Ultrasound after miscarriage
Ultrasound is a Critical Tool of Managing Miscarriage
This story originally appeared in Diagnostic Imaging's sister site, Contemporary Ob/Gyn
Introduction
Early pregnancy loss (miscarriage) is defined as a nonviable, intrauterine pregnancy with either an empty gestational sac or a gestational sac containing an embryo or fetus without cardiac activity within the first 12 6/7 weeks of gestation.1
The cessation of development occurs in approximately 10 percent to 20 percent of clinically recognized pregnancies, increasing with advancing parental age.1-3 With the adoption of early home pregnancy testing, women are commonly referred for sonographic evaluations very early in gestation to determine pregnancy location and viability.
Although we believe ultrasound to be indispensable for the management of suspected early pregnancy failure, if performed too early or without strict adherence to guidelines, it may lead to inconclusive results or an incorrect diagnosis of an early pregnancy loss. 4
Ultrasonography (usually transvaginal) in combination with β-hCG and clinical history is instrumental for making the diagnosis of a nonviable pregnancy with certainty.
Historically, these criteria were based on small studies; a CRL of ≥ 5mm and mean sac diameter of≥ 16-17 mm without an embryo were considered diagnostic for an early pregnancy loss.1,5 Over the last decade, the reliability of these thresholds has been called into question.6,7
In 2013, the Society of Radiologists in Ultrasound (SRU) convened a multispecialty panel on early first-trimester diagnosis of miscarriage and exclusion of a viable intrauterine pregnancy (cannot result in the birth of a live baby) and published a more conservative approach to defining a pregnancy as nonviable.5
This change was made with the expectation of a diagnostic specificity of 100 percent (no false positives), while accounting for intra and inter-observer variability in measurements as well as a range in practice conditions and experience. 6,7 Inadvertent misclassification of potentially viable pregnancy as nonviable with resultant medical or surgical intervention resulting in the iatrogenic termination of a desired pregnancy has significant consequences to the family and may be an inciting factor in malpractice cases.8,9
6,7 Inadvertent misclassification of potentially viable pregnancy as nonviable with resultant medical or surgical intervention resulting in the iatrogenic termination of a desired pregnancy has significant consequences to the family and may be an inciting factor in malpractice cases.8,9
This article will focus on the criteria for the sonographic diagnosis of a nonviable intrauterine pregnancy early in gestation, those sonographic findings that are suspicious to result in an early pregnancy loss, and the vital role of ultrasound in these frequent clinical scenarios.
The sonographic findings are only one part of the puzzle in determining if a pregnancy is nonviable.
In order to apply the findings to a clinical situation, the obstetric care provider must take other clinical factors into consideration, such as accounting for the certitude of menstrual dating, the woman’s desire to continue the pregnancy until the definitive diagnosis is made along with logistical challenges such as the possibility of heavy bleeding leading to emergency room visits, unexpected passage of products of conception or unscheduled surgical procedures.
On another note, when diagnosing a complete miscarriage, care must be taken that an intrauterine pregnancy has previously been confirmed. If not, serial β-hCG should be performed so as to not miss the diagnosis of an ectopic pregnancy.
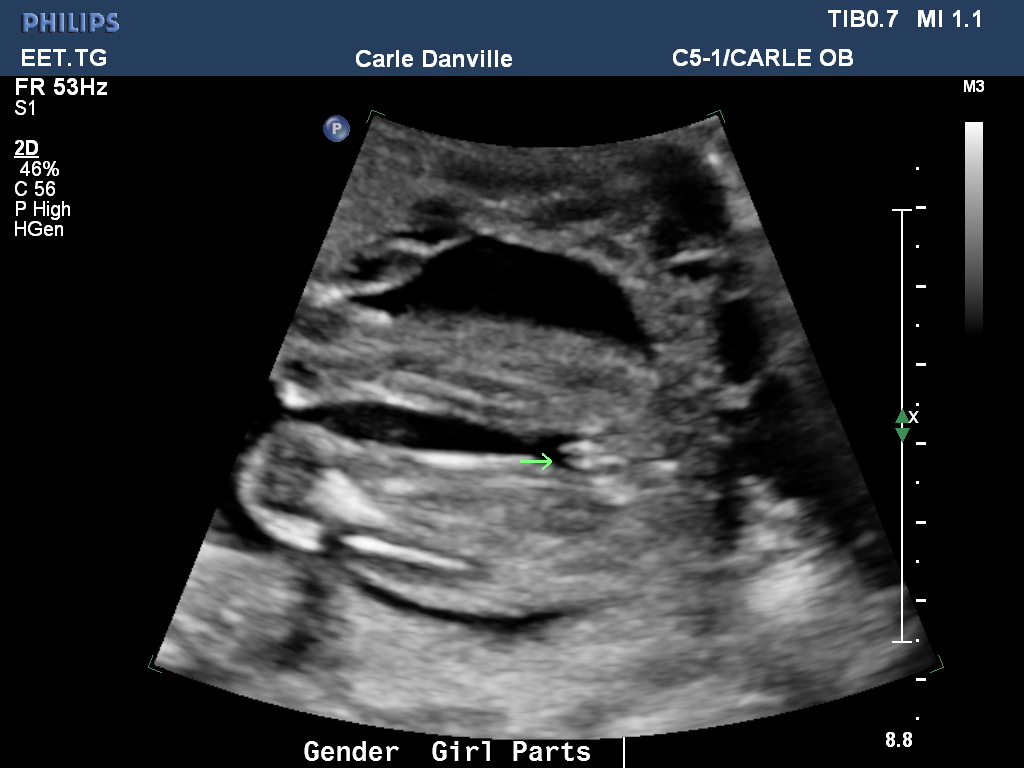
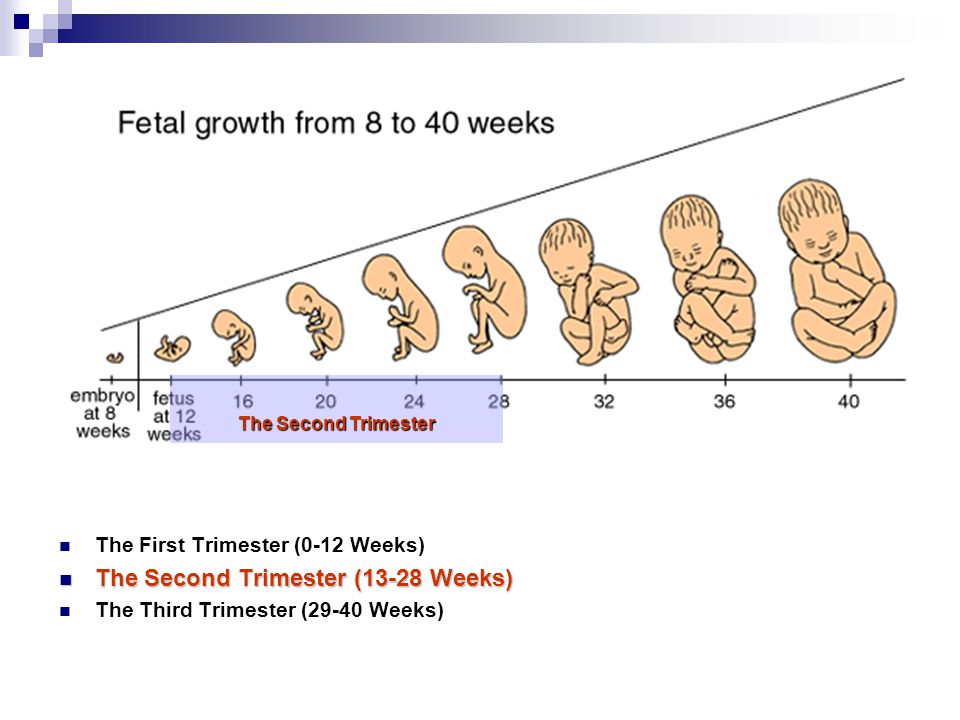
Embryologic development in early pregnancy is quite linear and follows a dependable and fairly tight timetable (Figs. 1A, B, C, D).
Ultrasound can reliably characterize the progression of a normally developing pregnancy from very early in gestation.
The gestational sac is first identified at approximately 5 weeks, the yolk sac is visible at approximately 5.5 weeks and an embryo with cardiac activity located in close proximity to the yolk sac should be evident at approximately 6 weeks gestation.
Embryonic cardiac activity is often seen when the embryo is first identified, measuring as little as 2 mm in length. The mean sac diameter is the average of three orthogonal diameters of the fluid portion of the gestational sac but is not as accurate as crown rump length for gestational dating. 10
10
Nomograms for development of embryonic length, heart rate, gestational sac diameter, and yolk sac diameter are available.11,12
Transvaginal sonographic findings diagnostic of an early pregnancy loss
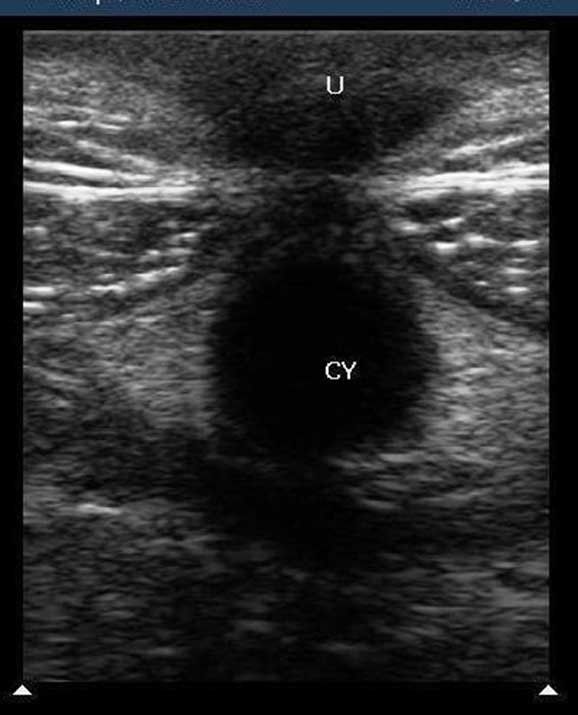
Given the newer, more conservative guidelines that are now well-accepted, a single transvaginal ultrasound identifying an embryo with a crown rump length of 7 mm or greater without cardiac activity or a gestational sac with a mean sac diameter of 25 mm or greater without an embryo is considered definitive proof that a pregnancy is nonviable5 (Figs. 2 and 3).
These metrics have also been validated in a prospective observational multicenter study to have a specificity of 100 percent.13
Given the expected linear development of normal early pregnancies, the definitive diagnosis of an early pregnancy loss can also be made based on sequential transvaginal ultrasound scans over a specified time interval (Figure 4).
In a normally developing viable pregnancy, an embryo with cardiac activity must be demonstrated ≥11 days after a gestational sac with a yolk sac or ≥14 days in which a gestational sac without a yolk sac was identified by transvaginal sonography.
The lack of cardiac activity after that interval of observation is definitive evidence for an early pregnancy loss. A shorter interval of observation with no embryonic heart motion would raise suspicion for an early pregnancy loss, however, it is not definitive.5,13
Predictably, patients are anxious when the results of an indeterminant status of viability are disclosed, and the rationale behind the recommended time interval for follow up of the sonographic evaluation should be communicated.
Transvaginal sonographic findings suspicious (but not diagnostic) for early pregnancy loss
If an embryo is seen with a crown-rump length of <7 mm and without cardiac activity, it is suspicious for an early pregnancy loss (Figure 5). Similarly, a gestational sac with a mean sac diameter of 16-24 mm and no embryo is suspicious for an early pregnancy loss.
Similarly, a gestational sac with a mean sac diameter of 16-24 mm and no embryo is suspicious for an early pregnancy loss.
The development of gestational sac landmarks is progressive and therefore the sonographic finding of an amnion with an adjacent yolk sac and without a visualized embryo is suspicious for an early pregnancy loss (Figure 6). It is important not to mistake a second yolk sac for the amnion as may be seen with early monochorionic diamniotic twins. If ascertainment of viability is indeterminant based on a suspicious finding, it is generally appropriate to repeat the ultrasound examination in 7-10 days.5,13
Sonographic signs concerning for an increased risk of early pregnancy loss
In embryos in which cardiac activity is demonstrated, there are additional sonographic features that may signal an increased risk for early pregnancy loss. These include findings such as embryonic bradycardia, a small gestational sac, a large yolk sac, and a subchorionic hematoma.
Embryonic or fetal bradycardia
In normal pregnancies, the embryonic heart rate progressively increases up to 8 weeks’ gestation. It has been 25 years since the seminal paper by Doubilet and Benson in which the rate of first-trimester pregnancy loss was directly correlated with embryonic heart rate 14 (Figure 7).
These investigators evaluated 1,185 early pregnancies and provided pregnancy loss rates stratified by the degree of bradycardia and gestational age. The slower the heart rate, the higher the risk of pregnancy loss (Table 1).
A recent systematic review and diagnostic accuracy meta-analysis evaluating the prediction of miscarriage found that the most predictive factor for early pregnancy loss was embryonic/fetal heart rate.16 This predictive effect was even more pronounced among those with bleeding in early pregnancy.
In their hierarchical summary receiver operating characteristic model curve, the authors found that bradycardia had a sensitivity of 68. 4 percent, specificity of 97.8 percent, positive likelihood ratio of 31.7, and negative likelihood ratio of 0.32 for predicting early pregnancy loss.
4 percent, specificity of 97.8 percent, positive likelihood ratio of 31.7, and negative likelihood ratio of 0.32 for predicting early pregnancy loss.
For those with bleeding the sensitivity of heart rate to predict miscarriage increased further (sensitivity, 84.2 percent, specificity, 95.7 percent, positive likelihood ratio, 19.51, and negative likelihood ratio, 0.16).
The authors found that the best cut-off for heart rate was <110 bpm for the prediction of miscarriage. A heart rate of >134 bpm at seven weeks’ gestation and a heart rate of >158 bpm at 8 weeks’ gestation were predictive of on-going pregnancies.
These data highlight the importance of assessing embryonic heart rate by M-mode while performing an early ultrasound, as it is the most predictive sign of pregnancy loss. It must be recognized, however, that in an embryo of less than 6 weeks gestation, the very initiation of cardiac pulsations may be reflected in a slower rate,17 which underscores the value of a repeat scan.
A bradycardic heart rate should prompt a follow-up sonographic examination to assess embryonic viability, whereas a normal heart rate provides considerable reassurance for the patient.
Small gestational sac in relation to crown-rump lengthOn occasion, an embryo with a normal heart rate will appear sonographically ‘crowded’ within the gestational sac (Figure 8), a finding which has been associated with an increased risk of early pregnancy loss.18,19
Objectively, this has been characterized as a mean sac size – crown rump length (MSS-CRL) of < 5 mm.18 Bromley et al. demonstrated that the risk of miscarriage was 94 percent with a small gestational sac in the first trimester despite a normal cardiac rate.
In a larger and more recent study of patients conceiving via IVF, the early pregnancy loss rate among patients with a MSS-CRL of< 5 mm was approximately 44 percent compared with a referent population with a MSS-CRL of 5-9. 9mm in whom the loss rate was 15.8 percent (P < .0001).19
9mm in whom the loss rate was 15.8 percent (P < .0001).19
Of note, there is no appreciable increase in the risk of early pregnancy loss between those conceiving using assisted reproductive technology compared with spontaneously conceived pregnancies.20 The sonographic finding of an embryo in a small gestational sac should prompt follow-up sonography to assess persistence of development.
Yolk sac size
The yolk sac is the first structure that is identifiable within the gestational sac by transvaginal ultrasound when the gestational sac reaches 8-10 mm. Abnormalities in size and appearance of the yolk sac have been reported to be associated with an increased risk of pregnancy loss, although not all studies have found this to be a useful metric for predicting pregnancy loss.5,12,21
The sonographic assessment of the yolk sac in asymptomatic patients as a predictor of miscarriage has shown sensitivities ranging from 17 percent to 69 percent and specificities ranging from 79 percent to 99 percent.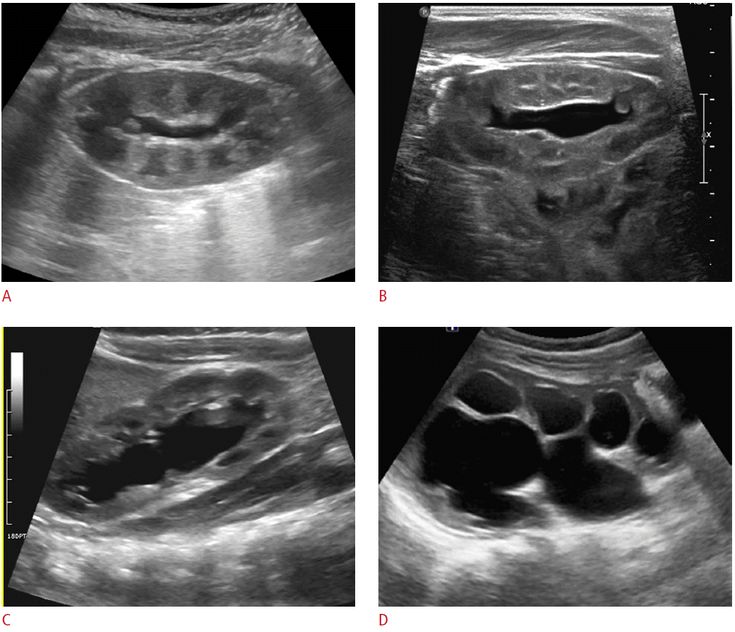 16 A yolk sac of greater than 7 mm has been suggested as a concerning threshold for an increased risk of pregnancy loss, although methods of measurement have been inconsistent.5
16 A yolk sac of greater than 7 mm has been suggested as a concerning threshold for an increased risk of pregnancy loss, although methods of measurement have been inconsistent.5
Recent data suggests yolk sac diameter does not improve the prediction of miscarriage over bradycardic heart rates and limited embryonic/fetal crown-rump length.22
One should be very cautious in the use of this sonographic sign, especially as an isolated finding, for prediction of first-trimester pregnancy loss until stronger guidance from the literature is available.
Crown-rump length
In a well dated pregnancy, a small crown-rump length for gestational age may reflect early growth disturbance and is associated with an increased risk of aneuploidy as well as early pregnancy loss.22 Among an IVF population with clear gestational age determination, those with a crown-rump length of < 10 percent had an increased risk of miscarriage as compared to those normally grown, 17. 2 percent vs. 6.6 percent,P = 0.005, OR = 2.93, 95% CI 1.2,6.7).23
2 percent vs. 6.6 percent,P = 0.005, OR = 2.93, 95% CI 1.2,6.7).23
Should a much smaller than expected crown-rump length be encountered in the first trimester, especially those that would lead to a change in pregnancy dating, a follow-up evaluation to assess interval growth in 2 weeks should be considered.
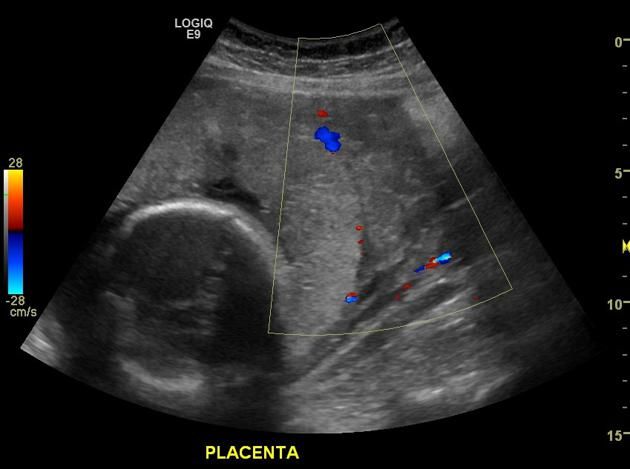
Subchorionic hematoma
Bleeding in early pregnancy is common, and a subchorionic hematoma can be sonographically identified in this setting (Figure 9). Subchorionic hematoma has been associated with an increased rate of pregnancy loss, especially if the hematoma is large, associated with bleeding or the patient is 35 years of age or older.24
The method of assessing the size of the subchorionic hematoma has been controversial, but it appears that in one study, the subjective assessment of hematoma size based on the fraction of the gestational sac size correlates best with first-trimester pregnancy outcome.25 The rate of spontaneous pregnancy loss in the first trimester is reported to be highest for those hematomas diagnosed before 8 weeks (19. 6 percent) compared to those diagnosed after 8 weeks (3.6 percent; P < .001).25
6 percent) compared to those diagnosed after 8 weeks (3.6 percent; P < .001).25
A review and meta-analysis demonstrated that the identification of a subchorionic hematoma was associated with an increased risk for miscarriage, increasing from 8.9 percent to 17.6 percent, pooled OR 2.18, 95% CI 1.29, 3.68).26
A recent retrospective cohort study of 2,446 patients with singletons presenting for ultrasound between 6 weeks and 13+6d weeks at a single center, demonstrated that subchorionic hematoma was associated with an increased risk of pregnancy loss before 20 weeks gestation (7.5 percent vs. 4.9 percent P=.026) on univariate analysis, however, when adjusting for patient age and bleeding, this association was no longer significant.27
Similarly, these authors showed no increased risk of adverse outcome later in gestation.28 Given the possible increased risk for pregnancy loss, follow-up sonography can be considered in these cases.
Chorionic Bump
A chorionic bump is a focal convex protuberance that develops at the choriodecidual surface and protrudes into the gestational sac in the early first trimester, likely reflecting a hematoma or necrotic decidua (Figure 10).
The finding has been associated with an increased risk of early pregnancy loss when identified before 11 weeks gestation. If a chorionic bump is identified and the pregnancy is otherwise normal in appearance with a normal heart rate, the live birth rate has been reported to be approximately 83 percent.29
In addition, there was no significant relationship between the volume of the chorionic bump or bleeding per vagina and the risk of pregnancy loss.29 In the latter part of the first trimester, the presence of a chorionic bump is not thought to be clinically relevant.30
Conclusions
Ultrasound is a powerful tool in the diagnosis and prediction of early pregnancy loss.
Practitioners must be diligent to follow guidelines for diagnosing a pregnancy as non-viable in order to prevent an iatrogenic pregnancy termination. Although some patients will have sonographic findings that definitively allow the diagnosis of a failed pregnancy, many will have findings that are suggestive or inconclusive of miscarriage. A follow-up scan can be very helpful in these cases.
The timing of the sonographic evaluation is important in management, as too early an evaluation is likely to lead to an ultrasound report of a pregnancy of unknown location or an intrauterine pregnancy of uncertain viability.
In a study of asymptomatic women attending an early pregnancy ultrasound unit, the diagnosis of a miscarriage could not be made on initial ultrasound examination until 35 days from LMP and most miscarriages were diagnosed when the first assessment was between 63 and 85 days after the LMP.4
These authors recommended that in order to reduce the number of inconclusive scans, asymptomatic women without a history of ectopic, delay an initial ultrasound until 49 days from LMP. 4
4
Healthcare providers taking care of women suspected of having or experiencing an early pregnancy loss should have training in how to compassionately and effectively communicate difficult news as the patient is at risk for posttraumatic stress, anxiety and depression.9
About the Authors
DR. BROMLEY practices in the Department of OB/GYN at Massachusetts General Hospital in Boston and with Diagnostic Ultrasound Associates, PC, in Brookline, Mass. She is a part-time professor at Harvard Medical School.
DR. SHIPP practices in the Department of OB/GYN at Brigham & Women’s Hospital in Boston and with Diagnostic Ultrasound Associates, PC, in Brookline, Mass. He is an associate professor at Harvard Medical School.
References1.ACOG Practice Bulletin No. 200: Early Pregnancy Loss. Obstet Gynecol. 2018;132(5):e197-e207.
2.Wise LA, Wang TR, Willis SK, Wesselink AK, Rothman KJ, Hatch EE.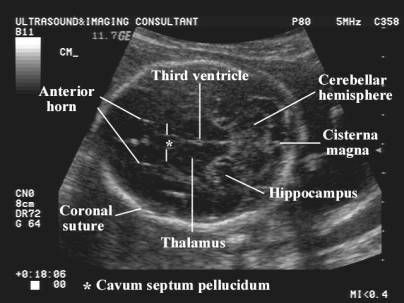 Effect of a Home Pregnancy Test Intervention on Cohort Retention and Pregnancy Detection: A Randomized Trial. Am J Epidemiol. 2020.
Effect of a Home Pregnancy Test Intervention on Cohort Retention and Pregnancy Detection: A Randomized Trial. Am J Epidemiol. 2020.
3.Ammon Avalos L, Galindo C, Li DK. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012;94(6):417-423.
4.Bottomley C, Van Belle V, Mukri F, et al. The optimal timing of an ultrasound scan to assess the location and viability of an early pregnancy. Hum Reprod. 2009;24(8):1811-1817.
5.Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369(15):1443-1451.
6.Pexsters A, Luts J, Van Schoubroeck D, et al. Clinical implications of intra- and interobserver reproducibility of transvaginal sonographic measurement of gestational sac and crown-rump length at 6-9 weeks' gestation. Ultrasound Obstet Gynecol. 2011;38(5):510-515.
2011;38(5):510-515.
7.Abdallah Y, Daemen A, Kirk E, et al. Limitations of current definitions of miscarriage using mean gestational sac diameter and crown-rump length measurements: a multicenter observational study. Ultrasound Obstet Gynecol. 2011;38(5):497-502.
8.Shwayder JM. Waiting for the tide to change: reducing risk in the turbulent sea of liability. Obstet Gynecol. 2010;116(1):8-15.
9.Farren J, Jalmbrant M, Falconieri N, et al. Posttraumatic stress, anxiety and depression following miscarriage and ectopic pregnancy: a multicenter, prospective, cohort study. Am J Obstet Gynecol. 2020;222(4):367 e361-367 e322.
10.Committee on Obstetric Practice tAIoUiM, the Society for Maternal-Fetal M. Committee Opinion No 700: Methods for Estimating the Due Date. Obstet Gynecol. 2017;129(5):e150-e154.
11.Papaioannou GI, Syngelaki A, Poon LC, Ross JA, Nicolaides KH. Normal ranges of embryonic length, embryonic heart rate, gestational sac diameter and yolk sac diameter at 6-10 weeks.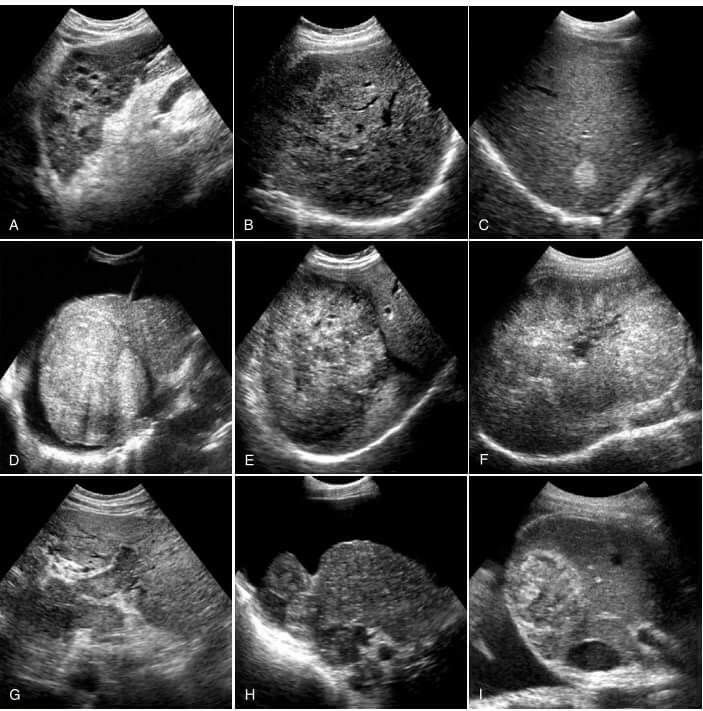 Fetal Diagn Ther. 2010;28(4):207-219.
Fetal Diagn Ther. 2010;28(4):207-219.
12.Detti L, Francillon L, Christiansen ME, et al. Early pregnancy ultrasound measurements and prediction of first trimester pregnancy loss: A logistic model. Sci Rep. 2020;10(1):1545.
13.Preisler J, Kopeika J, Ismail L, et al. Defining safe criteria to diagnose miscarriage: prospective observational multicentre study. BMJ. 2015;351:h5579.
14.Bromley B, Doubilet P, Frigoletto FD, Jr., Krauss C, Estroff JA, Benacerraf BR. Is fetal hyperechoic bowel on second-trimester sonogram an indication for amniocentesis? Obstet Gynecol. 1994;83(5 Pt 1):647-651.
15.Doubilet PM, Benson CB. Embryonic heart rate in the early first trimester: what rate is normal? J Ultrasound Med. 1995;14(6):431-434.
16.Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis.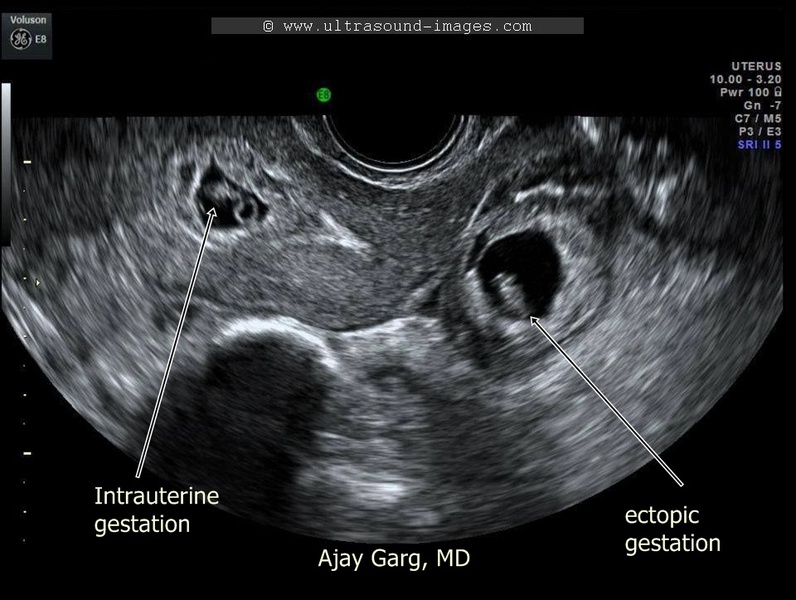 Eur J Obstet Gynecol Reprod Biol. 2018;220:122-131.
Eur J Obstet Gynecol Reprod Biol. 2018;220:122-131.
17.DuBose TJ. Embryonic heart rates. Fertil Steril. 2009;92(4):e57; author reply e58.
18.Bromley B, Harlow BL, Laboda LA, Benacerraf BR. Small sac size in the first trimester: a predictor of poor fetal outcome. Radiology. 1991;178(2):375-377.
19.Kapfhamer JD, Palaniappan S, Summers K, et al. Difference between mean gestational sac diameter and crown-rump length as a marker of first-trimester pregnancy loss after in vitro fertilization. Fertil Steril. 2018;109(1):130-136.
20.Schieve LA, Tatham L, Peterson HB, Toner J, Jeng G. Spontaneous abortion among pregnancies conceived using assisted reproductive technology in the United States. Obstet Gynecol. 2003;101(5 Pt 1):959-967.
21.Taylor TJ, Quinton AE, de Vries BS, Hyett JA. First-trimester ultrasound features associated with subsequent miscarriage: A prospective study. Aust N Z J Obstet Gynaecol. 2019;59(5):641-648.
Aust N Z J Obstet Gynaecol. 2019;59(5):641-648.
22.DeVilbiss EA, Mumford SL, Sjaarda LA, et al. Prediction of pregnancy loss by early first trimester ultrasound characteristics. Am J Obstet Gynecol. 2020.
23.Gabbay-Benziv R, Dolev A, Bardin R, Meizner I, Fisch B, Ben-Haroush A. Prediction of fetal loss by first-trimester crown-rump length in IVF pregnancies. Arch Gynecol Obstet. 2017;295(3):771-775.
24.Bennett GL, Bromley B, Lieberman E, Benacerraf BR. Subchorionic hemorrhage in first-trimester pregnancies: prediction of pregnancy outcome with sonography. Radiology. 1996;200(3):803-806.
25.Heller HT, Asch EA, Durfee SM, et al. Subchorionic Hematoma: Correlation of Grading Techniques With First-Trimester Pregnancy Outcome. J Ultrasound Med. 2018;37(7):1725-1732.
26.Tuuli MG, Norman SM, Odibo AO, Macones GA, Cahill AG. Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis. Obstet Gynecol. 2011;117(5):1205-1212.
Obstet Gynecol. 2011;117(5):1205-1212.
27.Naert MN, Khadraoui H, Muniz Rodriguez A, Naqvi M, Fox NS. Association Between First-Trimester Subchorionic Hematomas and Pregnancy Loss in Singleton Pregnancies. Obstet Gynecol. 2019;134(2):276-281.
28.Naert MN, Muniz Rodriguez A, Khadraoui H, Naqvi M, Fox NS. Association Between First-Trimester Subchorionic Hematomas and Adverse Pregnancy Outcomes After 20 Weeks of Gestation in Singleton Pregnancies. Obstet Gynecol. 2019;134(4):863-868.
29.Arleo EK, Dunning A, Troiano RN. Chorionic bump in pregnant patients and associated live birth rate: a systematic review and meta-analysis. J Ultrasound Med. 2015;34(4):553-557.
30.Sepulveda W. Chorionic bump at 11 to 13 weeks' gestation: Prevalence and clinical significance. Prenat Diagn. 2019;39(6):471-476.
Ultrasound scans - The Miscarriage Association
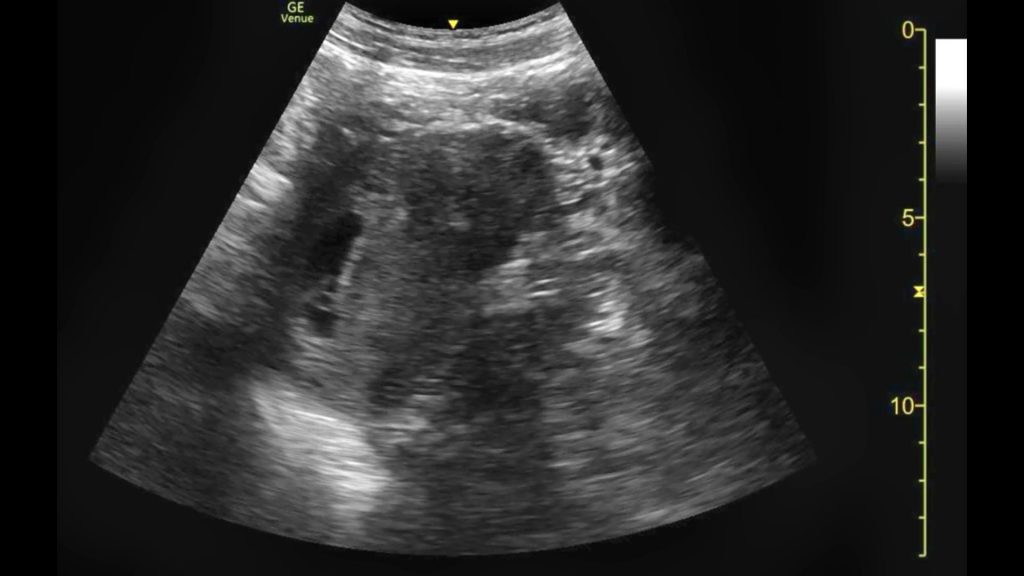
Ultrasound scans in pregnancy may be routine or they may be offered because of pain or bleeding or because of problems in a previous pregnancy.
There are two ways of doing an ultrasound scan.
In early pregnancy, especially before 11 weeks, it is usual to have a trans-vaginal (internal) scan, where a probe is placed in the vagina. This gives the clearest and most accurate picture in early pregnancy. It may also be offered after 11 or 12 weeks if a trans-abdominal scan doesn’t give a clear enough picture.
From 11 or 12 weeks, including at the routine booking-in scan, it is more common to have a trans-abdominal scan. The person doing the scan spreads a special gel on your lower abdomen (below your belly button and above the line of pubic hair). He or she then moves the scanner over the gel, sometimes pressing down, until the uterus (womb) and pregnancy can be seen.
What if I don’t want an internal scan?If you don’t want a trans-vaginal scan, you can ask for a trans-abdominal scan. That may give some information about your pregnancy, but it is less clear than an internal scan and that could possibly delay diagnosis.
There is no evidence that having a vaginal or an abdominal scan will cause a miscarriage or harm your baby. If you bleed after a vaginal scan, it will most likely be because there was already blood pooled higher in the vagina and the probe dislodged it.
When can I have an ultrasound scan? When can you see the baby’s heartbeat?An ultrasound scan may be able to detect a pregnancy and a heartbeat in a normal pregnancy at around 6 weeks, but this varies a great deal and isn’t usually advised. All too often, a scan at 6 weeks shows very little or nothing, even in a perfectly developing pregnancy, whereas waiting a week or 10 days will make the findings much clearer.
Routine scansMost pregnant women are referred for their first routine (or booking or dating) ultrasound scan somewhere between 11 and 14 weeks of pregnancy. The purpose of the scan is:
The purpose of the scan is:
- to confirm that there is a heartbeat
- to assess the baby’s size and growth
- to estimate the delivery date and
- to check whether there is one baby, or twins or more.
Some women may be offered a nuchal scan between 11 and 14 weeks. The purpose of this scan is to try to detect some chromosome abnormalities, such as Downs syndrome.
Most hospitals also offer a further anomaly scan at 20 weeks, making a more detailed check of the baby’s development.
You can find out more about routine, nuchal and anomaly scans at the website of the charity ARC – Antenatal Results and Choices
Sadly…Sadly, sometimes these scans show that the baby has died, possibly some weeks earlier and often without any signs or symptoms such as bleeding or pain. This is often called a “missed”, “silent” or “delayed” miscarriage. This can come as a considerable shock and it may take time before you can take this information in.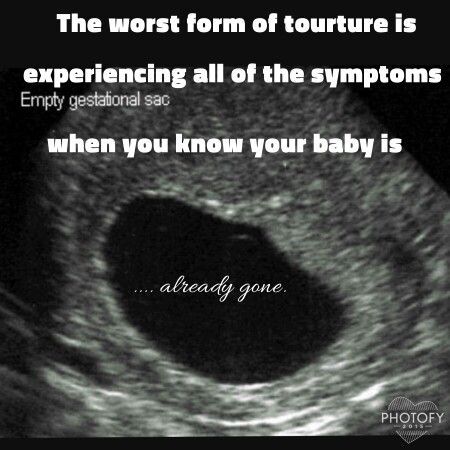 You can find information about missed miscarriage here.
You can find information about missed miscarriage here.
You may also have to make some difficult decisions about how to manage the miscarriage process. You can read more about this here.
Early scansYou may be referred for an early scan because of vaginal bleeding or spotting, or possibly because you have had problems in a previous pregnancy.
The best time to have a scan is from about 7 weeks’ gestation when it should be possible to see the baby’s heartbeat in a normal pregnancy. But it can be hard to detect a heartbeat in early pregnancy and in those cases it can be hard to know whether the baby has died or not developed at all, or whether it is simply smaller than expected but still developing.
For that reason, you may be asked to return for another scan a week or so later. At that time, the person doing the scan will be looking for a clear difference in the size of the pregnancy sac and for a developing baby and a heartbeat.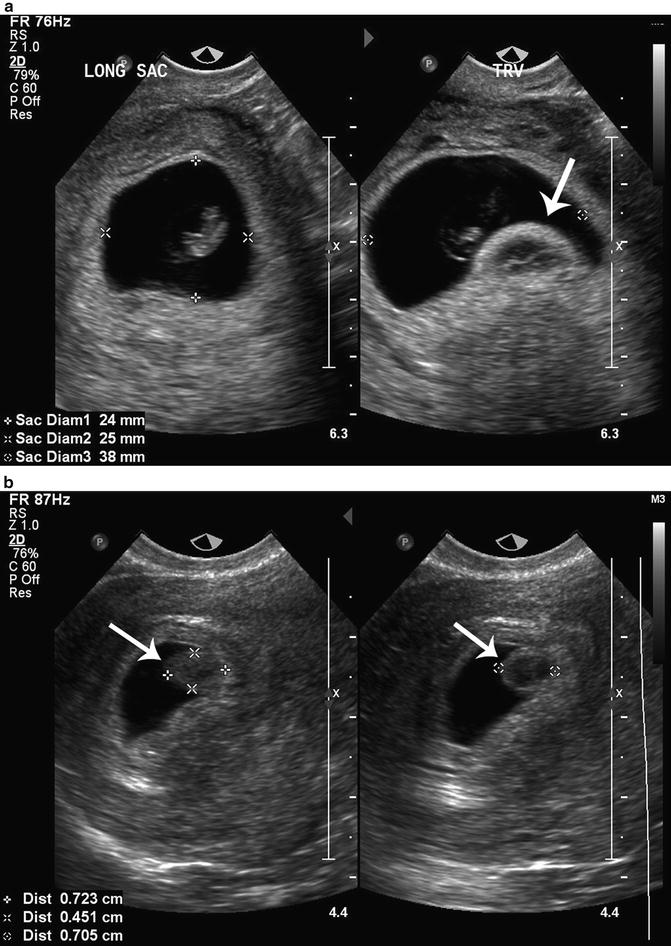
Sometimes, it can take several scans before you know for sure what is happening. It can be very stressful dealing with this uncertainty – some women describe it as being “in limbo”. You may need to find some support for yourself if this happens to you.
There’s a heartbeat, but I’m still bleeding…If the scan does pick up a heartbeat and the baby appears to be the right size according to your dates, this can be very reassuring, even if you are still bleeding. Seeing a heartbeat on scan also increased the likelihood of the pregnancy continuing.
Research amongst women with a history of recurrent miscarriage has shown that while those who reached six weeks of pregnancy had a 78% chance of the pregnancy continuing, seeing a heartbeat at 8 weeks increased the chance of a continuing pregnancy to 98% and at 10 weeks that went up to 99.4%.
The numbers may be even more positive for women without previous miscarriages.
So things could still go wrong and sadly sometimes do, but once a heartbeat is seen, the risk of miscarriage decreases as the weeks go by.
In some cases, if there is no sign of a pregnancy in the uterus, you may be given a blood test and possibly asked to return two days later for a repeat test.
These blood tests measure the level of the pregnancy hormone ßhCG. In a normally developing pregnancy the hormone levels roughly double about every 48 hours and if the pattern is different, this can help to identify what is happening to the pregnancy.
If there is no sign of a pregnancy in the uterus and you have symptoms that suggest ectopic pregnancy, you are more likely to have both a blood test and an investigation called a laparoscopy, which is done under general anaesthetic. You can read more about this here and in our leaflet Ectopic pregnancy.
Ultrasound scan results – and what they meanThe ultrasound scan may show:
- A viable ongoing pregnancy. There is a heartbeat (or heartbeats if it’s a twin or multiple pregnancy) and the pregnancy is the “right size for dates” – that is, the size that would be expected based on the first day of your last period.
 Those are positive signs, but if you continue to bleed, you may need a further scan in a week or two to check what’s happening.
Those are positive signs, but if you continue to bleed, you may need a further scan in a week or two to check what’s happening.
- An ongoing pregnancy that suggests a problem. The pregnancy may be much smaller than it should be according to dates or the heartbeat might be particularly slow or faint. Perhaps there is something that suggests a problem with the baby’s development. With a twin or multiple pregnancy, the scan may show that one (or more) baby has a heartbeat and one (or more) doesn’t. You may be asked to come back for another scan, possibly in a week or two when things should be clearer.
- A pregnancy of unknown location (PUL). The pregnancy is not visible and it’s not clear what is happening. You may be asked to come back for another scan, possibly in a week or two when things should be clearer. Or if the doctor thinks you might have an ectopic pregnancy, you will have blood tests and/or a laparoscopy (keyhole surgery to look inside the abdomen).
- A complete miscarriage. The pregnancy has miscarried. There may still be a small amount of pregnancy tissue or blood in the uterus.
- A non-viable pregnancy. This means a pregnancy that hasn’t survived but hasn’t yet miscarried. You may hear this described in one of the following ways:
- Missed miscarriage (also called silent or delayed miscarriage or early embryonic demise) This is where the baby has died or failed to develop but your body has not miscarried him or her. The scan picture shows a pregnancy sac with a baby (or fetus or embryo) inside, but there is no heartbeat and the pregnancy looks smaller than it should be at this stage. You may have had little or no sign that anything was wrong and you may still feel pregnant. You might still have a positive pregnancy test.
- Blighted ovum or anembryonic pregnancy (which means a pregnancy without an embryo). This is a rather old-fashioned way of describing a missed miscarriage (see above).
 The scan picture usually shows an empty pregnancy sac.
The scan picture usually shows an empty pregnancy sac.
- Blighted ovum or anembryonic pregnancy (which means a pregnancy without an embryo). This is a rather old-fashioned way of describing a missed miscarriage (see above).
- Incomplete miscarriage The process of miscarriage has started but there is still pregnancy tissue in the uterus (womb) and you may still have pain and heavy bleeding.
In all of these situations, the pregnancy will fully miscarry with time, but there are several ways of managing the process. You may be offered a choice, or the hospital might make a recommendation. In most cases, you should be able to have time to think about what you can best cope with. You can read more here.
The ultrasound scan might show- An ectopic pregnancy. This means a pregnancy that is developing outside the uterus (Ectopic means “out of place”). Ectopic pregnancies usually develop in one of the Fallopian tubes, but they can develop elsewhere inside the abdomen.
- A molar pregnancy. This is a pregnancy where the baby can’t develop but the cells of the placenta grow very quickly.
 It can’t always be diagnosed on scan so you might find out only after the miscarriage.
It can’t always be diagnosed on scan so you might find out only after the miscarriage.
Perform an ultrasound scan after an abortion (abortion) in the NEOMED clinic
High-quality ultrasound after an abortion in the NEOMED clinic is a guarantee of women's health!
Ultrasound of the pelvic organs in the NEOMED clinic is performed by experienced specialists, using expert-class equipment with the highest resolution and color image quality - SonoAce X8.
-
Description
-
Ultrasound of the pelvic organs is performed to assess the condition of the reproductive organs after an abortion and to prevent the development of complications.
Ultrasound of the pelvic organs is mandatory for every woman after an abortion. No modern abortion method guarantees 100% safety. Timely diagnosis of such consequences allows the gynecologist to take appropriate actions to eliminate them, prevent the threat of infertility and other serious problems.
Ultrasound of the pelvic organs in the NEOMED clinic is performed by experienced specialists, using expert-class equipment with the highest resolution and color image quality - SonoAce X8.
Indications for pelvic ultrasound after abortion
Preventive pelvic ultrasound is performed approximately 7-10 days after abortion .
Ultrasound allows the gynecologist to:
- exclude the remains of blood clots, fetal egg in the patient's uterine cavity;
- examine the condition of the tubes and ovaries, make sure there are no inflammatory processes.
Also an indication for an ultrasound examination is the manifestation of alarming symptoms in a woman:
- severe bleeding;
- sharp pains;
- chills, fever;
- dizziness, malaise, weakness, etc.
Ultrasound after an abortion
Ultrasound of the pelvic organs is absolutely harmless for a woman, the procedure is not associated with pain or discomfort. In the process of conducting this study, the uterus, vagina, fallopian tubes and ovaries, bladder are studied. Ultrasound of the pelvis after an abortion can be performed transvaginally (through the vagina) and transabdominal (through the abdomen) method.
In the process of conducting this study, the uterus, vagina, fallopian tubes and ovaries, bladder are studied. Ultrasound of the pelvis after an abortion can be performed transvaginally (through the vagina) and transabdominal (through the abdomen) method.
During the pelvic ultrasound, the patient is in the supine position. If a transabdominal ultrasound is performed, a small amount of a special gel is applied to the woman's lower abdomen. This improves the contact of the sensor with the skin. The procedure takes a minimum amount of time.
Preparing for ultrasound
The preparation rules depend on which ultrasound method is used:
- before transabdominal ultrasound, you should drink 0.5-1 liter of non-carbonated liquid (about an hour), do not urinate before the procedure;
- Before a transvaginal ultrasound, the patient, on the other hand, should empty her bladder.
In addition, a couple of days before the transvaginal ultrasound, it is advisable to follow a special diet (do not eat vegetables and fruits, bread, flour, dairy products).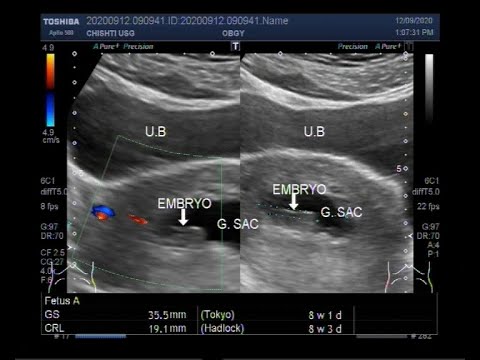 This is necessary in order to prevent excessive gas formation, which can distort the results of the study.
This is necessary in order to prevent excessive gas formation, which can distort the results of the study.
The text is hidden. Select a menu item to read more information.
Shares
and offers
In the formation of the information, practitioners of the clinic Neo -Mad took part:
Gladkov Sergey Yuryevich
Medical experience: since 2007
Schooldova Inna Mingiyanovna
Medical experience: since 1997
Evgeny Vladimirovich
. 2001
Zvonkova Zhanna Alexandrovna
Medical experience: since 2000
Shapovalov Alexander Sergeevich
Medical experience: since 2006
Schostak Igor Viktorovich
Medical experience: since 1988
Belova Lyubov Vladimirovna
Medical Medican: since 2006
Marmyl Svetlana Svetlana Svetlana Svetlana, 9008 Medical experience: since 1994
| Prices for services | |
| Ultrasound of the bladder and kidneys | 1200 |
| Renal ultrasound | 800 |
| Abdominal Ultrasound | 1500 |
| Ultrasound examination (ultrasound) of the abdominal cavity and kidneys | 1950 |
| Female pelvic ultrasound | 1500 |
| Male pelvic ultrasound | 1500 |
Make an appointment online - our operators will call you back to clarify a convenient time for visiting a doctor.
Appointment
21 years of care
Reviews
Valentina, 05/06/2019
Many thanks to the doctor who correctly examined and prescribed pills after which I got on my feet, And I suffered for a year after radiation therapy, How few such experienced doctors are, once again many heartfelt thanks
Read full review
Irina, 08/25/2016
I had several ultrasounds (folliculometry in the cycle) with Zvonkova Zhanna. I liked the way the doctor treats the procedure and the patient. Each time I carefully took all the indicators (M-ECHO, the number of follicles, the size of the dominant follicle). The doctor commented on everything he saw, explained. Usually you will not get any information from ultrasound specialists except "everything is within the normal range"
Read full review
Izmailova Kristina, 08/29/2018
I can only praise this medical institution. Very comfortably. In one evening after work, I resolved the issue with an ultrasound of the abdominal cavity, and had time for a consultation! Definitely a client oriented clinic!
Very comfortably. In one evening after work, I resolved the issue with an ultrasound of the abdominal cavity, and had time for a consultation! Definitely a client oriented clinic!
Read full review
Tatyana, 09/14/2018
Did a gynecological ultrasound. Conclusions about the center are favorable. Clean, front desk is fast. The appointment for ultrasound was checked before the appointment, they immediately offered a consultation with their gynecologist. The clinic is convenient for me both in terms of location and prices for services. I will contact if necessary.
Read full review
Arina, 09/10/2018
The doctor seemed to me a very competent specialist and a pleasant person. Yulia Valerievna received me on time, listened to me, carefully performed an ultrasound scan and scheduled an additional examination. I received the most complete consultation, I was given more than enough time. I have already scheduled a second appointment with the doctor and in the future I also plan to contact her.
Read full review
Elena, 01.01.1970
I visited the clinic several times. I liked it very much! The atmosphere is pleasant. No queues. Always taken at the appointed time (for me it was very important, because I value my time). I really liked the doctor who did the ultrasound of the abdominal organs. He looked at everything very carefully and for a long time (not like in other clinics for three minutes), gave a lot of useful advice. Unfortunately I don't remember his last name. Thank you for being!
Read full review
Alex, 10/18/2016
I want to express my gratitude to the wonderful doctor - Shostak I.V., who did an ultrasound of the abdominal cavity for me. Thank you for the clear and professional description of the ultrasound picture! Thanks to you, an accurate diagnosis was made and timely treatment was prescribed, which brought good results! Very good impressions from the clinic as a whole, thanks to everyone!
Read full review
Any questions? Just call us
Or send a request for a call back - and we will call you back!
+7 (812) 249-0-249 Request a call back
The medical service is provided by doctors
Gladkov Sergey Yuryevich
Acusher-gynecologist, gynecologist-endocrinologist, surgeon, Ultrasound diagnostic doctor
Online record
Details
SLEAKODOVA
9002 , gynecologist-endocrinologist, surgeon, doctor of ultrasound diagnostics.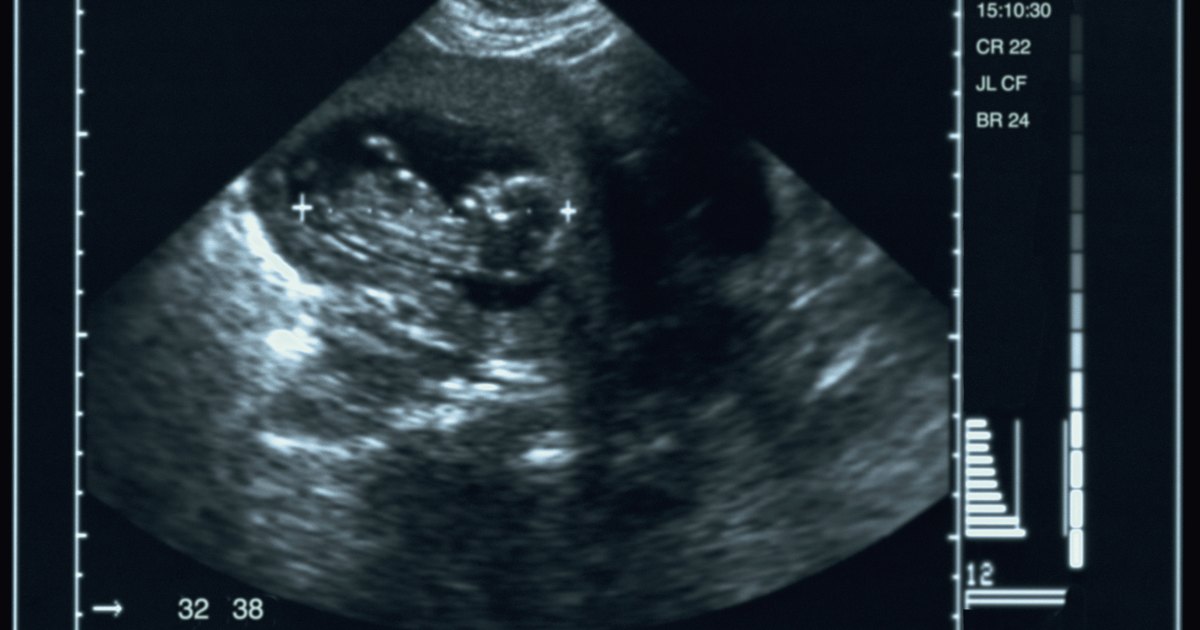
Read more
Evgeny Vladimirovich Evgeny
urologist, andrologist, ultrasound diagnostic doctor, operating urologist, KMN
Online record
Read more
Ultrazovka-vikusherta. first medical category
ONLINE BOOKING FOR AN APPOINTMENT
More details
Alexander Sergeevich Shapovalov
Surgeon, phlebologist, doctor of ultrasonic diagnostics of blood vessels.
BOOK ONLINE
More details
Nearest metro stations
Art. "Ozerki" 3 min. 1 min.
Art. "Prospect Education" 18 min. 4 min. 8 min.
Art. "Specific" 32 min. 11 min. 14 min.
Art.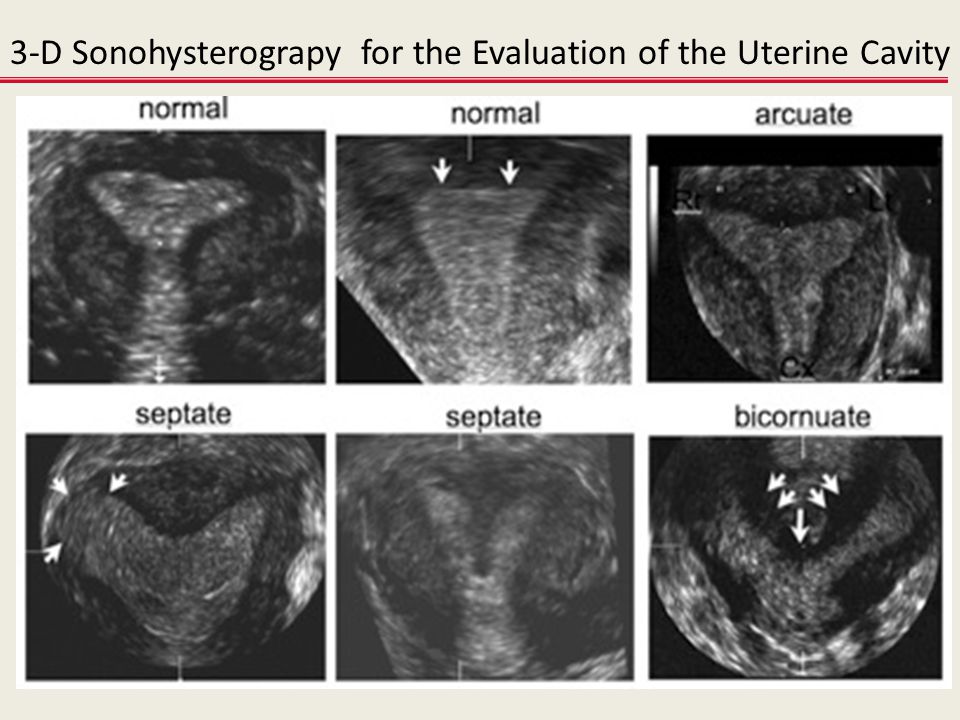 "Commandant Avenue" 24 min. 30 min.
"Commandant Avenue" 24 min. 30 min.
Art. "Polytechnic" 24 min. 30 min.
Art. "Civil Prospect" 17 min. 27 min.
What to do after a miscarriage
If a woman has a miscarriage, it is important to take competent measures to restore health. This will help to cope mentally and prepare the ground for a new pregnancy. According to medical statistics, 15-20% of pregnancies end in spontaneous termination for various reasons. The symptoms of what happened rarely go unnoticed, which makes it possible to diagnose the pathology in time, consult a gynecologist, undergo adequate treatment and plan the birth of a child for the future.
Experts classify spontaneous abortion into two categories:
1. Termination of biochemical pregnancy - the embryo leaves the uterine cavity in the first or third weeks after conception. A woman during this period most often does not suspect that she is carrying a child. Pregnancy becomes known only when testing for the content of hCG in the urine and blood. The blood that has left the body is usually perceived as menstruation, which, for unknown reasons, began outside the scheduled time. Units who carefully monitor their health go to the doctor.
Pregnancy becomes known only when testing for the content of hCG in the urine and blood. The blood that has left the body is usually perceived as menstruation, which, for unknown reasons, began outside the scheduled time. Units who carefully monitor their health go to the doctor.
2. Spontaneous abortion or miscarriage in early pregnancy - up to 22 weeks, when the weight of the embryo does not reach 0.4 kg.
What is a miscarriage like? If parts of the fetus remain in the uterus, they speak of an incomplete miscarriage, which occurs more often in the early stages of pregnancy. To neutralize the negative consequences, to prevent the development of an infectious process in the tissues, the product of conception is evacuated from the uterine cavity by the methods of medical interruption, gynecological curettage, and vacuum aspiration. Therapy may include the use of drugs aimed at contracting the uterus and pushing the contents out. Ultrasound examination is considered to be the control method of diagnostics.

Why the body rejects the embryo
The causes of miscarriage often lie in the presence of chromosomal abnormalities in the fetus. Among the factors provoking rejection of embryos are also:
- Heredity and genetic failure at the stage of fertilization of the egg by the sperm.
- A non-viable fetus may appear as a result of various risk factors - environmental conditions, occupational hazards, viral illness of parents. It is impossible to neutralize these factors. The only way out of the situation is to reduce the likelihood of their manifestation by protecting the expectant mother from dangers during gestation.
- Hormonal imbalance caused by disruption of the endocrine system. The situation can be affected by an insufficient amount of progesterone in the mother's body or an excess of testosterone. With early detection of a failure of the hormonal system, a woman undergoes specially organized therapy before pregnancy.

- The presence of tumors , neoplasms in the pelvic organs.
- Isthmic-cervical insufficiency when the isthmus and cervix dilate prematurely, unable to cope with the increasing pressure caused by the growing fetus in the body.
- There is a risk of miscarriage in the presence of anomalies in the work of the cardiovascular and renal systems.
- Drug addiction , alcohol addiction, substance abuse of mother and father.
- Depressive conditions , stress, nervous stress of a pregnant woman.
- Mechanical stress , blows, bruises, excessive physical labor of the future woman in labor.
- X-ray examination - radiation can cause miscarriage.
- Drug use . In the first trimester, you can not use potent medicinal formulas. Drugs can cause the development of defects in the embryo.
 Some decoctions of herbs are also contraindicated - parsley, tansy, cornflower, nettle, St. John's wort. It is forbidden to self-medicate. Each drug is agreed with the attending physician.
Some decoctions of herbs are also contraindicated - parsley, tansy, cornflower, nettle, St. John's wort. It is forbidden to self-medicate. Each drug is agreed with the attending physician. - Infectious and viral process in the body. Any sexually transmitted infection can provoke a miscarriage, which must be cured before pregnancy, otherwise there is a high risk of infection of the fetus in the womb. A great threat of miscarriage in the early stages exists due to viral infections and inflammation of the internal organs. A dangerous symptom is the high temperature of the mother, accompanied by intoxication of the body. At the stage of pregnancy planning, it is important to stop chronic diseases.
- History of abortion , unsuccessful surgery, unprofessionalism of the doctor and unfortunate circumstances.
- Immunological factors .
The list of causes of miscarriage in the early stages of pregnancy and in the later period may be more extensive, in each case, doctors identify the pathology individually.
Isthmic-cervical insufficiency (ICI)
One of the most common causes of spontaneous miscarriage during pregnancy is CCI - dilatation of the cervix and isthmus of the uterus as a result of increasing pressure from the growing fetus. Pre-pregnancy manipulations with the uterus (cervical dilation due to abortion, childbirth or curettage) affect the condition of the muscle ring. Damaged areas are tightened by scar tissue that does not have elasticity, is not amenable to stretching and contraction. ICI also has a functional nature when there is a hormonal imbalance.
ICI occurs in the period from the 11th to the 27th week after conception, when the embryo begins to produce androgens in the mother's body with the launch of the adrenal glands. Taking into account the mother's hormones, their indicator can be exceeded - this softens the cervix, opens and shortens it. Harmful bacteria and microorganisms penetrate into the formed channel, infecting the fetal egg. The initial stages of ICI do not have obvious symptoms, since they do not entail the tone of the uterine muscles. With the loss of strength of the membranes, amniotic fluid pours out. There are no pain sensations.
With the loss of strength of the membranes, amniotic fluid pours out. There are no pain sensations.
If a woman has had a miscarriage that started with amniotic fluid, she should report it to her doctor when monitoring a subsequent pregnancy.
Treatment of isthmic-cervical insufficiency
Endocrine disorders are corrected by prescribing hormonal drugs. An assessment of the condition of the uterus is carried out by a doctor a couple of weeks after the start of taking medications. They say about positive dynamics when the opening is suspended and no further expansion of the neck is observed. In the absence of the planned effect, surgical intervention is prescribed. Similar measures are used for the traumatic nature of the neck deformity. You should not be afraid of the operation, the doctor acts delicately, without causing additional injuries to the patient, without causing discomfort to the baby growing in the womb. The procedure is most effective in the early stages of pregnancy. Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity.
Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity.
Surgical intervention takes place in a hospital. Before the operation, the pregnant woman is examined. After the procedure, the vagina is sanitized, for which the suturing site is treated with chlorhexidine and furatsilin for three days. The patient needs to undergo a weekly follow-up examination with the attending physician, where he assesses the situation, making adjustments to the therapeutic protocol if necessary. The sutures are removed at the 38th week of pregnancy. During this time, the neck matures, preparing the birth canal for the passage of the fetus. Many women in labor worry that they will need a caesarean section if they have stitches, but this is not true. In most cases, women give birth on their own.
Immediate action is recommended if the amniotic sac prolapses (falls out) into the cervix between 16 and 24 weeks. The suturing of the neck obliges the woman to observe bed rest, strictly follow the daily routine, avoid physical exertion, and do not skip taking medications. In rare cases, complications occur. Among them, the eruption of sutures through the tissues, provoked by the frequent tension of the muscles of the uterus. To prevent tone, tocolytics are prescribed - medicines to prevent premature birth. The expectant mother should be prepared for frequent examinations and smears, which may be caused by the likelihood of accumulation of pathological microflora on the suture threads.
In rare cases, complications occur. Among them, the eruption of sutures through the tissues, provoked by the frequent tension of the muscles of the uterus. To prevent tone, tocolytics are prescribed - medicines to prevent premature birth. The expectant mother should be prepared for frequent examinations and smears, which may be caused by the likelihood of accumulation of pathological microflora on the suture threads.
It is also important to conduct psychological therapy, where a woman is taught relaxation techniques. The behavior of the future mother is a decisive factor in the successful bearing of the fetus in case of pregnancy complications. Panic and fuss create an unfavorable prognosis in stabilizing the situation. If a spontaneous abortion occurred for reasons of ICI, when you can get pregnant after a miscarriage, the doctor will say. Ideally, the period should be at least two years. The specialist must also take measures to prevent a repeated situation of losing a child.
In addition to the suture, ICI correction is also carried out using an obstetric pessary. An alternative method is the imposition of a special ring of hypoallergenic materials on the cervix. Silicone is the most commonly used. The ring creates additional support, preventing the opening of the neck.
Uterine hypertonicity - risk prevention
Uterine contractions before natural delivery is called hypertonicity. The condition is not an independent disease, it signals a malfunction in the body, often manifesting itself in the early stages of pregnancy. The causes of the pathological phenomenon are:
- Hormonal disorders caused by insufficient function of the placenta, ovaries, problems with the adrenal glands, causing imbalance.
- Genital infantilism , organ defects.
- Neoplasms , tumors in the uterus that are not necessarily malignant (eg, fibroids).
- During pregnancy infectious processes, viral diseases.

- CCI - opening of the neck under increasing pressure created by the growing embryo.
- Immunological problems .
- Chronic diseases of the body (cardiovascular disorders, renal insufficiency).
- Past miscarriages early pregnancy, symptoms of which may recur, induced abortions.
In addition to physiological causes, psychological factors are of no small importance. A woman who is in a depressed state can provoke hypertonicity in herself.
You can feel the tension of the muscles of the uterus on your own, without the help of a specialist. This is evidenced by the heaviness that appears in the lower abdomen, pulling pains in the lumbar region. Symptoms are similar to painful menstruation. Arising in the first trimester, the condition provokes spontaneous abortion, missed pregnancy, death of the fetal egg. In the subsequent period, premature birth due to hypertonicity is likely.
Why does the tension of the walls of the uterus cause irreversible consequences? The reason is the disturbed blood supply to the placental tissues, the occurrence of hypoxia of the embryo and the slowdown in the development of the emerging child. Following the contraction of the muscles of the uterus, the placenta does not contract, which causes its detachment and provoking the release of the fetal bladder.
Hypertonicity is diagnosed during a scheduled visit to a specialist. Stabilization of the situation requires the appointment of sedative drugs and antispasmodics. A strengthening effect is provided by therapy with the inclusion of vitamin B6, magnesium. In most cases, the measures taken are sufficient to neutralize the risks. Self-treatment, which can cause irreversible consequences, is strictly prohibited. With hypertonicity, the main rule for a pregnant woman is calmness and lack of physical activity. Some women who have had a successful delivery say they "didn't get up" during their entire pregnancy. With hypertonicity, sexual intercourse is also excluded.
With hypertonicity, sexual intercourse is also excluded.
If the threat cannot be neutralized, hospitalization is recommended. It is especially dangerous when severe cramping pain is complemented by spotting. To lie down "for preservation" is an adequate measure in the struggle for the birth of a healthy and strong baby. In the hospital walls, a pregnant woman is prescribed a vaginal examination, ultrasound. If necessary, a woman takes urine and blood tests, checks the hormonal background, and is examined for the presence of STIs.
At the onset of labor activity before the 34th week, the condition is tried to be stabilized with tocolytics. The most dangerous period is from the 25th to the 28th week, when the woman is recommended the maximum possible bed rest. After that, the fetus has every chance of survival. In order to quickly form the pulmonary system of the embryo, allowing it to survive with an early birth, hormones are prescribed.
Having an unfavorable prognosis for miscarriage and the threat of miscarriage, it is necessary to take up prevention at the stage of conception planning.
Stages of spontaneous termination of pregnancy
There are certain signs that attract attention and divide the course of a miscarriage into specific stages:
Symptoms of miscarriage - how not to miss the threat
If there is a threat of miscarriage in the early stages, the following symptoms may occur: The pain may be monotonous or come in waves.
A woman who does not know how an early miscarriage occurs should listen to her inner state.
Should alert:
- spasmodic pain impulses;
- Drawing pain in the lumbar region.
In the later stages, the above symptoms are added:
- liquid discharge from the vagina, which may indicate damage to the amniotic sac;
- pain when urinating;
- internal bleeding, which warns of a deterioration in the general condition, fainting, dizziness, pallor of the skin. All this is an indication for emergency hospitalization of a pregnant woman.
The beginning of an abortion is characterized by more pronounced symptoms of a miscarriage - contraction-like pain, severe dizziness, loss of strength. Instead of smearing discharges, clot-like ones appear, abundantly manifested during movement. Pregnancy can be saved if the area of detachment of the fetal egg is small and the fetal heartbeat is determined.
Instead of smearing discharges, clot-like ones appear, abundantly manifested during movement. Pregnancy can be saved if the area of detachment of the fetal egg is small and the fetal heartbeat is determined.
The third stage is useless for saving the fetus. There is girdle pain in the lower back and abdomen. Together with abundant blood loss, a fetal egg comes out of the uterus. Incomplete miscarriage requires curettage of the uterine cavity if parts of the embryo or membranes of the fetal egg remain in it, otherwise there is a high risk of complications that will endanger the life of the mother.
In rare cases, complications and serious health consequences can occur after a spontaneous abortion. But in the majority of situations, the body independently copes with what happened, expelling the parts remaining in the uterine cavity with a natural contraction of the muscles. An early spontaneous miscarriage does not always occur, a dangerous condition can also occur in the later stages. Some women try to provoke the release of the fetus with decoctions of herbs and medications. This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible.
Some women try to provoke the release of the fetus with decoctions of herbs and medications. This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible.
Methods of diagnosis
Symptoms of a threatened miscarriage at an early stage will be determined by a doctor during a visit to the antenatal clinic. The specialist will check the size of the uterus, determine the tone of its muscles, the condition of the cervix, and examine the discharge from the genital organs. A reliable method to identify the existing threat is transvaginal ultrasound diagnostics. The doctor draws attention to segmental muscle contractions of the uterus, detachment of the fetal egg. Genetic testing will help analyze the likely causes of a miscarriage. The patient's history is carefully collected.
Medical therapy
Any method is useful to maintain pregnancy. A qualified doctor develops an individual treatment protocol based on the available diagnostic data. Drugs used may include:
Drugs used may include:
- sedatives;
- restorative therapy;
- hormonal stabilizing drugs;
- uterine antispasmodics;
- vitamin and mineral supplements.
The specialist eliminates the threat of miscarriage in the early stages, tells how to prevent a relapse. In the later stages, the cervix is fixed with a special suturing (usually for a period of 16-25 weeks, if there is an ICI).
In case of an unsuccessful attempt to stop a spontaneous abortion, the following treatment tactics are used:
- Waiting - an organism that has freed itself from an embryo does not require specialized treatment.
- Drug therapy - the patient is prescribed drugs that complete the removal of foreign tissues from the body. By causing severe spasms of the muscular walls of the uterus, the tablets provoke the expulsion of residues from the cavity.
- Surgery - is used in case of complications or inconvenient for the independent exit of the fetus, the bending of the uterus.

Curettage
Having symptoms of a miscarriage in early pregnancy and faced with the need for a curettage (gynecological cleansing), a woman worries about the state of her reproductive system. It is not worth doing this, the operation takes place in a gentle mode, with maximum delicacy in relation to the patient's childbearing ability. Curettage is performed when there is a risk of incomplete exit of the embryo from the uterine cavity and the development of infection in the pelvic organs due to the elements remaining in it. Ignoring the procedure can lead to blood poisoning and the formation of a pathology that prevents re-conception.
Vacuum aspiration, however, is performed more frequently, which is more gentle. The complex application of the method with hysteroscopy allows you to carefully examine the internal contents of the uterus in order to prevent poorly cleaned areas on the mucous membrane.
Preparation for gynecological cleaning (curettage)
Gynecological cleaning is performed for diagnostic and therapeutic purposes for various indications :
- after childbirth;
- in missed pregnancy, miscarriages;
- for menstrual irregularities;
- for accurate diagnosis of gynecological disorders.
Curettage is recommended a few days before the onset of menstruation. In this case, blood loss decreases and a favorable prognosis is given for rapid tissue recovery. The operation requires a preliminary examination, testing. This is :
- complete blood count;
- blood coagulation test;
- smear for examination of the bacteriological environment;
- analysis for STIs.
Before curettage, you stop taking any medications, dietary supplements that have not been discussed with a specialist. Even plant components that can affect blood clotting and provoke blood loss during surgery can be dangerous. Your healthcare provider should be made aware of the medications you are taking so that they know what risks may arise.
Rules for preparing for the procedure:
- refrain from sexual intercourse three days before the operation;
- avoid the use of intimate hygiene products (gels, creams, ointments, liquids), suppositories, tablets and vaginal sprays;
- Do not douche;
- 10 hours before surgery, do not eat, drink.
 This is necessary for high-quality anesthesia.
This is necessary for high-quality anesthesia.
Cleaning
Curettage is carried out in a hospital, the woman is placed on the gynecological chair of the operating room. The doctor removes the upper layer of the mucous lining the uterine cavity from the inside. The exclusion of pain involves anesthesia. If there were signs of miscarriage in the early stages of pregnancy or at a later period, after which it spontaneously terminated, the dilated cervix allows for curettage without anesthesia. For anesthesia, intravenous administration of the drug is used, selected individually, taking into account the characteristics of the patient's body. A few seconds after the injection, the woman falls into a shallow sleep, the discomfort disappears, which makes the doctor's actions painless.
A dilator inserted into the cervix straightens the walls of the organ, facilitating access to the internal cavity. Holding the neck, the specialist inserts a rounded probe with a small diameter, after which he replaces it with a more voluminous analogue. A special video camera attached to the end of the probe allows for hysteroscopy - examination of the cavity before curettage. Cleaning is done with a curette, shaped like a small spoon on a long handle. Carefully collected tissues are stored in a specialized sterile tube, which is later sent to the laboratory for histological examination.
A special video camera attached to the end of the probe allows for hysteroscopy - examination of the cavity before curettage. Cleaning is done with a curette, shaped like a small spoon on a long handle. Carefully collected tissues are stored in a specialized sterile tube, which is later sent to the laboratory for histological examination.
The procedure rarely takes more than one hour, usually 20 minutes is enough for the doctor. Together with the cavity, the cervical canal is cleaned. Manipulations are called RDV - separate diagnostic curettage. Collected samples are placed separately. Histology is used to identify the structure of tissues in order to exclude the presence of atypical cells in them, indicating cancerous lesions, precancerous conditions. The study is carried out within two weeks, after receiving the results, the woman revisits the gynecologist for a follow-up examination.
Curettage is often carried out for diagnostic purposes to determine the symptoms of pathological conditions in the functioning of the organs of the reproductive system. These can be:
These can be:
- irregular cycle;
- voluminous discharge and painful menstruation;
- bleeding during menopause;
- difficulties in conception in the absence of visible causes of pathology;
- suggestion of developing uterine cancer.
Possible complications
Complications can occur, as after any surgical intervention. A serious consequence is the discovery of uterine bleeding. In order to prevent it, oxytocin is used - injections stimulate the cessation of abnormal blood flow. Oxytocin will help if the bleeding is due to insufficient contraction of the uterus. In violation of blood clotting, it is ineffective.
Another complication of is hematometra, when blood clots accumulate in the uterine cavity, which can cause an inflammatory process in the tissues. It is caused by a spasm of the cervix that occurred immediately after cleaning, which interferes with the evacuation of blood. Experts recommend the use of antispasmodics that relax the muscles of the organ and contribute to the normal outflow of blood. A woman should be alerted by pulling pains in the lower abdomen and a sharp cessation of discharge.
Experts recommend the use of antispasmodics that relax the muscles of the organ and contribute to the normal outflow of blood. A woman should be alerted by pulling pains in the lower abdomen and a sharp cessation of discharge.
After cleansing, endometritis may occur when inflammation affects the lining of the uterus. A measure of therapy for a dangerous diagnosis is a course of antibiotics. Pain in the abdomen and a sharp increase in body temperature testify to the pathology. Any dangerous change in condition should be reported to the doctor immediately. In this case, countermeasures will be taken in a timely manner, which will eliminate the risks of developing more formidable complications.
How to behave after a miscarriage
A miscarriage that has occurred requires a certain tactic of behavior. Among the measures recommended by doctors:
- It is advisable to postpone a new pregnancy attempt for 3-6 months . Otherwise, the risk of repeating the undesirable development of events is high.
 If pregnancy occurs before the expiration date, there is no need to panic. The main thing is the supervision of a specialist.
If pregnancy occurs before the expiration date, there is no need to panic. The main thing is the supervision of a specialist. - If you are waiting for , ask for advice on effective contraception.
- Follow your doctor's advice .
- Pass the necessary examinations , take tests.
Consult what effect the medicines you take will have on the fetus if you become pregnant during therapy. Find out after what period of time you can fearlessly try to conceive a child.
How to detect genetic pathologies during repeated pregnancy
If a miscarriage of the first pregnancy occurs due to a genetic factor, it is especially scary to decide on a second one. But you should not be afraid of this, with a well-designed therapy, the chances of success are more than great. Diagnostic procedures today are highly accurate and allow you to identify pathology in the early stages. Examination in this case is mandatory, as well as the following:
- who are over 35;
- has screening changes;
- who had markers of chromosomal pathologies and malformations of the embryo;
- who already have children with chromosomal abnormalities.

Ultrasound diagnostics can detect malformations in 80-85% of cases. However, the technology is not impeccably reliable, as it misses pathologies in 20% of situations. Biochemical screening, invasive examinations have valid data. The latest version of the study allows you to identify up to 99% anomalies. No less popular is the high-precision PANORAMA test for determining DNA pathologies.
When planning a new pregnancy, it is imperative to visit a geneticist. Screening diagnostics for the detection of abnormal genes will help eliminate the risks of possible pathologies, the factor of heredity and genetic failure during conception. Sometimes the threat of miscarriage in the early stages exists in almost healthy carriers. The examination will allow you to find out about the anomaly in advance and undergo treatment.
Planning a new pregnancy
The medical community is unanimous in the issue of planning a new pregnancy after a spontaneous abortion. Conception is not recommended for at least 3-6 months. During this period, the woman's body will recover and gain strength to bear the fetus. Observation by a doctor, harmonization of hormonal levels, examination of parents to identify possible pathologies are important. In order not to become pregnant in the first months, it is recommended to use contraceptive methods prescribed by your doctor.
During this period, the woman's body will recover and gain strength to bear the fetus. Observation by a doctor, harmonization of hormonal levels, examination of parents to identify possible pathologies are important. In order not to become pregnant in the first months, it is recommended to use contraceptive methods prescribed by your doctor.
Examination after a miscarriage includes blood and urine tests, examination of the microflora of the vagina with a smear, detection of overt and latent genital infections, glucose and hormone testing, examination of partners for biological compatibility. Planning is an important step towards having a healthy baby. After the studies, the woman is prescribed strengthening therapy. It is important to completely reconsider eating habits, to exclude factors that are harmful to well-being. Vitamins, folic acid are used. Fast food, food containing carcinogens and preservatives are excluded from the diet. Subject to the rules recommended by the doctor, a successful pregnancy with a favorable outcome is likely.
It is not uncommon for a pregnancy test to show two lines after a miscarriage. This is due to the restructuring of the body, the organs of the reproductive system. It is important to report the incident to your doctor. The presence of remnants of embryonic tissue in the uterus can provoke a positive test result. In this case, immediate curettage is necessary, which neutralizes the risk of inflammation and infection. To accurately determine her condition, a woman needs to undergo an ultrasound diagnosis, take tests to determine hCG in the blood.
The question of whether it is possible to get pregnant after a miscarriage worries many parents. The answer is unequivocal - yes, if you follow the recommendations of experts, carefully plan a new conception, monitor your well-being and state of your health.
Components of success after a miscarriage
Spontaneous abortion can provoke not only the health of the patient, but failure to follow simple rules can become a threat. To reduce the risk of losing a child during pregnancy, required:
To reduce the risk of losing a child during pregnancy, required:
1. Keep calm – it is important for a mother to exclude from her life all the factors that make her nervous. Irritation is not the best way to normalize the condition. In order to stabilize the emotional background, rest is recommended, the use of soothing teas with the permission of the doctor. Good results are given by decoctions of chamomile, lemon balm, mint.
2. Avoid taking unnecessary medicines and preparations. But it is unacceptable to stop the therapy prescribed by the doctor on your own. Each step must be discussed with the gynecologist.
3. Eliminate harmful occupational factors. Work in the chemical industry and other hazardous facilities can create an undesirable background in the body, which prevents normal gestation. It is important to understand what is of great value to the mother - the birth of a healthy baby or a career factor. Many refuse to work to increase the chance of having a baby.
Many refuse to work to increase the chance of having a baby.
4. Eliminate bad habits. It is unacceptable for a woman who has experienced miscarriage to drink alcohol and smoke. It is forbidden to do this and the future father. This negatively affects the quality of spermatozoa, provokes difficulties with conception and risks of deviations in the development of the embryo.
5. Take vitamin complexes, specially designed to prepare the body for pregnancy, the formation of basic conditions for its favorable course.
6. Eat right. A complete, balanced diet works wonders. With a lack of weight, a nutritionist will develop an adequate diet for a woman with the inclusion of a large amount of protein foods rich in vitamins and trace elements of vegetables, fruits, and cereals. Recommended fats contained in fish, seeds, nuts, avocados, olives.
7. Get rid of extra pounds. Obesity adversely affects the development of pregnancy. Science has proven that enhanced nutrition during this period is not required. The main thing is its balance.
Science has proven that enhanced nutrition during this period is not required. The main thing is its balance.
Infections during pregnancy
Infectious processes transferred before pregnancy develop immunity in the mother to similar agents of influence. Primary infection poses a great threat, so vaccination will be useful before planning conception. Perinatal diagnosis allows you to detect the infectious process at the initial stage and prevent its harmful effects. This is possible if the pregnant woman is registered from an early date.
Infection may develop due to an infection transmitted by airborne droplets. It is the most dangerous, since it is almost impossible to prevent it. This applies to mumps, measles, rubella. HIV and hepatitis infect the body through sexual contact, similar to chlamydia. Listeriosis is transmitted with poor-quality products. A pregnant woman can pass infections to a developing baby. Pathology is determined by profile tests of latent infection.
Routine pregnancy monitoring involves regular testing. Sexual infections are determined using a smear, ultrasound shows deviations in the development of the baby, and KGT is aimed at listening to the work of the fetal heart muscle. If there is a suspicion of a serious infection of the embryo, blood sampling from the umbilical cord and amniotic fluid analysis are practiced.
Infection of a child also depends on concomitant factors. The speed of diagnosis, the literacy of the treatment, the type of pathogen, the duration of the pregnancy are taken into account. The following infectious processes deserve special attention:
1. Viral etiology - a huge number of viruses pose a danger to a pregnant woman. The threat is genital herpes, rubella, infectious type erythema, cytomegalovirus, hepatitis B, measles, mumps, chickenpox.
2. Bacterial infections, detected during the analysis of biological materials (feces, urine, blood), examination of certain organs of the body. Active reproduction provokes a rapid growth in the number of bacteria in the vagina. Not all microorganisms pose a threat to the child. Dangerous candidiasis, streptococcus, chlamydia, bacterial vaginosis, cystitis.
Active reproduction provokes a rapid growth in the number of bacteria in the vagina. Not all microorganisms pose a threat to the child. Dangerous candidiasis, streptococcus, chlamydia, bacterial vaginosis, cystitis.
The successful course of pregnancy is threatened by intestinal infections, often activated in the summer. Their carriers can be animals and poorly processed food before consumption. Of particular danger are listeriosis, salmonellosis, toxoplasmosis.
Prevention of infections during pregnancy
Infection in the mother poses a threat to the life of the fetus. From the 3rd to the 12th week, the infected organism responds with a miscarriage or the formation of malformations of the child. From the 11th to the 25th - developmental delay. At a later date, organs are deformed and prerequisites for premature birth are created. In order to prevent intrauterine infection, it is recommended to apply a number of rules:
- be examined for the detection of STIs;
- examine blood, determine the presence of antibodies to infection carriers, pathogens;
- avoid contact with sick people, visits to crowded places where there is a possibility of infection by airborne droplets;
- examine domestic animals for dangerous infections, treat them if necessary, or remove them from the home until the threat is eliminated;
- exclude fast food, store-bought semi-finished products from the diet, subject meat and fish to thorough heat treatment;
- remove from the diet sushi and other culinary delights purchased in restaurants, cafes;
- thoroughly wash hands, fruits, vegetables with special disinfectants that are not capable of harming the pregnant woman and the child;
- it is planned to visit a gynecologist, undergo examinations recommended by a doctor, take tests, take vitamins;
- register at the first sign of pregnancy;
- prepare for conception, cure infections, vaccinate.

It is also important for the child's father to follow most of the recommended rules. If only the mother undergoes treatment, a relapse is likely during sexual intercourse, neutralizing the beneficial effect of therapy.
A woman who has had a miscarriage in the past should be alerted to any deviations from the norm in her state of health. It is important to pay attention to ailments, pain, weakness, dizziness. Accounting for an early consultation will create conditions for the bearing of the fetus and the birth of a child. There is no need to be afraid that a miscarriage will forever deprive the joy of motherhood.
Having completed a course of examinations, passing tests and following the measures prescribed by the doctor to treat imbalances in the body, you will create all the conditions for a favorable pregnancy outcome. Tune in to the positive, protect yourself from worries, worries, stress. Feel the support of loved ones, hope for the best! Get advice from good specialists to rule out any unfavorable prognosis before conception or take steps to neutralize them.