Vomiting and diarrhea during pregnancy
Vomiting and diarrhea when pregnant: Is it serious?
Vomiting and diarrhea are common during pregnancy. They can vary in duration and severity.
Below, we investigate what leads to both vomiting and diarrhea during pregnancy and which treatments work.
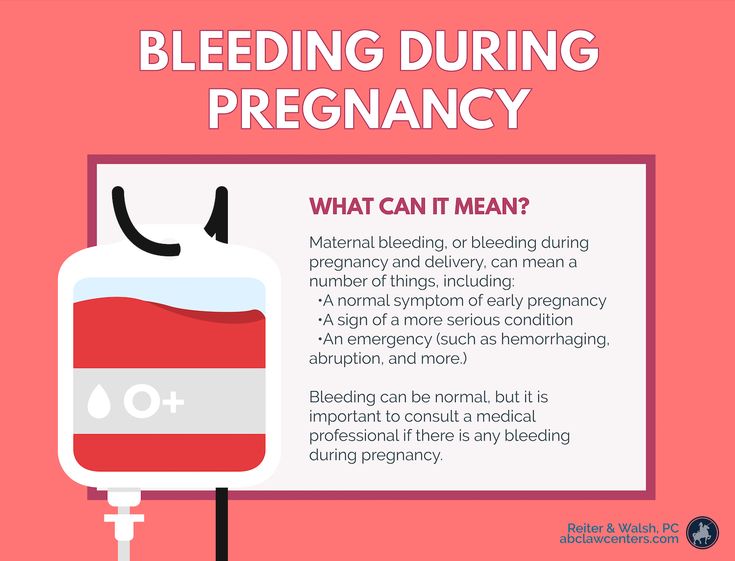
Share on PinterestMany women experience vomiting and diarrhea during pregnancy.Pregnant women frequently experience vomiting and diarrhea, and these issues sometimes overlap. This does not always indicate an underlying health problem.
It is also worth keeping in mind that the two symptoms may have different causes, and one, both, or neither may stem from pregnancy.
So what causes digestive issues such as vomiting and diarrhea during pregnancy? The answers can vary, based on the stage of the pregnancy:
First trimester
During the first trimester, one of the most common symptoms of pregnancy is morning sickness. This involves nausea and vomiting and typically occurs before week 17.
For most women, morning sickness lasts for a few weeks to months, but it can last for the entire pregnancy. Some women vomit once or twice a day, while others feel nauseous all day.
One medical review reports that anxiety, depression, and negative relationships with family can each make nausea and vomiting worse or occur more frequently.
Learn more about morning sickness here.
Meanwhile, stress can also cause gastrointestinal symptoms, including diarrhea.
Other common causes of diarrhea during pregnancy include viral and bacterial infections and certain medications. It is important to note that diarrhea can be dangerous, leading to potentially serious issues such as dehydration.
Learn more about dehydration during pregnancy here.
Second trimester
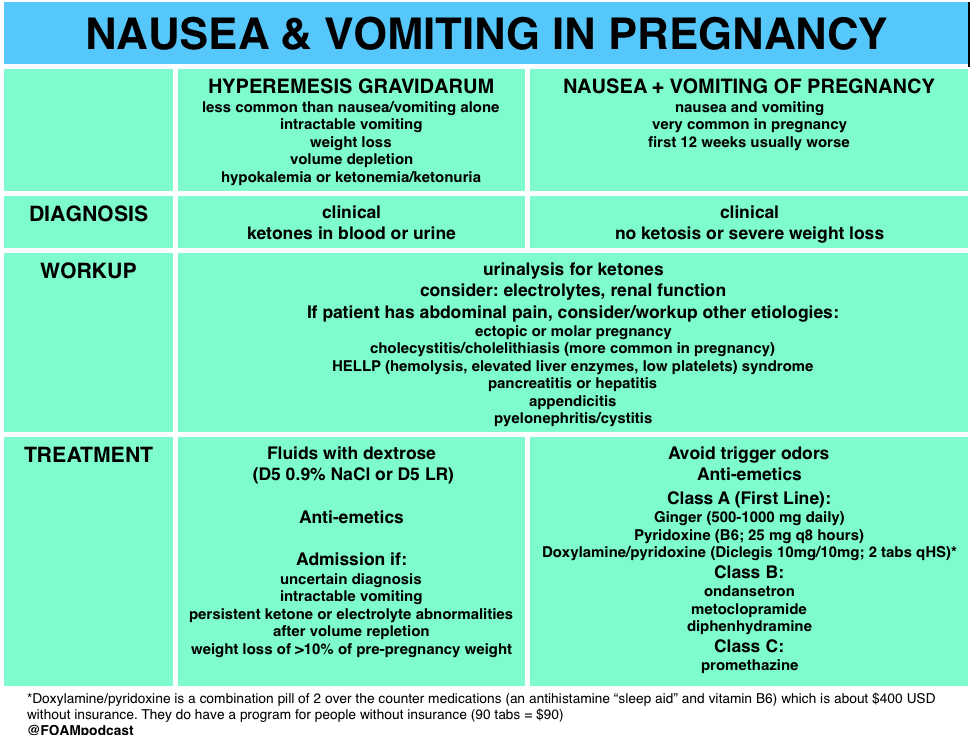
If vomiting starts or continues into the second trimester, it may indicate hyperemesis gravidarum.
This rare disorder causes vomiting and nausea that can be severe enough to require hospitalization. It can also lead to vitamin and mineral deficiencies, dehydration, and a 5% loss in original body weight.
About 22% of women with hyperemesis gravidarum experience the symptoms — nausea and vomiting — throughout their pregnancies.
On the other hand, nausea and vomiting that appear after the end of week 16 may not be related to pregnancy. In this case, the cause can range from a stomach virus to a more serious issue, such as an ulcer or hepatitis.
Third trimester
Heartburn is common during pregnancy, especially later on, as the growing fetus places pressure on the stomach. Also, the sphincter between the stomach and the esophagus relaxes during pregnancy.
As a result of either or both factors, stomach acid can rise up into the esophagus, causing heartburn.
Learn more about heartburn during pregnancy here.
It is important to note that a sudden onset of nausea and vomiting during the second half of pregnancy can stem from preeclampsia, a serious complication that can lead to preterm delivery.
Some other signs and symptoms of preeclampsia include high blood pressure, heartburn, and swelling of the face and hands.
Learn more about preeclampsia here.
Also, diarrhea can be a sign of preterm labor. In some cases, a woman experiences no other signs, or there may be mucus-like vaginal discharge and lower back pain.
Various common health issues can cause both diarrhea and vomiting, including:
- food poisoning
- the stomach flu
- pancreatitis
- a food allergy
However, having diarrhea and vomiting at the same time does not necessarily mean that they are symptoms of one health issue.
Factors such as stress and preexisting conditions can also lead to either or both of these symptoms.
Mild vomiting and diarrhea during pregnancy typically require no specialized treatment. The symptoms may resolve on their own.
Some home care strategies include:
- eating bland foods, such as toast, bananas, crackers, and rice
- taking a prenatal vitamin
- eating more frequently
- eating toast or crackers in bed first thing in the morning, before moving
- taking frequent, single bites of foods such as nuts or crackers
If symptoms are more severe or are otherwise negatively affecting daily life, the following treatment options are safe during pregnancy:
- vitamin B6, which is available over the counter
- doxylamine, an ingredient in sleep aids
- prescription medication that contains both B6 and doxylamine
- prescription antiemetic drugs
It is especially important to consult a doctor about diarrhea and safe treatments, which can include loperamide (Imodium).
Learn how to manage and treat vomiting.
It may not be possible to prevent nausea, vomiting, or diarrhea, but taking the following steps may help:
- eating smaller meals
- eating foods that are easy to digest
- drinking plenty of fluids
- avoiding taste or smell triggers for nausea
A pregnant woman should see a doctor about vomiting or diarrhea that is severe or lasts for more than a few days.
In general, it is a good idea to contact a doctor about any diarrhea, lower back pain, and an increase in vaginal discharge.
Also, see a doctor about any symptoms of dehydration, including:
- dizziness or fainting when standing
- low amounts of urine, which is dark
- an inability to urinate
- a pounding heartbeat
- being unable to keep down liquids
It may be best to contact a doctor about any health concerns or unusual physical changes during pregnancy.
Diarrhea and vomiting are common during pregnancy, especially during the first trimester.
Either issue can lead to complications, and a woman should receive prompt medical care for severe diarrhea or vomiting. A doctor may recommend dietary changes, vitamins, medications, or a combination.
4 common pregnancy-related GI issues, and when to call the doctor | Your Pregnancy Matters
Mild gastrointestinal issues are common during pregnancy, but if you’re concerned, call your doctor.Gastrointestinal (GI) issues are common during pregnancy. As your baby grows, you’ll have less available real estate in your abdomen for your intestines, stomach, and esophagus to function. Additionally, hormonal changes can affect digestion and other GI functions.
Most GI symptoms pass relatively quickly during pregnancy and can be treated with over-the-counter remedies at home. However, to avoid potential complications, women should be aware of what’s normal and when to call the doctor when it comes to GI health during pregnancy.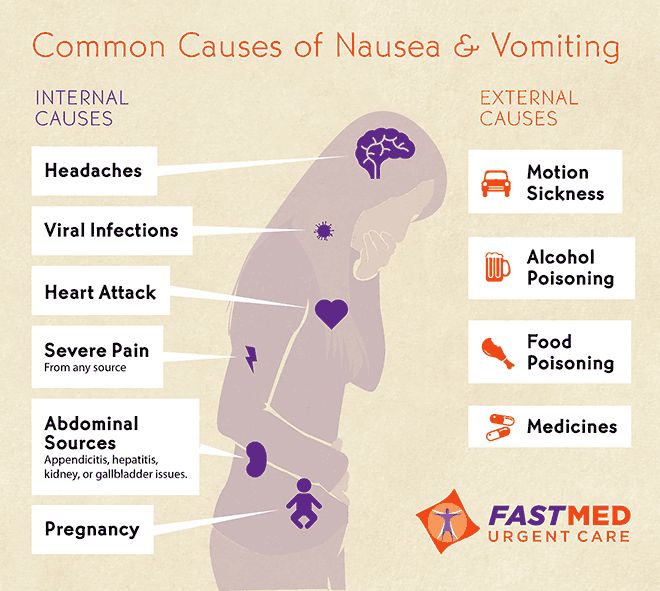
1. Nausea and vomiting
During the first 16 weeks of pregnancy, we expect some mild to moderate nausea and vomiting – the infamous period of morning sickness. In fact, for many women, nausea is one of the earliest symptoms of pregnancy.
If you have severe symptoms, a doctor can recommend medication to reduce dehydration and discomfort. For mild symptoms, or if you prefer not to take medication, you can usually manage symptoms with dietary changes or vitamin therapy under the care of your doctor.
After 16 weeks of pregnancy, vomiting typically is not pregnancy-related and might be due to a bug or infection. In rare cases, vomiting can be caused by more serious medical concerns, such as hepatitis, pancreatitis, or ulcers. If you experience nausea or vomiting past the first trimester of pregnancy, don’t assume it’s pregnancy-related, and don’t let your doctor assume so, either, without checking for underlying causes.
2. Heartburn
Heartburn, or gastroesophageal reflux, affects three of five people in the general population. By the time women reach the third trimester, as many as half will experience heartburn at one point or another. During pregnancy, the muscle between the esophagus and stomach relaxes due to hormonal changes related to pregnancy. At the same time, the growing uterus puts increased pressure on the stomach. The combination is a perfect storm for heartburn.
By the time women reach the third trimester, as many as half will experience heartburn at one point or another. During pregnancy, the muscle between the esophagus and stomach relaxes due to hormonal changes related to pregnancy. At the same time, the growing uterus puts increased pressure on the stomach. The combination is a perfect storm for heartburn.
Eating smaller, more frequent meals can help stave off heartburn. Standard treatments – antacids, proton pump inhibitors (Prevacid), or h3 blockers (Tagamet or Pepcid) – are generally safe during pregnancy.
However, if you experience pain below the ribs in your upper abdomen, call your doctor. Although rare, epigastric pain can be a sign of fatty liver disease or preeclampsia, a serious blood pressure disease that can arise suddenly during pregnancy.
3. Diarrhea
Let’s face it – diarrhea is the worst. When it lasts just a few days, diarrhea typically is related to an infection (usually gastroenteritis) or eating something that upsets your stomach. Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Diarrhea that develops without an identifiable trigger or in combination with low back pain and increased vaginal discharge or mucus can be symptoms of preterm labor. Call your doctor immediately if you experience this combination of symptoms.
4. Constipation
Pregnancy hormones affect the lower GI tract, effectively slowing down the transit of stool through the bowels. This slow-motion process allows more water to be absorbed in the stools, which makes them hard to pass. Certain prenatal vitamins and iron therapy also can contribute to constipation. Later in pregnancy, pressure from the growing uterus can also make it harder to pass stools, which increases the risk of hemorrhoids.
Drinking more fluids and eating more fiber is effective in reducing and preventing constipation. Stool softeners are safe to use as well, and some iron supplements actually contain them. More severe constipation might require a mild laxative. Talk to your doctor about additional treatments if you experience abdominal pain, bloody stools, or painful hemorrhoids.
More severe constipation might require a mild laxative. Talk to your doctor about additional treatments if you experience abdominal pain, bloody stools, or painful hemorrhoids.
Most women will experience GI concerns at some point during pregnancy. If your symptoms are serious or if you are concerned, talk to your doctor. It’s better to be safe, and we’re here to help your pregnancy – and GI tract – flow smoothly.
Stay on top of health care news. Subscribe to our blog today.
Diarrhea during pregnancy. What is Diarrhea During Pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Diarrhea during pregnancy is a pathological condition during gestation, characterized by the rapid release of unformed feces. Disorder of the stool can proceed painlessly or be accompanied by belching, nausea, vomiting, discomfort in the mouth, abdominal pain, imperative urge to defecate, fever, weight loss, weakness, fatigue. To determine the cause of diarrhea, clinical, bacteriological, biochemical studies of feces, blood, probing, sigmoidoscopy are carried out. Treatment is most often conservative - medications, dietary adjustments.
Disorder of the stool can proceed painlessly or be accompanied by belching, nausea, vomiting, discomfort in the mouth, abdominal pain, imperative urge to defecate, fever, weight loss, weakness, fatigue. To determine the cause of diarrhea, clinical, bacteriological, biochemical studies of feces, blood, probing, sigmoidoscopy are carried out. Treatment is most often conservative - medications, dietary adjustments.
ICD-10
K59.1 A09.0
- Causes
- Pathogenesis
- Classification
- Symptoms
- Complications
- Diagnostics
- Treatment
- Prognosis and prevention
- Prices for treatment
General
Diarrhea (diarrhea) - an increase in the frequency of bowel movements up to four or more times a day with the separation of liquid or mushy stools, the volume of which exceeds 200-300 ml. Diarrhea is not a separate disease, but one of the manifestations of a violation of the functions or anatomical structure of any organ or body system. Sometimes diarrhea is the first symptom of a pathology that can complicate gestation. The frequency of diarrhea in obstetrics is 34%. Diarrhea is recorded less frequently than constipation, it is more susceptible to age-related (after 35 years), as well as young (under 19years) mother. Usually there are forms with a mild course, ending in a quick recovery. Severe forms pose a serious threat to the life of the mother and fetus. Inpatient treatment with intensive care is necessary for 1.5% of pregnant women suffering from diarrhea.
Sometimes diarrhea is the first symptom of a pathology that can complicate gestation. The frequency of diarrhea in obstetrics is 34%. Diarrhea is recorded less frequently than constipation, it is more susceptible to age-related (after 35 years), as well as young (under 19years) mother. Usually there are forms with a mild course, ending in a quick recovery. Severe forms pose a serious threat to the life of the mother and fetus. Inpatient treatment with intensive care is necessary for 1.5% of pregnant women suffering from diarrhea.
diarrhea during pregnancy
Causes
Most often, diarrhea during pregnancy is caused by physiological (that occurred during gestation, associated with this condition, which is a variant of the norm during this period) changes in the digestive, endocrine, and nervous systems. Another common reason is dietary errors. Diarrhea is manifested by diseases that developed during gestation in women whose body could not adapt to increased stress, and that arose before conception. There are the following sources of intestinal upset in pregnant women:
There are the following sources of intestinal upset in pregnant women:
- Non-communicable diseases of the digestive system. Diarrhea may be accompanied by a physiological decrease in gastric secretion during gestation, as well as pathologies: dysbiosis, cholestatic hepatosis of pregnant women, hypoacid gastritis, less often - ulcerative colitis, Crohn's disease, chronic pancreatitis, tumors.
- Features of the diet. Diarrhea can lead to addiction to coffee, excessive consumption of fatty (including nuts), spicy, spicy foods, sweets, pastries, as well as foods containing a large amount of fiber (fruits, vegetables, cereals). In addition, diarrhea may be accompanied by hypovitaminosis of pregnant women, which occurs due to an imbalance or scarcity of the diet.
- Food intolerance. The cause of diarrhea can be a food idiosyncrasy associated with a lack of enzyme production (for example, lactulose with intolerance to whole milk) or an allergic reaction (more often to citrus fruits, berries, cereals, eggs, chocolate, legumes).
 At the same time, hypersensitization often develops for the first time during the gestational period.
At the same time, hypersensitization often develops for the first time during the gestational period. - Neurogenic factors. By the last trimester of pregnancy, the processes of excitation of the cerebral cortex begin to prevail over the mechanisms of inhibition, which increases the likelihood of developing irritable bowel syndrome. Other causes of neurogenic diarrhea are prolonged psycho-emotional stress, neuropathy.
- Infections and infestations. Diarrhea is caused by acute intestinal infections - bacterial, viral, protozoal, affecting the digestive tract. Nonspecific infections may be the result of the growth of opportunistic flora against the background of a natural decrease in immune activity during pregnancy. The flu is often accompanied by diarrhea. Of the helminths, roundworms are most often involved in diarrhea.
- Taking medications. Iron preparations, magnesium salts, antibiotics, antacids, sugar substitutes, antidiabetic, laxatives, dietary supplements cause diarrhea, using various mechanisms of gastrointestinal dysfunction.
Other, more rare causes of diarrhea in pregnant women include metabolic endocrine diseases (diabetes mellitus, hyperthyroidism, amyloidosis), surgical pathologies (acute appendicitis, intestinal obstruction, mesenteric vascular embolism). False diarrhea is sometimes accompanied by persistent constipation, which is often observed in pregnant women: a prolonged stay of feces leads to irritation of the colon wall, increased secretion of mucus, and the release of liquid stools.
Pathogenesis
About nine liters of fluid enter the intestinal lumen daily, 22% of which is water obtained from food, the rest is formed as a result of the secretion of the digestive organs. About 89% of this liquid is absorbed by the small intestine, about 10% - by the large intestine, only 1.1% (about 100 ml) is excreted in the feces. Diarrhea occurs with increased fluid intake (mostly due to excess intestinal secretion) or as a result of a decrease in absorption capacity. Hypersecretion of the small intestine is associated with infection by pathogenic microorganisms, the use of irritant laxatives. The secretion of the lower intestine is most often increased due to a decrease in the absorption of bile acids.
Hypersecretion of the small intestine is associated with infection by pathogenic microorganisms, the use of irritant laxatives. The secretion of the lower intestine is most often increased due to a decrease in the absorption of bile acids.
Enzymatic deficiency and acceleration of the passage of contents leads to a disorder in the absorption capacity of the small intestine. At the same time, unabsorbed substances accumulate in its lumen, retaining water due to their osmotic action. Reduced absorption in the lower sections is a consequence of increased fluid intake from the ileum, damage to the epithelium, impaired motility of the colon, and a lack of bacteria that ferment carbohydrates. As a result of severe diarrhea, hypovolemia, acidosis, deficiency of nutrients, vitamins, microelements develop. Irritation of the colon leads to a reflex increase in the tone of the pregnant uterus, and the release of active substances associated with inflammation into the blood enhances the effect.
Classification
According to the form of the flow, acute and chronic diarrhea are distinguished. The acute form is characterized by vivid symptoms observed for no more than 3 weeks. The chronic course is characterized by a longer duration of manifestations and less pronounced symptoms. According to the pathogenetic mechanism that contributed to the development of the disorder, four types of diarrhea are distinguished:
- Secretory. This type of diarrhea develops with an increase in the secretion of fluid and electrolytes in the intestine due to damage by pathogenic microorganisms, their toxins, as well as an excess of bile acids.
- Hyperosmolar. Occurs due to the influx of water during the accumulation in the intestine of osmotically active substances (potassium and sodium ions, glucose) as a result of impaired digestion and absorption (with chronic pancreatitis, dysbiosis, enteritis, food intolerance, amyloidosis, obstruction of the biliary tract), intake of excessively salty or sweet food .

- Hyperexudative. Diarrheal syndrome is caused by sweating of exudate through the damaged mucosa in autoimmune, neoplastic diseases of the intestine, some infections (dysentery, salmonellosis, intestinal tuberculosis, campylobacteriosis).
- Motor (dyskinetic). The cause of diarrhea is an increase or decrease in the rate of chyme transit due to impaired intestinal motility. Hyperkinetic diarrhea is accompanied by nervous shocks, neuroses, neuropathies, hyperthyroidism, taking laxatives. The hypokinetic type is associated with small bowel obstruction.
Symptoms
Symptoms of diarrhea during pregnancy depend on the causes of diarrhea, its type, localization of the lesion, intensity of manifestation. Enteritis is manifested by abundant voluminous loose stools without impurities, bowel emptying is often "explosive" in nature. Colitis is characterized by sharp tenesmus (frequency up to 30 times a day), increased defecation with scanty mucous discharge, often mixed with pus and blood. A significant increase in stool in acute diarrhea leads to a rapid decline in strength, severe weakness. Chronic diarrhea is characterized by fatigue, weight loss.
A significant increase in stool in acute diarrhea leads to a rapid decline in strength, severe weakness. Chronic diarrhea is characterized by fatigue, weight loss.
Secretory diarrhea is characterized by abundant light watery or frothy stools without severe abdominal pain, the disorder does not depend on diet, and is not stopped by fasting. Osmolar diarrhea is manifested by an abundant separation of feces containing particles of undigested food: light, pasty in case of pathologies of the hepatobiliary system and gray, with a rancid odor in case of pancreatic insufficiency; diarrhea usually resolves after fasting. The exudative type is characterized by an admixture of blood and pus in the feces. A distinctive feature of hyperkinetic diarrhea is a slight increase in the daily volume of liquefied yellow or greenish stools. With diarrhea caused by decreased motor function, mucus is usually present in the stool.
Diarrhea may be accompanied by other pathological manifestations. Fever accompanies infectious and autoimmune enterocolitis. Tachycardia, sweating is accompanied by a significant loss of water and electrolytes, hyperthyroidism, irritable bowel syndrome. The latter also proceeds with alternating diarrhea with constipation, epigastric discomfort; there may be intense pain, simulating a picture of an acute abdomen, characteristic of surgical pathologies. Epigastric discomfort is also observed with diarrhea associated with the pathology of the liver, pancreas, dysbiosis. Cholestatic diarrhea is accompanied by jaundice, and caused by autoimmune colitis, amyloidosis - inflammation of the joints. With diarrhea associated with Addison's disease, diabetes mellitus, skin pigmentation disorders are observed.
Fever accompanies infectious and autoimmune enterocolitis. Tachycardia, sweating is accompanied by a significant loss of water and electrolytes, hyperthyroidism, irritable bowel syndrome. The latter also proceeds with alternating diarrhea with constipation, epigastric discomfort; there may be intense pain, simulating a picture of an acute abdomen, characteristic of surgical pathologies. Epigastric discomfort is also observed with diarrhea associated with the pathology of the liver, pancreas, dysbiosis. Cholestatic diarrhea is accompanied by jaundice, and caused by autoimmune colitis, amyloidosis - inflammation of the joints. With diarrhea associated with Addison's disease, diabetes mellitus, skin pigmentation disorders are observed.
Complications
The most common and dangerous complication of diarrhea is miscarriage. In 30-44% of cases, the cause of spontaneous abortion is gastrointestinal diseases that occur with diarrhea. Severe diarrhea with a large loss of fluid poses a threat to the life of the patient due to the development of collapse and shock, often leading to death. For the mother and the unborn child, it is also not the intestinal disorder itself that can be dangerous, but its causes. So, the result of an intestinal infection can be purulent-inflammatory gynecological complications (the most formidable is obstetric sepsis) in a woman and intrauterine infection with the development of fetal pathology in the fetus.
For the mother and the unborn child, it is also not the intestinal disorder itself that can be dangerous, but its causes. So, the result of an intestinal infection can be purulent-inflammatory gynecological complications (the most formidable is obstetric sepsis) in a woman and intrauterine infection with the development of fetal pathology in the fetus.
Diagnostics
Diagnostic search is aimed at finding out the causes of diarrhea (alimentary factors, internal diseases, endocrine, neurological or obstetric pathology). Most often, to establish the root cause, it is enough to consult a therapist and an obstetrician-gynecologist: differential diagnosis is carried out on the basis of anamnesis data (information on the frequency and volume of defecation, the nature of the stool, dietary characteristics, the presence of general somatic diseases) and the results of an objective examination (identification and evaluation of concomitant symptoms). To clarify the diagnosis, narrow specialists (gastroenterologist, infectologist, endocrinologist) are involved and instrumental and laboratory research methods are used:
- Fecal analysis.
 Bacterial culture allows you to identify the pathogen in case of infection and choose an antibiotic for its treatment. According to the results of the coprogram, it is possible to confirm or exclude functional pathologies of the stomach, digestive glands, intestines, and also to suspect a violation of the integrity of the mucous membranes (by occult blood). A positive test result for helminth eggs indicates a helminthic invasion.
Bacterial culture allows you to identify the pathogen in case of infection and choose an antibiotic for its treatment. According to the results of the coprogram, it is possible to confirm or exclude functional pathologies of the stomach, digestive glands, intestines, and also to suspect a violation of the integrity of the mucous membranes (by occult blood). A positive test result for helminth eggs indicates a helminthic invasion. - Blood tests. Based on the results of the general clinical analysis, it is possible to establish the inflammatory, allergic nature of diarrhea, suggest malabsorption or malignancy. Biochemical research allows to reveal pathologies of the hepatobiliary system, pancreas, diabetes mellitus.
- Endoscopy. Sigmoidoscopy is performed to detect colitis, tumor changes. With the help of gastric and duodenal sounding, it is possible to detect a decrease in the pH of gastric juice, an increase in the concentration of bile acids, and violations of the exogenous function of the pancreas.

Treatment
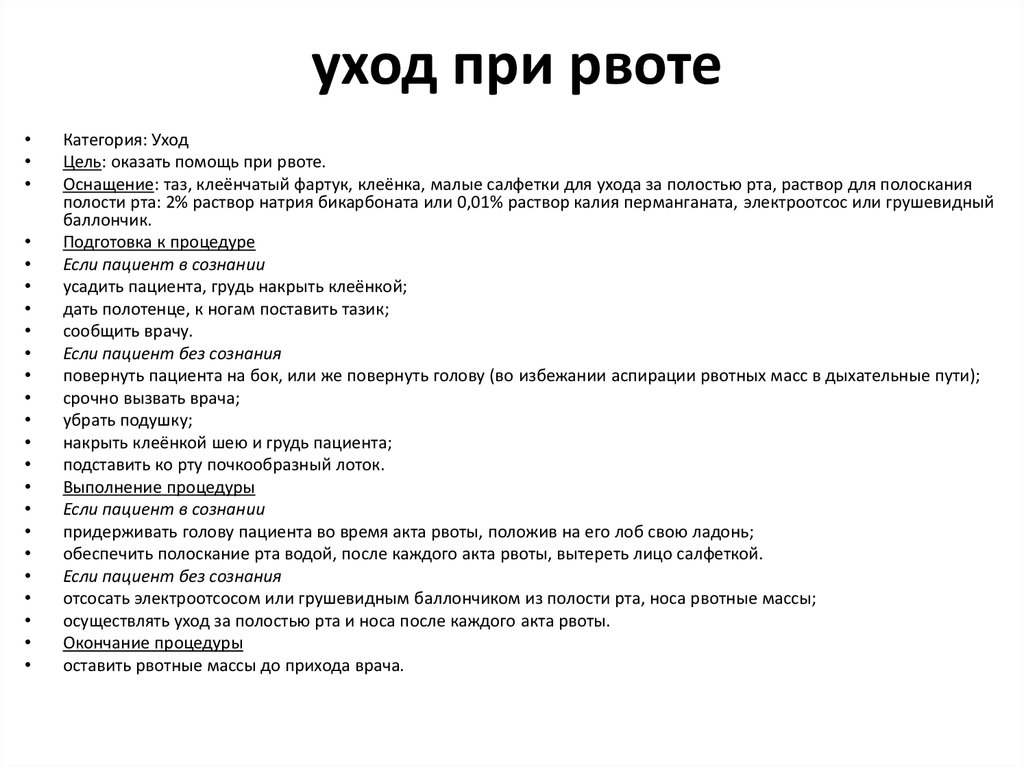
Treatment of diarrhea during pregnancy is carried out under the supervision of an obstetrician-gynecologist. In mild cases, symptomatic and etiotropic therapy is prescribed, aimed at eliminating intoxication and correcting the water-salt balance: enterosorbents, oral rehydration solutions. Particular attention is paid to the diet: food should not irritate the mucous membranes of the gastrointestinal tract, increase peristalsis, or cause fermentation. Fresh pastries, cabbage, legumes, onions, garlic, spices, seasonings, strong broths, fried and stewed foods, carbonated drinks are excluded from the diet. With severe dehydration, intensive therapy is used. Specific treatment is prescribed for chronic, severe acute diarrhea and is selected depending on the underlying disease.
Prognosis and prevention
The prognosis depends on the cause of the intestinal disorder. With alimentary diarrhea, neurogenic diarrhea, easily occurring infections, recovery occurs quickly, complications do not develop. With advanced, progressive pathologies manifested by chronic diarrhea, severe infections, the prognosis worsens, especially for the fetus. Preventive measures include the identification and treatment of chronic internal diseases before pregnancy, regular visits to the antenatal clinic during the gestational period, hygiene, eating fresh, optimally balanced in vitamins, macro- and micronutrients food, avoiding uncontrolled intake of drugs, herbs, dietary supplements, fight against constipation.
With advanced, progressive pathologies manifested by chronic diarrhea, severe infections, the prognosis worsens, especially for the fetus. Preventive measures include the identification and treatment of chronic internal diseases before pregnancy, regular visits to the antenatal clinic during the gestational period, hygiene, eating fresh, optimally balanced in vitamins, macro- and micronutrients food, avoiding uncontrolled intake of drugs, herbs, dietary supplements, fight against constipation.
You can share your medical history, what helped you in the treatment of diarrhea during pregnancy.
Sources
- Acute diarrhea in obstetric practice / Uspenskaya Yu.B. - 2014.
- Differential diagnosis of internal diseases / Hagglin R. - 1993.
- Difficult diagnosis: in 2 volumes / Taylor R.B. - 1991 - T1.
- This article was prepared based on the site: https://www.krasotaimedicina.ru/
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects the digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6.
 Note
Note
Changes in the functioning of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.

If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during a previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Increased levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and will pass by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
Rarely, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea during pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Lactose and gluten use for those intolerant to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Some antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you've recently returned from a holiday in an exotic country with nausea and diarrhea and find out you're pregnant, see your doctor as soon as possible.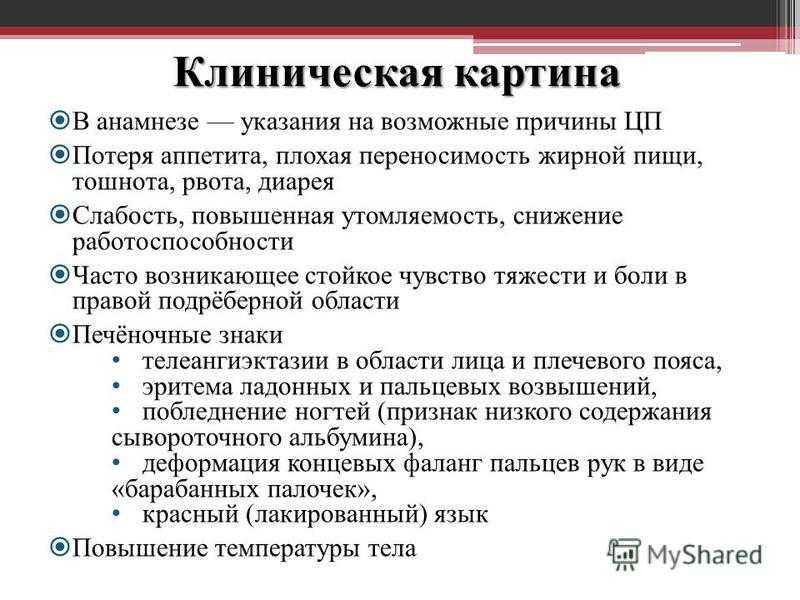
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern.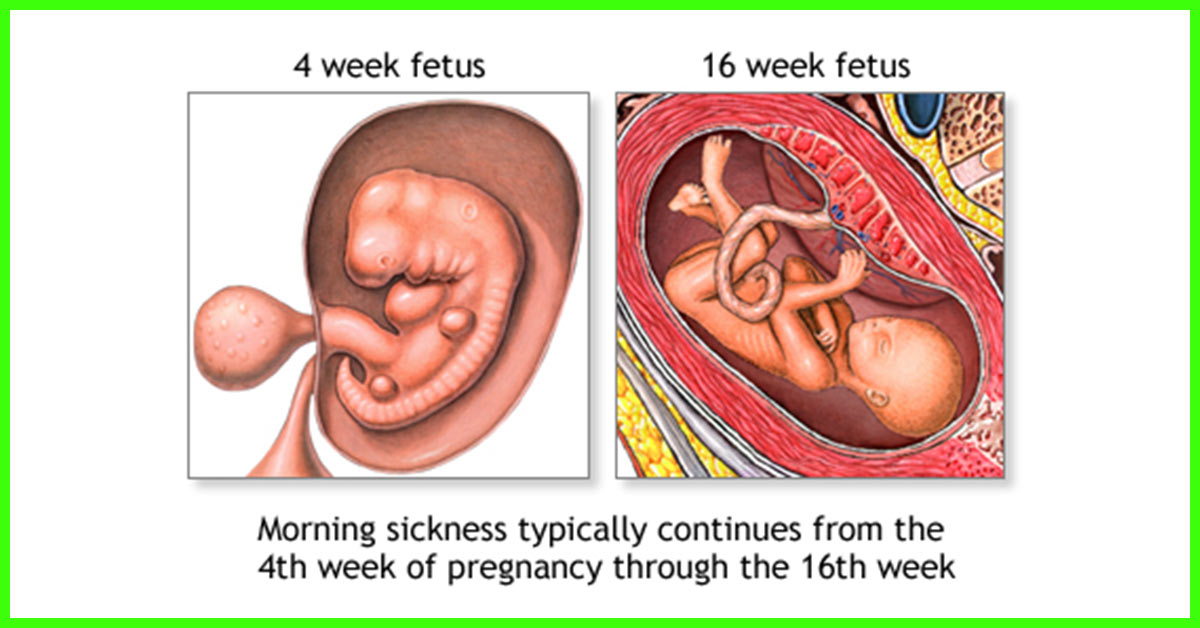 However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Use the Atlas Microbiota Test to find out your body's ability to break down lactose and gluten.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
Avoid cramps and heartburn during pregnancy is unlikely. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular seizures | Unusual vaginal discharge/ spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut.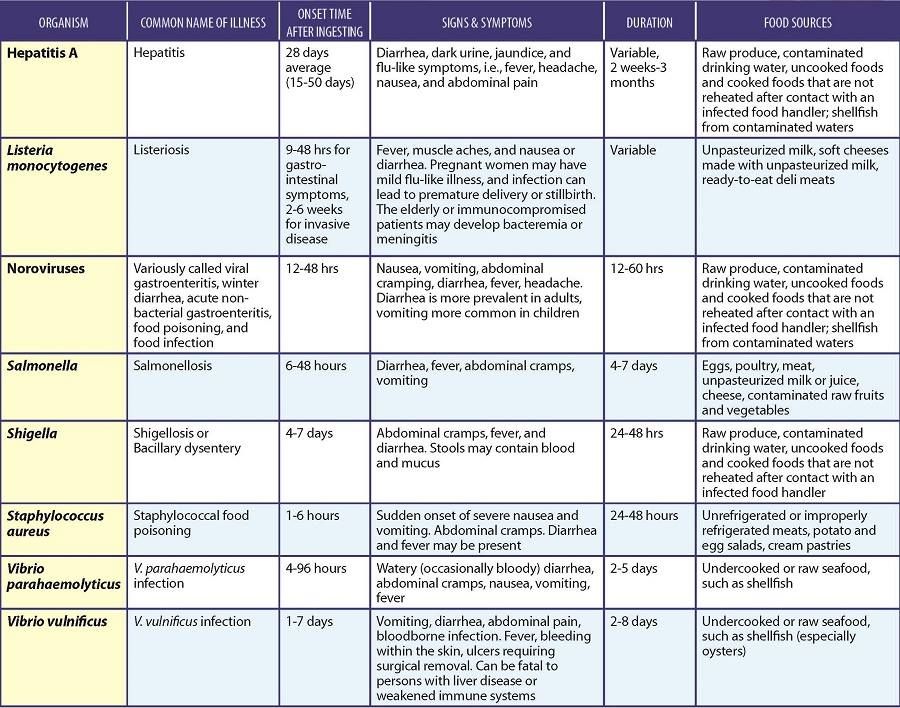 Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test helps you understand how to prepare your gut for future pregnancies and reduce the risk of digestive problems.
☝️ Take note
Now you have all the knowledge and tools you need to help you cope with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.