Weak pelvic floor after birth
Female Pelvic Medicine and Reconstructive Surgery
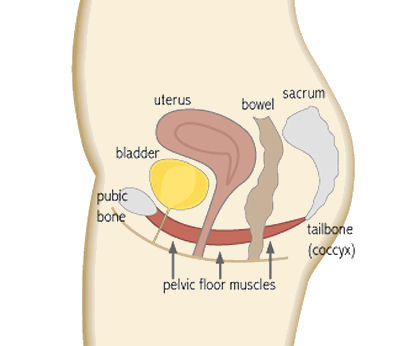
What Happens to Your Pelvic Floor After Childbirth: The Woman’s Center : Female Pelvic Medicine and Reconstructive SurgeryThe female pelvic system is a complex network of muscles and nerves, so it’s hardly surprising that giving birth can have lasting effects on the body. Luckily, as the field of urogynecology grows, doctors are better able to understand just how the pelvic system is impacted by pregnancy and childbirth, and how to help women who have sustained injuries as a result.
Here are several important things to know about childbirth injury, their causes, their symptoms, and how they can be treated.
Vaginal deliveries can result in damage to key muscles.
The levator ani muscle serves two major functions in the female body: supporting the vagina and pelvic organs and maintaining urinary and bowel continence. As a woman enters her third trimester and prepares for birth, these muscles become strained to support the baby’s growth and delivery. More than 30% of women who give birth vaginally will experience pelvic trauma that causes damage to this muscle group.
Vaginal delivery can also increase the risk of pelvic organ prolapse.
The levator ani is also responsible for supporting pelvic organs, so if those muscles and nerves are damaged, the uterus and vaginal walls may begin to collapse into the vaginal canal. According to the Women’s Health Foundation, there are quite a few risk factors that can also increase the likelihood of levator ani damage, such as:
- Delivery time (pushing more than 90 minutes can increase risk of damage)
- Large birth weight
- Forcep and vacuum deliveries
- Age of the mother
- Previous pelvic surgery
- Poor diet
- Smoking
Emptying disorders are also a common result of childbirth and pelvic injury.
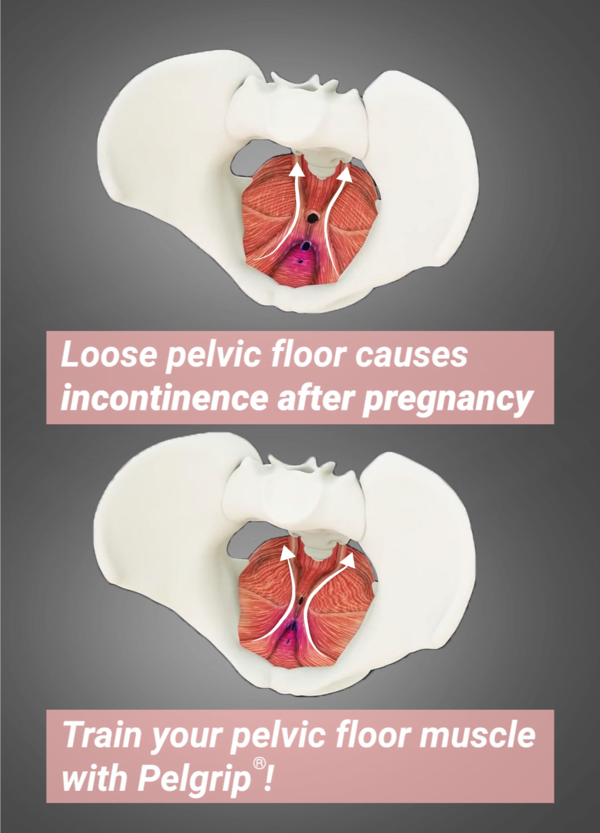
Since the muscles that are responsible for controlling bladder and bowel urges can be damaged by pregnancy, women are likely to experience incontinence after giving birth. One study in Oregon found that 1 in 4 women experience involuntary passage of gas and bowel leakage within six months of childbirth. In addition, urinary incontinence can start during the third trimester and persist for months. If you or a loved one has experienced involuntary bowel leakage or urinary incontinence for more than three to six months after giving birth, it might be time to see a doctor and evaluate treatments, such as physical therapy or surgery.
One study in Oregon found that 1 in 4 women experience involuntary passage of gas and bowel leakage within six months of childbirth. In addition, urinary incontinence can start during the third trimester and persist for months. If you or a loved one has experienced involuntary bowel leakage or urinary incontinence for more than three to six months after giving birth, it might be time to see a doctor and evaluate treatments, such as physical therapy or surgery.
Most postpartum symptoms resolve themselves.
According to the Women’s Health Foundation, 70% of U.S. women who’ve just given birth find that certain symptoms of childbirth (like urinary incontinence and accidental bowel leakage) go away after a few months.
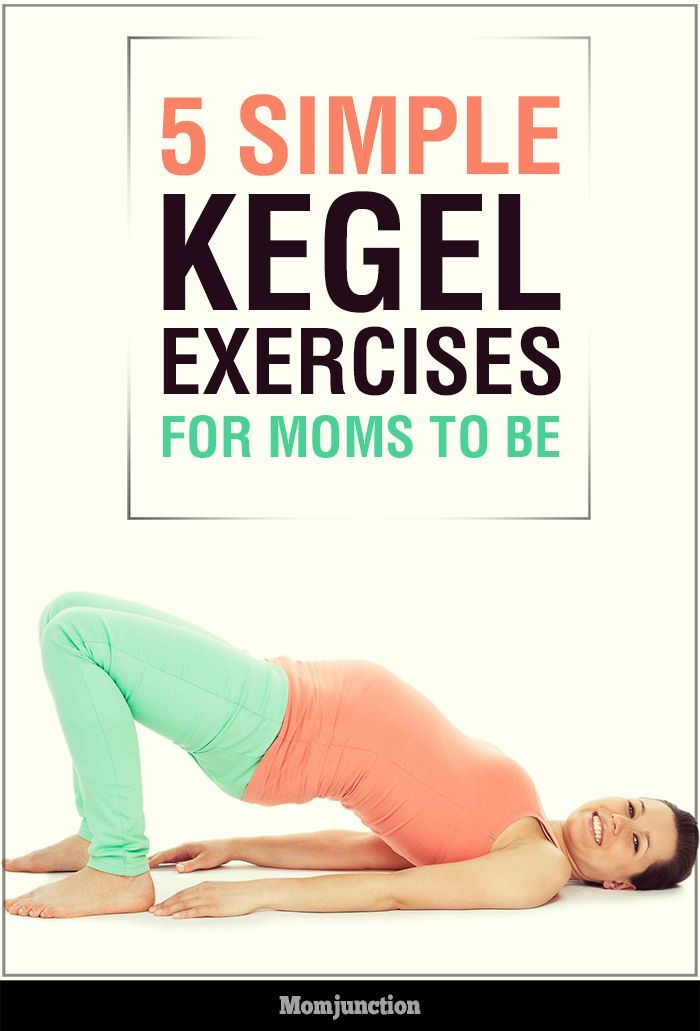
Physical therapy and pelvic floor exercise are crucial to preventing — and healing from — injury.
Pelvic floor exercises during and after pregnancy and physical therapy can help mitigate the stress that pregnancy and delivery places on the body. In one study, women who received pelvic floor therapy during their third trimester and after giving birth were less likely to report urinary incontinence. Doctors universally agree that Kegel exercises are vital to keep the pelvic floor muscles strong during and after pregnancy, and more comprehensive treatment can be given by a physical therapist.
In one study, women who received pelvic floor therapy during their third trimester and after giving birth were less likely to report urinary incontinence. Doctors universally agree that Kegel exercises are vital to keep the pelvic floor muscles strong during and after pregnancy, and more comprehensive treatment can be given by a physical therapist.
Surgery is often necessary to correct pelvic floor damage.
Every year, nearly 400,000 women in the U.S. undergo surgery for urinary incontinence or pelvic organ prolapse. It’s important to follow up with your doctors after the birth to assess any damages done to the pelvic floor and surrounding muscles. It might be necessary to seek corrective surgery to ensure that your body recovers from the strain of pregnancy and birth.
Dr. Ryan Stratford is board-certified in Female Pelvic Medicine and Reconstructive Surgery (FPMRS) as well as Obstetrics and Gynecology (Ob/Gyn) with a wealth of clinical and research experience.
Kegel Exercises: Benefits, Instructions, and Helpful Tips
Pelvic floor exercises, also called Kegel (kay-gull) exercises after Dr. Arnold Kegel who developed them, strengthen the pelvic floor muscles. These muscles play a role in supporting the bladder ad urethra.
Treatment Options For Overactive Bladder (OAB)
Is your daily schedule controlled by your bladder? Do you know where every single bathroom is within a 20-mile radius of your home? If you answered yes to either of these questions, you may have symptoms of overactive bladder (OAB).
How To Heal Your Pelvic Floor After Birth
By Anna Scammell
Masters-trained Women’s Health & Pelvic Floor Physiotherapist
Since pregnancy and childbirth is such a transformative time physically, it’s critical that every woman knows how to look after her pelvic floor after birth. This is especially pertinent in the event of a perineal tear, episiotomy or instrumental vaginal delivery (forceps or suction).
This is especially pertinent in the event of a perineal tear, episiotomy or instrumental vaginal delivery (forceps or suction).
Optimising the recovery of your pelvic floor will help to prevent unwanted issues, such as prolapse https://www.thewholemother.com/prolapse-all-your-questions-answered/, incontinence or pain with intercourse.
1. Know the Details of Your Labour.Often there is so much going on during the birth of your babythat women don’t know to ask the details of their birth. So make sure you find out:
- If you had a tear and if so, where is it and what grade is it.
- If you had an episiotomy.
- If forceps or suction were used.
This information is important to give to your Women’s Health Physiotherapist down the track.
2. Personal Hygiene.- Make sure you keep the area clean and dry.
- Wash your perineal area with water (no soap) and gently pat yourself dry after a shower.

- After urinating pat the area from front to back with toilet paper.
- Avoid rubbing the area.
- Wash the area with water after you use your bowels.
- Change your sanitary pad every 4-6 hours.
The vaginal area is likely to be inflamed and swollen after childbirth so ice and compression will help to reduce this and provide pain relief. A good idea is to ask the nursing staff to put some of your maternity pads in the freezer. Put the cold pad inside a supportive pair of underpants to provide some comfortable compression.Ice is in particularly important intermittently in the first 48 hours after birth, but if it is soothing for you then continue to use it when you go home.
Once you are able, I also recommend wearing a compression garment (SRC recovery shorts) to provide your pelvic floor and abdominal muscles with support.
4. Pain ReliefYour doctor will prescribe you with pain relief when you leave hospital. Make sure you take it if the area is painful.
Make sure you take it if the area is painful.
A key strategy to maximizing pelvic floor recovery is starting gentle pelvic floor contractions the day after giving birth (even if you have had stitches). This helps to increase circulation to the area and reduce swelling. Gentle pelvic floor exercises also help to re-activate neural pathways to these muscles to regain strength and motor control over time. I recommend doing little bits often, so 4-5 gentle pelvic floor contractions each time you feed your baby. Focus on gently lifting the pelvic floor and then releasing the muscle completely. Breathing into your belly between each contraction can help to achieve complete relaxation.
The key to pelvic floor exercises is doing them correctly. Hopefully you saw a Women’s Health Physiotherapist during your pregnancy to teach you this, but if not, you can download my FREE Pelvic Floor Guide here: https://www.thewholemother. com/freebies/. As the days and weeks progress work back up to your normal pelvic floor regime pre-birth.
com/freebies/. As the days and weeks progress work back up to your normal pelvic floor regime pre-birth.
It is a common misconception that women who have a caesarian section will be free from pelvic floor issues. The weight of the baby in utero on the pelvic floor can be enough to create pelvic floor weakness postpartum. As a result, pelvic floor exercises after birth are essential for all women.
6. RestPrioritise rest in the first 1-2 weeks after birth to eliminate gravity from adding extra downward pressure on your pelvic floor. It’s important for you to both move about as you feel comfortable and spend some time lying down/sleeping to encourage healing of your pelvic floor or c-section. If you experience any vaginal heaviness or dragging sensation, make sure you spendtime off your feet, especially at the end of the day. If you are able to breastfeed your baby lying down, then this is another good chance to maximize rest.
7. PostureOptimal posture and body awareness in these early days will also set you up for a better pelvic floor and core recovery. Make sure you sit & stand upright, lengthening your spine and gently drawing your shoulder blades back. It is important to get into good postural habits as soon as possible after you have your baby. This is because an upright position (rather than slumped) isthe optimalposition to start exercising your pelvic floor & deep abdominal muscles.
Make sure you sit & stand upright, lengthening your spine and gently drawing your shoulder blades back. It is important to get into good postural habits as soon as possible after you have your baby. This is because an upright position (rather than slumped) isthe optimalposition to start exercising your pelvic floor & deep abdominal muscles.
Be mindful of the way you move to avoid putting pressure through your stomach and pelvic floor. Examples are:
- Roll to one side to get out bed instead of sitting straight up
- Avoid lifting your suitcase, pram or other children in the first few weeks.
I recommend doing a pelvic floor contractionbefore you lift your baby in and out of their bassinet or car seat.
9. Avoid Constipation/Straining.In order to promote healing of your pelvic floor, it’s important that you do not strain to use your bowels. Ensure you keep your diet high in wholefoods, especially fruit and veggies, and drink 2-3L of fluid (especially water). This may involve organising your partner or family to bring healthy meals into hospital to ensure you are getting adequate nutrients and fibre, as we all know that hospital food can be less than desirable!
This may involve organising your partner or family to bring healthy meals into hospital to ensure you are getting adequate nutrients and fibre, as we all know that hospital food can be less than desirable!
It may be a good idea to use a laxative in these early days after childbirth, to soften your bowel motion and prevent straining. Your nurse should provide you with a laxative, or otherwise ask. If you are prone to constipation, continue using the laxative when you get home.
The way you sit on the loo will also help you to avoid straining. Click here to see how: https://www.thewholemother.com/my-top-tips-for-treating-constipation-improving-gut-health/
10. Support your Perineum.Manually supporting your perineum (vaginal area before anus) when you are using your bowels is a good idea if you have had stitches. To do so, fold over toilet paper and hold it on your perineumapplying some pressure with your fingers. You may also want to support the area with your hand when you sneeze, cough or laugh.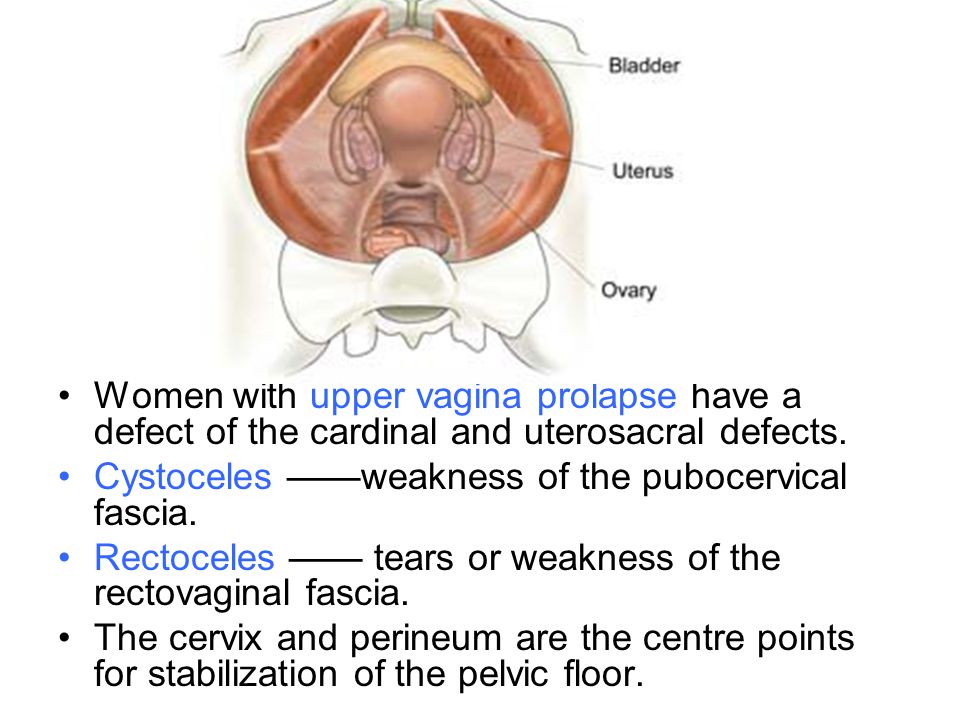
It is common for women to disconnect from their vaginal area after pelvic floor injury or a traumatic birth, as the area feels different/strange/uncomfortable and they don’t feel like themselves. It’s really important to recognise that your body had just achieved an amazing feat of giving birth, and your vagina is not meant to bounce back and feel “normal” straight away. Disassociating or ignoring your downstairs area can contribute to dysfunction down the track. So know that your vagina is likely to feel or look different to before you had your baby for awhile, and this is OKAY! Your pelvic floor is currently healing, just like any other muscle needs to heal after an injury. The ability of your pelvic floor to heal and recover will be heightened by the amount of care & attention you give it.
I recommend eventually getting a small mirror and looking at your vagina. It’s important to accept what you see. This might sound daunting to many, but your vagina is an incredibly primitive part of your body, and should be treated with the same respect as any other area.
Another effective way to reconnect with your vagina is to comfortably lie down on your side in a relaxing environment (ie. when your baby is sleeping), close your eyes and start breathing into your belly (rather than chest). This allows your diaphragm to descend and helps relax your pelvic floor.As you do it, imagine the breath moving down into your pelvis, to your pelvic floor, bringing healing energy to it. This technique is called diaphragmatic breathing.I recommend doing it for 5-10 minutes daily.
Breathing and pelvic floor relaxation is also really important to help prevent the development of pelvic floor tension or overactivity, which can occur as a protective response to birth injury or trauma. Because pelvic floor overactivity can lead to pain with intercourse, I recommend all women prioritise diaphragmatic breathing.
During the day, it is also a good idea to bring your awareness to your pelvic floor. Are you sucking it in without even realising? If so, breathe into your belly and soften through your stomach, letting your pelvic floor muscles relax. Remember the aim of pelvic floor recovery is not to suck it in all day long.
Remember the aim of pelvic floor recovery is not to suck it in all day long.
At 6-weeks postpartum it is essential that every womanhas an assessment with a Women’s Health & Pelvic Floor Physiotherapist. We specialise in pelvic floor recovery and perform thorough internal assessment of your muscles. We will assess for pelvic floor tension or overactivity, pain, prolapse, pelvic floor strength, endurance, motor control, and set you up with an exercise program specific to you. We will also provide manual therapy for the treatment of pelvic floor overactivity or scar tissue, and give you lifestyle advice.
14. Self-massage for scar tissue.After your 6-week check up with your Doctor and your scar has healed, I recommend regularly massaging your scar with your thumb/fingers using a natural lubricant or oil tohelp soften the scar tissue. This is because scar tissue and increased sensitivity in the area can lead to tension and pain in the pelvic floor muscles.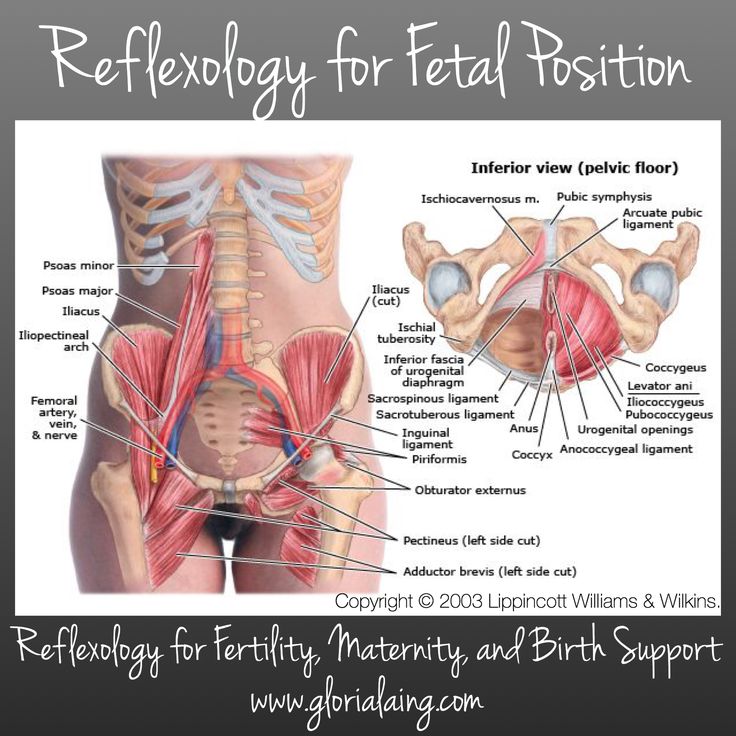 Your Women’s Health Physio can teach you how to do self-massage.
Your Women’s Health Physio can teach you how to do self-massage.
Returning to intercourse following childbirth will be different for every women depending on multiple factors, but is not safe until after your 6-week postpartum check up with your doctor. For some women they may not be ready for several months.
Whilst sex for the first time may feel uncomfortable or different initially, it should not be painful. If it is, make sure you stop and do not push through any pain. Instead speak to your Women’s Health Physio to assess why this might be the case.
16. Return to exercise safely.How and when you return to exercise post-birth is very important for your pelvic floor recovery. Your Women’s Health Physio will guide you on this as every woman’s birth experience and pelvic floor is different.
Some Guidelines are as follows:*
- 0-6 weeks: Focus on pelvic floor and gentle core muscle exercises, postural exercises, gentle walking and stretching.
- 6-12 weeks: Postnatal Pilates or yoga, low-impact cardio exercise like walking, swimming and light strength training.
- 3-6 months: Progress core work and Pilates, gradually increase intensity and duration of low-impact cardio & strength training, introduce light jogging.
- 6+ months: Progress all of above, introduce higher-impact exercise like jumping, running if that is a goal of yours.
*It is imperative that you do not experience any vaginal heaviness (prolapse), bladder leakage, pain or abdominal doming during or after any exercise.
For more information on the safe return to postpartum exercise grab my FREE Guide here: https://www.thewholemother.com/freebies/
Bio:Anna Scammell is a Masters-trained Women’s Health & Pelvic Floor Physiotherapist in Sydney, and Founder of www.thewholemother.com. Anna consults out of Sevenways Health Centre in North Bondi, offers home visits to women around Sydney and online consults.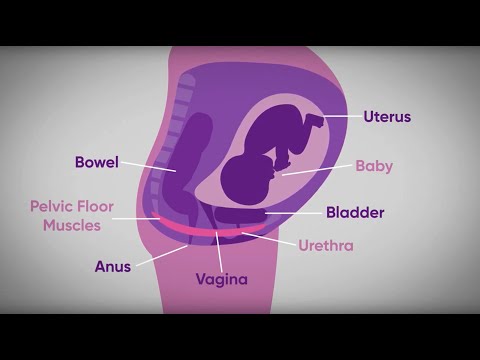 She combines her 10+ years of clinical experience, evidence based knowledge, and passion for health & wellbeing. Anna’s mission is to educate, empower & inspire as many women as possible to be the best version of themself during their childbearing years and beyond.
She combines her 10+ years of clinical experience, evidence based knowledge, and passion for health & wellbeing. Anna’s mission is to educate, empower & inspire as many women as possible to be the best version of themself during their childbearing years and beyond.
As always, this information is intended for general educational purposes only. It is not medical advice. Please discuss any medical issues with your own doctor. Read our full medical disclaimer here.
Sex after childbirth: training intimate muscles
These muscles are often referred to as the intimate muscles. Well-developed pelvic floor muscles are the key to sexual pleasure: their volume and tone affect the degree of closure of the genital gap and, accordingly, the strength of arousal and orgasm. But very often after pregnancy and childbirth, these muscles weaken and lose their tone. Why is this happening?
NO MOTION
“Almost half of women leave the maternity hospital with weakness of the pelvic floor muscles (and even more if it is a repeated birth), says gynecologist Elena Silantyeva. - After all, the muscles of the pelvic floor, like all striated muscles, develop only in work, in active movement. But what kind of life do we lead? Most often - sedentary, which is why the muscles are inactive and atrophy. And during childbirth, when the birth canal is stretched, these flaccid muscles are more quickly stretched and injured. For this reason, a woman may experience a syndrome of "wide vagina" (vaginal relaxation). An infection easily penetrates into a wide open genital slit, thrush, colpitis or vaginitis may develop. And close contact of the vaginal mucosa with linen leads to its drying and partial atrophy. It is not surprising that the sensitivity of the mucosa as an erogenous zone is reduced. Moreover: during the love act, there is no tight fit of the partner's penis to the inner walls of the vagina. And as a result, not only the woman herself ceases to feel any pleasure during contact, but also the man (especially the elderly one): after all, the strength of his erection largely depends on the degree of fit.
- After all, the muscles of the pelvic floor, like all striated muscles, develop only in work, in active movement. But what kind of life do we lead? Most often - sedentary, which is why the muscles are inactive and atrophy. And during childbirth, when the birth canal is stretched, these flaccid muscles are more quickly stretched and injured. For this reason, a woman may experience a syndrome of "wide vagina" (vaginal relaxation). An infection easily penetrates into a wide open genital slit, thrush, colpitis or vaginitis may develop. And close contact of the vaginal mucosa with linen leads to its drying and partial atrophy. It is not surprising that the sensitivity of the mucosa as an erogenous zone is reduced. Moreover: during the love act, there is no tight fit of the partner's penis to the inner walls of the vagina. And as a result, not only the woman herself ceases to feel any pleasure during contact, but also the man (especially the elderly one): after all, the strength of his erection largely depends on the degree of fit.
HEALING ORGASM
Weak sensitivity of erogenous zones leads to another serious problem: a woman may experience a pronounced sexual desire, but cannot get an orgasm. And it's pretty bad for her reproductive system. After all, an orgasm not only gives pleasure and provides emotional release, but also supports women's health. “Orgasm causes an instant spasm of the smallest vessels of the arterial bed, blood renewal, an increase in the tone of the venous system,” explains Elena Silantyeva. - If discharge does not occur, then the outflow of venous blood slows down and congestion develops in the vessels of the small pelvis, which manifest themselves later in various painful sensations. And gynecologists treat these pains with antibiotics, which in turn destroy the microflora of the vagina, and a more serious infection enters the body. Actually, this is another reason to establish a harmonious sex life.
INTIMATE MUSCLES TRAINERS
What should a woman do if her pelvic floor muscles have weakened after childbirth and “wide vagina” syndrome has appeared? Elena Silantieva offers several methods.
- Physiotherapy. First of all, immediately after childbirth, in the first day or two, a woman needs restorative treatment using classical types of physiotherapy - a magnetic field, UHF and others that reduce inflammation and quickly heal damaged, stretched muscle tissue.
- Physical exercise. As soon as the muscles have healed (not earlier than a month after the birth), you can gradually start working with them. But when exactly - only the doctor decides. Any physical activity that has no contraindications is welcome. But Pilates, yoga, and physiotherapy exercises, which were so popular in Soviet times, are especially useful - these complexes usually include exercises that at least indirectly involve the muscles of the pelvic floor.
- biofeedback therapy. This is a hardware-computer complex, with the help of which women learn to do Kegel exercises, specially designed for training intimate muscles.
 Of course, these exercises can be done at home, but it is very important to master the correct technique under the supervision of a specialist, because women often confuse muscles and pump the wrong thing at all. If the muscles have not worked for many years, how can you know how to feel these muscles, put them into work? For this, BOS-therapy is needed. What is its essence? An individual electrode is inserted into the vagina. And when the woman tenses and relaxes the corresponding muscles, the electrode receives an electrical impulse from them, and the data is displayed on the computer screen. If a woman does not relax her muscles well or by mistake uses the muscles of the anterior abdominal wall, the doctor, looking at the screen, coordinates her work, gradually changing and complicating the task. For 15-20 sessions, you can develop a stable skill in order to continue to practice at home on your own. As a result of such exercises, the volume, strength, endurance of intimate muscles, their ability to relax and stretch increases.
Of course, these exercises can be done at home, but it is very important to master the correct technique under the supervision of a specialist, because women often confuse muscles and pump the wrong thing at all. If the muscles have not worked for many years, how can you know how to feel these muscles, put them into work? For this, BOS-therapy is needed. What is its essence? An individual electrode is inserted into the vagina. And when the woman tenses and relaxes the corresponding muscles, the electrode receives an electrical impulse from them, and the data is displayed on the computer screen. If a woman does not relax her muscles well or by mistake uses the muscles of the anterior abdominal wall, the doctor, looking at the screen, coordinates her work, gradually changing and complicating the task. For 15-20 sessions, you can develop a stable skill in order to continue to practice at home on your own. As a result of such exercises, the volume, strength, endurance of intimate muscles, their ability to relax and stretch increases.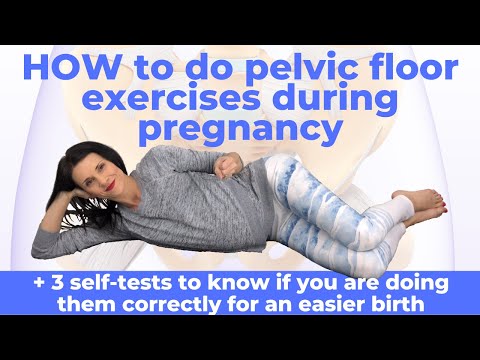 There is nothing surprising and mysterious in this: just as a man in the gym, pumping up his biceps, increases their volume, so a woman can double - and this is easily confirmed by ultrasound diagnostics - the volume of her levators (those muscles that lie around the entrance to the vagina) . The genital gap closes and becomes tight, the sensitivity of the erogenous zones is restored.
There is nothing surprising and mysterious in this: just as a man in the gym, pumping up his biceps, increases their volume, so a woman can double - and this is easily confirmed by ultrasound diagnostics - the volume of her levators (those muscles that lie around the entrance to the vagina) . The genital gap closes and becomes tight, the sensitivity of the erogenous zones is restored. - Laser vulvo-vaginal rejuvenation and intimate cosmetology (plasma therapy and mesotherapy) are modern technologies that involve laser exposure or intradermal injections in the intimate area. They are designed to improve the quality of the mucosa of the external genital organs (and, if desired, change their aesthetic characteristics), improve their flora, and increase the sensitivity of erogenous zones.
Questionnaires conducted by physicians after the completion of these procedures show that women experience more vivid sensations during sex as a result, feel more satisfied at the moment of orgasm, and the orgasmic discharge itself occurs more often than before.
Weak pelvic floor muscles. How dangerous is it? How can you strengthen and restore your muscles on your own?
- Share
- Tweet
Childbirth, genital surgery and the woman's age are the main factors affecting the deterioration of the pelvic floor muscles and the vagina in particular. Up to 40% of women worldwide suffer from this problem. It is the weak tone of the pelvic floor muscles that causes urinary incontinence, prolapse (prolapse) of the uterus and frequent infectious diseases. Uterine prolapse can lead to problems with internal organs, such as adhesions and inflammation of the abdominal cavity. Also, low muscle tone of the vagina leads to problems in intimate life. Sometimes pain even leads to the refusal of sexual intercourse. These problems occur not only in older women, but also in fairly young women.
Causes leading to weakening of the vaginal muscles:
- Childbirth;
- Abortion and other surgical interventions;
- Low levels of the female hormone estrogen;
- Congenital malformations of the pelvic organs or defects of the pelvic floor, and others.

But, unlike visible muscles, it is not easy to understand that you have weakened pelvic floor muscles. In the initial stages, a woman may not be aware that she has weak pelvic floor muscle tone and vaginal prolapse if the symptoms are not noticeable.
Symptoms of weakness of the pelvic floor muscles:
- Urinary incontinence, including when laughing, running, exercising, coughing, sneezing;
- The need to use a sanitary napkin in case of imperceptible leakage of urine;
- Heaviness and pain in the lower abdomen, worse during long standing, not associated with other gynecological diseases;
- Lack of orgasm, decreased sexual pleasure;
- Prolapse of the walls of the vagina and uterus, revealed during a gynecological examination.
If you have any of the above symptoms, you need to strengthen your pelvic floor muscles to prevent prolapse and prolapse of the vagina and uterus. Most women find out about this already when they have problems.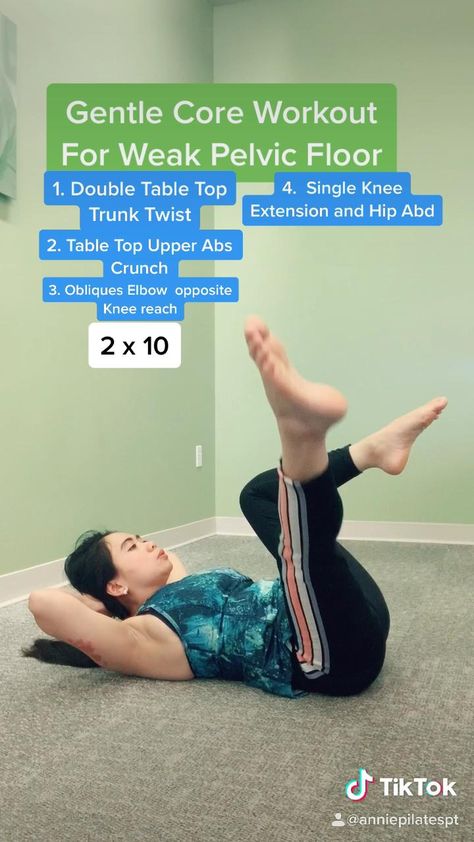 So, in order to prevent the occurrence of diseases associated with a decrease in the tone of the muscles of the vagina, every woman should be able to diagnose their weakening.
So, in order to prevent the occurrence of diseases associated with a decrease in the tone of the muscles of the vagina, every woman should be able to diagnose their weakening.
Vaginal Muscle Test
You can test your muscle tone with your fingers. Just insert a clean moistened finger into the vagina and try to squeeze it with the internal muscles. You will feel which wall of the vagina compresses more and which is weaker. Also, the ribbed surface of the wall will indicate normal muscle tone, and smooth and soft means that the muscles hardly work. But do not despair, all diseases associated with a decrease in the tone of the pelvic floor muscles can be treated. How exactly?
Solving pelvic floor problems
Only in the most difficult cases surgery is required, but in the earlier stages of treatment it is possible on the woman's own! The pelvic floor muscles are trained just like any other muscle. In fact, it is not at all necessary to wait for problems with intimate health.