giving birth by caesarean section in the past.
- TOLAC: an attempted delivery after a caesarean section is when a woman in labor tries to give birth vaginally after caesarean section or VBAC.
If unsuccessful, a repeat caesarean section (RCS) is performed.
A caesarean section is a surgical procedure in which an incision is made along the abdomen and through the uterus. The baby is born through this incision. Some women choose to give birth by caesarean section. However, in most cases, caesarean section is resorted to due to complications or risk factors that occur during pregnancy or childbirth. Typically, a caesarean section is performed under regional anesthesia, which means you won't feel anything from the waist down. Recovery from the procedure usually means 3 days or so in the hospital, followed by several weeks of rest and recovery after returning home. nine0003
A caesarean section may be performed for a variety of reasons, including the following:
- The baby is not in the correct birth position (the head is not pointing towards the birth canal).
- The child may be in an obvious state of distress.
- The mother may have multiple births (eg, twins, triplets, or more).
- The mother may have already given birth by caesarean section.
This list is not exhaustive, but it does provide some of the most common reasons for a caesarean section. nine0003
What is a unipolar vertex caesarean section?
Singleton-Vertex caesarean section is a caesarean section that delivers one baby with the baby's head in the face down position. Singleton-Vertex caesarean delivery is closely monitored by healthcare professionals because it is often optional. This can provide healthcare professionals with a good data set to compare the health and safety of caesarean section versus vaginal delivery. nine0003
However, on a case-by-case basis, caesarean section in singleton-vertex form may be performed for a variety of reasons, some of which are optional and some of which are a reaction to complications. So don't let the jargon fool you! Many caesarean sections are unimodal caesarean sections. This nomenclature is simply a way of referring to the number of children born and the position of the child (head facing the birth canal).
Operative vaginal delivery
In an operative vaginal delivery, the OB/GYN uses forceps, vacuum extraction, or a combination of both to help the woman in labor. Operative vaginal delivery is usually used only when there are problems or complications during childbirth - usually in the second stage. Therefore, an operative vaginal delivery is not something that expectant mothers can choose for themselves (as, for example, with a caesarean section), it must be performed by a qualified doctor, for example obstetrician-gynecologist . However, the possibility of using these methods is a good reason to discuss this procedure with your OB/GYN or midwife.
When is operative vaginal delivery used?
Operative vaginal delivery is an interventional approach to help a woman in labor when she has problems. Your OB/GYN or midwife will use either forceps or vacuum extraction (or a combination of both) depending on a number of factors. Using these tools, your OB/GYN will attempt to gently guide the baby through the birth canal. nine0003
nine0003
An operative vaginal delivery is usually performed in the following cases:
- The progress of labor has slowed down, even if contractions continue (and the mother continues to actively push).
- There are indications that the child is in serious condition.
- Operative vaginal births account for about 3% of all births. So they're not exactly common, but they do happen.
TOLAC and VBAC
TOLAC stands for Trial of Labor After C-Section. Successful TOLAC results in vaginal delivery after caesarean section (VBAC). After a caesarean section, a woman may experience certain complications that can make vaginal delivery more difficult. TOLAC is designed to help a woman give birth again without the need for a caesarean section. nine0% of women who have had a caesarean section are candidates for a vaginal delivery. But VBAC is not for everyone. Your OB/GYN or midwife will have a consultation with you to discuss the risks and benefits and make sure you are healthy enough to have a vaginal birth after a caesarean section.
You may not qualify for VBAC if you:
- You have had multiple births by caesarean section.
- You have a previous vertical incision along the uterus. nine0011 Your c-section scar has already ruptured on previous occasions.
- You have undergone some other surgical procedure (for example, removal of a fibroid).
However, everyone's body is different, so your gynecologist or midwife will carefully review your history and advise you on the risks and benefits. Usually VBAC is done because it provides significant benefits. These benefits include:
- Lower risk of complications such as infection, heavy bleeding or blood clots. nine0012
- Shorter hospital stay and recovery time after childbirth.
- More options for future births. Most women who have had two caesareans in a row cannot safely choose VBAC as an option. This also means that you will have more options to customize your birth plan.

The best candidates for VBAC are usually women who have had a vaginal birth in the past.
Choosing the right birth option for you
When you work with an OB/GYN or midwife, you will have the opportunity to create a birth plan that best suits your medical needs and desires. Sometimes a caesarean section, or VBAC, is part of this plan.
In other cases, caesarean section or operative vaginal delivery may be required due to complications during delivery. The more you know about these methods in advance, the fewer questions you may have at the moment, so be sure to discuss all possibilities with your obstetrician or midwife. nine0003
Topical issues of choosing the method of delivery for women with a history of caesarean section
The medical and social significance of the problem of abdominal delivery is determined by its prevalence, the impact on the most important health indicators, parameters of maternal and perinatal mortality. The frequency of caesarean section (CS) is uncontrollably and constantly growing, which gives rise to new problems of delivery of previously operated women, which in Ukrainian realities are solved mainly unilaterally, in favor of an elective repeat CS. Relevant data of mainly foreign authors on the most debatable aspects of the problem are presented: the risk of primary CS, ways to control the overall frequency of CS, the frequency and possibilities of predicting the success of vaginal delivery. nine0003
Relevant data of mainly foreign authors on the most debatable aspects of the problem are presented: the risk of primary CS, ways to control the overall frequency of CS, the frequency and possibilities of predicting the success of vaginal delivery. nine0003
Key words: delivery by caesarean section, frequency, causes, repeated caesarean section, vaginal delivery.
1. Domingues R. M. S. M. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de Parto Final / R. M. S. M. Domingues, M. A. B. Dias, M. Nakamura-Pereira [et al.] // Cad Saude Publica. –2014. – 30.–S101–S116. https://doi.org/10.1590/0102-311X00105113
2.Gibbons L. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage / L. Gibbons, J. Belizán, J. Lauer, [et al.] // World Health report. - 2010. - R.30. nine0003
3. Orlova V.S. Abdominal delivery as a medical and social problem of modern obstetrics / V. S. Orlova, I.V. Kalashnikova, E.V. Bulgakov, Yu.V. Voronova // Journal of obstetrics and women's diseases. - 2013. - T. LXII, No. 4. - P. 6-14.
S. Orlova, I.V. Kalashnikova, E.V. Bulgakov, Yu.V. Voronova // Journal of obstetrics and women's diseases. - 2013. - T. LXII, No. 4. - P. 6-14.
4. Radzinsky V.E. Obstetric aggression / V.E. Radzinsky. - M. : Status Praesens Publishing House, 2011. - 688 p.
5. Radzinsky V.E. obstetric risk. Maximum information - minimum danger for mother and baby / V.E. Radzinsky, S.A. Knyazev, I.N. Kostin. – M.: Eksmo, 2009. - 288 p.
6. Bailit J. L. Rates of labor induction without medical indication are overestimated when derived from birth certificate data / J. L. Bailit // Am J Obstet. Gynecol. –2010. – 203:269. – e1-3.
7. Little S. E. The relationship between variations in cesarean delivery and regional health care use in the United States / S. E. Little, E. J. Orav, J. N. Robinson [et al.] //Am J Obstet Gynecol. –2016. – 214:735.e1.–R. eight.
8. Application of the Robson classification of cesarean section in focus: Robson group / Budhwa T. [et al.] A report by the child health network for the greater Toronto area. – Toronto, 2010. – 60 p. nine0003
– Toronto, 2010. – 60 p. nine0003
9. Armstrong J. C. Comparing variation in hospital rates of cesarean delivery among low-risk women using 3 different measures / J. C. Armstrong, K. B. Kozhimannil, P. McDermott [et al.] // FEBRUARY 2016 American Journal of Obstetrics & Gynecology. . –2016. –Vol. 214, Issue 2. -P. 153-163. https://doi.org/10.1016/j.ajog.2015.10.935; PMid:26593970
10. American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine; A. B. Caughey, A. G. Cahill, J. M. Guise, D. J. Rouse / Safe prevention of the primary cesarean delivery. 2014.-210:179. -R. 93.
11. Shields L. The SMFM cesarean birth rate can be safely reduced without increasing maternal or neonatal morbidity / L. Shields, C. Klein, B. Pelletreau, S. Wiesner // American Journal of Obstetrics & Gynecology. - 2018. - P. 541-542. https://doi.org/10.1016/j.ajog.2017.11.500
12. Caughey A.B. Systematic review: elective induction of labor versus expectant management of pregnancy / A. B. Caughey, V. Sundaram, A.J Kaimal, et al. // Ann Intern Med. – 2009. -151:252. – R. 63. https://doi.org/10.7326/0003-4819-151-4-200908180-00007; PMid:19687492
B. Caughey, V. Sundaram, A.J Kaimal, et al. // Ann Intern Med. – 2009. -151:252. – R. 63. https://doi.org/10.7326/0003-4819-151-4-200908180-00007; PMid:19687492
13. Burke N. Effect of induction of labor on cesarean delivery rates in nulliparous patients: results from the prospective multi-center Genesis Study / N. Burke, G. Burke, F. Breathnach [et al.] // American Journal of Obstetrics & Gynecology. –2016. – S.343. https://doi.org/10.1016/j.ajog.2015.10.691
14. Nicholson M. Active management of risk in nulliparous pregnancy at term: association between a higher preventive labor induction rate and improved birth outcomes / J. M. Nicholson, M. H. Stenson, L. Kellar [et al.] // Am J Obstet Gynecol. –2009.–200: 254.e1.–R. 254.
15. Melman S. Analysis of current Dutch practice on cesarean deliveries / S. Melman, E. Schoorel, F. Vrouenraets [et al.] // American Journal of Obstetrics & Gynecology. - 2013. - R. 327. https://doi.org/10.1016/j.ajog.2012.10.118
16. Rossi A. C. Maternal morbidity following a trial of labor after cesarean section vs elective repeat cesarean delivery: a systematic review with metaanalysis A. Cristina Rossi, Vincenzo D’Addario // American Journal of Obstetrics & Gynecology. - 2008. - Vol. nineteen9, Issue 3. - P.224-231. https://doi.org/10.1016/j.ajog.2008.04.025; PMid:18511018
Rossi A. C. Maternal morbidity following a trial of labor after cesarean section vs elective repeat cesarean delivery: a systematic review with metaanalysis A. Cristina Rossi, Vincenzo D’Addario // American Journal of Obstetrics & Gynecology. - 2008. - Vol. nineteen9, Issue 3. - P.224-231. https://doi.org/10.1016/j.ajog.2008.04.025; PMid:18511018
17. Are we trending back to “once a cesarean birth, always a cesarean birth”? / S. Tucker, C. Kanaan, M. Plevyak [et al.] // American Journal of Obstetrics & Gynecology. - 2003. - Vol. 189, Issue 6. - P. 139.
18. Polenov N.I. Functional state of the lower segment of the uterus in pregnant women after caesarean section: Abstract of the thesis. diss. … cand. honey. Sciences: 14.01.01. Obstetrics and gynecology; 14.00.16. – Pathological physiology. - St. Petersburg, 2008. - 28 p. nine0003
19. Khatib N. New model, based on cervical length, predicts successful VBAC / N. Khatib, M. Emad, R. Beloosesky [et al.] // American Journal of Obstetrics & Gynecology. - 2015. - Vol. 212, Issue 1, Supplement. - P. 195-S196. https://doi.org/10.1016/j.ajog.2014.10.418
20. Ruhstaller K. Trial of labor after cesarean delivery: the impact of BMI / K. Ruhstaller, M.K. hoffman. A. sciscione // Am. J. Obste. Gynecol. - 2012 - R. 295-296.
21. Vaginal birth after cesarean: neonatal outcomes and United States birth setting / E.L. Tilden, M. Cheyney, J.-M. Guise [et al.] // Am J Obstet Gynecol. – 2017. – 216:403.e1. - R. 1–8. nine0003
22. Perminova E.I. Pathological analysis of myometrial scars after caesarean section and conservative myomectomy: Abstract of the thesis. diss. … cand. honey. Sciences: 14.03.02. – Pathological anatomy; 01/14/01. – Obstetrics and Gynecology // Research Institute of Regional Pathology and Pathomorphology of the Siberian Branch of the Russian Academy of Medical Sciences. - Novosibirsk, 2010. - 25 p.
23. Worstell T. Inducing a TOLAC: worth the risk? / T. Worstell, A. Kaimal, A. Cahill [et al.] // Am. J. Obstet. Gynecol. - 2015. - Jan., Sup. - R. 205-206. nine0003
J. Obstet. Gynecol. - 2015. - Jan., Sup. - R. 205-206. nine0003
24. Nazarenko L.G. Criteria for the prognosis of the success of vaginal canopies in women with a history of caesarean rupture / L.G. Nazarenko, K.M. Nedorezova // Obstetrics. Gynecology. Genetics. - 2016. - No. 3. - P. 5–10.
25. Schoorel E. Probability of vaginal birth after caesarean: don’t ask the obstetrician / E. Schoorel, H. Scheepers, D. Hunen [et al.]. // American Journal of Obstetrics & Gynecology. - 2014. - R. 283. https://doi.org/10.1016/j.ajog.2013.10.608
26. Vdovichenko Yu.P. Algorithm for diagnosis, prevention and treatment of sexual dysfunctions in women after caesarean section / Yu.P. Vdovichenko, O.Yu. Gurzhenko // Women's Health. - 2015. - No. 10. - P. 70–72.
27. Gorbunova O.V. Pathology of the reproductive system in women with an operated uterus: Abstract of the thesis. dis. … Dr. med. Sciences: 14.01.01. - Obstetrics and gynecology. - K., 2007. - 31 p.
28. Poluyanova O. M. Optimization of pregravid training in women with a scar on the mat after caesarean section: Dis. … cand. honey. Sciences: 14.01.01. – Obstetrics and gynecology // NMAPE. - K., 2015. - 135 p. nine0003
M. Optimization of pregravid training in women with a scar on the mat after caesarean section: Dis. … cand. honey. Sciences: 14.01.01. – Obstetrics and gynecology // NMAPE. - K., 2015. - 135 p. nine0003
29. Wu S. Abnormal placentation: Twenty-year analysis / S. Wu, M. Kocherginsky, J. U. Hibbard // Am. J. Obstet Gynecol. - 2005. - Vol. 192, Issue 5. - R.1458-1461. https://doi.org/10.1016/j.ajog.2004.12.074; PMid:15902137
30. Kaelin A. A. The clinical outcome of cesarean scar pregnancies implanted “on the scar” versus “in the niche”/ A. A. Kaelin, G. Cali, A. Monteagudo [et al.] // Am. J. Obstet. Gynecol. –2017. –216:510.e.1-6.
31. Roberge S. Impact of single- vs double-layer closure on adverse outcomes and uterine scar defect: a systematic review and metaanalysis / S. Roberge, S. Demers, V. Berghella [et al.] // American Journal of Obstetrics & Gynecology. –2014. – Vol. 211, Issue 5. - P.453-460. https://doi.org/10.1016/j.ajog.2014.06.014; PMid:24912096
32. Macones G. A. Clinical outcomes in VBAC attempts: what to say to patients? / G. A. Macones // American Journal of Obstetrics & Gynecology. – 2008 – https://doi.org/10.1016/j.ajog.2008.03.040.
Macones G. A. Clinical outcomes in VBAC attempts: what to say to patients? / G. A. Macones // American Journal of Obstetrics & Gynecology. – 2008 – https://doi.org/10.1016/j.ajog.2008.03.040.
33. Arikan I. Cesarean section with relative indications versus spontaneous vaginal delivery: short-term outcomes of maternofetal health / I. Arikan, A. Barut, M. Harma [et al.] // Clinical And Experimental Obstetrics & Gynecology. - 2012. - Vol. 39, no. 3. – P. 288–292.PMid:23157026
34. Metz T. Validation of vaginal birth after cesarean prediction model in women with two prior cesarean deliveries / T. Metz, A. Allshouse, W. Grobman // American Journal of Obstetrics & Gynecology. – 2015.–Vol. 212.-Issue 1.-R.74.
35. Bujold E. An innovative scoring system to counsel patients with a prior cesarean delivery: a step towards a safer and more successful trial of labor / E. Bujold, R. Gauthier // Am. J. Obstet. Gynecol. - 2003. - Vol.189, Issue 6, Supplement. – Page S139. https://doi. org/10.1016/j.ajog.2003.10.284
org/10.1016/j.ajog.2003.10.284
36. Krasnopolsky V. I. Reproductive problems of the operated uterus / V. I. Krasnopolsky, L. S. Logutova, S. N. Buyanova. - M., 2015. - 160 p.
37. Goncharuk N. P. Diagnosis of impossibility of the scar on the mother after caesarean section (Review of the literature) / N. P. Goncharuk, N. R. Covida // Women's health. - 2016. - No. 7. - P.171-173.
38. Mardy A. H. prediction model of vaginal birth after cesarean in the preterm period / A. H. Mardy, C. V. Ananth, W. A. Grobman, C. Gyamfi-Bannerman // Am. J. Obstet. Gynecol. – 2016.–Vol. 214. - Issue 1. - R. 198-S199. https://doi.org/10.1016/j.ajog.2015.10.393
39. Miller E. Does midtrimester cervical length aid in predicting vaginal birth after cesarean? / E. Miller, A. Sakowicz, E. Donelan, W. Grobman // American Journal of Obstetrics & Gynecology. - 2015. - Vol. 212, Issue 1. - R. 75-S76. https://doi.org/10.1016/j.ajog.2014.10.162
40. Khatib N. New model, based on cervical length, predicts successful VBAC / N. Khatib, M. Emad, R. Beloosesky [et al.] // American Journal of Obstetrics & Gynecology. –2015. –Vol. 212, Issue 1, Supplement. – P. S195–196.
Khatib, M. Emad, R. Beloosesky [et al.] // American Journal of Obstetrics & Gynecology. –2015. –Vol. 212, Issue 1, Supplement. – P. S195–196.
41. Elkousyi M. Mothers with macrosomic fetuses should not be discouraged from vaginal dirth after cesarean section / M. Elkousyi, D. Marchiano, S. Parry [et al] // Am. J. Obstet. Gynecol. - 2001. -Vol. 185. - No. 6. -SMFM Abstracts. -R. 209.
42. Erfani H.TOLAC success in twin pregnancies in the United States (2013-2015) / H. Erfani, C. Davidson, M. Gandhi [et al.] // Am. J. Obstet. Gynecol. - 2018. - Vol. 218, Issue 1, Supplement. - P. S148. https://doi.org/10.1016/j.ajog.2017.10.154 nine0003
43. Silver R. K. Predictors of vaginal delivery in patients with a previous cesarean section, who require oxytocin / R. K. Silver, R. S. Gibbs // American Journal of Obstetrics & Gynecology. - 1987. - Vol. 156, Issue 1. - P. 57-60. https://doi.org/10.1016/0002-9378(87)
-X
44. Son M. Attempted operative vaginal delivery versus repeat cesarean in the second stage in women undergoing a trial of labor after cesarean / M. Son, A. Roy, W. A. Grobman // American Journal of Obstetrics & Gynecology. - 2017. -Vol. 216, Issue 1. - P. 68-S69. https://doi.org/10.1016/j.ajog.2016.11.984
Son, A. Roy, W. A. Grobman // American Journal of Obstetrics & Gynecology. - 2017. -Vol. 216, Issue 1. - P. 68-S69. https://doi.org/10.1016/j.ajog.2016.11.984
45. Maggio L. Association of Montevideo units with uterine rupture in women undergoing a trial of labor after cesarean delivery / L. Maggio., J. Forbes, H. Sangi-Haghpeykar, C. Davidson // Am. J. Obstet. Gynecol. – Jan, 2012, suppl. – R. 296. https://doi.org/10.1016/j.ajog.2011.10.680
46. Gabidullina R.I. Clinical and morphological parallels in the assessment of the state of the scar on the uterus after cesarean section / R.I. Gabidullina, I.F. Fatkullin, A.P. Kiyasov [et al.] // Kazan Medical Journal. - 2002. - T. 83, No. 6. - S. 424-429.
47. Nezhdanov I.G. Some aspects of uterine rupture along the scar after cesarean section / I.G. Nezhdanov, R.V. Pavlov, V.A. Aksenenko, I.V. Telegina // Medical Bulletin of the North Caucasus. - 2012. - No. 2. - P. 82–83.
48. Harper L. M. Association of induction of labor and uterine rupture in women attempting vaginal birth after cesarean: a survival analysis / L.