Getting induced what to expect
I’m Being Induced! What Should I Expect?
Home / Community / News Releases / Maternity / I’m Being Induced! What Should I Expect?
Posted on
The goal of any healthcare practitioner is to carry all pregnancies to term, or 39 weeks. This means that generally speaking, labor shouldn’t be induced electively before that time—however, certain situations can come up when your body’s natural processes need a little nudge in the right direction.
What Does It Mean to be Induced?Being induced simply means that your labor contractions are started using medications or other methods because they aren’t starting naturally. There are a series of steps your doctor will follow to try to induce your labor, and most women don’t have to go through all of them!
Reasons Your Doctor Might Induce LaborYour baby is overdue.
If it’s time for your baby to make their debut, but there are no signs of action from your body, your doctor might induce labor around the 42-week mark.
You’re experiencing complications.
Conditions like preeclampsia, diabetes or gestational diabetes, issues with your placenta, or problems with your amniotic fluid make it risky to keep carrying your pregnancy. Your doctor may choose to induce your labor as soon as it’s safe to reduce the effects of these risks.
Broken water, but no contractions.
If your water has broken, but your contractions don’t start on their own within 24 hours, your doctor might need to get them started for you.
You live far from the hospital.
If you live far away from your hospital, your doctor might choose to induce labor to minimize the risk of not making it in time. On average, second-time moms experience much shorter labor than they did during their first time—so if your first baby came very quickly, your doctor might decide to induce your second to make sure you’re at the hospital when you need to be. This is known as an elective induction because it’s planned ahead of time and occurs no earlier than 39 weeks.
As mentioned above, there are a series of steps your doctor will go through to induce your labor. It’s fairly rare that a doctor has to go through every step to jumpstart your labor, but it is possible.
The first thing your doctor will try is ripening your cervix. Typically in natural labor, your cervix will open up, soften, and thin out in preparation for your baby. Your doctor might have to move things alone themselves, and they’ll do this by applying a topical form of the hormone prostaglandin to your cervix. After a few hours, labor could be well on its way—if it isn’t, your doctor will continue down the chain of steps toward successfully inducing your labor.
If your amniotic sac is still intact, meaning your water hasn’t broken, your doctor may get things started by swiping their finger across the fine membranes that connect it—the goal here isn’t to break your water, although that’s a possibility. Your doctor’s goal is to encourage your uterus to release prostaglandin as you would naturally if your labor was starting. This should cause your cervix to soften, and your contractions to start. This is called “membrane stripping.”
This should cause your cervix to soften, and your contractions to start. This is called “membrane stripping.”
If your cervix has started dilating, but your water hasn’t broken yet, your doctor might break it artificially. They’ll do this with an instrument that looks like a long crochet hook with a sharp tip—but don’t worry, while it might not be the most comfortable experience, it shouldn’t be painful.
If nothing your doctor tries is bringing on regular contractions, they will slowly start to give you Pitocin via IV. Pitocin is a synthetic form of the naturally occurring hormone oxytocin and should induce contractions. Contractions typically start about 30 minutes after you’ve been given the medication, and they’re usually stronger, more regular, and more frequent than natural labor contractions. If you’d like an epidural, you should ask your doctor about getting that started while the Pitocin is being administered, so that it’s ready to go once your labor starts.
When is a C-Section the Best Option?There are exceptions to every rule when it comes to pregnancy and the human body, which means that there are certain situations where labor shouldn’t be induced—in these situations, your doctor will recommend a c-section instead. Here are a few reasons you might have a c-section instead of being induced:
Here are a few reasons you might have a c-section instead of being induced:
- If there’s a need for immediate delivery, i.e. there’s no time to waste
- If there’s any doubt at all that your baby can fit through your pelvis
- If you’ve had a c-section before, and now you’re attempting a vaginal birth
- If the placenta is near or covering your cervix
- If there’s a prolapsed cord, i.e. it has slipped down into the vagina before the baby’s head
- If you’re experiencing a genital herpes outbreak
- If you’re carrying multiple babies
- If your baby is breech
Keep in mind that your doctor’s goal is to minimize interventions as best they can, and will only induce your labor or recommend a c-section if they decide it’s necessary.
Looking for more pregnancy advice? Visit our website today.
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery.
 Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
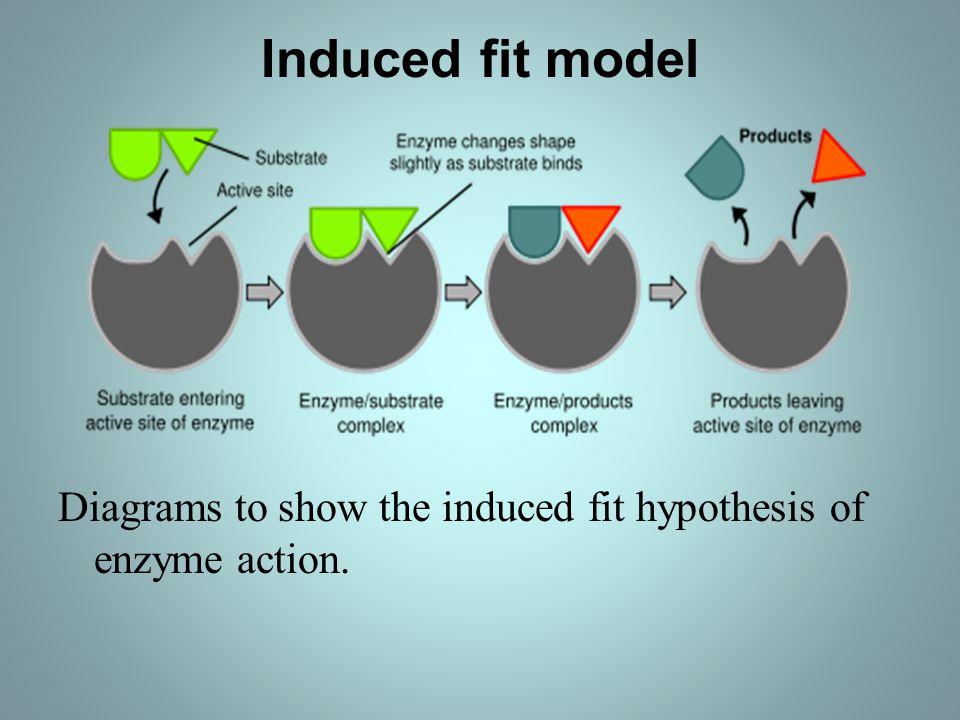
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
What to expect in 2022?
No one should be surprised if we say that 2021 has been one of the most turbulent years in the history of the information security industry. There were several high-profile cyber-attacks during the year. Many believe that cybercriminals led to the first death of a person caused directly by a ransomware attack - in the summer, the Wall Street Journal reported the first death from a ransomware in a hospital in Alabama (USA). In addition, many companies around the world have lost hundreds of billions of dollars due to ransomware. The number of data breaches that have been publicly reported has surpassed that of 2020, and this year is close to being the year of record breaches in history. Information about the next data breach in any company or organization, regardless of its size (small, medium or large), often made headlines in the media. And, according to WatchGuard experts, 2022 is likely to be as turbulent as 2021 .
In addition, many companies around the world have lost hundreds of billions of dollars due to ransomware. The number of data breaches that have been publicly reported has surpassed that of 2020, and this year is close to being the year of record breaches in history. Information about the next data breach in any company or organization, regardless of its size (small, medium or large), often made headlines in the media. And, according to WatchGuard experts, 2022 is likely to be as turbulent as 2021 .
State Sponsored Attacks
2021 has shown us that cyberattacks against critical infrastructure can impact masses of people and have real catastrophic consequences. In 2021, for example, cyber-attacks triggered a fuel buying panic on the US East Coast and temporary meat supply issues with the world's largest meat producer. State-sponsored hackers are aware of their potential and will most likely look for ways to strike critical infrastructure in 2022 .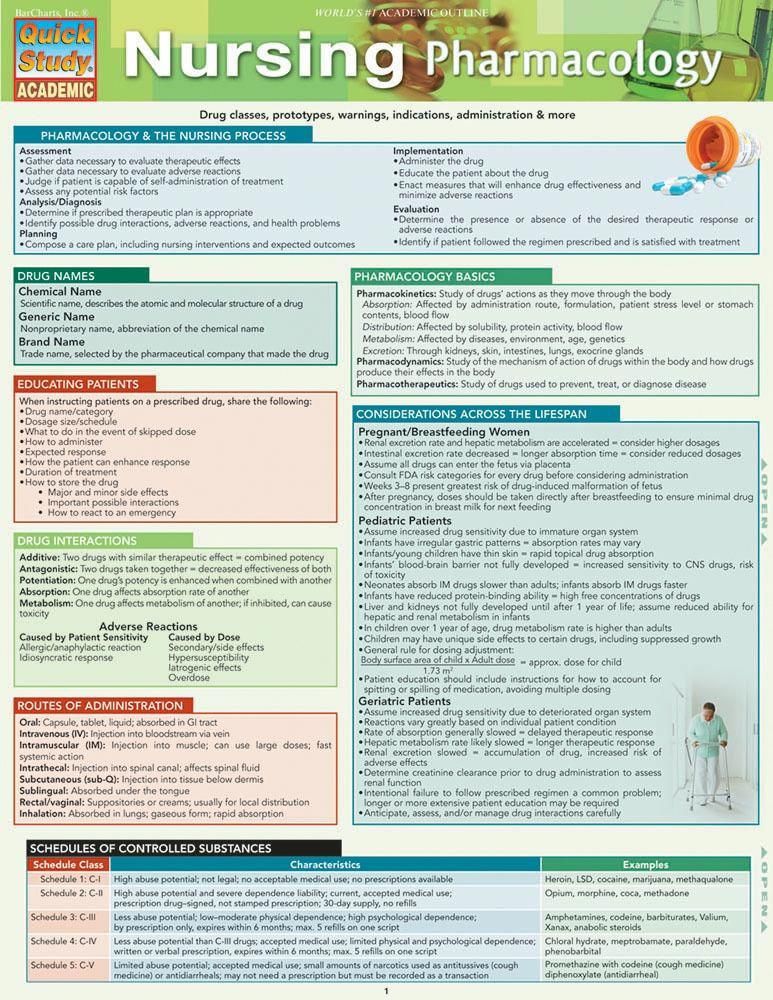 Such cyber-attacks are capable of triggering a war without firing a single live bullet. In this regard, the governments of all countries of the world must monitor their basic infrastructure.
Such cyber-attacks are capable of triggering a war without firing a single live bullet. In this regard, the governments of all countries of the world must monitor their basic infrastructure.
Space cyber attacks
Leading countries have been very active lately when it comes to space. For example, less than two years ago, the US even founded the United States Space Force (USSF). With so much attention being paid to the outside world, WatchGuard draws attention to the fact that in 2022 the probability of "hacking in space" will be very high . Both private organizations and government agencies are involved in the space race, and one way or another, hackers may find their way there too. Some of the satellites that fly over the Earth are relatively outdated and their ability to meet today's protection and safety requirements is questionable.
SMSishing or SMS phishing
SMS phishing has been around for quite some time. Experts believe that 2022 will be no exception to this threat. Many believe that attacks will become even more sophisticated . Over the next year, cybercriminals will continue to impersonate other people to trick unsuspecting users into clicking on malicious links. More and more companies are relying on messaging apps to interact with employees. Many people share sensitive information in these messengers, so it is necessary to ensure that mobile phones are well protected. Don't leave an open door for cyber-attackers and avoid clicking on links that look suspicious. This can cost you dearly, both personally and professionally.
Many believe that attacks will become even more sophisticated . Over the next year, cybercriminals will continue to impersonate other people to trick unsuspecting users into clicking on malicious links. More and more companies are relying on messaging apps to interact with employees. Many people share sensitive information in these messengers, so it is necessary to ensure that mobile phones are well protected. Don't leave an open door for cyber-attackers and avoid clicking on links that look suspicious. This can cost you dearly, both personally and professionally.
Failures in passwordless authentication methods
Many companies, including Microsoft, have begun implementing ways for users to interact with services and platforms without the use of passwords. As with any new technology, the start will not be easy, and the more companies that adopt similar practices, the more likely we are to see such practices fail. Of course, pioneers can always be admired, but, unfortunately, they are the ones to blame if something goes wrong. It won't be a surprise if in 2022 we see hackers who somehow find way to cause damage bypassing such authorization methods .
It won't be a surprise if in 2022 we see hackers who somehow find way to cause damage bypassing such authorization methods .
Cryptocurrencies and mobile wallets
It looks like cryptocurrencies will be with us for a long time . The adoption of mobile wallets will continue and crypto may even become mainstream eventually. This will no doubt continue to attract the attention of cyber criminals. Attacks can take many forms: users may be prompted to download malicious mobile applications or infected after visiting an insecure site. Hackers can be very creative and explore other routes, but the end goal is usually the same - to gain access to their victims' digital wallets. Cryptocurrencies are not easy to track, so the theft of this kind of funds is even a priority for cyber criminals . In 2022, we will most likely see an increase in the number of cyber attacks related to cryptocurrencies and digital wallets.
The coming year 2022 will indeed be as turbulent as 2021 . Will we see more high-profile hacks and attacks on ordinary people? Maybe yes. Especially in the context of the ongoing Covid 19 coronavirus pandemic, humanity will continue to rely on the Internet in daily life. While the remote nature of communication may be safer as all people avoid contracting the new virus, more people going digital will also mean more opportunities for troublemakers to attack.
Will we see more high-profile hacks and attacks on ordinary people? Maybe yes. Especially in the context of the ongoing Covid 19 coronavirus pandemic, humanity will continue to rely on the Internet in daily life. While the remote nature of communication may be safer as all people avoid contracting the new virus, more people going digital will also mean more opportunities for troublemakers to attack.
Cloud solutions
[email protected]https://www.cloudav.ru
The world is going crazy, but it's not too late to fix it. Subscribe to the SecLabnews channel and do your part to prevent the cyber apocalypse!
Childbirth - what to expect really? | Libresse
So you're getting ready to give birth
Becoming a mother is a truly special experience full of excitement and happiness. But you can also experience stress and fear – especially at a time like this.
Your body is changing, your emotions are changing quickly - and this is easy to understand, because you are preparing for childbirth during a global pandemic. All this (and more!) when you know your life is about to change forever. It's not hard to see how frightening this can be.
All this (and more!) when you know your life is about to change forever. It's not hard to see how frightening this can be.
Even in a situation where social distancing has to be maintained, which has created a whole host of new challenges, you can still have a positive experience of having a baby. In the end, you are still in control of your choices.
Fortunately, you are not alone. Every woman who experiences pregnancy and childbirth today is going through changes and emotions like yours.
Your body changes during pregnancy
The obvious changes in your body during pregnancy are hard to miss. But a lot goes on behind the scenes. From the moment you conceive, your uterus, vagina, and vulva prepare for the birth of your baby.
Many women notice that their labia changes color and size during pregnancy. Others feel changes in the size of their vagina. It's just the way your body prepares for childbirth. All this is quite natural and normal.
If your delivery is vaginal, there may be other changes. Women's bodies are designed to make childbirth possible, the vagina is structurally capable of stretching, but some tears during childbirth are still common. As one mom told us in our project #StoriesVinsideUs: "It's like a cozy garden full of beautiful flowers that suddenly changed forever." If you've had a rupture - or had an episiotomy (an incision made to reduce the damage that a natural tear might cause) - you can get stitches, and they can change the look of your vulva and how you feel during sex.
Women's bodies are designed to make childbirth possible, the vagina is structurally capable of stretching, but some tears during childbirth are still common. As one mom told us in our project #StoriesVinsideUs: "It's like a cozy garden full of beautiful flowers that suddenly changed forever." If you've had a rupture - or had an episiotomy (an incision made to reduce the damage that a natural tear might cause) - you can get stitches, and they can change the look of your vulva and how you feel during sex.
Pain or dryness is common but luckily improves over time and lubricants can help. Many women also experience weakening of the pelvic floor, which can affect the ability to regulate excretory functions. Indeed, vaginal delivery increases the chances of incontinence by 2-3 times [1].
Treat your body with love after childbirth
Society puts a lot of pressure on women to "return to shape" after birth. As one woman told us, "I was surrounded by diet and fitness advice, it felt like I had all these expectations of my body. "
But as any mother who has recently given birth will tell you, "getting back into shape" is a ridiculous expectation. Your body has done an incredible job of carrying and delivering a baby, and now it needs time to heal itself.
In time your body will recover and change again. Not to the same shape that was before the baby was born, but to a new, normal one for you. This may mean that your vulva will look different. Or your vagina will feel different. Or something completely different. All of these changes are part of having a baby, which can ultimately also change who you are and how you see the world at the deepest level.
So even though you may be pressured to look a certain way after giving birth, remember that you have had a baby. This is your time to take care of yourself and nurture your body, accepting all the changes that come with your creation of a small life.
As one mother told us: “Being a mother is wonderful. Why look at stretch marks as what we are “left with”? This is what we have acquired.