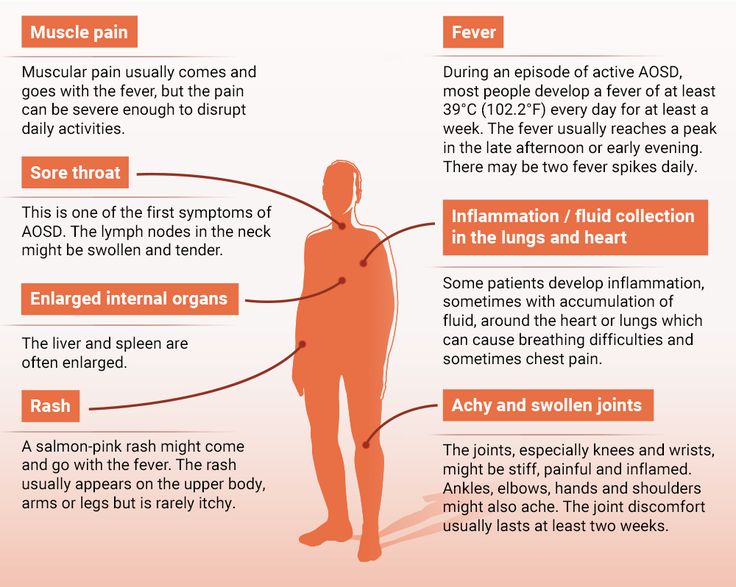
Types of children rashes
Skin rashes in children | NHS inform
Childhood rashes are common and aren't usually a cause for concern. Most rashes are harmless and disappear without the need for treatment.
However, see your GP if your child has a rash and seems unwell, or if you're worried. They'll be able to investigate the cause and recommend any necessary treatment.
This page may give you a better idea about what could be causing the rash, but don't use this to self-diagnose your child's condition – always see a GP for a proper diagnosis.
The most common causes of rashes in children are:
- cellulitis
- chickenpox
- eczema
- erythema multiforme
- hand, foot and mouth disease
- impetigo
- keratosis pilaris ("chicken skin")
- measles
- molluscum contagiosum
- pityriasis rosea
- prickly heat
- psoriasis
- ringworm
- scabies
- scarlet fever
- slapped cheek syndrome
- urticaria (hives)
Although meningitis has become less common over recent years, it's important to be aware of the rash and the other signs and symptoms of meningitis.
Cellulitis
Cellulitis is an infection of the deeper layers of skin and underlying tissue. The affected area will be red, painful, swollen and hot. It often affects the legs, but can occur anywhere on the body. Your child will probably also have a fever.
See your GP immediately if an area of your child's skin suddenly turns red, hot and tender. If you can't see your GP on the same day, go to a walk-in centre or minor injuries unit.
Cellulitis can usually be diagnosed by assessing the symptoms and examining the skin. It usually responds well to treatment with antibiotics.
Chickenpox
Chickenpox is a viral illness that most children catch at some point. It most commonly affects children under 10 years of age.
A rash of itchy spots turns into fluid-filled blisters. They crust over to form scabs, which after a while drop off. Some children only have a few spots, whereas others have them over their entire body. The spots are most likely to appear on the face, ears and scalp, under the arms, on the chest and belly, and on the arms and legs.
There's no specific treatment for chickenpox, but you can take steps to relieve the symptoms. For example, paracetamol can help relieve fever (don't give aspirin to children under 16), and calamine lotion and cooling gels can be used to ease itching.
Read more about treating chickenpox.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked. The most common type is atopic eczema, which mainly affects children but can continue into adulthood.
Atopic eczema commonly develops behind the knees or on the elbows, neck, eyes and ears. It isn't a serious condition, but if your child later becomes infected with the herpes simplex virus, it can cause the eczema to flare up into an outbreak of tiny blisters called eczema herpeticum, and will cause a fever.
About one in five children in the UK has eczema, and in eight out 10 cases it develops before the age of five, often before a child's first birthday.
Read about treating atopic eczema.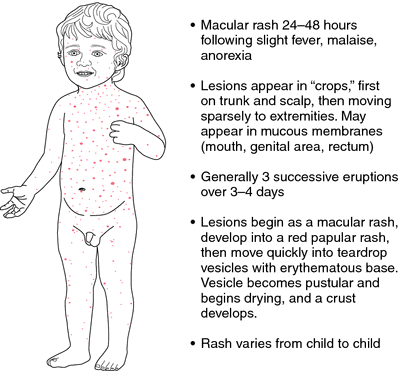
Erythema multiforme
Erythema multiforme is a skin rash (usually mild) that's caused by an allergic reaction to the herpes simplex virus.
The spots look like targets, with a dark red centre and paler ring around the outside. The hands or feet tend to be affected first, followed by the limbs, upper body and face.
Your child will probably feel unwell and may have a fever, which you should be able to treat with over-the-counter medicine. It may take from two to six weeks before they feel better. See your GP if your child has a rash and seems unwell.
In rare cases, erythema multiforme can be triggered by a reaction to certain medications, such as an antibiotic or anticonvulsant. This more severe form is called Stevens-Johnson syndrome and it can be life-threatening.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, contagious infection that causes mouth ulcers and spots and blisters on the palms of the hands and soles of the feet.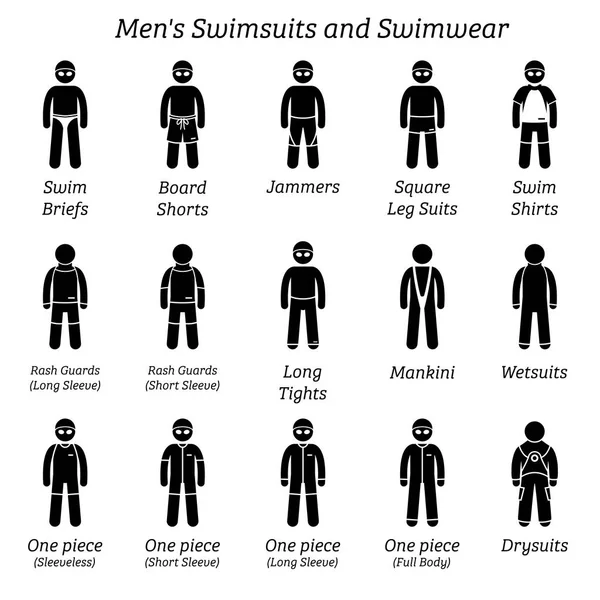
It's most common in young children (particularly those under 10), but it can also affect older children and adults.
There's no cure for hand, foot and mouth disease and it's easily spread, so you should keep your child away from school or nursery until they're better. Your child's immune system will fight the virus and it should clear up after about seven to 10 days.
Make sure your child drinks plenty of fluid, and if eating and swallowing is uncomfortable, give them soft foods, such as mashed potatoes, yoghurt and soup.
Impetigo
Impetigo is a common and highly contagious skin infection that causes sores and blisters. It isn't usually serious and often improves within a week of treatment. There are two types of impetigo called non-bullous and bullous.
Non-bullous impetigo typically affects the skin around the nose and mouth, causing sores that quickly burst to leave a yellow-brown crust.
Bullous impetigo typically affects the trunk (the area of the body between the waist and neck), and causes fluid-filled blisters that burst after a few days to leave a yellow crust.
See your GP or pharmacist if you think your child has impetigo. Antibiotics, in the form of a cream or tablets, will be prescribed. This should reduce the length of the illness to around seven to 10 days.
Keratosis pilaris ("chicken skin")
Keratosis pilaris is a common and harmless skin condition. The skin on the back of the upper arms becomes rough and bumpy, as if covered in permanent goose pimples. Sometimes, the buttocks, thighs, forearms and upper back can also be affected.
Keratosis pilaris typically begins in childhood and gets worse during puberty. Some people find it improves after this and may even disappear in adulthood.
There's no cure for keratosis pilaris, and it often gets better on its own without treatment. However, there are some measures you can take that may improve your child's rash, such as using non-soap cleansers rather than soap, and an emollient to moisturise their skin. Your GP or pharmacist will be able to recommend a suitable cream.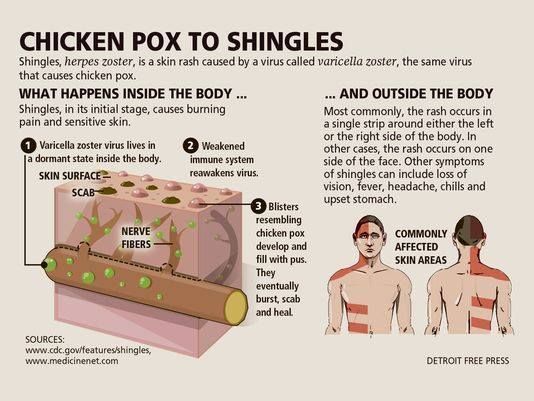
Measles
Measles is a highly infectious illness that most commonly affects young children. It's now rare in the UK because of the effectiveness of the measles, mumps and rubella (MMR) vaccine.
The measles rash is red-brown blotches. It usually starts on the head or upper neck and then spreads outwards to the rest of the body. Your child may also have a fever and cold-like symptoms.
Call your GP surgery immediately if you think your child has measles. It's best to phone before visiting because the surgery may need to make arrangements to reduce the risk of spreading the infection to others.
Measles usually passes in about seven to 10 days without causing further problems. Paracetamol or ibuprofen can be used to relieve fever, aches and pains (don't give aspirin to children under 16). Also, make sure your child drinks plenty of water to avoid dehydration.
Read more about treating measles.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that causes clusters of small, firm, raised spots to develop on the skin.
It commonly affects young children aged one to five years, who tend to catch it after close physical contact with another infected child.
The condition is usually painless, although some children may experience some itchiness. It usually goes away within 18 months without the need for treatment.
Molluscum contagiosum is highly infectious. However, most adults are resistant to the virus, which means they're unlikely to catch it if they come into contact with it.
Pityriasis rosea
Pityriasis rosea is a relatively common skin condition that causes a temporary rash of raised, red scaly patches to develop on the body. Most cases occur in older children and young adults (aged between 10 and 35).
The rash can be very itchy. In most cases, it clears up without treatment in 2 to 12 weeks, although in rare cases it can last up to five months.
Emollients, steroid creams and antihistamines can be used to help relieve the itchiness. The rash doesn't usually leave scars, although the skin can sometimes be discoloured afterwards.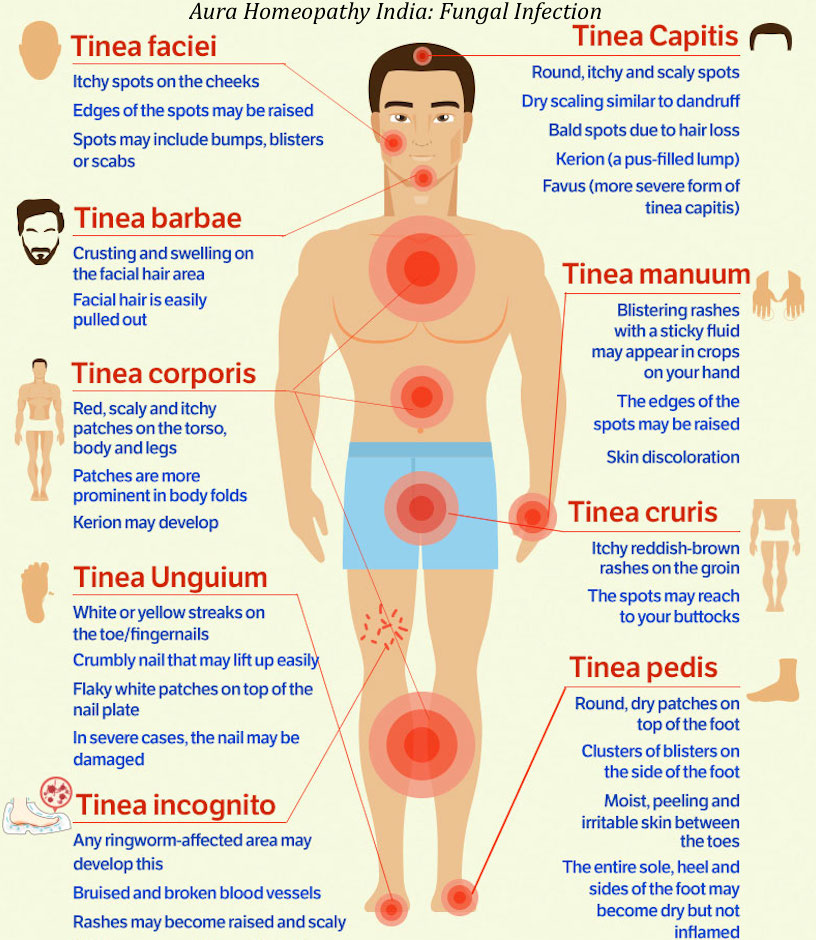
Prickly heat (heat rash)
Prickly heat (heat rash), also known as miliaria, is an itchy rash of small, raised red spots that causes a stinging or prickly sensation on the skin.
It occurs when the sweat ducts in the outer layer of skin (epidermis) are obstructed. You can get a heat rash anywhere on your body, but the face, neck, back, chest or thighs are most often affected.
Infants can sometimes get a prickly heat rash if they sweat more than usual – for example, when it's hot and humid or if they're overdressed. It isn't a serious condition and rarely requires any specific treatment.
Psoriasis
Psoriasis is a long-lasting (chronic) skin condition that causes red, flaky, crusty patches of skin covered with silvery scales.
The severity of psoriasis varies greatly from person to person. For some people, it's just a minor irritation, but for others it can have a major impact on their quality of life.
There's no cure for psoriasis, but there are a number of treatments that can help improve the symptoms and appearance of skin patches.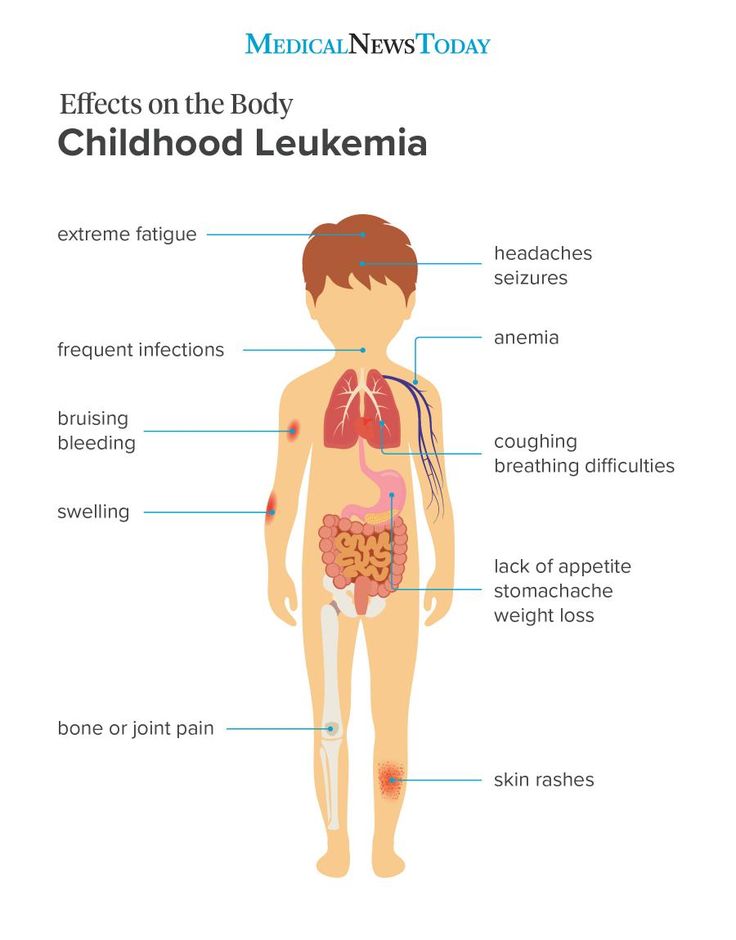 For example, topical corticosteroids are creams and ointments that can be applied to the skin.
For example, topical corticosteroids are creams and ointments that can be applied to the skin.
Ringworm
Ringworm is a highly infectious fungal skin infection that causes a ring-like red or silvery patch on the skin that can be scaly, inflamed or itchy.
Ringworm often affects the arms and legs, but it can appear almost anywhere on the body. Other similar fungal infections can affect the scalp, feet, groin and nails.
Ringworm can usually be easily treated with antifungal medicines, which are available from a pharmacy. Ringworm of the scalp can cause scaling and patches of hair loss. It's treated with antifungal tablets, often combined with antifungal shampoo.
Scabies
Scabies is a contagious skin condition that's intensely itchy. It's caused by tiny mites that burrow into the skin.
In children, scabies is usually spread through prolonged periods of skin-to-skin contact with an infected adult or child – for example, during play fighting or hugging.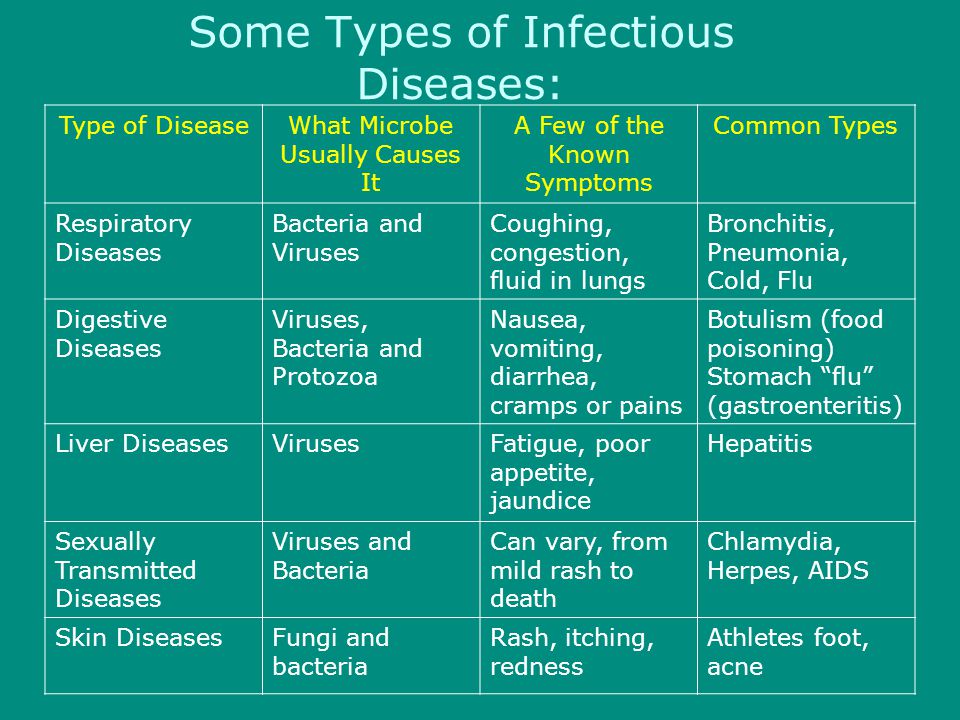
The mites like warm places, such as skin folds, between the fingers, under fingernails, or around the buttock creases. They leave small red blotches, which are often found on the palms of the hands or soles of the feet. In infants, blisters are commonly found on the soles of the feet.
See your GP if you think your child has scabies. It's not usually a serious condition, but it does need to be treated. Your GP will prescribe a lotion or cream. Read more about treating scabies.
Scarlet fever
Scarlet fever is a highly contagious bacterial infection that usually affects children between two and eight years of age. It causes a distinctive pink-red rash, which feels like sandpaper to touch and may be itchy.
It often starts with a sore throat, fever and headache, with the rash developing two to five days after infection. The rash usually occurs on the chest and stomach before spreading to other areas of the body, such as the ears and neck.
Scarlet fever usually clears up after about a week, but see your GP if you think your child may have it.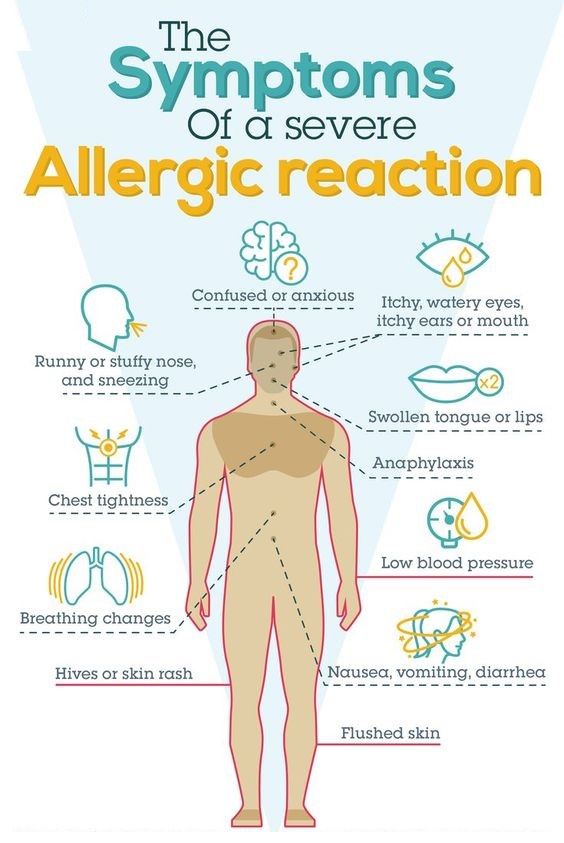 Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Slapped cheek syndrome
Slapped cheek syndrome – also known as fifth disease or parvovirus B19 – is a viral infection that's common in children aged six to 10.
It causes a distinctive bright red rash to develop on both cheeks. This can look alarming, but it usually clears up by itself in one to three weeks.
Unless your child is feeling unwell, they don't need to stay away from school. Once the rash appears, the infection is no longer contagious. However, it's a good idea to notify your child's school about the infection.
Urticaria (hives)
Urticaria – also known as hives, weals, welts or nettle rash – is a raised, itchy rash that can affect one part of the body or be spread across large areas. It's a common skin reaction that often affects children.
Urticaria occurs when a trigger causes high levels of histamine and other chemical messengers to be released in the skin.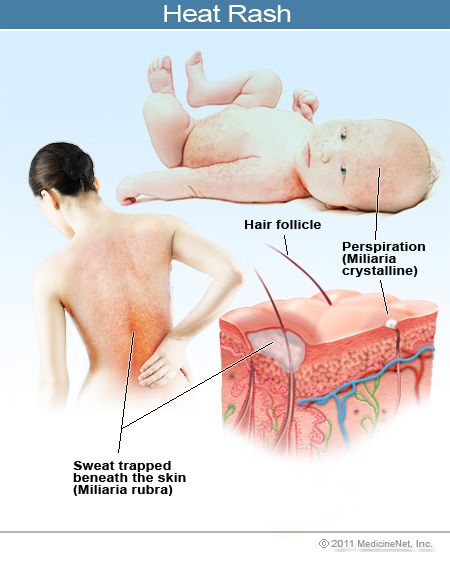 These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
There are many possible triggers of urticaria, including allergens, such as food or latex, irritants, such as nettles, medicines, and physical factors, such as heat or exercise. Sometimes, a cause can't be identified.
The rash is usually short-lived and mild, and can often be controlled with antihistamines.
Nappy rash - NHS
Nappy rash is common in babies and can usually be treated at home.
Check if your baby has nappy rash
Symptoms of nappy rash can include:
- red or raw patches on your baby’s bottom or the whole nappy area
- skin that looks sore and feels hot to touch
- scaly and dry skin
- an itchy or painful bottom
- your baby seeming uncomfortable or distressed
- spots, pimples, or blisters on bottom (spots can appear red or brown, but may be less noticeable on brown and black skin)
Credit:
HOUIN / BSIP / SCIENCE PHOTO LIBRARY: https://www. sciencephoto.com/media/615341/view
sciencephoto.com/media/615341/view
Things you can do to help with nappy rash
Nappy rash can be treated and prevented by following some simple advice.
Do
-
change wet or dirty nappies as soon as possible
-
keep the skin clean and dry – pat or rub the skin gently to dry it
-
leave nappies off when possible
-
use extra absorbent nappies
-
make sure your baby's nappies fit properly
-
clean your baby’s skin with water or fragrance-free and alcohol-free baby wipes
-
bath your baby daily (but not more than twice a day, as washing too much can make the skin dry out)
-
use olive oil to remove nappy rash ointment rather than water
Don’t
-
do not use soaps, baby lotion or bubble bath as they can irritate the skin
-
do not use talcum powder or antiseptics on nappy rash
-
do not put nappies on too tightly as it can irritate the skin
A pharmacist can help with nappy rash
If the rash is causing your baby discomfort, a pharmacist can recommend a nappy rash cream or medicine to treat it at home.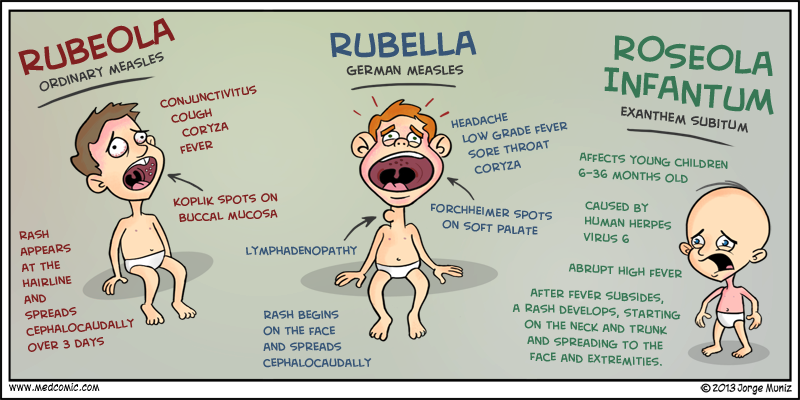
They may suggest using a thin layer of a barrier cream to protect the skin or giving your baby child's paracetamol for pain relief (only suitable for babies over 2 months old).
Non-urgent advice: See a health visitor or GP if:
- your baby's nappy rash does not go away, gets worse or spreads to other areas
- your baby has a high temperature
- your baby seems very uncomfortable
Treatment for nappy rash
A GP may prescribe treatment if your baby is in a lot of discomfort or they think your baby might have an infection.
They may prescribe:
- a steroid cream or ointment to help with redness and soreness
- an antifungal cream, if they think your baby has a thrush infection
- antibiotics, if they think your baby has a bacterial infection
Causes of nappy rash
It's normal for babies to sometimes get nappy rash.
It can be caused by:
- your baby's skin being in contact with pee or poo for a long time
- not cleaning the nappy area or changing the nappy often enough
- the nappy rubbing against your baby's skin
- an allergic reaction to soap, detergent or bubble bath
- irritation from fragranced baby wipes or wipes containing alcohol
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
- thrush (a fungal infection)
Page last reviewed: 1 January 2023
Next review due: 1 January 2026
Have you noticed a rash on your child's skin? Contact your pediatrician to find out the reason. Redness itself is not a disease, but can signal internal disorders in the body.
In the article we will talk about the causes, types and methods of treating rash in children.
What causes a rash?
Rashes on the skin of a child do not appear just like that. In any case, this is the body's immune response to the influence of external or internal factors. nine0003
Different types of rashes are similar in appearance, especially for parents who are faced with a problem for the first time. But if some spots are completely harmless, then others can threaten health. That is why it is important to understand their origin.
The main causes of the rash:
- Reaction to stimuli. If the child is dressed too warmly, the rash may be due to overheating and excessive sweating. Most often, prickly heat occurs on the back, neck, chest and abdomen. The same goes for the diaper. If you do not arrange air baths and do not change it to a new one in time, the skin in the inguinal region and on the buttocks will disappear.
 nine0020 Prickly heat does not require special treatment, it is only important to eliminate the irritating factor.
nine0020 Prickly heat does not require special treatment, it is only important to eliminate the irritating factor. - Physiological. In the first months of life, breastfed babies are often diagnosed with infantile acne. With milk, maternal hormones enter the body, which activate the sebaceous glands. As a result, small comedones and pimples appear on the face. Over time, they disappear.
- Viral and bacterial infections. Measles, chicken pox, rubella, herpes simplex virus, roseola, scarlet fever, meningococcal infection, fungus and streptoderma. These diseases are characterized by specific rashes on the arms, legs and other parts of the body. Many are accompanied by itching and a steady increase in body temperature for 3-5 days. nine0021
- Allergy. Urticaria and various types of atopic dermatitis: eczema, diathesis, neurodermatitis. Spots without suppuration may cover the head, face, shoulders, armpits, back and groin.
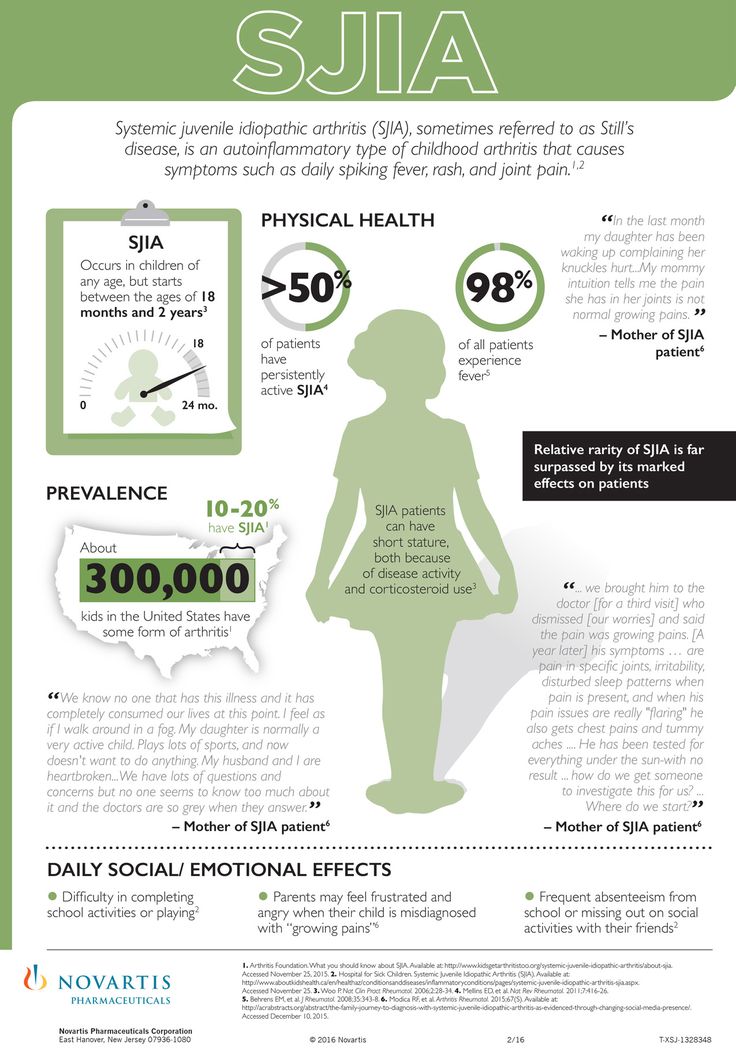
- Comorbidities. Rash may indicate gastrointestinal, vascular, or kidney problems.
Eruptions in children
Depending on the appearance, localization and size, the following types are distinguished:
- Tubercles. nine0017 Vesicles.
- Blisters.
- Purples.
- Pustules.
- Stains.
- Erythema.
Why are rashes dangerous?
With any kind of redness, it is important to consult a doctor to determine the cause. The most dangerous rash of viral and bacterial origin, especially if there are other symptoms:
- cough;
- sore throat;
- enlarged tonsils and lymph nodes;
- tearing; nine0021
- temperature increase.
Without timely treatment, complications are possible. For example, measles can lead to pneumonia, meningitis, and hearing loss.
With skin allergic reactions, it is important to determine the source of the problem. A neglected allergy can cause swelling and suffocation.
A neglected allergy can cause swelling and suffocation.
What should parents do?
If you find bumps, vesicles or redness on the child's body, proceed in sequence:
- examine the entire skin; nine0021
- estimate the area and number of lesions;
- check throat, tonsils and take temperature;
- remember what the child ate, did or touched before the redness appeared.
Is the baby already talking? Then try to figure out what's bothering him. Ask about the sensations (spots hurt, itch) and general well-being.
If you have a high temperature, call your doctor at home. It could be a contagious infectious disease that definitely shouldn't be spread. But even if the child looks healthy and vigorous, do not postpone a visit to a specialist - make an appointment at a medical facility. nine0003
It is strictly forbidden to self-medicate, comb or squeeze out neoplasms.
Diagnostics
Diagnostic measures help to choose the right therapy. First, the pediatrician prescribes to small patients:
First, the pediatrician prescribes to small patients:
- analysis of blood, urine and feces;
- skin scrapings;
- collection of exudate samples, in the presence of watery formations.
Based on the results, the doctor makes a preliminary conclusion and sends the parents with the child for examination to narrow specialists: an allergist, dermatologist, endocrinologist or gastroenterologist. nine0003
Treatment
Treatment of rashes is carried out in a complex way to eliminate both the symptoms and the cause. A young patient is prescribed anti-allergic, anti-inflammatory or hormonal drugs in the form of tablets, ointments or suspensions.
Along with this, parents are advised to reconsider nutrition and living conditions:
- exclude potentially allergenic products;
- use gentle detergents for the body, dishes and laundry; nine0017 wear loose clothing made from natural fabrics;
- dress the child according to the weather, do not wrap too tightly to avoid overheating;
- change the diaper in a timely manner, arrange air baths and lubricate the groin area with a special cream.

Conclusion
Rashes in a child are a common problem that can bother from birth. Innocent at first glance spots are sometimes a sign of a serious illness. Consult a doctor to determine the cause in time and start treatment. nine0003
GET PRICES
Types of baby rashes: instructions for parents
Anna Devyatukhina
Journalist, author Daily Baby
#skin rashes #health #children #rash
The appearance of rashes in a child is often not perceived by parents as a serious reason to see a doctor. Often, mothers and fathers attribute the rash to an allergy, but there are more than a hundred reasons for its occurrence - alas, not all of them are harmless. The author of The Daily Baby prepared instructions for parents: how to determine what kind of rash attacked the child, how dangerous it is and when to run to the doctor. nine0003
From prickly heat to severe infection
Children's skin is incredibly delicate, so redness and rashes often appear on it.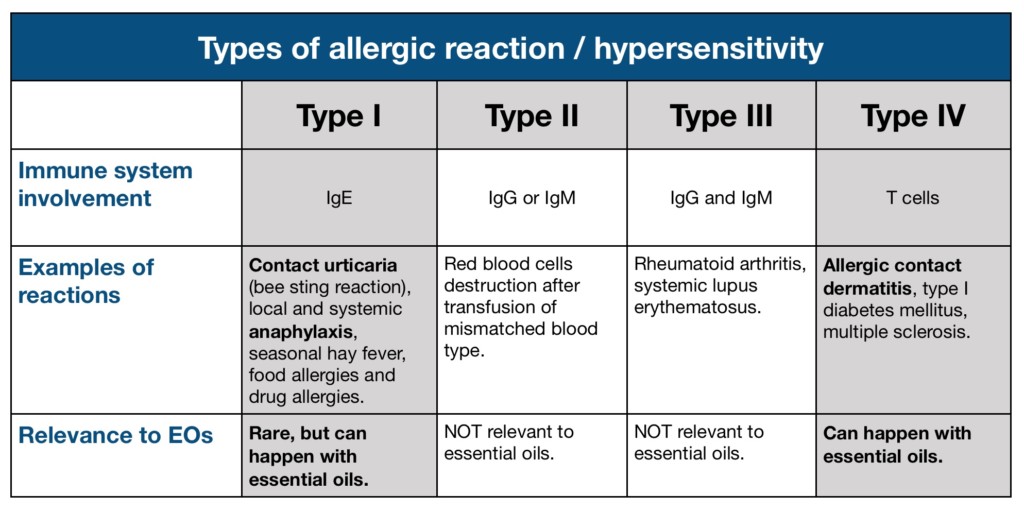 External changes in the skin, of course, signal some kind of malfunction in the body.
External changes in the skin, of course, signal some kind of malfunction in the body.
- There are dozens of various types of skin rashes. Among them, there are dangerous ones that require an emergency visit to a pediatrician, and there are those that can be observed at home, without a doctor.
The most important thing is to learn how to identify a hemorrhagic rash. This type always requires a doctor's consultation on the same day. Especially if the child has a temperature. nine0003
Hemorrhagic rash - one that will not disappear if you press on it with a glass. This rash looks like this: like a hemorrhage into the skin. It can be very small, the size of a dot, or it can cover the skin with large spots. Regardless of the size, we need a doctor and urgently,” says Anna Ganina, mother of three children, pediatrician at the Family Doctor clinic, Kemerovo.
Pediatrician of the mobile clinic DOC+ Natalia Makarova notes: the rash itself is not a disease, it is a symptom of some disease or a reaction to an external irritant.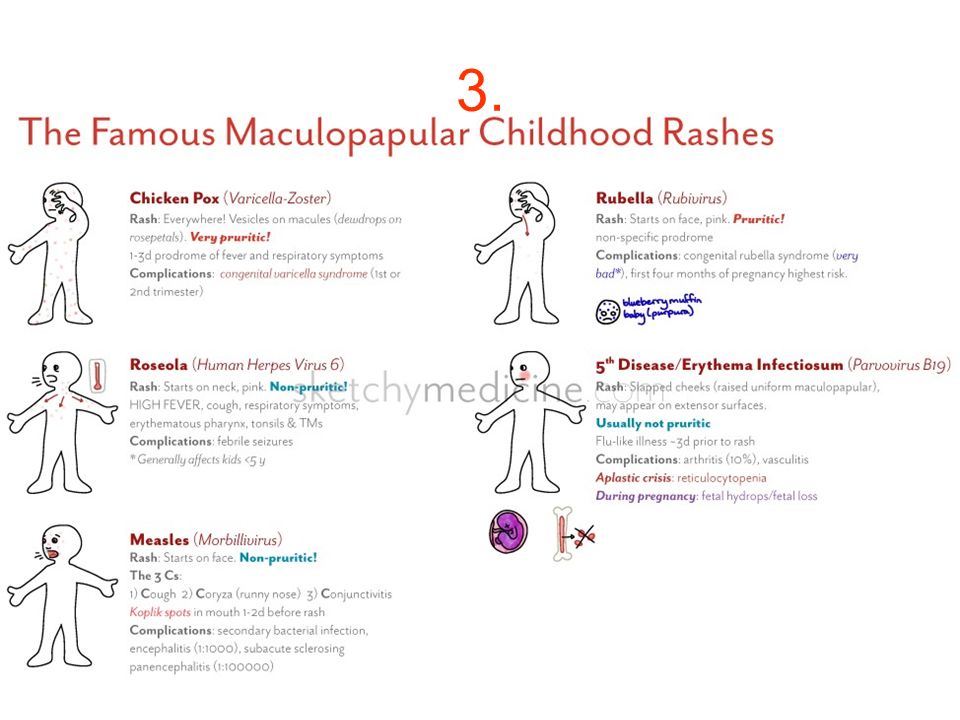 nine0003
nine0003
- A rash is a pathological change on the skin and mucous membranes. It can be divided into two main groups: infectious and non-infectious. Non-infectious include allergic reactions, insect bites, prickly heat. Infectious rashes appear with various infections, most often viral.
On examination, the doctor pays attention to the location, area of the rash, the nature of the rash, concomitant symptoms, and the patient's complaints. As a rule, if the rash is accompanied by severe intoxication - an increase in body temperature, weakness, refusal to eat and drink - the doctor decides on hospitalization. nine0003
Doctor of the highest category, candidate of medical sciences, allergist-immunologist Galina Chernyshova recommends that in any case, if a rash appears, contact a specialist in a timely manner, who will find out its cause and tell you what to do next.
- The cause of rashes on the body of a child can be either a banal food allergy or a severe infectious disease. The rash is never a separate disease or cause of the disease. The most common causes of its occurrence in children are allergic reactions, insect bites, infections, clotting disorders, mechanical damage to the skin and allergies to the sun. nine0003
The rash is never a separate disease or cause of the disease. The most common causes of its occurrence in children are allergic reactions, insect bites, infections, clotting disorders, mechanical damage to the skin and allergies to the sun. nine0003
Manifestations are very variable, from red or almost any shade of pale pink to bright brown speck, vesicle, bump to hemorrhage or even bruising.
Pediatrician Anna Ganina advises, first of all, to find out why a rash appeared on the child's body.
- Many rashes in children do not require self-treatment. We are waiting for it to pass by itself, and at the same time we are looking for the cause - a viral, bacterial infection, a blood clotting disorder.
It is often difficult to deal with a rash on your own: there are a lot of their types. Parents should immediately show the child to the doctor if it is hemorrhagic. If the rash is not hemorrhagic, but with a temperature, it is also advisable to show the doctor in the next day or two.
And if it appeared against the background of full health and it does not particularly disturb the child, the skin does not suffer - show the pediatrician in a calm planned manner.
Types of rash and their degree of danger
There are a lot of types of children's rash, they differ visually and are caused by different reasons. Consider some types of rashes - from the rare and most dangerous to the most common. nine0003
Meningococcal infection
© medmoon.ru
What it looks like: purple or red star-shaped spots located on the buttocks, thighs, legs, less often on the arms, torso, face. The temperature rises strongly, vomiting appears, impaired consciousness.
Hazard: high.
What to do: urgently call an ambulance and hospitalize the child.
Measles
What it looks like: Measles presents with cough, runny nose, conjunctivitis, sore throat, fever, and a red patchy rash on the skin that appears as bright pink patches that may coalesce.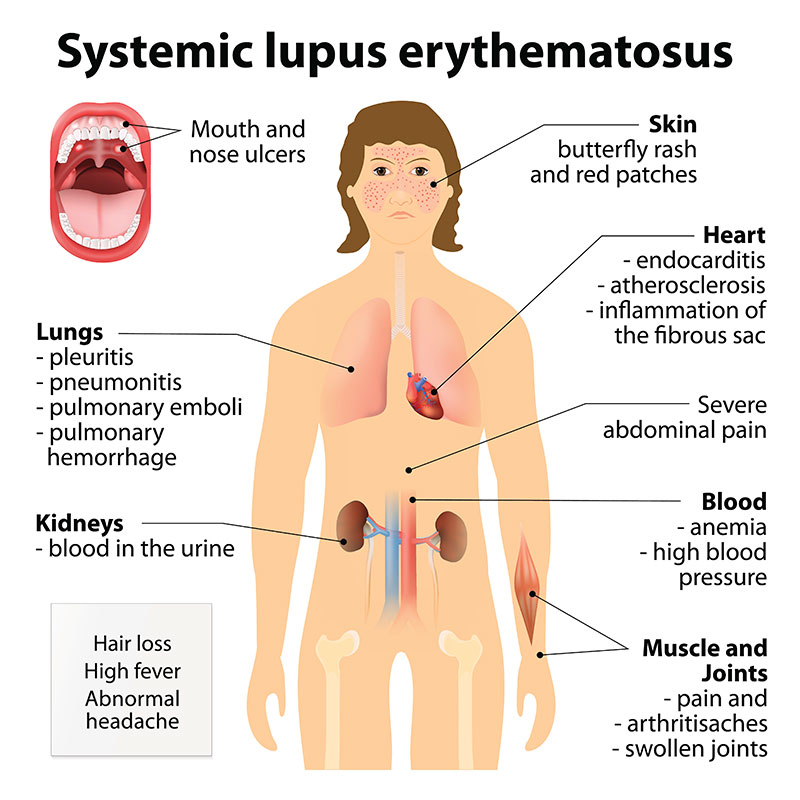
Hazard: high.
What to do: Seek immediate medical attention, do not self-medicate.
Coxsackie
What it looks like: reddish itchy blisters that appear all over the body and even on the mucous membranes of the child. The temperature rises, appetite disappears, nausea, vomiting, dehydration are possible. nine0003
Hazard: high.
What to do: contact a doctor immediately.
Chickenpox
What it looks like: first small bubbles appear with clear contents, then it becomes cloudy, the blisters break out and a crust forms. Eruptions occur all over the body and cause itching. Other symptoms: fever, usually up to 4 days, abdominal pain, itching, headache, malaise, lack of appetite, cough and runny nose, sore throat. nine0003
Hazard: medium.
What to do: be sure to contact a doctor who will diagnose and prescribe treatment.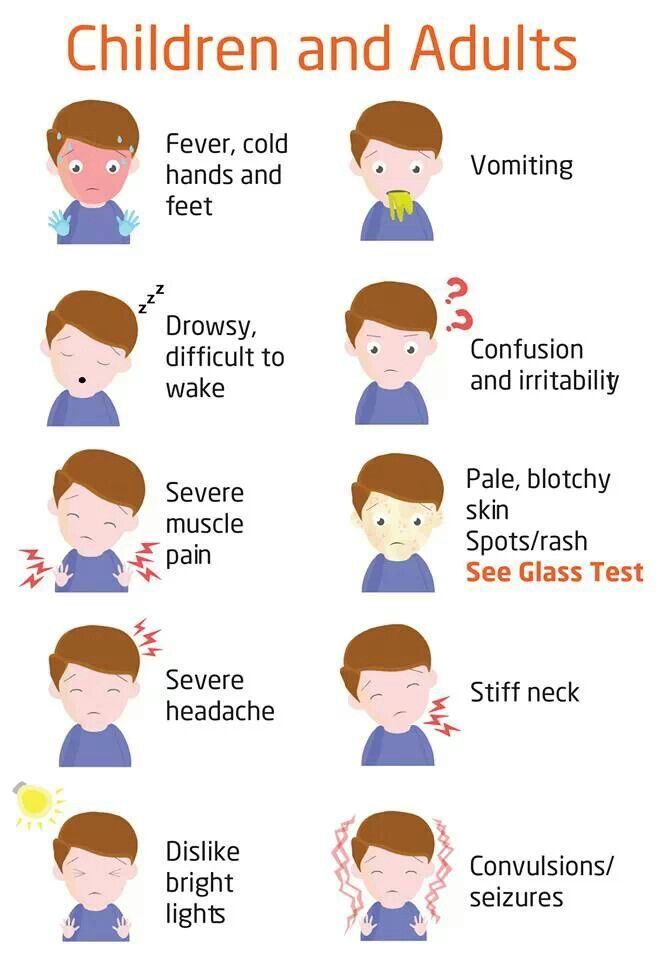
Rubella
It is poured all over the body, the temperature rises, the state of health worsens.
Danger level: medium.
What to do: consult a doctor.
Allergy
Appearance: rash usually red or pink, unevenly distributed over the skin, similar to small pimples. May cause itching.
Danger level: medium.
What to do: avoid contact with the allergen, if you guess what could have provoked the rash, give the child an antihistamine and consult a doctor.
Atopic dermatitis or diathesis
Appearance: the skin turns red and begins to peel off, sometimes weeping crusts are observed.
Danger level: medium.
What to do: avoid contact with the allergen, improve hygiene, give the child an antihistamine. If necessary, contact a doctor.
Roseola
What it looks like: Most common in children under 2 years of age.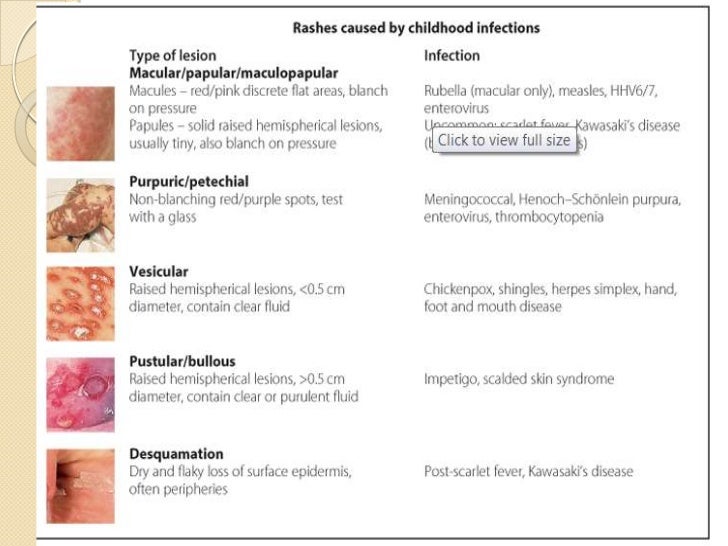 A rubella-like rash appears after 2-5 days of fever, while the child has almost no other symptoms (cough, runny nose). Roseola is usually not complicated by anything, and a rash means that the child is on the mend. nine0003
A rubella-like rash appears after 2-5 days of fever, while the child has almost no other symptoms (cough, runny nose). Roseola is usually not complicated by anything, and a rash means that the child is on the mend. nine0003
Hazard: medium/low.
What to do: The main thing is to exclude the presence of more serious diseases in the child. Treatment for roseola in children includes bed rest, drinking plenty of fluids, and medications to reduce fever.
Insect bites
What it looks like: pink or red swelling with a bite mark in the center.
Hazard: low. nine0003
What to do: If you are sure that the child was bitten by a mosquito or midge, just spread the bite with a special ointment or cream. If you suspect a bite from another insect, you should go to the hospital.
Newborn acne
Hazard: low.
What to do: go to the hospital to determine the cause of the rash.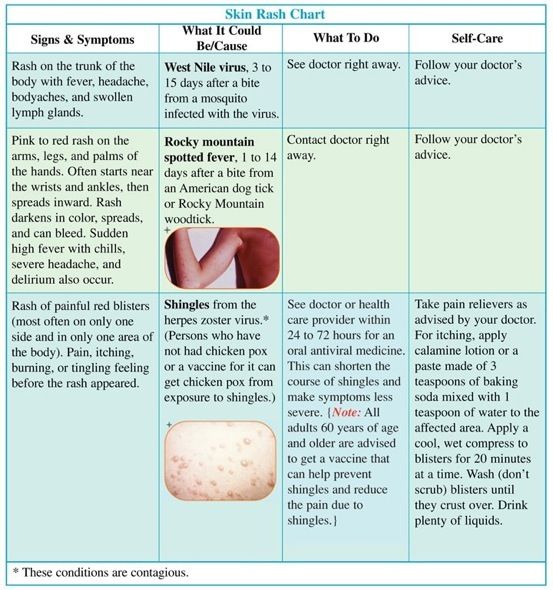
Diaper dermatitis
What it looks like: slight reddening of the skin, usually occurs in the delicate intimate parts of the baby. Blisters and redness of the skin may appear.
Hazard: low.
What to do: regularly wash your baby, change diapers in a timely manner and arrange air baths for the baby's skin. You don’t have to go to the doctor, the main thing is to improve hygiene, and the rash will pass. nine0003
Milia
What it looks like: appears on the skin as whiteheads.
Hazard: low.
What to do: milia do not have a negative effect on the child's body and after a while, most likely, they will disappear on their own. If the appearance of whiteheads is accompanied by poor health of the child, fever and itching, you should consult a doctor.
— share with your friends! nine0003
Experts: Anna Ganina Natalia Makarova Galina Chernyshova
Read more
- 4 times more people got measles this year than last year
- "There are no hypoallergenic animals.