What causes fetal distress
Fetal distress | Pregnancy Birth and Baby
beginning of content4-minute read
Listen
Fetal distress is a sign your baby isn’t coping with labour. It might mean they need closer monitoring and possibly a caesarean to speed up the birth.
What is fetal distress?
Fetal distress is a sign that your baby is not well. It happens when the baby isn’t receiving enough oxygen through the placenta.
If it’s not treated, fetal distress can lead to the baby breathing in amniotic fluid containing meconium (poo). This can make it difficult for them to breathe after birth, or they may even stop breathing.
Fetal distress can sometimes happen during pregnancy, but it’s more common during labour.
What causes fetal distress?
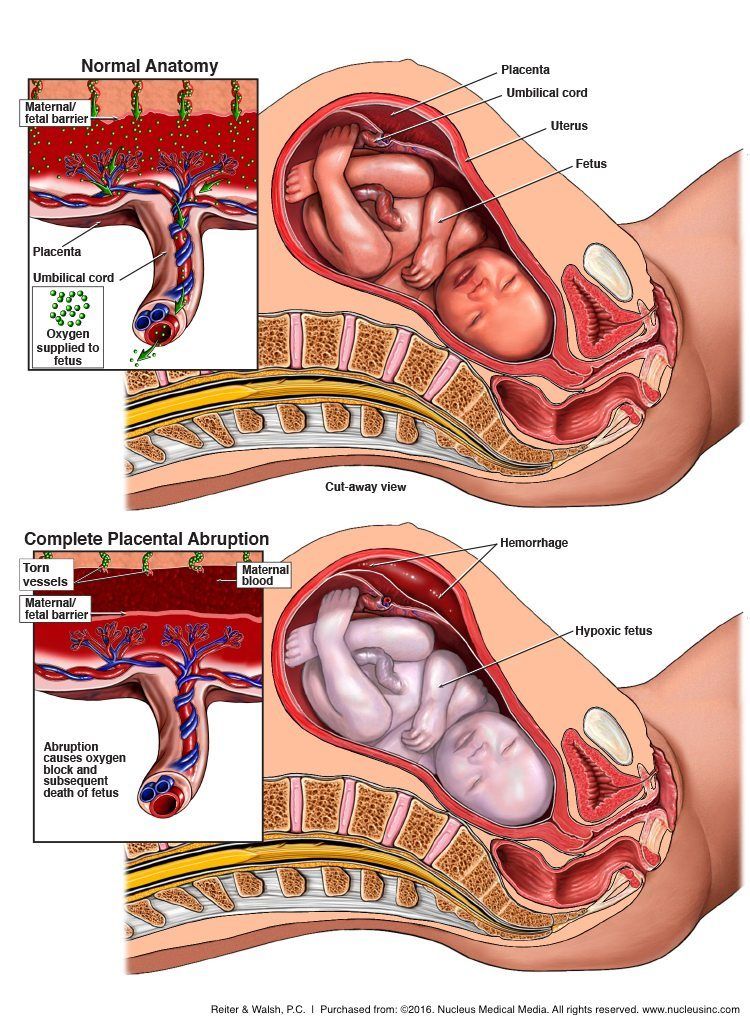
The most common cause of fetal distress is when the baby doesn’t receive enough oxygen because of problems with the placenta (including placental abruption or placental insufficiency) or problems with the umbilical cord (for example, if the cord gets compressed because it comes out of the cervix first).
Fetal distress can also occur because the mother has a health condition such as diabetes, kidney disease or cholestasis (a condition that affects the liver in pregnancy).
It is more common when pregnancy lasts too long, or when there are other complications during labour. Sometimes it happens because the contractions are too strong or too close together.
You are more at risk of your baby experiencing fetal distress if:
- you are obese
- you smoke
- you have high blood pressure in pregnancy or pre-eclampsia
- you have a chronic disease, such as diabetes or kidney disease
- you have a multiple pregnancy
- your baby has intrauterine growth restriction
- you have had a stillbirth before
How is fetal distress diagnosed?
Fetal distress is diagnosed by reading the baby’s heart rate. A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
Sometimes fetal distress is picked up when a doctor or midwife listens to the baby’s heart during pregnancy.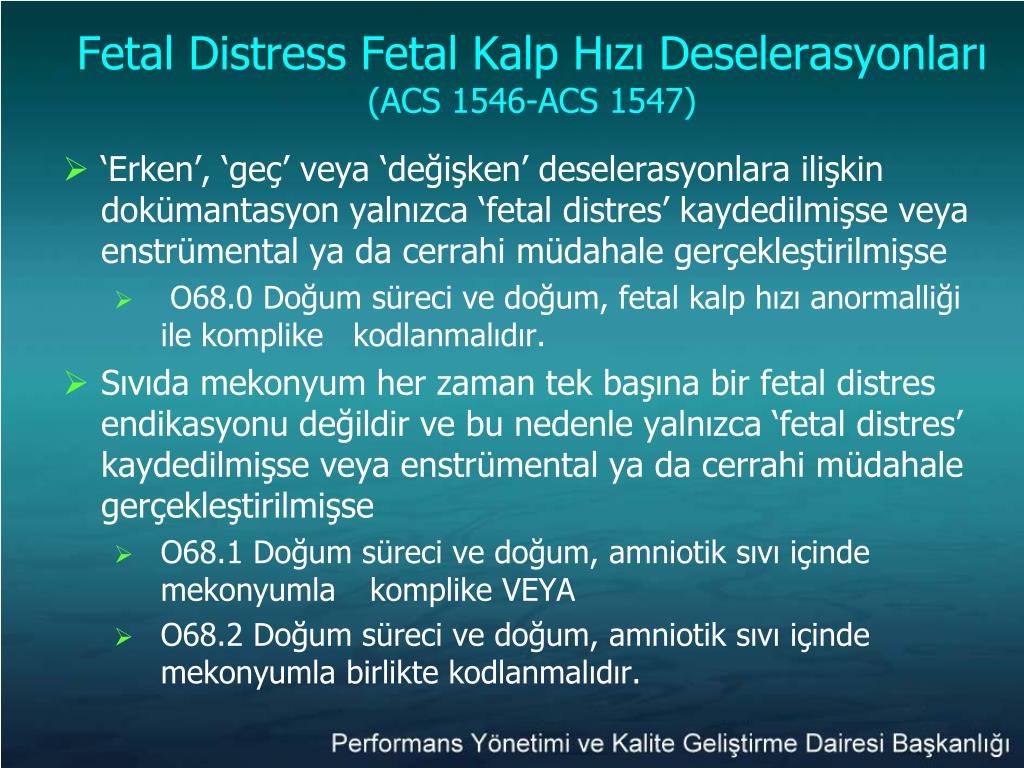 The baby’s heart rate is usually monitored throughout the labour to check for signs of fetal distress.
The baby’s heart rate is usually monitored throughout the labour to check for signs of fetal distress.
Another sign is if there is meconium in the amniotic fluid. Let your doctor or midwife know right away if your notice the amniotic fluid is green or brown since this could signal the presence of meconium.
How is fetal distress managed?
The first step is usually to give the mother oxygen and fluids. Sometimes, moving position, such as turning onto one side, can reduce the baby’s distress.
If you had drugs to speed up labour, these may be stopped if there are signs of fetal distress. If it’s a natural labour, then you may be given medication to slow down the contractions.
Sometimes a baby in fetal distress needs to be born quickly. This may be achieved by an assisted (or instrumental) delivery which is when the doctor uses either forceps or ventouse (vacuum extractor) to help you deliver the baby, or you might need to have an emergency caesarean.
Does fetal distress have any lasting effects?
Babies who experience fetal distress, such as having an usual heart rate or passing meconium during labour, are at greater risk of complications after birth.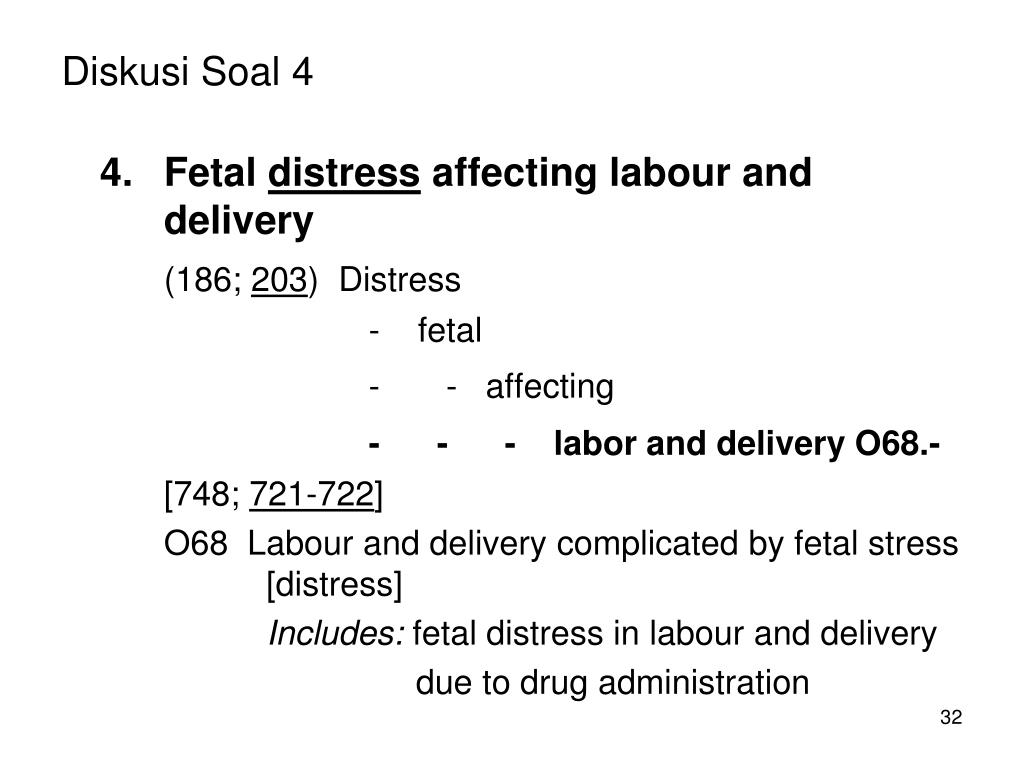 Lack of oxygen during birth can lead to very serious complications for the baby, including a brain injury, cerebral palsy and even stillbirth.
Lack of oxygen during birth can lead to very serious complications for the baby, including a brain injury, cerebral palsy and even stillbirth.
Fetal distress often requires birth by caesarean section. While this is a safe operation, it carries extra risks to both the mother and baby, including blood loss, infections and possible birth injuries.
Babies born with an assisted delivery can also be at greater risk of short-term problems such as jaundice, and may have some difficulty feeding. Having lots of skin-to-skin contact with your baby after the birth and breastfeeding can help reduce these risks.
You won’t necessarily experience fetal distress in your next pregnancy. Every pregnancy is different. If you’re worried about future pregnancies, it can help to talk to your doctor or midwife so they can explain what happened before and during the birth.
Women whose labour didn’t go to plan often feel quite negative about their birth experience.
If you feel sad or disappointed or traumatised about what happened, it is important to talk to someone.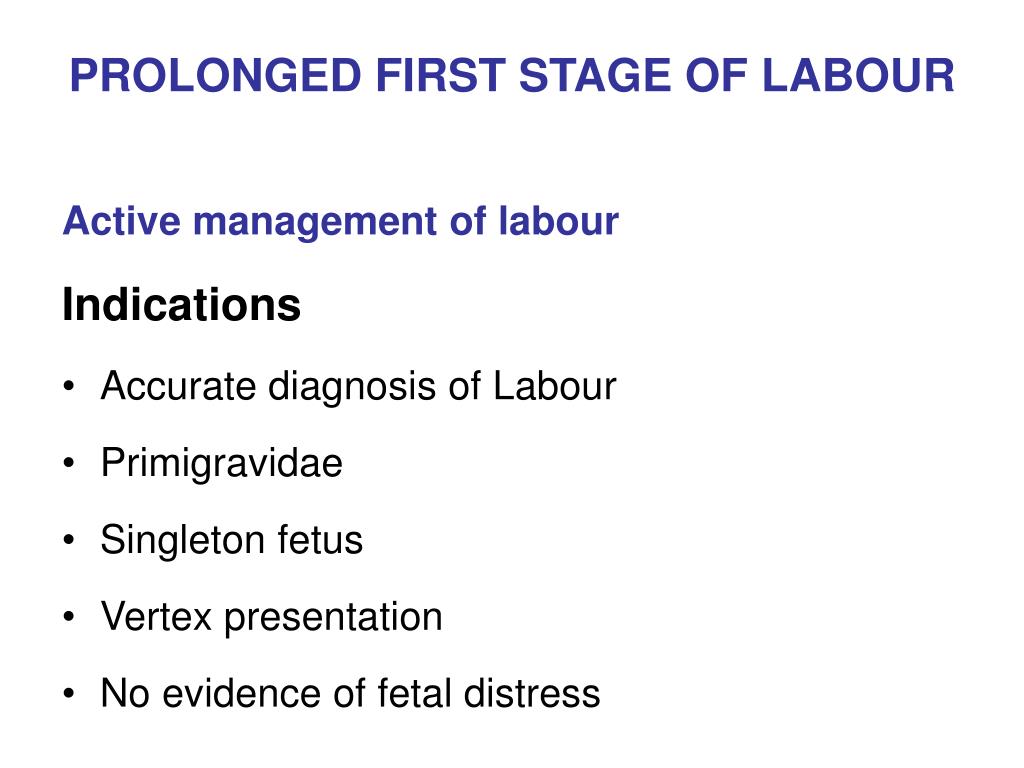 You can contact or talk to a range of people and organisations, including:
You can contact or talk to a range of people and organisations, including:
- Your doctor
- PANDA on 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blue on 1300 22 4636
- Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436
Sources:
Australian Family Physician (Decreased fetal movements: a practical approach in primary care setting), Australasian Birth Trauma Association (What is birth trauma?), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Provision of routine intrapartum care in the absence of pregnancy complications), Birth (The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age), MSD Manual (Fetal distress), Kidspot (All about foetal distress), King Edward Memorial Hospital (Fetal compromise), Journal of Translational Medicine (Reducing the risk of fetal distress with sildenafil study)Learn more here about the development and quality assurance of healthdirect content.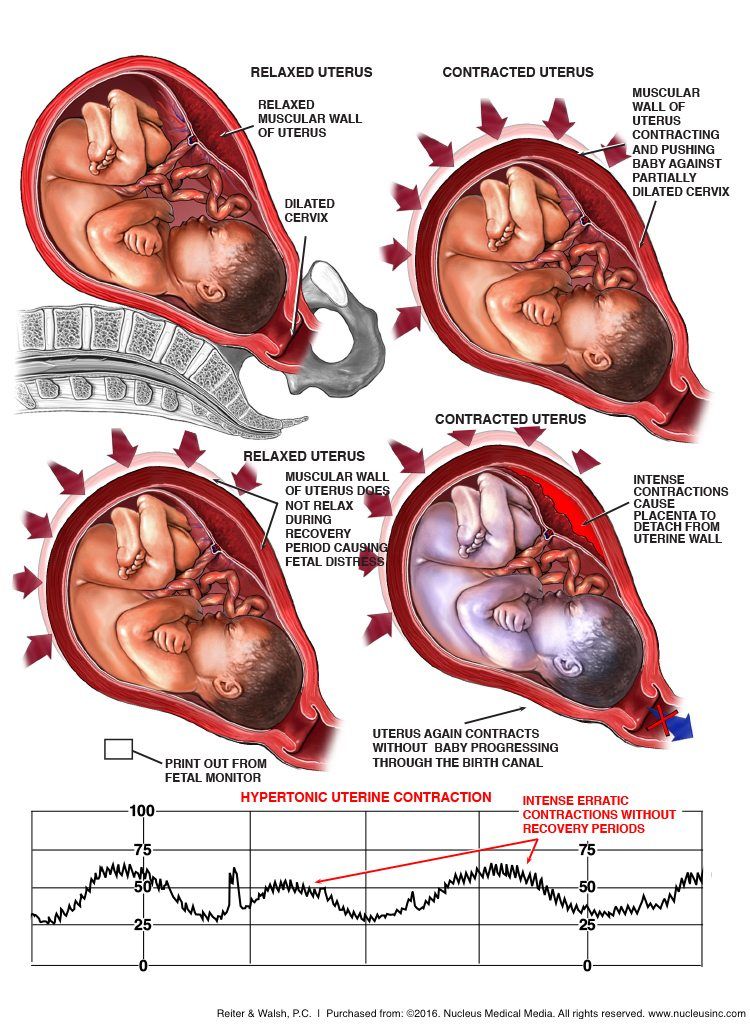
Last reviewed: January 2020
Back To Top
Related pages
- Labour complications
- Interventions during labour
- Induced labour
- Giving birth - stages of labour
- Fetal heart rate monitoring
- Baby movements during pregnancy
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fetal Distress - American Pregnancy Association
Historically, the term fetal distress has been used to describe when the fetus does not receive adequate amounts of oxygen during pregnancy or labor. It is oftentimes detected through an abnormal fetal heart rate. However, while the term fetal distress is commonly used, it is not well defined.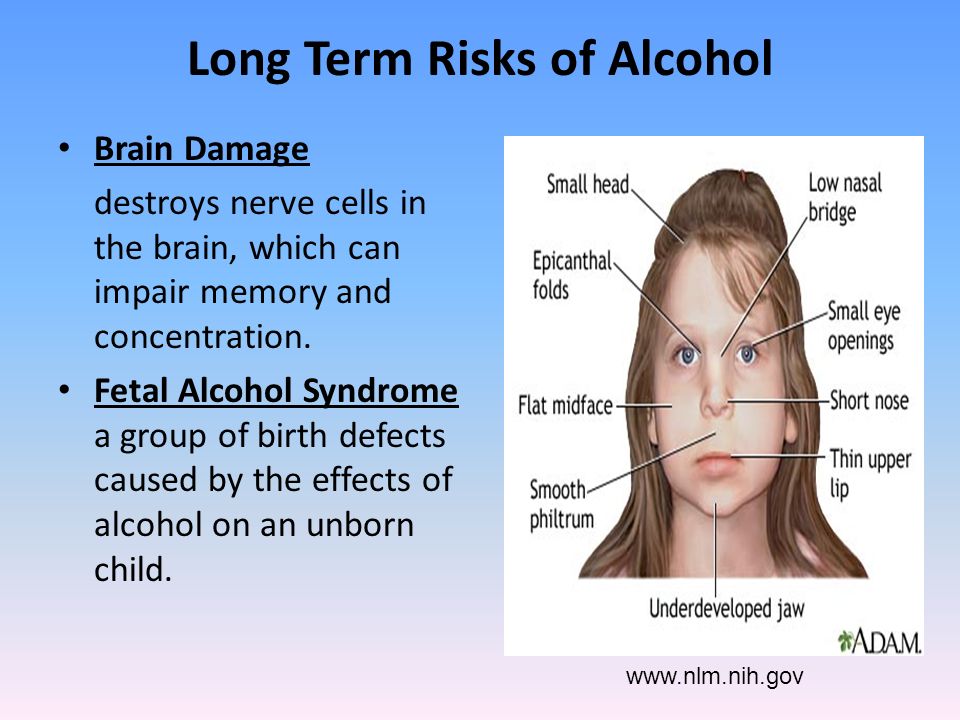 This makes it more difficult to make an accurate diagnosis and provide proper treatment. Because of the term’s ambiguity, its use has the potential to lead to improper treatment.
This makes it more difficult to make an accurate diagnosis and provide proper treatment. Because of the term’s ambiguity, its use has the potential to lead to improper treatment.
Fetal distress is commonly confused with the term birth asphyxia. Birth asphyxia occurs when the baby does not have adequate amounts of oxygen before, during, or after labor. This may have multiple causes, some of which include low oxygen levels in the mother’s blood or reduced blood flow due to compression of the umbilical cord.
As many have incorrectly used fetal distress and birth asphyxia as interchangeable terms, the Committee on Obstetric Practice of the American Congress of Obstetricians and Gynecologists (ACOG) has expressed concern regarding the use of the two terms. ACOG recommends that the term fetal distress be replaced with “non-reassuring fetal status.”
Along with this new term, ACOG further recommends physicians add to the diagnosis a list of additional findings such as fetal tachycardia, bradycardia, repetitive variable decelerations, low biophysical profile, and late decelerations. ACOG’s Committee on Obstetric Practice has also stated that the term birth asphyxia should no longer be used as it is too vague of diagnosis for medical use.
ACOG’s Committee on Obstetric Practice has also stated that the term birth asphyxia should no longer be used as it is too vague of diagnosis for medical use.
Fetal Distress Diagnosis
It is important for physicians to monitor the fetus throughout pregnancy to detect any potential complications. One of the more widely used methods of monitoring is electronic fetal heart rate (FHR) monitoring.
Benefits of FHR monitoring include:
- The ability to recognize the development of hypoxia (when the fetus does not receive adequate amounts of oxygen) by analyzing patterns in the fetal heart rate
- The ability to monitor the mother’s contractions
- The ability to monitor the response of the fetus to hypoxia
- A more positive outcome for high-risk deliveries
Nonetheless, FHR monitoring does come with risks as well, including an increased likelihood of having a cesarean section due to misinterpretation of FHR monitoring results.
Conditions Behind Fetal Distress
Potential precursors to fetal distress or non-reassuring fetal status may include:
- Anemia (the most prevalent obstetric condition seen behind non-reassuring fetal status)
- Oligohydraminos (a condition in which there is a lower level of amniotic fluid around the fetus)
- Pregnancy Induced Hypertension (PIH)
- Post-term pregnancies (42 weeks or more)
- Intrauterine Growth Retardation (IUGR)
- Meconium-stained amniotic fluid (a condition in which meconium, a baby’s first stool, is present in the amniotic fluid which can block fetal airways)
Treatment
The primary treatment used for non-reassuring fetal status is intrauterine resuscitation. This will help prevent any unnecessary procedures.
Some means of intrauterine resuscitation include:
- Changing the mother’s position
- Ensuring the mother is well-hydrated
- Ensuring the mother has adequate oxygen
- Amnioinfusion (the insertion of fluid into the amniotic cavity to alleviate compression of the umbilical cord)
- Tocolysis (a therapy used to delay preterm labor by temporarily stopping contractions)
- Intravenous hypertonic dextrose
Nonetheless, there are cases in which an emergency cesarean section is necessary.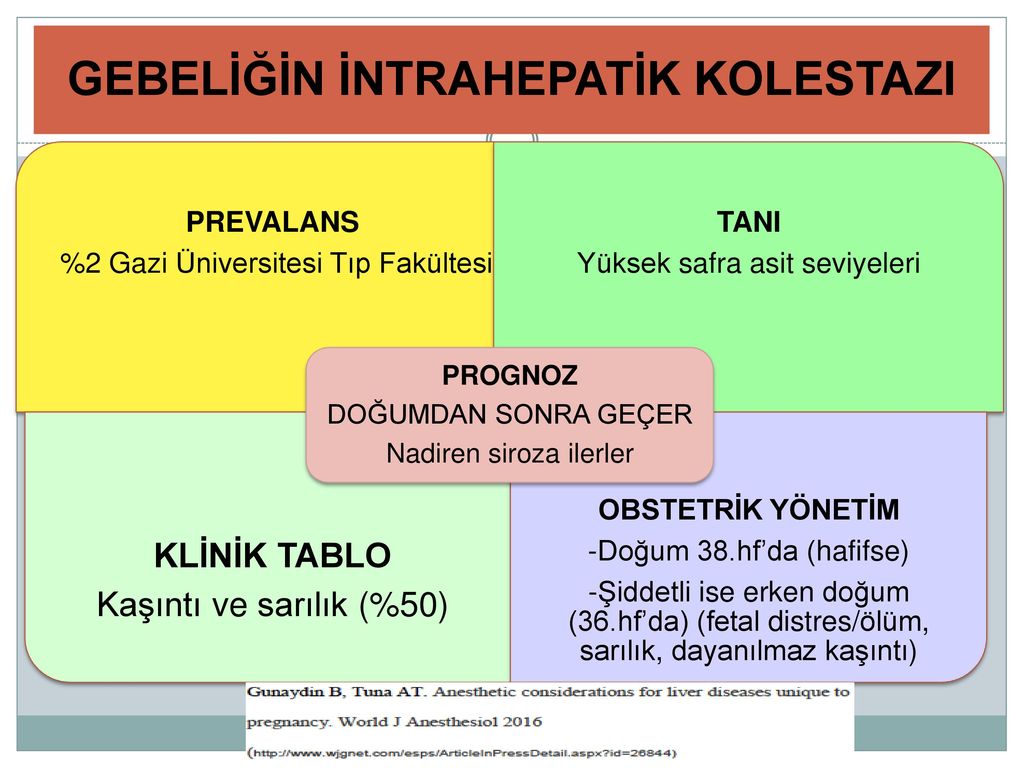 However, due to the over-diagnosis of fetal distress and potential misinterpretation of the fetal heart rate, it is recommended to confirm a potential fetal distress diagnosis with a fetal blood acid-base study. Overall, this condition points to the importance of prenatal care and proper monitoring of the mother and fetus throughout pregnancy.
However, due to the over-diagnosis of fetal distress and potential misinterpretation of the fetal heart rate, it is recommended to confirm a potential fetal distress diagnosis with a fetal blood acid-base study. Overall, this condition points to the importance of prenatal care and proper monitoring of the mother and fetus throughout pregnancy.
Want to Know More?
- Most Common Pregnancy Complications
- What is a High-Risk Pregnancy?
Compiled from the following References:
ACOG Committee on Obstetric Practice. (2005). Inappropriate use of the terms of fetal distress and birth asphyxia. Committee Opinion, 326.
Beckmann, C. R. B., Ling, F. W., Barzansky, B. M., Herbert, W. N. P., Laube, D. W., & Smith, R. P. (2010). Obstetrics and gynecology (6th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Bucklin, B. A., Gambling, D. R., & Wlody, D. J. (2009). A practical approach to obstetric anesthesia. Gravlee, G. P. (Ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Gravlee, G. P. (Ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Kaur, J., & Kaur, K. (2012). Conditions behind fetal distress. Annals of Biological Research, 3(10). Retrieved from https://scholarsresearchlibrary.com/ABR-vol3-iss10/ABR-2012-3-10-4845-4851.pdf
Mayo Clinic. (2012). Biophysical profile: Why it’s done.
Merck Manuals. (n.d.) Fetal distress.
The American Congress of Obstetricians and Gynecologists (ACOG). (2013, October 22). Ob-gyns redefine the meaning of “term pregnancy.”
University of California San Francisco Benioff Children’s Hospital. (n.d.). Birth asphyxia. Retrieved from https://www.ucsfbenioffchildrens.org/conditions/birth_asphyxia/
Parete
Updated
Content:
Disocation of oxygen in the fetus during pregnancy
,Distress of the fetus during birth of
Causes management of childbirth
Consequences
Video
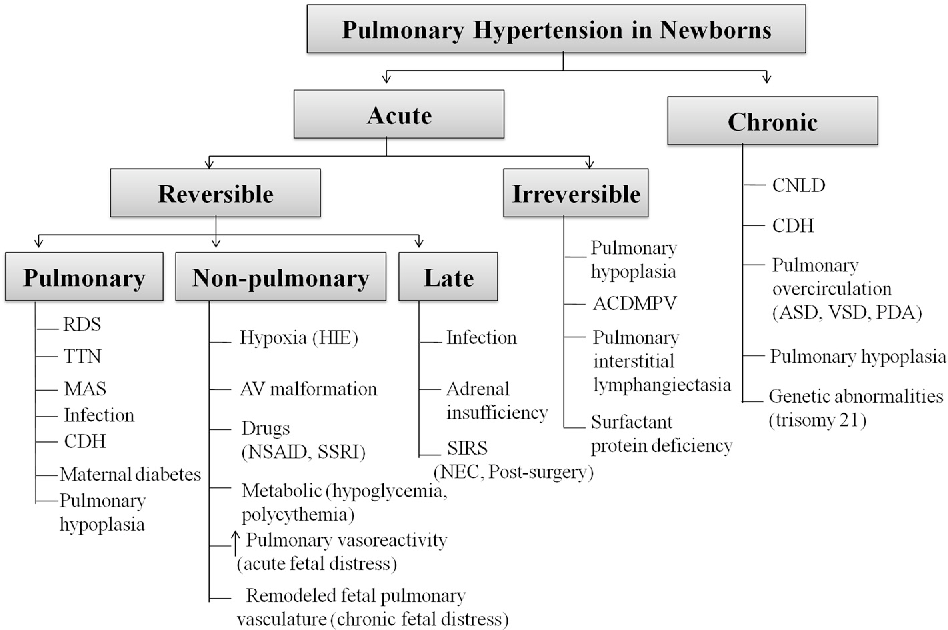
Fetal distress can occur both during pregnancy and during childbirth.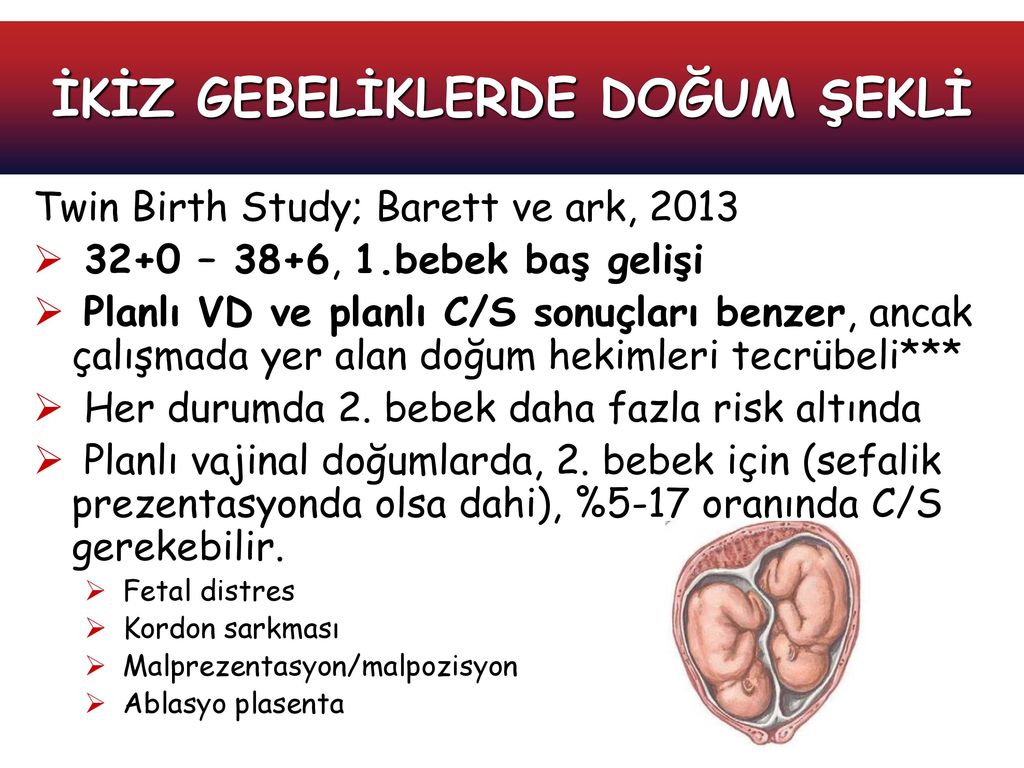 This general term refers to violations of the functional state of the fetus during pregnancy and / or childbirth. Separately, respiratory (respiratory) distress of the fetus associated with a lack of oxygen is isolated.
This general term refers to violations of the functional state of the fetus during pregnancy and / or childbirth. Separately, respiratory (respiratory) distress of the fetus associated with a lack of oxygen is isolated.
Fetal oxygen deficiency during pregnancy
Fetal position during pregnancyFetal distress is often synonymous with fetal hypoxia.
The mechanism of development of such a respiratory pathology is as follows:
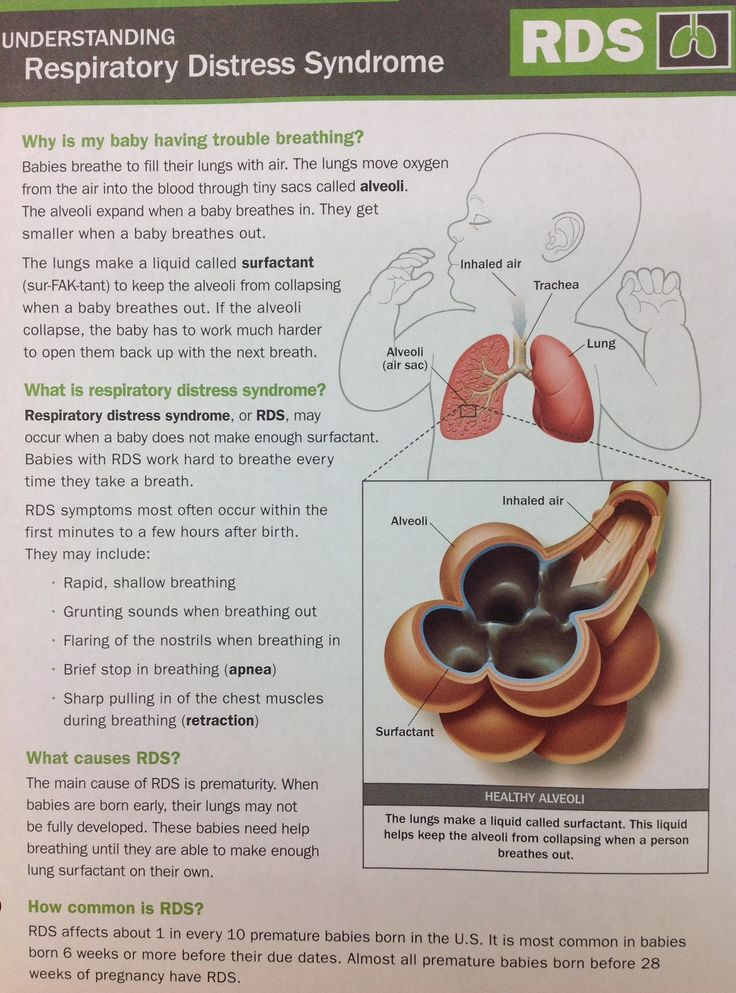
- The production of surfactant (a fluid that lubricates the alveoli) in the fetus begins after 20 weeks, and the respiratory system matures almost before the birth itself.
- In case of pathologies in the mother or problems during pregnancy, there may be a deficiency in the production of surfactant or its insufficient activity.
- Problems with surfactant lead to edema, reduced lung capacity in the child, and breathing problems.
The condition is diagnosed in several ways:
- Listening to cardiac activity.
 Manipulation is carried out starting from the 20th week of pregnancy, when the gynecologist can listen to the fetal heartbeat through the mother's stomach during regular examinations. The normal heart rate is considered to be 110-170 beats per minute. Deviation in the direction of increasing or decreasing the number of strokes may be a sign of oxygen deficiency.
Manipulation is carried out starting from the 20th week of pregnancy, when the gynecologist can listen to the fetal heartbeat through the mother's stomach during regular examinations. The normal heart rate is considered to be 110-170 beats per minute. Deviation in the direction of increasing or decreasing the number of strokes may be a sign of oxygen deficiency. - Biophysical profile assessment. The procedure is carried out from the 30th week of pregnancy and includes the evaluation of several indicators, each of which is estimated from 0 to 2 points. The resulting total value gives an understanding of the degree of development of the fetus and allows you to suspect violations in time. The following parameters are taken for evaluation: physical activity, respiration, cardiac activity, volume of amniotic fluid. An oxygen deprivation syndrome can be suspected with a score below 7 points.
- Doppler. Evaluation of blood flow makes it possible to evaluate the work of the placenta.
Pathological is a condition with slow blood flow, zero or reverse.
Fetal distress during birth
The process of childbirth is physically very difficult for both mother and baby. During the entire birth process, starting from admission to the hospital, doctors constantly monitor the condition of the child. To do this, they evaluate the heart rate and other parameters. It is very important to carefully and regularly monitor the child's condition in order to suspect hypoxia in a timely manner and take measures to save the baby's life.
Signs of oxygen deprivation during childbirth may include:
- heartbeat above 170 and below 110 beats per minute, except for the moment of uterine contraction;
- pathological color of amniotic fluid.
When in doubt, examinations are carried out in more detail, for which the heartbeat is heard with the help of auscultation, as well as cardiotocography.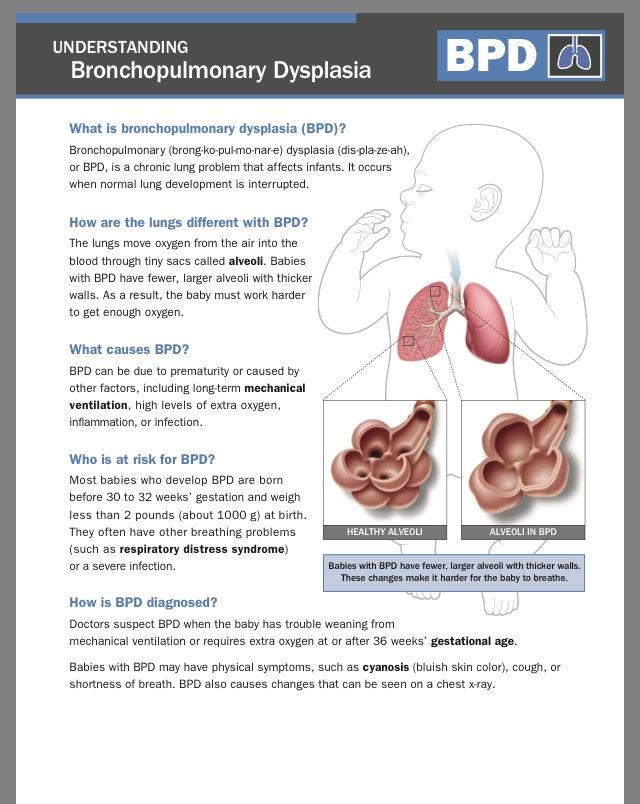 A significant deviation from the norm and diagnosed fetal hypoxia are an indication for emergency delivery. If the problem is discovered in the second stage of labor, a caesarean section becomes impossible, but the process of having a baby is accelerated. For this, a vacuum extraction of the fetus or the use of obstetric forceps is performed.
A significant deviation from the norm and diagnosed fetal hypoxia are an indication for emergency delivery. If the problem is discovered in the second stage of labor, a caesarean section becomes impossible, but the process of having a baby is accelerated. For this, a vacuum extraction of the fetus or the use of obstetric forceps is performed.
Such methods are quite risky and can have unpredictable consequences, so it is important to detect hypoxia in time and prevent its occurrence.
Causes of fetal distress and management of labor
Intrauterine hypoxia cannot be visually identified, so the condition is assessed by clinical signs. Emergency measures must be taken if the child's condition is dangerous for the development of persistent pathologies or can lead to death.
Oxygen deficiency can be triggered by the following intranatal factors:
- induction of labor if deemed necessary by the physician;
- preeclampsia
- prolonged delivery;
- meconium impurities;
- oligohydramnios.
Other triggers may be:
- maternal endocrine disorders;
- multiple pregnancy;
- presence of infection;
- Rhesus conflict.
If there is an abnormal heartbeat, the gynecologist may puncture the amniotic sac to assess the condition and color of the amniotic fluid. If they are stained with meconium, an emergency cesarean is performed.
If the mother's heartbeat is normal, but the fetus's is elevated in the absence of a contraction, this is a sure sign of hypoxia. To eliminate hypoxia, the following preventive measures can be used:
- stop oxytocin administration;
- put the woman on her left side;
- use an oxygen mask.
Extra fluid may also be given intravenously.
Consequences
Intranatal distress even in utero causes oxygen deficiency, metabolic acidosis and adversely affects the respiratory and nervous system of the child. After birth, these children have:
After birth, these children have:
- acute respiratory syndrome with respiratory failure;
- retraction of the chest on inspiration;
- cyanosis of the skin and mucous membranes, their blanching;
- crepitus.
To avoid serious consequences, doctors begin treatment immediately after the baby is born. Measures taken in the first hour can reduce the severity of manifestations, prevent disability and improve the quality of life of the baby.
Prophylaxis, if at risk, should be carried out throughout pregnancy. To do this, a woman may be prescribed drugs that improve oxygenation. It is important to visit the doctor in charge of the pregnancy in a timely manner and carefully follow his appointments.
Video
Read the following article: vacuum fruit extraction
* The information provided cannot be used for self-diagnosis, treatment determination and does not replace a visit to a doctor!
HeadingExaminations, analyzes
HCG during a missed pregnancy - does the hormone level change
The size of the uterus in women is normal
Small deeds done with great love turn into something great
Comments .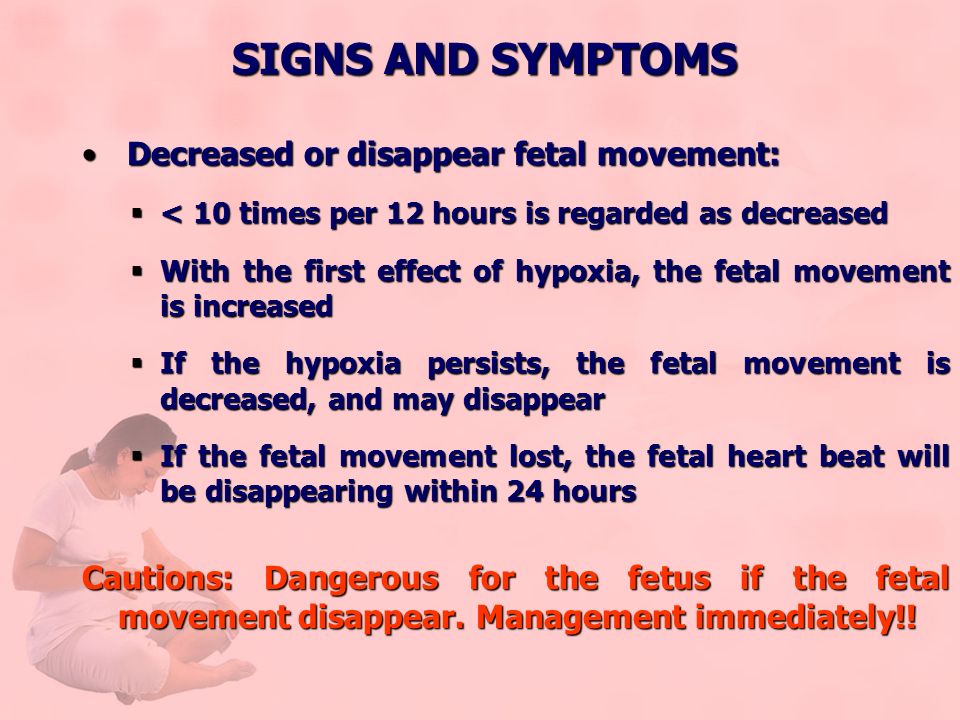 ru is a treasure trove of useful information
ru is a treasure trove of useful information
30 steps to strong immunity! Happiness - when everyone is healthy! New technologies in education How to help a child with a choice of profession? Safe Internet for a child Bullying at school: how to protect a child? with ARVIThe first first aid kit for a babyGallery of your baby's spots
Respiratory distress syndrome - how to diagnose pediatrician's advice
How to diagnose respiratory distress syndrome of a newborn: Respiratory distress syndrome of the newborn (RDS) occurs when the baby's lungs are not fully developed and cannot supply enough oxygen, causing difficulty in breathing. Primary diagnosis of respiratory distress syndrome of the newborn will require consultation with a therapist. As an additional examination based on the results of the examination, the doctor may prescribe:
- X-ray
- CT scan of the chest.
Quick navigation
This disease usually develops in premature babies.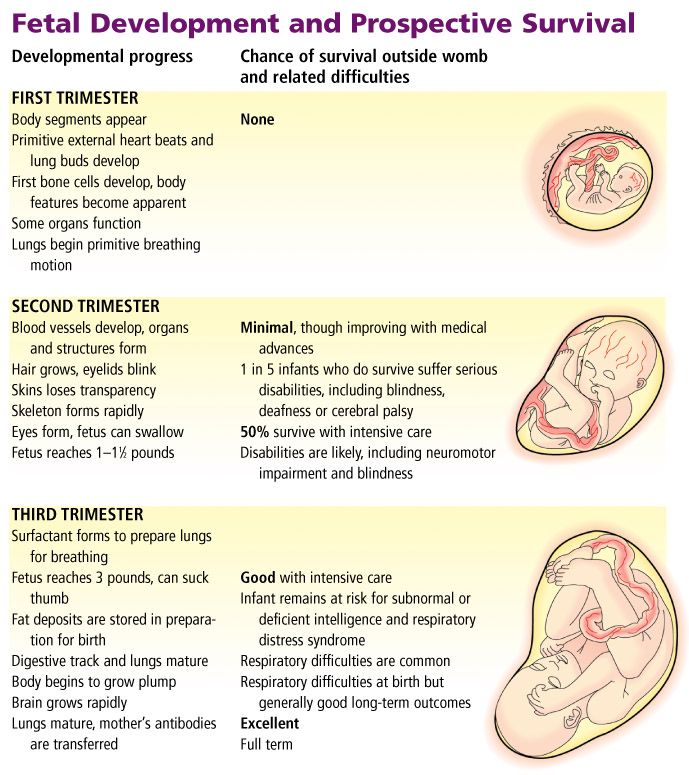 It is also known as childhood respiratory distress syndrome, hyaline membrane disease, or surfactant deficiency lung disease. Despite the similar name, respiratory distress syndrome is not related to acute respiratory distress syndrome.
It is also known as childhood respiratory distress syndrome, hyaline membrane disease, or surfactant deficiency lung disease. Despite the similar name, respiratory distress syndrome is not related to acute respiratory distress syndrome.
Causes of neonatal respiratory distress syndrome
Neonatal respiratory distress syndrome usually occurs when a baby's lungs do not produce enough surfactant, a protein and fat substance that helps maintain lung inflation and prevents them from collapsing. The fetal lungs usually start producing surfactant somewhere between 24 and 28 weeks of pregnancy. Most babies produce enough surfactant by 34 weeks to breathe on their own at birth at that time. If the baby is born earlier, then there is a high probability of insufficient production of surfactant. More often, respiratory distress syndrome affects premature babies, for example, when:
- mother has diabetes;
- the child is underweight;
- the child's lungs are not developing properly.

Approximately half of all babies born between 28 and 32 weeks of gestation develop this pathology. In recent years, the number of premature babies born with respiratory distress syndrome has decreased due to steroid injections that can be given to mothers at risk of preterm birth.
Symptoms of respiratory distress syndrome
Symptoms of neonatal respiratory distress syndrome are often noticeable immediately after birth and worsen over the next few days. These may include:
- newborn blue lips, fingers and toes;
- rapid, shallow breathing;
- flaring nostrils;
- grunting sound when breathing.
Diagnosis of respiratory distress syndrome
A number of tests are used to diagnose neonatal respiratory distress syndrome and rule out other possible causes. These include:
- physical examination;
- blood tests to measure the amount of oxygen in the child's blood and check for infection;
- pulse oximetry test to measure the amount of oxygen in a child's blood using a sensor attached to a finger, toe, or ear;
- X-ray or CT scan of the chest to determine the characteristic cloudy appearance of the lungs in distress syndrome.
Respiratory Distress Treatment
The main goal of treating respiratory distress syndrome is to help the child breathe.
Treatment before birth
If there is a high risk of preterm birth before 34 weeks of gestation, treatment for RDS can be started before delivery. For this, a single injection of steroids is performed, and then the second dose is administered 24 hours after the first. Steroids stimulate the development of the baby's lungs and the production of surfactant. Treatment is estimated to help prevent respiratory distress syndrome in a third of preterm births.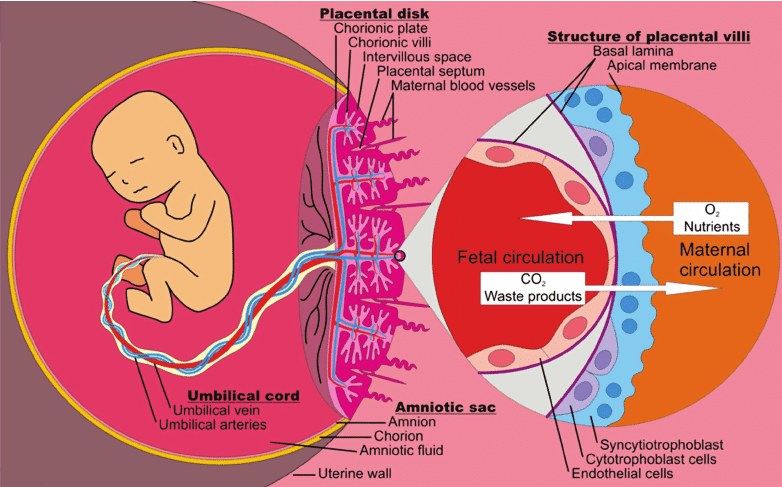 The patient may also be offered magnesium sulfate to reduce the risk of developmental problems associated with early birth. If the course of treatment with magnesium sulfate is more than 5-7 days or is carried out several times during pregnancy, then additional examinations may be offered to the newborn child. This is because long-term use of magnesium sulfate during pregnancy rarely leads to bone problems in newborns.
The patient may also be offered magnesium sulfate to reduce the risk of developmental problems associated with early birth. If the course of treatment with magnesium sulfate is more than 5-7 days or is carried out several times during pregnancy, then additional examinations may be offered to the newborn child. This is because long-term use of magnesium sulfate during pregnancy rarely leads to bone problems in newborns.
Postpartum care
A newborn with respiratory distress syndrome may be transferred to a specialized unit for premature babies (neonatal unit). If the symptoms are mild, he may only need supplemental oxygen. It is usually injected into the nose through an incubator or through a tube. If the symptoms are more severe, the child will be put on a breathing machine (ventilator) to either support or take over his breathing. These procedures are often started immediately in the delivery room before transfer to the neonatal unit. Also, a child with respiratory distress syndrome may be given a dose of artificial surfactant through a breathing tube. Evidence suggests that early treatment within 2 hours of delivery is more effective than if it is delayed. Distressed children will also be given fluids and food through a tube connected to a vein. Some will only need help with breathing for a few days, but some premature babies, usually born earlier, may need support for weeks or even months. The length of a baby's stay in the neonatal unit will depend on how early he was born and what his condition is.
Evidence suggests that early treatment within 2 hours of delivery is more effective than if it is delayed. Distressed children will also be given fluids and food through a tube connected to a vein. Some will only need help with breathing for a few days, but some premature babies, usually born earlier, may need support for weeks or even months. The length of a baby's stay in the neonatal unit will depend on how early he was born and what his condition is.
Complications of neonatal respiratory distress syndrome
Most infants with respiratory distress syndrome can be successfully treated, although they remain at an increased risk of developing other problems later in life.
Sometimes air can escape from the child's lungs and accumulate in the child's chest. This condition is called pneumothorax. The air pocket puts extra pressure on the lungs, causing them to collapse and leading to additional breathing problems. Air leaks can be repaired by inserting a tube into the chest to allow trapped air to escape.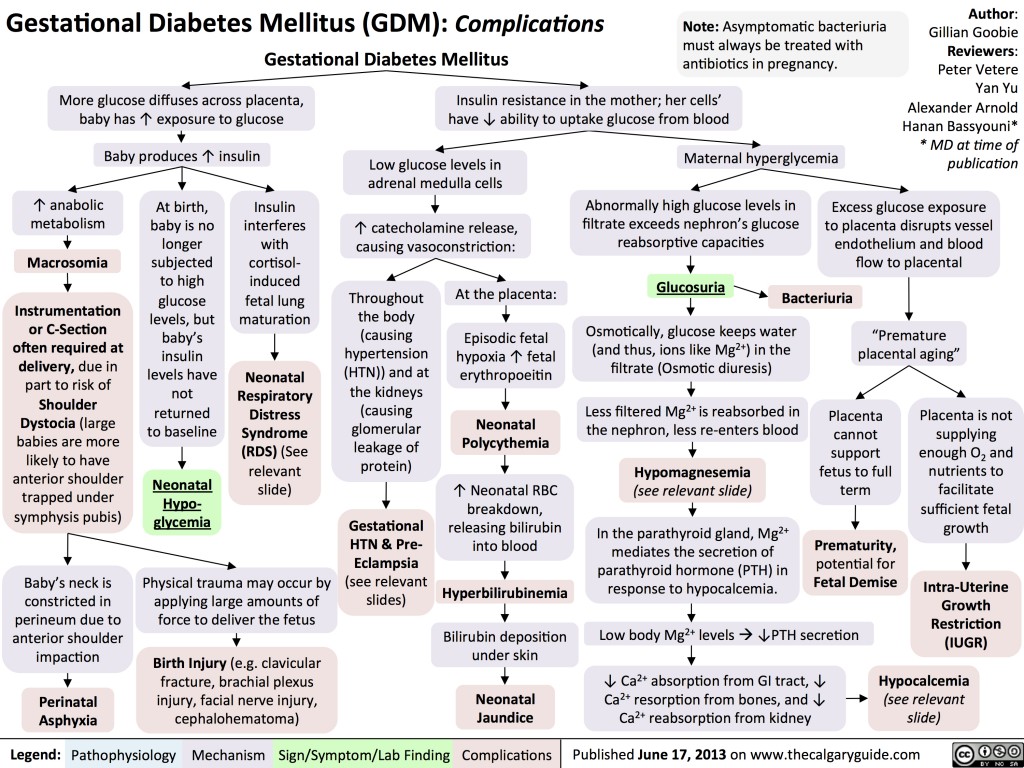
Distressed infants have a significantly increased risk of bleeding inside the lungs (pulmonary hemorrhage) and the brain (cerebral hemorrhage). Pulmonary bleeding is treated with air pressure from a ventilator to stop it and a blood transfusion. Cerebral hemorrhage is quite common in premature babies, but most bleeding is mild and does not cause long-term problems.
Occasionally, ventilation started within 24 hours of birth or a surfactant used to treat respiratory distress syndrome causes scarring of the baby's lungs, which affects their development. This complication is called bronchopulmonary dysplasia. Symptoms of dysplasia include rapid shallow breathing and shortness of breath. Babies with a severe complication like this usually need supplemental oxygen through their nose to help them breathe. Supplemental oxygen support is usually needed for several months while the lungs heal. But some children with bronchopulmonary dysplasia may need regular medications, such as bronchodilators, to widen the airways and make breathing easier.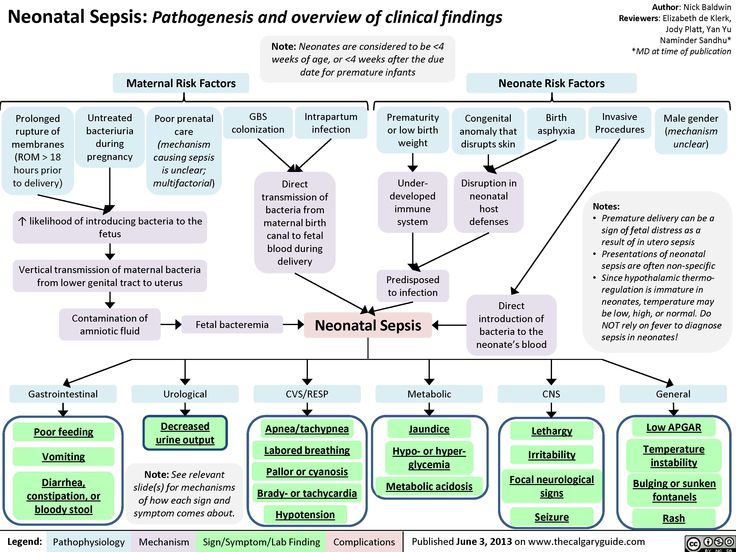
If a child's brain is damaged as a result of developing respiratory distress syndrome, either due to bleeding or lack of oxygen, all this can lead to long-term developmental disabilities such as learning difficulties, movement problems, hearing impairment and vision. But these developmental problems are usually not serious. For example, a study found that 3 out of 4 children with developmental problems have only mild disabilities, which should not prevent them from leading a normal adult life.
Author: Belyakov Nikolai Grigorievich
Specialization: Pediatrician
Where does the reception: Clinic General Medical Center (GMC), St. Petersburg
4.5+
Zakharova Victoria Valerievna
Specialization: Pediatrician
Medical experience: since 2016
Where does the reception: MC Baltmed Ozerki
Malina Valeria Aleksandrovna
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Baltmed Ozerki
Egorova Nina Alexandrovna
Specialization: Pediatrician
Medical experience: since 2011
Where does the reception: MC Baltmed Ozerki
Kovzalova Irina Sergeevna
Specialization: Pediatrician
Medical experience: since 2021
Where does the reception: MC Baltmed Ozerki
Pushkareva (Vinogradova) Irina Alekseevna
Specialization: Cardiologist, Pediatrician
Medical experience: since 2009
Place of admission: MC Baltmed Ozerki, Clinical Hospital No.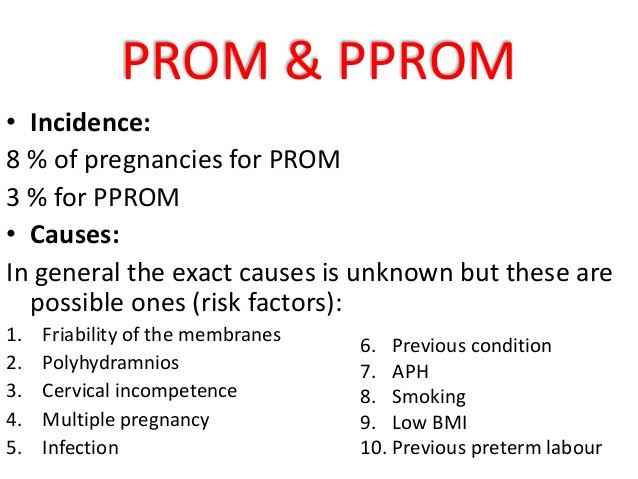 31, Medswiss Gakkelevskaya
31, Medswiss Gakkelevskaya
Bunyakova Elena Vladimirovna
Specialization: Pediatrician, Rheumatologist
Medical experience: since 2008
Where does the reception: MC Baltmed Ozerki
Strekalova Elena Vladimirovna
Specialization: Therapist, Pediatrician, General Practitioner
Medical experience: since 1999
Where does the reception: MC Baltmed Ozerki
Klimanova Darya Alexandrovna
Specialization: Pediatrician, Neonatologist, Allergist, Immunologist
Medical experience: since 2013
Where does the reception: MC Baltmed Ozerki
Tashtemirov Tokhirjon Makhamatvosilovich
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Medicenter
Normurodov Alisher Khusan ugli
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: Medicenter
Markov Anton Ivanovich
Specialization: Pediatrician
Medical experience: since 2011
Where does the reception: MC Medicenter
Babikova Daria Konstantinovna
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Medicenter
Kim Irina Efremovna
Specialization: Pediatrician
Medical experience: since 1985
Where does the reception: MC Medicenter
Egorova Victoria Alexandrovna
Specialization: Pediatrician
Medical experience: since 2016
Where does the reception: MC Medicenter
Anastasia Anatolyevna Voloshina
Specialization: Pediatrician
Medical experience: since 2020
Where does the reception: MC Medicenter
Budginayte Ksenia Alexandrovna
Specialization: Endocrinologist, Pediatrician
Medical experience: since 2018
Where does the reception: MC Medicenter, Children's Medical Center ONNI
Alla Belyakova
Specialization: Neurologist, Pediatrician, Reflexologist
Medical experience: since 1983
Where does the reception: MC Medicenter, MC Profimedica, MC Family Doctor
Bashmakova Elena Olegovna
Specialization: Pediatrician
Medical experience: since 2018
Where does the reception: Polikarpov Medical Center Medical Center
Anastasia Vasilievna Baramyka
Specialization: Pediatrician
Medical experience: since 2006
Where does the reception: MC Medicenter
Balkova Irina Anatolyevna
Specialization: Pediatrician
Medical experience: since 2013
Where does the reception: MC Medicenter
Radchenko Sergey Ivanovich
Specialization: Gastroenterologist, Pediatrician, General Practitioner
Medical experience: since 1989
Where does the reception: Polikarpov Medical Center Medical Center
Tarasova Rosina Vasilievna
Specialization: Neurologist, Ultrasound Doctor, Pediatrician
Medical experience: since 1990
Where does the reception: MC Medpomoshch 24 Zanevsky, Clinic Miracle Children
Abramova Elena Mikhailovna
Specialization: Pediatrician
Medical experience: from 1976 years old
Where does the reception: MC Energy of Health, MC Poem of Health
Bystritskaya Natalya Vladimirovna
Specialization: Pediatrician
Medical experience: since 1989
Where does the reception: MC Long Vita, Research Institute of Obstetrics and Gynecology.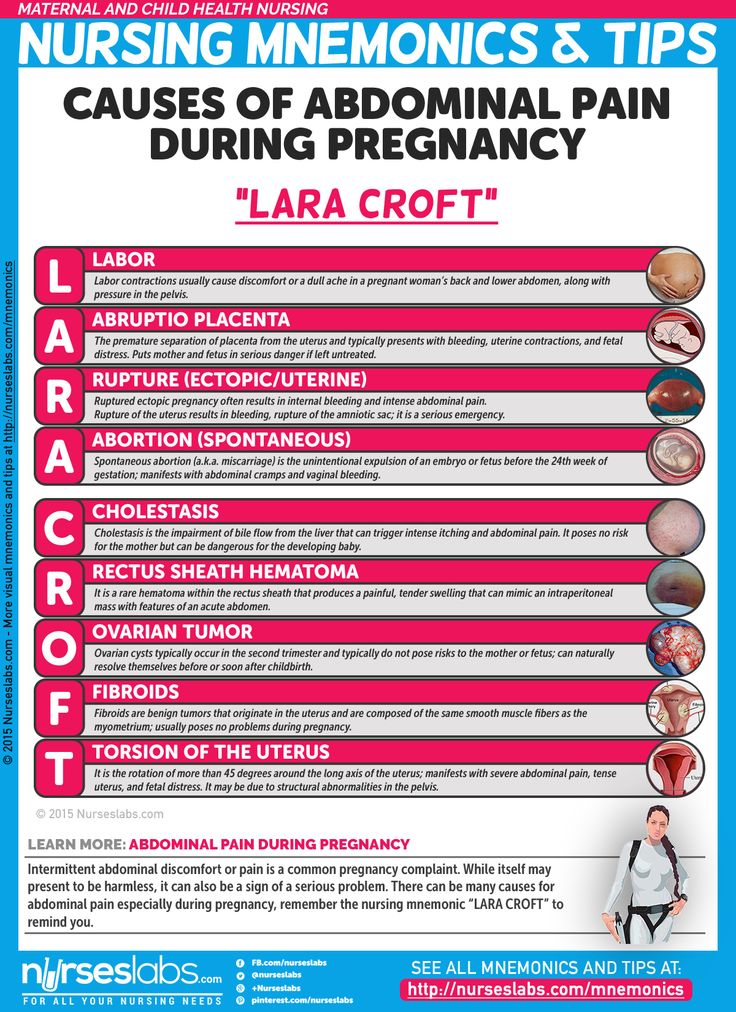 Otta
Otta
Bochkova Olga Yurievna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2006
Where does the reception: SM-Clinic on Vyborgsky
Khvatova Elena Anatolievna
Specialization: Ultrasound doctor, Gastroenterologist, Pediatrician
Medical experience: since 2006
Where does the appointment: SM-Clinic on Danube, SM-Clinic on Malaya Balkanskaya
Svechina Evgenia Alekseevna
Specialization: Gynecologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Danube
Lidia Alvinovna Nereutsa
Specialization: Pediatrician, Pulmonologist, Allergist, Immunologist
Medical experience: since 2003
Where does the reception: SM-Clinic on Danube
Borisova Daria Sergeevna
Specialization: Pediatrician, Pulmonologist
Medical experience: since 2016
Where does the reception: SM-Clinic on Vyborgsky
Laborer Ksenia Andreevna
Specialization: Pediatrician
Medical experience: since 2013
Where does the reception: SM-Clinic on Marshal Zakharov, Children's Clinic No.![]() 75
75
Olga V. Lashcheva
Specialization: Endocrinologist, Pediatrician
Medical experience: since 2003
Where does the reception: SM-Clinic on Udarnikov
Terekhova Olga Borisovna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Udarnikov
Mikhailova Victoria Evgenievna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Vyborgsky
Belotitskaya Valeria Eduardovna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2015
Where does the reception: SM-Clinic on Danube
Meshcheryakova Irina Fedorovna
Specialization: Cardiologist, Pediatrician
Medical experience: since 1999
Where does the reception: SM-Clinic on Udarnikov
Goltsman Kirill Efimovich
Specialization: Somnologist, Pediatrician, Functional diagnostics doctor, Epileptologist
Medical experience: since 2013
Where he receives: Clinic Osnova Children, Clinic of the Pediatric Academy
Tarasova Larisa Anatolyevna
Specialization: Gastroenterologist, Pediatrician, Nephrologist, Infectionist
Medical experience: since 1989
Where does the appointment: Dr. Pel's Clinic
Pel's Clinic
Ulyanova Inna Vladimirovna
Specialization: Hepatologist, Pediatrician, Pulmonologist, Infectionist
Medical experience: since 1990
Where does the appointment: Dr. Pel's Clinic
Kudryashova Maria Yurievna
Specialization: Cardiologist, Pediatrician, Doctor of functional diagnostics
Medical experience: since 1990
Where does the appointment: Dr. Pel's Clinic, MEDA Clinic, Children's Clinic No. 39
References:
- Grebennikov V.A. et al. Respiratory distress syndrome of newborns. Replacement therapy with synthetic surfactant Exosurf Neonatal. M. -1995. -S. 10-16, 54-69
- Bagdatiev V. E. Respiratory distress syndrome / V. E. Bagdatiev, V. A. Gologorsky, B. R. Gelfand // Vestn. intensive care. 1996. - No. 2. - S. 15-25.
- Kuzovlev A.N., Moroz V.V., Golubev A.M., Zarzhetsky Yu.V. Differential diagnosis of pneumonia and acute lung injury // Mat.
 All-Russian conference with international participation "Belomorsky Symposium III". 2009. Arkhangelsk. S. 81.
All-Russian conference with international participation "Belomorsky Symposium III". 2009. Arkhangelsk. S. 81. - Bochun O.N., Savello V.E., Zhidkov K.P. The role of computed tomography in the detection of pulmonary complications in traumatic disease / International Congress "Nevsky Radiological Forum-2005m: Materials of the Congress.-SPb.2005.-C.326.
- Tyurin I.E. Computed tomography of the chest cavity. S-PB., 2006.
Latest diagnostic articles
Lung transplant
Lung transplant is an operation to remove and replace a diseased lung with a healthy lung from a donor. The donor is usually a deceased person, but in rare cases, part of a lung may be taken from a living donor. Lung transplants are performed infrequently, mainly due to a lack of available donors as the demand for transplants far exceeds the available supply of donated lungs. This means that an organ transplant will only be performed if there is a relatively high chance of success.