What are the signs of stillbirth
Stillbirth symptoms and risks | Tommy's
We understand that reading about the symptoms of stillbirth can be very worrying during pregnancy. If you are struggling to manage anxious feelings or thoughts, please talk to your midwife about how you’re feeling. Your healthcare team is there to support you if you have any concerns about your and your baby's health. Please don’t worry about speaking up, asking questions and requesting further investigations.
Even if you do experience some of the symptoms or conditions listed below, please remember that you’re likely to go on to have a healthy pregnancy and baby.
If you’re looking for more information about what causes stillbirth, our information about the causes of stillbirth more helpful.
Baby’s movements in pregnancy
You may feel your baby move as early as 16 weeks of pregnancy, but most people usually feel something between 16 and 20 weeks, although it can sometimes be later than this.
If this is your first pregnancy, you may not notice your baby’s movements until you are more than 20 weeks pregnant. Movements feel different to everyone, but you might feel kicking, swirling, fluttering or rolling. It is not true that babies move less towards the end of pregnancy. You should continue to feel your baby move right up to the time you go into labour and during labour.
Every baby has its own pattern of movement – for example your baby may move more in the evenings when you are resting, or before you go to sleep at night. You may also find certain activities like taking a bath, putting your feet up and resting on the sofa, or eating and drinking seem to encourage your baby to move more.
As the weeks go on, you may notice a pattern of movements that becomes familiar to you. The movements usually become fairly regular by 28 weeks. Get to know your baby’s pattern of movements so you can notice any changes.
If a baby is not well, or not receiving enough nutrients and oxygen, they are likely to move less to save energy. Noticing when this happens and contacting your hospital immediately is very important.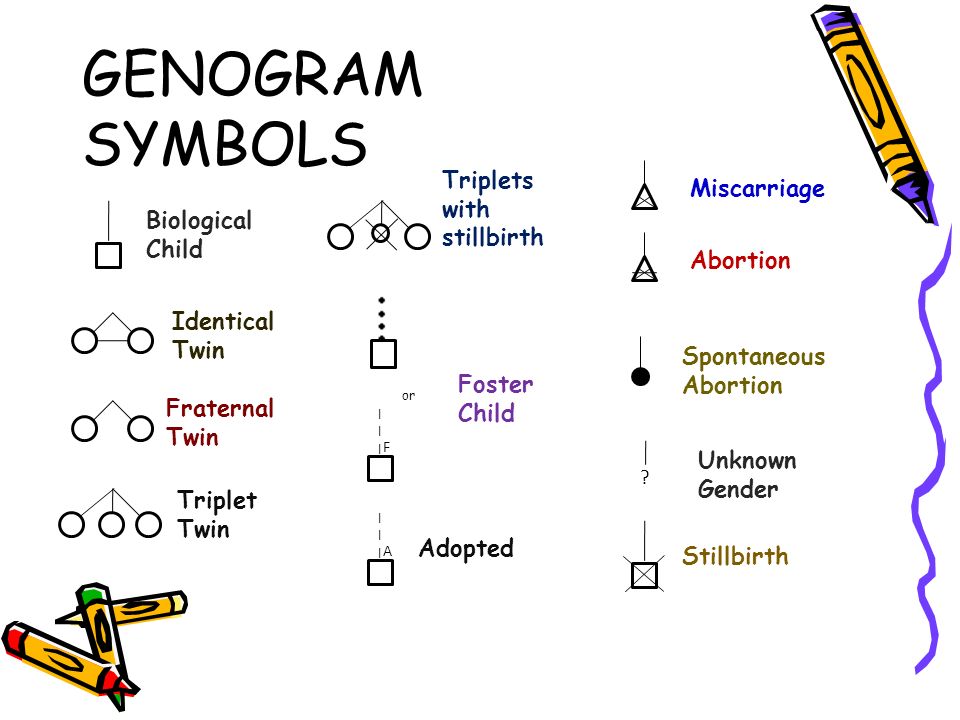 Studies have shown that around 55% of people who experienced a stillbirth noticed a reduction in baby movements before their baby died.
Studies have shown that around 55% of people who experienced a stillbirth noticed a reduction in baby movements before their baby died.
Read more about your baby’s movements in pregnancy.
If there is a change in your baby’s movements
Contact your midwife or maternity unit immediately if you think your baby’s movements have slowed down, stopped or changed. There are staff on the hospital maternity unit 24 hours a day, 7 days a week. Do not wait until the evening or the next day – seek help even if it is the middle of the night or the weekend.
If you think there might be a change in your baby’s movements
If you have any concerns, call your midwife or maternity unit immediately. Trust your instincts.
Who will I talk to if I report a change in my baby's movements?
Unless you have been given alternative numbers to ring during your pregnancy, the best place to ring is usually the labour ward. The labour ward is not just for people in labour but also for emergencies in pregnancy.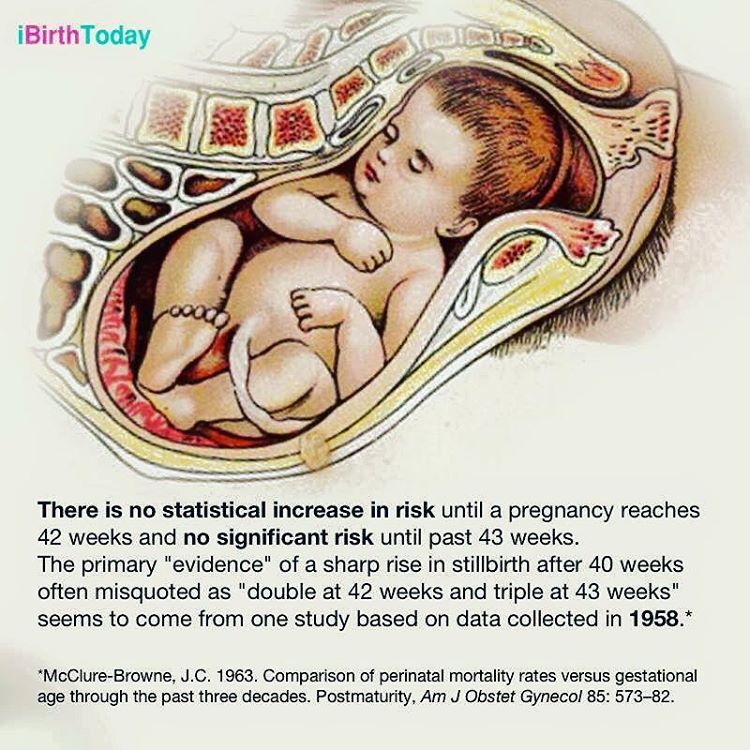 The ward should be open 24 hours a day and there should always be a midwife there who will be able to listen to your worries and advise you. Midwives often receive calls about reduced baby movements – they would much rather you got in touch than didn’t.
The ward should be open 24 hours a day and there should always be a midwife there who will be able to listen to your worries and advise you. Midwives often receive calls about reduced baby movements – they would much rather you got in touch than didn’t.
What will happen if I go into hospital?
Once at the hospital, they will probably check you over and listen to the baby’s heartbeat. If you are more than 28 weeks pregnant they may attach you to a heart rate monitor which records a trace of the baby’s heartbeat. You may also be given a button to push every time you feel the baby move. This can also be seen on the print out of the baby’s heartbeat.
It's quite common that once you lie down, hear the baby’s heartbeat and relax you start to feel the baby kicking. Don’t feel embarrassed about this – midwives see this every day. It is much better to go and be checked so that any potential problems can be picked up.
Find out more about what should happen if you report a change in fetal movements.
Leaking fluid or vaginal discharge in pregnancy
If you experience any leaking of fluid from your vagina during your pregnancy, you should contact your hospital immediately and go into be monitored. It could be your waters breaking early or a sign of infection of the womb.
Waters breaking early in pregnancy
Waters can sometimes break early in pregnancy, not just in the last couple of weeks, and this can lead to premature birth. If you feel a gush or trickle of fluid from your vagina, or feel damp, it could be a sign that your waters have broken. Put on a clean sanitary towel (not a tampon) and call the maternity unit straight away. They may ask you to sniff the pad – as it is common to leak urine in pregnancy – or they may ask you to check the pad again in around 20 minutes to see if it is damp.
Amniotic fluid (the fluid from around the baby) smells different to urine and is usually clear, pinkish or can be green or brown. If you think it might be amniotic fluid, it is important to go straight to the hospital to be examined. You may be asked to wear a special panty liner for up to 12 hours to confirm if you are leaking amniotic fluid, and you may need an internal examination (inside the vagina) to look for signs that your cervix is opening or softening for labour.
You may be asked to wear a special panty liner for up to 12 hours to confirm if you are leaking amniotic fluid, and you may need an internal examination (inside the vagina) to look for signs that your cervix is opening or softening for labour.
Infection in pregnancy
You should report any discharge from your vagina which is smelly, and any colour other than white, as it may be a sign of an intrauterine infection. Infections can weaken the bag of membranes around the baby, cause an infection inside the womb or make your waters break.
If you experience an unusual discharge, contact your midwife, GP or hospital and ask for a swab to be taken to look for infection. Other symptoms of an infection include a high temperature or stomach pain.
Diabetes in pregnancy
People with diabetes in pregnancy are more affected by:
- miscarriage
- pre-eclampsia
- preterm labour
- stillbirth
- problems with the baby (while in the womb, at delivery and after the birth).
It’s very important to control your blood sugar levels and get regular monitoring during your pregnancy. Whether you had diabetes already, or develop diabetes during pregnancy (gestational diabetes), you will be closely monitored during your pregnancy. You will need to be aware of how best to care for yourself and your baby during your pregnancy.
What to do if you have diabetes in pregnancy
The best way to reduce the risks to you and your baby is to make sure that your diabetes is well controlled before you get pregnant. Before you start trying for a baby, ask your GP or diabetes specialist for advice. They will be able to give you information about how pregnancy and diabetes may affect you.
If you are pregnant with diabetes, you will probably be regularly seen by a consultant and a specialist diabetes midwife and/or diabetes specalist. Make sure that you attend all your scheduled appointments so your healthcare team can monitor your condition. Seek help immediately from your GP, midwife or hospital doctors if you are concerned about your blood sugar control or any other factors affecting your pregnancy or your diabetes.
Monitoring the growth and movements of your baby is very important. If you’re worried, do not wait until the next day to get help – you can contact the labour ward to speak to a midwife 24 hours a day, 7 days a week.
If you have any of the risk factors for developing gestational diabetes, including having a BMI of 30 or over, you should be offered a blood sugar test between 24 and 28 weeks. It is important to go to this blood test.
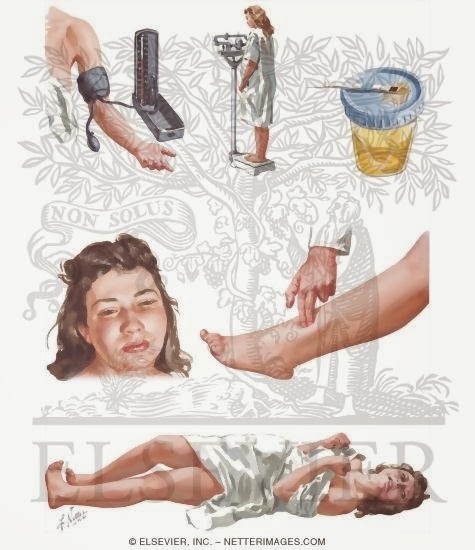
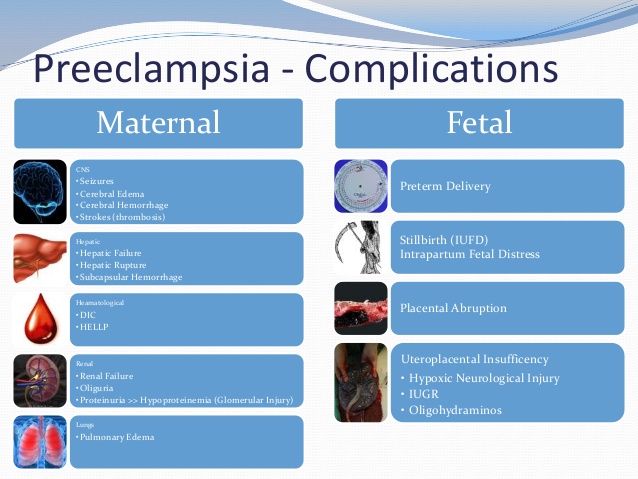
Pre-eclampsia and stillbirth
Pre-eclampsia is common. It is usually mild and normally has very little effect on pregnancy. However, it is important to know if you have the condition because, in a small number of cases, it can develop into a more serious illness. Severe pre-eclampsia can be life-threatening for both the mum/birthing person and the baby.
Early signs of pre-eclampsia include having high blood pressure (hypertension) and protein in your urine (proteinuria).
Pre-eclampsia is one of the pregnancy conditions your midwife will be testing for at your antenatal appointments, which is why it’s important to attend all of your appointments.
Signs of pre-eclampsia
Look out for any of the warning signs of pre-eclampsia, such as:
- severe headaches
- vision problems, such as blurring or flashing
- sudden swelling, particularly of your feet, ankles, hands and face
- pain just under the ribs
- vomiting.
If you notice any of these, contact your GP, midwife or maternity unit straightaway. Don’t wait until your next scheduled appointment. You should be seen by a healthcare professional the same day.
Read more about risk factors, diagnosis and treatment of pre-eclampsia.
Obstetric cholestasis (intrahepatic cholestasis)
Intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC), is a liver disorder that can develop during pregnancy. It has been linked to an increased risk of stillbirth in some cases. The main symptom is itching, usually without a rash. This is often worse at night and more noticeable on the palms of the hands and soles of the feet.
Itching is very common in pregnancy and only a small number of pregnant will have ICP. But if you are having itching, it’s important to tell your midwife or doctor.
Read more about obstetric cholestasis.
Finding the causes of stillbirth
Sadly, many parents never find out why their baby died. A report of all UK stillbirths showed around 35.5% of stillbirths were unexplained in 2018.
Tommy’s researchers are investigating the causes of stillbirth because unless we know why it happens, we can't find treatments or predict who may be at risk.
Read more about Tommy's research into stillbirth.
What is a stillbirth? | Pregnancy Birth and Baby
What is a stillbirth? | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is stillbirth?
In Australia, stillbirth is the birth of a baby who has died any time from 20 weeks into the pregnancy. The baby may have died during the pregnancy or, less commonly, during birth.
The baby may have died during the pregnancy or, less commonly, during birth.
If the length of pregnancy is not known, the birth will be considered a stillbirth if the baby weighs 400 grams or more.
A miscarriage is when a pregnancy ends before 20 weeks of pregnancy.
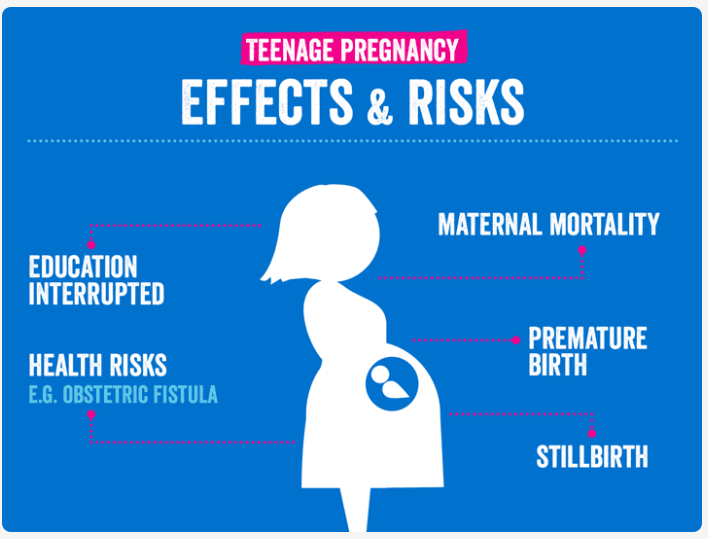
Every day in Australia, 6 babies are stillborn.
What can cause stillbirth?
Unfortunately, we often don’t known what causes a stillbirth.
Some of the possible causes of stillbirth include the following.
- Congenital abnormalities, such as a genetic condition or heart condition.
- A premature birth, where the baby is too immature to survive.
- A medical condition in the mother, such as diabetes, high blood pressure in pregnancy or pre-eclampsia.
- Problems that can cause bleeding during pregnancy, such as placental abruption or placenta praevia.
- Complications during birth.
- Certain infections.
- Problems with the umbilical cord or placenta.
- Major injury or trauma to the mother's abdomen (the tummy area).
You should be checked early in pregnancy for potential problems. This is so that they can be closely monitored. Your doctor and midwife will talk with you about monitoring and the best timing for the birth of your baby.
Can the risk of a stillbirth be reduced?
In many cases, the cause of stillbirth is not known. But there are some things you can do that can help lower the risk of stillbirth.
- Avoid smoking while pregnant. Smoking in pregnancy is one of the main causes of stillbirth. Quitting at any time reduces the risk of harm to your baby.
- Go to your antenatal appointments, where your doctor or midwife can check your baby’s growth. Regular ultrasound scans may be recommended if your baby isn't growing as expected.
- Be aware of your baby's movements, especially in the third trimester. Get to know the usual pattern of your baby’s movements.
 If you think your baby's movements have changed, speak to your doctor or midwife immediately.
If you think your baby's movements have changed, speak to your doctor or midwife immediately. - Go to sleep on your side as your pregnancy progresses, especially from 28 weeks. Lying on your back puts pressure on major blood vessels. This can reduce the flow of blood to your womb and restrict your baby’s oxygen supply. Research has shown that going to sleep on your side can halve the risk of stillbirth compared to going to sleep on your back.
Your doctor will talk with you about the timing of your birth if you have any risk factors.
When should I see my doctor?
Contact your doctor or midwife immediately if you are pregnant and:
- you think your baby has stopped moving or is moving differently or less than usual
- you have strong pain or cramping in your abdomen or back
- you receive a hard knock or blow to your abdomen
- you are bleeding or have more discharge than normal from your vagina
- you feel dizzy, experience changes to your vision, or have severe or long-lasting headaches
- your face, feet or hands suddenly swell or you have painful swelling in your legs
- you have severe or ongoing nausea and vomiting that affects your eating or drinking
- you have a fever or chills
- you sense that something doesn't feel right
If you can't contact your doctor or midwife, go to the local hospital emergency department.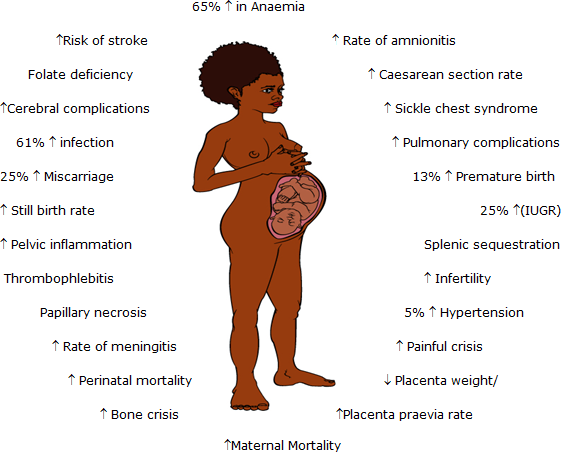 If you think it is an emergency, phone triple zero (000) for an ambulance.
If you think it is an emergency, phone triple zero (000) for an ambulance.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is a stillbirth diagnosed?
A stillbirth is diagnosed if your baby’s heart has stopped beating. During pregnancy, this can be detected with an ultrasound scan.
An obstetrician or midwife will let you know if your baby is not showing any signs of life. They will support you while they give you this news.
Grieving the loss of a baby is a very traumatic experience. It’s normal to feel a range of emotions, including shock, disbelief, deep sadness, anger and emptiness. There is no right or wrong way to feel and it’s okay for you to take as much time as you need.
How is the baby usually delivered?
If you are still pregnant, you will need to give birth to your baby. This is an extremely traumatic time for parents.
Your midwife or obstetrician will discuss with you the best way for you to give birth and the types of pain relief available. You may be able to go home for a day or 2 before coming back to the hospital to give birth to your baby.
In most cases, they will suggest inducing a vaginal birth rather than a caesarean birth. Your feelings are important as well as your preferences about the birth. Your care team will support you during and after the birth. Your care team will also discuss with you some options for after the baby is born.
Resources and support
The death of a baby is highly distressing, and grief is a normal response to stillbirth. Unfortunately, many bereaved parents report feeling isolated in their grief, and that the magnitude of their loss is not well understood.
Support is very important for parents and families who have experienced a stillbirth. There is an increased risk of parents having mental health issues such as anxiety, depression and post-traumatic stress.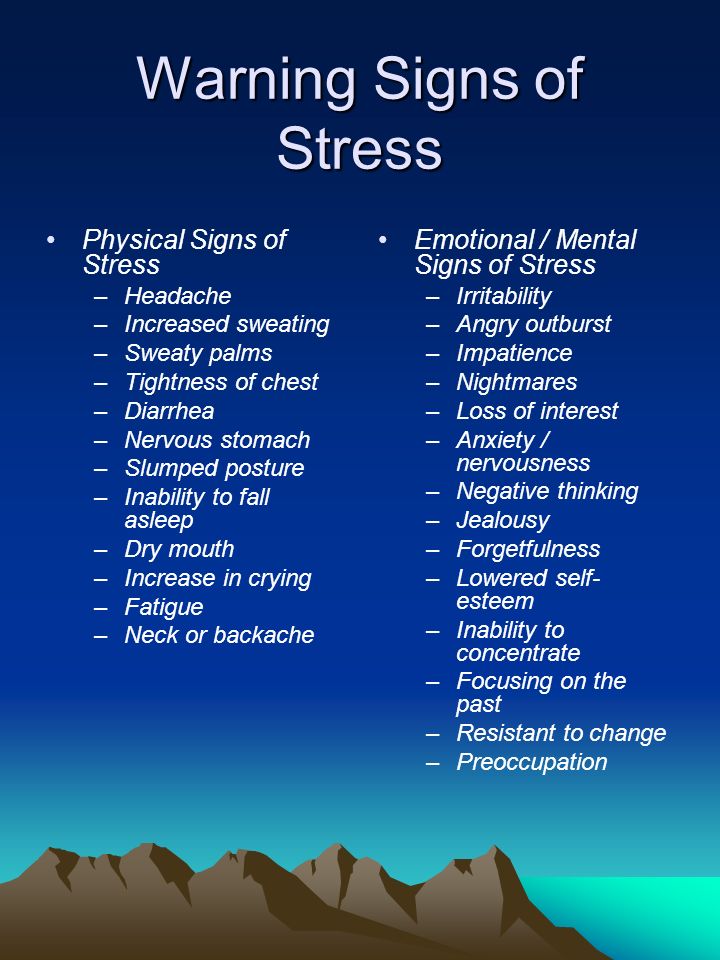
If you have experienced stillbirth you can get support from SANDS Australia by calling 1300 308 307, 24 hours a day.
Still Aware is an Australian stillbirth awareness organisation, providing education and support to parents and health professionals.
Stillbirth Foundation Australia also has information and support for families and health professionals.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Centre of Research Excellence in Stillbirth (Clinical Practice Guideline - for Care Around Stillbirth and Neonatal Death), The Centre of Research Excellence in Stillbirth (Frequently asked questions), Australian Institute of Health and Welfare (AIHW) (Australias mothers and babies), The Centre of Research Excellence in Stillbirth (Safer baby in pregnancy), The Royal Women’s Hospital (Birth after a baby has died), Queensland Clinical Guidelines (Stillbirth care)Learn more here about the development and quality assurance of healthdirect content.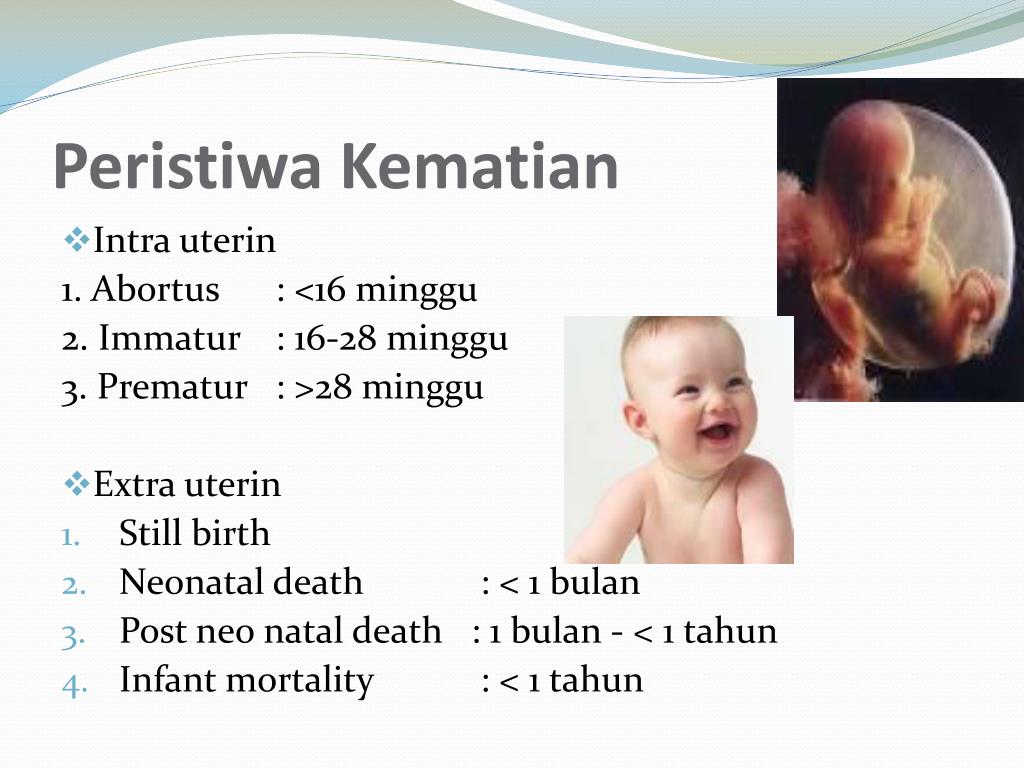
Last reviewed: August 2022
Back To Top
Related pages
- Experiencing a pregnancy loss
- Your body after stillbirth or neonatal death
- What happens after a stillbirth?
Need more information?
Stillbirth
Stillbirth Stillbirth is defined as the tragic loss of a baby from 20 weeks gestation or 400g of body weight, if gestation is unknown
Read more on Gidget Foundation Australia website
Stillbirth and newborn death | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Support after the death of a baby through stillbirth or newborn death
Read more on Sands Australia website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
What happens after a stillbirth?
A stillbirth is deeply traumatic and distressing, but you will have support and information available to help you through this painful time. Learn more here.
Read more on Pregnancy, Birth & Baby website
Better support and information for stillbirth and pregnancy loss
Safer Baby Bundle is an education and awareness program for parents and health professionals and hopes to reduce the rates of stillbirth in Australia.
Read more on Pregnancy, Birth & Baby website
Reducing the risk of stillbirth | Raising Children Network
You can reduce risk of stillbirth by eating well and exercising, sleeping on your side, and seeking immediate medical help if your baby’s movements change.
Read more on raisingchildren.net.au website
Stillbirth and neonatal death | Raising Children Network
Information about pregnancy loss, stillbirth and neonatal death, including grief and getting support.
Read more on raisingchildren.net.au website
Coping with grief | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Not-for-profit for bereaved parents from pregnancy loss from miscarriage stillbirth newborn death
Read more on Sands Australia website
Your body after stillbirth or neonatal death
After a stillbirth or neonatal death, your body may still experience the same changes it would after an uncomplicated birth. Find out what to expect and where to go for support.
Find out what to expect and where to go for support.
Read more on Pregnancy, Birth & Baby website
Grief after stillbirth or neonatal death | Raising Children Network
When a baby dies because of stillbirth or neonatal death, there’s no right way for you to grieve. People deal with grief in their own ways.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.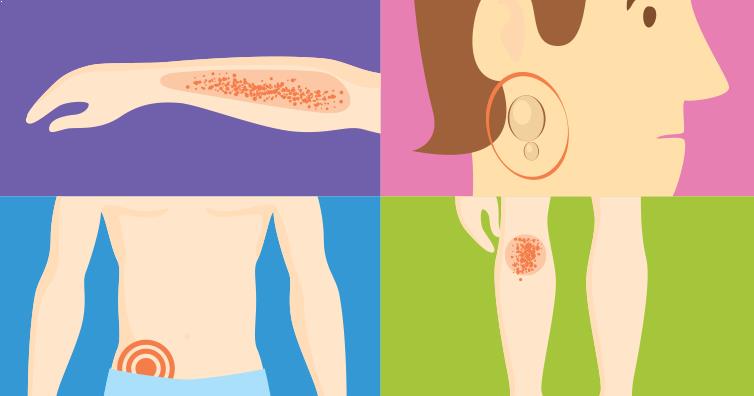
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Independent examination of neonatal death. Price. Examples.
Examination of the causes of death of newborns is a post-mortem examination of the corpse of a newborn child. The basis for the appointment of such an examination is the traces of violent actions on the body of the child or the suspicion that such actions were committed.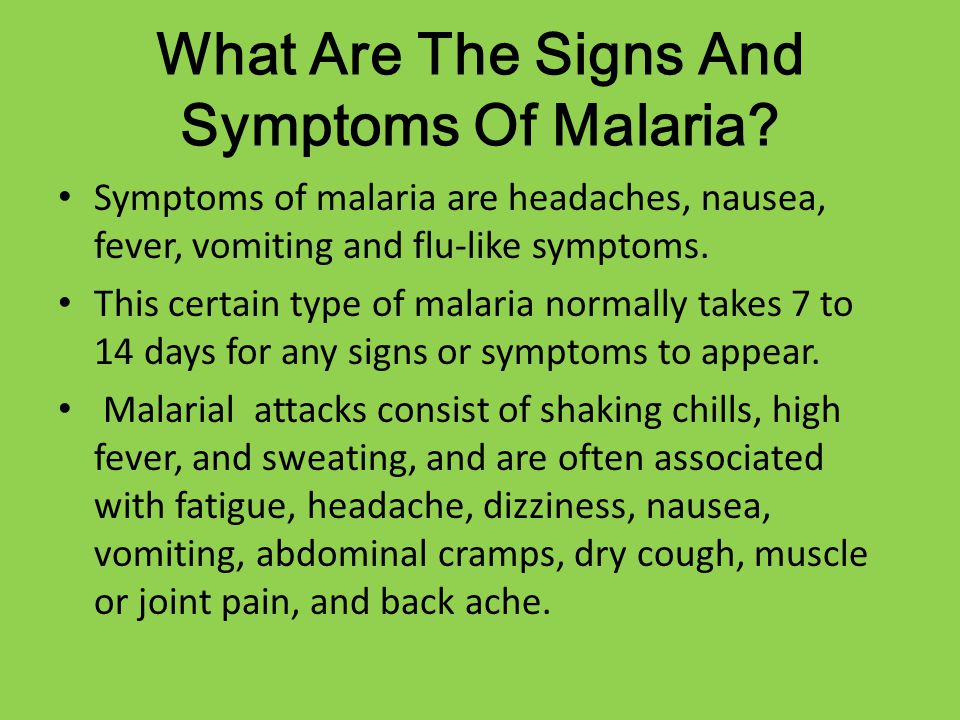 The death of a newborn may occur as a result of intentional actions of the mother or another person, as a result of accidental injuries during childbirth, especially independent, outside the walls of a specialized medical institution. Also, death can be caused by congenital diseases or injuries received during the passage of the child through the birth canal. The most dangerous injuries include craniocerebral injuries during rapid delivery or head presentation of the fetus. The lethal outcome, in addition, is due to intrauterine asphyxia, which is the result of premature detachment of the placenta or tight entanglement of the neck with the umbilical cord. Establishing the true cause of death and the mechanism of its occurrence is the main task of a forensic medical examination, in which a complete examination of the corpse of a newborn is performed, including external examination, autopsy, special analyzes, and so on.
The death of a newborn may occur as a result of intentional actions of the mother or another person, as a result of accidental injuries during childbirth, especially independent, outside the walls of a specialized medical institution. Also, death can be caused by congenital diseases or injuries received during the passage of the child through the birth canal. The most dangerous injuries include craniocerebral injuries during rapid delivery or head presentation of the fetus. The lethal outcome, in addition, is due to intrauterine asphyxia, which is the result of premature detachment of the placenta or tight entanglement of the neck with the umbilical cord. Establishing the true cause of death and the mechanism of its occurrence is the main task of a forensic medical examination, in which a complete examination of the corpse of a newborn is performed, including external examination, autopsy, special analyzes, and so on.
In forensic practice, active and passive infanticide are distinguished. With active infanticide, actions are performed aimed at the rapid termination of the vital functions of a newborn - strangulation by hand or with the help of improvised means, closing the openings of the nose and mouth, mechanical compression of the abdomen and chest, inflicting injury with a blunt object or cutting and piercing weapon, drowning. Leaving a child without care and necessary assistance is considered passive infanticide. In this case, death occurs most often from hypothermia or bleeding from the vessels of an unligated umbilical cord, less often due to hunger, a sudden cessation of the functioning of the respiratory or cardiovascular system. Signs of a neglected newborn include blood and cheese on the newborn's body and no food in the stomach.
With active infanticide, actions are performed aimed at the rapid termination of the vital functions of a newborn - strangulation by hand or with the help of improvised means, closing the openings of the nose and mouth, mechanical compression of the abdomen and chest, inflicting injury with a blunt object or cutting and piercing weapon, drowning. Leaving a child without care and necessary assistance is considered passive infanticide. In this case, death occurs most often from hypothermia or bleeding from the vessels of an unligated umbilical cord, less often due to hunger, a sudden cessation of the functioning of the respiratory or cardiovascular system. Signs of a neglected newborn include blood and cheese on the newborn's body and no food in the stomach.
Peculiarities of examination of the causes of death of newborns
Distinctive features of the examination of the causes of death of newborns are caused by a number of goals and objectives that cannot be set in principle during the examination of the corpse of an adult. These research issues include:
- Determining whether a deceased child is a newborn.
- Whether this child was mature and full-term during life.
- Whether the deceased child was viable, that is, whether any congenital diseases or birth injuries incompatible with life are found in him.
- Was this child born alive or dead? Did death occur after he was removed from the womb?
- What is the intrauterine life expectancy of this child?
- How long after birth was the baby alive?
These tasks, due to their exclusivity, require the use of special research methods. An unusual technique and research methodology is to conduct the following expert activities:
- Opening of the cranial cavity of a newborn corpse.
- Making a number of incisions in the area below the patella to identify the ossification nuclei.
- Gastrointestinal and pulmonary swimming test.
- Carrying out a number of anthropometric studies.
- Study and subsequent description of overlays on the surface of the skin.
- Examination of specific signs of the development of the genital organs.
- Additional examination of the umbilical cord, as well as the placenta (if they are submitted for examination).
Establishing the maturity, full term, newborn and viability of an infant in the process of performing an examination of the causes of death of newborns
In forensic practice, a newborn is an infant within the first twenty-four hours after the fact of birth. If it is necessary to make a decision on infanticide, the newborn baby is established on the basis of the following criteria:
- The presence of cheese-like grease on the body of an infant.
- The presence of blood on the body of an infant in the absence of visible injuries.
- Presence of a birth tumor.
- Detection of original feces (meconium).
- The umbilical cord is juicy, there are no signs of a demarcation ring in the area of rejection.
Maturity of an infant is understood as the level of fetal development at which extrauterine life is possible. An infant is considered mature if it exhibits the following characteristics:
- Weight exceeds 2500 grams.
- Skin elastic, pink. Developed subcutaneous fat layer.
- There are two to three centimeters long hair on the head.
- The cartilages of the nose and ears are elastic.
- The length of the umbilical cord is from forty-five to sixty centimeters.
- Nails are elastic. On the hands, the nails extend beyond the edge of the nail phalanx. On the legs - reach its edge.
- In boys, the testicles descend into the scrotum. In girls, the small labia are covered with large ones. In the lower epiphysis of the thigh, the ossification nucleus reaches sizes from five to seven millimeters.
A full-term infant is one born after forty to forty-two weeks of intrauterine development. Full-term babies have a height of forty-eight to fifty-two centimeters, chest circumference from thirty-two to thirty-four centimeters.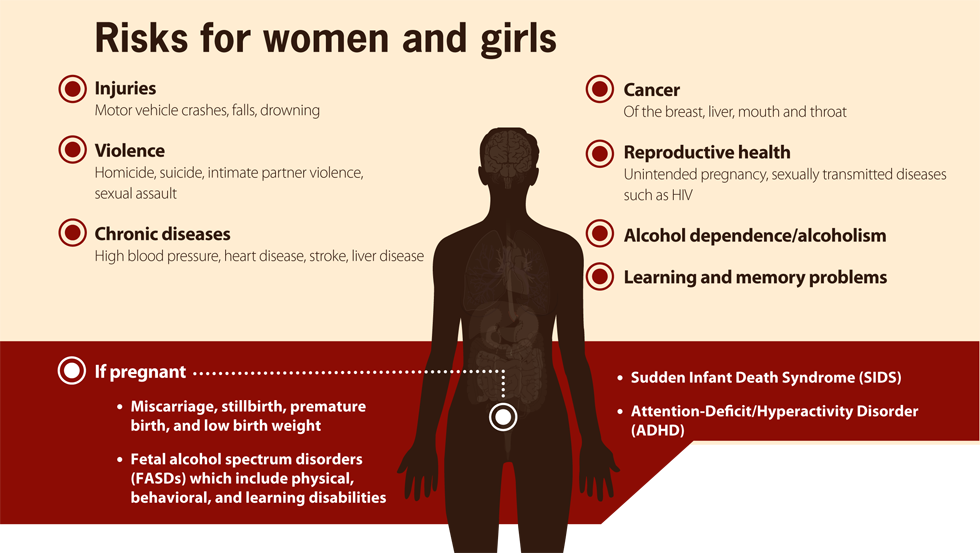 Also, babies show all the necessary signs of maturity.
Also, babies show all the necessary signs of maturity.
A viable infant is one who can continue extrauterine life. A viable child has no congenital malformations and birth injuries incompatible with life. Under the conditions of childbirth outside a medical facility, babies with a body length exceeding forty centimeters, a head circumference of at least twenty-eight centimeters, and a weight of more than one and a half kilograms are considered viable. For babies born in a maternity hospital, if medical care is available, viability is established at lower rates.
Determination of the fact of the birth of a live (dead) child during the examination of the causes of death of newborns
Determination of the fact that the baby was born alive is carried out by establishing the presence of air in the lungs, intestines and stomach. To detect air, a gastric or pulmonary swimming test is performed, which is widely used in forensic practice. Also, before the autopsy of the infant's corpse, an X-ray examination of the whole body and isolated lungs and gastrointestinal tract is performed.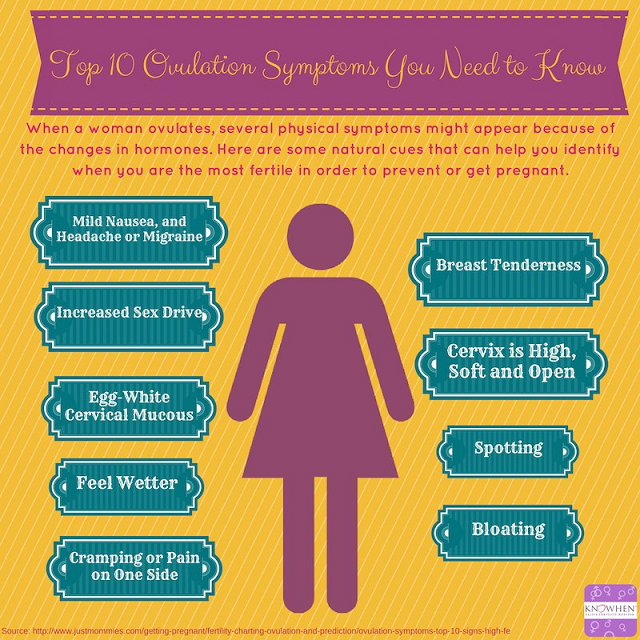 However, in some cases, these samples are unreliable, for example, air entering the gastrointestinal tract and lungs may be due to artificial respiration. In addition, with secondary atelectasis of the lungs, air, on the contrary, may be absent in a previously breathing child. As a result, to establish the birth of a live child, histological and spectral methods for examining the tissues of the lungs, umbilical cord and birth tumor are used.
However, in some cases, these samples are unreliable, for example, air entering the gastrointestinal tract and lungs may be due to artificial respiration. In addition, with secondary atelectasis of the lungs, air, on the contrary, may be absent in a previously breathing child. As a result, to establish the birth of a live child, histological and spectral methods for examining the tissues of the lungs, umbilical cord and birth tumor are used.
Determination of intrauterine and extrauterine life expectancy of an infant when conducting an examination of the causes of death of newborns
Determining the duration of intrauterine life of a fetus is based on making correspondences with body length. With a body length of more than twenty-five centimeters, the duration of the intrauterine period is determined in months - by dividing the body length in centimeters by 5. If the body length does not reach twenty-five centimeters, then the square root is taken from the body length indicator to determine the number of months of intrauterine life.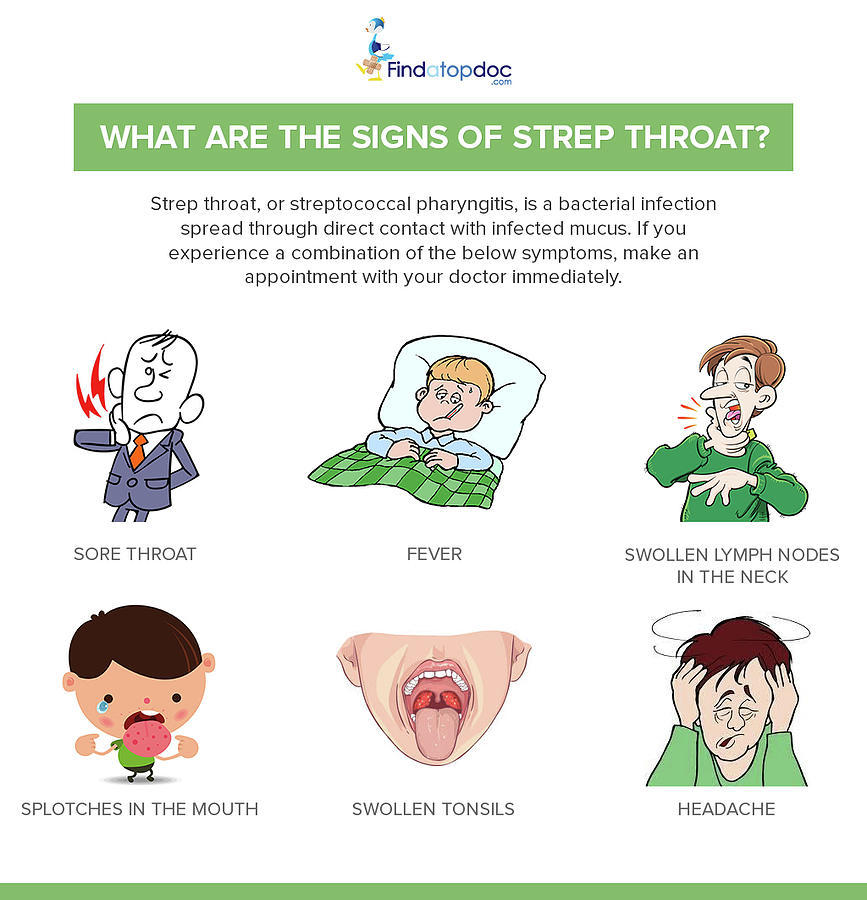
When conducting an examination of the causes of death of newborns, there are a number of signs according to which the duration of the extrauterine life of a newborn baby is established. So, a demarcation inflammatory line appears on the umbilical cord, which after six hours after birth is weakly expressed, and a day later it is already very clearly visible. The umbilical cord dries up on the second or third day after childbirth, and disappears after five to seven days. A gastrointestinal test is also used to determine life expectancy after birth. For its implementation, the stomach is bandaged on both sides, and the intestines - in several places. Further, according to the degree of air movement in the gastrointestinal tract, the approximate life expectancy is calculated. The presence of air only in the stomach indicates that the child lived only a few minutes after birth. The air in the small and large intestine speaks of several hours of life. Another indicator used in this case is the content in the intestines of the child of the original feces - meconium, which is completely removed from the intestines by the end of the third day of the baby's life.
Legal basis for the examination of the causes of death of newborns
The Criminal Code of the Russian Federation distinguishes cases of murder by a mother of her child in a separate group of crimes. Accordingly, the measure of restraint in such cases is specifically stipulated in Article 106 of the Criminal Code of the Russian Federation. The punishment of a mother for killing her own child is more lenient and amounts to a restriction of liberty for a period of two to four years. Punishment may also be expressed in the form of forced labor for up to five years or in the form of imprisonment for the same period. The article stipulates that such a preventive measure is intended for mothers who killed their child directly during childbirth or immediately after their completion, as well as the murder of a newborn child by his own mother, who is in a state of mental disorder while maintaining sanity, or by a mother who is in conditions psychotraumatic circumstances.
This is due to the fact that the complex hormonal and physiological processes occurring in the mother's body during childbirth and on the first day after its completion, aggravated by the lack of someone's help, can lead to unexpected, unpredictable actions on the part of the mother, especially if she is in a stressful situation.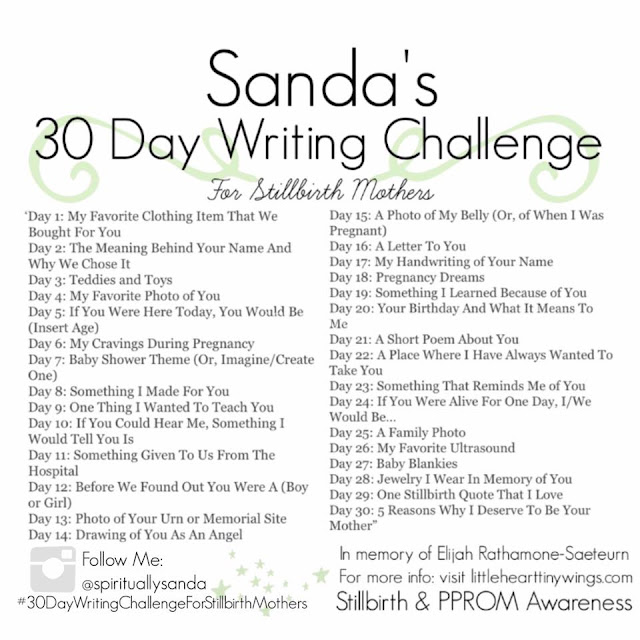
Questions to be put before a specialist conducting an examination of the causes of death of newborns
In each specific case of an examination of the causes of death of newborns, the number and composition of questions addressed to an expert may vary depending on the goals and objectives of the study. The above list of questions is general and subject to correction depending on the characteristics of the appointed expertise and the set of expert measures. In general, the specialist is asked the following questions:0003
- Was the deceased child a newborn?
- What is the sex of the newborn baby?
- What are the general physiological parameters of the infant?
- What evidence, found during examination of the child's body or during the production of an autopsy, testifies in favor of the fact that he was a newborn?
- Was there a child. Whose corpse is presented for examination, full-term?
- What are the indicators of the maturity of an infant?
- Was this infant viable?
- Does the infant have a birth injury, congenital disease, or malformation?
- Was this baby born alive?
- How long is the prenatal period for this baby?
- How long did the child live after birth?
- Was the baby cared for after birth?
- Are there injuries, injuries or other signs of external influence on the baby's body?
- Are these injuries life-threatening?
- What is the mechanism of this damage?
- Is there air in the infant's lungs and gastrointestinal tract?
- Has meconium been found in the infant's intestines?
- Was a cheese-like lubricant found on the body of a newborn baby?
- Were there traces of the mother's blood on the child's body?
- Are there signs of a demarcation ring on the umbilical cord?
- What is the cause of death of a newborn baby?
Expertise in a criminal case
According to the Decision of the Plenum of the Supreme Court of the Russian Federation of December 21, 2010 N 28 "On judicial expertise in criminal cases" expertise in a criminal case can be carried out either by the state an expert institution, or a non-profit organization established in accordance with the Civil Code of the Russian Federation and the Federal Law "On non-profit organizations", carrying out forensic activities in accordance with the statutes adopted by them.
Commercial organizations and laboratories, individual entrepreneurs, educational institutions, as well as non-profit organizations for which expert activity is not statutory, do not have the right conduct a criminal investigation. Expertise prepared by these organizations within the framework of criminal process, may be recognized as inadmissible evidence, i.e. evidence obtained from violation of the requirements of the procedural law.
Inadmissible evidence may not be used in the process of proof, including examination or be announced at the court session, and are subject to exclusion from the materials of the criminal case.
Since ANO "Forensic Expert" is an autonomous non-profit organization , and conducting judicial expertise is its main statutory activity (see section "Documents organization"), then it has the right to conduct examinations, including in criminal cases.
Lead poisoning | Symptoms, complications, diagnosis and treatment
Lead poisoning occurs when lead accumulates in the body, often over several months or years. Even small amounts of lead can cause serious health problems. Children under the age of 6 are particularly vulnerable to lead poisoning, which can seriously affect mental and physical development. At very high levels, lead poisoning can be fatal.
Even small amounts of lead can cause serious health problems. Children under the age of 6 are particularly vulnerable to lead poisoning, which can seriously affect mental and physical development. At very high levels, lead poisoning can be fatal.
Paint and lead-contaminated dust in old buildings are the most common sources of lead poisoning in children. Other sources include polluted air, water and soil. Adults who work with batteries, do home repairs, or work in auto repair shops can also be exposed to lead.
There is treatment for lead poisoning, but taking some simple precautions can help protect you and your family from lead exposure before harm occurs.
Symptoms
Initially, lead poisoning can be difficult to detect - even people who appear healthy may have high levels of lead in their blood. Signs and symptoms usually do not appear until dangerous amounts of the substance have accumulated in the body.
Signs and symptoms of lead poisoning in children include:
- Developmental delay
- Learning problems
- Irritability
- Loss of appetite
- Weight Loss
- Lethargy and fatigue
- Abdominal pain
- Vomiting
- Constipation
- Hearing loss
- Seizures
Symptoms of lead poisoning in adults
Although children are primarily at risk, lead poisoning is also dangerous for adults. Signs and symptoms in adults may include:
Signs and symptoms in adults may include:
- High blood pressure
- Muscle pain
- Difficulties with memory or concentration
- Headache
- Abdominal pain
- Mood disorders
- Reduction in sperm count and abnormal semen
- Miscarriage, stillbirth or premature birth in pregnant women
Causes
Lead is a metal that occurs naturally in the earth's crust, but human activities - mining, burning fossil fuels and manufacturing - have caused it to become more widespread. Lead was also once used in paint and gasoline, and is still used in batteries, solder, pipes, ceramics, roofing materials, and some cosmetics.
Lead in paint
Lead-based home paint, children's toys, and home furniture have been banned in the United States since 1978. But lead-based paint is still found on walls and woodwork in many older homes and apartments.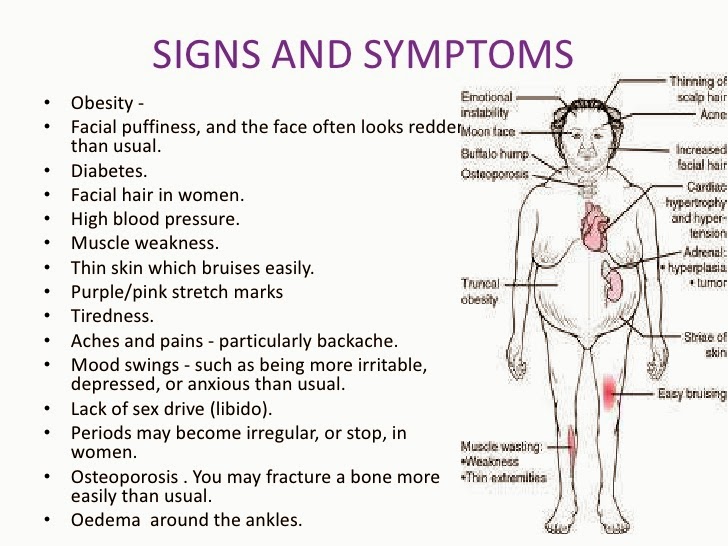 Most lead poisoning in children is the result of ingestion of deteriorating lead-based paint chips.
Most lead poisoning in children is the result of ingestion of deteriorating lead-based paint chips.
Lead can sometimes also be found in:
- Soil. Lead particles from leaded gasoline or paint are deposited on soil and can last for years. Lead-contaminated soil continues to be a major problem on highways and in some urban environments. Some soils near the walls of old houses contain lead.
- Household dust. Household dust may contain lead from lead paint chips or contaminated soil from outside.
- Ceramic. Glazes found on some pottery, china may contain lead, which can leach into food served or stored in the pottery.
- Toys. Lead is occasionally found in toys and other products made abroad.
- Cosmetics. Tiro, an eye cosmetic from Nigeria, has been linked to lead poisoning.
- Herbal or folk remedies.
 Lead poisoning has been associated with grita and azarkon, traditional Latin American medicines, and some from India, China, and other countries.
Lead poisoning has been associated with grita and azarkon, traditional Latin American medicines, and some from India, China, and other countries. - Sweets. Tamarind, an ingredient used in some sweets, may contain lead.
- Professions . People are exposed to lead and can bring it home on their clothes when they work in auto repair, mining, pipe fittings, battery manufacturing, painting, construction, and some other areas.
Factors that may increase the risk of lead poisoning include:
- Age . Infants and young children are more likely to be exposed to lead than older children. They may chew on paint that has peeled off walls and woodwork, and their hands may become contaminated with lead dust. Young children also absorb lead more easily and are more harmful than adults and older children.
- Life in an old house. Although the use of lead-based paint has been banned since the 1970s, old houses and buildings often retain traces of this paint.