Early pregnancy miscarriage clot
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
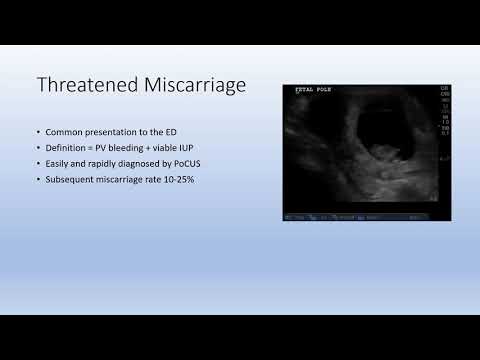
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen. Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean. If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.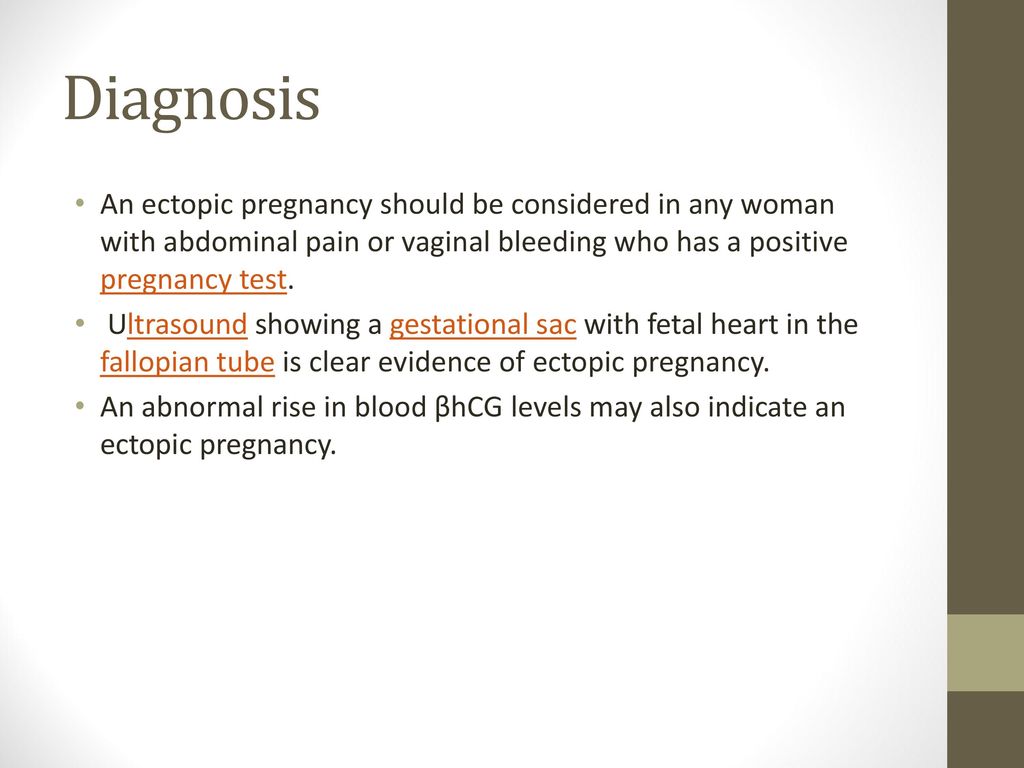
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
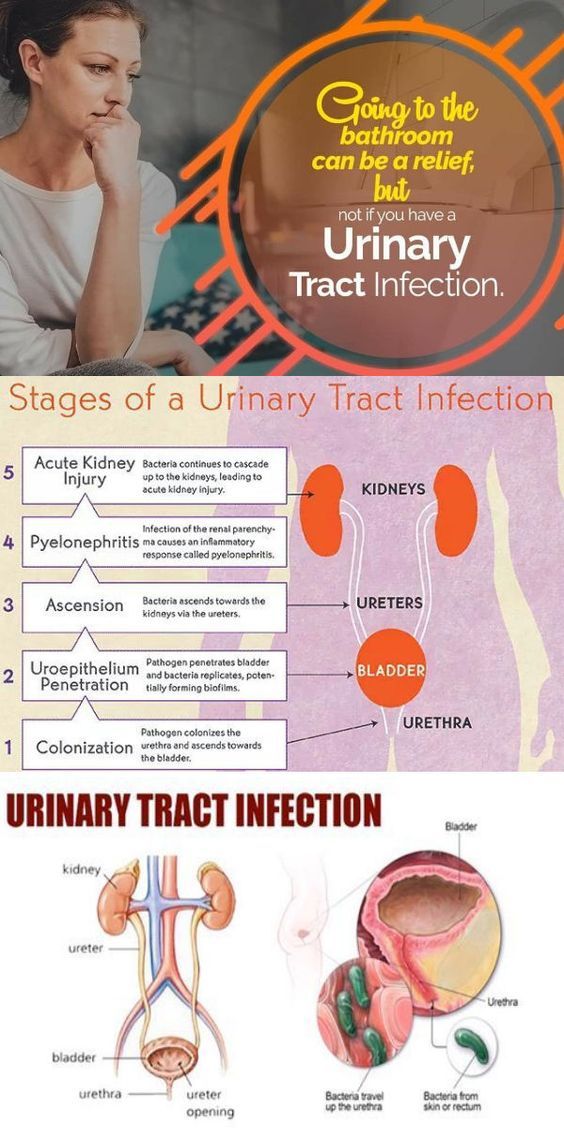
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
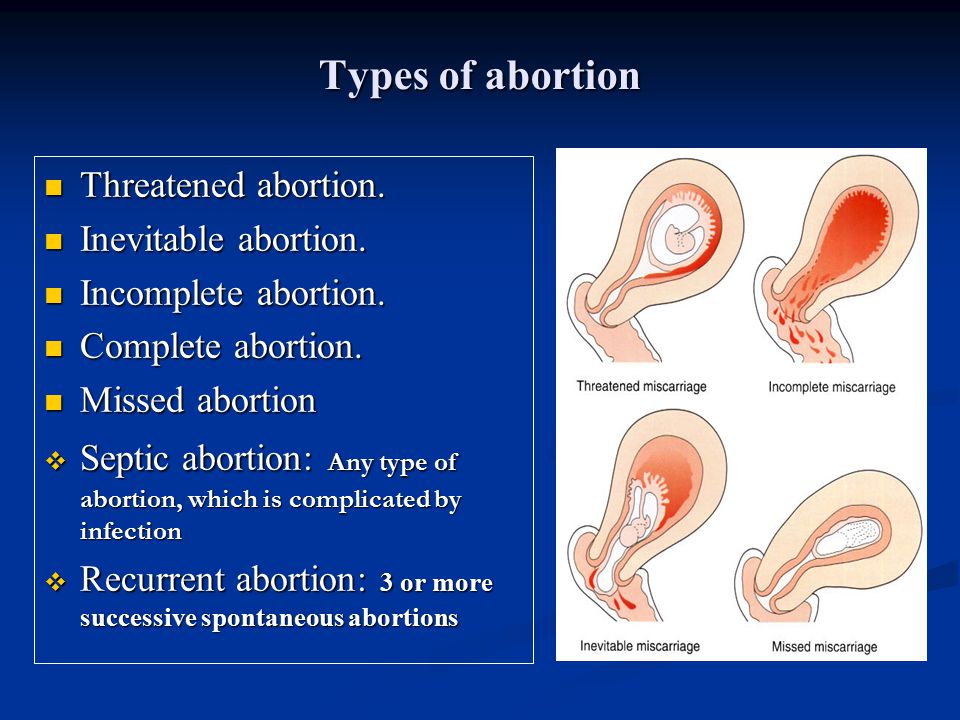
There’s no way to stop a miscarriage in progress. If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining. This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week. It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
How to identify a miscarriage: early signs
15-20% of pregnant women experience early pregnancy loss. It is important to know the earliest symptoms of a miscarriage in order to have time to seek help and, possibly, save the pregnancy.
Vera Ermakova
According to a study published in 2015 in the American Journal of Obstetrics and Gynecology, 41% of women who experienced a miscarriage felt guilty about what happened. Meanwhile, according to the American College of Obstetricians and Gynecologists (ACOG), at least half of miscarriages (pregnancy losses before 20 weeks) are due to chromosomal abnormalities that cannot be prevented. Nevertheless, given that up to 20% of pregnancies end in miscarriages, it is worth knowing its early signs in order to consult a doctor in time.
Nevertheless, given that up to 20% of pregnancies end in miscarriages, it is worth knowing its early signs in order to consult a doctor in time.
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
Very heavy bleeding
Not all bleeding that a pregnant woman may experience is indicative of a miscarriage: for example, small spots of blood may appear when a fertilized egg is implanted in the uterus. In addition, the developing placenta can also cause bleeding. But if the color of the discharge is bright red and they themselves are very intense, you should consult a doctor - this can be a dangerous sign.
Pink discharge and tissue clots
Not only blood: it is worth paying attention to any discharge that you may encounter during pregnancy. Light pink vaginal fluid, which is also accompanied by the release of clots, is a very alarming symptom.
Light pink vaginal fluid, which is also accompanied by the release of clots, is a very alarming symptom.
Pain and cramps
The cramps and cramps that many women experience during their premenstrual period or during their period are unpleasant, but in most cases they are not dangerous. But if you experience these sensations during pregnancy, you should consult a doctor as soon as possible. Cramps, pains and spasms can signal not only a miscarriage, but also an ectopic pregnancy, a deadly condition.
Lower back pain
During pregnancy, even if it is normal, the pressure on the back and especially on the lumbar increases. Therefore, almost all pregnant women feel pain in this area and discomfort in this area, from slight to very strong. But since pain and cramps in the lumbar region can also warn of a miscarriage (and especially if they are accompanied by bleeding or abdominal pain), you should definitely tell your doctor about them.
Absence of fetal heartbeat
Sometimes a miscarriage is not accompanied by any "external" symptoms, and in these cases, the absence of a heartbeat in the fetus is the only manifestation. However, the disappearance of toxicosis and other signs accompanying the first trimester of pregnancy can also be considered an indirect symptom.
By the way: Miscarriage: 7 dangerous myths that have nothing to do with the truth
Help with early miscarriage
- home /
- Blog /
- How to avoid early miscarriage
A miscarriage occurs when the fetus is shed from the endometrium, the inner lining of the uterus. According to experts, two out of 10 clinically established pregnancies end in spontaneous abortion. It is necessary to understand in more detail the causes, symptoms and methods of dealing with miscarriage.
How early miscarriage occurs
This process takes three consecutive steps. First, the fetus dies, after which it detaches from the endometrial layer. This is manifested by the fact that bleeding begins.
At the third stage, everything that has exfoliated is removed from the uterine cavity. The process may be complete or incomplete. In the early stages - five to six weeks - the process resembles ordinary menstruation. They are characterized by painful and much more unpleasant sensations. You can find out that it was just an early miscarriage by taking tests for the ratio of hCG in the blood.
Symptoms of a miscarriage
Signs of miscarriage are abdominal cramps, cramps or spotting. However, they do not always appear. It is necessary to note the most typical manifestations of the presented state and their main characteristics.
Temperature
For a short period of time, hyperthermia may well not be observed. Fever is not the most common symptom. In some cases, the thermometer readings really rise to 38 degrees or more.
In some cases, the thermometer readings really rise to 38 degrees or more.
At the same time, when hyperthermia is accompanied by a number of additional symptoms, a septic miscarriage is likely. These are its signs:
- severe pain in the abdomen and deep in the vagina;
- increase in the tone of the uterus, which is felt by shocks inside;
- pungent, pungent and unpleasant odour.
All this indicates that the infection has joined. In such a case, emergency hospitalization is strongly recommended to stop the development of the process. It is better not to engage in self-medication or the use of folk recipes.
Discharge
Early miscarriage can indeed be accompanied by discharge. They may be habitual, as during menstruation. Also, the discharge may be smearing, insignificant.
Brown, scanty secretion, much less likely to end in spontaneous abortion. Most often, this is indicated by abundant and bright red discharge. It is blood that normally appears when the fetus is rejected from the inner layer of the uterus.
It is blood that normally appears when the fetus is rejected from the inner layer of the uterus.
Pain
The severity of unpleasant and specific sensations may differ from each other depending on the duration of pregnancy. Probably the accession of pain, similar to menstruation. Most often, a similar symptom indicates an early miscarriage - no more than six weeks.
Probably cramping pains in the abdomen, which pull in the back. Their strength can vary from subtle to much more pronounced. In the rarest cases, when the clinical picture is complicated by a long course, this leads to a state of shock.
Another typical manifestation of pain is discomfort in the back or abdomen. Only then are the discharges identified. A similar situation is most typical for spontaneous abortion at the seventh or eighth week of pregnancy.
Causes of miscarriage
The first factor is genetic abnormalities in the development of the fetus. It is they who most often lead to miscarriage in the early stages. Violations can be expressed in qualitative or quantitative failures in chromosomes. In this regard, the female body recognizes the defect, and therefore does not allow such a fetus to develop further. Most often, such rejection is noted in the third week of pregnancy.
Violations can be expressed in qualitative or quantitative failures in chromosomes. In this regard, the female body recognizes the defect, and therefore does not allow such a fetus to develop further. Most often, such rejection is noted in the third week of pregnancy.
The next reason that an early miscarriage has developed may be disturbances in the work of the endocrine gland. Hormones determine not only the success and regularity of the cycle, but also how well the fetus is attached to the mucous surface of the uterus. If, due to a malfunction of the thyroid gland, the endometrium is not able to provide the fetus with all the necessary components, the pregnancy will not go well. Most often, a miscarriage occurs at the beginning or at the end of the fourth week.
Other reasons why pregnancy is terminated:
- Rhesus conflict. If the parents have different Rh factors, then the risk that a miscarriage will occur after the first weeks of pregnancy increases significantly.
 This happens if a woman has a negative Rh, and the child has a positive, inherited from the father. In such a situation, the female body recognizes the fetus as a foreign object. Therefore, it is excreted from the uterus. Timely diagnosis allows you to save the child through full-fledged drug therapy.
This happens if a woman has a negative Rh, and the child has a positive, inherited from the father. In such a situation, the female body recognizes the fetus as a foreign object. Therefore, it is excreted from the uterus. Timely diagnosis allows you to save the child through full-fledged drug therapy. - Sexually transmitted diseases, other infections. Similar problematic conditions also lead to spontaneous abortion. In this case, the embryo is infected at a very early stage. That is why the body will perceive it as a foreign object. In this regard, a miscarriage will occur already in the fifth week.
- Previous abortions. Another common reason why a miscarriage occurred. Abortion is a huge stress for the reproductive system, which leads to thinning of the lining of the uterus. That is why the risk of miscarriage may be greater.
Abdominal injuries should not be excluded from the injury list. Sharp pressure on the peritoneum, including when lifting weights, can provoke an abortion. Also on the list are severe stress, anxiety and depression. Anything that violates the normal state of a woman can lead to serious consequences.
Also on the list are severe stress, anxiety and depression. Anything that violates the normal state of a woman can lead to serious consequences.
How to avoid miscarriage
The main goal of treatment is to relieve tension in the uterus. It will be equally important to stop the bleeding and prolong the pregnancy, but only on the condition that the fetus is viable. The sooner medical assistance is provided, the higher the likelihood of preserving the fetus, without the need to determine the expected timing of miscarriages.
Our specialists will help you with this. Only we have the most qualified and experienced doctors who know exactly how to treat even the most difficult cases. They will conduct a full diagnosis and prescribe the most effective, effective medicines.
Drug treatment
Hormonal drugs are used. They at an early stage determine the normal course of pregnancy. Medicines based on the hormone progesterone are effective.
- The use of hemostatic drugs.
 In the case of pregnant women, droppers are used with drugs such as Dicinon or Tranexam. They are needed to stop bleeding.
In the case of pregnant women, droppers are used with drugs such as Dicinon or Tranexam. They are needed to stop bleeding. - Antispasmodics. Experts recommend injections of Drotaverin, followed by a switch to painkillers such as No-shpa. Papaverine suppositories, droppers with the addition of magnesia are also used. All of them are necessary in order to remove a number of signs of a pathological condition, namely, an increased tone of the uterus and pronounced pain.
- Use of Tocopherol. Vitamin E is an indispensable component for women, including pregnant women. It ensures the normal and full functioning of the ovaries. Tocopherol also strengthens the vascular walls, eliminates the formation of blood clots.
- Sedatives. Use motherwort or valerian tincture. The presented measure is recommended for increased irritability or nervousness of a pregnant woman.
To prevent early miscarriage, our clinic's specialists recommend glucocorticosteroids. Apply Dexamethasone or Metipred. They are prescribed to patients with diagnosed immune disorders that can lead to early termination of pregnancy.
Apply Dexamethasone or Metipred. They are prescribed to patients with diagnosed immune disorders that can lead to early termination of pregnancy.
Optionally, a special relief ring can be installed. The presented procedure is carried out in the second trimester, or rather after the 20th week of gestation.
Remove such device not earlier than 38 weeks. It is necessary for a woman to maintain the correct position of the uterus. Also, the unloading ring helps to prevent premature birth.
Additional measures
To prevent early miscarriage, it is recommended to stop physical activity. Especially when it comes to jumping, lifting weights. Rest, lack of sudden physical activity and adherence to bed rest will help to keep the pregnancy.
Another preventive measure will be the exclusion of sudden movements. At any stage of pregnancy, they can provoke detachment of the embryo or lead to serious complications in its development.
An early miscarriage will be excluded by:
- emotional calm and absence of stress;
- refusal to take a hot bath or visit a bath, sauna - this is due to the fact that high temperatures provoke increased bleeding, as well as detachment of the fetus;
- restriction of sexual intercourse - if there is a threat that an early miscarriage will occur, they refuse to have sex;
- exclusion of alcohol, nicotine addiction.