Risks of being induced
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
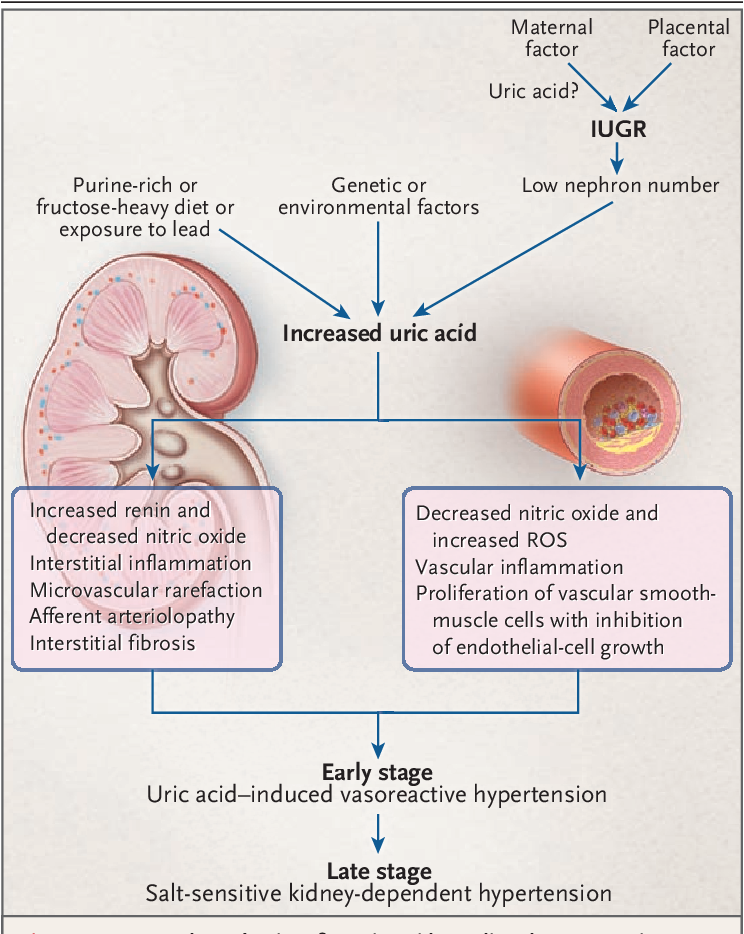
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).

- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.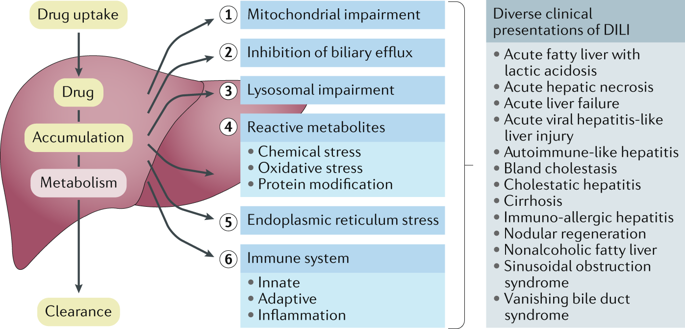 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
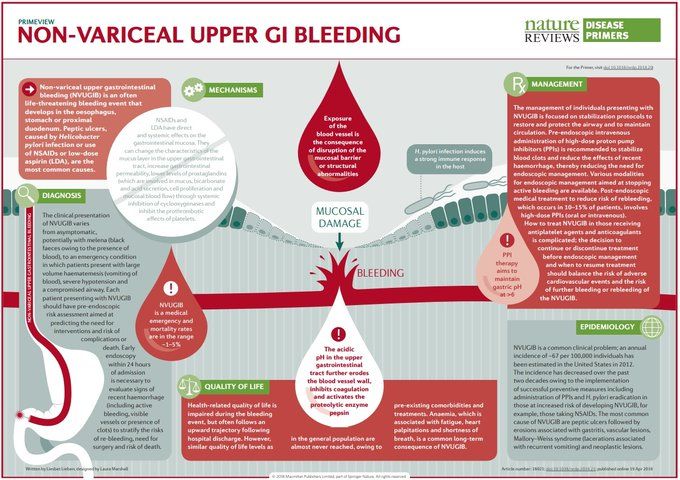
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
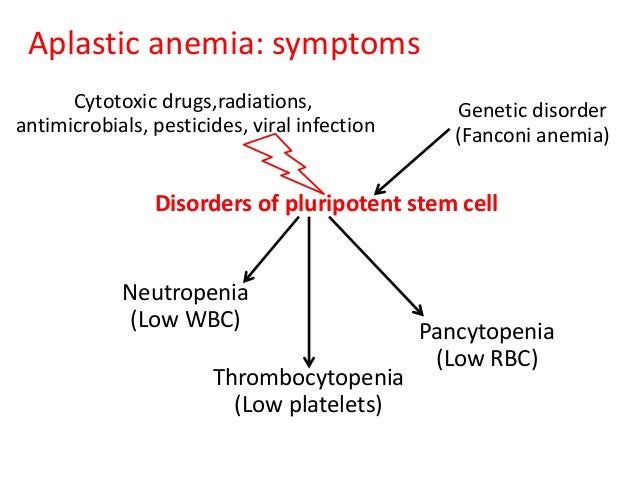
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery. Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
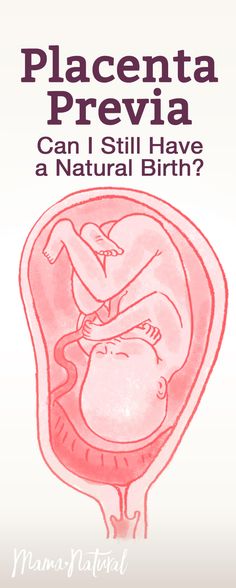
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.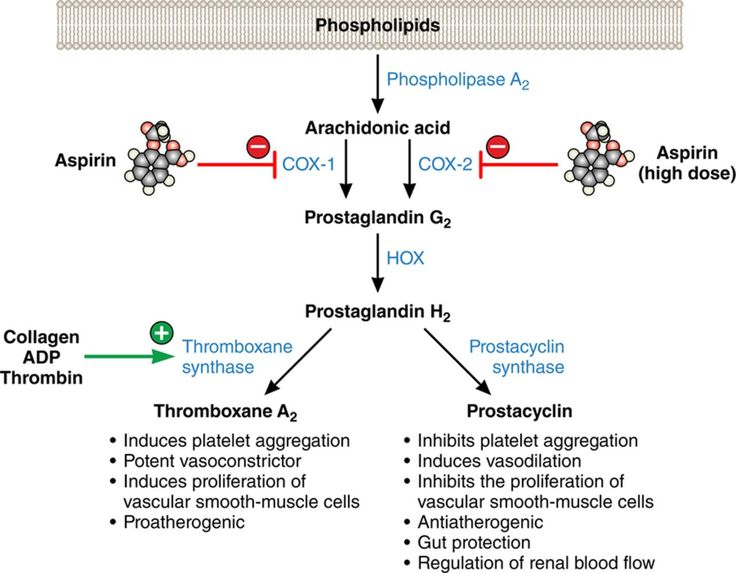
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Stripping Membranes and Breaking Water for Labor Induction, Augmentation
Written by WebMD Editorial Contributors
In this Article
- What Is Labor Induction?
- Why Is Labor Induced?
- Reasons Not to Induce
- How Is Labor Induced?
- What Are the Risks of Inducing Labor?
- Can I Induce Labor Myself?
What Is Labor Induction?
If your doctor or midwife has concerns about your health or your baby's health toward the end of your pregnancy, they might suggest speeding up the process.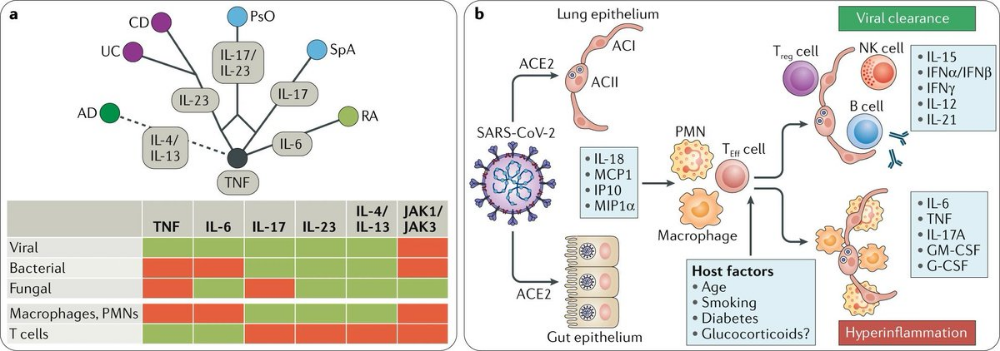 This is called inducing labor, or induction. Instead of waiting for labor to start naturally, your doctor or midwife will use drugs or a procedure to start it sooner.
This is called inducing labor, or induction. Instead of waiting for labor to start naturally, your doctor or midwife will use drugs or a procedure to start it sooner.
Induction can be the right choice for some women, but it has risks. And it doesn’t always work. If it doesn’t, you may need another induction or a c-section. Most experts say it's best to let labor begin on its own and progress naturally unless there's a clear medical reason.
Why Is Labor Induced?
Induction is very common -- 1 out of 4 women in the U.S. starts labor with induction. Many times it's done for medical reasons, but it can be elective.
Why do some women need to have labor induced?
You’re 1-2 weeks past your due date. Studies show that inducing labor at 39 weeks doesn’t raise the risk for having a C-section or birth complications for the baby. After 41 weeks, you and your baby are at greater risk for complications.
 Being a little "late" isn’t a reason to induce. You also don’t want to be induced too early. Babies born before 39 weeks are more likely to have health problems, longer hospital stays, and time in neonatal intensive care.
Being a little "late" isn’t a reason to induce. You also don’t want to be induced too early. Babies born before 39 weeks are more likely to have health problems, longer hospital stays, and time in neonatal intensive care.Your water breaks but labor doesn’t start. Once your water breaks, you and your baby have a higher risk of infection. You might not need induction right away, though. Check with your doctor or midwife. Sometimes it's still safe to let labor begin on its own. After your water breaks, your doctor will limit the number of vaginal exams performed because of the potential for infection.
A problem puts you or your baby’s health at risk. Examples are infection (chorioamnionitis), too little amniotic fluid (oligohydramnios), and placental abruption. If you have conditions like diabetes, high blood pressure, preeclampsia, or eclampsia, your doctor or midwife might want to induce labor.
If your baby isn’t growing as it should be, or has an abnormal heart rate, your doctor or midwife might want to induce labor.
Some doctors recommend "elective" inductions for non-medical reasons. Maybe you live far from the hospital and your doctor worries that you won't get there in time. Or maybe your doctor asks you to accommodate their schedule. Experts say you should reconsider, though. Because induction poses some risks, experts say that women shouldn't be induced unless it's medically necessary.
Reasons Not to Induce
You doctor shouldn’t induce if:
You had C-section before that involved a classical incision or major surgery
The placenta is covering the cervix (placenta previa)
Your baby is in the wrong position (sideways or feet-first)
How Is Labor Induced?
There are a few ways a doctor or midwife can induce your labor, including:
Stripping the membranes.
 In this procedure, your doctor or midwife will use a gloved finger to gently separate the amniotic sac from the wall of the uterus at the cervix. This releases hormones that can trigger contractions. You can get it done in your doctor's or midwife's office. It can be uncomfortable. Afterward, you’ll probably go home to wait for contractions. You might have cramping and spotting.Studies disagree about how well membrane stripping works. Considering that and the discomfort it causes, talk over the pros and cons with your doctor or midwife beforehand.
In this procedure, your doctor or midwife will use a gloved finger to gently separate the amniotic sac from the wall of the uterus at the cervix. This releases hormones that can trigger contractions. You can get it done in your doctor's or midwife's office. It can be uncomfortable. Afterward, you’ll probably go home to wait for contractions. You might have cramping and spotting.Studies disagree about how well membrane stripping works. Considering that and the discomfort it causes, talk over the pros and cons with your doctor or midwife beforehand.Hormones. At the hospital, your doctor will give you hormones called prostaglandins to open the cervix and trigger contractions. If you’ve had a C-section in the past, your doctor won’t use this treatment, because it raises the risk of uterine rupture.
Mechanical dilation. Another way your doctor or midwife triggers labor is with a balloon catheter.
 At the hospital, your doctor inserts a thin tube through your vagina into your cervical opening. Then the doctor uses water to inflate the balloon at the end of the tube, causing your cervix to expand.
At the hospital, your doctor inserts a thin tube through your vagina into your cervical opening. Then the doctor uses water to inflate the balloon at the end of the tube, causing your cervix to expand.Medications. The medicine Pitocin (oxytocin) can start contractions. You get this at the hospital through an IV tube in your arm. Your doctor or midwife starts with a small dose and gradually increases it until your contractions are strong and frequent enough for your baby to be born.
Some women go into labor and deliver within a few hours after induction. Others take 1 or 2 days to start labor. If none of these methods starts your labor, and staying the course isn’t a good option, you'll most likely need a C-section, especially if your water has broken.
What Are the Risks of Inducing Labor?
Induction doesn’t work for everyone, and every pregnant mom’s body reacts differently to induction technique.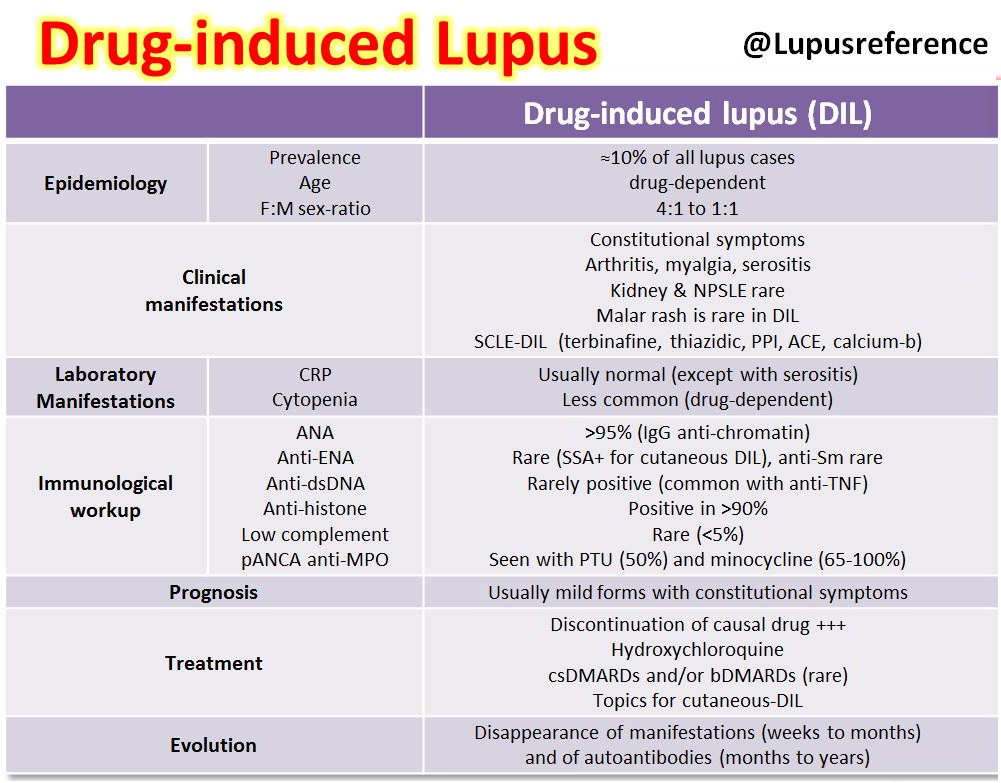 Generally, inducing labor is safe, but there are risks:
Generally, inducing labor is safe, but there are risks:
Longer hospital stay. If you're induced, you may be in the hospital longer during labor and delivery. If you wind up needing a C-section after induction, your time in the hospital will be even longer.
Increased need for pain medicine. Inducing labor might cause contractions to come on stronger and more often than they would naturally. You're more likely to need an epidural or another medicine to manage the pain.
Increased risk of infection. Breaking the amniotic sac can lead to infection if you don't deliver within a day or two after induction.
Health problems for your baby. Women who are induced before the 39th week for medical reasons may deliver a baby who has problems with breathing.
 These babies have a higher risk of long-term developmental problems.
These babies have a higher risk of long-term developmental problems.Complications during delivery. Induction, especially with medications, might not be safe for women who’ve had a previous C-section or other surgery to the uterus. They have a higher risk of uterine rupture. Intense contractions also cause the placenta to detach from the wall of the uterus, called placental abruption. Both of these conditions are serious but rare, even with induction.
If your doctor or midwife recommends induction, ask questions. You want to be absolutely sure that it's the best decision for your health and your baby's health.
Can I Induce Labor Myself?
Tales abound of home remedies that supposedly bring on labor, but there is no scientific evidence to back them up. These methods include:
Having sex
Gently stimulating your nipples
Herbal remedies including blue or black cohosh (some herbs can be dangerous if you don’t use them properly)
Drinking small amounts of castor oil (Recent, well-controlled studies say it’s safe during late pregnancy but castor oil can have unpleasant side effects, like diarrhea.
 )
)Walking
Don’t try any of these methods without first talking to your doctor or midwife. Some can cause side effects or pose risks.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Risk factors for drug-induced diseases. Part 1. Classification, non-modifiable risk factors » Doctor's Library
1) Russian Medical Academy of Continuing Professional Education, Moscow, Russia;
2) Central State Medical Academy of the Office of the President of the Russian Federation, Moscow, Russia;
3) First Moscow State Medical University. THEM. Sechenov (Sechenov University), Moscow, Russia
Drug-induced diseases (LIDs) are highly prevalent in the population and cause symptoms that require medical attention or lead to hospitalization, incl. to the intensive care unit, also a number of LIHs can increase mortality. Some patients are more predisposed to the development of LIS due to the presence of a number of risk factors (RFs). LIS risk factors are divided into general, specific for a particular drug (drug) or class of drugs, as well as specific risk factors that increase the risk of developing a particular LIS. General RFs include non-modifiable, partially modifiable and modifiable RFs. This article describes in detail the most important non-modifiable risk factors, the presence of which increases the likelihood of developing LIH, as well as examples of their clinical consequences and methods of prevention. Non-modifiable risk factors include older age, female sex, race, pregnancy, and genetic characteristics. For effective prevention of the development of LIH, it is important to assess the presence of risk factors for their development in a patient before starting to take drugs. In the case of detection of non-modifiable risk factors, it is necessary to use all known measures to prevent the development of potentially possible LID, to educate patients, in addition, it is very important to carefully monitor the condition of patients for the timely detection of potentially possible LID against the background of ongoing therapy.
to the intensive care unit, also a number of LIHs can increase mortality. Some patients are more predisposed to the development of LIS due to the presence of a number of risk factors (RFs). LIS risk factors are divided into general, specific for a particular drug (drug) or class of drugs, as well as specific risk factors that increase the risk of developing a particular LIS. General RFs include non-modifiable, partially modifiable and modifiable RFs. This article describes in detail the most important non-modifiable risk factors, the presence of which increases the likelihood of developing LIH, as well as examples of their clinical consequences and methods of prevention. Non-modifiable risk factors include older age, female sex, race, pregnancy, and genetic characteristics. For effective prevention of the development of LIH, it is important to assess the presence of risk factors for their development in a patient before starting to take drugs. In the case of detection of non-modifiable risk factors, it is necessary to use all known measures to prevent the development of potentially possible LID, to educate patients, in addition, it is very important to carefully monitor the condition of patients for the timely detection of potentially possible LID against the background of ongoing therapy. nine0005
nine0005
Introduction
Drug-induced illness (DID) is a variant of an adverse reaction (AE) that can increase mortality and/or morbidity and/or cause symptoms that compel the patient to seek medical attention or lead to hospitalization [1, 2]. LIDs are characterized by a high prevalence, an increased risk of hospitalizations, incl. in intensive care units, and mortality, they cause an increase in the cost of treatment (primarily the cost of hospitalization) [1, 2]. Mortality in hospitalized patients with LID can reach 5%, which is several times higher than the rate of hospital deaths from other causes [2]. Drug-induced symptoms, syndromes and diseases are very diverse, they develop against the background of taking almost all groups of drugs (drugs) with a greater or lesser probability, therefore they are found in the practice of doctors of all specialties. nine0005
Some patients are more likely to develop LID due to the presence of a number of risk factors (RFs). Risk factors for LYS are divided into general (RFs for the development of any LYS and / or development of LYS against the background of the use of any drugs), RFs for LIZs specific to a particular drug or class of drugs, as well as specific FRs that increase the risk of developing a particular LYS ( Table 1) [1–6].
General risk factors for the development of LIH are classified into non-modifiable, partially modifiable and modifiable (Table 1) [1, 3]. Non-modifiable risk factors include the patient's age, gender, race, pregnancy, and genetic characteristics [1, 3]. These RFs must be taken into account before prescribing drugs. In addition, all modifiable risk factors for LIH should be identified and, if possible, adjusted or minimized, which include smoking, alcohol abuse, drug abuse, interdrug interactions, drug-food interactions, low patient adherence to drug intake, errors in prescribing drugs [1, 3] . Those comorbid diseases that increase the likelihood of developing LIH can be attributed to partially modifiable risk factors. nine0005
Further in this article we will consider non-modifiable risk factors, the presence of which increases the likelihood of developing LIH.
Elderly and senile age
Elderly and senile age is considered one of the main risk factors for the development of LIH [1, 3].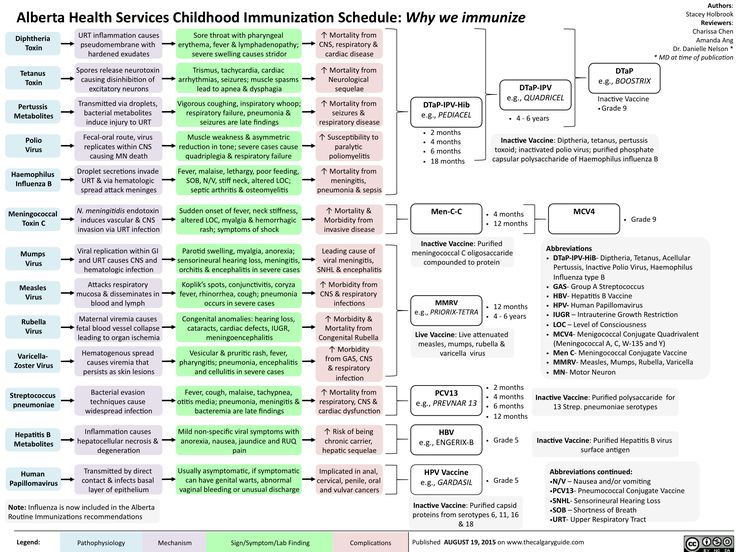 HP in the elderly is a frequent cause of hospitalization, occurs more frequently during hospitalization, and is more likely to cause morbidity and death [1, 3]. Thus, according to an observational study in Germany [7], the incidence of LID increased with increasing age from 3.8 per 10,000 treated patients not older than 30 years to 20 per 10,000 patients aged 70 years and older. In another observational study, also conducted in Germany [8], when comparing age groups nine0005
HP in the elderly is a frequent cause of hospitalization, occurs more frequently during hospitalization, and is more likely to cause morbidity and death [1, 3]. Thus, according to an observational study in Germany [7], the incidence of LID increased with increasing age from 3.8 per 10,000 treated patients not older than 30 years to 20 per 10,000 patients aged 70 years and older. In another observational study, also conducted in Germany [8], when comparing age groups nine0005
In a number of studies, the authors studied the occurrence of HP in older people who were in long-term care homes (nursing homes). Thus, in a prospective cohort study of patients in long-term care homes in the United States, it was shown that within 12 months, at least 14% of patients experienced AR [11]. In a study examining the hospitalization of HP-related nursing home residents, 15.7% of 332 nursing home residents had at least one hospitalization and this event was found to be directly related to the number of medications taken per day [12].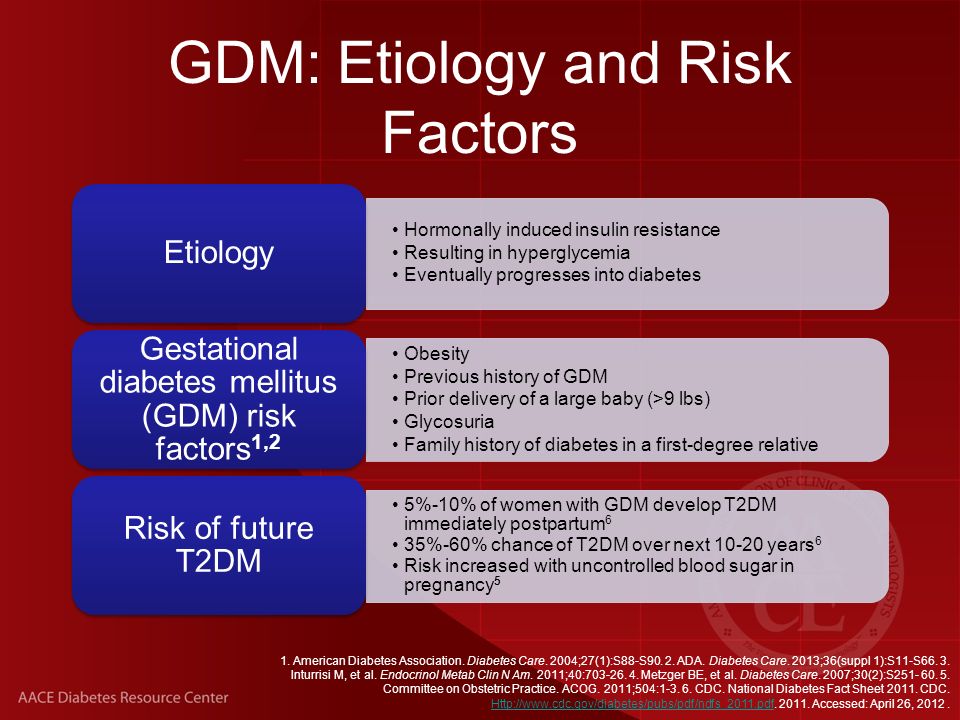 nine0005
nine0005
J. Stevenson et al. [13] expressed the belief that an integrated approach is needed for the prevention and correction of HP in the elderly, and the occurrence of HP in them should be considered as a geriatric syndrome (a multifactorial age-associated clinical condition that worsens the quality of life ...
D.A. Sychev, O. D. Ostroumova, M. S. Chernyaeva, A. P. Pereverzev, A. I. Kochetkov, T. M. Ostroumova, M. V. Klepikova, E. Yu. Ebzeeva, V. A. De
Induction of labor or induction of labor
The purpose of this information material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby, and it is not possible to wait for the onset of spontaneous labor.
The goal of stimulation is to initiate labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix in the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body. It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
- Balloon Catheter – A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination. nine0052
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already sufficiently dilated, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously administered synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions). The dose of the drug can be increased as needed to achieve regular uterine contractions.
 nine0052
nine0052
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy. nine0052
- Fetal problems, eg, fetal development problems, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
 nine0052
nine0052 - Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, the patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.