Radiation when pregnant
Radiation and Pregnancy: Information for Clinicians
This overview provides physicians with information about prenatal radiation exposure as an aid in counseling pregnant women.
How to use this document
This information is for clinicians. If you are a patient, we strongly advise that you consult with your physician to interpret the information provided, as it may not apply to you. Information on radiation exposure during pregnancy for members of the public can be found on the Health Information for Specific Groups webpage.
CDC recognizes that providing information and advice about radiation to expectant mothers falls into the broader context of preventive healthcare counseling during prenatal care. In this setting, the purpose of the communication is always to promote health and long-term quality of life for the mother and child.
This page is also available as a PDF pdf icon[365 KB]
Radiation exposure to a fetus
Most of the ways a pregnant woman may be exposed to radiation, such as from a diagnostic medical exam or an occupational exposure within regulatory limits, are not likely to cause health effects for a fetus. However, accidental or intentional exposure above regulatory limits may be cause for concern.
Although radiation doses to a fetus tend to be lower than the dose to the mother, due to protection from the uterus and surrounding tissues, the human embryo and fetus are sensitive to ionizing radiation at doses greater than 0.1 gray (Gy). Depending on the stage of fetal development, the health consequences of exposure at doses greater than 0.5 Gy can be severe, even if such a dose is too low to cause an immediate effect for the mother. The health consequences can include growth restriction, malformations, impaired brain function, and cancer.
Estimating the Radiation Dose to the Embryo or Fetus
Health effects to a fetus from radiation exposure depend largely on the radiation dose. Estimating the radiation dose to the fetus requires consideration of all sources external and internal to the mother’s body, including the following:
- Dose from an external source of radiation to the mother’s abdomen.

- Dose from inhaling or ingesting a radioactive substance that enters the bloodstream and that may through the placenta.
- Dose from radioactive substances that may concentrate in maternal tissues surrounding the uterus, such as the bladder, and that could irradiate the fetus.
Most radioactive substances that reach the mother’s blood can be detected in the fetus’ blood. The concentration of the substance depends on its specific properties and the stage of fetal development. A few substances needed for fetal growth and development (such as iodine) can concentrate more in the fetus than in corresponding maternal tissue.
Consideration of the dose to specific fetal organs is important for substances that can localize in specific organs and tissues in the fetus, such as iodine-131 or iodine-123 in the thyroid, iron-59 in the liver, gallium-67 in the spleen, and strontium-90 and yttrium-90 in the skeleton.
Radiation experts can assist in estimating the radiation dose to the embryo or fetus
Hospital medical physicists and health physicists are good resources for expertise in estimating the radiation dose to the fetus. In addition to the hospital or clinic’s specialized staff, physicians may access resources from or contact the following organizations for assistance in estimating fetal radiation dose.
In addition to the hospital or clinic’s specialized staff, physicians may access resources from or contact the following organizations for assistance in estimating fetal radiation dose.
- The National Council on Radiation Protection and Measurementsexternal icon’ Report No. 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013] provides detailed information for assessing fetal doses from internal uptakes.
- The International Commission on Radiological Protection’s “Publication 84: Pregnancy and Medical Radiation”external icon [ICRP2000] provides fetal dose estimations from medical exposures to pregnant women.
- The Conference of Radiation Control Program Directorsexternal icon maintains a list of state Radiation Control/Radiation Protection program contact information.
- The Health Physics Societyexternal icon maintains a list of active certified Health Physicists.
- The American Association of Physicists in Medicineexternal icon provides information resources.

Once the fetal radiation dose is estimated, potential health effects can be assessed.
Potential Health Effects of Prenatal Radiation Exposure (Other Than Cancer)
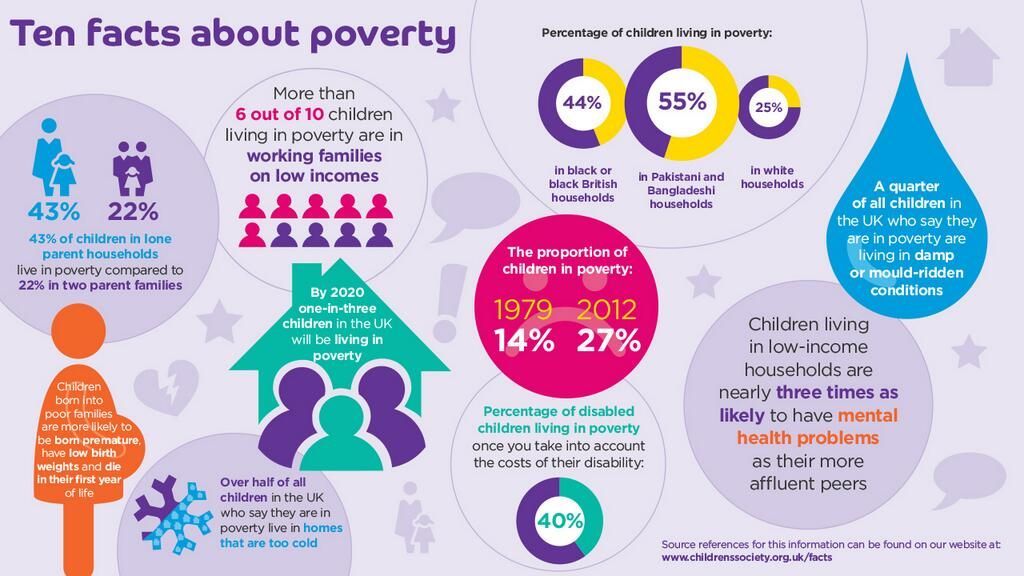
Table 1 summarizes the potential non-cancer health risks of concern. This table is intended to help physicians advise pregnant women who may have been exposed to radiation, not as a definitive recommendation. The indicated doses and times post-conception are approximations.
| Acute Radiation Dose* to the Embryo/Fetus | Time Post Conception (up to 2 weeks) | Time Post Conception (3rd to 5th weeks) | Time Post Conception (6th to 13th weeks) | Time Post Conception (14th to 23rd weeks) | Time Post Conception (24th week to term) |
|---|---|---|---|---|---|
<0. 10 Gy 10 Gy (10 rads) | Noncancer health effects NOT detectable | ||||
| 0.10–0.50 Gy (10–50 rads) | Failure to implant may increase slightly, but surviving embryos will probably have no significant (non-cancer) health effects. | Growth restriction possible | Growth restriction possible | Noncancer health effects unlikely | |
| > 0.50 Gy (50 rads) The expectant mother may be experiencing acute radiation syndrome in this range, depending on her whole-body dose. | Failure to implant will likely be high, depending on dose, but surviving embryos will probably have no significant (non- cancer) health effects. | Probability of miscarriage may increase, depending on dose. Probability of major malformations, such as neurological and motor deficiencies, increases. Growth restriction is likely | Probability of miscarriage may increase, depending on dose. Growth restriction is likely. | Probability of miscarriage may increase, depending on dose. Growth restriction is possible, depending on dose. (Less likely than during the 6th to 13th weeks post conception) Probability of major malformations may increase | Miscarriage and neonatal death may occur, depending on dose. § |
| 8th to 25th Weeks Post Conception: The most vulnerable period for intellectual disability is 8th to 15th weeks post conception Severe intellectual disability is possible during this period at doses > 0.5 Gy Prevalence of intellectual disability (IQ<70) is 40% after an exposure of 1 Gy from 8th to 15th week Prevalence of intellectual disability (IQ<70) is 15% after an exposure of 1 Gy from 16th to 25th week Table adapted from Table 1.1. of the National Council on Radiation Protection and Measurements’ Report No. | |||||
Gestational age and radiation dose are important determinants of potential non-cancer health effects. The following points are of particular note.
- During the first 2 weeks post-conception, the health effect of concern from an exposure of ≥ 0.1 Gy is the possibility of death of the embryo. Because the embryo is made up of only a few cells, damage to one cell, the progenitor of many other cells, may cause the death of the embryo, and the blastocyst may fail to implant in the uterus. Embryos that survive, however, are unlikely to exhibit congenital abnormalities or other non-cancer health effects, no matter what dose of radiation they received.
- In all stages post-conception, radiation-induced non-cancer health effects are not detectable for fetal doses below about 0.10 Gy.
Carcinogenic Effects of Prenatal Radiation Exposure
Radiation exposure to an embryo/fetus may increase the risk of cancer in the offspring, especially at radiation doses > 0. 1 Gy, which are well above typical doses received in diagnostic radiology. However, attempting to quantify cancer risks from prenatal radiation exposure presents many challenges. These challenges include the following:
1 Gy, which are well above typical doses received in diagnostic radiology. However, attempting to quantify cancer risks from prenatal radiation exposure presents many challenges. These challenges include the following:
- The primary data for the risk of developing cancer from prenatal exposure to radiation come from the lifespan study of the Japanese atomic bomb (A-bomb) survivors. [Preston et al. 2008]. The analysis of that cohort includes cancer incidence data only up to the age of 50 years. This precludes making lifespan risk estimates as a result of prenatal radiation exposure.
- From the Japanese lifespan study [Preston et al. 2008], it can be concluded that for those exposed
in early childhood (birth to age 5 years), the theoretical risk of an adult-onset cancer by age 50 is approximately ten-fold greater than the risk for those who received prenatal exposure. Therefore, the risk following prenatal exposure may be considerably lower than for radiation exposure in early childhood
[NCRP2013].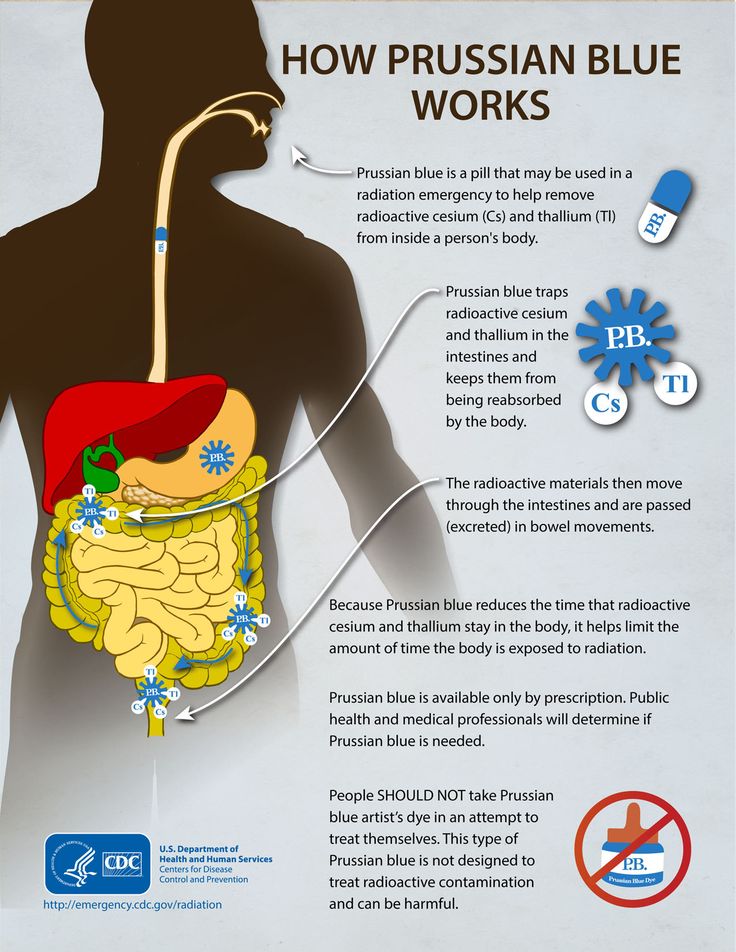
- No reliable epidemiological data are available from studies to determine which stage of pregnancy is the most sensitive for radiation-induced cancer in the offspring [NCRP2013].
The lifespan study of the Japanese A-bomb survivors is continuing as the cohort ages. Future analyses of the accumulating data should provide a better understanding of the lifetime risk of cancer from prenatal and early childhood radiation exposure.
References
ICRP2000] International Commission on Radiological Protection. 2000. Valentin, J. (2000). Pregnancy and medical radiation. Oxford: Published for the International Commission on Radiological Protection.
[NCRP2013] National Council on Radiation Protection and Measurements. 2013. Preconception and Prenatal Radiation Exposure Health Effects and Protective Guidance. (2013). Bethesda: National Council on Radiation Protection & Measurements.
Preston DL, Cullings H, Suyama A, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K, Kasagi F, Shore RE. 2008. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428-436.
2008. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428-436.
[UNSCEAR2013] United Nations Scientific Committee on the Effects of Atomic Radiation. 2013. Sources, effects and risks of ionizing radiation. Vol. II, Scientific Annex B: Effects of radiation exposure of children.
For more information on medical management and other topics on radiation emergencies:
Radiation Emergency Assistance Center/Training Siteexternal icon (REAC/TS) is a program uniquely qualified to teach medical personnel, health physicists, first responders and occupational health professionals about radiation emergency medical response.
Radiation Emergency Medical Management (REMM)external icon provides guidance to health care providers (primarily physicians) about clinical diagnosis and treatment of radiation injury during radiological and nuclear emergencies.
Conference of Radiation Control Program Directorsexternal icon
Health Physics Societyexternal icon
International Commission on Radiological Protectionexternal icon
National Council on Radiation Protection and Measurementsexternal icon
American Association of Physicists in Medicineexternal icon
Radiation Exposure In Pregnancy - StatPearls
Ilsup Yoon; Todd L. Slesinger.
Slesinger.
Author Information
Last Update: May 8, 2022.
Introduction
Choosing the most appropriate imaging modality for pregnancy patients is a common clinical question encountered daily. The general principle for imaging during pregnancy is similar to imaging for the general population, with the goal of radiation exposure being as low as reasonably achievable (ALARA). What is unique during pregnancy is that fetus radiation exposure is an essential factor in deciding optimal imaging studies. Understanding of consequences of radiation exposure on a fetus, degrees of fetal radiation exposure by each imaging modality, and techniques on reducing fetal radiation exposure is vital in choosing the best diagnostic imaging modality. While it is crucial to minimize fetal radiation exposure as much as possible, it is essential to remember that diagnostic studies should not be avoided for fear of radiation exposure, especially when these studies can dramatically change patient management. This activity will discuss the consequences of radiation exposure on a fetus, degrees of radiation exposure by each modality, and techniques of reducing fetal radiation exposure. Solid understanding of how each imaging modality contributes to fetal radiation dose will significantly help in choosing the most appropriate imaging study that provides the best diagnostic information at the lowest level of radiation exposure.
This activity will discuss the consequences of radiation exposure on a fetus, degrees of radiation exposure by each modality, and techniques of reducing fetal radiation exposure. Solid understanding of how each imaging modality contributes to fetal radiation dose will significantly help in choosing the most appropriate imaging study that provides the best diagnostic information at the lowest level of radiation exposure.
The consequence of radiation exposure in fetuses is mostly based on observations rather than based on scientific research. Ethical issues prohibit researching on the fetus. Therefore, most of the data on the impact of radiation on the fetus derives from observations of patients who suffered Japan’s Hiroshima bombing and the Chernobyl nuclear power plant disaster.[1][2] Based on the observations made from the victims of the high level of radiation exposure, the consequences of radiation exposure can categorize into four broad groups, including pregnancy loss, malformation, developmental delay or retardation, and carcinogenesis. [1] Pregnancy loss most often happens when radiation exposure happens during early gestation (less than two weeks).[2] Malformations of body parts and developmental delays occur during the organogenesis period (2 weeks to 8 weeks) and are dependent on the radiation dose.[2] Below the threshold level of radiation exposure, there is minimal disruption of organogenesis. Above the threshold, the degree of malformation is related to the dose of the radiation. Lastly, carcinogenesis is considered a stochastic effect. In other words, cancer can develop at any level of radiation exposure. However, the probability of developing cancer increases with the increase in the dose of radiation.
[1] Pregnancy loss most often happens when radiation exposure happens during early gestation (less than two weeks).[2] Malformations of body parts and developmental delays occur during the organogenesis period (2 weeks to 8 weeks) and are dependent on the radiation dose.[2] Below the threshold level of radiation exposure, there is minimal disruption of organogenesis. Above the threshold, the degree of malformation is related to the dose of the radiation. Lastly, carcinogenesis is considered a stochastic effect. In other words, cancer can develop at any level of radiation exposure. However, the probability of developing cancer increases with the increase in the dose of radiation.
In the United States, the background radiation exposure for the whole body per year is estimated to be 3.1 mSv (310 mrem). United States Nuclear Regulation Commission (USNRC) also recommends total fetus exposure during pregnancy to be less than 5.0 mSv (500 mrem). The fetus radiation dose below 50 mGy is considered safe and not cause any harm. According to the Center for Disease Control (CDC), radiation dose between 50 mGy to 100 mGy is regarded inconclusive in terms of impact on the fetus. Doses above 100 mGy, especially doses above 150 mGy, are viewed as the minimum amount of dosage at which negative fetal consequences will occur, based on observation. The majority of the diagnostic studies performed during the pregnancy are below the threshold level.
According to the Center for Disease Control (CDC), radiation dose between 50 mGy to 100 mGy is regarded inconclusive in terms of impact on the fetus. Doses above 100 mGy, especially doses above 150 mGy, are viewed as the minimum amount of dosage at which negative fetal consequences will occur, based on observation. The majority of the diagnostic studies performed during the pregnancy are below the threshold level.
The effect of radiation exposure during pregnancy also depends on the gestational age of the fetus. The embryo/fetus is most susceptible to radiation during organogenesis (2 to 7 weeks gestational age) and in the first trimester. The fetus is more resistant to the radiation during the second and third trimester. Dose between 0.05 to 0.5 Gy is generally considered safe for the fetus during the second and third trimester while it is considered potentially harmful during the 1st-trimester fetus. Even though the fetus is more resistant to the radiation during the second and third trimester, a high dose of radiation (greater than 0. 5 Gy or 50 rad) may result in adverse effects including miscarriage, growth reduction, IQ reduction, and severe mental retardation. Therefore, clinicians and radiologists should counsel the pregnant patient regardless of the gestational age.[3]
5 Gy or 50 rad) may result in adverse effects including miscarriage, growth reduction, IQ reduction, and severe mental retardation. Therefore, clinicians and radiologists should counsel the pregnant patient regardless of the gestational age.[3]
Occupational radiation exposure for a pregnant employee should be monitored to make sure the total amount of radiation exposure is under the regulatory limit. According to the National Council of Radiation Protection and Measurement (NCRP), the total dose equivalent to the embryo/fetus should not exceed 500 mRem during the length of the pregnancy. It should not exceed 50mRem in any month during pregnancy.[4]
The practice decision on selecting the most appropriate imaging modality for pregnancy should have their basis in the expert opinions of the treating clinician. Nonetheless, the American College of Radiology does provide recommendations on the appropriateness of imaging modalities in accessing common clinical conditions. Each imaging modality is categories into usually appropriate, may be appropriate, and usually not appropriate. For instance, for a pregnant patient presenting with right lower abdominal pain concerning for appendicitis, ultrasound and MRI are usually appropriate imaging modality. CT abdomen and pelvis with or without contrast is categorized as may be appropriate. Abdominal radiograph, Tc-99m WBC scan, and fluoroscopy contrast enema are considered usually not appropriate. The American College of Radiology appropriateness criteria provides the current practice policies and guidelines in the US regarding imaging in pregnant patients.
For instance, for a pregnant patient presenting with right lower abdominal pain concerning for appendicitis, ultrasound and MRI are usually appropriate imaging modality. CT abdomen and pelvis with or without contrast is categorized as may be appropriate. Abdominal radiograph, Tc-99m WBC scan, and fluoroscopy contrast enema are considered usually not appropriate. The American College of Radiology appropriateness criteria provides the current practice policies and guidelines in the US regarding imaging in pregnant patients.
Anatomy
Understanding the anatomic location of the uterus is essential in understanding why a particular type of study contributes to a higher radiation dose. The uterus is located within the female pelvis. Therefore, studies that are further away from the pelvis contribute to less radiation dose than the studies that aim at the pelvis. Additionally, the uterus is located superior and anterior aspect of the pelvis during the pregnancy. X-ray beams that project in a posterior to anterior (PA) direction contribute to less radiation than the beam projected in anterior to posterior (AP) direction because, in PA projection, the X-ray gets attenuated before reaching anteriorly located uterus.
Plain Films
A single plain radiograph does not contribute to a significant radiation dose to the fetus. The estimated radiation dose to the fetus varies and ranges from 0.001 mGy to 10 mGy depending on the type of the study.[5] The highest radiation dose is the lumbar spine radiograph, which has a maximal fetal radiation dose of 10 mGy.[5] Nonetheless, even fetus radiation exposure for the lumbar spine radiograph is significantly lower than the threshold limit of the safe radiation exposure dose of 50 mGy, radiation level that is considered safe and without significant harm.
Regardless of the radiation dose, it is vital to reduce radiation exposure to the fetus as much as possible. Plain films are obtained more frequently than computed tomography (CT), and radiation doses from multiple plains films can easily accumulate. Therefore, it is essential to employee dose reducing techniques as often as possible. When performing plain film examination of non-pelvis structure, pelvic lead apron should always be utilized to reduced unnecessary fetus radiation. PA projection of the pelvis also contributes to the lower dose than the AP projection. Technologists should optimally position patients before taking a radiograph to reduce the number of repeat examinations from unsatisfactory views. Lastly, clinicians should obtain radiographs only when it is helping clinical management.
PA projection of the pelvis also contributes to the lower dose than the AP projection. Technologists should optimally position patients before taking a radiograph to reduce the number of repeat examinations from unsatisfactory views. Lastly, clinicians should obtain radiographs only when it is helping clinical management.
Computed Tomography
On the other hand, CT contributes to a significant amount of fetal radiation. The amount of fetus radiation exposure again varies by the type of study with CT pelvis contributing the highest amount of fetal radiation of 50 mGy.[5] This dose is right at the limit above which there is a documented negative impact to the fetus.
Because CT contributes to much higher fetal radiation, it is essential always to be considerate of other options when contemplating utilizing CT on pregnancy patients. Other imaging modalities, including MRI, plain radiograph, ultrasound, and nuclear medicine studies, should be considered first before performing CT. Common clinical presentations like appendicitis first require evaluation with MRI instead of CT.[6] Right upper quadrant ultrasound should be utilized if there is a clinical concern for cholecystitis.[7] Renal ultrasound should merit consideration before CT for nephrolithiasis and collecting system obstruction. If CT is the first indicate study of choice as in traumatic pregnancy patients to evaluate for intra-abdominal trauma, it is crucial to optimize CT setting to minimize the dose. Using wide pitch and narrow collimation can reduce the radiation dose. Besides, CT protocols should be optimized to minimize unnecessary radiation exposure. Clinicians should only perform additional delayed imaging when there is a clinical indication. Unnecessary multiphasic protocols should get simplified into a single-phase protocol.
Common clinical presentations like appendicitis first require evaluation with MRI instead of CT.[6] Right upper quadrant ultrasound should be utilized if there is a clinical concern for cholecystitis.[7] Renal ultrasound should merit consideration before CT for nephrolithiasis and collecting system obstruction. If CT is the first indicate study of choice as in traumatic pregnancy patients to evaluate for intra-abdominal trauma, it is crucial to optimize CT setting to minimize the dose. Using wide pitch and narrow collimation can reduce the radiation dose. Besides, CT protocols should be optimized to minimize unnecessary radiation exposure. Clinicians should only perform additional delayed imaging when there is a clinical indication. Unnecessary multiphasic protocols should get simplified into a single-phase protocol.
When obtaining CT images of body parts outside of the abdomen and pelvis, the scattered radiation exposure to the fetus is minimal. Therefore, a shield does not significantly reduce the radiation exposure on the fetus during the CT scan. A lead shield may be an unnecessary precaution. However, it does minimally reduce the dose from scatter radiation and may provide patients a sense of reassurance and protection. The use of a lead shield is up to the discretion of the institution and provider.[8]
A lead shield may be an unnecessary precaution. However, it does minimally reduce the dose from scatter radiation and may provide patients a sense of reassurance and protection. The use of a lead shield is up to the discretion of the institution and provider.[8]
Magnetic Resonance
MRI uses a magnetic field to generate diagnostic images and does not contribute to ionizing radiation.
Ultrasonography
Ultrasound uses sound waves to generate diagnostic images and does not contribute to ionizing radiation.
Nuclear Medicine
In nuclear medicine, radiopharmaceuticals are injected into patients. These radiopharmaceuticals are distributed throughout the body and emit radiation at the target location. Radiation energies from these radiotracers then convert into diagnostic images. The overall radiation exposure to the fetus depends on how much radiotracer gets delivered to or near the fetus. Fetal radiation exposure in nuclear medicine depends on multiple variables, including maternal excretion and uptake of the radiopharmaceutical, fetal distribution of the radiopharmaceutical, placental permeability of the radiopharmaceutical, tissue affinity of the radiopharmaceutical, the half-life of the radiotracer, the dose of the radiotracer, and type of radiation emitted from the radiotracer. Generally, for nuclear medicine studies utilizing a radiopharmaceutical that gets excreted through the kidneys, patients are encouraged to hydrate and urinate to maximize the urinary excretion of radiopharmaceuticals.
Generally, for nuclear medicine studies utilizing a radiopharmaceutical that gets excreted through the kidneys, patients are encouraged to hydrate and urinate to maximize the urinary excretion of radiopharmaceuticals.
Specific clinical scenarios worth mentioning for nuclear medicine study is pregnancy patient with concern for pulmonary embolism. The first imaging modality should be an ultrasound of lower extremity to look for deep venous thrombosis. If there is still clinical suspicion for pulmonary embolism, CT pulmonary angiogram (CTPA) is preferable to the ventilation-perfusion (VQ) scan. The fetal dose of VQ is much higher than CTPA, even though the maternal dose is much lower. Due to the lower fetal dose, CTPA is the preferred test of choice.[9]
The thyroid iodine scan is not an option during pregnancy. Iodine 121 and 131 are taken up by fetus thyroid and therefore contraindicated.[10]
Angiography
Fetal radiation exposure from angiography and fluoroscopy should only be for emergent clinical settings. A physician performing fluoroscopy should utilize essential dose reducing techniques including pulse fluoroscopy instead of continuous fluoroscopy, last image hold rather than full exposure, and colimitation to appropriate field of view. Magnification increases the radiation dose and should be used only if necessary.
A physician performing fluoroscopy should utilize essential dose reducing techniques including pulse fluoroscopy instead of continuous fluoroscopy, last image hold rather than full exposure, and colimitation to appropriate field of view. Magnification increases the radiation dose and should be used only if necessary.
Patient Positioning
Appropriate patient positioning is vital in producing a diagnostic quality of images and prevent repeat examination that increases fetal radiation. Technologists should optimally position patients before imaging to obtain appropriate views for the exam. Obtaining diagnostic imaging at the first attempt eliminates the need for a repeat examination and significantly reduces unnecessary radiation exposure to the fetus.
Clinical Significance
The plain film, CT, nuclear medicine studies, and fluoroscopy uses ionizing radiation to obtain diagnostic images. A high level of radiation has adverse effects on the fetus; therefore, referring clinicians should consider alternative imaging modalities for pregnancy patients. If diagnostic studies that expose radiation to the fetus are clinically required, it should be performed without delay but must take place in a way that minimizes radiation exposure to the fetus. Solid understanding of how each imaging modality contributes to fetal radiation exposure, techniques to reducing radiation exposure in the fetus, and adverse consequences of high radiation exposure is critical in providing the most appropriate imaging studies for pregnant patients.
If diagnostic studies that expose radiation to the fetus are clinically required, it should be performed without delay but must take place in a way that minimizes radiation exposure to the fetus. Solid understanding of how each imaging modality contributes to fetal radiation exposure, techniques to reducing radiation exposure in the fetus, and adverse consequences of high radiation exposure is critical in providing the most appropriate imaging studies for pregnant patients.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009 Jan;200(1):4-24. [PubMed: 19121655]
- 2.
De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A.
 Radiation effects on development. Birth Defects Res C Embryo Today. 2007 Sep;81(3):177-82. [PubMed: 17963274]
Radiation effects on development. Birth Defects Res C Embryo Today. 2007 Sep;81(3):177-82. [PubMed: 17963274]- 3.
Williams PM, Fletcher S. Health effects of prenatal radiation exposure. Am Fam Physician. 2010 Sep 01;82(5):488-93. [PubMed: 20822083]
- 4.
McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, LeRoy AJ. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007 Jul-Aug;27(4):909-17; discussion 917-8. [PubMed: 17620458]
- 5.
Tremblay E, Thérasse E, Thomassin-Naggara I, Trop I. Quality initiatives: guidelines for use of medical imaging during pregnancy and lactation. Radiographics. 2012 May-Jun;32(3):897-911. [PubMed: 22403117]
- 6.
Vu L, Ambrose D, Vos P, Tiwari P, Rosengarten M, Wiseman S. Evaluation of MRI for the diagnosis of appendicitis during pregnancy when ultrasound is inconclusive. J Surg Res. 2009 Sep;156(1):145-9. [PubMed: 19560166]
- 7.

Wallace GW, Davis MA, Semelka RC, Fielding JR. Imaging the pregnant patient with abdominal pain. Abdom Imaging. 2012 Oct;37(5):849-60. [PubMed: 22160283]
- 8.
Uzoigwe CE, Middleton RG. Occupational radiation exposure and pregnancy in orthopaedics. J Bone Joint Surg Br. 2012 Jan;94(1):23-7. [PubMed: 22219242]
- 9.
Pahade JK, Litmanovich D, Pedrosa I, Romero J, Bankier AA, Boiselle PM. Quality initiatives: imaging pregnant patients with suspected pulmonary embolism: what the radiologist needs to know. Radiographics. 2009 May-Jun;29(3):639-54. [PubMed: 19270072]
- 10.
Jain C. ACOG Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstet Gynecol. 2019 Jan;133(1):186. [PubMed: 30575654]
Is X-ray examination dangerous during pregnancy - MEDSI
01/15/2018
Is X-ray examination dangerous during pregnancy
X-ray examinations are carried out to determine the presence of any pathologies, neoplasms or diseases. For this, a directed beam of electromagnetic waves of a given length and frequency is used. It passes through human organs, the tissues of which reflect and absorb it in different ways.
For this, a directed beam of electromagnetic waves of a given length and frequency is used. It passes through human organs, the tissues of which reflect and absorb it in different ways.
Due to this difference, various anomalies can be seen. The result is sent to the screen or recorded on a special film.
During a preventive examination, this examination is carried out in a special room. In case of injury to the patient, it can be used immediately in the emergency department, operating room or intensive care unit.
Influence of irradiation on the fetus
X-rays in general are not always beneficial for the body, as it destroys those of its cells that are in a state of constant division. This leads to the destruction or mutation of DNA chains.
There are not many such newly formed cells in the body of an adult. But in the fetus in the early stages of development, they are the basis. Therefore, such an examination is quite dangerous for him. The most likely occurrence of complications when using x-rays during pregnancy in its first trimester (initial 12 weeks).
What problems can X-rays cause in early pregnancy?
Due to the gradual development of the fetus, in each week of its existence, the formation of future systems of the child's body takes place. Therefore, the mother's body receiving a large amount of X-rays at these stages can have various serious consequences:
- The first two weeks. Possible death of the embryo, miscarriage, ectopic pregnancy.
- Weeks three and four. Pathologies at an early stage of fetal development, miscarriage.
- Fifth-sixth weeks. Disturbances in the development of a number of organs and systems: thyroid, thymus and gonads; immune, nervous, circulatory, endocrine systems.
- Seventh week. Damage to the liver, intestines. Metabolic disease.
- Eighth. Pathologies of the development of joints and limbs, the oral cavity.
- Ninth week. Damage to the respiratory and reproductive systems.
- Tenth and eleventh weeks.
 Problems associated with the development of teeth. Heart disease.
Problems associated with the development of teeth. Heart disease. - Twelfth week. Pathology of the thyroid gland, disorders of the immune system.
After this period, the effect of radiation on the fetus decreases, but it is still not recommended to do such a study until the end of pregnancy, except in cases of emergency.
X-rays in early pregnancy
Doctors try not to prescribe X-rays to pregnant women, because even a minimal risk of harm from radiation always remains. It is especially great in the first twelve weeks.
The most dangerous tests for the fetus are:
- Abdominal X-ray
- X-ray of the pelvis and spine
- Mammography
- Fluorography
- Computed tomography
- Isotope scanning
Less dangerous X-rays are:
- Chest (lungs, heart)
- Brain
- Limbs
Are there any non-hazardous examinations?
The safest types of X-ray examination are:
- X-ray of teeth
- X-ray of the nose
In these cases, the exposure occurs locally, so the radiation dose is minimal.
The amount of radiation that a fetus can receive in two months is regulated by the Sanitary Rules and Regulations and should not exceed 1 millisievert (mSv).
There are other types of examinations that can be used instead of X-ray during pregnancy:
- MRI
- Visiography
- Ultrasound
Nevertheless, doctors try not to prescribe MRI in the first trimester of pregnancy, since statistical studies are not enough to clarify its safety during this period.
What if X-rays are indispensable?
X-rays for pregnant women may be necessary in a situation where the disease or injury threatens the life and health of the mother and child, and it is impossible to use other diagnostic methods. And the harm from not using x-rays outweighs the potential harm from its use.
- If it is necessary to examine an area that does not touch the pelvis, abdomen or spine, they must be shielded with lead aprons and pads.
- If an X-ray is to be taken directly through the fetus in early pregnancy, the doctor may suggest that it be interrupted to avoid mutations and miscarriage.

- A woman may refuse to have an abortion, but in this case she must understand the risks she is taking and the pathologies that may appear in the fetus.
In all these cases, after passing the examination, it is recommended to go for an ultrasound scan to monitor the condition of the fetus and the appearance of certain pathologies.
If it is possible to postpone the use of x-rays until the last trimester or postpartum, then this should be done.
At the earliest possible time, a woman may not be aware of the pregnancy. Therefore, before x-rays, it is recommended to undergo an additional examination.
Benefits of X-ray analysis at MEDSI:
- 30 x-ray examinations
- The latest equipment with the ability to control the intensity of radiation
- Urgent examination in case of injury or other medical indications
- Technologies suitable for both adults and children
- Radiologists of high qualification categories, candidates of medical sciences
- Appointment for research and consultation by phone 8 (495) 7-800-500
- More than 20 diagnostic centers
Do not delay treatment, see a doctor right now:
- Pregnancy tests
- Planning and management of pregnancy
- Obstetrician-gynecologist appointment
Is it possible for pregnant women to undergo fluorographic and X-ray examinations?
Decree of the Chief State Sanitary Doctor of the Russian Federation of February 18, 2003 N 8 "On the Enactment of SanPiN 2.
 6.1.1192-03"
6.1.1192-03" VII. Requirements for ensuring radiation safety of patients and the public
7.1. The referral of the patient for medical radiological procedures is carried out by the attending physician according to justified clinical indications. Physicians performing medical x-ray examinations need to be aware of expected patient dose levels, possible body reactions, and risks of long-term effects.
7.2. At the request of the patient, he is provided with full information about the expected or received radiation dose and about the possible consequences. The right to decide on the use of radiological procedures for diagnostic purposes is granted to the patient or his legal representative.
7.3. The patient has the right to refuse medical radiological procedures, with the exception of preventive studies (FLG) conducted in order to identify diseases that are epidemiologically dangerous.
7.4. The final decision on the feasibility, scope and type of examination is made by the radiologist, in the absence of a radiologist, the decision is made by the doctor who sent for the X-ray examination, who was trained in radiation safety in an institution licensed for educational activities in this field.
7.5. In case of unreasonable referrals for x-ray examination (lack of diagnosis, etc.), the radiologist may refuse to conduct an x-ray examination for the patient, having previously informed the attending physician about this and recorded the refusal in the medical history (outpatient card).
7.6. The radiologist (or radiologist) registers the value of the individual effective dose of the patient in the sheet for recording dose loads during x-ray examinations (the sheet is pasted into the medical record of the outpatient or the history of the development of the child) and in the register of daily radiological examinations. When a patient is discharged from a hospital or after an x-ray examination in specialized medical institutions, the value of the dose load is entered into the extract. Subsequently, the dose is transferred to the sheet for recording dose loads of the outpatient medical record (history of the development of the child). Determination and accounting of dose loads is carried out using approved methods, methods for performing measurements and types of measuring instruments.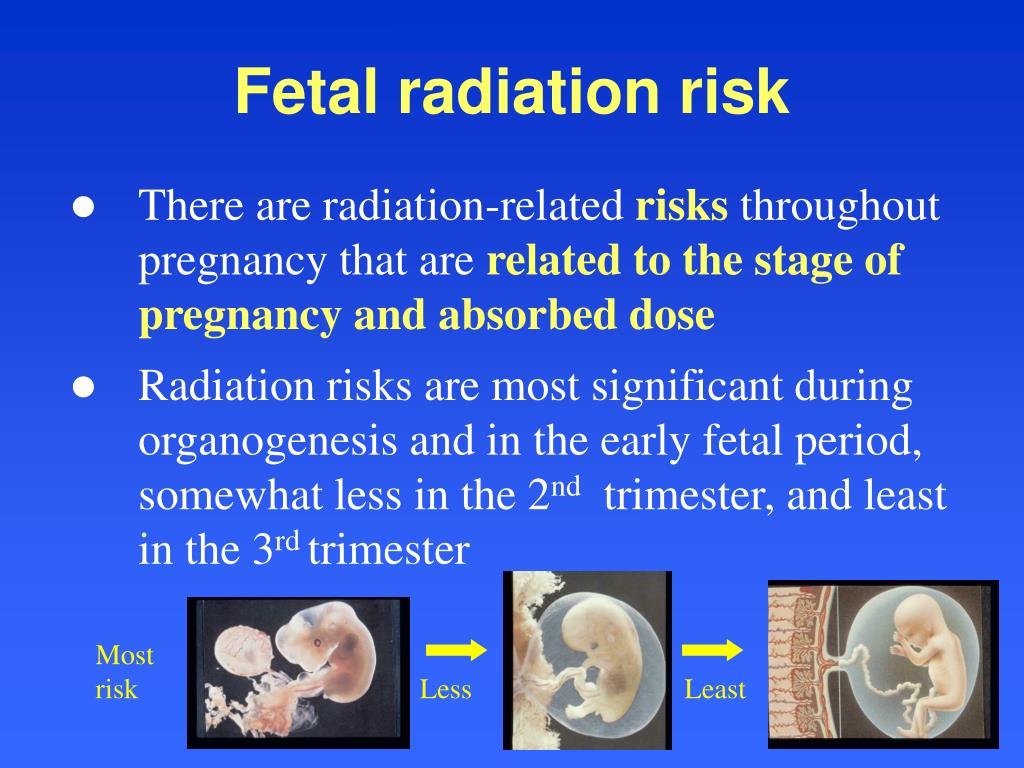
7.7. In order to prevent unreasonable re-exposure of patients at all stages of medical care, the results of previously conducted X-ray studies and the doses received during the year are taken into account. When a patient is referred for an x-ray examination, consultation or inpatient treatment, when a patient is transferred from one hospital to another, the results of x-ray studies (description, images) are transmitted along with an individual card.
7.8. X-ray examinations performed on an outpatient basis should not be duplicated in a hospital setting. Repeated studies are carried out only when the course of the disease changes or a new disease appears, as well as when it is necessary to obtain extended information about the patient's health status.
7.9. The established standard for annual preventive exposure during preventive medical X-ray examinations and scientific studies of practically healthy persons is 1 mSv.
Preventive examinations by fluoroscopy are not allowed.
Conducting scientific research with radiation sources on humans is carried out by decision of the federal health authority. This requires the mandatory written consent of the subject and the provision of information about the possible consequences of exposure.
7.10. Limits of radiation doses for patients with diagnostic purposes are not established. To optimize patient protection measures, it is necessary to comply with the requirements of clause 2.2 of these Rules.
When the accumulated dose of medical diagnostic exposure of a patient reaches 500 mSv, measures should be taken to further limit his exposure, if radiation procedures are not dictated by vital indications.
When members of the public receive an annual effective dose of more than 200 mSv or a cumulative dose of more than 500 mSv from one of the main sources of exposure or 1000 mSv from all sources of exposure, a special medical examination is required, organized by the health authorities.
7. 11. In order to protect the skin during X-ray procedures, the following minimum allowable distances from the focus of the X-ray tube to the surface of the patient's body are established.
11. In order to protect the skin during X-ray procedures, the following minimum allowable distances from the focus of the X-ray tube to the surface of the patient's body are established.
7.12. During x-ray examination, screening of the pelvic area,
thyroid gland, eyes and other parts of the body is mandatory, especially in persons of reproductive age. In young children, full-body shielding should be provided outside of the area being examined.
7.13. If it is necessary to provide the patient with emergency or emergency care, X-ray examinations are performed in accordance with the instructions of the doctor providing assistance.
7.14. When referring to sanatorium-and-spa treatment, the results of X-ray examinations and radiation doses obtained during the observation of the patient in the previous year are entered into the sanatorium-and-spa cards. When referring to the medical and labor expert commission (VTEC), the data of X-ray studies carried out in the process of monitoring the patient are attached.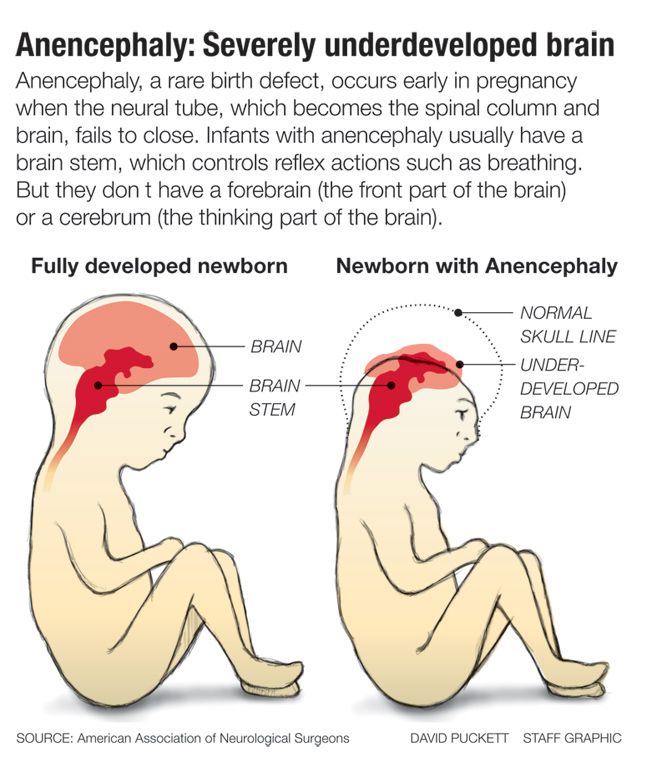
7.15. When referring women of childbearing age for an x-ray examination, the attending physician and radiologist specify the time of the last menstruation in order to choose the time of the x-ray procedure. X-ray studies of the gastrointestinal tract, urography, radiography of the hip joint and other studies related to radiation exposure to the gonads are recommended during the first decade of the menstrual cycle.
7.16. The appointment of pregnant women for X-ray examination is carried out only according to clinical indications. Studies should, if possible, be carried out in the second half of pregnancy, except in cases where the issue of termination of pregnancy or the need for emergency or emergency care must be decided. If pregnancy is suspected, the question of the admissibility and necessity of an x-ray examination is decided on the assumption that there is a pregnancy.
7.17. Pregnant women are not allowed to participate in x-ray studies (support for a child or a seriously ill relative).
7.18. X-ray examinations of pregnant women are carried out using all possible means and methods of protection so that the dose received by the fetus does not exceed 1 mSv in two months of undiagnosed pregnancy. If the fetus receives a dose exceeding 100 mSv, the doctor must warn the patient about the possible consequences and recommend terminating the pregnancy.
7.19. X-ray examinations of children under 12 years of age are performed in the presence of a nurse, nurse or relatives, whose duties are to accompany the patient to the place of examination and monitor him during their conduct.
7.20. In X-ray examinations of young children, special immobilizing devices are used, eliminating the need for the assistance of personnel. In the absence of a special device, the support of children during the study may be entrusted to relatives not younger than 18 years of age. All persons assisting in such studies must be instructed in advance and equipped with personal radiation protection equipment.

 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013].
174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013].