Down syndrome diagnosis test
Down syndrome - Diagnosis and treatment
Diagnosis
The American College of Obstetricians and Gynecologists recommends offering the option of screening tests and diagnostic tests for Down syndrome to all pregnant women, regardless of age.
- Screening tests can indicate the likelihood or chances that a mother is carrying a baby with Down syndrome. But these tests can't tell for sure or diagnose whether the baby has Down syndrome.
- Diagnostic tests can identify or diagnose whether your baby has Down syndrome.
Your health care provider can discuss the types of tests, advantages and disadvantages, benefits and risks, and the meaning of your results. If appropriate, your provider may recommend that you talk to a genetics counselor.
Screening tests during pregnancy
Screening for Down syndrome is offered as a routine part of prenatal care. Although screening tests can only identify your risk of carrying a baby with Down syndrome, they can help you make decisions about more-specific diagnostic tests.
Screening tests include the first trimester combined test and the integrated screening test.
The first trimester combined test
The first trimester combined test, which is done in two steps, includes:
- Blood test. This blood test measures the levels of pregnancy-associated plasma protein-A (PAPP-A) and the pregnancy hormone known as human chorionic gonadotropin (HCG). Abnormal levels of PAPP-A and HCG may indicate a problem with the baby.
- Nuchal translucency test. During this test, an ultrasound is used to measure a specific area on the back of your baby's neck. This is known as a nuchal translucency screening test. When abnormalities are present, more fluid than usual tends to collect in this neck tissue.
Using your age and the results of the blood test and the ultrasound, your doctor or genetic counselor can estimate your risk of having a baby with Down syndrome.
Integrated screening test
The integrated screening test is done in two parts during the first and second trimesters of pregnancy. The results are combined to estimate the risk that your baby has Down syndrome.
The results are combined to estimate the risk that your baby has Down syndrome.
- First trimester. Part one includes a blood test to measure PAPP-A and an ultrasound to measure nuchal translucency.
- Second trimester. The quad screen measures your blood level of four pregnancy-associated substances: alpha fetoprotein, estriol, HCG and inhibin A.
Diagnostic tests during pregnancy
If your screening test results are positive or worrisome, or you're at high risk of having a baby with Down syndrome, you might consider more testing to confirm the diagnosis. Your health care provider can help you weigh the pros and cons of these tests.
Diagnostic tests that can identify Down syndrome include:
- Chorionic villus sampling (CVS). In CVS, cells are taken from the placenta and used to analyze the fetal chromosomes. This test is typically performed in the first trimester, between 10 and 13 weeks of pregnancy.
 The risk of pregnancy loss (miscarriage) from a CVS is very low.
The risk of pregnancy loss (miscarriage) from a CVS is very low. - Amniocentesis. A sample of the amniotic fluid surrounding the fetus is withdrawn through a needle inserted into the mother's uterus. This sample is then used to analyze the chromosomes of the fetus. Doctors usually perform this test in the second trimester, after 15 weeks of pregnancy. This test also carries a very low risk of miscarriage.
Preimplantation genetic diagnosis is an option for couples undergoing in vitro fertilization who are at increased risk of passing along certain genetic conditions. The embryo is tested for genetic abnormalities before it's implanted in the womb.
Diagnostic tests for newborns
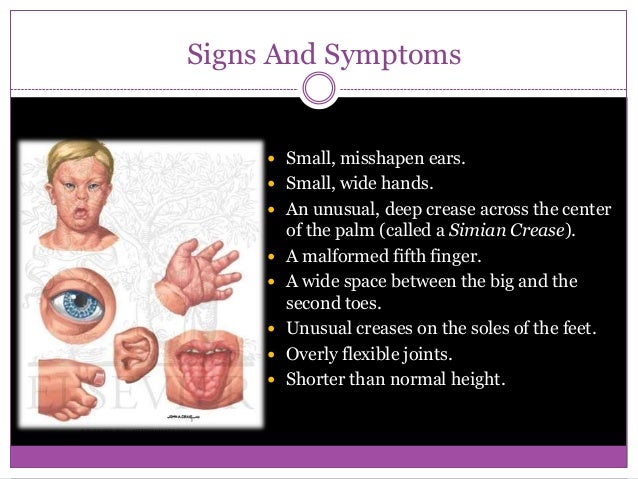
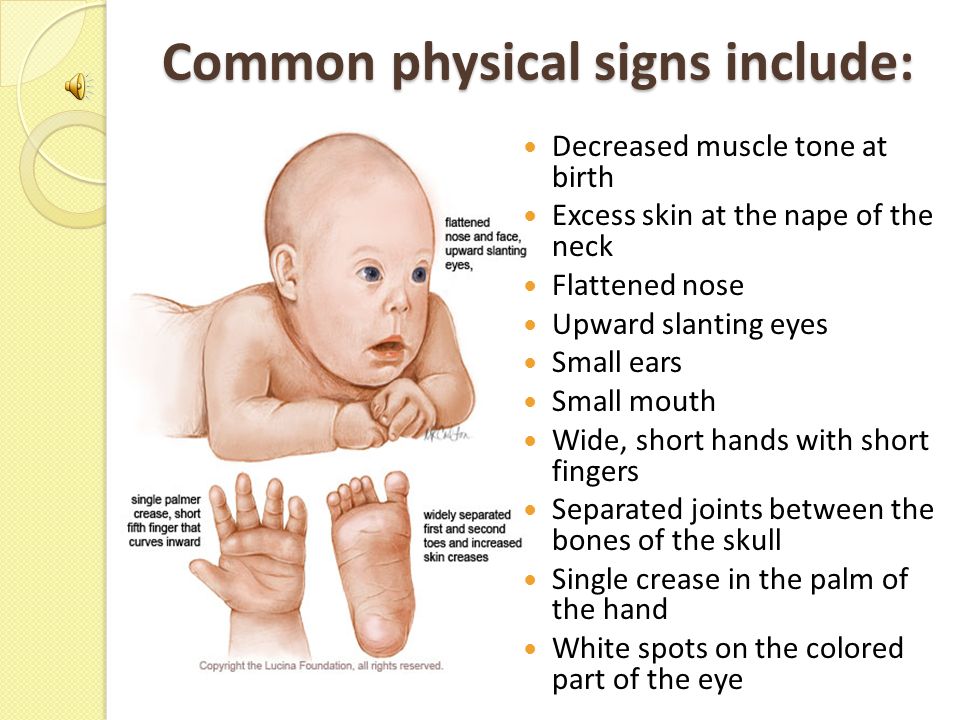
After birth, the initial diagnosis of Down syndrome is often based on the baby's appearance. But the features associated with Down syndrome can be found in babies without Down syndrome, so your health care provider will likely order a test called a chromosomal karyotype to confirm diagnosis. Using a sample of blood, this test analyzes your child's chromosomes. If there's an extra chromosome 21 in all or some cells, the diagnosis is Down syndrome.
Using a sample of blood, this test analyzes your child's chromosomes. If there's an extra chromosome 21 in all or some cells, the diagnosis is Down syndrome.
More Information
- Amniocentesis
- Genetic testing
- Ultrasound
Treatment
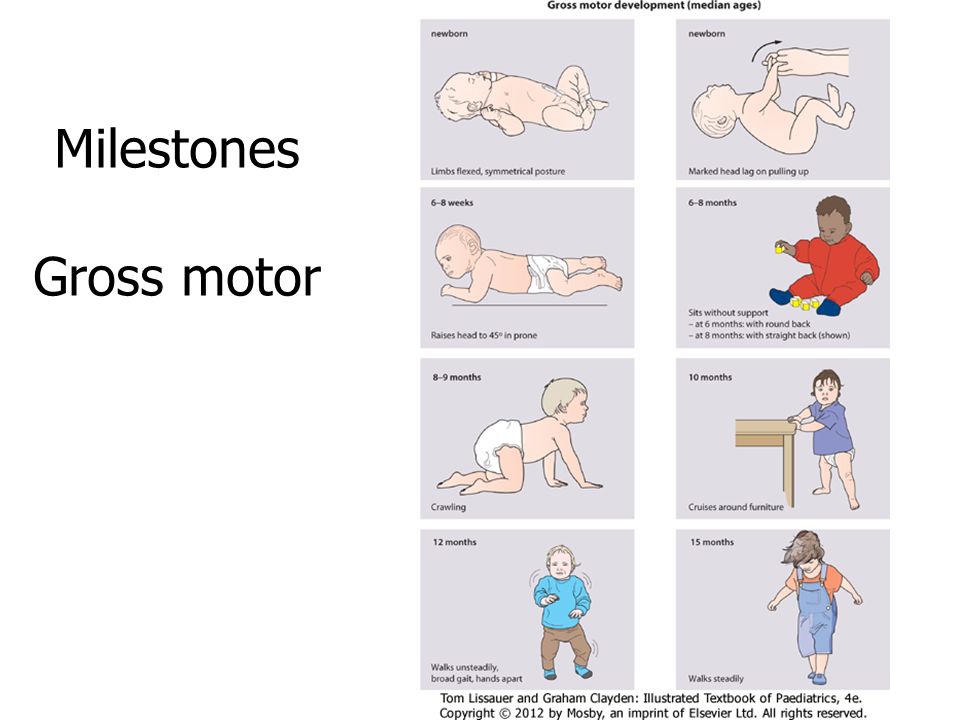
Early intervention for infants and children with Down syndrome can make a major difference in improving their quality of life. Because each child with Down syndrome is unique, treatment will depend on individual needs. Also, different stages of life may require different services.
Team care
If your child has Down syndrome, you'll likely rely on a team of specialists that can provide medical care and help him or her develop skills as fully as possible. Depending on your child's particular needs, your team may include some of these experts:
- Primary care pediatrician to coordinate and provide routine childhood care
- Pediatric cardiologist
- Pediatric gastroenterologist
- Pediatric endocrinologist
- Developmental pediatrician
- Pediatric neurologist
- Pediatric ear, nose and throat (ENT) specialist
- Pediatric eye doctor (ophthalmologist)
- Audiologist
- Speech pathologist
- Physical therapist
- Occupational therapist
You'll need to make important decisions about your child's treatment and education. Build a team of health care providers, teachers and therapists you trust. These professionals can help evaluate the resources in your area and explain state and federal programs for children and adults with disabilities.
Build a team of health care providers, teachers and therapists you trust. These professionals can help evaluate the resources in your area and explain state and federal programs for children and adults with disabilities.
Request an Appointment at Mayo Clinic
Coping and support
When you learn your child has Down syndrome, you may experience a range of emotions, including anger, fear, worry and sorrow. You may not know what to expect, and you may worry about your ability to care for a child with a disability. The best antidote for fear and worry is information and support.
Consider these steps to prepare yourself and to care for your child:
- Ask your health care provider about early intervention programs in your area. Available in most states, these special programs offer infants and young children with Down syndrome stimulation at an early age (typically until age 3) to help develop motor, language, social and self-help skills.
- Learn about educational options for school.
 Depending on your child's needs, that may mean attending regular classes (mainstreaming), special education classes or both. With your health care team's recommendations, work with the school to understand and choose appropriate options.
Depending on your child's needs, that may mean attending regular classes (mainstreaming), special education classes or both. With your health care team's recommendations, work with the school to understand and choose appropriate options. - Seek out other families who are dealing with the same issues. Most communities have support groups for parents of children with Down syndrome. You can also find internet support groups. Family and friends can also be a source of understanding and support.
- Participate in social and leisure activities. Take time for family outings and look in your community for social activities such as park district programs, sports teams or ballet classes. Although some adaptations may be required, children and adults with Down syndrome can enjoy social and leisure activities.
- Encourage independence. Your child's abilities may be different from other children's abilities, but with your support and some practice your child may be able to perform tasks such as packing lunch, managing hygiene and dressing, and doing light cooking and laundry.

- Prepare for the transition to adulthood. Opportunities for living, working, and social and leisure activities can be explored before your child leaves school. Community living or group homes, and community employment, day programs or workshops after high school require some advance planning. Ask about opportunities and support in your area.
Expect a bright future. Most people with Down syndrome live with their families or independently, go to mainstream schools, read and write, participate in the community, and have jobs. People with Down syndrome can live fulfilling lives.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Prenatal Testing for Down Syndrome | Patient Education
Screening tests
All pregnant individuals in California have access to California prenatal screening (CA PNS), also called sequential integrated screening. This noninvasive process is carried out in two steps.
This noninvasive process is carried out in two steps.
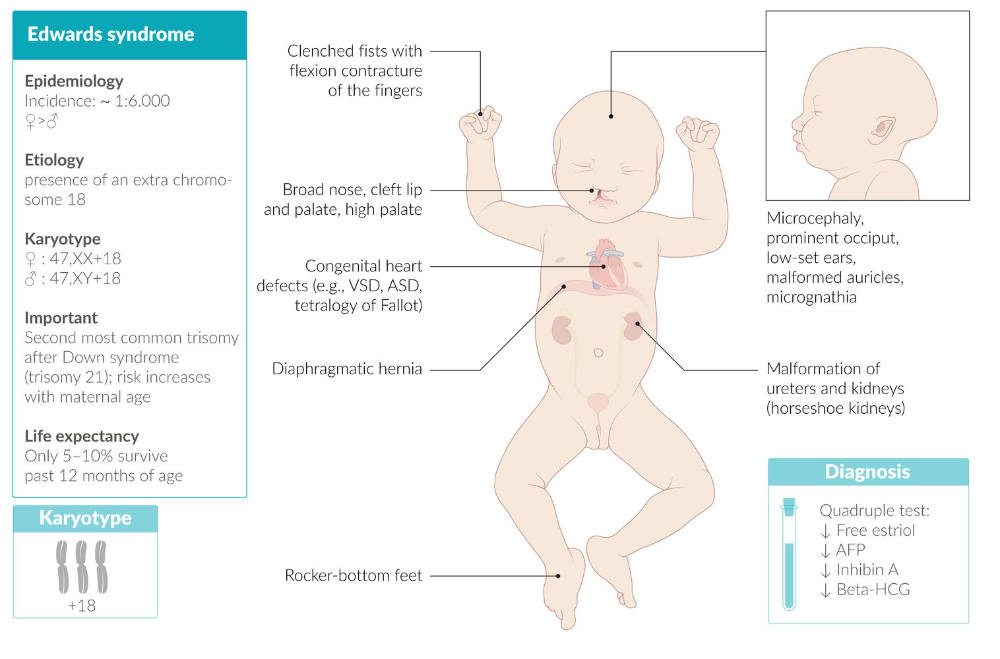
In the first step, which is performed when the pregnancy is between 10 and 14 weeks, a blood sample is taken from the pregnant person and a nuchal translucency ultrasound is performed to measure the fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide those results at the end of your ultrasound appointment. The blood test results, nuchal translucency measurement and pregnant person's age are together used to estimate the risk for Down syndrome and trisomy 18 (a genetic condition, also called Edwards syndrome, that affects fetal development).
The second step is a test performed with a blood sample from the pregnant person when the pregnancy is between 15 and 20 weeks. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome (a genetic condition that can slow growth and cause intellectual disability), an open neural tube defect (a problem with the formation of the embryo's nervous system, such as spina bifida) or an abdominal wall defect (an abnormal opening in the abdomen).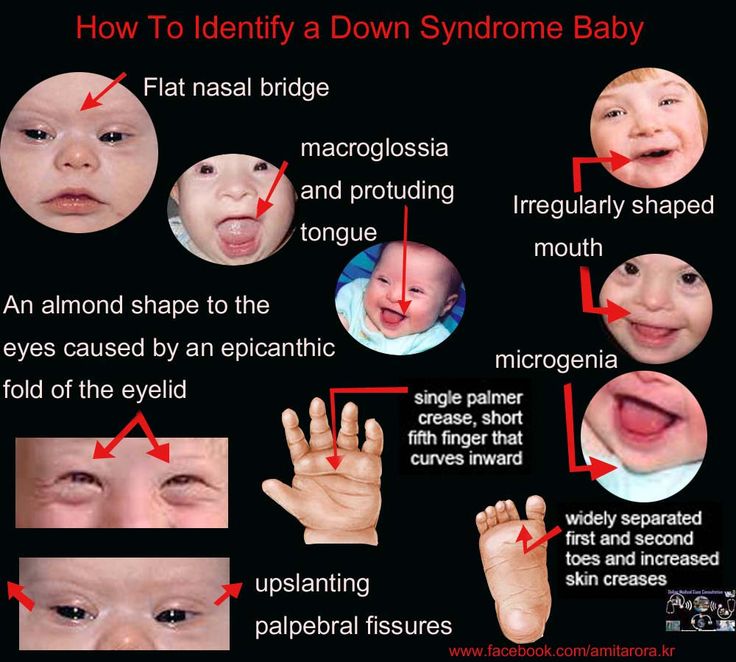
Diagnostic tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis is the test we most commonly use to identify chromosomal problems, such as Down syndrome. (In at-risk fetuses, it can be used to detect other genetic diseases, such as cystic fibrosis, Tay-Sachs disease and sickle cell disease.)
An amniocentesis procedure for genetic testing is typically performed when the pregnancy is between 15 and 20 weeks. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small sample of amniotic fluid. Cells from the fluid are cultured and a karyotype test – an analysis of the cells' chromosomal makeup – is performed. It takes about two weeks to receive the results. Amniocentesis detects most chromosomal disorders with a high degree of accuracy.
There is a low risk of miscarriage as a result of amniocentesis – about 1 in 900. Miscarriage rates for amniocentesis performed at UCSF are extremely low.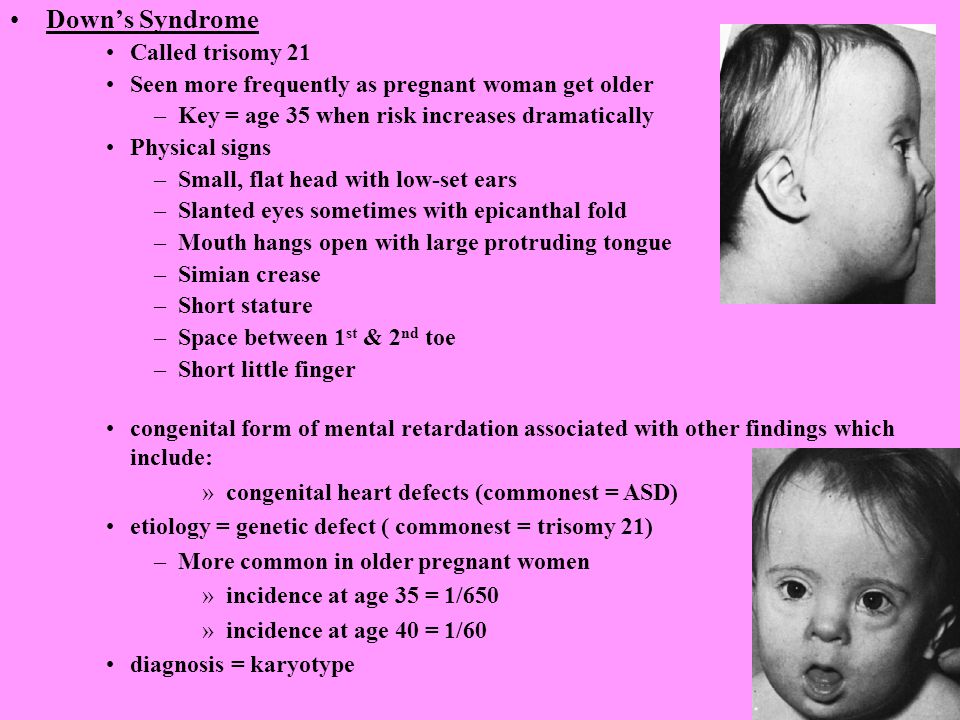
Like amniocentesis, chorionic villus sampling is most commonly used to identify chromosomal problems, such as Down syndrome. (It can also be used to detect other genetic diseases – including cystic fibrosis, Tay-Sachs disease and sickle cell disease – in at-risk fetuses.) The main advantage over amniocentesis is that CVS is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta for analysis. Under ultrasound guidance, this sample is obtained either with a needle inserted through the abdomen or a catheter inserted through the vagina and into the cervix (outer end of the uterus). The tissue is cultured and a karyotype test of the cells' chromosomal makeup is performed. It takes about two weeks to receive the results.
While it can provide information earlier in pregnancy than amniocentesis, CVS does not detect spinal cord defects. However, we can screen for spinal cord defects later in the pregnancy using expanded alpha-fetoprotein (AFP) blood testing or ultrasound.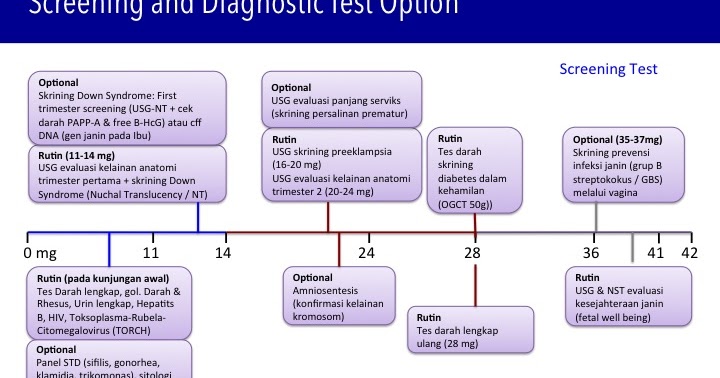
There is a low risk of miscarriage as a result of CVS – about 1 in 450. Miscarriage rates for CVS procedures performed at UCSF are very low.
While the primary purpose of ultrasound is to determine the pregnancy's status – due date, size of the fetus and whether there's more than one baby – ultrasound can also provide some information about possible birth defects. All pregnant UCSF patients undergo a comprehensive ultrasound exam before any invasive tests are performed. We will explain your ultrasound results at the time of your visit.
In some patients, an ultrasound raises concern for a fetal abnormality. This possibility makes ultrasound expertise crucial, so you may find it reassuring that we have extensive experience in performing and interpreting ultrasound exams in pregnancy.
The meaning of a positive result
If you receive positive results on a screening test, we recommend that you discuss its implications and your options with your doctor and a genetic counselor.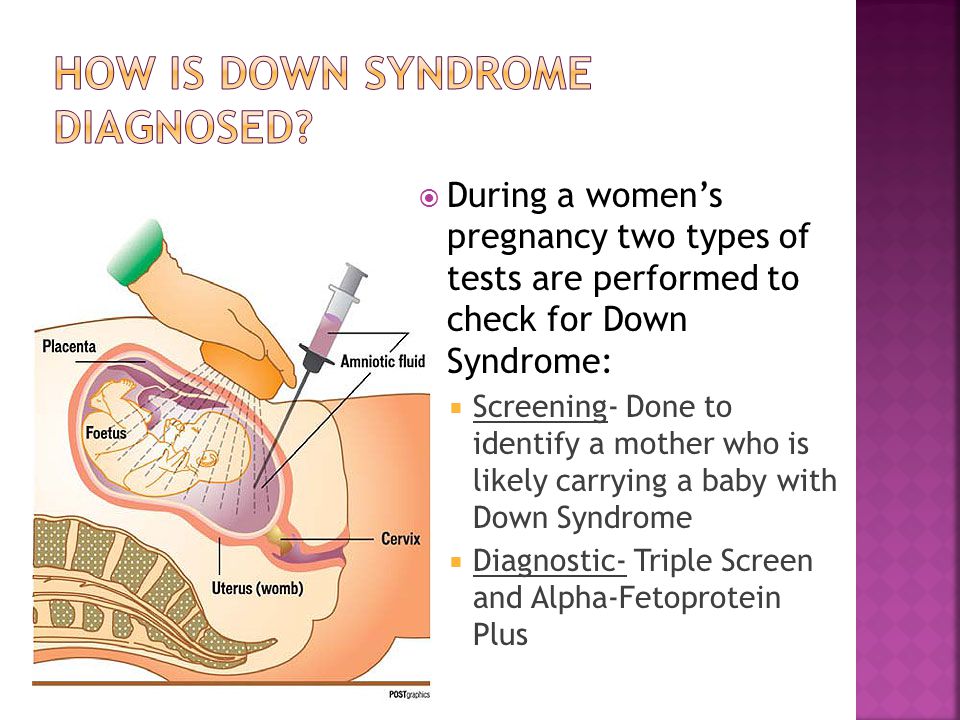 They will explain what types of diagnostic testing are available. Whether to have invasive genetic testing is your decision.
They will explain what types of diagnostic testing are available. Whether to have invasive genetic testing is your decision.
If a diagnostic test finds a genetic abnormality, we recommend discussing the significance of the result with experts on the condition, including a medical geneticist and a genetic counselor, as well as your doctor.
Down syndrome screening tests in the first 24 weeks of pregnancy
Relevance
Down syndrome (also known as Down syndrome or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, there is great variation in how Down syndrome affects people. Some individuals are severely affected, while others have minor problems and are able to lead relatively normal lives. It is impossible to predict how badly each child may be affected. nine0006
Parents-to-be are given the choice of being tested for Down syndrome during pregnancy to help them make decisions.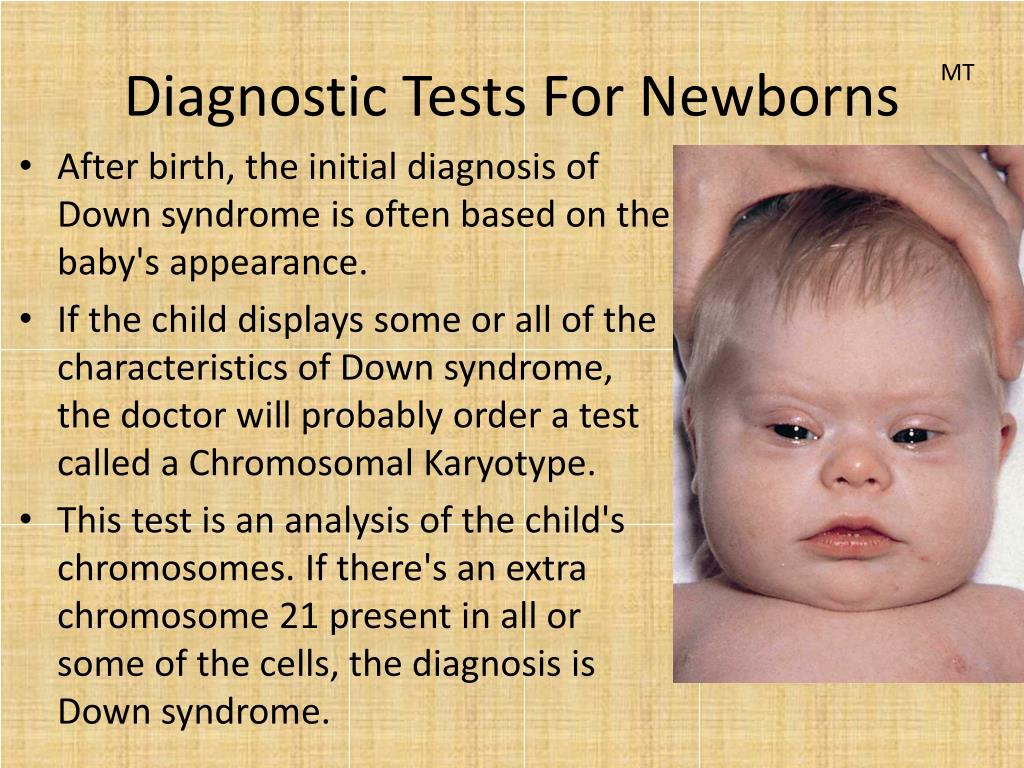 If the expectant mother is carrying a child with Down syndrome, then it is necessary to decide whether to terminate or continue the pregnancy. This information gives parents the opportunity to plan life with a Down child.
If the expectant mother is carrying a child with Down syndrome, then it is necessary to decide whether to terminate or continue the pregnancy. This information gives parents the opportunity to plan life with a Down child.
The most accurate tests for detecting Down include testing of amniotic fluid (amniocentesis) or placental tissue (chorionic villus sampling (CVS)) for abnormal chromosomes associated with Down. Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, these tests are not suitable for all pregnant women. Instead, screening uses tests that measure markers in the mother's blood, urine, or baby's ultrasound. These screening tests are not perfect, they can miss cases of Down and also provide a "high risk" result for women whose children do not have Down. Thus, a pregnancy defined as Down's "high risk" using these screening tests requires further testing by amniocentesis (from 15 weeks gestation) or CVS (from 10+0 to 13+6 weeks gestation) to confirm the diagnosis.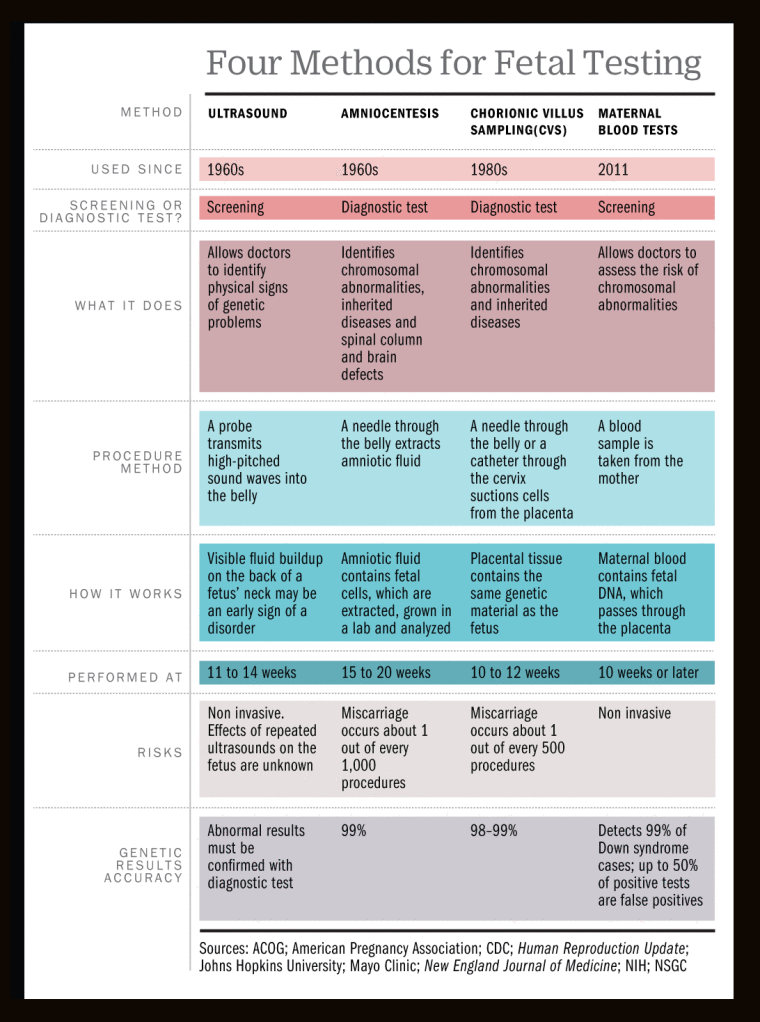 Down. nine0006
Down. nine0006
What we did
The purpose of this review was to find out which of the ultrasound screening tests done in the first trimester of pregnancy, with or without screening for serum marker levels in the first 14 weeks of pregnancy, is the most accurate in predicting Down's risk of pregnancy. We studied 11 different ultrasound markers and 12 different serum markers, which can be used alone, in ratios, or in combination, taken up to 14 weeks of gestation, which together create 60 screening tests for Down. We found 126 studies involving 1,604,040 pregnant women (including 8454 fetuses with Down syndrome). nine0005
What we found
For screening for Down's syndrome during the first 14 weeks of pregnancy, study results support the use of first trimester ultrasound screening tests in combination with two tests to determine levels of serum (blood) markers - mainly pregnancy-associated plasma protein-A (PAPP-A ) and the free β-subunit of human chorionic gonadotropin (ßhCG), given the age of the mother. Overall, these tests are better than ultrasonic markers alone. They find nine out of 10 pregnancies with Down syndrome. Five percent of women who do this test will have a "high risk" result, although most of these pregnancies will not actually have Down's syndrome. nine0006
Overall, these tests are better than ultrasonic markers alone. They find nine out of 10 pregnancies with Down syndrome. Five percent of women who do this test will have a "high risk" result, although most of these pregnancies will not actually have Down's syndrome. nine0006
Other important information to study
Ultrasound tests in and of themselves have no adverse effects on the woman, and blood tests may cause discomfort, bruising, and, rarely, a risk of infection. However, some women who have a "high risk" screening test and who are undergoing amniocentesis or CVS are at risk of miscarriage in a child who does not have Down syndrome. Parents will need to weigh this risk when deciding whether or not to have an amniocentesis or CVS following the results of a "high risk" screening test. nine0006
Translation notes:
Translation notes: Translation: Ekaterina Evgenievna Mukhamadeeva. Editing: Alexandrova Elvira Grigorievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University).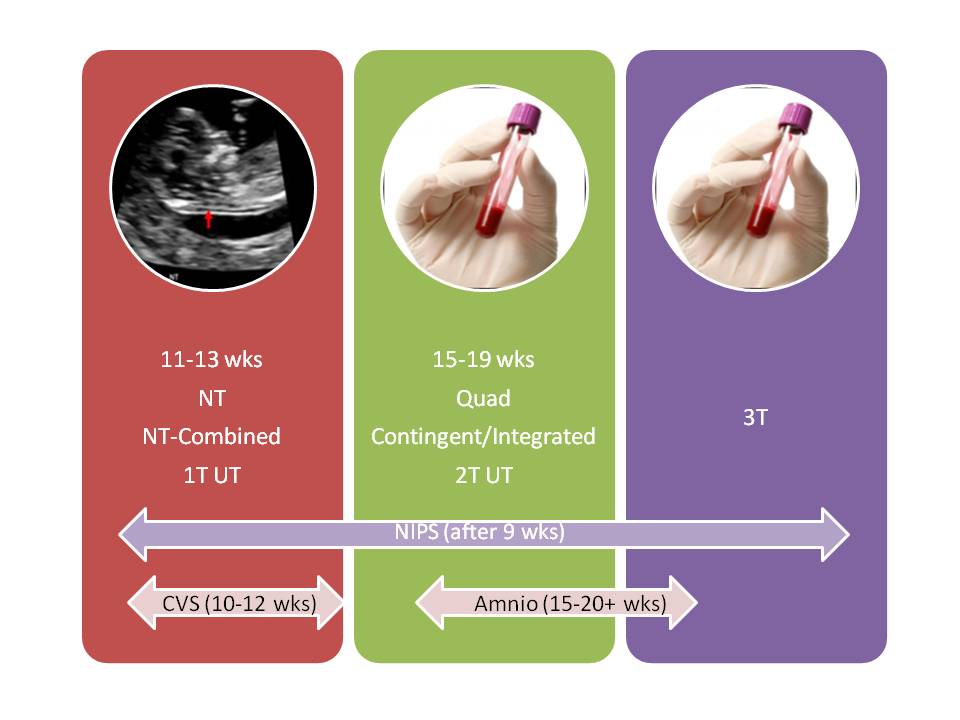 For questions regarding this transfer, please contact us at: [email protected]
For questions regarding this transfer, please contact us at: [email protected]
Screening tests for Down syndrome in the first 24 weeks of pregnancy
Relevance
Down's syndrome (also known as Down's disease or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, Down syndrome affects people in completely different ways. Some have significant symptoms, while others have minor health problems and are able to lead relatively normal lives. There is no way to predict how badly a child might be affected. nine0006
Expectant parents during pregnancy are given the opportunity to have a screening test for Down syndrome in their baby to help them make a decision. If a mother is carrying a child with Down syndrome, then a decision should be made whether to terminate the pregnancy or keep it. The information gives parents the opportunity to plan life with a child with Down syndrome.
The most accurate screening tests for Down syndrome include amniotic fluid (amniocentesis) or placental tissue (chorionic villus biopsy (CVS)) to identify abnormal chromosomes associated with Down syndrome.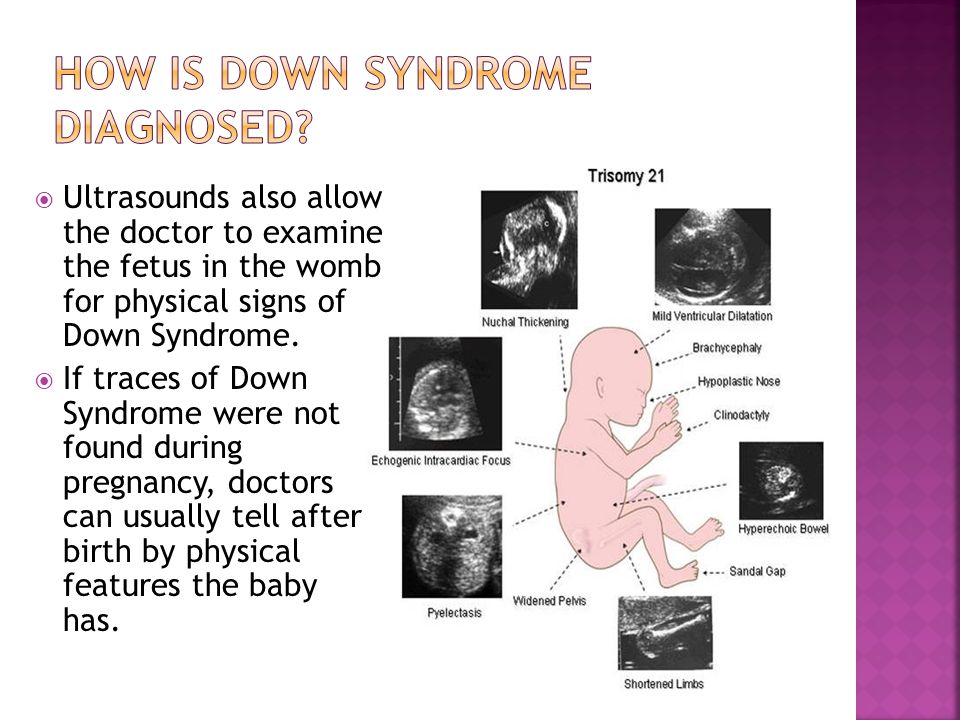 Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, screening tests are not suitable for all pregnant women. Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome. Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome. nine0006
Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, screening tests are not suitable for all pregnant women. Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome. Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome. nine0006
What we did
We analyzed combinations of serum screening tests in the first (up to 14 weeks) and second (up to 24 weeks) trimesters of pregnancy with or without ultrasound screening in the first trimester. Our goal was to identify the most accurate tests for predicting the risk of Down syndrome during pregnancy. One ultrasound index (neckfold thickness) and seven different serological indexes (PAPP-A, total hCG, free beta-hCG, unbound estriol, alpha-fetoprotein, inhibin A, ADAM 12) were studied, which can be used separately, in ratios or in combination with each other, obtained before 24 weeks of gestation, thereby obtaining 32 screening tests for the detection of Down's syndrome.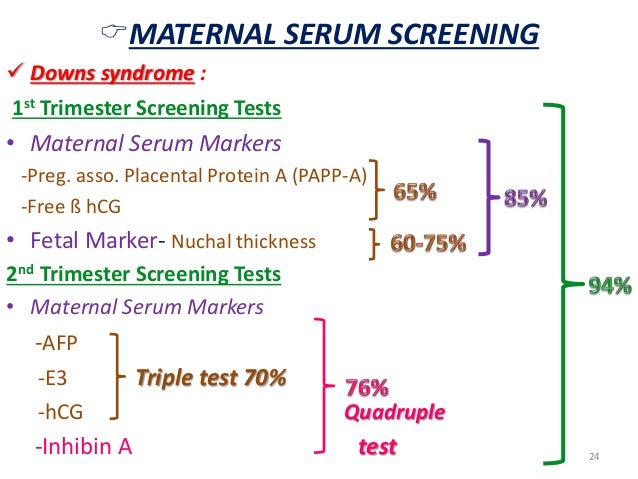 We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome). nine0005
We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome). nine0005
What we found
During Down Syndrome screening, which included tests during the first and second trimesters that combined to determine overall risk, we found that a test that included neckfold measurement and PAPP- A in the first trimester, as well as the determination of total hCG, unbound estriol, alpha-fetoprotein and inhibin A in the second trimester, turned out to be the most sensitive, as it allowed to determine 9out of 10 pregnancies associated with Down syndrome. Five percent of pregnant women who were determined to be at high risk on this combination of tests would not have a child with Down syndrome. There have been relatively few studies evaluating these tests, so we cannot draw firm conclusions or recommendations about which test is best.
Other important information to consider
Ultrasounds themselves have no adverse effects on women, and blood tests can cause discomfort, bruising, and, in rare cases, infection.