Can you have a natural birth with preeclampsia
Preeclampsia | March of Dimes
Preeclampsia is a pregnancy complication characterized primarily by high blood pressure, edema, and protein spillage in the urine-- occurring frequently after the 20th week of pregnancy or after giving birth.
Most pregnant women with preeclampsia have healthy babies. But if not treated, it can cause serious problems, like premature birth and even death.
If you’re at risk for preeclampsia, your provider may want you take low-dose aspirin to help prevent it.
If you have blurred vision, swelling in your hands and face or severe headaches or belly pain, call your provider right away.
You can have preeclampsia and not know it, so go to all of your prenatal care visits, even if you’re feeling fine.
Download our English and Spanish health action sheets on low-dose aspirin.
What is preeclampsia?
Preeclampsia is a serious blood pressure condition that can happen after the 20th week of pregnancy or after giving birth (called postpartum preeclampsia). It’s when a woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working normally. Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy.
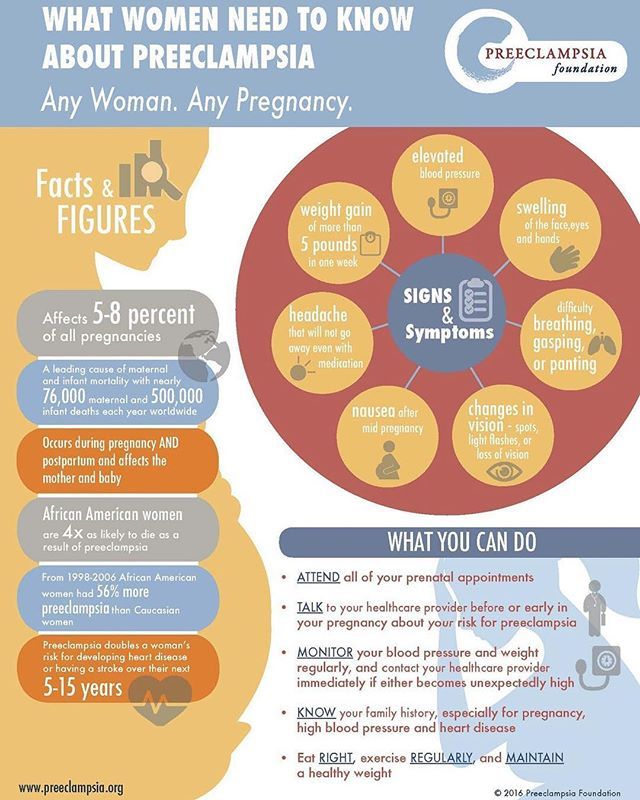
Preeclampsia is a serious health problem for women around the world. It affects 2 to 8 percent of pregnancies worldwide (2 to 8 in 100). In the United States, it’s the cause of 15 percent (about 3 in 20) of premature births. Premature birth is birth that happens too early, before 37 weeks of pregnancy.
Most women with preeclampsia have healthy babies. But if not treated, it can cause severe health problems for you and your baby.
Can taking low-dose aspirin help reduce your risk for preeclampsia and premature birth?
For some women, yes.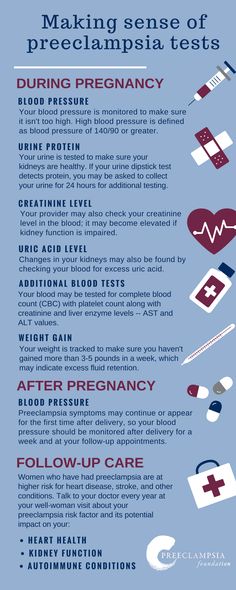 If your provider thinks you’re at risk for preeclampsia, he may want you to take low-dose aspirin to help prevent it. Low-dose aspirin also is called baby aspirin or 81 mg (milligrams) aspirin. Talk to your provider to see if treatment with low-dose aspirin is right for you.
If your provider thinks you’re at risk for preeclampsia, he may want you to take low-dose aspirin to help prevent it. Low-dose aspirin also is called baby aspirin or 81 mg (milligrams) aspirin. Talk to your provider to see if treatment with low-dose aspirin is right for you.
You can buy low-dose aspirin over-the-counter, or your provider can give you a prescription for it. A prescription is an order for medicine from your provider. If your provider wants you to take low-dose aspirin to help prevent preeclampsia, take it exactly as she tells you to. Don’t take more or take it more often than your provider says.
If you’re at high risk for preeclampsia, your provider may want you to start taking low-dose aspirin after 12 weeks of pregnancy. Or your provider may ask you to take low-dose aspirin if you have diabetes or high blood pressure. If your provider asks you to take low-dose aspirin, take it as recommended.
According to the American College of Obstetricians and Gynecologists (also called ACOG), daily low-dose aspirin use in pregnancy has a low risk of serious complications and its use is considered safe.
Are you at risk for preeclampsia?
We don’t know for sure what causes preeclampsia, but there are some things that may make you more likely than other women to have it. These are called risk factors. If you have even one risk factor for preeclampsia, tell your provider.
You’re at high risk for preeclampsia If:
- You’ve had preeclampsia in a previous pregnancy. The earlier in pregnancy you had preeclampsia, the higher your risk is to have it again. You’re also at higher risk if you had preeclampsia along with other pregnancy complications.
- You’re pregnant with multiples (twins, triplets or more).
- You have high blood pressure, diabetes, kidney disease or an autoimmune disease like lupus or antiphospholipid syndrome. Diabetes is when your body has too much sugar in the blood. This can damage organs, like blood vessels, nerves, eyes and kidneys. An autoimmune disease is a health condition that happens when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake.

Other risk factors for preeclampsia:
- You’ve never had a baby before, or it’s been more than 10 years since you had a baby.
- You’re obese. Obese means being very overweight with a body mass index (also called BMI) of 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi.
- You have a family history of preeclampsia. This means that other people in your family, like your sister or mother, have had it.
- You had complications in a previous pregnancy, like having a baby with low birthweight. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces.
- You had fertility treatment called in vitro fertilization (also called IVF) to help you get pregnant.
- You’re older than 35.
- You’re African-American. African-American women are at higher risk for preeclampsia than other women.
- You have low socioeconomic status (also called SES).
 SES is a combination of things, like a person’s education level, job and income (how much money you make). A person with low SES may have little education, may not have a job that pays well and may have little income or savings.
SES is a combination of things, like a person’s education level, job and income (how much money you make). A person with low SES may have little education, may not have a job that pays well and may have little income or savings.
What are the signs and symptoms of preeclampsia?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Signs and symptoms of preeclampsia include:
- Changes in vision, like blurriness, flashing lights, seeing spots or being sensitive to light
- Headache that doesn’t go away
- Nausea (feeling sick to your stomach), vomiting or dizziness
- Pain in the upper right belly area or in the shoulder
- Sudden weight gain (2 to 5 pounds in a week)
- Swelling in the legs, hands or face
- Trouble breathing
Many of these signs and symptoms are common discomforts of pregnancy.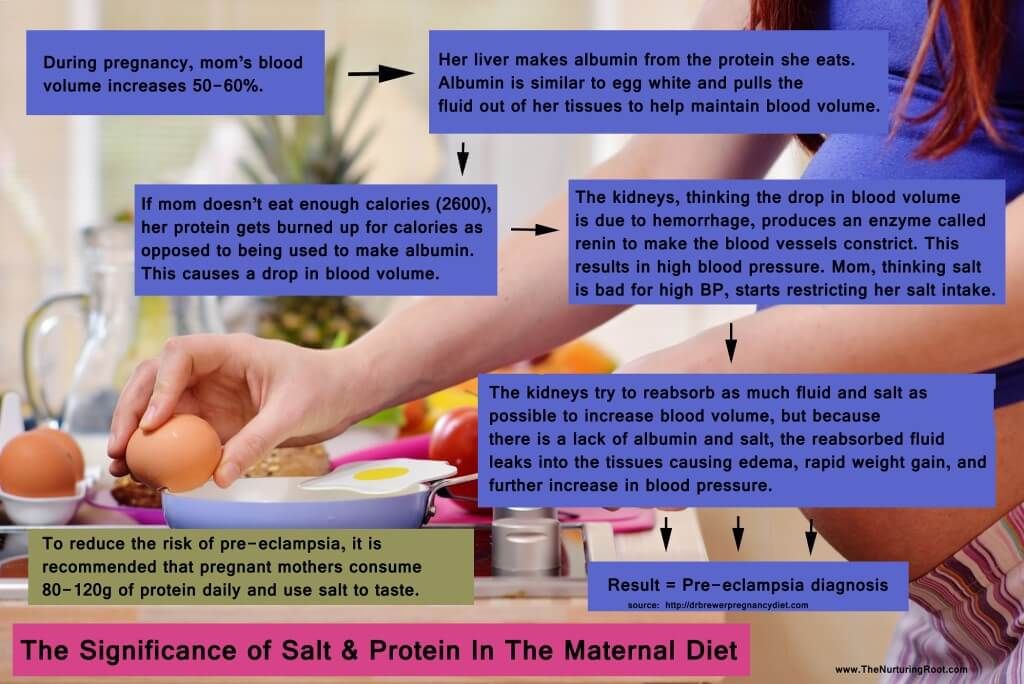 If you have even one sign or symptom, call your provider right away.
If you have even one sign or symptom, call your provider right away.
How can preeclampsia affect you and your baby?
Without treatment, preeclampsia can cause serious health problems for you and your baby, even death. You may have preeclampsia and not know it, so be sure to go to all your prenatal care checkups, even if you’re feeling fine. If you have any sign or symptom of preeclampsia, tell your provider.
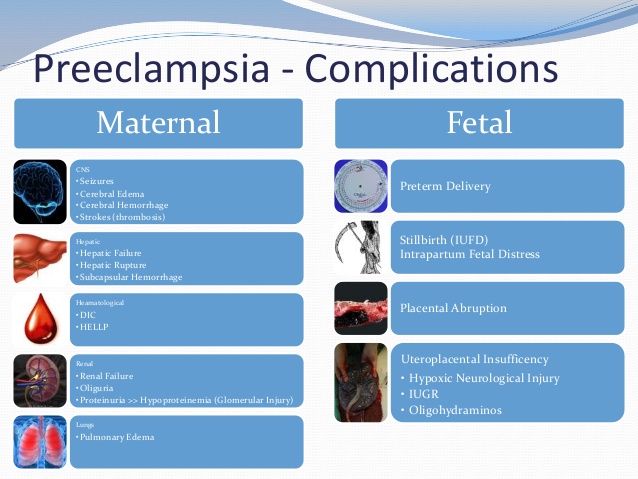
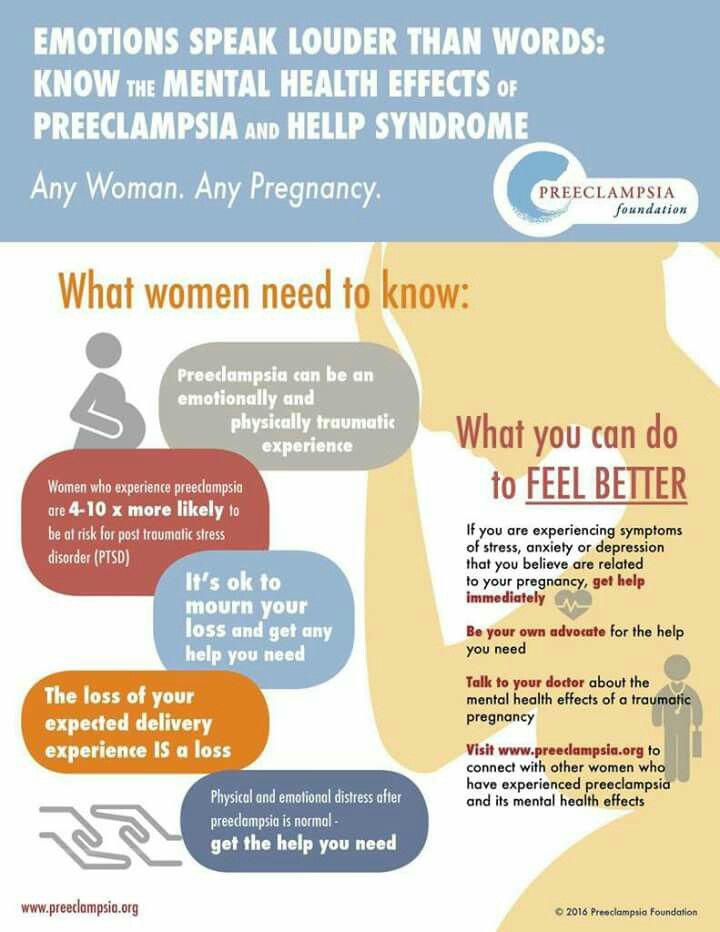
Health problems for women who have preeclampsia include:
- Kidney, liver and brain damage
- Problems with how your blood clots. A blood clot is a mass or clump of blood that forms when blood changes from a liquid to a solid. Your body normally makes blood clots to stop bleeding after a scrape or cut. Problems with blood clots can cause serious bleeding problems.
- Eclampsia. This is a rare and life-threatening condition. It’s when a pregnant woman has seizures or a coma after preeclampsia.
 A coma is when you’re unconscious for a long period of time and can't respond to voices, sounds or activity.
A coma is when you’re unconscious for a long period of time and can't respond to voices, sounds or activity. - Stroke. This is when the blood supply to the brain is interrupted or reduced. Stroke can happen when a blood clot blocks a blood vessel that brings blood to the brain, or when a blood vessel in the brain bursts open.
Pregnancy complications from preeclampsia include:
- Premature birth. Even with treatment, you may need to give birth early to help prevent serious health problems for you and your baby.
- Placental abruption. This is when the placenta separates from the wall of the uterus (womb) before birth. It can separate partially or completely. If you have placental abruption, your baby may not get enough oxygen and nutrients. Vaginal bleeding is the most common symptom of placental abruption after 20 weeks of pregnancy. If you have vaginal bleeding during pregnancy, tell your health care provider right away.
- Intrauterine growth restriction (also called IUGR). This is when a baby has poor growth in the womb. It can happen when mom has high blood pressure that narrows the blood vessels in the uterus and placenta. The placenta grows in the uterus and supplies your baby with food and oxygen through the umbilical cord. If your baby doesn’t get enough oxygen and nutrients in the womb, he may have IUGR.
- Low birthweight
Having preeclampsia increases your risk for postpartum hemorrhage (also called PPH). PPH is heavy bleeding after giving birth. It’s a rare condition, but if not treated, it can lead to shock and death. Shock is when your body’s organs don’t get enough blood flow.
Having preeclampsia increases your risk for heart disease, diabetes and kidney disease later in life.
How is preeclampsia diagnosed?
To diagnose preeclampsia, your provider measures your blood pressure and tests your urine for protein at every prenatal visit. Additional lab work evaluating your blood count, clotting factors, liver and kidney function are also assessed.
Additional lab work evaluating your blood count, clotting factors, liver and kidney function are also assessed.
Your provider may check your baby’s health with:
- Ultrasound. This is a prenatal test that uses sound waves and a computer screen to make a picture of your baby in the womb. Ultrasound checks that your baby is growing at a normal rate. It also lets your provider look at the placenta and the amount of fluid around your baby to make sure your pregnancy is healthy.
- Nonstress test. This test checks your baby’s heart rate.
- Biophysical profile. This test combines the nonstress test with an ultrasound.
- Doppler analysis. This is a sonographic test to evaluate the blood flow through the baby’s umbilical cord -- it can provide information as to how blood flow -- which carries oxygen - is getting to your baby
Treatment depends on how severe your preeclampsia is and how far along you are in your pregnancy. Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse.
Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse.
How is mild preeclampsia treated?
Most women with mild preeclampsia are delivered by 37 weeks of pregnancy . If you have mild preeclampsia before 37 weeks:
- Your provider checks your blood pressure and urine regularly. She may want you to stay in the hospital to monitor you closely. If you’re not in the hospital, your provider may want you to have checkups once or twice a week. She also may ask you to take your blood pressure at home.
- Your provider may ask you to do kick counts to track how often your baby moves. There are two ways to do kick counts: Every day, time how long it takes for your baby to move ten times. If it takes longer than 2 hours, tell your provider. Or three times a week, track the number of times your baby moves in 1 hour. If the number changes, tell your provider.
- If you’re at least 37 weeks pregnant and your condition is stable, your provider may recommend that you have your baby early.
 This may be safer for you and your baby than staying pregnant. Your provider may give you medicine or break your water (amniotic sac) to make labor start. This is called inducing labor.
This may be safer for you and your baby than staying pregnant. Your provider may give you medicine or break your water (amniotic sac) to make labor start. This is called inducing labor.
How is severe preeclampsia treated?
If you have severe preeclampsia, you most likely stay in the hospital so your provider can closely monitor you and your baby. Your provider may treat you with medicines called antenatal corticosteroids (also called ACS). These medicines help speed up your baby’s lung development. You also may get medicine to control your blood pressure and medicine to prevent seizures (called magnesium sulfate).
If your condition gets worse, it may be safer for you and your baby to give birth early. Most babies of moms with severe preeclampsia before 34 weeks of pregnancy do better in the hospital than by staying in the womb. If you’re at least 34 weeks pregnant, your provider may recommend that you have your baby as soon as your condition is stable. Your provider may induce your labor, or you may have a c-section. If you’re not yet 34 weeks pregnant but you and your baby are stable, you may be able to wait to have your baby.
Your provider may induce your labor, or you may have a c-section. If you’re not yet 34 weeks pregnant but you and your baby are stable, you may be able to wait to have your baby.
If you have severe preeclampsia and HELLP syndrome, you almost always need to give birth early. HELLP syndrome is a rare but life-threatening liver disorder. About 2 in 10 women (20 percent) with severe preeclampsia develop HELLP syndrome. You may need medicine to control your blood pressure and prevent seizures. Some women may need blood transfusions. A blood transfusion means you have new blood put into your body.
If you have preeclampsia, can you have a vaginal birth?
Yes. If you have preeclampsia, a vaginal birth may be better than a cesarean birth (also called c-section). A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. With vaginal birth, there's no stress from surgery. For most women with preeclampsia, it’s safe have an epidural to manage labor pain as long as your blood clots normally.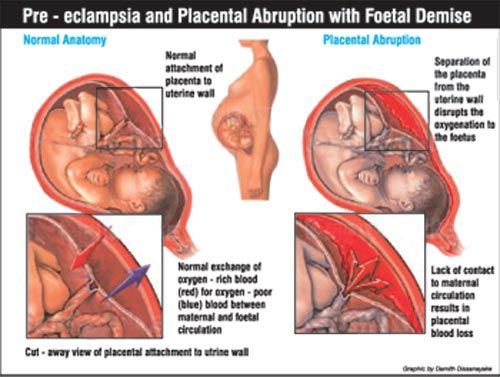 An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief during labor.
An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief during labor.
What is postpartum preeclampsia?
Postpartum preeclampsia is a rare condition. It’s when you have preeclampsia after you’ve given birth. It most often happens within 48 hours (2 days) of having a baby, but it can develop up to 6 weeks after a baby’s birth. It’s just as dangerous as preeclampsia during pregnancy and needs immediate treatment. If not treated, it can cause life-threatening problems, including death.
Signs and symptoms of postpartum preeclampsia are like those of preeclampsia. It can be hard for you to know if you have signs and symptoms after pregnancy because you’re focused on caring for your baby. If you do have signs or symptoms, tell your provider right away.
We don’t know exactly what causes postpartum preeclampsia, but these may be possible risk factors:
- You had gestational hypertension or preeclampsia during pregnancy.
 Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth.
Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth. - You’re obese.
- You had a c-section.
Complications from postpartum preeclampsia include these life-threatening conditions:
- HELLP syndrome
- Postpartum eclampsia (seizures). This can cause permanent damage to our brain, liver and kidneys. It also can cause coma.
- Pulmonary edema. This is when fluid fills the lungs.
- Stroke
- Thromboembolism. This is when a blood clot travels from another part of the body and blocks a blood vessel.
Your provider uses blood and urine tests to diagnose postpartum preeclampsia. Treatment can include magnesium sulfate to prevent seizures and medicine to help lower your blood pressure. Medicine to prevent seizures also is called anticonvulsive medicine. If you’re breastfeeding, talk to your provider to make sure these medicines are safe for your baby.
Reviewed October 2020
Planned caesarean section versus planned vaginal birth for severe pre-eclampsia
Language:
- English
- Deutsch
- Español
- فارسی
- Bahasa Malaysia
- Português
More languages available
Show fewer languages
Cochrane Evidence Synthesis and Methods ►
What is the issue?
To assess the effects of a policy of planned caesarean section versus planned vaginal birth for women with severe pre-eclampsia on mortality and morbidity for mother and baby.
Why is this important?
Pre-eclampsia is a very frequent problem during pregnancy that affects up to one in 10 pregnant women. Pregnant women with pre-eclampsia have symptoms such as high blood pressure, headache, problems with vision and swelling of hands, legs or feet. If untreated, serious pre-eclampsia may lead to poor health or even death both for pregnant women and for their babies. More women in low-income countries and in difficult economic circumstances suffer and die from pre-eclampsia. The only definitive treatment for this illness is the birth of the infant. It is therefore very common for doctors and pregnant women with serious pre-eclampsia to discuss delivering the baby after 34 or 37 weeks of pregnancy, with the timing dependent upon the health of the mother and the baby. We wanted to know whether planned caesarean section or planned vaginal birth was safest for women with serious pre-eclampsia and their babies.
Serious pre-eclampsia is one of the most common reasons for pregnant women to give birth early. Often the baby needs to be born before a woman is in labour. Many doctors prefer to perform caesareans for women with serious pre-eclampsia, even when the baby is healthy. Nevertheless, observational studies have demonstrated that caesarean section may worsen the outlook for mother and baby, with an increased risk of complications.The best way to deliver the baby for women with serious pre-eclampsia is not yet known.
Often the baby needs to be born before a woman is in labour. Many doctors prefer to perform caesareans for women with serious pre-eclampsia, even when the baby is healthy. Nevertheless, observational studies have demonstrated that caesarean section may worsen the outlook for mother and baby, with an increased risk of complications.The best way to deliver the baby for women with serious pre-eclampsia is not yet known.
What evidence did we find?
Randomised clinical trials are considered to be the best way to test different treatment options and decide which treatment is safer and better overall. We searched for studies on 6 September 2017, but did not find any randomised clinical trials comparing planned caesarean section versus planned vaginal birth for women with severe pre-eclampsia. There is no evidence from RCTs to help decide which type of birth is better for pregnant women with serious pre-eclampsia and their babies.
What does this mean?
We do not have any information from randomised clinical trials to assess whether caesarean section or vaginal birth is better for pregnant women with severe pre-eclampsia, and their babies.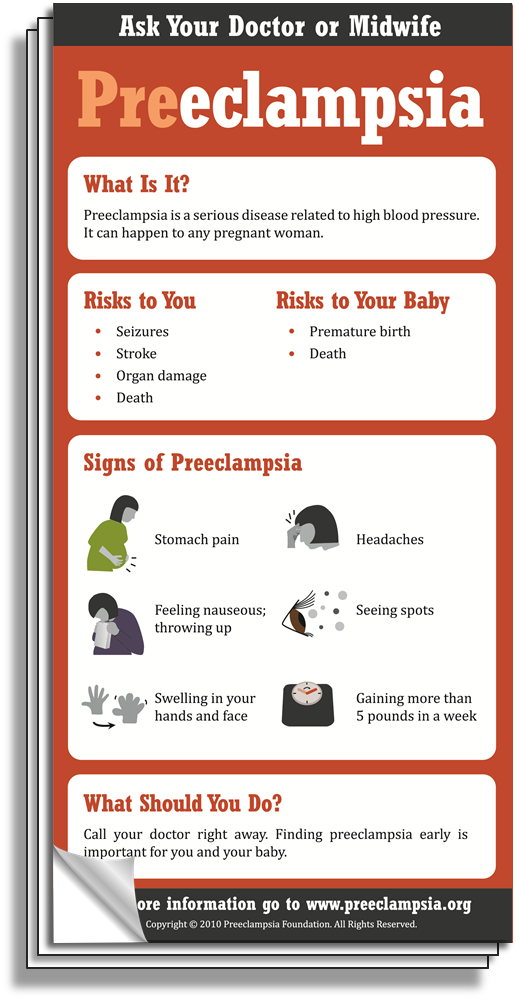 Until such time as we have good randomised clinical trials, pregnant women with severe pre-eclampsia need to talk with their doctors about their options for delivering their baby safely and with the best possible results. Doctors and pregnant women can then decide together if caesarean section or vaginal birth is best for the short- and long-term health of mother and baby.
Until such time as we have good randomised clinical trials, pregnant women with severe pre-eclampsia need to talk with their doctors about their options for delivering their baby safely and with the best possible results. Doctors and pregnant women can then decide together if caesarean section or vaginal birth is best for the short- and long-term health of mother and baby.
Authors' conclusions:
There is a lack of robust evidence from randomised controlled trials that can inform practice regarding planned caesarean section versus planned vaginal birth for women with severe pre-eclampsia. There is a need for high-quality randomised controlled trials to assess the short- and long-term effects of caesarean section and vaginal birth for these women and their babies.
Read the full abstract...
Background:
Pre-eclampsia is a very frequent complication of pregnancy, and anticipation of birth is often necessary. However, the best mode of giving birth remains to be established, although observational studies suggest better maternal and perinatal outcomes with vaginal birth.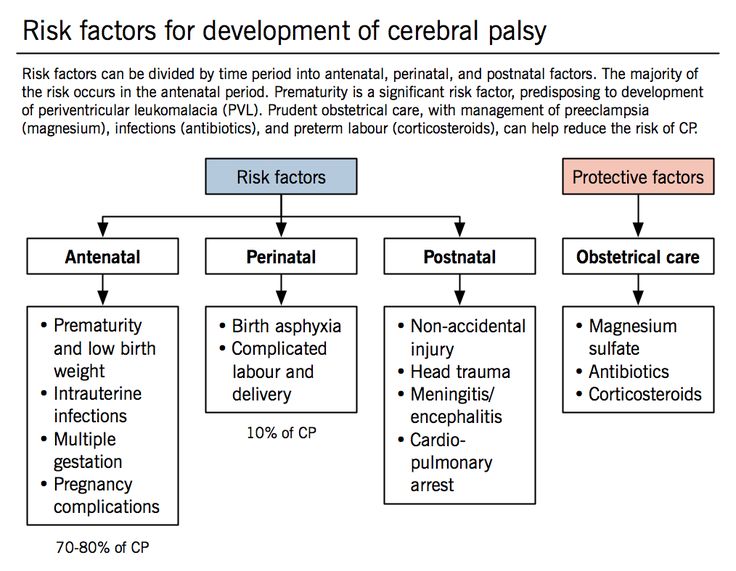
Objectives:
To assess the effects of a policy of planned caesarean section versus planned vaginal birth for women with severe pre-eclampsia on mortality and morbidity for mother and baby.
Search strategy:
We searched Cochrane Pregnancy and Childbirth's Trials Register, ClinicalTrials.gov, the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (6 September 2017) and reference lists of retrieved studies.
Selection criteria:
We planned to include all randomised trials of planned caesarean section versus planned vaginal birth for pregnant women with severe pre-eclampsia. Quasi-randomised and non-randomised studies are not eligible for inclusion in this review.
The focus of this review is severe pre-eclampsia; studies of planned caesarean section versus planned vaginal birth in pregnant women with eclampsia are not eligible for inclusion.
Data collection and analysis:
We identified no studies that met the inclusion criteria.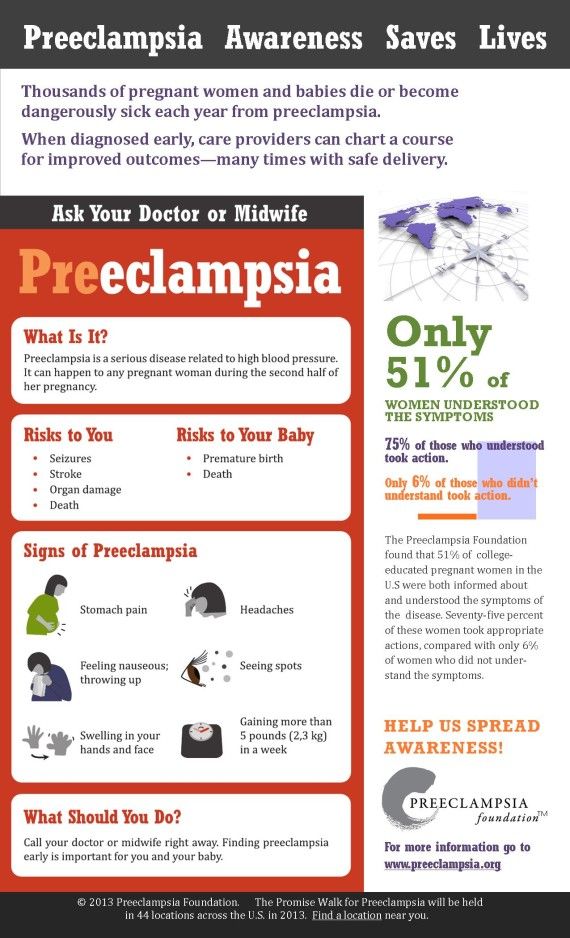 We excluded two studies.
We excluded two studies.
Main results:
There are no included studies in this review.
Health topics:
Pregnancy & childbirth > Caesarian section > Other interventions
Preeclampsia and pregnancy | Ida-Tallinna Keskaigla
Preeclampsia and pregnancy
The purpose of this information leaflet is to provide the patient with information about the nature, occurrence, risk factors, symptoms and treatment of preeclampsia.
What is preeclampsia?
Pre-eclampsia is a disease that occurs during pregnancy and is characterized by high blood pressure and protein in the urine. Preeclampsia is one of the most common complications of pregnancy. Epilepsy-like seizures occur in severe preeclampsia and are life-threatening. nine0005
What symptoms may indicate the development of preeclampsia?
High blood pressure - blood pressure values are 140/90 mmHg. Art. or higher. If systolic (upper) or diastolic (lower) blood pressure rises by 30 mm Hg. Art. or more, then such an increase cannot be ignored.
Art. or higher. If systolic (upper) or diastolic (lower) blood pressure rises by 30 mm Hg. Art. or more, then such an increase cannot be ignored.
Protein in urine - 300 mg in urine collected over 24 hours, or +1 value on a rapid test.
Swelling of the arms, legs or face , especially under the eyes or if the skin is pitted when pressed. Edema can occur in all pregnant women and is generally harmless, but rapidly developing edema should be taken into account.
Headache that does not improve after taking pain medication.
Visual disturbances - double vision or blurred vision, dots or flashes before the eyes, auras.
Nausea or pain in the upper abdomen - These symptoms are often mistaken for indigestion or gallbladder pain. Nausea in the second half of pregnancy is not normal.
Sudden weight gain - 2 kg or more per week.
As a rule, there is a mild course of the disease that occurs at the end of pregnancy and has a good prognosis.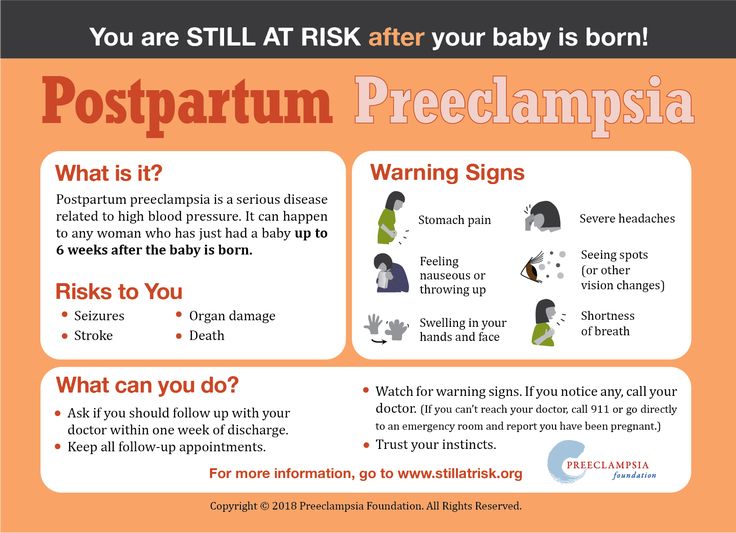 Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance. nine0005
Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance. nine0005
Unfortunately, most women develop symptoms in the final stages of the disease. If you experience any of the above symptoms, you should contact your midwife, gynecologist, or the Women's Clinic emergency department.
Is preeclampsia called toxemia of pregnancy?
Previously, pre-eclampsia was really called toxicosis, or toxemia, since it was believed that the cause of the disease was toxins, that is, poisons in the blood of a pregnant woman.
What is the difference between preeclampsia and gestational hypertension?
Pregnancy hypertension is an increase in blood pressure above normal after the 20th week of pregnancy. With hypertension of pregnant women, protein in the urine is not observed.
What is HELLP syndrome?
HELLP syndrome is one of the most severe forms of preeclampsia. HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold. nine0005
HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold. nine0005
When does preeclampsia occur?
Preeclampsia usually occurs after the 20th week of pregnancy. As a rule, preeclampsia goes away after delivery, but complications can occur up to six weeks after delivery, during which careful monitoring of the condition is necessary. If by the sixth week after birth, blood pressure does not return to normal, then you need to contact a cardiologist, who will begin treatment against hypertension.
What is the cause of preeclampsia? nine0004
The causes of the disease are still not clear, there are only unproven hypotheses.
How does the disease affect pregnant women and pregnancy?
Most preeclamptic pregnancies have a favorable outcome and a healthy baby is born. However, the disease is very serious and is one of the most common causes of death of the child and mother.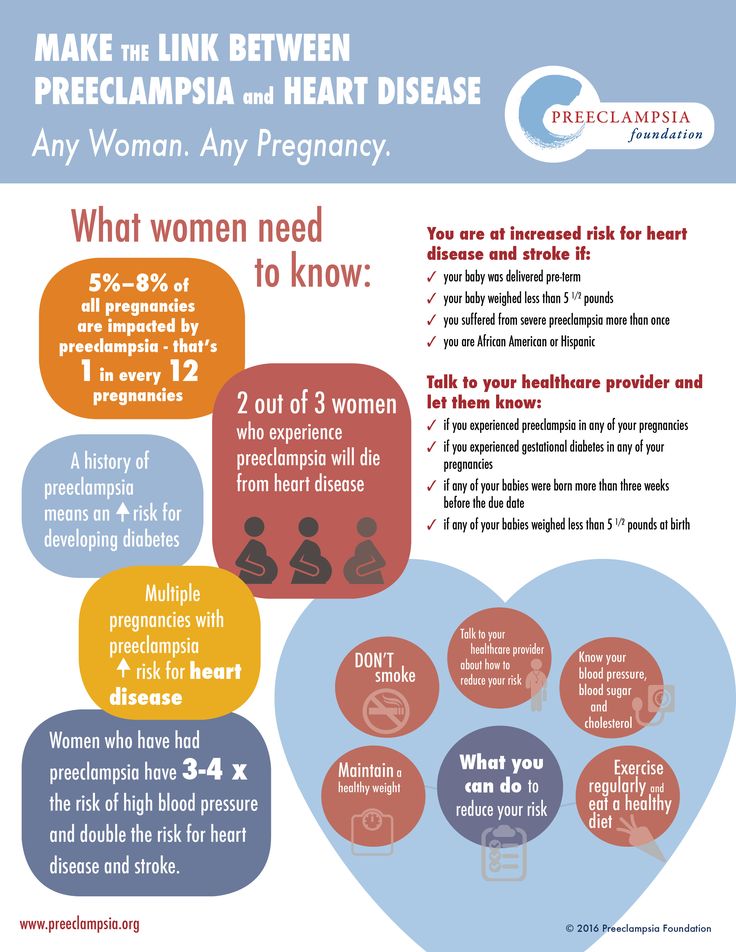 Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death. nine0005
Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death. nine0005
How does the disease affect the fetus?
In preeclampsia, the fetus does not receive enough oxygen and nutrients to grow, and intrauterine growth retardation may occur. In addition, the placenta may separate from the uterine wall before the baby is born. Since the only treatment for preeclampsia is childbirth, sometimes a pregnancy has to be terminated prematurely. Until the 34th week of pregnancy, the lungs of the fetus have not yet matured, and steroid hormones are injected intramuscularly into the pregnant woman to prepare his lungs. In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases. nine0005
Who is at risk of developing preeclampsia?
Preeclampsia occurs in approximately 8% of pregnant women, many of whom have no known risk factors.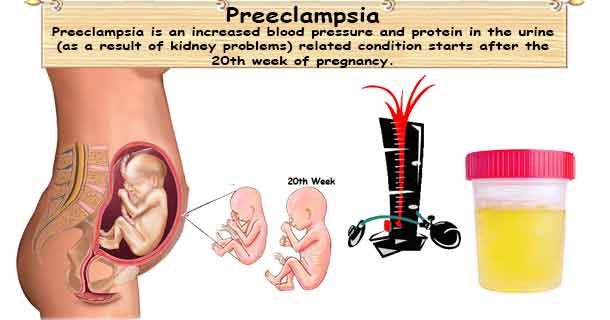
What are the risk factors for preeclampsia?
Patient-related risk factors
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- High blood pressure before pregnancy
- Diabetes before or during pregnancy
- Multiple pregnancy
- Overweight (BMI> 30)
- Systemic lupus erythematosus or other autoimmune disease
- Polycystic ovary syndrome
- Long interval between two pregnancies
Risk factors associated with the patient's family
- Pre-eclampsia in the mother's or father's family
- Parental high blood pressure or heart disease
- Diabetes mellitus
What is the prevention and treatment of preeclampsia
The first trimester screening or Oscar test also calculates the risk of preeclampsia in addition to the most common chromosomal disorders.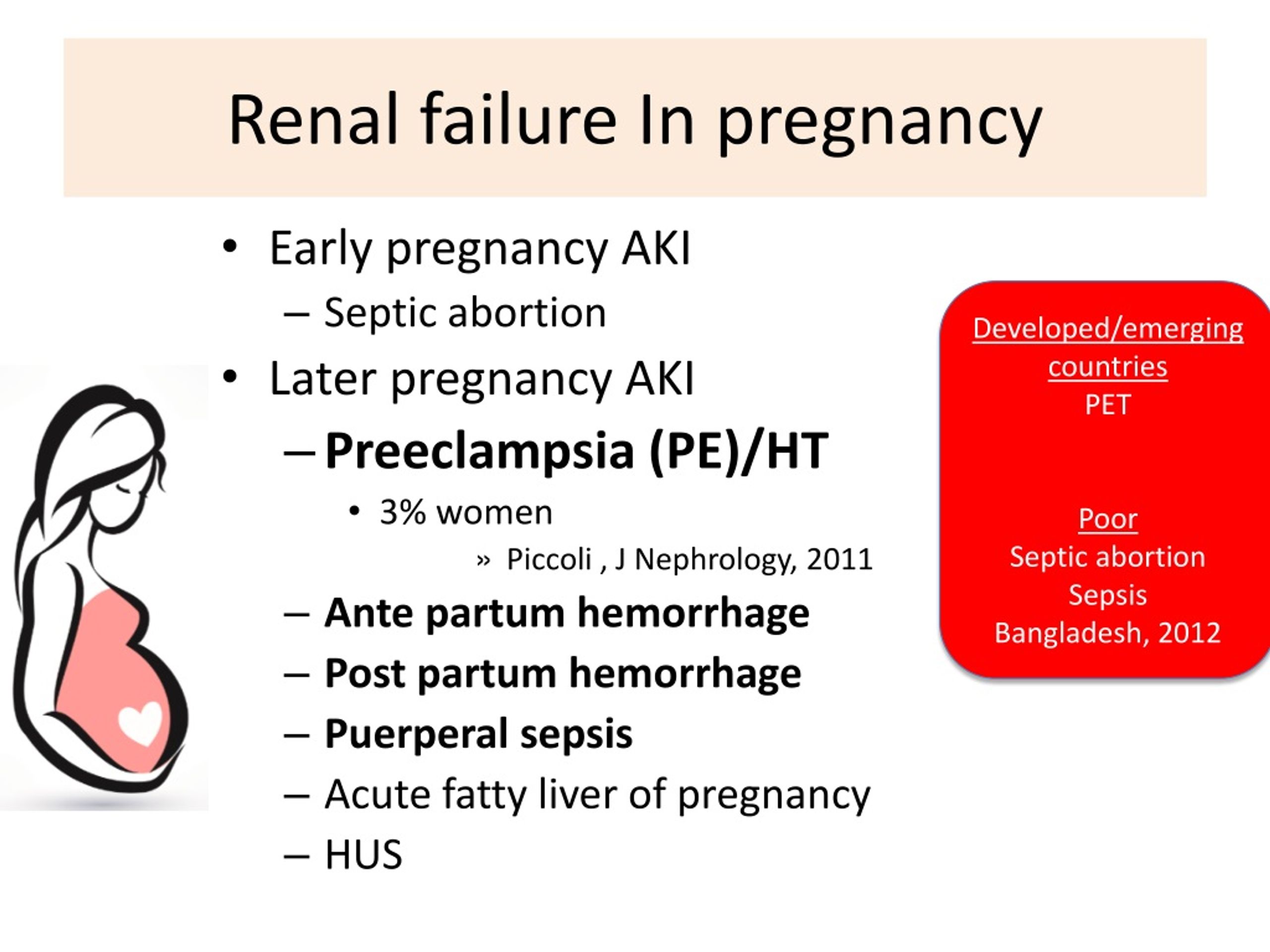 In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0005
In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0005
Childbirth is the only treatment for preeclampsia. Sometimes a child can be born naturally, but sometimes, if the disease is very acute, an emergency caesarean section is necessary. The best time to have a baby is after the 37th week of pregnancy. Bed rest, medications, and, if necessary, hospitalization can sometimes help bring the condition under control and prolong the pregnancy. Often, a doctor will refer a woman with preeclampsia to the hospital for observation, as the condition of the fetus and pregnant woman may suddenly worsen. nine0005
Does bed rest help?
Sometimes bed rest is enough to control mild preeclampsia. In this case, the patient often visits a doctor who measures blood pressure, does blood and urine tests, and monitors the course of the disease. The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
Are drugs used to treat preeclampsia?
High blood pressure sometimes requires medication. The medications used have few side effects, the drugs prescribed do not have much effect on the fetus, but are very important in the treatment of maternal high blood pressure. nine0005
Seizures are a rare but very serious complication of preeclampsia. Magnesium sulfate is sometimes given intravenously to prevent seizures in a pregnant woman with preeclampsia both during and after childbirth. It is safe for the fetus, but the mother may experience side effects such as hot flashes, sweating, thirst, visual disturbances, mild confusion, muscle weakness, and shortness of breath. All these side effects disappear when the drug is discontinued.
Can preeclampsia recur? nine0004
Preeclampsia does not necessarily recur in the next pregnancy, but the main risk factor for preeclampsia is the presence of preeclampsia in a previous pregnancy(s).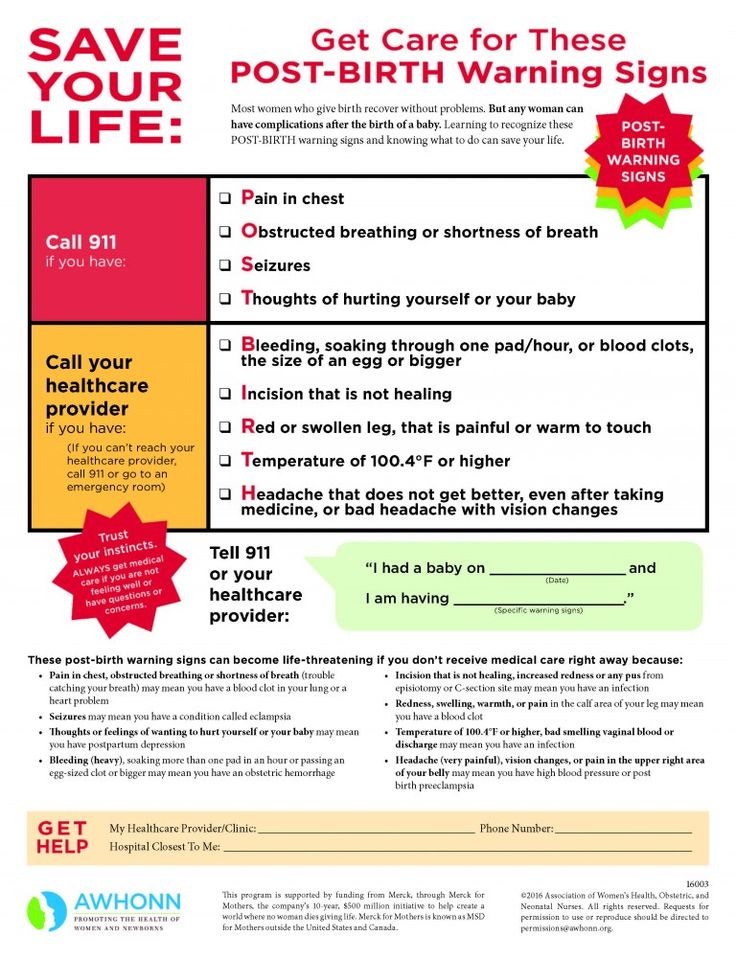 Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
ITK1013
The information material was approved by the Health Care Quality Committee of East-Tallinn Central Hospital on 11/30/2022 (Minutes No. 18-22).
Is it safer to induce labor immediately or wait if the mother has elevated but not persistently high blood pressure after 34 weeks of pregnancy?
What is the problem?
Women with high blood pressure (hypertension) during pregnancy or who develop preeclampsia (high blood pressure with protein in the urine or involvement of other organs or systems, or both) can develop serious complications. Possible maternal complications include worsening preeclampsia, seizures and eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), placental abruption, liver failure, kidney failure, and breathing problems due to fluid buildup in the lungs.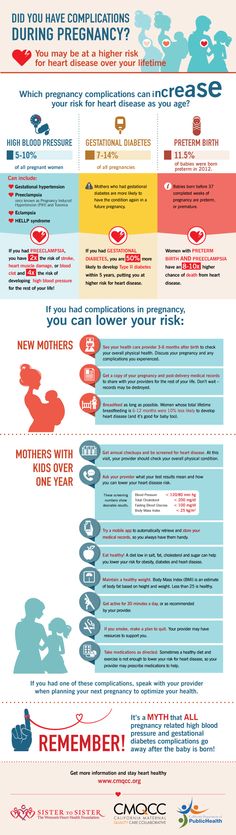 . nine0005
. nine0005
Delivery usually prevents worsening of hypertension, but a premature baby has other health problems, such as respiratory problems due to lung immaturity. Inducing labor can lead to overstimulation of contractions and fetal distress. Another option is to wait for natural childbirth, carefully monitoring the condition of the mother and child.
Why is this important?
Because there are benefits and risks to both planned preterm birth and expectant management when the mother has high blood pressure towards the end of pregnancy, we wanted to know which was the safest strategy. We reviewed clinical trials that compared planned preterm delivery by induced labor versus caesarean section versus expectant management. nine0005
What evidence did we find?
We searched for evidence up to 12 January 2016 and found five randomized trials involving 1819 women. The two studies were large and of high quality and included 704 women with gestational hypertension, mild preeclampsia, or exacerbation of existing hypertension at 34–37 weeks, and 756 pregnant women with hypertension or mild preeclampsia at 36–41 weeks.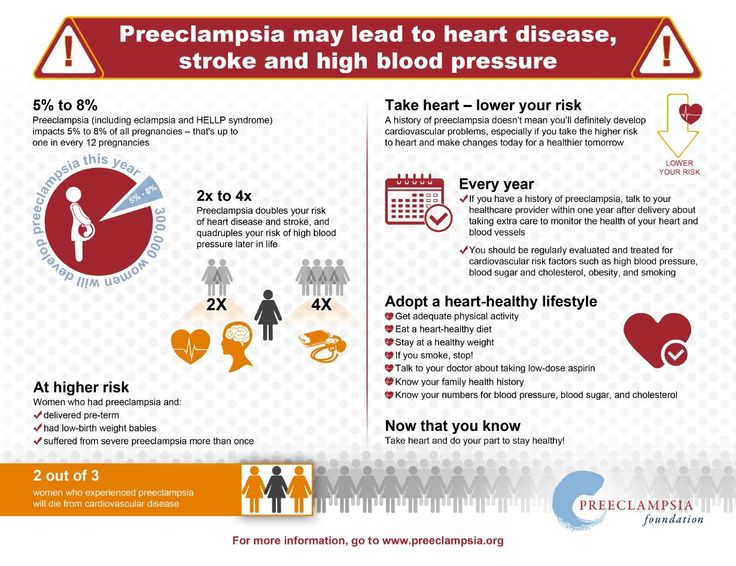 . Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate-quality evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women).
. Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate-quality evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women). nine0005
nine0005
Two studies compared women with preterm labor at 34 to 36 weeks and 34 to 37 weeks of gestation with a control group who followed up to 37 weeks when labor was induced if it did not start spontaneously. Three studies compared women in induced labor with a normal or near-normal duration of pregnancy at 37 completed weeks and between 36 and 41 weeks and women seen before 41 weeks when labor was induced if they didn't start spontaneously. Inclusion and exclusion criteria also differed across the five studies. nine0005
Information regarding which study group women belonged to was not withheld from both women and clinicians. Women and staff were made aware of this intervention, which could affect aspects of care and decision making. Most of the evidence was of moderate quality, so we can be relatively confident in the results.
What does this mean?
In general, if labor was induced immediately after 34 weeks of gestation, the risk of complications for the mother was lower and there was generally no apparent difference in the rate of complications for the baby, but information was limited.