Vitamin d supplement for pregnant
Vitamin D and Pregnancy - American Pregnancy Association
Vitamin D is a steroid vitamin from a group of fat-soluble prohormones. Vitamin D and pregnancy are important together. Expecting mothers need to make sure they get the recommended amounts of vitamin D during pregnancy for both their own well being and the healthy development of their baby. The most significant compounds for human development are D2 and D3.
Vitamin D is beneficial for your own personal health. Vitamin D now has extensive research supporting its role in immune function, healthy cell division, and bone health.
Vitamin D is necessary for the absorption and metabolism of calcium and phosphorus. Many studies are finding a connection between low serum vitamin D levels and an increased risk of certain types of cancers, autoimmune disease, neurological disease, insulin resistance, and cardiovascular disease.
Vitamin D invests in the well-being of your baby by supporting healthy bone development. Deficiency with vitamin D is also related to preeclampsia.
Does my prenatal vitamin have enough vitamin D?
It is unlikely your prenatal vitamin provides enough vitamin D. A recent study found women taking 4,000 IU of vitamin D daily had the greatest benefits in preventing preterm labor/births and infections.
The study confirmed vitamin D at this level is not only safe for you, but for your baby, and the researchers from this study now recommend this daily dosage of vitamin D for all pregnant women. The average prenatal vitamin only contains 400 IU of vitamin D, so additional supplementation should be taken daily.
What contributes to vitamin deficiency?
At this time, 40-60% of the entire U.S. population is vitamin D deficient, including pregnant women. The reasons for this widespread deficiency are many, and to begin to unfold this issue you can start with understanding there is a very short list of foods that contain vitamin D.
These foods are egg yolk, salmon and cod liver oil, however, most vitamin D is consumed through fortified foods like milk. For 75% of the population that is lactose intolerant, fortified milk products are not a reliable source of vitamin D consumption.
Additionally, many factors influence the body’s ability to make and absorb vitamin D. These factors include: where you live, the season, how much time you spend outdoors without sunscreen, skin pigmentation, age, obesity, pollution, and having healthy intestines with optimal absorption capacity. These factors come in to play because Vitamin D is actually a hormone and needs sunlight, in order for the body to manufacture it properly.
At this time, a large part of the U.S. population falls into one, or more, of these categories:
- Obese
- Uses sunscreen
- Is a senior citizen (50+), so it is not surprising that vitamin D deficiencies have risen to such proportions.
What steps can you take to get Vitamin D?
You can begin by making an effort to eat more vitamin D containing foods. Next, research suggests sensible sun exposure (usually 5-10 min of exposure of the arms and legs or the hands, arms, and face, 2 or 3 times per week) can help as well.
Next, research suggests sensible sun exposure (usually 5-10 min of exposure of the arms and legs or the hands, arms, and face, 2 or 3 times per week) can help as well.
However, the best way to really ensure adequate vitamin D is through simple supplementation. When supplementing, your choices will be between two forms of vitamin D. Ergocalciferol is the vegetarian form of vitamin D and cholecalciferol is the animal-sourced form, usually derived from fish liver oil or lanolin from sheep.
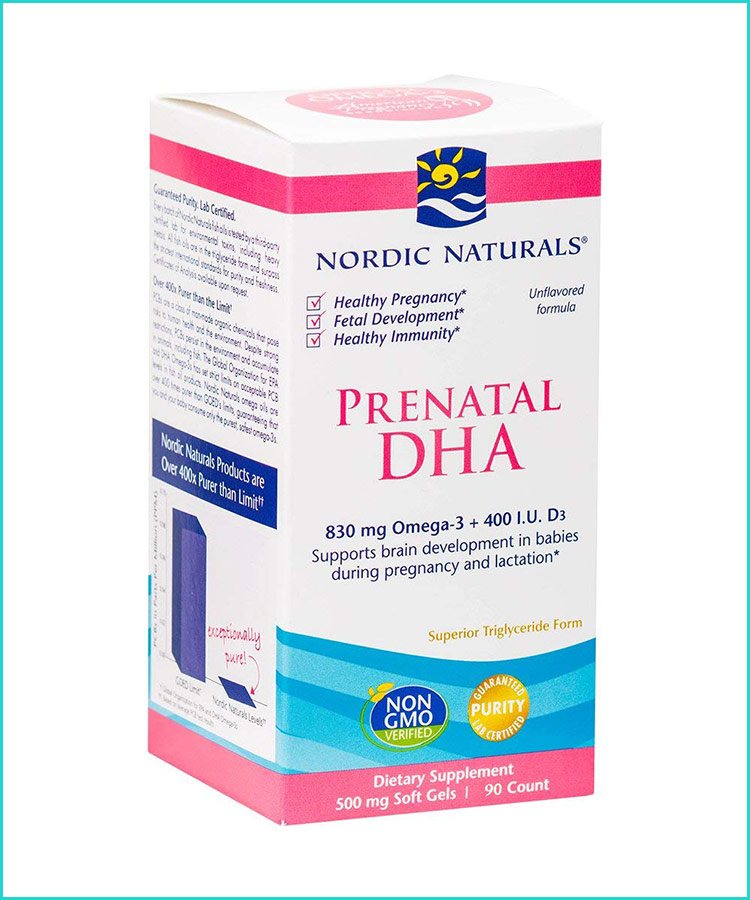
The cholecalciferol form is the most absorbable and utilized form for the body, but if you are vegan you should choose ergocalciferol. Quality is important. We recommend Nordic Naturals Vitamin D3 (1000 IU per soft gel) in the natural form cholecalciferol form.
The carrier oil is organic, extra virgin olive oil and they come in small, soft gels that are very easy to swallow. We also recommend Nordic Naturals Prenatal DHA with added vitamin D3 (400 IU per 2 soft gels). This product provides two of the most important nutrients for pregnant women backed by a long-standing, reliable company that guarantees optimum purity, quality and freshness.
- Pregnancy Nutrition
- Types of Prenatal Vitamins
- Nordic Naturals Prenatal DHA
Compiled using information from the following sources:
1. Vitamin D Supplementation during Pregnancy Part 2 NICHD/CTSA Randomized Clinical Trial (RCT): Outcomes.
2. Carol L. Wagner, Donna Johnson, Thomas C. Hulsey, Myla Ebeling, Judy Shary, Pamela G. Smith, Betty Bivens, Bruce W. Hollis. Pediatrics/Obstetrics, Medical University of SC, Charleston, SC.Maternal Vitamin D and Fetal Growth in Early-Onset Severe Preeclampsia.
3. Christopher Robinson, Carol Wagner, Bruce Hollis, John Baatz, and Donna Johnson. American Journal of Obstetrics and Gynecology 2011 June.
Vitamin D: Screening and Supplementation During Pregnancy
By reading this page you agree to ACOG's Terms and Conditions. Read terms
Number 495 (Reaffirmed 2021)
Committee on Obstetric Practice
This document reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed.
The information should not be construed as dictating an exclusive course of treatment or procedure to be followed.
ABSTRACT: During pregnancy, severe maternal vitamin D deficiency has been associated with biochemical evidence of disordered skeletal homeostasis, congenital rickets, and fractures in the newborn. At this time, there is insufficient evidence to support a recommendation for screening all pregnant women for vitamin D deficiency. For pregnant women thought to be at increased risk of vitamin D deficiency, maternal serum 25-hydroxyvitamin D levels can be considered and should be interpreted in the context of the individual clinical circumstance. When vitamin D deficiency is identified during pregnancy, most experts agree that 1,000–2,000 international units per day of vitamin D is safe. Higher dose regimens used for treatment of vitamin D deficiency have not been studied during pregnancy. Recommendations concerning routine vitamin D supplementation during pregnancy beyond that contained in a prenatal vitamin should await the completion of ongoing randomized clinical trials.
Vitamin D is a fat-soluble vitamin obtained largely from consuming fortified milk or juice, fish oils, and dietary supplements. It also is produced endogenously in the skin with exposure to sunlight. Vitamin D that is ingested or produced in the skin must undergo hydroxylation in the liver to 25-hydroxyvitamin D (25-OH-D), then further hydroxylation primarily in the kidney to the physiologically active 1,25-dihydroxyvitamin D. This active form is essential to promote absorption of calcium from the gut and enables normal bone mineralization and growth. During pregnancy, severe maternal vitamin D deficiency has been associated with biochemical evidence of disordered skeletal homeostasis, congenital rickets, and fractures in the newborn 1 2.
Recent evidence suggests that vitamin D deficiency is common during pregnancy especially among high-risk groups, including vegetarians, women with limited sun exposure (eg, those who live in cold climates, reside in northern latitudes, or wear sun and winter protective clothing) and ethnic minorities, especially those with darker skin 3 4 5.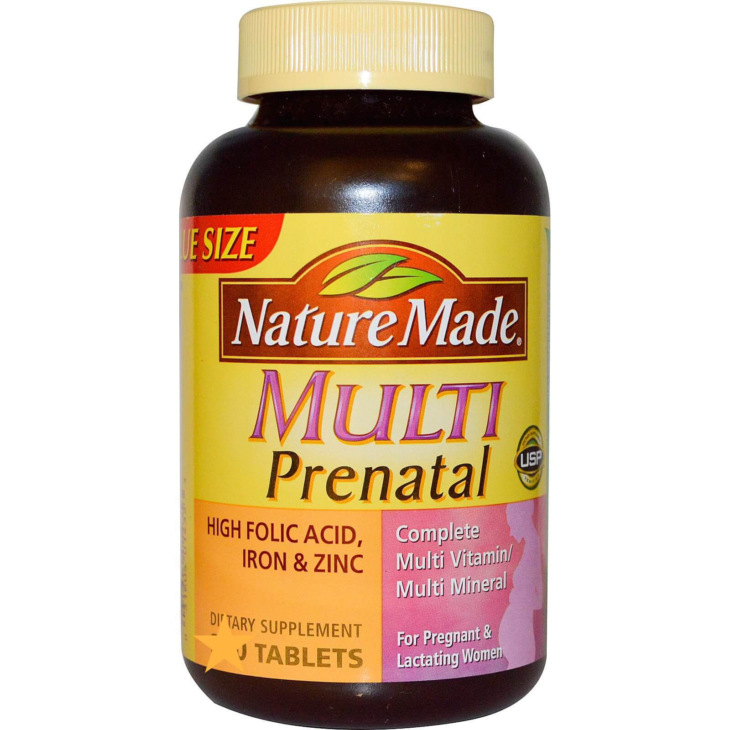 Newborn vitamin D levels are largely dependent on maternal vitamin D status. Consequently, infants of mothers with or at high risk of vitamin D deficiency are also at risk of vitamin D deficiency 5 6.
Newborn vitamin D levels are largely dependent on maternal vitamin D status. Consequently, infants of mothers with or at high risk of vitamin D deficiency are also at risk of vitamin D deficiency 5 6.
For the individual pregnant woman thought to be at increased risk of vitamin D deficiency, the serum concentration of 25-OH-D can be used as an indicator of nutritional vitamin D status. Although there is no consensus on an optimal level to maintain overall health, most agree that a serum level of at least 20 ng/mL (50 nmol/L) is needed to avoid bone problems ref07 8 9 10. Based on observations of biomarkers of vitamin D activity, such as parathyroid hormone, calcium absorption, and bone mineral density, some experts have suggested that vitamin D deficiency should be defined as circulating 25-OH-D levels less than 32 ng/mL (80 nmol/L) 11. An optimal serum level during pregnancy has not been determined and remains an area of active research.
In 2010, the Food and Nutrition Board at the Institute of Medicine of the National Academies established that an adequate intake of vitamin D during pregnancy and lactation was 600 international units per day 12. Most prenatal vitamins typically contain 400 international units of vitamin D per tablet. Summarizing recent observational and interventional studies, the authors of a recent clinical report from the Committee on Nutrition of the American Academy of Pediatrics suggested that a daily intake higher than that recommended by the Food and Nutrition Board may be needed to maintain maternal vitamin D sufficiency 13. Although data on the safety of higher doses are lacking, most experts agree that supplemental vitamin D is safe in dosages up to 4,000 international units per day during pregnancy or lactation 12.
Most prenatal vitamins typically contain 400 international units of vitamin D per tablet. Summarizing recent observational and interventional studies, the authors of a recent clinical report from the Committee on Nutrition of the American Academy of Pediatrics suggested that a daily intake higher than that recommended by the Food and Nutrition Board may be needed to maintain maternal vitamin D sufficiency 13. Although data on the safety of higher doses are lacking, most experts agree that supplemental vitamin D is safe in dosages up to 4,000 international units per day during pregnancy or lactation 12.
At this time there is insufficient evidence to support a recommendation for screening all pregnant women for vitamin D deficiency. For pregnant women thought to be at increased risk of vitamin D deficiency, maternal serum 25-OH-D levels can be considered and should be interpreted in the context of the individual clinical circumstance. When vitamin D deficiency is identified during pregnancy, most experts agree that 1,000–2,000 international units per day of vitamin D is safe. Higher dose regimens used for the treatment of vitamin D deficiency have not been studied during pregnancy. Recommendations concerning routine vitamin D supplementation during pregnancy beyond that contained in a prenatal vitamin should await the completion of ongoing randomized clinical trials. At this time, there is insufficient evidence to recommend vitamin D supplementation for the prevention of preterm birth or preeclampsia.
Higher dose regimens used for the treatment of vitamin D deficiency have not been studied during pregnancy. Recommendations concerning routine vitamin D supplementation during pregnancy beyond that contained in a prenatal vitamin should await the completion of ongoing randomized clinical trials. At this time, there is insufficient evidence to recommend vitamin D supplementation for the prevention of preterm birth or preeclampsia.
- Pawley N, Bishop NJ. Prenatal and infant predictors of bone health: the influence of vitamin D. Am J Clin Nutr 2004;80:1748S–51S.
Article Locations:Article Location
- Gale CR, Robinson SM, Harvey NC, Javaid MK, Jiang B, Martyn CN, et al. Maternal vitamin D status during pregnancy and child outcomes. Princess Anne Hospital Study Group. Eur J Clin Nutr 2008;62:68–77.
Article Locations:Article Location
- Hollis BW, Wagner CL. Assessment of dietary vitamin D requirements during pregnancy and lactation.
 Am J Clin Nutr 2004;79:717–26.
Am J Clin Nutr 2004;79:717–26.
Article Locations:Article Location
- Lee JM, Smith JR, Philipp BL, Chen TC, Mathieu J, Holick MF. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin Pediatr (Phila) 2007;46:42–4.
Article Locations:Article Location
- Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM. High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J Nutr 2007;137:447–52.
Article Locations:Article LocationArticle Location
- Dijkstra SH, van Beek A, Janssen JW, de Vleeschouwer LH, Huysman WA, van den Akker EL. High prevalence of vitamin D deficiency in newborn infants of high-risk mothers [published erratum appears in Arch Dis Child 2007;92:1049]. Arch Dis Child 2007;92:750–3.
Article Locations:Article Location
- Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266–81.
- Bouillon R, Norman AW, Lips P.
 Vitamin D deficiency. N Engl J Med 2007;357:1980–1; author reply 1981–2.
Vitamin D deficiency. N Engl J Med 2007;357:1980–1; author reply 1981–2.
Article Locations:Article Location
- Vitamin D supplementation: Recommendations for Canadian mothers and infants. Paediatr Child Health 2007;12:583–98.
Article Locations:Article Location
- National Institutes of Health, Office of Dietary Supplements. Vitamin D. Available at: http://ods.od.nih.gov/factsheets/list-all/VitaminD. Retrieved December 16, 2010.
Article Locations:Article Location
- Hollis BW, Wagner CL. Normal serum vitamin D levels. N Engl J Med 2005;352:515–6; author reply 515–6.
Article Locations:Article Location
- Institute of Medicine of the National Academies (US). Dietary reference intakes for calcium and vitamin D . Washington, DC: National Academy Press; 2010.
Article Locations:Article LocationArticle Location
- Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents.
 American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee on Nutrition [published erratum appears in Pediatrics 2009;123:197]. Pediatrics 2008;122:1142–52.
American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee on Nutrition [published erratum appears in Pediatrics 2009;123:197]. Pediatrics 2008;122:1142–52.
Article Locations:Article Location
Copyright July 2011 by the American College of Obstetricians and Gynecologists, 409 12th Street, SW, PO Box 96920, Washington, DC 20090-6920. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, posted on the Internet, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission from the publisher. Requests for authorization to make photocopies should be directed to: Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923, (978) 750-8400.
ISSN 1074-861X
Vitamin D: screening and supplementation during pregnancy. Committee Opinion No. 495. American College of Obstetricians and Gynecologists. Obstet Gynecol 2011;118:197–8.
Obstet Gynecol 2011;118:197–8.
Topics
Delivery of health care Dietary supplements Health personnel Mass screening Pregnancy Pregnancy complications Vitamins
the effect of hypovitaminosis on the intelligence of a child
Vitamin D plays a special role in a woman's fertility. The influence of vitamin D on the regulation of the menstrual cycle, namely its participation in the maturation of follicles, ovulation and the formation of the corpus luteum 1 was shown. Therefore, maintaining normal levels of Vitamin D is important at all stages: preparation for pregnancy, pregnancy and lactation.
Vitamin D in pregnancy
During pregnancy, vitamin D deficiency is associated with the risk of developing preeclampsia (preeclampsia is defined as a multisystem pathological condition that occurs after the 20th week of pregnancy, characterized by arterial hypertension in combination with proteinuria (0. 3 g / l in daily urine), often, edema, and manifestations of multiple organ failure), diabetes mellitus in pregnancy, premature birth, the birth of small children, as well as the development of skeletal disorders in them due to rickets. Vitamin D deficiency is associated with an increased risk of cardiovascular disease, diabetes, cancer 2
3 g / l in daily urine), often, edema, and manifestations of multiple organ failure), diabetes mellitus in pregnancy, premature birth, the birth of small children, as well as the development of skeletal disorders in them due to rickets. Vitamin D deficiency is associated with an increased risk of cardiovascular disease, diabetes, cancer 2
Vitamin D during breastfeeding
During lactation, the mother loses vitamin D and other substances in breast milk, taking even small doses of vitamin D before and after childbirth can have a beneficial effect on the provision of vitamin D to mother and baby 3 .
How much vitamin D should pregnant women take?
Since Russia belongs to an endemic region for vitamin D deficiency, it is advisable for all women preparing to conceive to receive vitamin D in prophylactic doses. In order to prevent vitamin D deficiency, women aged 18-50 years are recommended to take at least 600-800 IU of vitamin D per day, when pregnancy occurs, the dose is increased to 800-1200 IU / day 2 . The decision on the need to take vitamin D and its dosing regimen is made by a specialist based on clinical examination data and laboratory diagnostics. Hypovitaminosis D requires mandatory correction 2 .
The decision on the need to take vitamin D and its dosing regimen is made by a specialist based on clinical examination data and laboratory diagnostics. Hypovitaminosis D requires mandatory correction 2 .
What foods contain vitamin D?
Dietary sources of vitamin D are fatty fish, liver, egg yolk, some cereals, vitamin D is also synthesized in the body when the skin is exposed to ultraviolet sunlight. For the synthesis of vitamin D in physiological quantities, it is necessary to expose the extremities to sunlight (from 10.00 am to 15.00 pm) at least 2 times a week, according to the recommendations of the US National Institutes of Health 2 .
Insufficient intake of vitamin D from food can be compensated by the intake of the vitamin as part of dietary supplements or vitamin-mineral complexes. 4
References:
- Yazykova OI, Khilkevich EG Pregnancy planning. Vitamin D deficiency – infertility, correction of vitamin D deficiency // Medical Council.
 – 2017. – no. 2.
– 2017. – no. 2. - Pregravid preparation: clinical protocol / [ed.-dev. V.E. Radzinsky and others]. - M .: Editorial staff of the Status Praesens magazine, 2016. - 80 from
- McDermott C.M., Beitz D.C., Littledike E.T., Horst R.L. Effects of dietary vitamin D3 on concentrations of vitamin D and its metabolites in blood plasma and milk of dairy cows. J Dairy Sci. 1985; 68:1959–67
- National program "Vitamin D deficiency in children and adolescents of the Russian Federation: modern approaches to correction", 2018
The effect of vitamin D on pregnancy and the health of newborns and young children: a modern view of the problem | Zakharova I.N., Maltsev S.V., Zubkov V.V., Kuryaninova V.A., Dmitriev A.V., Maltseva L.I., Verisokina N.E., Klimov L.Ya., Vasilyeva E. .N., Malyavskaya S.I., Zaplatnikov A.L.
Introduction
Currently, there is more and more data on the pleiotropic effect of vitamin D, including those related to its effect on the body of a pregnant woman and the fetus. At the same time, it was found that a sufficient level of vitamin D is necessary throughout pregnancy, starting from the moment of implantation and the formation of the placenta. Vitamin D plays an important role in the adequate functioning of the mother-placenta-fetus system, and also has a positive effect on embryogenesis, the course of intra- and postnatal periods [1].
At the same time, it was found that a sufficient level of vitamin D is necessary throughout pregnancy, starting from the moment of implantation and the formation of the placenta. Vitamin D plays an important role in the adequate functioning of the mother-placenta-fetus system, and also has a positive effect on embryogenesis, the course of intra- and postnatal periods [1].
Calcidiol (25(OH)D 3 ) takes part in the development and formation of the child's place - the placenta. The placenta begins to form on the 4th week. pregnancy. Since that time, vitamin D of a pregnant woman penetrates into the fetus and largely determines the development of the bone and immune systems, and then other organs and systems. The concentration of calcitriol (1.25 (OH) 2 D 3 ) by 12 weeks. pregnancy increases by 2-3 times, which is associated with an increase in the production of a metabolite in the kidneys of a pregnant woman, as well as in the trophoblast, decidual tissue and placenta. In the decidual tissue and the outer cell layer of the blastocyst, when gene 9 is expressed0063 CYP27B1 (encodes 1α-hydroxylase) 1,25(OH) 2 D 3 is formed, the maximum production of which was noted in the I–II trimesters of pregnancy [2, 3].
In the decidual tissue and the outer cell layer of the blastocyst, when gene 9 is expressed0063 CYP27B1 (encodes 1α-hydroxylase) 1,25(OH) 2 D 3 is formed, the maximum production of which was noted in the I–II trimesters of pregnancy [2, 3].
Historically, the placenta was one of the first extrarenal tissues capable of synthesizing 1,25(OH) 2 D 3 [4], but only calcidiol (25(OH)D 3 ) passes through the placental barrier and provides the need for the fetus [ 2]. In early pregnancy, vitamin D stimulates gene expression HOXA10 and HOXA11 , which provides decidual transformations of the endometrium, control of the mother's immune response (regulation of the ratio of cytokines), stimulates the hormonal function of the placenta and provides the antimicrobial effect of the trophoblast and placenta.
During pregnancy, vitamin D receptors (VDRs) and enzymes that regulate metabolism are expressed in the placenta and decidual tissue of the uterus, indicating a critically active point of immunomodulation at the mother-fetus interface. The level of vitamin D-binding protein in the blood increases during pregnancy from 46% to 103% [5].
The level of vitamin D-binding protein in the blood increases during pregnancy from 46% to 103% [5].
The role of vitamin D as a potential modulator of immune responses during pregnancy was first reported over 50 years ago, but the specific mechanisms for fulfilling this role have only recently received due attention [6]. Already in the first weeks of pregnancy, the trophoblast simultaneously synthesizes and responds to the action of vitamin D, which locally implements an anti-inflammatory function and simultaneously stimulates the growth of decidual tissue necessary for normal pregnancy [7].
In the body of the fetus, 25(OH)D 3 is converted into the active form - 1.25(OH) 2 D 3 , which, interacting with VDR in organs and tissues, implements the classic effects of vitamin D (Fig. 1) [9].
Vitamin D receptors (VDRs) are found in most cells of the body, and many tissues contain the enzyme 1α-hydroxylase, which is necessary for the synthesis of the active form of the D-hormone — 1,25(OH) 2 D 3 [4]. There is evidence that 1,25(OH) 2 D 3 coordinates the transcription and function of genes associated with trophoblast invasion, implantation, and angiogenesis [10]. The level of 1,25(OH) 2 D 3 in the fetus and cord blood is lower than in adults and significantly lower than in the mother's blood. During the first day of life, in response to a decrease in calcium levels and an increase in the concentration of parathyroid hormone in the blood of newborns, the synthesis of 1,25(OH) 2 D 3 9 is activated0058, which is apparently associated with the need to activate calcium absorption in the intestine immediately after birth [11].
There is evidence that 1,25(OH) 2 D 3 coordinates the transcription and function of genes associated with trophoblast invasion, implantation, and angiogenesis [10]. The level of 1,25(OH) 2 D 3 in the fetus and cord blood is lower than in adults and significantly lower than in the mother's blood. During the first day of life, in response to a decrease in calcium levels and an increase in the concentration of parathyroid hormone in the blood of newborns, the synthesis of 1,25(OH) 2 D 3 9 is activated0058, which is apparently associated with the need to activate calcium absorption in the intestine immediately after birth [11].
Vitamin D and pregnancy
Pregnancy is a risk factor for the development of 25(OH)D deficiency 3 . Thus, the incidence of vitamin D deficiency varies widely, reaching, for example, 98% in women from the United Arab Emirates (Fig. 2) [1, 12].
Vitamin D deficiency in pregnant women and their newborns is extremely high in Arab countries: almost 85% of pregnant women and 88% of their newborns have vitamin D deficiency or insufficiency [14]. In a number of European studies, the optimal concentration of vitamin D (>30 ng / ml) was noted only in 10.6% of pregnant women, vitamin D deficiency was found in 10% in a multinational cohort of patients in Sweden, in 35% in the UK, in 50% in Germany [15].
In a number of European studies, the optimal concentration of vitamin D (>30 ng / ml) was noted only in 10.6% of pregnant women, vitamin D deficiency was found in 10% in a multinational cohort of patients in Sweden, in 35% in the UK, in 50% in Germany [15].
Numerous studies indicate that vitamin D levels less than 50 nmol/l (<20 ng/ml) are associated with a number of complications during pregnancy - the threat of preterm birth, the development of placental insufficiency, abortion, preeclampsia, the formation of gestational diabetes mellitus, bacterial vaginosis , increased risk of violation of the contractile activity of the uterus, an increase in the frequency of operative delivery [16].
To eliminate the risk of complications associated with 25(OH)D deficiency 3 , pregnant women are advised to maintain calcidiol levels >75 nmol/l (>30 ng/ml), but sufficient conversion of vitamin D to 1.25(OH) 2 D 3 is achieved at a level of 25(OH)D 3 >100 nmol/l (>40 ng/ml) [3]. Women with optimal vitamin D levels (≥75 nmol/L, or ≥30 ng/mL) have a significantly higher live birth rate [10].
Women with optimal vitamin D levels (≥75 nmol/L, or ≥30 ng/mL) have a significantly higher live birth rate [10].
The association between low levels of 25(OH)D 3 in a pregnant woman and an increased risk of developing gestational diabetes has been proven. The influence of calcidiol on glucose homeostasis was determined, including the presence of specific VDRs on pancreatic β-cells and skeletal muscles, the expression of 1α-hydroxylase in pancreatic β-cells, which catalyzes the conversion of 25(OH)D 3 to 1.25(OH) 2 D 3 [17]. In women with vitamin D deficiency in the second trimester, the risk of developing gestational diabetes is 4.46 times higher than in women without deficiency (odds ratio 4.46, 95% confidence interval 1.15–17.3) [18]. In a study by C. Zhang et al. [19] not only found a relationship between a decrease in the level of calcidiol <50 nmol/l (<20 ng/ml) and the development of diabetes in pregnant women, but also found that as the level of 25(OH)D 3 decreased for every 12, 5 nmol / l (5 ng / ml) increases the risk of developing gestational diabetes mellitus by 1.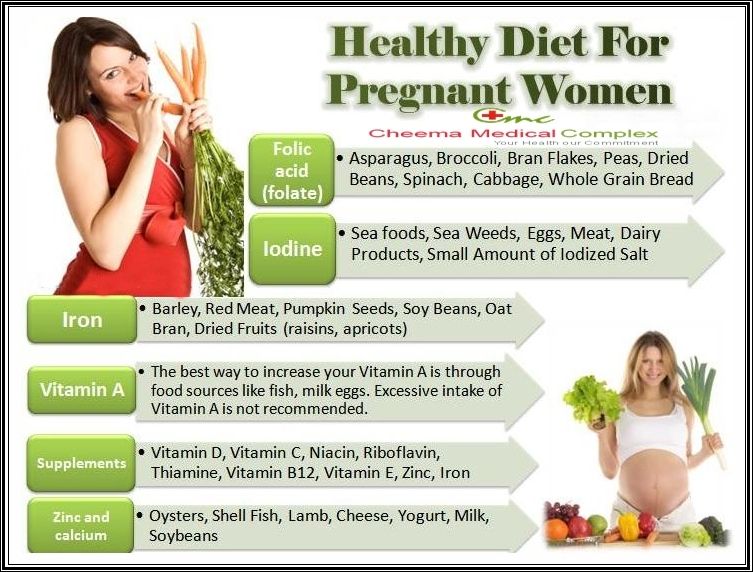 29 times.
29 times.
Large cohort studies in Ireland and Denmark have shown that low serum vitamin D levels are associated with a high incidence of eclampsia. This led the authors to suggest that sufficient levels of vitamin D provide a physiological interface between the fetus, placenta, and uterus. From the earliest stages of implantation of the trophoblast (the outer layer of the fertilized egg) into the uterine lining, vitamin D is believed to optimize blood vessel development, allowing more efficient nutrient transfer to the fetus and lower rates of pregnancy-induced hypertension or eclampsia. Vitamin D deficiency in early pregnancy is associated with a fivefold increase in the risk of preeclampsia, the pathogenesis of which is based on placental and endothelial dysfunction and a pronounced inflammatory response that disrupts the metabolism between the mother's body and the fetus. It has been suggested that sufficient levels of vitamin D in placental tissues are more important for pregnancy outcomes than serum levels. At the same time, it was shown that the second hydroxylation of vitamin D can occur in the placenta with the formation of 1,25(OH) 2 D 3 in the same way as it happens in the kidneys. The results of studies conducted over the past 15 years (more than 10 thousand observations) have shown that in women who want to become pregnant, as well as in women from the earliest period of pregnancy, the concentration of 25(OH)D 3 should be maintained at a level of at least 100 nmol / l (40 ng/ml). This reduces the risk of preeclampsia, preterm birth and asthma in offspring. This requires taking vitamin D at a dose of at least 4000 IU / day. It was shown that in this case the content of 25(OH)D 3 in the blood of a pregnant woman reaches a level of at least 100 nmol / l (40 ng / ml), which ensures the optimal content of vitamin D in a newborn. These doses have proven safe in thousands of patients. This dose of vitamin D becomes an alternative to direct exposure to sunlight, since daily intake of 4000 IU of vitamin D gives a result comparable to the concentration of 25(OH)D 3 in pregnant women living in sunny regions and receiving vitamin D under sunlight [20– 22].
At the same time, it was shown that the second hydroxylation of vitamin D can occur in the placenta with the formation of 1,25(OH) 2 D 3 in the same way as it happens in the kidneys. The results of studies conducted over the past 15 years (more than 10 thousand observations) have shown that in women who want to become pregnant, as well as in women from the earliest period of pregnancy, the concentration of 25(OH)D 3 should be maintained at a level of at least 100 nmol / l (40 ng/ml). This reduces the risk of preeclampsia, preterm birth and asthma in offspring. This requires taking vitamin D at a dose of at least 4000 IU / day. It was shown that in this case the content of 25(OH)D 3 in the blood of a pregnant woman reaches a level of at least 100 nmol / l (40 ng / ml), which ensures the optimal content of vitamin D in a newborn. These doses have proven safe in thousands of patients. This dose of vitamin D becomes an alternative to direct exposure to sunlight, since daily intake of 4000 IU of vitamin D gives a result comparable to the concentration of 25(OH)D 3 in pregnant women living in sunny regions and receiving vitamin D under sunlight [20– 22].
The relationship between mode and timing of delivery and maternal vitamin D status is also of interest. Several studies that have assessed 25(OH)D 3 levels during early pregnancy (12 weeks) or at delivery have reported an increased risk of caesarean section in women. deficient in 25(OH)D 3 . When comparing obstetric outcomes in pregnant women receiving 4000 and 400 IU daily of vitamin D, it turned out that the frequency of delivery by caesarean section was lower among women with high vitamin D [23].
The effect of vitamin D on the fetus and early child development
Since the fetus undergoes physiological changes during pregnancy associated with rapid growth, vitamin D and its metabolites influence the realization of the genetic characteristics of the developing fetus and minimize the risk of adverse pregnancy outcomes. At the same time, it was found that vitamin D deficiency in pregnant women is not only associated with an increased risk of preterm birth, high rates of neonatal morbidity and mortality, but also adversely affects the postnatal development of children, especially when the level of vitamin D in the mother's blood serum is less than 50 nmol/l ( <20 ng/ml) [24].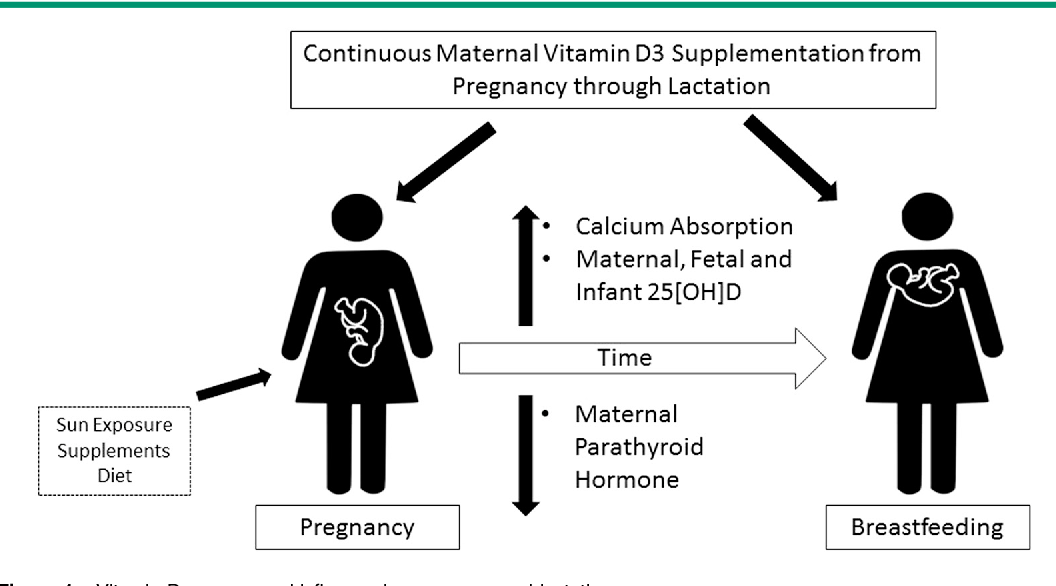 Thus, it was found that the administration of vitamin D to pregnant women at a dose of 2400 IU/day significantly improved bone mineralization in preschool children compared to those whose mothers received standard supplements (400 IU/day).
Thus, it was found that the administration of vitamin D to pregnant women at a dose of 2400 IU/day significantly improved bone mineralization in preschool children compared to those whose mothers received standard supplements (400 IU/day).
In a study performed in Russia, a comparative assessment of the condition of newborns from women at high risk of preeclampsia (kidney disease, hypertensive conditions, antiphospholipid syndrome, obesity) with pregravid preparation with vitamin D at a dose of 4000 IU/day and those who did not receive vitamin D was carried out (Table 1). ) [25]. It was shown that in newborns from women who received 4000 IU/day of vitamin D, the level of 25(OH)D 3 was 2.2 times higher (28.3±1.5 ng/ml versus 12.4±1, 1 ng/ml, respectively, p<0.05), and the frequency of clinical syndromes is significantly lower than in the control group.
A connection was established between the height and body weight of children at 1.5 years of age and the provision of vitamin D at birth, as well as the indicators of the physical development of children at the age of 9 with the content of vitamin D in the mother's blood [26]. At a concentration of 25(OH)D 3 in the blood below 25 nmol/l (<10 ng/ml), a newborn may show radiological signs of osteopenia [9].
At a concentration of 25(OH)D 3 in the blood below 25 nmol/l (<10 ng/ml), a newborn may show radiological signs of osteopenia [9].
Insufficient intake of calcidiol in the fetal body can lead to metabolic changes, prematurity, delayed formation of brain structures, physical development, hypocalcemic seizures, hyperbilirubinemia, an increase in the incidence of necrotizing enterocolitis and bronchopulmonary dysplasia, as well as increase the risk of lower respiratory tract infections and sepsis [25-33 ]. At the same time, in recent years, more and more studies are related to the study of the role of vitamin D deficiency in the development of infections in children and newborns [30]. It has been established that one of the properties of calcidiol is its ability to stimulate the formation of antimicrobial peptides (β 2 -defensins and cathelicidins), which have a pronounced bactericidal activity [34]. Thus, vitamin D deficiency is a significant factor in reducing the level of antimicrobial peptides, which is accompanied by an increased risk of sepsis in newborns. The noted significant effect of vitamin D deficiency on the increase in the incidence of neonatal sepsis was observed in a series of controlled studies conducted in various regions [31, 32].
The noted significant effect of vitamin D deficiency on the increase in the incidence of neonatal sepsis was observed in a series of controlled studies conducted in various regions [31, 32].
Given the high basal expression CYP27B1 and VDR in placental trophoblastic cells suggest that the anti-inflammatory effects of vitamin D may be particularly important in this organ [2]. Vitamin D metabolites determine the formation of surfactant and the development of lung tissue. Deficiency of vitamin D and its metabolites increases the need for oxygenation in newborns, especially premature ones, and is considered as a risk factor for the development of respiratory distress syndrome and respiratory tract infections [28, 29].
By now, the impact of vitamin D deficiency on the development of the central nervous system is well known. It has been proven that with a deficiency of 25 (OH) 2 D in the antenatal and early postnatal periods, delayed speech development, fainting, epilepsy, and a number of demyelinating diseases may occur. In addition, it was shown that preschool children with attention deficit hyperactivity disorder at birth had low levels of 25(OH)D 3 in cord blood compared with newborns without this pathology [26, 35].
In addition, it was shown that preschool children with attention deficit hyperactivity disorder at birth had low levels of 25(OH)D 3 in cord blood compared with newborns without this pathology [26, 35].
The level of 25(OH)D 3 in the umbilical cord blood of a child is 50-80% of its level in the mother's blood serum (p=0.001), regardless of the gestational age. And since the deficiency of 25(OH)D 3 is widely distributed among pregnant women, which explains the large number of newborns with vitamin D deficiency. children is vitamin D supplementation during pregnancy [36–38].
Median blood levels of vitamin D in infants in the first week of life do not reach 15 ng/mL, and the majority (85% of newborns) have vitamin D metabolite levels below 20 ng/mL and even 10 ng/mL. More pronounced vitamin D deficiency is detected in very preterm infants in the winter season compared with the summer period (8.1 [3.3–14.5] ng/mL versus 17.9[4.5–29. 3] ng/mL, p<0.05) [39]. However, even in the south of the Russian Federation, the level of 25(OH)D 3 in the blood serum of newborns is 9.9 ± 0.7 ng / ml (in full-term newborns - 9.2 ± 0.8 ng / ml, in preterm infants - 10, 7±1.1 ng/ml) [40].
3] ng/mL, p<0.05) [39]. However, even in the south of the Russian Federation, the level of 25(OH)D 3 in the blood serum of newborns is 9.9 ± 0.7 ng / ml (in full-term newborns - 9.2 ± 0.8 ng / ml, in preterm infants - 10, 7±1.1 ng/ml) [40].
Correction of hypovitaminosis D
Doses of vitamin D recommended during pregnancy are 800–1200 IU/day. However, in most pregnant women, this dose does not provide a sufficient level of 25(OH)D 3 . Increasing the dose to 2000 IU/day provides optimal levels of vitamin D in the blood for most women. For some complications of pregnancy (preeclampsia, placental insufficiency, gestational diabetes mellitus), the optimal and safe dose is 4000 IU/day throughout pregnancy [38].
Practical recommendations for the correction of hypovitaminosis D in the postnatal period currently take into account not only the effect of vitamin D on the musculoskeletal system, but also a wide range of biological effects on other organs and systems of the child's body. In this regard, various options for the prophylactic intake of vitamin D in children are discussed. Thus, it was found that with daily intake of vitamin D at a dose of 400 IU / day, the level of 25 (OH) D 3 in blood serum reaches 20 ng / ml (50 nmol / l), and this is enough to prevent rickets and osteomalacia in children . Serum concentration of 25(OH)D 9 is required to ensure pleiotropic action.0057 3 in the range of 30–50 ng/ml (75–125 nmol/l), which is achieved only with a daily intake of a higher dose of vitamin D, up to 2000 IU/day [41].
In this regard, various options for the prophylactic intake of vitamin D in children are discussed. Thus, it was found that with daily intake of vitamin D at a dose of 400 IU / day, the level of 25 (OH) D 3 in blood serum reaches 20 ng / ml (50 nmol / l), and this is enough to prevent rickets and osteomalacia in children . Serum concentration of 25(OH)D 9 is required to ensure pleiotropic action.0057 3 in the range of 30–50 ng/ml (75–125 nmol/l), which is achieved only with a daily intake of a higher dose of vitamin D, up to 2000 IU/day [41].
According to European recommendations, the daily vitamin D supplementation after birth should be 400 IU, regardless of the type of feeding. In the second half of the year, the dose increases to 600 IU / day, taking into account the intake of vitamin D from food. At the same time, it is considered that the dose up to 1000 IU / day is safe. Preterm infants are given 400-800 IU/day until 40 weeks post-conceptual age, and then switched to doses recommended for full-term infants [37, 42]. ESPGHAN recommends 800–1000 IU/day of vitamin D in preterm infants. It has been shown that a daily dose of 800 IU in preterm infants increases vitamin D concentration significantly faster over 4 weeks than a dose of 400 IU [42, 43].
ESPGHAN recommends 800–1000 IU/day of vitamin D in preterm infants. It has been shown that a daily dose of 800 IU in preterm infants increases vitamin D concentration significantly faster over 4 weeks than a dose of 400 IU [42, 43].
In the southern regions of Europe, regardless of the type of feeding, vitamin D is prescribed from birth at a dose of 400 IU / day throughout the first year of life. At the same time, in certain groups of children (black, with pathology of internal organs, with malabsorption), the dose is increased to 1000 IU/day [44]. The same authors recommend prescribing 200–400 IU/day of vitamin D to preterm infants from the first days of life (taking into account intake with parenteral nutrition, fortifiers, formula for preterm infants). Upon reaching the volume of enteral nutrition of 100 ml / kg and body weight of 1500 g, the dose of vitamin D is increased to 400-800 IU / day.
In turn, in the United States, newborns with very low birth weight are recommended to start prophylactic vitamin D intake with a dose of 200-400 IU / day. With a body weight of more than 1500 g and complete enteral nutrition, the dose is increased to 400 IU / day (maximum up to 1000 IU / day) [45]. At the same time, in premature babies, the recommended doses do not always allow reaching a sufficient level of calcidiol in the blood. At the initial low level of 25(OH)D 3 even after 1 month. taking vitamin D at a dose of 800 IU/day, only in 1/4 of cases, the content of calcidiol exceeded 30 ng/ml [46]. A multicentre European six-year study showed the low efficacy of standard doses of vitamin D in older children [47].
With a body weight of more than 1500 g and complete enteral nutrition, the dose is increased to 400 IU / day (maximum up to 1000 IU / day) [45]. At the same time, in premature babies, the recommended doses do not always allow reaching a sufficient level of calcidiol in the blood. At the initial low level of 25(OH)D 3 even after 1 month. taking vitamin D at a dose of 800 IU/day, only in 1/4 of cases, the content of calcidiol exceeded 30 ng/ml [46]. A multicentre European six-year study showed the low efficacy of standard doses of vitamin D in older children [47].
In accordance with the foregoing, the appearance on the Russian pharmaceutical market of a new form of vitamin D release in the form of dietary supplement Detrimax® Baby is of particular interest. Detrimax ® Baby is a pure oil solution containing 200 IU of cholecalciferol per drop and can be used in children from birth [48]. The bottle is provided with a special pump dispenser, which allows you to very accurately titrate the required dose, which is especially important for meeting the daily requirement for vitamin D in small and premature babies. At the same time, it should be especially noted that the appearance of cholecalciferol with a dose of 200 IU in 1 drop in the arsenal of neonatologists makes it possible to adequately select an individual dose of vitamin D for small, premature and full-term newborns.
At the same time, it should be especially noted that the appearance of cholecalciferol with a dose of 200 IU in 1 drop in the arsenal of neonatologists makes it possible to adequately select an individual dose of vitamin D for small, premature and full-term newborns.
Conclusion
Thus, vitamin D deficiency is a public health problem worldwide. Due to the multifaceted regulatory effect (on immunity, on biochemical and cellular processes), vitamin D is an extremely significant factor determining the favorable course of pregnancy, as well as adequate intrauterine and postnatal development of the child. In this regard, the prevention of insufficient supply of vitamin D in pregnant and newborn children should become an obligatory component in the preventive work not only of pediatricians and neonatologists, but also of obstetricians and gynecologists.
Gratitude
The editors would like to thank Unipharm for their assistance in ensuring interaction between the authors of this publication.
Acknowledgment
The Editorial Board is grateful to Unipharm for the assistance in cooperation between the authors of this publication.
Information about the authors:
Zakharova Irina Nikolaevna — Doctor of Medical Sciences, Professor, Head of the Department of Pediatrics. Academician G.N. Speransky, FGBOU DPO RMANPO of the Ministry of Health of Russia, 125993, Russia, Moscow, st. Barrikadnaya, 2/1, building 1, ORCID iD 0000-0003-4200-4598.
Maltsev Stanislav Viktorovich - Doctor of Medical Sciences, Professor of the Department of Pediatrics. Academician G.N. Speransky, FGBOU DPO RMANPO of the Ministry of Health of Russia, 125993, Russia, Moscow, st. Barrikadnaya, 2/1, building 1, ORCID iD 0000-0002-6203-2134.
Zubkov Viktor Vasilyevich — Doctor of Medical Sciences, Professor, Director of the Institute of Neonatology and Pediatrics, FSBI “N.N. IN AND. Kulakov" of the Ministry of Health of Russia, 117997, Russia, Moscow, st. Academician Oparina, 4, ORCID iD 0000-0001-8366-5208.
Academician Oparina, 4, ORCID iD 0000-0001-8366-5208.
Kuryaninova Viktoria Aleksandrovna — Candidate of Medical Sciences, Associate Professor of the Department of Propaedeutics of Children's Diseases, StSMU, 355017, Russia, Stavropol, st. Mira, 310, ORCID iD 0000-0002-0731-7153.
Dmitriev Andrey Vladimirovich — Doctor of Medical Sciences, Associate Professor, Head of the Department of Children's Diseases with a Course of Hospital Pediatrics, Ryazan State Medical University of the Ministry of Health of Russia, 3, Russia, Ryazan, st. Vysokovoltnaya, 9; Professor of the Department of Neonatology named after prof. V.V. Gavryushov, FGBOU DPO RMANPO of the Ministry of Health of Russia, 125993, Russia, Moscow, st. Barrikadnaya, 2/1, building 1, ORCID iD 0000-0002-8202-3876.
Maltseva Larisa Ivanovna — Doctor of Medical Sciences, Professor of the Department of Obstetrics and Gynecology, KSMA — branch of FGBOU DPO RMANPO, 420012, Russia, Kazan, st. Butlerova, 36, ORCID iD 0000-0003-0999-4374.
Butlerova, 36, ORCID iD 0000-0003-0999-4374.
Verisokina Natalya Evgenievna — Assistant of the Department of Faculty Pediatrics, StGMU of the Ministry of Health of Russia, 355017, Russia, Stavropol, st. Mira, 310, ORCID iD 0000-0001-5444-8351.
Klimov Leonid Yakovlevich — Doctor of Medical Sciences, Associate Professor, Dean of the Faculty of Pediatrics, StGMU of the Ministry of Health of Russia, 355017, Russia, Stavropol, st. Mira, 310, ORCID iD 0000-0001-7248-1614.
Vasilyeva Elvira Nikolaevna — Candidate of Medical Sciences, Associate Professor, Associate Professor of the Department of Obstetrics and Gynecology I.N. Ulyanova, 428015, Russia, Cheboksary, Moskovsky prospect, 15, ORCID iD 0000-0002-7677-7735.
Malyavskaya Svetlana Ivanovna — Doctor of Medical Sciences, Professor, Head of the Department of Pediatrics, SSMU (Arkhangelsk) of the Ministry of Health of Russia, 163000, Russia, Arkhangelsk, Prospect Troitsky, 51, ORCID iD 0000-0003- 2521-0824.
Andrey Leonidovich Zaplatnikov — Doctor of Medical Sciences, Professor, Head of the Department of Neonatology. prof. V.V. Gavryushova, Professor of the Department of Pediatrics. Academician G.N. Speransky, Vice-Rector for Academic Affairs, FGBOU DPO RMANPE of the Ministry of Health of Russia, 125993, Russia, Moscow, st. Barrikadnaya, 2/1, building 1, ORCID iD 0000-0003-1303-8318.
Contact information: Andrey Leonidovich Zaplatnikov, e-mail: [email protected]. Transparency of financial activities: none of the authors has a financial interest in the presented materials or methods. There is no conflict of interest. Article received on 08/18/2020, received after review on 09/01/2020, accepted for publication on 09/15/2020.
About the authors:
Irina N. Zakharova - Doct. of Sci. (Med.), Professor, Head of Academician G.N. Speranskiy Department of Pediatrics, Russian Medical Academy of Continuous Professional Education, 2/1, Barrikadnaya str. , Moscow, 125993, Russian Federation, ORCID iD 0000-0003-4200-4598.
, Moscow, 125993, Russian Federation, ORCID iD 0000-0003-4200-4598.
Stanislav V. Mal'tsev - Doct. of Sci. (Med.), professor of Academician G.N. Speranskiy Department of Pediatrics, Russian Medical Academy of Continuous Professional Education, 2/1, Barrikadnaya str., Moscow, 125993, Russian Federation, ORCID iD 0000-0002-6203-2134.
Viktor V. Zubkov - Doct. of Sci. (Med.), Professor, Director of the Institute of Neonatology & Pediatrics, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, 4, Academician Oparin str., Moscow, 117997, Russian Federation, ORCID iD 0000-0001-8366-5208.
Viktoriya A. Kur'yaninova - Cand. of Sci. (Med.), associate professor of the Department of Propaedeutics of Children’s Diseases, Stavropol State Medical University, 310, Mira str., Stavropol, 355017, Russian Federation, ORCID iD 0000-0002-0731-7153.
Andrey V. Dmitriev - Doct. of Sci.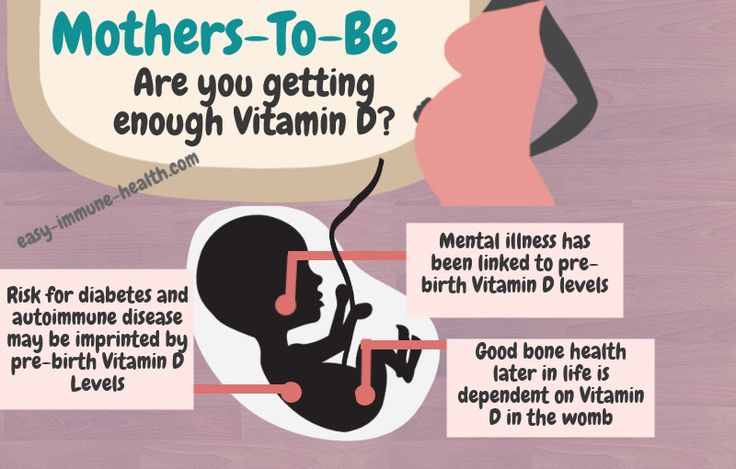 (Med.), Associate Professor, Head of the Department of Children’s Diseases with the Course of Hospital Pediatrics, Ryazan State Medical University, 9, Vysokovol’tnaya str., 3
(Med.), Associate Professor, Head of the Department of Children’s Diseases with the Course of Hospital Pediatrics, Ryazan State Medical University, 9, Vysokovol’tnaya str., 3, Russian Federation; professor of Prof. V.V. Gavryushov Department of Neonatology, Russian Medical Academy of Continuous Professional Education, 2/1, Barrikadnaya str., Moscow, 125993, Russian Federation, ORCID iD 0000-0002-8202-3876.
Larisa I.Maltseva - Doct. of Sci. (Med.), professor of the Department of Obstetrics & Gynecology, Kazan State Medical University — Branch of the Russian Medical Academy of Continuous Professional Education, 49, Butlerov str., Kazan, 420012, Russian Federation, ORCID iD 0000-0003-0999 -4374.
Natal'ya E. Verisokina - assistant of the Department of Faculty Pediatrics, Stavropol State Medical University, 310, Mira str., Stavropol, 355017, Russian Federation, ORCID iD 0000-0001-5444-8351.
Leonid Ya. Klimov-Doct. of Sci. (Med.), Associate Professor, Dean of the Pediatric Faculty, Stavropol State Medical University, 310, Mira str., Stavropol, 355017, Russian Federation, ORCID iD 0000-0001-7248-1614.
of Sci. (Med.), Associate Professor, Dean of the Pediatric Faculty, Stavropol State Medical University, 310, Mira str., Stavropol, 355017, Russian Federation, ORCID iD 0000-0001-7248-1614.
Elvira N. Vasil'eva - Cand. of Sci. (Med.), Associate Professor, associate professor of the Department of Obstetrics & Gynecology, I.N. Ul'yanov Cheboksary State University, 15, Moskovskiy av., Cheboksary, 428015, Russian Federation, ORCID iD 0000-0002-7677-7735.
Svetlana I. Malyavskaya - Doct. of Sci. (Med.), Professor, Head of the Department of Pediatrics, North State Medical University, 51, Troitskiy av., Arkhangelsk, 163000, Russian Federation, ORCID iD 0000-0003-2521-0824.
Andrey L. Zaplatnikov - Doct. of Sci. (Med.), Professor, Head of Prof. N.N. Gavryushov Department of Neonatology, professor of Acad. G.N. Speranskiy Department of Pediatrics, Vice-chancellor for Instructional Work, Russian Medical Academy of Continuous Professional Education, 2/1, Barrikadnaya str.