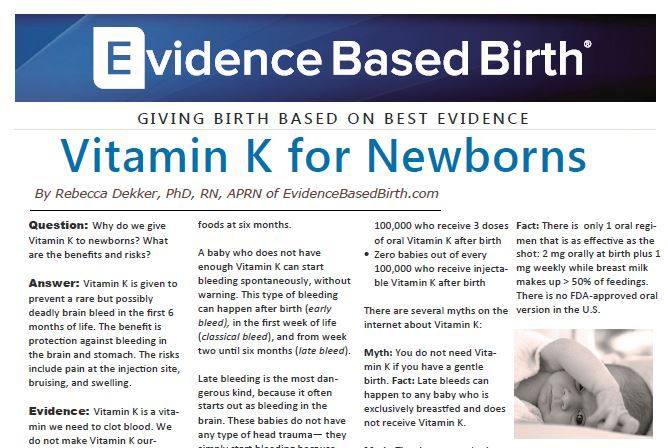
Vitamin k injections for babies
Protect Your Baby from Bleeds – Talk to Your Healthcare Provider about Vitamin K
Download and print this fact sheet pdf icon[PDF – 473 KB, 2 Pages]
Protect Your Baby from Vitamin K Deficiency Bleeding
Before having a baby, most parents don’t give much thought to the vitamin K injection (shot) for their newborn. It’s just not something that is talked about during prenatal checkups, even though babies have been routinely given this important shot at birth since the practice was first recommended by the American Academy of Pediatrics in 1961.
Vitamin K is needed for blood to clot normally. Babies are born with very small amounts of vitamin K in their bodies which can lead to serious bleeding problems. Research shows that a single vitamin K shot at birth protects your baby from developing dangerous bleeding which can lead to brain damage and even death. Ask your healthcare provider about the benefits of Vitamin K before your delivery. Protect your newborn by making sure he or she gets the shot after birth.
What is vitamin K deficiency bleeding (VKDB)?
Vitamin K deficiency bleeding or VKDB, is a condition that occurs when the baby does not have enough Vitamin K.
Without enough vitamin K, your baby has a chance of bleeding into his or her intestines, and brain, which can lead to brain damage and even death. Infants who do not receive the vitamin K shot at birth can develop VKDB up to 6 months of age.
How can I prevent VKDB?
The good news is that VKDB is easily prevented. The easiest and most reliable way to give babies vitamin K is by a shot into a muscle in the leg. One shot given after birth will protect your baby from VKDB.
What is vitamin K?
Vitamin K is a vital nutrient that our body needs for blood to clot and stop bleeding. We get vitamin K from the food we eat. Some vitamin K is also made by the good bacteria that live in our intestines.
Babies have very little vitamin K in their bodies at birth because:
Why does my baby need a vitamin K shot?
- Vitamin K from the mom is not easily shared with the developing baby during the pregnancy
- The intestine of the newborn baby has very little bacteria so they do not make enough vitamin K on their own.

Without enough vitamin K, blood cannot clot well. As a result, bleeding can occur anywhere in the body. This means not only that bleeding from a cut or bruise may continue for a long time, but that uncontrolled bleeding into the brain and other organs may occur.
About half of all babies who develop VKDB bleed into their brains.
Is Vitamin K safe?
A study from the early 1990’s found a possible link between getting vitamin K and developing childhood cancer. Pediatricians became very concerned about this and have done many studies since then, in many different ways, trying to see if this link was true. None of the studies found this link again, even though doctors and scientists looked very hard for it.
Does my baby get vitamin K from breast milk?
Yes, but not enough to prevent VKDB. There is only a little vitamin K in breast milk. Breastfed babies are low in vitamin K for several weeks until they start eating regular foods, usually at 4-6 months, and until the normal intestinal bacteria start making vitamin K.
Should all babies get a vitamin K shot at birth?
Yes. Babies do not have enough vitamin K at birth and are, therefore, at risk for having serious bleeding. Thus, it is very important that all babies get a vitamin K shot to prevent VKDB.
Where can I get more information?
For more information, please visit our website at:
http://www.cdc.gov/ncbddd/vitamink/index.html
FAQs About Vitamin K Deficiency Bleeding
Since 1961, the American Academy of Pediatrics has recommended supplementing low levels of vitamin K in newborns with a single shot of vitamin K given at birth. Low levels of vitamin K can lead to dangerous bleeding in newborns and infants. The vitamin K given at birth provides protection against bleeding that could occur because of low levels of this essential vitamin.
Below are some commonly asked questions and their answers. If you continue to have concerns about vitamin K, please talk to your pediatrician or healthcare provider.
Q: What is vitamin K, and how do low levels of vitamin K and vitamin K deficiency bleeding occur in babies?
A: Vitamin K is used by the body to form clots and to stop bleeding. Babies are born with very little vitamin K stored in their bodies. This is called “vitamin K deficiency” and means that a baby has low levels of vitamin K. Without enough vitamin K, babies cannot make the substances used to form clots, called ‘clotting factors.’ When bleeding happens because of low levels of vitamin K, this is called “vitamin K deficiency bleeding” or VKDB. VKDB is a serious and potentially life-threatening cause of bleeding in infants up to 6 months of age. A vitamin K shot given at birth is the best way to prevent low levels of vitamin K and vitamin K deficiency bleeding (VKDB).
Q: Why do ALL babies need a vitamin K shot – can’t I just wait to see if my baby needs it?
A: No, waiting to see if your baby needs a vitamin K shot may be too late. Babies can bleed into their intestines or brain where parents can’t see the bleeding to know that something is wrong. This can delay medical care and lead to serious and life-threatening consequences. All babies are born with very low levels of vitamin K because it doesn’t cross the placenta well. Breast milk contains only small amounts of vitamin K. That means that ALL newborns have low levels of vitamin K, so they need vitamin K from another source. A vitamin K shot is the best way to make sure all babies have enough vitamin K. Newborns who do not get a vitamin K shot are 81 times more likely to develop severe bleeding than those who get the shot.
Babies can bleed into their intestines or brain where parents can’t see the bleeding to know that something is wrong. This can delay medical care and lead to serious and life-threatening consequences. All babies are born with very low levels of vitamin K because it doesn’t cross the placenta well. Breast milk contains only small amounts of vitamin K. That means that ALL newborns have low levels of vitamin K, so they need vitamin K from another source. A vitamin K shot is the best way to make sure all babies have enough vitamin K. Newborns who do not get a vitamin K shot are 81 times more likely to develop severe bleeding than those who get the shot.
Q: Doesn’t the risk of bleeding from low levels of vitamin K only last a few weeks?
A: No, VKDB can happen to otherwise healthy babies up to 6 months of age. The risk isn’t limited to just the first 7 or 8 days of life and VKDB doesn’t just happen to babies who have difficult births. In 2013, the Centers for Disease Control and Prevention (CDC) investigated 4 cases of infants with bleeding from low levels of vitamin K. All four were over 6 weeks old when the bleeding started and they had been healthy and developing normally. None of them had received a vitamin K shot at birth.
In 2013, the Centers for Disease Control and Prevention (CDC) investigated 4 cases of infants with bleeding from low levels of vitamin K. All four were over 6 weeks old when the bleeding started and they had been healthy and developing normally. None of them had received a vitamin K shot at birth.
Q: Isn’t VKDB really rare?
A: VKDB is rare in the United States, but only because most newborns get the vitamin K shot. Over the past two decades, many countries in Europe have started programs to provide vitamin K at birth – afterward, they all saw declines in the number of cases of VKDB to very low levels. However, in areas of the world where the vitamin K shot isn’t available, VKDB is more common, and many cases of VKDB have been reported from these countries
In the early 1980s in England, some hospitals started giving vitamin K only to newborns that were thought to be at higher risk for bleeding. They then noticed an increase in cases of VKDB. This tells us that giving vitamin K to prevent bleeding is what keeps VKDB a rare condition – when vitamin K is not given to newborns, cases of bleeding occur and VKDB stops being rare.
This tells us that giving vitamin K to prevent bleeding is what keeps VKDB a rare condition – when vitamin K is not given to newborns, cases of bleeding occur and VKDB stops being rare.
Q: What happens when babies have low levels of vitamin K and get VKDB?
A: Babies without enough vitamin K cannot form clots to stop bleeding and they can bleed anywhere in their bodies. The bleeding can happen in their brains or other important organs and can happen quickly. Even though bleeding from low levels of vitamin K or VKDB does not occur often in the United States, it is devastating when it does occur. One out of every five babies with VKDB dies. Of the infants who have late VKDB, about half of them have bleeding into their brains, which can lead to permanent brain damage. Others bleed in their stomach or intestines, or in other parts of the body. Many of the infants need blood transfusions, and some need surgeries.
Q: I heard that the vitamin K shot might cause cancer.
 Is this true?
Is this true?A: No. In the early 1990s, a small study in England found an “association” between the vitamin K shot and childhood cancer. An association means that two things are happening at the same time in the same person, but doesn’t tell us whether one causes the other. Figuring out whether vitamin K might cause childhood cancer was very important because every newborn is expected to get a vitamin K shot. If vitamin K was causing cancer, we would expect to see the same association in other groups of children. Scientists looked to see if they could find the same association in other children, but this association between vitamin K and childhood cancer was never found again in any other study.
Q: Can the other ingredients in the shot cause problems for my baby? Do we really know that the vitamin K shot is safe?
A: Yes, the vitamin K shot is safe. Vitamin K is the main ingredient in the shot. The other ingredients make the vitamin K safe to give as a shot. One ingredient keeps the vitamin K mixed in the liquid; another keeps the liquid from being too acidic. One of the ingredients is benzyl alcohol, a preservative. Benzyl alcohol is a common ingredient in many medications.
One ingredient keeps the vitamin K mixed in the liquid; another keeps the liquid from being too acidic. One of the ingredients is benzyl alcohol, a preservative. Benzyl alcohol is a common ingredient in many medications.
In the 1980s, doctors recognized that very premature infants who were in neonatal intensive care units might become sick from benzyl alcohol toxicity because many of the medicines and fluids needed for their intensive care contained benzyl alcohol as a preservative. Although the toxicity was only reported for very premature infants, since then doctors have tried to minimize the amount of benzyl-alcohol-containing medications they give. Clearly, the small amount of benzyl alcohol in the vitamin K shot is not enough to be dangerous, even when given in combination with other medications that also contain small amounts of this preservative.
Q: The dose of the shot seems high. Is that too much for my baby?
A: No, the dose in the vitamin K shot is not too much for babies. The dose of vitamin K in the shot is high compared to the daily requirement of vitamin K. But remember babies don’t have much vitamin K when they are born and won’t have a good supply of vitamin K until they are close to six months old. This is because vitamin K does not cross the placenta and breast milk has very low levels of vitamin K.
The dose of vitamin K in the shot is high compared to the daily requirement of vitamin K. But remember babies don’t have much vitamin K when they are born and won’t have a good supply of vitamin K until they are close to six months old. This is because vitamin K does not cross the placenta and breast milk has very low levels of vitamin K.
The vitamin K shot acts in two ways to increase the vitamin K levels. First, part of the vitamin K goes into the infant’s bloodstream immediately and increases the amount of vitamin K in the blood. This provides enough vitamin K so that the infant’s levels don’t drop dangerously low in the first few days of life. Much of this vitamin K gets stored in the liver and it is used by the clotting system. Second, the rest of the vitamin K is released slowly over the next 2-3 months, providing a steady source of vitamin K until an infant has another source from his or her diet.
Q: Can I increase vitamin K in my breast milk by eating different foods or taking multivitamins or vitamin K supplements?
A: We encourage moms to eat healthy and take multivitamins as needed. Although eating foods high in vitamin K or taking vitamin K supplements can slightly increase the levels of vitamin K in your breast milk, neither can increase levels in breast milk enough to provide all of the vitamin K an infant needs.
Although eating foods high in vitamin K or taking vitamin K supplements can slightly increase the levels of vitamin K in your breast milk, neither can increase levels in breast milk enough to provide all of the vitamin K an infant needs.
When infants are born, their already low levels of vitamin K fall even lower. Infants need enough vitamin K to (a) make up for their extra-low levels, (b) start storing it in the liver for future use, and (c) ensure good bone and blood health. Breast milk – even from mothers supplementing with vitamin K sources – can’t provide enough to do all of these things.
Q: My baby is so little. What can I do to make the vitamin K shot less painful and traumatic?
A: Babies, just like us, feel pain, and it is important to reduce even small amounts of discomfort. Babies feel less pain from shots if they are held and allowed to suck.You can ask to hold your baby while the vitamin K shot is given so that your baby can be comforted by you. Breastfeeding while the shot is given and immediately after can be comforting too. All of these are things parents can do to ease pain and soothe their baby.
Breastfeeding while the shot is given and immediately after can be comforting too. All of these are things parents can do to ease pain and soothe their baby.
Remember that if your baby does not get the vitamin K shot, his or her risk of developing severe bleeding is 81 times higher than if he or she got the shot. Diagnosis and treatment of VKDB often involves many painful procedures, including repeated blood draws.
Q: Overall, what are the risks and benefits of the vitamin K shot?
The risks of the vitamin K shot are the same risks that are part of getting most any other shot. These include pain or even bruising or swelling at the place where the shot is given. A few cases of skin scarring at the site of injection have been reported. Only a single case of allergic reaction in an infant has been reported, so this is extremely rare.
Although there have been concerns about some other risks, like a risk for childhood cancer or risks because of additional ingredients, none of these risks have been proven by scientific studies.
The main benefit of the vitamin K shot is that it can protect your baby from VKDB, a dangerous condition that can cause long-term disability or death. In addition, the diagnosis and treatment of VKDB often includes multiple and sometimes painful procedures, such as blood draws, CT scans, blood transfusions, or anesthesia and surgery.
The American Academy of Pediatrics has recommended the Vitamin K shot since 1961, and has repeatedly stood by that recommendation because the risks of the shot don’t outweigh the risks of VKDB, which are based on decades of evidence and decades of experience with babies who were hospitalized or died from VKDB.
Your child’s doctor is the best person to talk to about vitamin K. Like you, your child’s doctor wants to see your children grow up safe and healthy and wants to support your efforts to make the best decisions for their health. If you have concerns about vitamin K, talk to your child’s doctor.
Why are newborns given vitamin K injections?
At Mother and Child clinics, we recommend vitamin K injections for all newborns to prevent hemorrhagic disease.
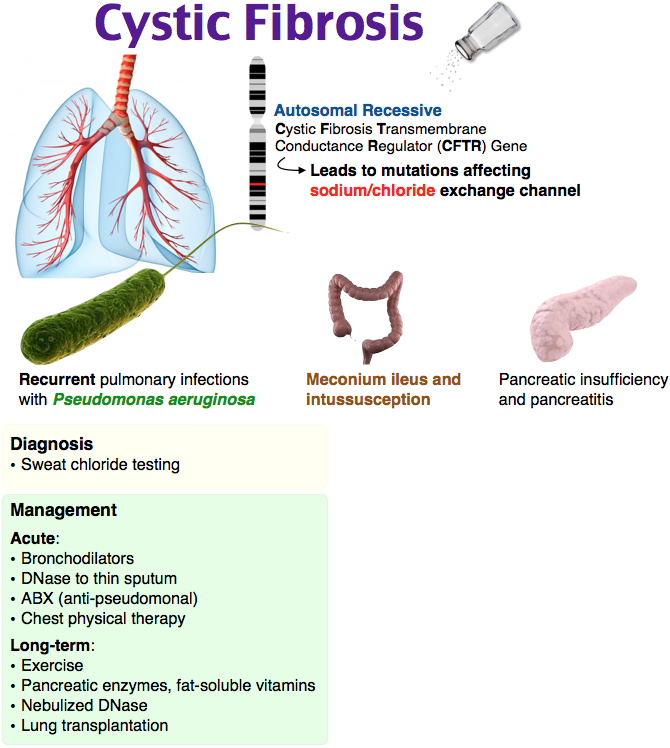
Hemorrhagic disease (HRD), or vitamin K-deficient hemorrhagic syndrome, is a disease manifested by increased bleeding in newborns and children during the first months of life, due to a deficiency of blood coagulation factors, the activity of which depends directly on vitamin K.
Vitamin K of plant origin, which is called vitamin K 1 or phylloquinone, enters the body with food - green vegetables, vegetable oils, dairy products. Another form of vitamin K, vitamin K2, or menaquinone, is of bacterial origin. Vitamin K 2 is mainly synthesized by the intestinal microflora, which is extremely poor in newborns.
In healthy newborns, the level of vitamin K-dependent coagulation factors in blood plasma is 30-60% of that in adults. Their concentration increases gradually and reaches the level of adults by the sixth week of life. In almost all healthy full-term infants in the first five days of life, there is a decrease in the level of procoagulants, physiological anticoagulants and plasminogen. nine0003
In almost all healthy full-term infants in the first five days of life, there is a decrease in the level of procoagulants, physiological anticoagulants and plasminogen. nine0003
For the newborn, the only source of vitamin K is mother's milk, formula or medicine. Moreover, the amount of vitamin K received by a child depends on the type of feeding. The level of vitamin K 1 in breast milk ranges from 1 to 10 µg/l, on average 2-2.5 µg/l, which is significantly lower than in artificial milk formulas (about 50 µg/l in mixtures for full-term babies; 60 -100 mcg / l - in mixtures for premature babies). Thus, newborns, due to their physiological characteristics of the coagulation system and vitamin K metabolism, are predisposed to the development of vitamin K-deficient hemorrhagic syndrome. nine0003
PLEASE NOTE! Poor blood clotting is a condition dangerous for the body, in which bleeding or hemorrhage is noted in various organs. This pathology develops in 0.25-0.5% of newborns.
RISK FACTORS FOR THE DEVELOPMENT OF RHD
• Exclusive breastfeeding
• Lack of prophylactic administration of vitamin K immediately after birth
• Chronic fetal hypoxia and asphyxia at birth
• Giving birth
• Intrauterine development delay
• Giving birth by cesarean section
• Nedness
• The use of a wide range of
• Long -term parenteral nutrition in the conditions of inadequate supply of
• Diseases and condition of the child that contribute impaired synthesis and absorption of vitamin K
• malabsorption syndrome (cystic fibrosis, diarrhea with fat malabsorption lasting more than one week)
• short bowel syndrome;
• cholestasis;
• pre-eclampsia
• maternal diseases (liver and intestinal diseases).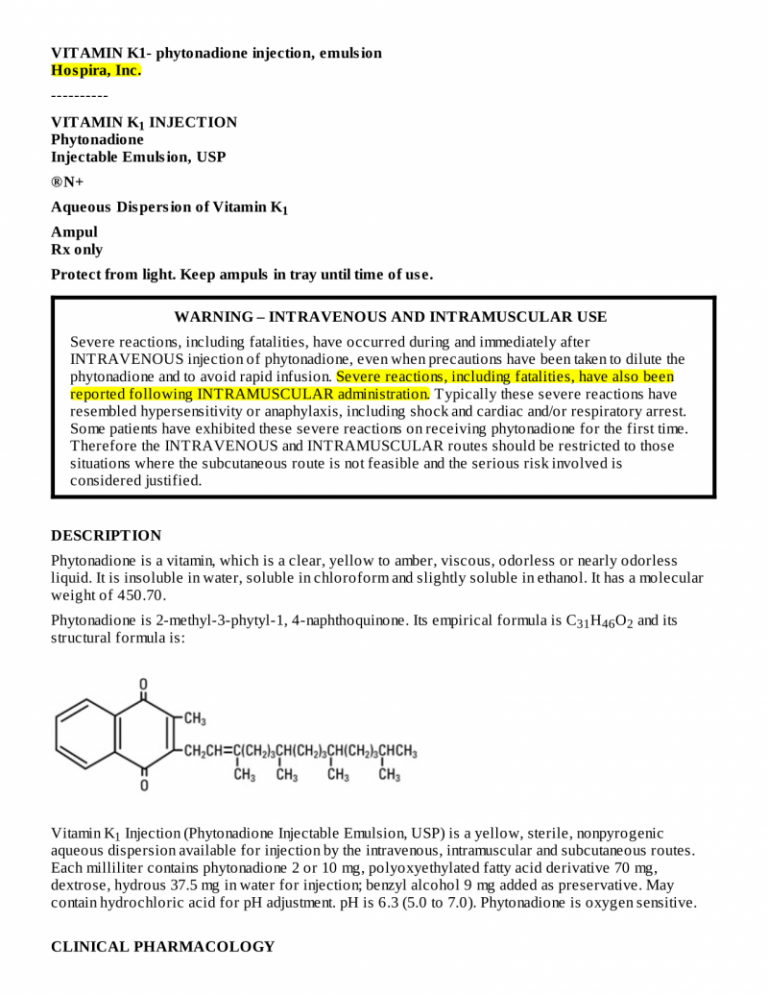
Understanding vaccinations. Part 29 Vitamin K: amantonio - LiveJournal
If you are not doing something controversial, you are not doing something important.
Michael Skinner
1. One procedure that almost every baby undergoes immediately after birth in most developed countries is the vitamin K injection. diseases of the newborn (VKDB). nine0004 2. Vitamin K in neonates: facts and myths. (Lippi, 2011, Blood Transfus)
Vitamin K was discovered in the early 1930s when a Danish biochemist discovered that chickens fed a low-fat, cholesterol-free diet developed subcutaneous and intramuscular bleeding. The vitamin was named with the letter K for coagulation.
Vitamin K1 is found in leafy green vegetables such as spinach, chard, turnips, kale (also cauliflower, Brussels sprouts, kale), some fruits (avocado, banana, kiwi), and some vegetable oils. Vitamin K2 is synthesized by many types of intestinal bacteria, but this is most likely not a particularly significant source.
 nine0054 The IOM recommended daily dose of the vitamin is 120 mcg for men and 90 mcg for women. In Europe, the recommended dose is much lower.
nine0054 The IOM recommended daily dose of the vitamin is 120 mcg for men and 90 mcg for women. In Europe, the recommended dose is much lower. The recommended dose for infants is 2 mcg/day. Breast milk contains 1-4 mcg/litre.
There are 3 types of hemorrhagic disease of the newborn (called VKDB - Vitamin K deficiency bleeding since 1999).
1) Early (in the first 24 hours after birth). It occurs almost exclusively in infants whose mothers have taken vitamin K inhibitory drugs (anticonvulsants and anti-tuberculosis drugs, some antibiotics, coumarin, etc.). It is observed in 6-12% (among those taking medications) and is usually difficult. nine0054 2) Classic (24 hours - 7 days after birth). Associated with malnutrition. It occurs in 0.25-1.5% (old data) and 0-0.44% (new data) and is usually mild. Includes bleeding from the umbilical cord, as well as bleeding after circumcision or injections.
3) Late (2-12 weeks after birth). Associated with exclusive breastfeeding (XF) (because vitamin K is added to infant formulas) and is associated with vitamin K malabsorption due to liver disease, and with inadequate intake of the vitamin.
 The incidence in non-vitamin K infants on exclusive breastfeeding is 1 in 15-20,000. It is severe (20% mortality and frequent neurological sequelae). nine0054 An obvious paradox in neonatal homeostasis is that coagulation tests do not indicate bleeding. Today it is clear to us that the physiology of hemostasis in childhood differs significantly from that in adults. Human and animal studies indicate that neonatal clotting ratios differ quantitatively from adults, but not qualitatively. [1] [2]
The incidence in non-vitamin K infants on exclusive breastfeeding is 1 in 15-20,000. It is severe (20% mortality and frequent neurological sequelae). nine0054 An obvious paradox in neonatal homeostasis is that coagulation tests do not indicate bleeding. Today it is clear to us that the physiology of hemostasis in childhood differs significantly from that in adults. Human and animal studies indicate that neonatal clotting ratios differ quantitatively from adults, but not qualitatively. [1] [2] The hemostasis system is fully developed at the age of 3-6 months. Therefore, it is important to recognize that the differences between adults and infants are probably physiological and are not always indicative of pathology. nine0054 Both oral and intramuscular vitamin K protect against the classic form of VKDB. However, a single oral dose does not protect all infants from late VKDB.
3. Vitamin K deficiency bleeding (VKDB) in early infancy. (Shearer, 2009, Blood Rev)
Even in developed countries, there are few accurate data on the prevalence of classic VKDB. In a British study in 1988-90, the incidence was ~1:20,000, i.e. it did not differ from the incidence of late VKDB. In the 1930s in Oslo, the incidence was 0.8%. In research at Cincinnati at 19In the 1960s, the incidence was 1.7% among breastfeeding infants. But these data cannot be representative, because the hospital served predominantly poor blacks.
In a British study in 1988-90, the incidence was ~1:20,000, i.e. it did not differ from the incidence of late VKDB. In the 1930s in Oslo, the incidence was 0.8%. In research at Cincinnati at 19In the 1960s, the incidence was 1.7% among breastfeeding infants. But these data cannot be representative, because the hospital served predominantly poor blacks.
Poverty predisposes to classic VKDB, and the incidence is much higher in poor countries than in developed countries.
Late VKDB is often preceded by warning bleeding that should be investigated.
Efficacy
4. Vitamin K prophylaxis for prevention of vitamin K deficiency bleeding: a systematic review. (Sankar, 2016, J Perinatol)
Systematic review of injection efficacy.
Among those who have not received vitamin K, the incidence of late VKDB in poor countries is 80 per 100,000 and in rich countries 8.8 per 100,000.
Routine prevention strategies are not without pitfalls. The usual prophylactic dose (1 mg) is 1000 times higher than the recommended daily requirement. Studies have shown an increased frequency of sister chromatid exchange in lymphocytes and mutagenic activity at such high concentrations. In addition, intramuscular administration can cause local trauma, vascular and nerve damage, abscesses, and muscle hematoma. Not surprisingly, some countries resist universal prophylaxis, and instead use selective prophylaxis only for newborns with an increased risk of bleeding. nine0054 Classic VKDB: One study showed a 27% reduction in the risk of injection-related bleeding and an 81% reduction in major bleeding. Another study showed an 82% reduction in bleeding after circumcision.
Studies have shown an increased frequency of sister chromatid exchange in lymphocytes and mutagenic activity at such high concentrations. In addition, intramuscular administration can cause local trauma, vascular and nerve damage, abscesses, and muscle hematoma. Not surprisingly, some countries resist universal prophylaxis, and instead use selective prophylaxis only for newborns with an increased risk of bleeding. nine0054 Classic VKDB: One study showed a 27% reduction in the risk of injection-related bleeding and an 81% reduction in major bleeding. Another study showed an 82% reduction in bleeding after circumcision.
There are no randomized trials of the effect of prophylaxis on late VKDB. According to observational studies, the risk of late VKDB is reduced in those who received the injection by 98%.
Cochrane systematic review found no difference in blood clotting after intramuscular and oral administration. nine0054 Oral vitamin intake is cheaper and has no theoretical risk of mutagenicity.
Synthetic vitamin K3 (menadione) has been used in the past and has been associated with an increased risk of hemolysis and kernicterus.
Vitamin K3 (Vikasol) is still used for the prevention of VKDB in Russia and Ukraine.
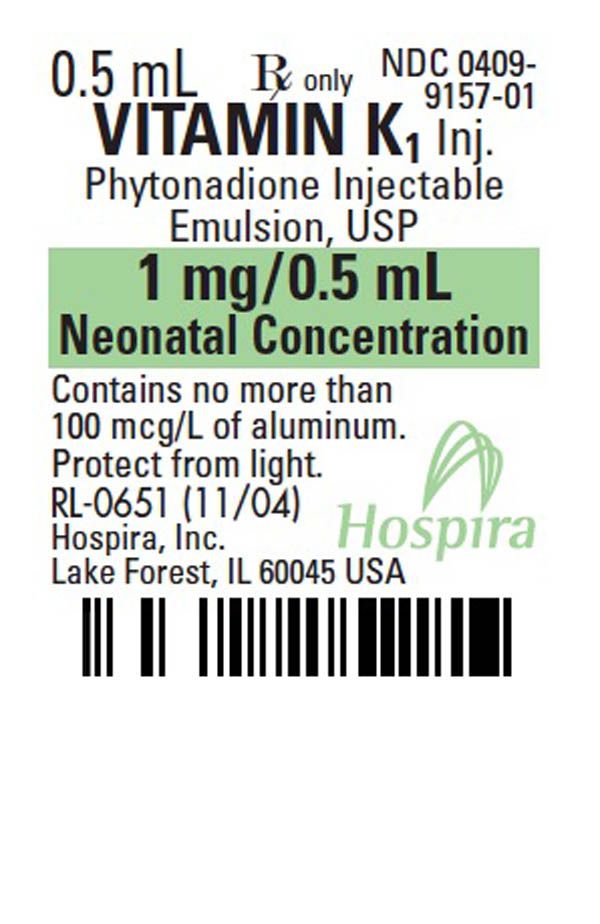
5. Vitamin K1 (phytomenadione/phylloquinone) has been used in developed countries since the early 1960s. (Hereinafter, vitamin K refers to K1) .
Injections from the following manufacturers are currently available:
AquaMEPHYTON (Merck)
Hospira
Amphastar
Konakion MM (Roche)
Oral
6. A new mixed micellar preparation for oral vitamin K prophylaxis: randomized controlled comparison with an intramuscular formulation in breast fed infants. (Greer, 1998, Arch Dis Child)
Those who received 3 oral doses (Konakion MM) had higher levels of vitamin K for 8 weeks compared to those who received the intramuscular injection.
7. There have been many more studies comparing intramuscular versus oral vitamin K.
Most concluded that oral administration is no less effective than intramuscular: [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15].
But there have also been studies showing that oral administration is less effective than intramuscular administration in preventing late VKDB: [1]
8. Prevention of vitamin K deficiency bleeding: efficacy of different multiple oral dose schedules of vitamin K. (Cornelissen, 1997, Eur J Pediatr)
This study compared different prevention regimens in 4 countries. The authors conclude that 3 oral doses are less effective than injection. But here, a previous version of Konakion was used (which also contained phenol and propylene glycol). In the Netherlands, a daily dose of 25 micrograms was used, which was as effective as an injection. nine0054 In subsequent studies, however, it turned out that a few cases of VKDB did occur in the Netherlands among infants with predisposing liver disease who received vitamin K orally.
In Denmark, 1 mg per week orally for 3 months was started and this reduced the incidence of late VKDB to zero.
29% of the oral vitamin is absorbed in the intestines.
In those born in summer, the blood coagulation status was significantly higher than in those born in the spring.
Effect of maternal vitamin levels
9. Vitamin K prophylaxis to prevent neonatal vitamin K deficient intracranial haemorrhage in Shizuoka prefecture. (Nishiguchi, 1996, Br J Obstet Gynaecol)
In Japan, the chance of intracranial hemorrhage was 1 in 4,000 newborns before vitamin K was used. In Germany and the UK, where vitamin K is used, the chance of hemorrhage was 1 in 30,000.
Infant blood clotting status was significantly higher when lactating mothers were given vitamin K2 (15 mg/day from day 14 postpartum for two weeks). nine0003
10. Are breast-fed infants vitamin K deficient? (Greer, 2001, Adv Exp Med Biol)
Breast milk contains very little vitamin K (~1 µg/L). But if a mother consumes more than 1 mcg/kg/day during pregnancy and lactation, this significantly increases the level of vitamin K in milk (up to 80 mcg/l) and in the infant's blood plasma. More: [1]
More: [1]
11. Vitamin K in preterm breastmilk with maternal supplementation. (Bolisetty, 1998, Acta Paediatr)
6 lactating mothers received 2.5 mg/day of vitamin K1 orally for 2 weeks. After the first dose, the amount of vitamin K in milk increased from an average of 3 µg/l to 23 µg/ml, and after 6 days it stabilized at 64 µg/l. nine0003
12. Vitamin K1 content of maternal milk: influence of the stage of lactation, lipid composition, and vitamin K1 supplements given to the mother. (von Kries, 1987, Pediatr Res)
The concentration of vitamin K in hindmilk is higher than in foremilk, which is not surprising since hindmilk is known to be more fatty. The concentration of vitamin K in colostrum is higher than in mature milk and correlates with cholesterol levels.
Maternal vitamin K supplementation (0.5–3 mg) significantly increased vitamin K concentrations in milk. nine0003
Neonatal jaundice
13. Effect of Vitamin-K Dosage on Plasma-Bilirubin Levels in Premature Infants. (Bound, 1956, Lancet)
(Bound, 1956, Lancet)
In the 1950s, large doses of vitamin K2 (up to 90 mg) were given to newborns. This study found that among preterm infants who received 30 mg of vitamin K over three days, 38% had high bilirubin levels (greater than 18 mg/100 ml) on the fifth day, and among those who received 1 mg, only 4% had high bilirubin levels. (High bilirubin is neonatal jaundice.) More: [1] [2] [3] [4]
14. Overnutrition in Prenatal and Neonatal Life: A Problem? (Cochrane, 1965, Can Med Assoc J)
Recent studies have confirmed the toxic effects of excessive amounts of synthetic vitamin K administered to neonates and preterm infants. It also turned out that the introduction of large amounts of vitamin K to the mother shortly before delivery leads to an increase in the level of bilirubin in the newborn. This substance, once thought to be harmless, is dangerous if given in large amounts to mothers before childbirth, so much lower doses are given today. Vitamin K of natural origin does not have a similar effect.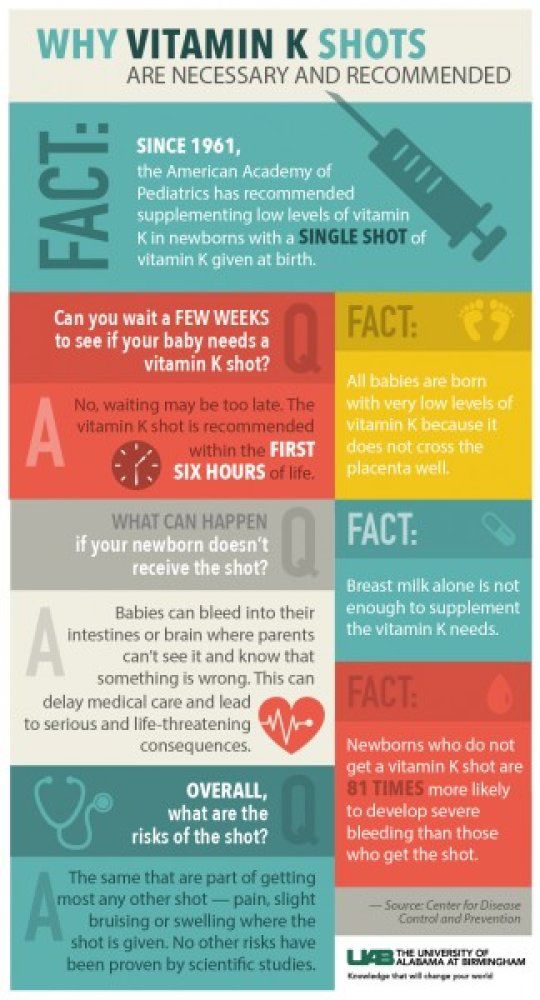 nine0003
nine0003
15. Merck and other manufacturers report that neonatal jaundice may be dose related. [1] [2] [3]
Dose
16. Vitamin K status of premature infants: implications for current recommendations. (Kumar, 2001, Pediatrics)
Preterm infants have very high vitamin K levels 2 weeks after injection. The authors suggest a dose reduction for premature infants.
17. Vitamin K prophylaxis for premature infants: 1 mg versus 0.5 mg. (Costakos, 2003, Am J Perinatol)
In premature infants, vitamin K levels on the second day after injection (0.5-1 mg) were 1900-2600 times higher than normal levels in adults, and on the tenth day - 550-600 times higher. Vitamin levels in the 0.5 mg group did not differ from those in the 1 mg group.
18. Plasma concentrations after oral or intramuscular vitamin K1 in neonates. (McNinch, 1985, Arch Dis Child)
The concentration of vitamin K in neonates 12 hours after injection was 9000 times higher and 24 hours later 2200 times higher than the normal concentration in an adult. nine0054 The concentration of vitamin K at 4 hours after an oral dose is 300 times higher, and after 24 hours 100 times higher than the usual concentration in an adult.
nine0054 The concentration of vitamin K at 4 hours after an oral dose is 300 times higher, and after 24 hours 100 times higher than the usual concentration in an adult.
Cow's milk contains significantly more vitamin K. When babies were given 90 ml of cow's milk for the first 48 hours 40 years ago, this reduced the incidence from 0.8% to almost zero.
It is reported here that the blood coagulation status of infants was dependent on the dose of breast milk in the first days of life. For those who received more than 100 ml of milk per day on the 3rd and 4th days, it was significantly higher than for those who received less than 100 ml/day in the first 4 days. More: [1]
It is reported here that infants who were fed immediately after birth had significantly higher blood clotting status than infants who were fed 24 hours after birth.
Cancer
19. Childhood cancer, intramuscular vitamin K, and pethidine given during labor. (Golding, 1992, BMJ)
Among those who received an intramuscular injection of vitamin K, the risk of cancer was 2 times higher. A similar result was obtained in another study by the same authors. nine0054 That is, preventing 30-60 cases of hemorrhagic disease will result in 980 additional cases of cancer.
A similar result was obtained in another study by the same authors. nine0054 That is, preventing 30-60 cases of hemorrhagic disease will result in 980 additional cases of cancer.
That evolution has allowed the development of vitamin K deficiency in normal breastfed infants, which results in a small risk of hemorrhagic disease, has always seemed physiologically flawed. The most likely explanation for this phenomenon is that there is some evolutionary advantage that outweighs this risk.
It is possible that a relative deficiency of vitamin K in the critical phase of rapid growth may protect vulnerable tissues from mutagenesis. nine0003
20. Case-control studies of relation between childhood cancer and neonatal vitamin K administration. (Passmore, 1998, BMJ)
The chance of bleeding among non-risk infants is 1 in 10,000. Among those who received the injection, the chance of bleeding is 1 in a million.
In this study, cancer (mainly leukemia) was associated with intramuscular injection of vitamin K (OR=1. 44, CI: 1.00-2.08). Children who were diagnosed before 12 months of age were excluded from the study. nine0054 There have been several other studies that have found no correlation between injection and increased risk of cancer. This study did not find a correlation between injection and cancer in general, but found a correlation with acute lymphoblastic leukemia up to 6 years of age (OR=1.79).
44, CI: 1.00-2.08). Children who were diagnosed before 12 months of age were excluded from the study. nine0054 There have been several other studies that have found no correlation between injection and increased risk of cancer. This study did not find a correlation between injection and cancer in general, but found a correlation with acute lymphoblastic leukemia up to 6 years of age (OR=1.79).
There is currently no link between vitamin K injection and cancer. However, no randomized trials have been conducted and a small increase in risk cannot be ruled out. nine0054 The authors believe that injections should only be used for infants at risk.
21. Vitamin K and childhood cancer: analysis of individual patient data from six case-control studies. (Roman, 2002, Br J Cancer)
The authors analyzed 6 studies on vitamin K injection and cancer, and concluded that if the data were analyzed one way, there was no association between the risk of leukemia and the injection, and if the other way, there was a slight association ( OR=1. 21, CI:1.02-1.44). When one study was excluded from the analysis, statistical significance disappeared (OR=1.16, CI: 0.97-1.39)).
21, CI:1.02-1.44). When one study was excluded from the analysis, statistical significance disappeared (OR=1.16, CI: 0.97-1.39)).
The authors conclude that although small effects cannot be ruled out, there is no strong evidence that vitamin K injection is associated with leukemia.
22.
23.
24. Why do we need a clinical trial for vitamin K. (Slattery, 1994, BMJ) at mother and GV.
Vitamin K is given to babies at birth, but we still don't know if it poses a significant risk. Although vitamin K has been used for 30 years, the first study of its long-term effects was published only 19 years ago.92 year. Since the drug is given to so many people, even a small risk can lead to a lot of side effects. Therefore, it is important to establish the potential harm of prevention. Only a large randomized trial including children at low risk of hemorrhagic disease, of which one group will receive vitamin K and the other will not, will be able to answer this question.
Other Ingredients
25. The CDC reports that all newborns are vitamin K deficient and that the injection is completely safe. Benzyl alcohol is used as a preservative, which is also completely safe and is used in many medicines. True, they write, in the 1980s they discovered that premature babies can get sick from the toxicity of benzyl alcohol, since many medicines contain it as a preservative. But despite the fact that toxicity was only found in premature babies, since then, doctors have been trying to minimize the amount of benzyl alcohol in the medicines they give to children. And it is clear, they write (although they do not say where), that the amount of benzyl alcohol in the injection is so low that it is safe. nine0003
26. The half-lethal dose of benzyl alcohol in mice is 0.48 g/kg. (Ordinary ethyl alcohol is 4 times less toxic than benzyl).
In total, an injection ampoule (from Hospira) contains 9 mg of benzyl alcohol per 2 mg of vitamin K. That is approximately 0.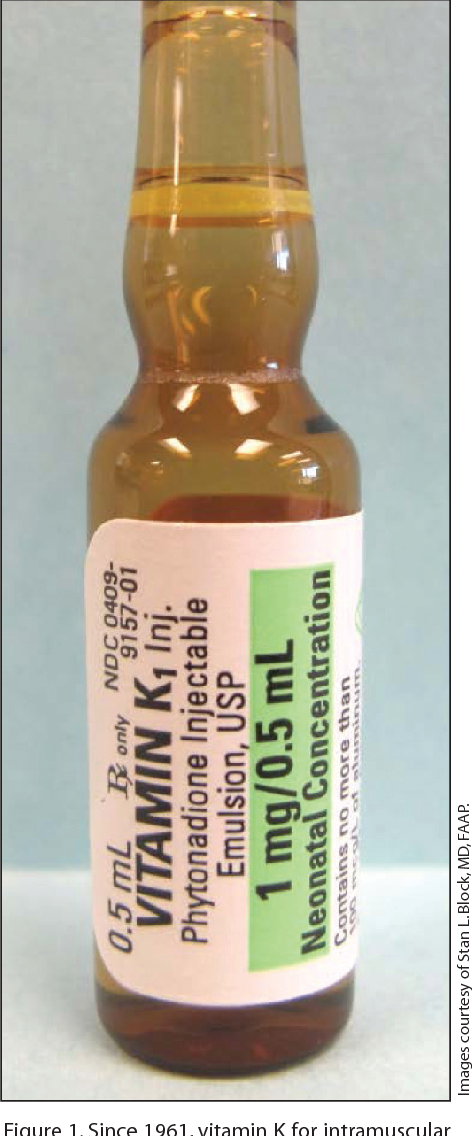 7% of the semi-lethal dose for a newborn (3 mg/kg).
7% of the semi-lethal dose for a newborn (3 mg/kg).
Wikipedia reports that:
1) benzyl alcohol is very toxic to the eyes. Pure benzyl alcohol leads to corneal necrosis.
2) benzyl alcohol is toxic to newborns, it causes gasping syndrome. nine0054 Gasping syndrome is a disease that no longer exists. It was caused by the fact that the skin of newborns until the 1980s was wiped with benzyl alcohol, from which some began to suffocate and die. The dose of benzyl alcohol for the development of this disease is 99 mg/kg.
The fact that benzyl alcohol is toxic has been known since at least the early 1970s. This did not stop it from being used without restriction in preterm infants until the early 80s, when it was proven to be toxic not only to dogs, but to babies as well. But even this did not stop its use in injections that are given on the first day after birth. nine0003
27. Amphastar makes vitamin K without benzyl alcohol. It uses propylene glycol as a preservative. Propylene glycol is also used as an antifreeze and brake fluid, can cause kidney failure, and is a neurotoxin.
28. Amphastar also adds polysorbate 80 to vitamin K. Moreover, it contains 10 mg of polysorbate 80, which is 200 times more than in Gardasil. (Kanavit also contains polysorbate 80.)
Konakion MM does not contain benzyl alcohol, propylene glycol or polysorbate 80.
29. Hospira reports that intravenous vitamin administration can be lethal. Serious consequences and deaths were also observed due to intramuscular injection.
Safety (other)
30. Anaphylactic shock due to vitamin K in a newborn and review of literature. (Koklu, 2014, J Matern Fetal Neonatal Med)
Infants are born with an immature innate immune system. Because their immune systems are weaker than adults, they are less likely to develop an anaphylactic reaction. A possible mechanism for the formation of anaphylaxis in newborns has not yet been elucidated. nine0054 This describes the first case of anaphylactic shock due to an injection of vitamin K. More: [1]
31. Nicolau's syndrome is a gangrenous dermatitis caused by various drugs. An injection of vitamin K can also occasionally cause it.
An injection of vitamin K can also occasionally cause it.
Texier's disease is a pseudo-sclerodermal reaction that rarely occurs after vitamin K injection and lasts for several years.
32. Sometimes, instead of vitamin K, an infant is injected with methylergometrine. It is a psychedelic alkaloid used to prevent bleeding after childbirth. It is confused with vitamin K because they have similar ampoules. Among the babies who received it orally, all survived. And among those who received it by injection, the mortality rate was 7.5%. [1] [2] [3] [4] [5] [6] [7]
Pain
33. Until 1999, it was believed that children begin to experience pain at 12 months of age.
34. Are There Long-Term Consequences of Pain in Newborn or Very Young Infants? (Page, 2004, J Perinat Educ)
For many years, physicians in the US did not consider infant pain as a risk or disadvantage in their treatment decisions. Superficial observations showed that pain medications had some risks, and babies seemed to forget the pain anyway.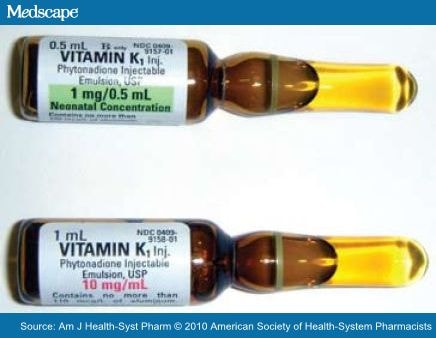 After all, if the patient does not come back with complaints of pain, what can be especially important in it? nine0054 However, research conducted in the 1990s revealed that pain experienced in infancy has long-term consequences. For example, infants who were circumcised without lidocaine ointment suffered more pain during vaccination than those who were circumcised with lidocaine, who in turn suffered more than uncircumcised infants.
After all, if the patient does not come back with complaints of pain, what can be especially important in it? nine0054 However, research conducted in the 1990s revealed that pain experienced in infancy has long-term consequences. For example, infants who were circumcised without lidocaine ointment suffered more pain during vaccination than those who were circumcised with lidocaine, who in turn suffered more than uncircumcised infants.
Newborn rat pups that were separated from their mothers for some time showed suppression of the immune system and were more susceptible to metastases.
In rat pups injected with endotoxin in infancy, an exacerbated stress response, increased susceptibility to metastases, and delayed wound healing were observed in adulthood, indicating a failure to form an inflammatory response. nine0054 Pups that were subjected to pain through paw pricks showed increased pain sensitivity during adolescence. In adulthood, they showed greater anxiety, social hypervigilance, and they observed cravings for alcohol.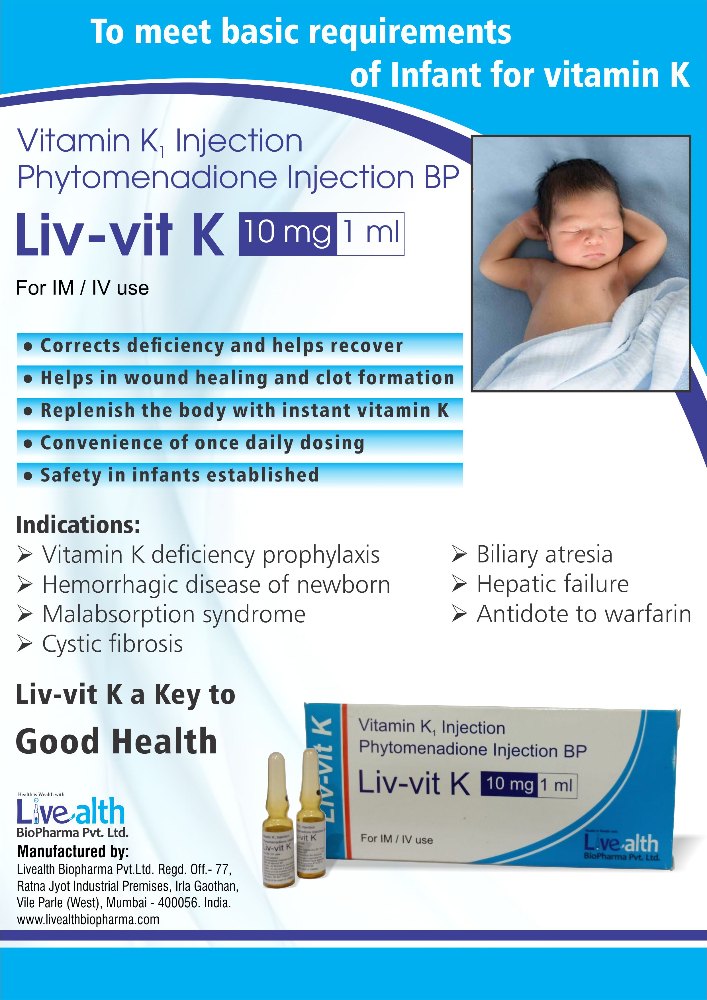
Premature babies (who had much more painful medical procedures than term babies) had reduced pain sensitivity.
Infants with multiple birth trauma had a 4.9 risk of violent suicidetimes higher in men and 4% higher in women. But if the mother received opioids during childbirth, the risk of suicide was 31% lower for both sexes, compared to those born without trauma.The authors conclude that although people do not remember early painful events, they are recorded somewhere in the body. The many medical procedures infants undergo, from heel injections to circumcision, can change a child's development. Children's pain should be avoided whenever possible and, if necessary, treated with the same care as adult pain. Physicians and parents must be aware that pain must be added to the list of risks in order to make decisions about treatment and consent to procedures that an infant is subjected to. This consideration was not part of the traditional decision-making model for most physicians.
 nine0004 35. Iatrogenic pain in newborns as a risk factor for chronic pain syndromes. (Reshetnyak, 2017, Russian Journal of Pain)
nine0004 35. Iatrogenic pain in newborns as a risk factor for chronic pain syndromes. (Reshetnyak, 2017, Russian Journal of Pain) Frequent pain stimuli in newborns, especially premature ones, lead to central sensitization of those areas of the cerebral cortex that make up the leading part of the pain neuromatrix and are responsible for the sensory, affective and cognitive components of pain perception. Central sensitization and dysfunction of the systems that regulate pain sensitivity are known to lead to the formation of chronic pain syndromes. nine0003
Miscellaneous
36. Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: a randomized, controlled trial. (Mercer, 2006, Pediatrics)
If you do not cut the umbilical cord immediately after birth, but wait at least 30-40 seconds, then the risk of intraventricular hemorrhage and sepsis is significantly reduced.
37. Breastmilk, PCBs, dioxins and vitamin K deficiency: discussion paper. (Koppe, 1989, JR Soc Med)
(Koppe, 1989, JR Soc Med)
Late form of hemorrhagic disease of the newborn is a new disease that was described in 1985, and is observed only in children with exclusive breastfeeding. Breast milk in industrialized countries is contaminated with polychlorinated biphenyls (PCBs), polychlorinated dibenzo-p-dioxins (PCDD) and polychlorinated dibenzofurans (PCDF).
Xenobiotics were found in the milk of Dutch mothers, but not in the milk of a recently immigrated woman from Suriname. A woman who immigrated from Suriname 15 years ago also had xenobiotics. nine0054 PCBs, PCDDs and PCDFs are known to cause liver enlargement, increased clotting time, liver cirrhosis, etc. The clinical symptoms of infants whose mothers were poisoned by these substances included stunted growth, smaller head circumference, hirsutism, etc. those who were fed breast milk containing PCBs experienced, among other things, fatigue, anorexia, abdominal pain, vomiting, and eczema. Monkeys have been found to have fatty liver, pancreatic atrophy, and GI hemorrhage after the high dose. Millions of chicks that die from contaminated food experience subepicardial bleeding. Mice have a cleft palate, bleeding, and subcutaneous edema. nine0054 The authors tested the levels of dioxins in the milk of 14 mothers. Mothers of 4 infants who bled had significantly higher levels of dioxin than ten other mothers. The authors consider that there is a likely causal relationship between PCBs, dioxins and furans in breast milk and late hemorrhagic disease. These xenobiotics may also be associated with prolonged neonatal jaundice. More: [1] [2]
Millions of chicks that die from contaminated food experience subepicardial bleeding. Mice have a cleft palate, bleeding, and subcutaneous edema. nine0054 The authors tested the levels of dioxins in the milk of 14 mothers. Mothers of 4 infants who bled had significantly higher levels of dioxin than ten other mothers. The authors consider that there is a likely causal relationship between PCBs, dioxins and furans in breast milk and late hemorrhagic disease. These xenobiotics may also be associated with prolonged neonatal jaundice. More: [1] [2]
38. Reasons for refusal of newborn vitamin K prophylaxis: implications for management and education. (Hamrick, 2016, Hosp Pediatr)
Among the parents who refused a vitamin K injection, the majority were white (78%), over 30 years old (57%), and with an academic education (65%). Most of them also refused hepatitis B vaccination and erythromycin eye ointment. They mostly got their information from the internet and were worried about the synthetic and toxic ingredients, overdose and side effects.