What is a neonatal unit
What is neonatal care? | Bliss
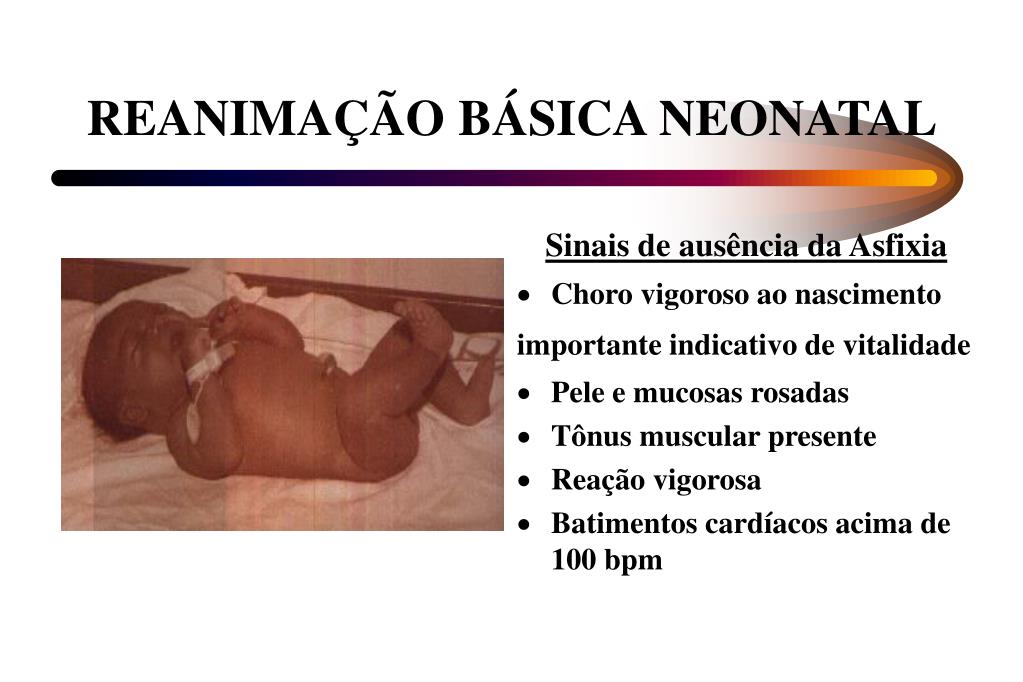
Neonatal care is the type of care a baby born premature or sick receives in a neonatal unit.
Units are a part of hospitals which provide care for babies who are born prematurely (before 37 weeks’ gestation), with a medical condition which needs treatment, or at a low birthweight.
The word ‘neonatal’ means newborn, or the first 28 days of life.
Over 90,000 babies are born premature or sick and needing neonatal care in the UK each year. That is one in seven babies, or around 250 babies every day.
We know that having a baby in neonatal care is likely to bring up a whole range of emotions, and some of these can be hard to face.
It may be that you feel anxious about why your baby has been born prematurely or sick, or about the treatment they are receiving. The team of health professionals can give you more information about your baby’s condition and the needs they have.
I found not holding my twin boys very difficult.
Deborah, mum to Nathaniel and AlexanderI found it helpful to tell myself that I was their mum. Whilst medical care was vital, no one knew or loved my babies like I did.
Why is my baby in neonatal care?
Babies are admitted into neonatal care for many different reasons. The main reasons for a baby to be admitted are:
- they are born prematurely
- they have a low birth weight
- they have a specific medical condition which needs treatment in hospital
Sometimes, the cause of premature birth or a medical condition will not be known, and you will not know exactly why this has happened to you.
You can always talk about why this might have happened at postnatal check-ups, with your midwife, or with a member of the neonatal staff on the unit.
What is a premature birth?
A baby who is born before 37 weeks of pregnancy will be called a premature baby. The neonatal team have different words for different levels of premature birth. They may also use the word ‘preterm’ to talk about your baby being born early.
The neonatal team have different words for different levels of premature birth. They may also use the word ‘preterm’ to talk about your baby being born early.
There are different ways of describing a premature birth.
- Term = A baby that has spent at least 37 weeks inside the womb (gestation)
- Preterm = A baby born before 37 weeks’ gestation
- Moderate to late preterm = A baby born between 32 and 37 weeks’ gestation
- Very preterm = A baby born between 28 and 32 weeks’ gestation
- Extremely preterm = A baby born at or before 28 weeks’ gestation
What does low birth weight mean?
Babies who are born small may need to spend time in the neonatal unit. You might hear the staff use these words if your baby has a low birthweight.
There are different ways of describing a low birthweight.
- Low birth weight = Born weighing less than 2500g (5lbs)
- Very low birth weight = Born weighing less than 1500g (3lbs)
- Extremely low birth weight = Born weighing less than 1000g (2lbs)
Remember
You need to register your baby's birth.
How are medical conditions treated in the neonatal unit?
Neonatal units treat a number of medical conditions.
This can include problems found before your baby was born. These might be conditions which are carried in your family (called genetic or inherited conditions) or where your baby has developed in an unusual or different way in the womb (called congenital conditions).
Your baby may have a condition because they were born early, or if they were born at term. The staff will give you information about your baby’s medical condition, but if you ever want to know more, you can ask them. They will be happy to talk to you about any questions you might have.
NHS Choices have useful pages with lots of conditions explained. You can search via nhs.uk
You are not alone
Take a look at our stories and features about babies born premature or sick, their families and the health professionals who care for them.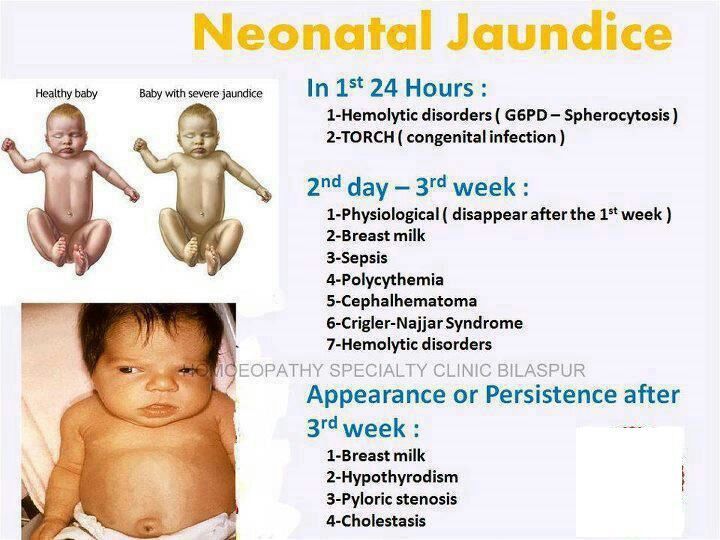
Read more
Want information about neonatal care for multiples? Visit Twins Trust's website, and download their neonatal guide for twin, triplets and more.
Related content
The information in this section is due for review May 2021
What are the different levels of neonatal care?
It can be confusing to understand your baby’s level of care. Here, we talk about the different levels of care neonatal units provide.
Why are there different levels of neonatal care?
There are different types of neonatal units in the NHS, and they are named depending on the level of specialist care they offer. Have a look at the section below to find out more about different types of unit.
Have a look at the section below to find out more about different types of unit.
Babies admitted to a neonatal unit get care according to what they need, and this care may change during the time they spend in hospital.
It is possible that your baby might have to be moved (often called ‘transferred’) to another hospital. You might also have been moved to a different hospital before your baby was born. This might not always be the hospital that is closest to your home, or where your baby was born.
However, staff will be specially trained to look after your baby. Take a look at our page on transfers for more information.
Special care baby unit (SCBU, sometimes called low dependency)
This is for babies who do not need intensive care. Often, this will be for babies born after 32 weeks’ gestation.
Care can include:
- Monitoring their breathing or heart rate
- Giving them more oxygen
- Treating low body temperature
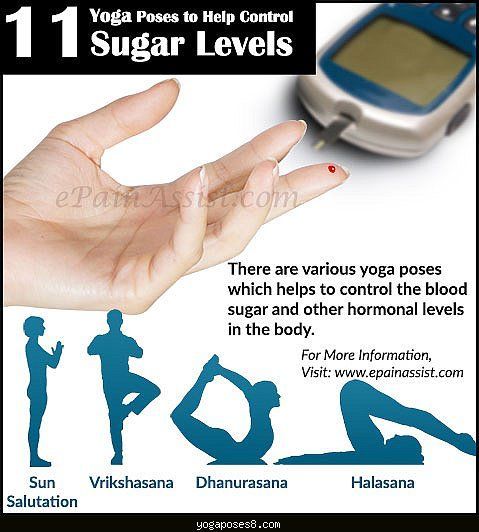
- Treating low blood sugar
- Helping them feed, sometimes by using a tube
- Helping babies who become unwell soon after birth
Sometimes, a baby might be admitted to a special care baby unit for phototherapy to treat jaundice.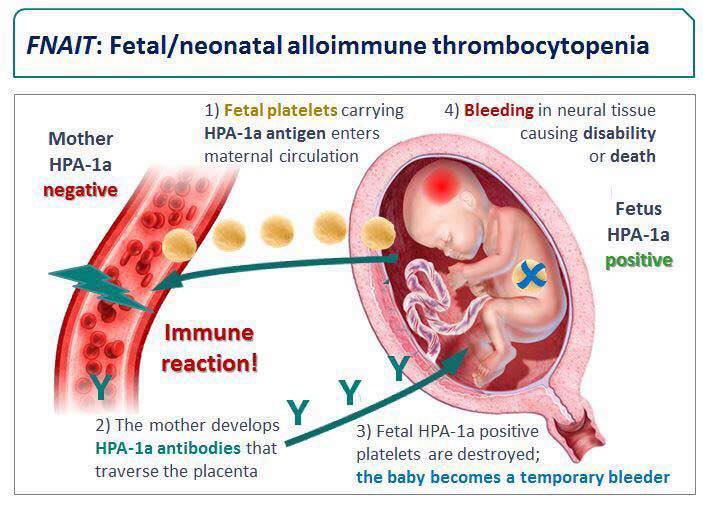 But sometimes, this condition is treated in transitional or postnatal care (see below).
But sometimes, this condition is treated in transitional or postnatal care (see below).
Local neonatal unit (LNU)
Babies who need a higher level of medical and nursing support are cared for here. If your baby was or will be born between 28 and 32 weeks’ gestation you may be transferred to an LNU.
Care on an LNU might include:
- Breathing support given through their windpipe (called ventilation)
- Short-term intensive care
- Care during short periods where they stop breathing (called apnoea)
- Continuous positive airway pressure (called CPAP) or high flow therapy for breathing support
- Feeding through a drip in their vein (called parenteral nutrition)
- Cooling treatment for babies who have had difficult births or are unwell soon after birth (before being transferred to a neonatal intensive care unit – see below)
- Helping babies who become unwell soon after birth
Neonatal intensive care unit (NICU)
This is the level of care for babies with the highest need for support. Often these babies will have been born before 28 weeks’ gestation, or be very unwell after birth.
Often these babies will have been born before 28 weeks’ gestation, or be very unwell after birth.
You might have been transferred to a different hospital which has a neonatal intensive care unit before your baby was born. This is usually because the staff feel your baby would benefit from this level of care, but that it is safer to transfer your baby before they are born.
Babies are cared for here when they:
- Need breathing support given through their windpipe (called ventilation)
- Have severe disease affecting their breathing (called respiratory disease)
- Need or have just had surgery
At a neonatal intensive care unit, all levels of care may also be given to babies from the local area.
Our friends at the Cambridge University Hospitals Trust and Rosie Maternity and Neonatal Voices Partnership have made a video about NICU, especially aimed at big brothers and sisters that helps to explain what NICU is.
Transitional care
This is where you and your baby stay together in hospital whilst you and the team care for your baby.
It means your baby is well enough to stay with you, either in the postnatal ward or a room on the neonatal unit, with support from the hospital staff. You will be in the hospital for 24 hours a day.
Some babies born between 32 and 37 weeks’ gestation, or babies with mild jaundice or feeding problems, get the care they need in this way.
I'm confused by the different levels of neonatal care
It can be confusing to understand your baby’s level of care.
Sometimes babies might be treated in different types of units because their condition has changed. It might not be clear straight away what type of care your baby is getting.
For example, your baby could be in a neonatal intensive care unit, but getting special care. You can always ask the staff if you want more information about the level of care your baby is getting.
You might hear staff on the unit call the different levels of care by different names than we've used here. Have a look through our neonatal words for some other ways people talk about levels of care.
Related content
Neonatology Department No. 1 - Children's Clinical Hospital named after Z.A. Bashlyaeva
Neonatology department No. 1 for newborns provides medical and diagnostic assistance to children with various neurological, somatic, infectious, cardiovascular and endocrinological pathologies coming from maternity hospitals, the intensive care unit of the hospital.
Opportunities DGKB them. BEHIND. Bashlyaeva allow to provide multidisciplinary medical care to newborn children, which allows to carry out a full range of examinations at the optimal time, clarify the diagnosis and prescribe adequate therapy, receive specialized consultations from leading specialists in various fields for the diagnosis and treatment of diseases of the neonatal period. nine0005
The department is designed for 30 beds. The wards for children available in the department are designed for 1-2 children, which creates an optimal treatment regimen for nursing sick children.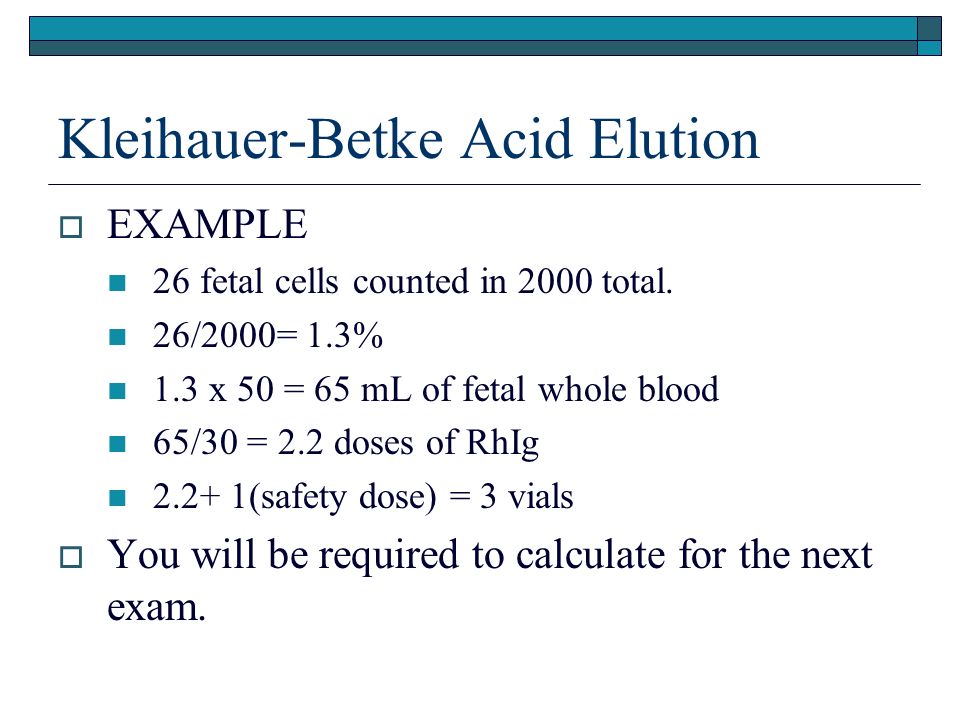
The department employs specialists of the highest qualification category - specially trained medical and nursing staff, providing round-the-clock qualified assistance to sick newborns.
All doctors of the department have special training in pediatrics, neonatology, the neonatal period, and endocrinology. nine0005
All nurses in the department are specialized in newborn care.
Consultations in the department are held jointly with Professor Zaplatnikov A.L. - Department of Pediatrics RMAPE, Professor Samsonova L.N. - Department of Endocrinology RMAPO, Professor Zykov V.P. - Department of Neurology and their staff, cardiologists of the hospital - Professor Sharykin A.S. , Professor Kotlukova N.P. , Professor Trunina I.I.
Treatment and all manipulations are carried out directly in the boxes. Care and medical manipulations are carried out by a specially trained nurse. Feeding is also carried out in boxes. In the department, in accordance with the recommendations of WHO and the Ministry of Health of the Russian Federation, events "In support of breastfeeding" are carried out. Feeding methods depend on the condition of the sick child, his illness, which was the reason for hospitalization. The mode of feeding is selected individually. Even without being in the department with the child, the mother can pass the expressed milk to him. Milk is taken daily from 8.00 to 10.00 at the checkpoint of the main entrance to the hospital. nine0005
Feeding is also carried out in boxes. In the department, in accordance with the recommendations of WHO and the Ministry of Health of the Russian Federation, events "In support of breastfeeding" are carried out. Feeding methods depend on the condition of the sick child, his illness, which was the reason for hospitalization. The mode of feeding is selected individually. Even without being in the department with the child, the mother can pass the expressed milk to him. Milk is taken daily from 8.00 to 10.00 at the checkpoint of the main entrance to the hospital. nine0005
For adequate nursing of newborns, the department has created conditions for both round-the-clock and daytime stay of a mother with a child.
While in the department, the mother participates in the feeding of the child, his bathing, which is carried out daily, learns the peculiarities of caring for her child.
The department conducts classes at the "School of Mothers", about the principles of breastfeeding, methods of care and features of the further development of a newborn child who has undergone various diseases in the neonatal period. nine0005
nine0005
Parents who have received a child's birth certificate are required to provide copies of the birth certificate and temporary health insurance policy to the department. Registration is carried out at the place of actual residence of the parents.
During the period of stay in the department, the mother must have: changeable shoes (not made of cloth), a dressing gown or dress, a tracksuit, a scarf on her head, socks or stockings, a nightgown, a towel, toiletries and hygiene products.
Newborns are hospitalized in a planned manner by agreement with the doctors of maternity hospitals, hospitals by phone: 8 (495) 496-66-04.
For the mother's hospitalization in the department, a good state of health is required, a ready-made result of a stool test for the intestinal group, copies of the passport and medical insurance.
Information about the child's health can be received directly from the attending physician on Monday, Wednesday and Friday from 12-30 min.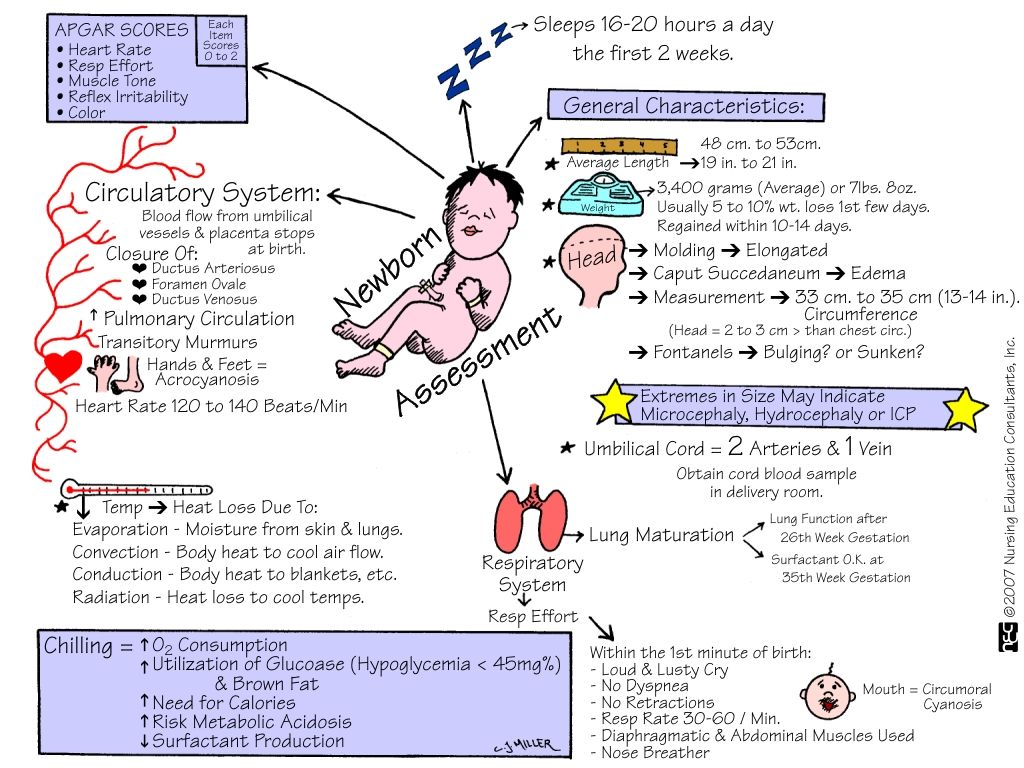 up to 13-30 min. in the department. nine0005
up to 13-30 min. in the department. nine0005
If you have any questions, please contact the head of the department Yudina Anastasia Evgenievna from 10-00 to 16-00 daily (except weekends and holidays) by phone 8 (495) 496-66-04, 8 (916) 120 -17-21
Contact center phone: 8-495-539-24-73
Visits hours: from 13.00 to 14.00, 19.00 to 20.00
Department
90,000 Neonatological department No. 2-DGKB named after Z.A. Bashlyaeva Neonatology Department No. 2 provides treatment and care for babies born with a pathology that does not allow them to be discharged home immediately, or those born prematurely and having a low body weight. We accept children from maternity hospitals, pathology departments of the Perinatal Centers and the Ort Department of our hospital. Since 2014, the department has been dealing with neonatal cardiology at the stage of preoperative preparation of newborns with complex combined CHD and drug therapy for various cardiac pathologies.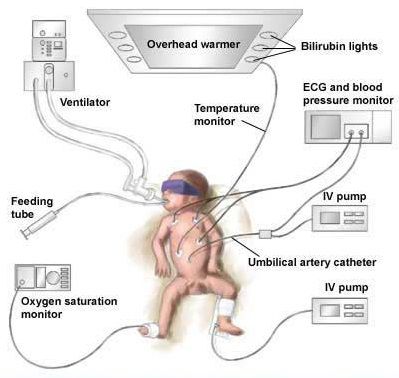 nine0005
nine0005
The department is designed for 22 beds with mothers and children, with various types of pathologies:
- Perinatal CNS lesions, including cerebral hemorrhages, hydrocephalus, malformations and lesions of peripheral nerves
- Respiratory diseases
- Diseases of the cardiovascular system: congenital heart disease, arrhythmias
- Hemolytic disease of the newborn, hyperbilirubinemia of various origins
- Diseases of the gastrointestinal tract
- Prematurity
- Anemia of various origins
- Intrauterine infections
- Intrauterine growth retardation and postnatal malnutrition
- Genetic syndromes, etc.
When examining children, modern research methods (laboratory, functional and radiation diagnostics) are used: The department has its own ultrasound diagnostic room. And, what is very important, all examinations (EEG, ECG, physiotherapy, phototherapy) are done at the child's bedside in the department ”(freshly expressed) milk, and in the absence of milk from the mother, an artificial mixture is individually selected.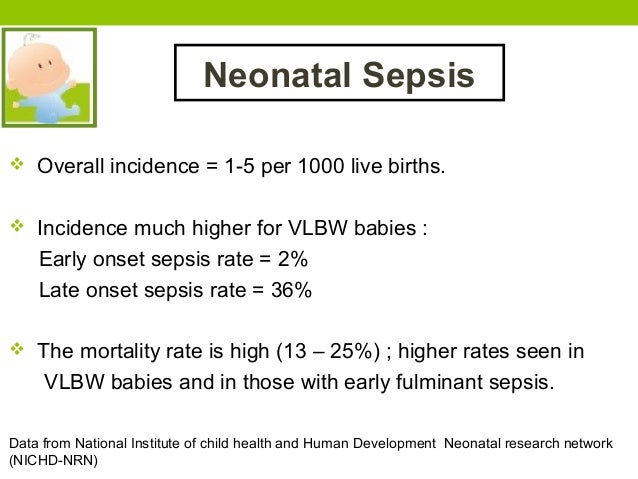 nine0005
nine0005
When nursing premature babies, the "kangaroo" method is actively used - contact "skin to skin", which improves the neuro-reflex activity of the child, stimulates the sucking reflex. All this increases the emotional stability of the mother and child. There is an increase in lactation in the mother and a faster adaptation of a premature baby to the conditions of extrauterine life.
There is continuity in further treatment and observation in the department: a child can be discharged home under the supervision of a district pediatrician, can be transferred to one of the departments of the hospital for aftercare: premature babies weighing up to 1500 g at birth are attached to the Rehabilitation Treatment Center for observation and rehabilitation, children with cardiac pathology continue to be monitored at the KDPO of our hospital. nine0005
In the department, we do not just allow parents to visit the child, but we try to actively involve the family in caring for the child.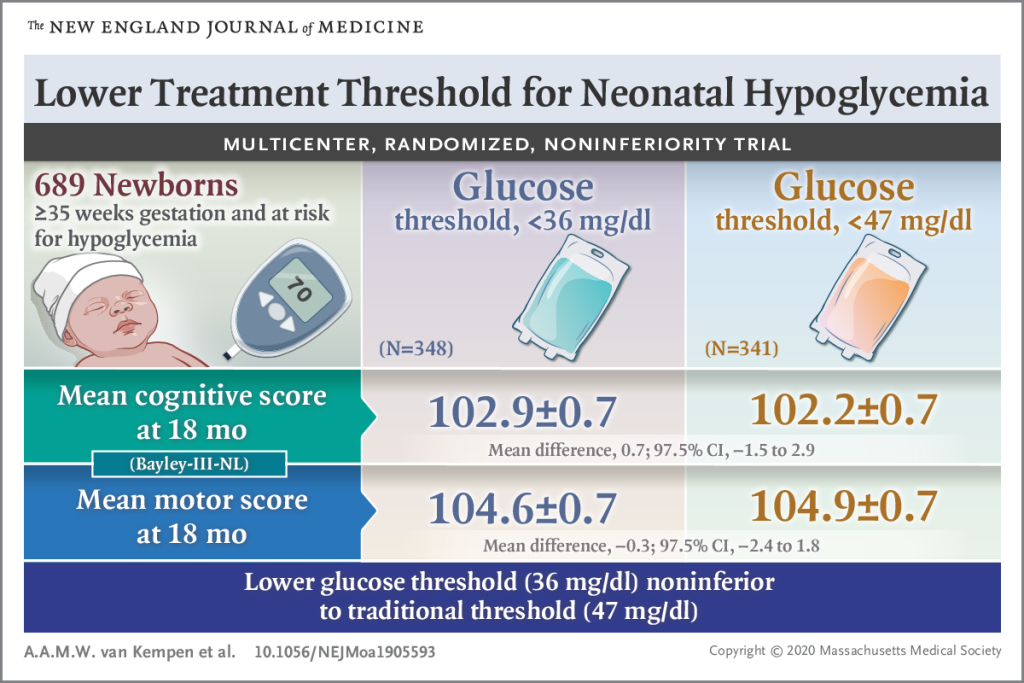 Parents communicate with their baby, take him in his arms, use tactile contact, which has a positive effect on the treatment of a sick child. The mothers of our patients can stay in our department around the clock or from 8:00 to 19:00 - (day hospital) only after passing the necessary tests. For hospitalization of the mother, it is necessary to pass tests for the intestinal group (Salmonella, Shigella). Hospitalization is carried out daily, the day of hospitalization is determined by the attending physician. With any visit option, the mother can feed the baby, take a direct part in caring for him, if his state of health allows it! In the Department for Newborns and Premature Babies, the "School of Mothers" is held, where classes are held with an active discussion about the principles of breastfeeding, care methods and features of the further development of our difficult babies. The department is equipped with multifunctional equipment (incubator with servo control, monitors, infusion pumps, phototherapy lamps, thermosystems) that allow performing VMP for nursing children with VLBW.
Parents communicate with their baby, take him in his arms, use tactile contact, which has a positive effect on the treatment of a sick child. The mothers of our patients can stay in our department around the clock or from 8:00 to 19:00 - (day hospital) only after passing the necessary tests. For hospitalization of the mother, it is necessary to pass tests for the intestinal group (Salmonella, Shigella). Hospitalization is carried out daily, the day of hospitalization is determined by the attending physician. With any visit option, the mother can feed the baby, take a direct part in caring for him, if his state of health allows it! In the Department for Newborns and Premature Babies, the "School of Mothers" is held, where classes are held with an active discussion about the principles of breastfeeding, care methods and features of the further development of our difficult babies. The department is equipped with multifunctional equipment (incubator with servo control, monitors, infusion pumps, phototherapy lamps, thermosystems) that allow performing VMP for nursing children with VLBW.