How long do rashes last on babies
Kids Health Information : Rashes
Rashes are very common in children and babies. Most rashes are caused by common viral infections, and are nothing to be worried about. Usually, rashes are harmless and will go away on their own.
Sometimes different viruses can cause rashes that look the same, while some viruses cause rashes that look quite unique.
Measles is a virus that causes a distinctive rash. Measles is very contagious and can be serious. If you think your child has measles, see your GP.
If your child has a rash of small, bright-red or purple spots or bruises that do not turn white (blanch) when you press on them, seek urgent medical attention.
Signs and symptoms
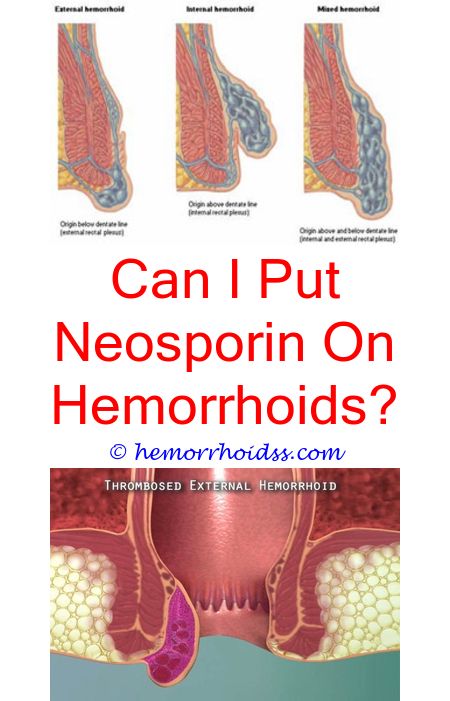
Rashes can have many different appearances: red, flat areas; raised bumps; blisters; welts; or any combination of these. It can be common for the rash to spread to most or all of the body before it goes away. The rash may last for days to weeks.
Most rashes are mild and do not cause your child any distress, although some rashes can cause a lot of itching.
Some rashes are quite distinctive. For more information about viruses that cause a rash, see our fact sheets:
-
Chickenpox
- Hand, foot and mouth disease
-
Henoch-Schönlein purpura
- Measles
-
Molluscum
- Roseola infantum
-
Slapped cheek (fifth disease)
When to see a doctor
Often the viral infection causing the rash will also cause your child to have a fever (see our fact sheet
Fever in children). The fever often happens at the start of the illness, before the rash appears. When the rash appears, it means your child is getting better. However, if your child has a fever with their rash, take them to see your GP.
However, if your child has a fever with their rash, take them to see your GP.
Measles can be dangerous, especially for young children and babies. If you think that your child might have measles, see your GP. Ask if your doctor can visit your child at home, or if you visit a medical clinic, tell the receptionist as soon as you arrive, to avoid spreading the infection to others.
If your child has a rash of small, bright-red or purple spots or bruises that do not turn white (blanch) when you push on them, along with a fever, headache, stiff neck or back pain, seek medical advice immediately from your GP or nearest hospital emergency department. See our fact sheet Meningococcal infection.
Care at home
In nearly all cases, it is not important to know which virus is causing the rash. Most rashes will get better on their own. Antibiotics do not work on viruses and are not given to children with rashes caused by viral infections.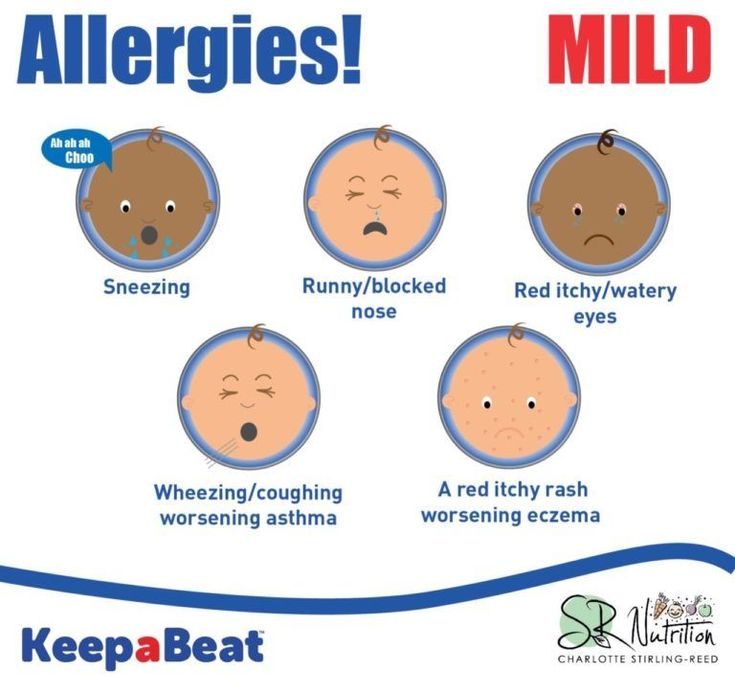
If your child's rash is itchy, talk to your local pharmacist about treatments that can help relieve the itch.
You can make your child feel more comfortable if the virus associated with the rash is making your child feel miserable. See our fact sheet Pain relief for children.
How are viral infections spread?
Viruses are spread by direct contact. The best way to prevent spreading and catching viruses is to wash your hands after touching any bodily fluid and avoid sharing items like cutlery, drinking cups, towels, toothbrushes and clothing.
Key points to remember
- Rashes caused by viruses are very common in children and babies.
- Most viral rashes are harmless and will go away on their own.
- If you are concerned your child has measles, see a doctor.
- If your child has a fever and a rash that does not turn white (blanch) when pressed or they are very unwell, seek emergency medical care.
For more information
- Dr Margie: Childhood rash symptoms and treatment
- Kids Health Info fact sheet: Measles
- Kids Health Info fact sheet: Chickenpox
- Kids Health Info fact sheet: Hand foot and mouth disease
- Kids Health Info fact sheet:
Roseola infantum
- Kids Health Info fact sheet: Slapped cheek (fifth disease)
- Kids Health Info fact sheet: Meningococcal infection
- Kids Health Info fact sheet: Viral illnesses
- Kids Health Info fact sheet: Hives
- Kids Health Info fact sheet: Fever in children
- Kids Health Info fact sheet:
Pain relief for children.

- See your GP or Maternal and Child Health Nurse.
Common questions our doctors are asked
Do I need to take my child to the doctor every time she has a rash?
No, if your child has a mild illness – like the common cold – and they are otherwise happy and eating and drinking, then the presence of a slight rash is not concerning.
My child has a rash and I am pregnant. Should I be worried?
Some viral infections can cause problems in early pregnancy. If you are pregnant, and your child has a rash and you are concerned, you should see your local doctor or obstetrician for advice.
Developed by The Royal Children's Hospital General Medicine department. We acknowledge the input of RCH consumers and carers.
Reviewed May 2018.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www. rchfoundation.org.au.
rchfoundation.org.au.
child under 2 years: MedlinePlus Medical Encyclopedia
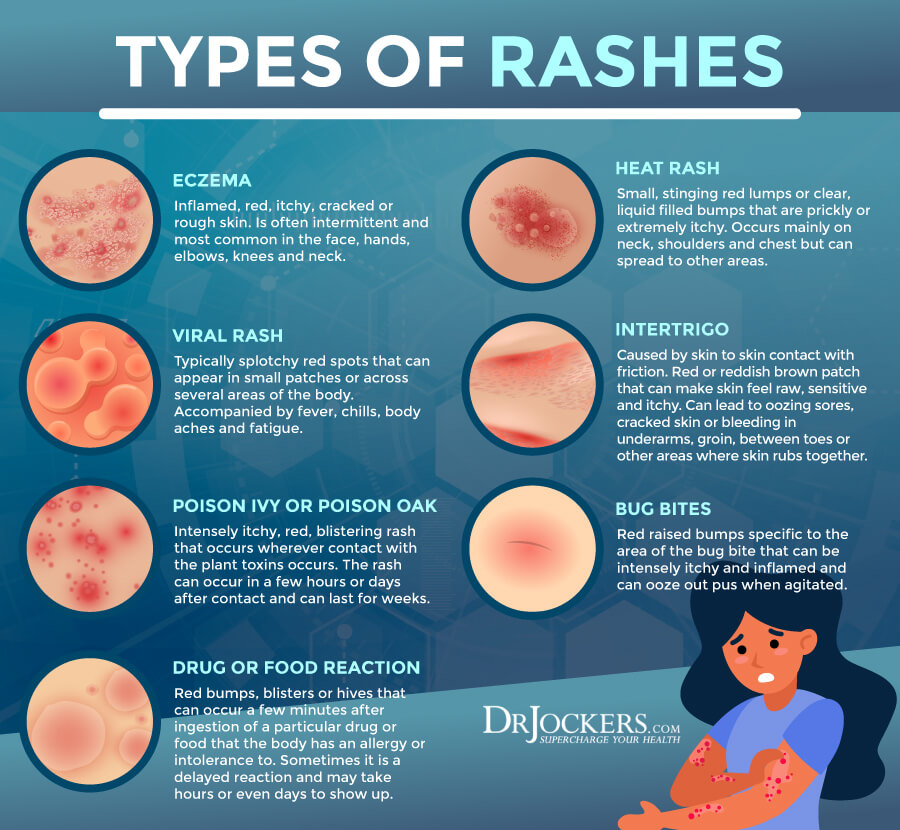
A rash is a change in the color or texture of the skin. A skin rash can be:
- Bumpy
- Flat
- Red, skin-colored, or slightly lighter or darker than skin color
- Scaly
Most bumps and blotches on a newborn baby are harmless and clear up by themselves.
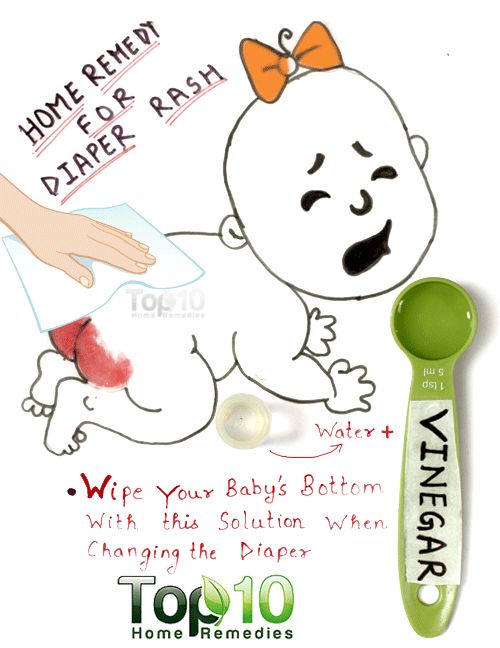
The most common skin problem in infants is diaper rash. Diaper rash is an irritation of the skin caused by dampness, urine, or feces. Most babies who wear diapers will have some type of diaper rash.
Other skin disorders can cause rashes. These are most often not serious unless they occur with other symptoms.
Causes may include:
- Diaper rash (rash in the diaper area) is a skin irritation caused by long-term dampness and by urine and feces touching the skin.
- Yeast diaper rash is caused by a type of yeast called candida, which also causes thrush in the mouth. The rash looks different from a regular diaper rash.
 It is very red, and there are usually small red bumps on the outer edges of the rash. This rash requires treatment with medicine.
It is very red, and there are usually small red bumps on the outer edges of the rash. This rash requires treatment with medicine. - Heat rash, or prickly heat, is caused by the blockage of the pores that lead to the sweat glands. It is most common in very young children but can occur at any age. It is more common in hot and humid weather. The sweat is held within the skin and forms little red bumps or occasionally small blisters.
- Erythema toxicum can cause flat red splotches (usually with a white, pimple-like bump in the middle) that appear in up to one half of all babies. This rash rarely appears after 5 days of age, and most often disappears in 7 to 14 days. It is nothing to worry about.
- Baby acne is caused by exposure to the mother's hormones. Red bumps, sometimes with white dots in the center, may be seen on a newborn's face. Acne most often occurs between 2 and 4 weeks of age, but may appear up to 4 months after birth and can last for 12 to 18 months.
- Cradle cap (seborrheic dermatitis) causes greasy, scaling, crusty patches on the scalp that appear in a baby's first 3 months.
 It most often goes away by itself, but some cases may require treatment with medicine.
It most often goes away by itself, but some cases may require treatment with medicine. - Eczema is a condition of the skin in which areas are dry, scaly, red (or darker than normal skin color), and itchy. When it goes on for a long time the areas become thickened. It is often associated with asthma and allergies, although it can often occur without either of these. Eczema often runs in families.
- Hives are red welts that appear to move around on the body. For example, if you drew a circle to mark one of the welts, a few hours later that circle would not have a welt in it, but there would be welts on other parts of the body. They differ in size and shape. Hives may last for a few weeks. The cause is uncertain.
DIAPER RASHES
Keep the skin dry. Change wet diapers as quickly as possible. Allow the baby's skin to air dry as long as is practical. Launder cloth diapers in mild soap and rinse well. Avoid using plastic pants. Avoid irritating wipes (especially those containing alcohol) when cleaning the infant.
Ointments or creams may help reduce friction and protect the baby's skin from irritation. Powders such as cornstarch or talc should be used cautiously, as they can be inhaled by the infant and may cause lung injury.
If your baby has a yeast diaper rash, the health care provider will prescribe a cream to treat it.
OTHER RASHES
Heat rash or prickly heat is best treated by providing a cooler and less humid environment for the child.
Powders are unlikely to help treat heat rash and should be stored out of reach of the infant to prevent accidental inhalation. Avoid ointments and creams because they tend to keep the skin warmer and block the pores.
Erythema toxicum is normal in newborn babies and will go away on its own in a few days. You do not need to do anything for it.
White or clear milia/miliaria will go away on their own. You do not need to do anything for it.
For hives, talk with your provider to try to find the cause. Some causes require prescription medicines. Antihistamines may help stop the itching.
Antihistamines may help stop the itching.
BABY ACNE
Normal washing is all that is necessary to treat baby acne most of the time. Use plain water or mild baby soap and only bathe your baby every 2 to 3 days. Avoid acne medicines used by adolescents and adults.
CRADLE CAP
For cradle cap, wash the hair or scalp with water or a mild baby shampoo. Use a brush to remove the flakes of dry skin. If this cannot be removed easily, apply an oil to the scalp to soften it. Cradle cap most often disappears by 18 months. If it does not disappear, it becomes infected, or if it is resistant to treatments, consult your provider.
ECZEMA
For skin problems caused by eczema, the keys to reducing rash are to reduce scratching and keep the skin moisturized.
- Keep the baby's fingernails short and consider putting soft gloves on the child at night to minimize scratching.
- Drying soaps and anything that has caused irritation in the past (including foods) should be avoided.
- Apply a moisturizing cream or ointment immediately after baths to avoid drying.
- Hot or long baths, or bubble baths, may be more drying and should be avoided.
- Loose, cotton clothing will help absorb perspiration.
- Consult a provider if these measures do not control the eczema, (your child may need prescription medicines) or if the skin begins to appear infected.
While the majority of children with eczema will outgrow it, many will have sensitive skin as adults.
Call your child's provider if your child has:
- A fever or other unexplained symptoms associated with the rash
- Any areas that look wet, oozing, or red, which are signs of infection
- A rash that extends beyond the diaper area
- A rash that is worse in the skin creases
- A rash, spots, blister, or discoloration and is younger than 3 months
- Blisters
- No improvement after 3 days of home treatment
- Significant scratching
The provider will perform a physical exam.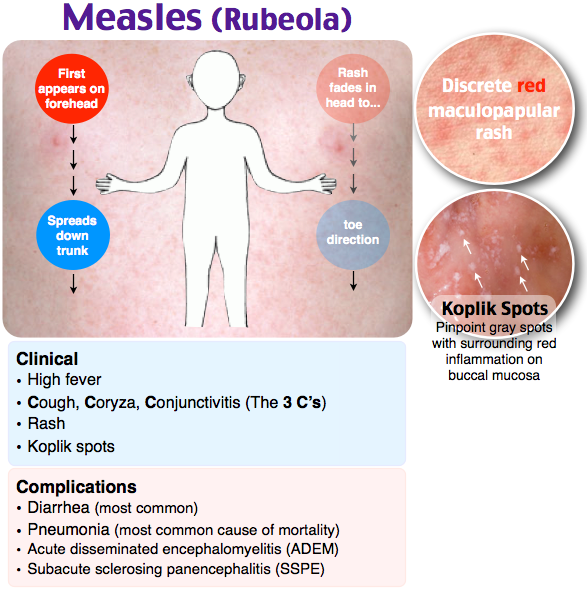 The baby's skin will be thoroughly examined to determine the extent and type of the rash. Bring a list of all the products used on the child's skin.
The baby's skin will be thoroughly examined to determine the extent and type of the rash. Bring a list of all the products used on the child's skin.
You may be asked questions such as:
- When did the rash start?
- Did symptoms begin at birth? Did they occur after fever was relieved?
- Is the rash related to skin injury, bathing, or exposure to sunlight or cold?
- What does the rash look like?
- Where on the body does the rash occur? Has it spread to other areas?
- What other symptoms are also present?
- What type of soaps and detergents do you use?
- Do you put anything on the skin (creams, lotions, oils, perfumes)?
- Is your child taking any medicines? How long has the child taken them?
- Has your child recently eaten any new foods?
- Has your child been in contact with grasses/weeds/trees recently?
- Has your child recently been sick?
- Do any skin problems run in your family? Does your child or anyone in your family have allergies?
Tests are seldom required but may include the following:
- Allergy skin tests
- Blood studies (such as CBC, blood differential)
- Microscopic examination of a sample of the affected skin
Depending on the cause of the rash, antihistamines may be recommended to decrease itching. Antibiotics may be prescribed if there is a bacterial infection.
Antibiotics may be prescribed if there is a bacterial infection.
The provider may prescribe a cream for diaper rash caused by yeast. If the rash is severe and not caused by yeast, a corticosteroid cream may be recommended.
For eczema, the provider may prescribe ointments or cortisone drugs to decrease inflammation.
Baby rash; Miliaria; Prickly heat
- Erythema toxicum on the foot
- Heat rash
- Miliaria profunda - close-up
- Erythema toxicum neonatorum - close-up
DiBiagio JR, Lloyd CM. Dermatology. In: Kleinman K, Mcdaniel L, Molloy M, eds. The Harriet Lane Handbook. 22nd ed. Philadelphia, PA: Elsevier; 2021:chap 8.
Gehris RP. Dermatology. In: Zitelli BJ, McIntire SC, Nowalk AJ, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 8.
Valeyrie-Allanore L, Obeid G, Revuz J. Drug reactions. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Limited; 2018:chap 21.
Dermatology. 4th ed. Philadelphia, PA: Elsevier Limited; 2018:chap 21.
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Allergic rash in children - treatment in Zelenograd - AKSIS Medical Center
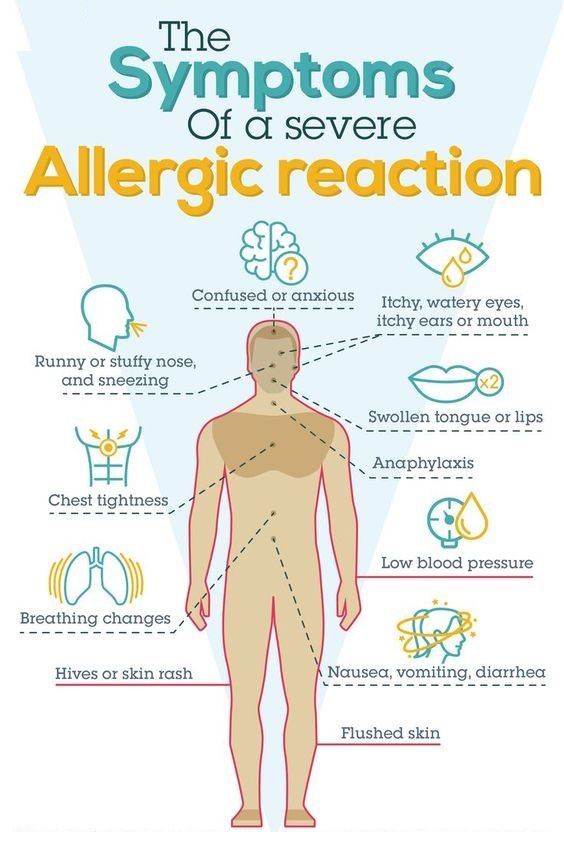
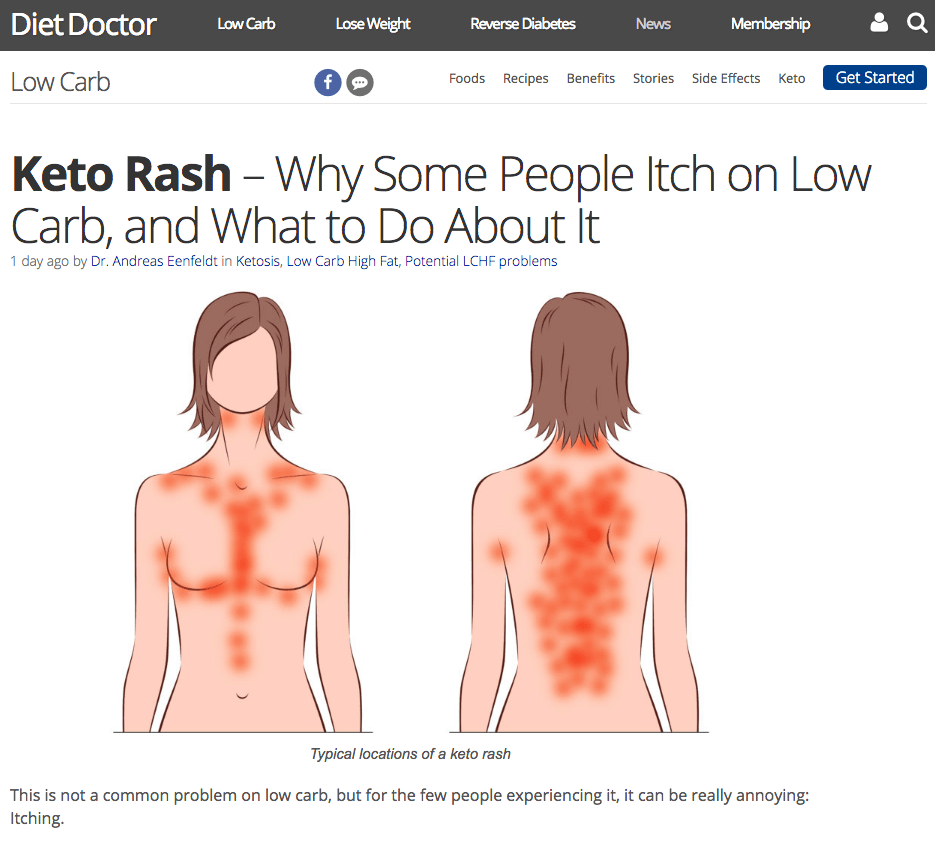
An unformed immune system in a child often causes allergic rashes. Outwardly, this is manifested by the appearance of redness on the skin, accompanied by itching, blisters and other skin rashes. Obviously, in this situation, a mother is concerned about many questions: “How to remove an allergic rash?”, “What to do so that a rash does not appear?”, “What is the first aid for an acute reaction of the body to an allergen?”, “How long does it take allergic rash?
Characteristic symptoms
It is important for young parents to find out whether the rash that has appeared is an allergic reaction or is it a source of dangerous infectious diseases.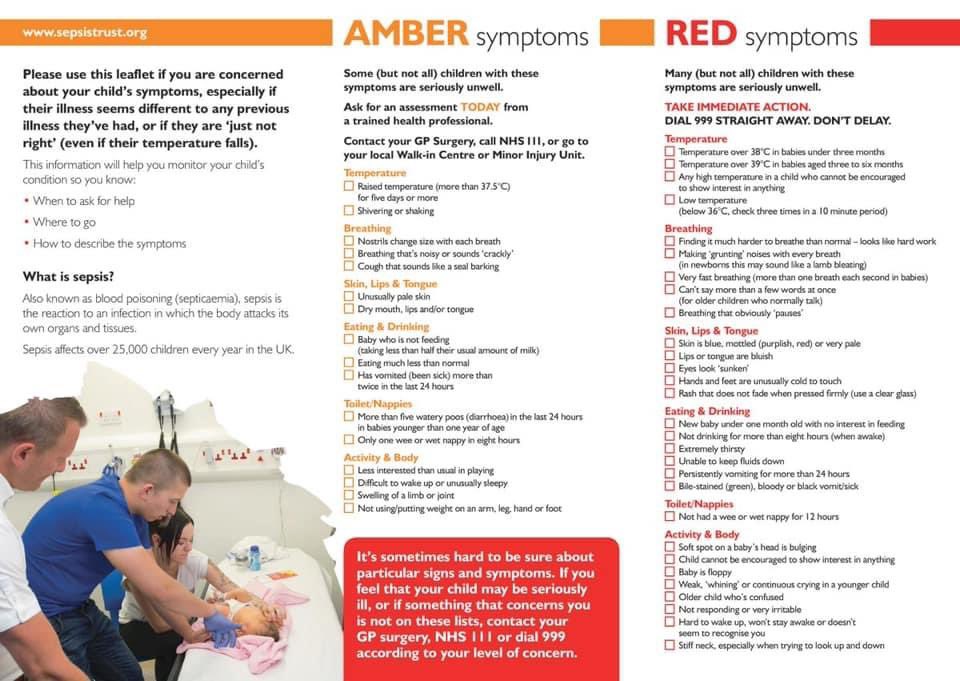
Characteristic features of an allergic rash in a child are:
Allergic rashes on the back, abdomen, neck, arms are often accompanied by discharge of clear mucus from the nose. In infectious diseases, the mucus quickly thickens, becomes cloudy, with a greenish tint.
The nature of possible rashes can be seen in the photo.
The skin reacts with the appearance of pimples, vesicles, papules, round spots, often with exudate, then they can develop into a continuous edematous surface, sometimes covered with a crust. With severe itching, irritability may appear.
An allergic rash in infants mainly appears in the upper body, in folds, may be accompanied by swelling of the facial organs: tongue, larynx, which causes the risk of suffocation. With the manifestation of such symptoms as nasal congestion, tearing, swelling of the cheeks, parents should not hesitate, but call an ambulance, since the development of Quincke's edema can become a complication.
With the manifestation of such symptoms as nasal congestion, tearing, swelling of the cheeks, parents should not hesitate, but call an ambulance, since the development of Quincke's edema can become a complication.
Diagnosis of rashes in babies
Due to the huge variety of causes of skin rashes in young children and types of rashes, it is necessary to immediately seek advice from a pediatrician, especially if an allergic rash is observed in a newborn. The reaction of the body to a particular allergen can be rapid.
During diagnostics:
- Blood biochemical analysis
- Allergy testing in progress
- The state of immunoglobulin in the blood is detected
For a doctor, in order to make a correct diagnosis and determine the appropriate treatment, it is important to know what the baby's diet was like the day before, whether the diet has changed, whether medications were taken, whether there was contact with chemical ingredients.
Major allergens in children
An allergic rash on the neck, abdomen, arms, legs is often the result of a reaction of the child's immune system to provoking factors. Allergens can be:
- Food: eggs, milk, fruits, honey, nuts, seafood
- Medicines: antibiotics, vitamins and other preparations
- Chemical agents: soap, washing powder used to wash the child's clothes
- Dust, wool, pollen from flowering plants
- Insect bites, plant leaf burns
- UV action
An allergic rash on the abdomen or arms may result from contact dermatitis. Doctors consider the lightning-fast reaction of the body to an allergen or irritant to be the most dangerous, when the symptoms of an allergic rash in children manifest themselves within 15-30 minutes after interacting with the allergen.
Genetic inheritance is considered a significant factor in the predisposition of children to atopic dermatitis. Provided that one of the adults (mother / father) often suffers from malaise as a result of a food, drug form of allergy, the likelihood of the disease in a child increases.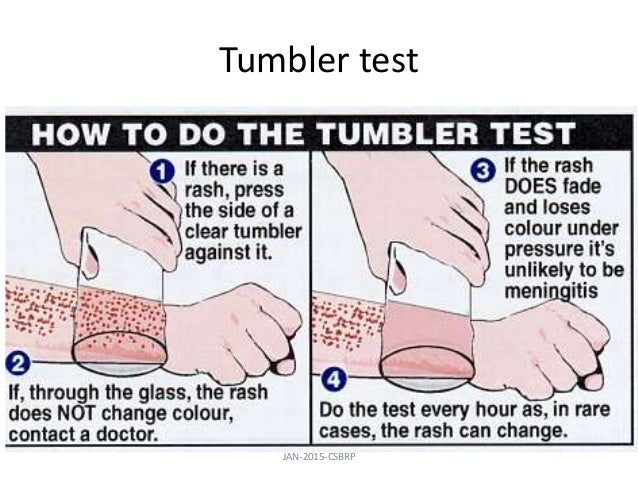
Treatment of rashes in children
“If your child has similar symptoms, we advise you to make an appointment with a doctor. You can also make an appointment by phone: +7 (499) 214-00-00
The list of medical methods for treating a sensitive reaction to an allergen in children is quite extensive, which makes it difficult to choose funds for independent use. Therefore, if an allergic rash occurs in a baby or an older child, the only right decision is to immediately contact a pediatrician or pediatric allergist-immunologist.
Rashes are treated by one or more methods in combination:
- Antihistamines (relieve swelling, itching, improve general condition)
- Diuretics, which can be used as herbs
- Nervous and sleep stabilizing sedatives
- Sorbents designed to remove the allergen from the body
- Antihistamine ointments, solutions of calcium chloride, diphenhydramine
- Herbal compresses (sometimes it is recommended to bathe a child with an allergic rash in herbal solutions, but this is individual, a specialist consultation is necessary)
- Glucocorticosteroids for severe reactions
When determining the methods of treatment, the doctor relies on the age of the child and his condition.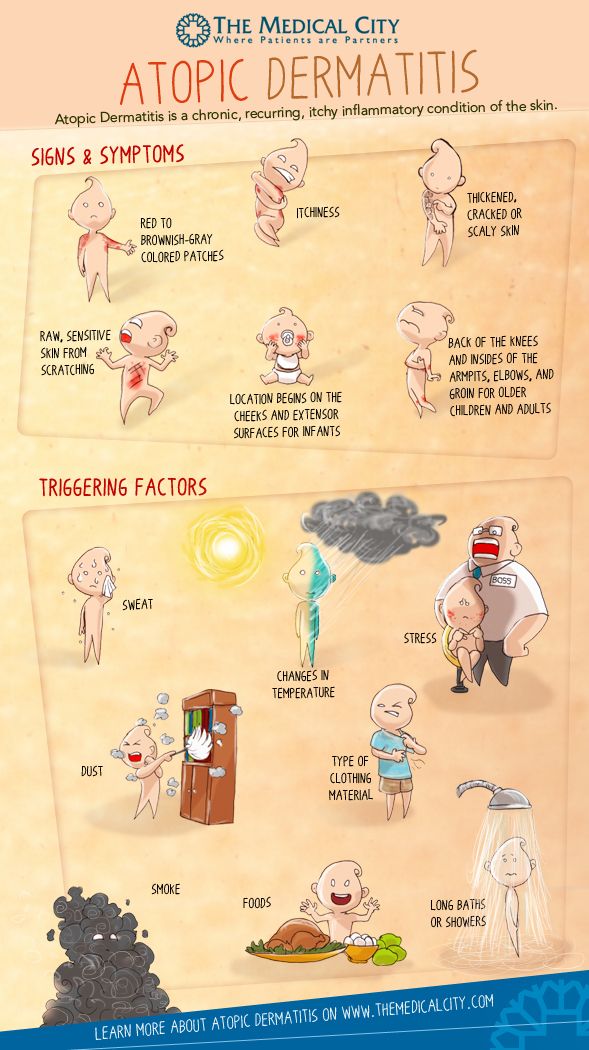 Parents are always worried about the question, after how many days does an allergic rash go away? With timely and proper treatment, the symptoms of allergic dermatoses are eliminated quite quickly, within a few days.
Parents are always worried about the question, after how many days does an allergic rash go away? With timely and proper treatment, the symptoms of allergic dermatoses are eliminated quite quickly, within a few days.
Preventive measures
Proper nutrition of the mother is a preventive measure that reduces the likelihood of developing an allergic reaction in the smallest - newborn babies. The composition of the milk of a nursing mother is affected by the diet of foods that she eats.
If you notice an allergic rash on your hands, cheeks, neck, forearm, do not expect it to spread to the entire area of the skin. As a preventive measure, use the following recommendations:
- Eat approved foods if breastfed
- Perform regular hygiene procedures
- Do not wrap your baby excessively, as overheating provokes prickly heat
- Be sure to wet clean the child's room to prevent dust accumulation
- It is not recommended to keep birds, cats, dogs in the house if the child is prone to allergies
- Strengthen your immune system with a balanced diet
When the first symptoms appear, immediately consult a pediatric allergist or a pediatrician at the Axis Medical Center for advice.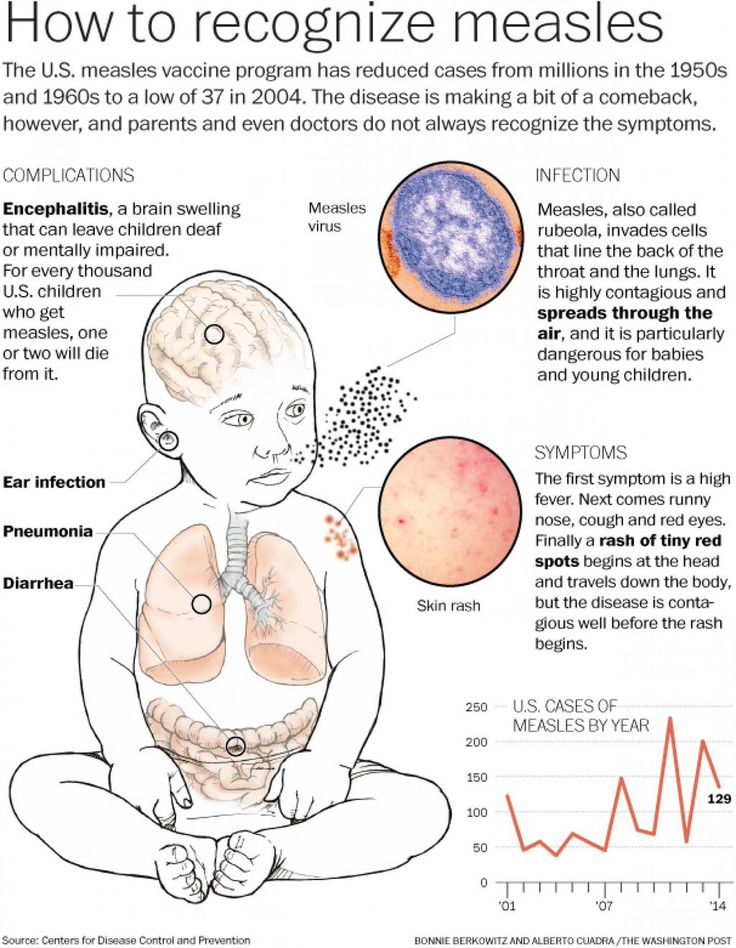
Parental leaflet on viral diseases
Parental leaflet.
Measles is a viral infection with a very high susceptibility. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus is highly volatile. The virus can spread through ventilation pipes and elevator shafts - at the same time, children living on different floors of the house get sick.
The period from contact with a person with measles to the appearance of the first signs of the disease lasts from 7 to 14 days.
The disease begins with a severe headache, weakness, fever up to 40 degrees C. A little later, a runny nose, cough and almost complete lack of appetite join these symptoms.
Very characteristic of measles is the appearance of conjunctivitis - inflammation of the mucous membrane of the eyes, which is manifested by photophobia, lacrimation, sharp redness of the eyes, and subsequently - the appearance of purulent discharge.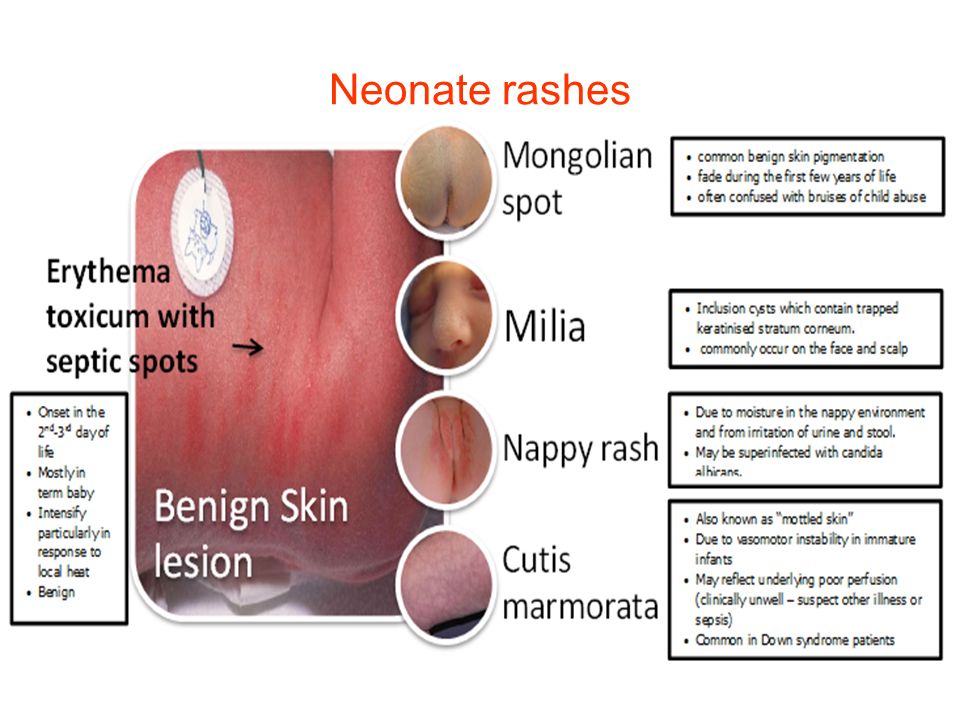 These symptoms last 2 to 4 days.
These symptoms last 2 to 4 days.
On the 4th day of illness, a rash appears , which looks like small red spots of various sizes (from 1 to 3 mm in diameter), with a tendency to merge. The rash occurs on the face and head (it is especially characteristic of its appearance behind the ears) and spreads throughout the body for 3-4 days. It is very characteristic of measles that the rash leaves behind pigmentation (dark spots that persist for several days), which disappears in the same sequence as the rash appears.
Measles can cause serious complications . These include inflammation of the lungs (pneumonia), inflammation of the middle ear (otitis media), and sometimes such a formidable complication as encephalitis (inflammation of the brain).
It must be remembered that after suffering from measles for a sufficiently long period of time (up to 2 months) there is a suppression of immunity, so the child can get sick with some cold or viral disease, so you need to protect him from excessive stress, if possible from contact with sick children.
After measles, lifelong immunity develops. All those who have had measles become immune to this infection.
The only reliable protection against the disease is vaccination against measles, which is included in the National Immunization Schedule.
Parent Guide.
Rubella is an airborne viral infection. As a rule, children who stay in a water room for a long time with a child who is a source of infection get sick. Rubella in its manifestations is very similar to measles, but it is much easier.
The period from contact to the appearance of the first signs of illness lasts from 14 to 21 days.
Rubella begins with an increase in the occipital lymph nodes and an increase in body temperature up to 38 degrees C. A runny nose, and sometimes a cough, joins a little later. A rash appears 2 to 3 days after the onset of the disease. Rubella is characterized by a pink, punctate rash that begins with a rash on the face and spreads throughout the body. Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
The treatment of rubella is to relieve the main symptoms - the fight against fever, if any, the treatment of the common cold, expectorants.
Complications from rubella are rare.
After rubella, immunity also develops, re-infection is extremely rare, but can occur.
Therefore, it is very important to get the rubella vaccine, which, like the measles vaccine, is included in the National Immunization Schedule.
Memo for parents.
Mumps (mumps) is a childhood viral infection characterized by acute inflammation in the salivary glands.
Infection occurs by airborne droplets. Susceptibility to this disease is about 50-60% (that is, 50-60% of those who were in contact and who were not ill and not vaccinated get sick).
It can take 11 to 23 days from contact with a sick mumps to the onset of illness.
Mumps begins with an increase in body temperature up to 39 degrees C and severe pain in or under the ear, aggravated by swallowing or chewing. At the same time, salivation increases. Swelling quickly grows in the area of the upper part of the neck and cheeks, touching this place causes severe pain in the child. Unpleasant symptoms disappear within three to four days: body temperature decreases, swelling decreases, pain disappears.
However, quite often mumps ends inflammation in the glandular organs , such as the pancreas (pancreatitis), gonads. Past pancreatitis in some cases leads to diabetes mellitus . Inflammation of the gonads (testicles) is more common in boys. This significantly complicates the course of the disease, and in some cases may result in infertility. In particularly severe cases, mumps can be complicated by viral meningitis (inflammation of the meninges), which is severe.
After a disease, a strong immunity is formed, but complications can lead to disability.
The only reliable protection against the disease is vaccination against mumps, which is included in the National Immunization Schedule.
Parent Guide.
Varicella (chickenpox) is a common childhood infection. Mostly young children or preschoolers are ill. Susceptibility to the causative agent of chickenpox (the virus that causes chickenpox refers to herpes viruses) is also quite high. About 80% of contact persons who have not been ill before develop chickenpox.
14 to 21 days pass from the moment of contact with a patient with chickenpox until the first signs of the disease appear.
The disease begins with a rash. Usually it is one or two reddish spots, similar to a mosquito bite. These elements of the rash can be located on any part of the body, but most often they first appear on the stomach or face. Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear.
Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear. This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears.
This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears.
Treatment of chickenpox is to reduce itching, intoxication and prevent bacterial complications. The elements of the rash must be lubricated with antiseptic solutions (as a rule, this is an aqueous solution of brilliant green or manganese). Treatment with coloring antiseptics prevents bacterial infection of rashes, allows you to track the dynamics of the appearance of rashes. It is necessary to monitor the hygiene of the mouth and nose, eyes - you can rinse your mouth with a solution of calendula, the mucous membranes of the nose and mouth also need to be treated with antiseptic solutions.
Complications of chickenpox include myocarditis - inflammation of the heart muscle, meningitis and meningoencephalitis (inflammation of the meninges, brain matter), inflammation of the kidneys (nephritis). Fortunately, these complications are quite rare.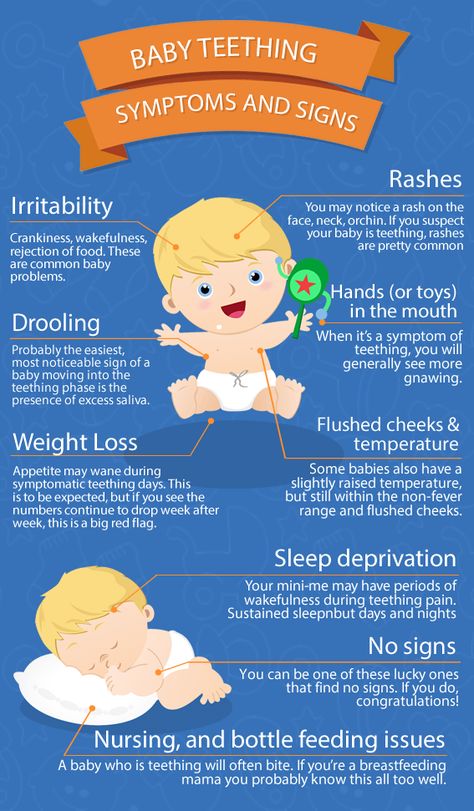 After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
Reminder for parents.
Scarlet fever is the only childhood infection caused not by viruses but by bacteria (group A streptococcus). This is an acute disease transmitted by airborne droplets. Infection through household items (toys, dishes) is also possible. Children of early and preschool age are ill. The most dangerous in terms of infection are patients in the first two to three days of the disease.
Scarlet fever begins very acutely with fever up to 39 degrees C, vomiting, headache. The most characteristic symptom of scarlet fever is tonsillitis, in which the mucous membrane of the pharynx has a bright red color, swelling is pronounced. The patient notes a sharp pain when swallowing. There may be a whitish coating on the tongue and tonsils.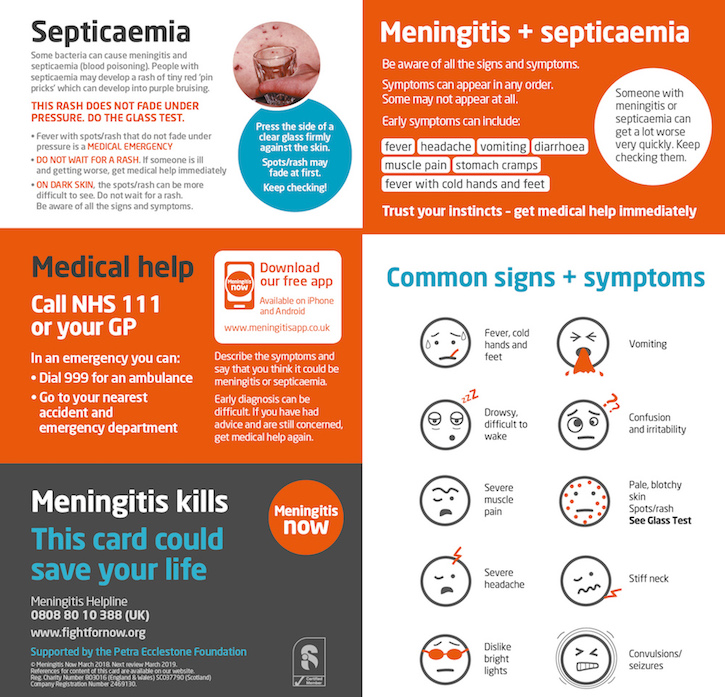 The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
By the end of the first beginning of the second day of illness, 9 appears0115 the second characteristic symptom of scarlet fever is a rash. It appears immediately on several parts of the body, most densely located in the folds (elbow, inguinal). Its distinguishing feature is that the bright red punctate scarlatinal rash is located on a red background, which gives the impression of a general confluent redness. Pressing on the skin leaves a white line . The rash may be spread all over the body, but there is always a clean (white) area of skin between the upper lip and nose, and also the chin. Itching is much less pronounced than with chicken pox.
Rash lasts up to 2 to 5 days. The manifestations of sore throat persist a little longer (up to 7-9 days).
Scarlet fever is usually treated with antibiotics because the causative agent of scarlet fever is a microbe that can be eliminated with antibiotics and strict adherence to bed rest . Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Almost exclusively children suffer from scarlet fever because with age a person acquires resistance to streptococci. Those who have been ill also acquire strong immunity.
Memo for parents.
Whooping cough is an acute infectious disease characterized by a long course. The hallmark of the disease is a spasmodic cough.
The mechanism of transmission of infection is airborne. A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
3 to 15 days pass from the moment of contact with a whooping cough patient until the first signs of the disease appear. Whooping cough feature is a gradual increase in cough within 2 to 3 weeks after its onset.
Typical signs of whooping cough:
- · persistent intensifying cough, gradually turning into spasmodic cough attacks (a series of coughing shocks rapidly following each other on one exhalation) with a convulsive breath, accompanied by a whistling lingering sound. In infants, such a cough can lead to respiratory arrest. Attacks of coughing are worse at night and end in the release of a small amount of viscous sputum, sometimes vomiting;
- puffiness of the face, hemorrhages in the sclera;
- ulcer on the frenulum of the tongue (due to injury from the edges of the teeth, since during a coughing fit the tongue protrudes to the limit, its tip bends upward).
Whooping cough is often complicated by bronchitis, otitis media, pneumonia, rectal prolapse, umbilical and inguinal hernias.
After having had whooping cough for a long time (several months), coughing fits may return, especially if the child catches a cold or during physical exertion.
The only reliable prevention against whooping cough is vaccination with DPT, a vaccine that is included in the National Immunization Schedule. Parents' fears about the harmful effects of the vaccine are unfounded. The quality of the DTP vaccine is not inferior in its properties to vaccines produced in other countries.
Memo for parents.
Acute intestinal infections is a large group of diseases that occur with more or less similar symptoms, but can be caused by a huge number of pathogens: bacteria, viruses, protozoa.
In summer, the number of intestinal infections in children inevitably increases. There are several reasons for this.
There are several reasons for this.
Firstly, , in summer, a large number of raw vegetables, fruits and berries are consumed, on the unwashed surface of which a huge number of microbes, including potentially dangerous ones, live.
Secondly, , children spend a lot of time outdoors in summer, and not always even their parents remember that eating with clean hands is a mandatory rule .
The third reason : in the summer, getting into food (dairy products, meat, fish, broths), some pathogens multiply at a tremendous speed and quickly reach the amount that successfully breaks through the protective barriers of the gastrointestinal tract.
It can take from several hours to 7 days from the moment of introduction of the pathogen into the gastrointestinal tract before the onset of the disease.
The disease begins with fever, malaise, weakness, lethargy. Appetite is sharply reduced, nausea, vomiting quickly joins. The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. Self-medication is not allowed .
Appetite is sharply reduced, nausea, vomiting quickly joins. The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. Self-medication is not allowed .
Prevention of intestinal infections requires strict adherence to general hygiene measures in the home, when preparing food and during meals.
In the summer, all foodstuffs should be protected from flies. Ready food should be stored in the refrigerator: at a low temperature, even if microbes get into the food, they will not be able to multiply. The disease can also be caused by illegibility when buying products that are eaten without heat treatment - from the hands, outside the markets, where they do not pass sanitary control. When swimming in open water, in no case should water be swallowed. If you eat on the beach, wipe your hands with at least special wet wipes.
If you eat on the beach, wipe your hands with at least special wet wipes.
And remember that parental example is the best way to teach a child.
Parent Guide .
Tuberculosis is a chronic infectious disease caused by mycobacterium human tuberculosis, affecting mostly the respiratory organs, as well as all organs and systems of the body.
The source of infection for is people with tuberculosis. The most common is the air way of infection. Transmission factors are nasopharyngeal mucus, sputum and dust containing bacteria.
Reproduction of tuberculosis bacteria in the child's body leads to significant functional disorders with symptoms of intoxication: irritability appears or, conversely, lethargy, fatigue, headache, sweating. With a long course of the disease, the child loses weight, the skin becomes pale, and there is a tendency to inflammatory diseases. For children, a reaction from the lymph nodes is typical: they increase in size, become dense.