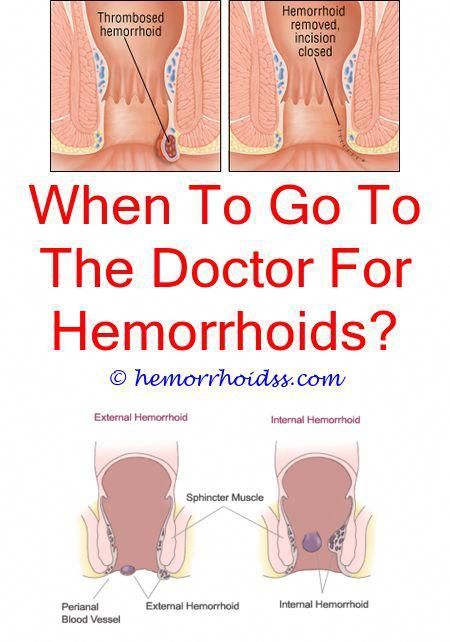
What are pregnancy hemorrhoids
Hemorrhoids During Pregnancy: Causes and Prevention
Hemorrhoids — swollen veins in the anus and rectum — are common during pregnancy, especially in the third trimester when the enlarged uterus puts pressure on the veins.
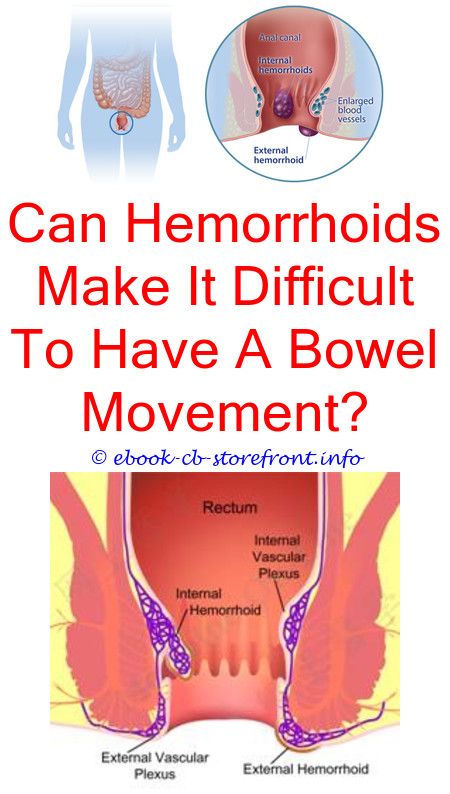
Hemorrhoids can be painful. They may also itch, sting, or bleed, especially during or after a bowel movement.
While your body is going through all sorts of physical changes during pregnancy, hemorrhoids can be one more unwanted irritation. But the good news is that they generally aren’t harmful to your health or the health of your baby, and they’re usually a short-term problem. Though pushing during labor can worsen hemorrhoids, they typically go away on their own after you give birth. (1)
Some women get hemorrhoids for the first time when they’re pregnant. But if you’ve had hemorrhoids before, you’re more likely to get them again when you’re pregnant.
What Can Cause Hemorrhoids During Pregnancy
As your unborn baby grows, your uterus gets bigger and begins to press against your pelvis. This growth puts a lot of pressure on the veins near your anus and rectum, and these veins may become swollen and painful as a result.
The increase in the hormone progesterone during pregnancy can also contribute to the development of hemorrhoids, as it relaxes the walls of your veins, making them more prone to swelling. An increase in blood volume, which enlarges veins, can also contribute to hemorrhoids during pregnancy. (1)
Three common additional causes of hemorrhoids during pregnancy include:
- Straining during bowel movements
- Straining from carrying extra pregnancy weight
- Sitting or standing for long periods of time
Hemorrhoids are most common in pregnant women who experience constipation.
As many as 38 percent of pregnant women become constipated at some point during their pregnancy, according to research published in the journal BMJ Clinical Evidence. (2)
One cause of constipation during pregnancy may be when the growing uterus pushes against the bowel.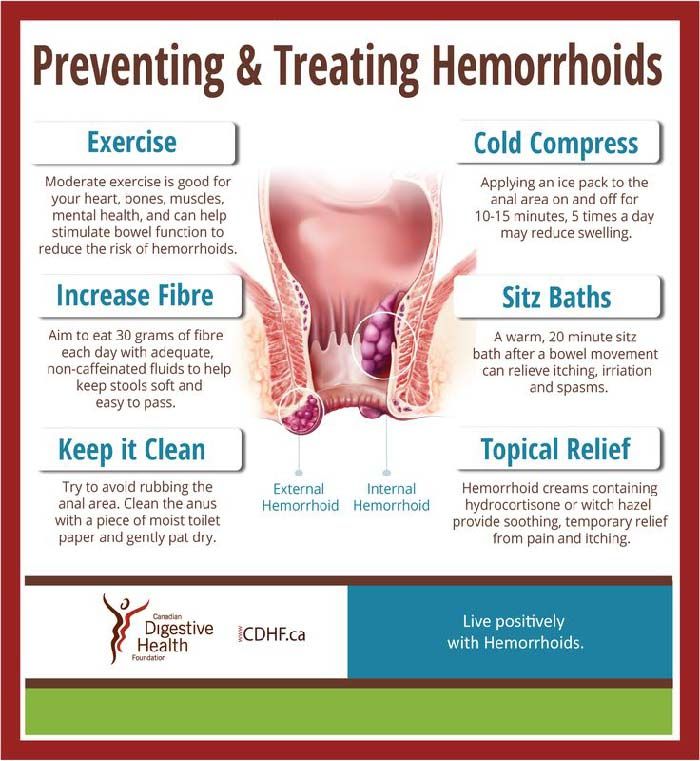 Iron supplements you may take can also contribute to constipation, so it’s worth trying to get the iron you need naturally through your diet. (3)
Iron supplements you may take can also contribute to constipation, so it’s worth trying to get the iron you need naturally through your diet. (3)
Pregnancy hormones can also slow down the movement of food through the digestive tract, making constipation more likely.
How to Prevent Hemorrhoids During Pregnancy
Avoiding constipation is key to preventing hemorrhoids during pregnancy. Here are some tips for preventing constipation:
Eat lots of high-fiber foods. There are plenty of good ways to incorporate more fiber into your diet. Fiber-filled foods include fruits like pears (especially when you include the skin), avocados, and berries; vegetables such as broccoli, artichokes, and Brussels sprouts; whole grains such as oatmeal, brown rice, quinoa, and even popcorn; legumes including various kinds of beans, lentils, and green peas; and don’t forget nuts and seeds.
RELATED: 11 High-Fiber Foods to Add to Your Diet
Drink plenty of fluids. Aim for 10 8-ounce glasses of water each day.
Aim for 10 8-ounce glasses of water each day.
Use the toilet as soon as you feel the urge. “Holding it in” can contribute to constipation.
Try not to sit or stand for long periods of time. If you sit down at work, make sure to get up and walk around for a few minutes every hour. At home, try to rest on your side when reading or watching TV, to relieve downward pressure on your rectal veins.
Ask your doctor about using a stool softener. This can help if other methods fail to ease your constipation. Using laxative pills for constipation is not recommended during pregnancy, as they can cause dehydration and might stimulate uterine contractions. (3)
Do Kegel exercises daily. Kegel exercises strengthen the pelvic floor muscles that help support your rectum and can improve circulation in the rectal area. You can do Kegel exercises just about anywhere — at home, in your car, at the office — but first you need to make sure you’re isolating and contracting the correct muscles.
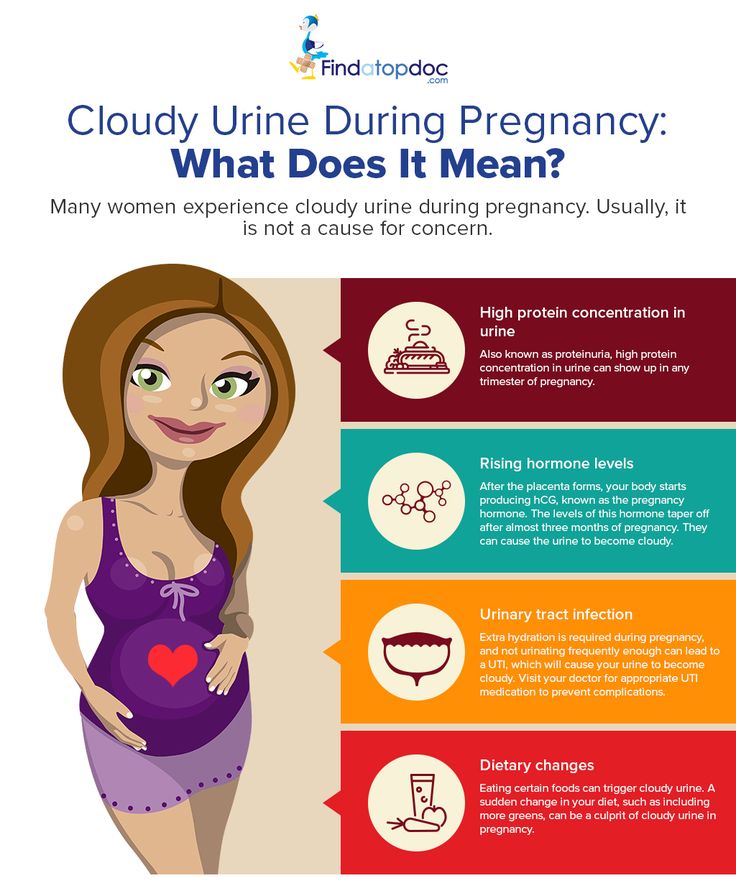
Identify the right muscles by stopping urination midstream. (This is strictly for the purpose of identifying which muscles we’re talking about — you don’t want to do Kegels while urinating, as this could increase your risk for a urinary tract infection). (4)
Once you know which muscles to use, tighten them and hold the contraction for five seconds. Then relax for five seconds. Work up to holding the contraction for 10 seconds. Try to do at least three sets of 10 reps a day.
RELATED: 10 Foods to Help Relieve Constipation
RELATED: Constipation Causes, Symptoms, and Relief
How to Treat Hemorrhoids During Pregnancy
Hemorrhoids usually get better on their own after pregnancy, but there are a number of things you can do to ease any itching and pain in the meantime:
Soak your rectal area in warm water several times a day. A sitz bath, or small basin that fits over the toilet seat, can help. These devices can be purchased at most drug stores. You can also fill your regular bathtub with a few inches of warm water to create a similar effect.
These devices can be purchased at most drug stores. You can also fill your regular bathtub with a few inches of warm water to create a similar effect.
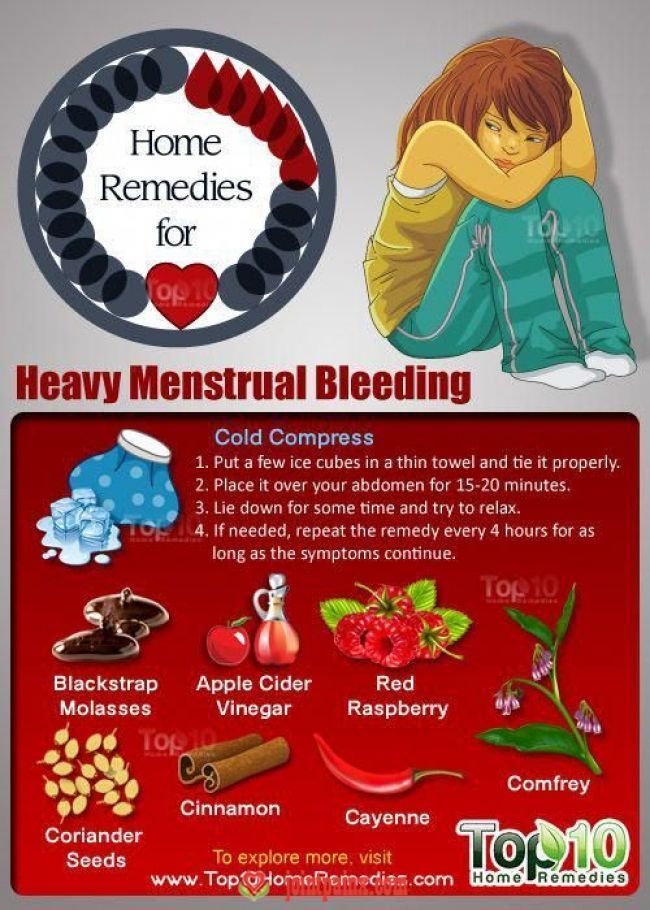
Apply ice packs or cold compresses to the area several times a day. The cold can reduce swelling and help relieve pain.
Keep the anus clean and dry. Try using moist towelettes or baby wipes to gently clean the area after bowel movements. This can be more gentle than dry toilet paper.
Be sure to pat — not wipe — the area dry after bathing or making a bowel movement. Excess moisture can cause irritation.
Apply baking soda (wet or dry) to the area to alleviate itching. (3)
Apply treatments containing witch hazel. Products like Tucks Medicated Cooling Pads can help keep the area clean and relieve pain and itching around the anus.
But before you use any products, be sure to ask your doctor or healthcare provider to recommend a topical hemorrhoid cream or medicated wipe that’s safe to take during your pregnancy.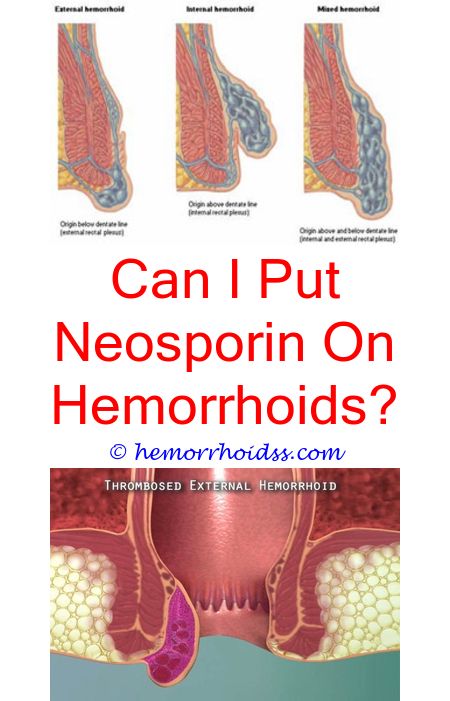
Additional reporting by Deborah Shapiro.
What Are Hemorrhoids? Symptoms, Causes, Diagnosis, Treatment, and Prevention
By Lindsey KonkelTreatment for Hemorrhoids
Most hemorrhoids can be treated at home or with simple medical procedures.
By Lindsey Konkel
8 Myths You’ve Been Told About Hemorrhoids
By Mikel TheobaldHow to Ease Ulcerative Colitis Symptoms During a Flare
Abdominal pain and diarrhea are just two of the unpleasant symptoms that can occur during an ulcerative colitis flare. Here’s what you can do to ease ...
By Marie Suszynski
Enjoying the Outdoors While Living With IBD
By Jenny HarrisonWhat to Eat and What to Avoid When You Have Diarrhea
Some foods can make diarrhea worse, and others can keep you nourished while you’re getting better. Learn what to eat and drink to get through a bout of...
Learn what to eat and drink to get through a bout of...
By Beth W. Orenstein
Gut Check: Is Bee Propolis Good for Your Gut Microbiome?
Health influencers claim the bee product has a number of benefits for humans, but while research is promising, it is still in early stages. Here’s what...
By Ashley Welch
Dealing with hemorrhoids during pregnancy
Hemorrhoids can also result from constipation since pregnancy hormones cause your bowels slow down. When stool is hard, the extra straining to eliminate it can put pressure on veins in your rectal area, causing them to become inflamed and bulge. "On top of that, higher progesterone levels cause the walls of the veins to relax and allow them to swell more easily," says Dr. Harris.
If you had hemorrhoids before pregnancy, you're more likely to have them during pregnancy. They can also develop postpartum because of pushing during labor.
They can also develop postpartum because of pushing during labor.
How can you prevent hemorrhoids during pregnancy?
Your body undergoes a lot of changes when you're expecting, and swelling veins can be one of them. Talk to other expectant moms during prenatal classes, share experiences or ask your instructor about natural remedies.
These steps may help you avoid hemorrhoids during pregnancy:
Avoid constipation
- Eat a high-fiber diet. Choose from fresh avocados, beans, and other fruits and vegetables.
- Don't delay going to the bathroom when you feel the urge. Make sure you don't sit on the toilet longer than necessary because this puts pressure on your rectal area.
- If you're already constipated, ask your healthcare provider about a fiber supplement or stool softener.
- Choose a food-based prenatal vitamin. Synthetic vitamins, especially iron, can cause constipation. Food-based prenatal vitamins are more absorbable.
Keep moving
- Get regular (and safe) exercise right up to your due date — as long as your provider says it's OK.
- Do Kegel exercises. They increase circulation in the rectal area and strengthen the muscles around the anus.
- Don't sit or stand for long stretches of time. If your job involves sitting at a desk, get up and move around for a few minutes every hour or so.
Promote good habits
- Drink plenty of water and other fluids. If you aren't drinking enough, your body will reabsorb water through the colon, leaving dry stool that's hard to push out.
- Lie on your side when sleeping, reading or watching TV to take the pressure off your rectal veins.
- Try not to gain more than the recommended amount of weight because the more you gain, the more pressure on the rectum.
How can you treat symptoms during pregnancy?
If you experience symptoms, try one of these remedies:
- Cold therapy can help reduce swelling and bring temporary relief.
 Apply an ice pack (with a covering) to the affected area.
Apply an ice pack (with a covering) to the affected area. - Soak in warm water several times a day. If you don't have a bathtub, you can buy a sitz bath. After getting out of the tub, pat the area dry.
- If sitting is uncomfortable, get a donut-shaped pillow to ease the pressure.
- Apply witch hazel pads to the area and change the pads frequently. Witch hazel has a cooling effect and helps reduce swelling.
- Baking soda – used wet or dry – can be applied topically to help alleviate itching.
- Coconut oil can relieve pain and inflammation. So can pure aloe vera without added chemicals and fragrances, or arnica.
- Stay clean and use soft, unscented toilet tissue or unscented wipes to avoid more irritation in the affected area.
- Acupuncture can also help.
When should you see your healthcare provider?
Consult your provider if preventive efforts and home treatments don't help, or if you have severe pain or rectal bleeding. In some cases, you may need professional help shrink your hemorrhoids.
In some cases, you may need professional help shrink your hemorrhoids.
Also, always check with your provider before taking any medication for hemorrhoids while you're pregnant. There are a lot of hemorrhoid relief products available. Keep in mind that most of these products should be used for no more than a week to avoid such side effects as skin irritation or thinning.
For many women, hemorrhoid symptoms resolve after delivery. If they persist, surgical treatment might be recommended.
Treatment of hemorrhoids during pregnancy | Articles of the medical center "SM-Clinic"
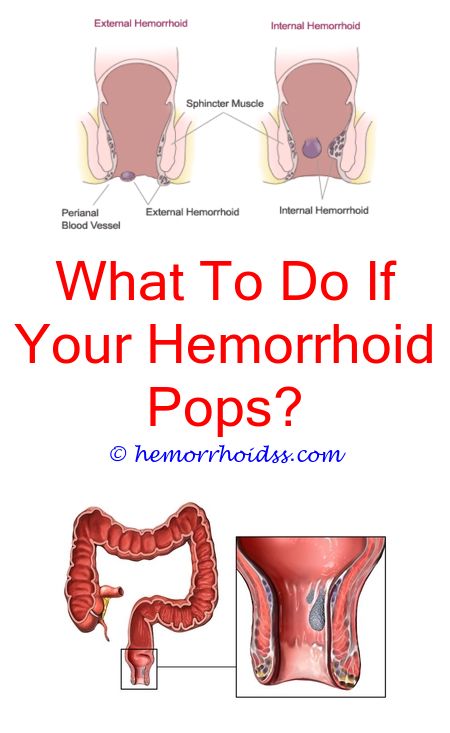
Hemorrhoids - a disease associated with inflammation and pathological expansion of the hemorrhoidal veins that form knots around the rectum. This is a very common disease, its cause is usually venous blood stagnation in the lower body and legs.
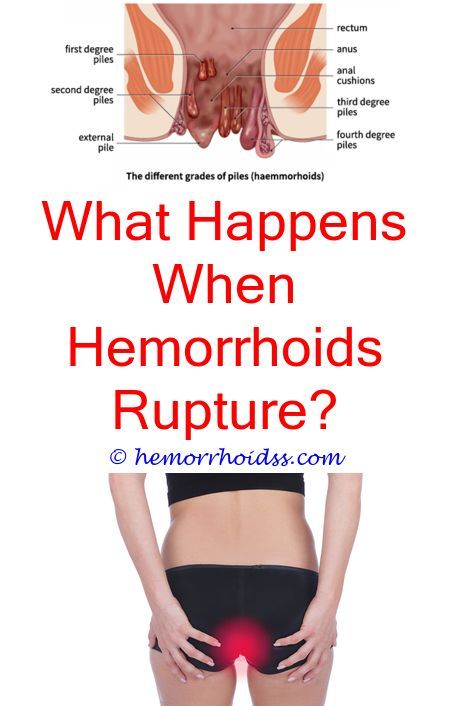
The development of hemorrhoids takes place gradually - in the initial stage, there is heaviness and itching in the anus, pain, constipation, later - bleeding, sagging and prolapse of elastic hemorrhoids.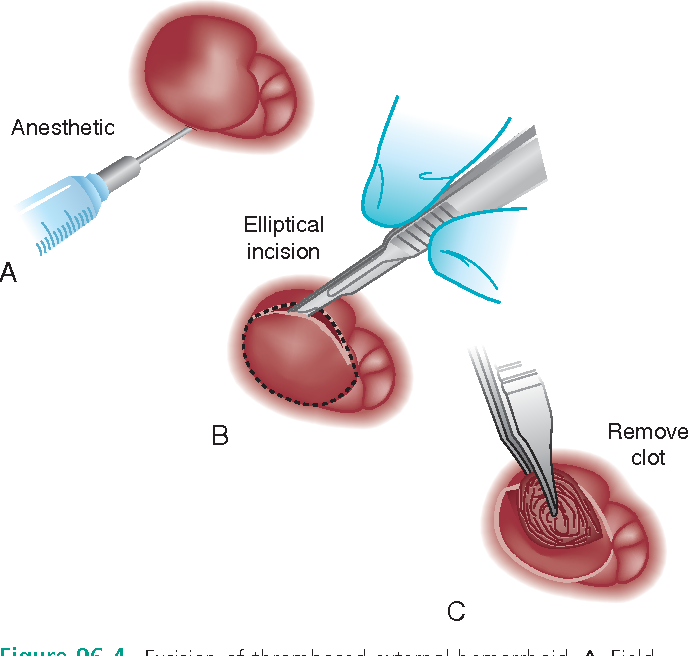
Factors that cause hemorrhoids are a sedentary lifestyle, unhealthy diet, obesity, alcohol abuse, cirrhosis of the liver of life.
This disease often accompanies pregnancy - about half of women who are expecting a child suffer from it. The main reasons for pregnant women are the pressure of the growing uterus on the lower abdomen, which compresses the veins, and constipation due to low intestinal motility.
In healthy women, hemorrhoids can develop in the second half of pregnancy, but if there is a hereditary predisposition, or the symptoms of hemorrhoids were manifested before pregnancy, then hemorrhoids can develop at an earlier date - already from the 12th week.
Symptoms of hemorrhoids during pregnancy
Hemorrhoids during pregnancy can occur in two forms:
- acute;
- chronic.
The acute form is characterized by the sudden formation of a blood clot in the veins of the rectum, which causes burning pain, especially after the defecation process. Dense external nodes are formed, the diameter of which can reach 2-3 cm, the skin under them swells and turns red.
Dense external nodes are formed, the diameter of which can reach 2-3 cm, the skin under them swells and turns red.
After 5-10 days, the acute form becomes chronic - the nodes soften and swell only when straining. The process is accompanied by discomfort in the anus and itching.
Blood appears in the fecal masses, sometimes in fairly large quantities, hemorrhoids can fall out of the anus, self-adjusting after some time. There may be no pain, there may be a feeling of incomplete emptying of the intestine, discomfort, bloating. Walking and sitting become painful.
Treatment of hemorrhoids during pregnancy
The main methods of treatment of non-acute hemorrhoids during pregnancy are strict adherence to diet and hygiene rules. The diet prescribed by a dietitian should help avoid constipation and regulate bowel movements - dried fruits, nuts, cereals, and sour-milk products are recommended for this. Spicy foods, rich products, strong tea should be excluded.
For hygiene procedures, it is recommended to use wet toilet paper, wash the anus after defecation. If external nodes occur, you can take baths with a weak solution of chamomile or potassium permanganate.
To reduce blood stasis, it is necessary to perform preventive gymnastics - its main exercises should be aimed at stimulating the muscles of the pelvis, anus and legs. In addition, it is necessary to adjust the daily routine - to take walks, combining them with moderate rest and sleep.
If these measures do not bring the desired result, it is possible to use medicines - suppositories, ointments, creams. However, it is worth remembering that any drug treatment must be agreed with the gynecologist - during pregnancy, self-medication and the use of drugs without a prescription is unacceptable.
If conservative treatment is ineffective, surgery may be required, but usually during gestation it is performed only in extreme cases, with careful monitoring of the proctologist and surgeon.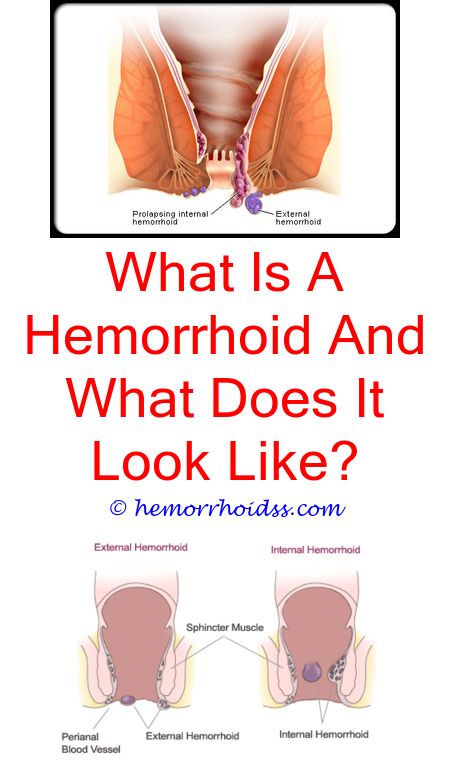 Usually, if there is a need for surgical intervention, the operation is postponed until the postpartum period.
Usually, if there is a need for surgical intervention, the operation is postponed until the postpartum period.
After childbirth, during the first two months, hemorrhoids may continue to bother, but usually - with the normalization of lifestyle and increased physical activity - it disappears. However, you should not run hemorrhoids during pregnancy - at the first sign, consult a doctor.
This will help to avoid complications, reduce discomfort, and also distinguish the disease from those that occur with similar symptoms (anal fissures, tumors), but require different treatment.
To learn more and sign up for a consultation with a specialist, you can call +7 (495) 292-39-72
Hemorrhoids in pregnancy: causes, symptoms, treatment
Despite the fact that hemorrhoids are more common in men than in women, there is a category of patients susceptible to this disease due to a special situation - pregnancy. Hemorrhoids in pregnant women occur mainly in the 2nd or 3rd trimester, as well as in the postpartum period.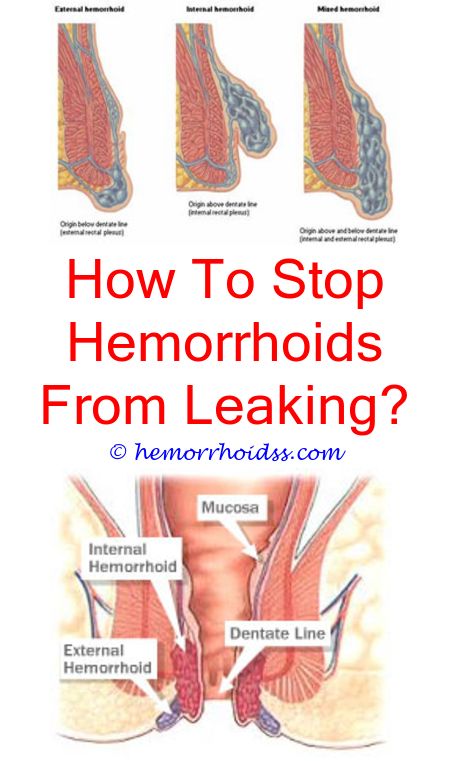 This vascular disease is associated with inflammation of internal or external hemorrhoids due to impaired venous outflow.
This vascular disease is associated with inflammation of internal or external hemorrhoids due to impaired venous outflow.
Causes of hemorrhoids during pregnancy
The development of hemorrhoids in expectant and young mothers is promoted by many factors that are associated with the physiological changes that occur in a woman's body during the period of bearing a child and after childbirth. These factors include:
- Changes in hormonal levels - increased estrogen levels weaken the muscle tone of the vascular wall
- Enlargement of the uterus - leads to an increase in venous pressure
- Hereditary predisposition
- Age of the future mother - in pregnant women aged 20-30 years, hemorrhoids are detected in 20% of cases, after 30 years - in 50% of cases.
- Frequent constipation
- Decreased or inactive physical activity
- Birth process - during childbirth, compression of blood vessels in the pelvic area occurs, which can lead to prolapse or rupture of hemorrhoids.
Symptoms of hemorrhoids in pregnancy
Experts report that some pregnant women may have asymptomatic hemorrhoids. In the rest, the disease usually manifests itself in the 2nd and 3rd trimesters of pregnancy. The main symptoms are:
- slight bleeding
- burning and anal itching
- discomfort and foreign body sensation
- pain during bowel movements
- in difficult cases - prolapse of internal hemorrhoids, the appearance of anal fissures, more abundant bleeding.
What is the danger of hemorrhoids in pregnant women
If you let the course of hemorrhoids in a pregnant woman take their own course, this can lead to serious consequences for the health of the fetus and expectant mother. Therefore, it is necessary to treat hemorrhoids at all stages.
Prolapsed hemorrhoids can cause venous rupture, anemia, and other complications that affect fetal development.
Constant constipation, straining with hemorrhoids lead to chronic spasm of the anal sphincter muscles and contributes to the formation of anal fissures.
Against the background of impaired blood circulation, hemorrhoidal thrombosis occurs, which, if left untreated, can lead to necrosis of the hemorrhoids.
Pregnant women need to be constantly monitored by a gynecologist and proctologist in order to detect signs of hemorrhoids in time and start treatment in the early stages.
Features of the treatment of hemorrhoids in pregnant women
The treatment of hemorrhoids in pregnant women requires a special approach. During pregnancy, there are many contraindications for the use of many medicines. Not all medicines, suppositories and ointments that are commonly used in the treatment of hemorrhoids are allowed for pregnant women. Such standard methods of stopping bleeding and treating hemorrhoids as sclerotherapy and laser coagulation are prohibited.
At the consultation of a proctologist, women who are carrying a child will be given an individual treatment in accordance with the current condition of the patient and taking into account the entire clinical picture.
In mild forms of hemorrhoids, pregnant women are prescribed special suppositories and ointments approved for use during pregnancy. Also, for the treatment of hemorrhoids in pregnant women, the doctor prescribes maintaining a special diet (consumption of foods with a high fiber content), increasing physical activity (swimming, walking), maintaining “wet” hygiene (using wet toilet paper and a hygienic shower).
Every woman carrying a child should be aware of the possible consequences of self-treatment or lack of treatment of a particular problem. If any alarming symptoms occur, as well as as a preventive measure, it is necessary to make an appointment with a specialist proctologist.
At the Naedine Clinic, you will be assisted by qualified gynecologists and proctologists who will conduct an accurate diagnosis and prescribe an effective and safe treatment.