Treating pelvic girdle pain
Pelvic pain in pregnancy - NHS
Some women may develop pelvic pain in pregnancy. This is sometimes called pregnancy-related pelvic girdle pain (PGP) or symphysis pubis dysfunction (SPD).
PGP is a collection of uncomfortable symptoms caused by a stiffness of your pelvic joints or the joints moving unevenly at either the back or front of your pelvis.
Symptoms of PGP
PGP is not harmful to your baby, but it can be painful and make it hard to get around.
Women with PGP may feel pain:
- over the pubic bone at the front in the centre, roughly level with your hips
- across 1 or both sides of your lower back
- in the area between your vagina and anus (perineum)
- spreading to your thighs
Some women may feel or hear a clicking or grinding in the pelvic area.
The pain can be worse when you're:
- walking
- going up or down stairs
- standing on 1 leg (for example, when you're getting dressed)
- turning over in bed
- moving your legs apart (for example, when you get out of a car)
Most women with PGP can have a vaginal birth.
Non-urgent advice: Call your midwife or GP if you have pelvic pain and:
- it's hard for you to move around
- it hurts to get out of a car or turn over in bed
- it's painful going up or down stairs
These can be signs of pregnancy-related pelvic girdle pain.
Treatments for PGP
Getting diagnosed as early as possible can help keep pain to a minimum and avoid long-term discomfort.
You can ask your midwife for a referral to a physiotherapist who specialises in obstetric pelvic joint problems.
Physiotherapy aims to relieve or ease pain, improve muscle function, and improve your pelvic joint position and stability.
This may include:
- manual therapy to make sure the joints of your pelvis, hip and spine move normally
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice and suggestions, including positions for labour and birth, looking after your baby and positions for sex
- pain relief, such as TENS
- equipment, if necessary, such as crutches or pelvic support belts
These problems tend not to get completely better until the baby is born, but treatment from an experienced practitioner can improve the symptoms during pregnancy.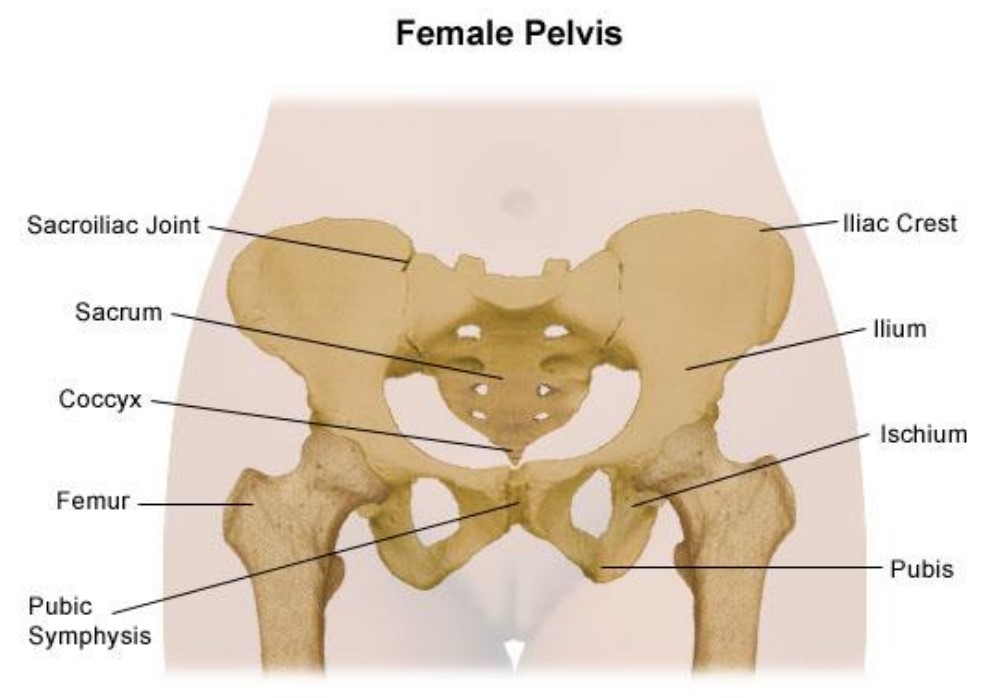
You can contact the Pelvic Partnership for information and support.
Coping with pelvic pain in pregnancy
Your physiotherapist may recommend a pelvic support belt to help ease your pain, or crutches to help you get around.
It can help to plan your day so you avoid activities that cause you pain. For example, do not go up or down stairs more often than you have to.
The Pelvic, Obstetric & Gynaecological Physiotherapy (POGP) network also offers this advice:
- be as active as possible within your pain limits, and avoid activities that make the pain worse
- rest when you can
- ask your family, friends or partner, if you have one, to help with everyday activities
- wear flat, supportive shoes
- sit down to get dressed – for example, do not stand on 1 leg when putting on jeans
- keep your knees together when getting in and out of the car – a plastic bag on the seat can help you swivel
- sleep in a comfortable position – for example, on your side with a pillow between your legs
- try different ways of turning over in bed – for example, turning over with your knees together and squeezing your buttocks
- take the stairs 1 at a time, or go upstairs backwards or on your bottom
- if you're using crutches, have a small backpack to carry things in
- if you want to have sex, consider different positions, such as kneeling on all fours
POGP suggests that you avoid:
- standing on 1 leg
- bending and twisting to lift, or carrying a baby on 1 hip
- crossing your legs
- sitting on the floor, or sitting twisted
- sitting or standing for long periods
- lifting heavy weights, such as shopping bags, wet washing or a toddler
- vacuuming
- pushing heavy objects, such as a supermarket trolley
- carrying anything in only 1 hand (try using a small backpack)
The physiotherapist should be able to provide advice on coping with the emotional impact of living with chronic pain, such as using relaxation techniques. If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
Download the POGP leaflet Pregnancy-related pelvic girdle pain for mothers-to-be and new mothers.
You can get more information on managing everyday activities with PGP from the Pelvic Partnership.
Labour and birth with pelvic pain
Many women with pelvic pain in pregnancy can have a normal vaginal birth.
Plan ahead and talk about your birth plan with your birth partner and midwife.
Write in your birth plan that you have PGP, so the people supporting you during labour and birth will be aware of your condition.
Think about birth positions that are the most comfortable for you, and write them in your birth plan.
Being in water can take the weight off your joints and allow you to move more easily, so you might want to think about having a water birth.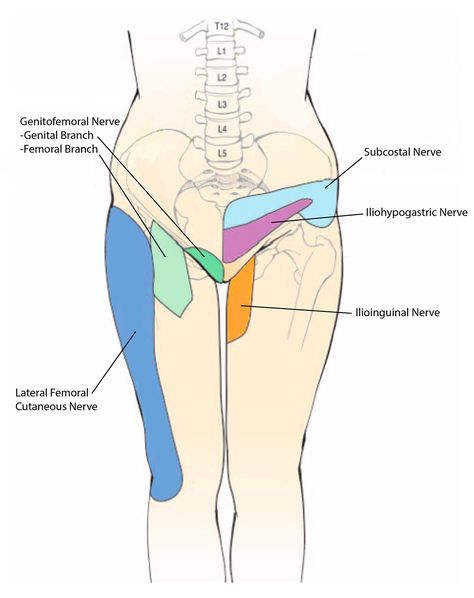 You can discuss this with your midwife.
You can discuss this with your midwife.
Your 'pain-free range of movement'
If you have pain when you open your legs, find out your pain-free range of movement.
To do this, lie on your back or sit on the edge of a chair and open your legs as far as you can without pain.
Your partner or midwife can measure the distance between your knees with a tape measure. This is your pain-free range.
To protect your joints, try not to open your legs wider than this during labour and birth.
This is particularly important if you have an epidural for pain relief in labour, as you won't be feeling the pain that warns you that you're separating your legs too far.
If you have an epidural, make sure your midwife and birth partner are aware of your pain-free range of movement of your legs.
When pushing in the second stage of labour, you may find it beneficial to lie on one side.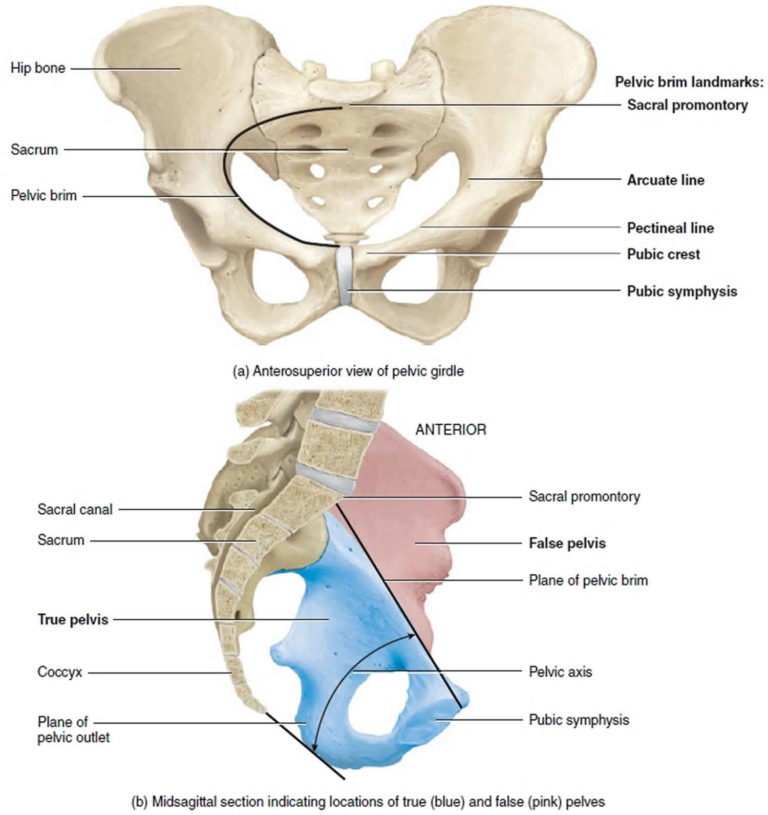
This prevents your legs from being separated too much. You can stay in this position for the birth of your baby, if you wish.
Sometimes it might be necessary to open your legs wider than your pain-free range to deliver your baby safely, particularly if you have an assisted delivery (for example, with the vacuum or ventouse).
Even in this case, it's possible to limit the separation of your legs. Make sure your midwife and doctor are aware that you have PGP.
If you go beyond your pain-free range, your physiotherapist should assess you after the birth.
Take extra care until they have assessed and advised you.
Who gets pelvic pain in pregnancy?
It's estimated that PGP affects up to 1 in 5 pregnant women to some degree.
It's not known exactly why pelvic pain affects some women, but it's thought to be linked to a number of issues, including previous damage to the pelvis, pelvic joints moving unevenly, and the weight or position of the baby.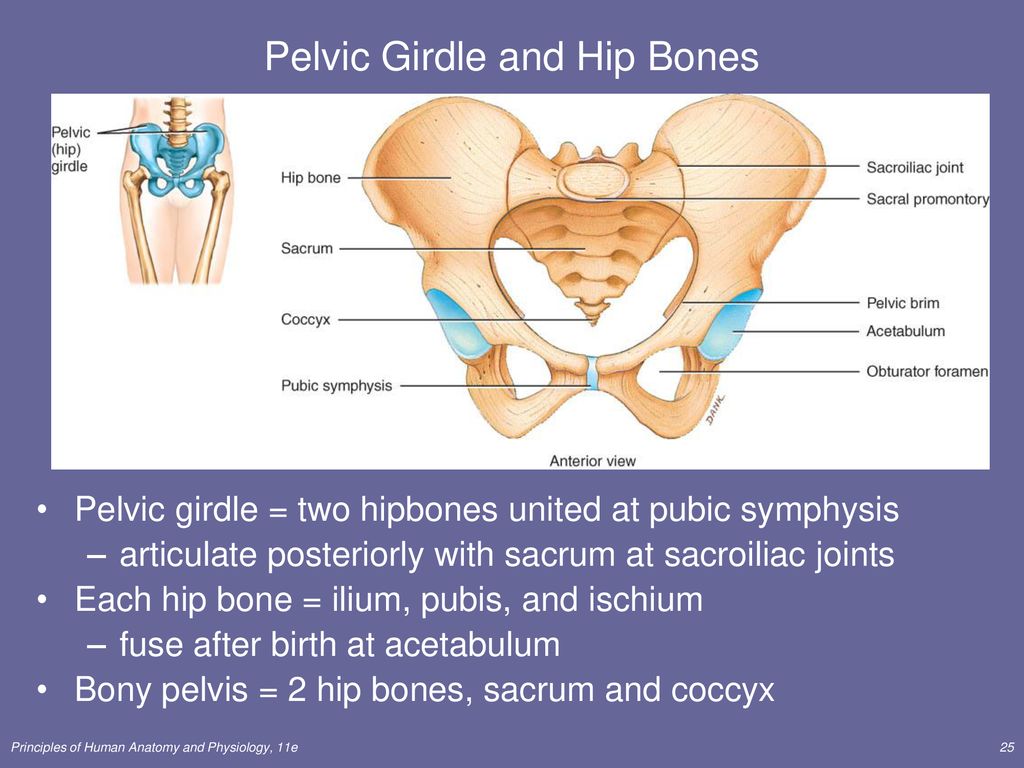
Factors that may make a woman more likely to develop PGP include:
- a history of lower back or pelvic girdle pain
- previous injury to the pelvis (for example, from a fall or accident)
- having PGP in a previous pregnancy
- a physically demanding job
- being overweight
- having a multiple birth pregnancy
healthtalk.org has interviews with women talking about their experiences of pelvic pain in pregnancy.
Read more about coping with common pregnancy problems, including nausea, heartburn, tiredness and constipation.
Find maternity services or physiotherapy services near you.
Community content from HealthUnlocked5 Ways to Get Pelvic Girdle Pain Relief During Pregnancy
pelvic floor postpartum care Sep 10, 2020
You don't have to accept pelvic girdle pain as a part of your pregnancy.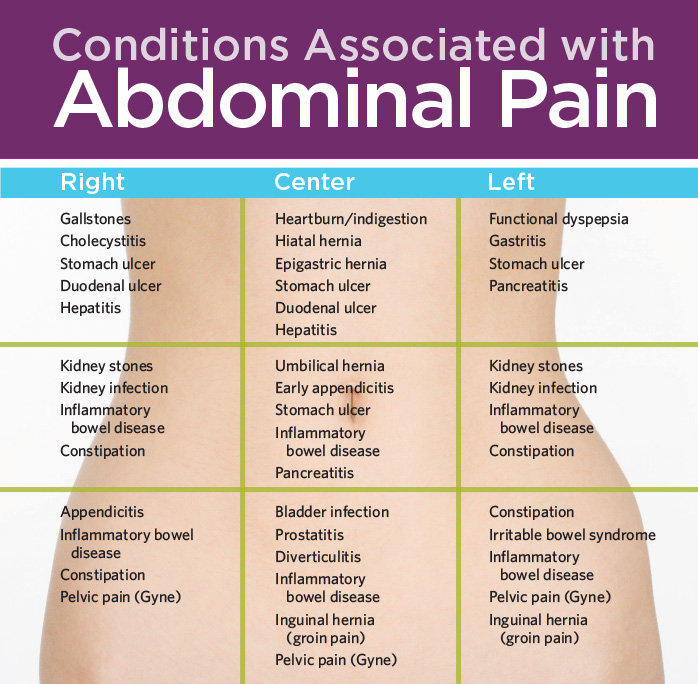 But did you know that it's so common that 25% of pregnant women will suffer from some kind of PGP through their pregnancy. We call this pregnancy-related PGP.
But did you know that it's so common that 25% of pregnant women will suffer from some kind of PGP through their pregnancy. We call this pregnancy-related PGP.
Trusted by thousands of women worldwide, PregActive has helped pregnant women enjoy a stronger, fitter and healthier pregnancy.
Will Pelvic Girdle Pain affect my baby or my labour?
While it may impact on you, it will not affect your baby in any way.
Will my pelvic pain persist after childbirth?
PGP can be managed throughout your pregnancy and most PGP recovers completely after childbirth. However, approximately 7-10% of cases can continue with pain. This is when you should book in an appointment with your physical therapists or physiotherapist.
5 Best Exercises for Pelvic Pain Pregnancy
What is Pelvic Girdle Pain?
Pelvic Girdle Pain (or PGP) refers to pain around the pelvis, usually focusing at your two sacroiliac joints, groin and your pubic symphysis.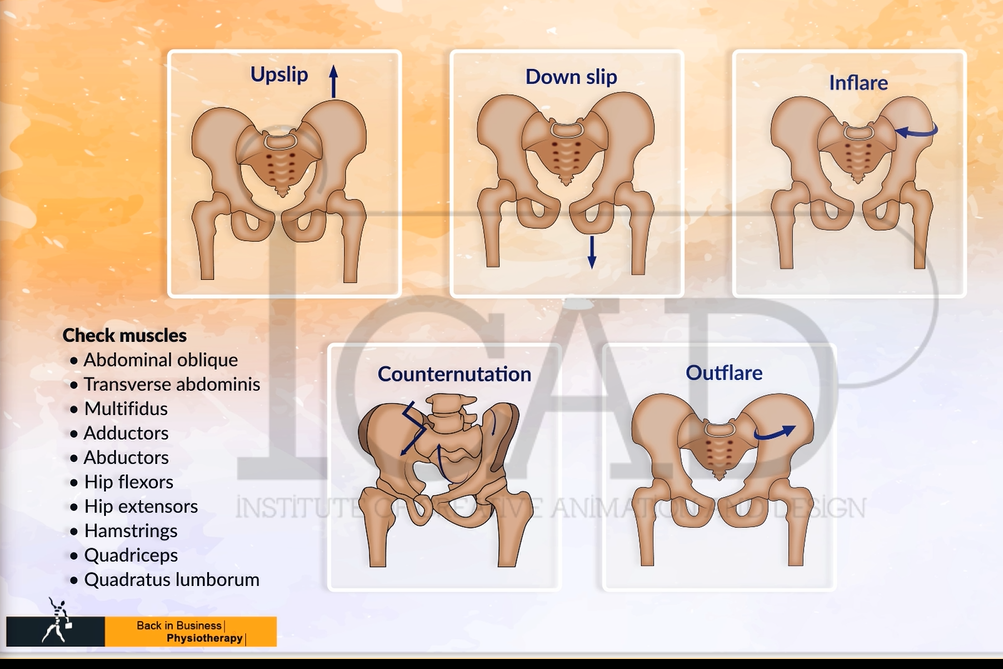 The pain can often refer down your legs into your thighs and also into your lower back.
The pain can often refer down your legs into your thighs and also into your lower back.
Pelvic Girdle Pain and You
This is when PGP can impact on your daily activities:
1. Single legged activities
2. Walking
3. Rolling over in bed
4. Walking up stairs
5. Getting in and out of the car
PGP can occur for a number of reasons:
1. Injury
2. High BMI
3. Weak pelvic floor muscles
4. Trauma
5. Arthritis
6. Rapid weight gain
Exercises to Help Pelvic Pain During Pregnancy
It is important that you continue to strengthen your pelvic floor throughout your pregnancy. This is why you receive a guided weekly pregnancy workout plan that includes pelvic floor exercises.
Tips to Relieve Pelvic Girdle Pain
1: Take smaller steps when you're walking
When you take smaller steps you will decrease the shearing forces through your pelvis which can help manage your pain by decreasing the stress at your pelvic joints.
2: Sleep with a pregnancy pillow between your legs.
When you do this, you can decrease the pressure through the front of your pelvis as well as avoiding twisting movements through the back of your pelvis.
3: Sit down whenever you need get dressed.
This will help to decrease the shearing forces at your pelvis during single leg standing.
4: Use correct sitting posture.
Try propping your feet up on a foot stool and make sure your bottom us right back in the chair.
5: Use correct standing posture.
I have numerous tips and videos on how to maintain correct posture. You can get these for free when you sign-up for a free trial of PregActive.com
6: You need to Avoid heavy lifting
Always bend with your hips and knees while keeping the natural curve in your back.
7: Avoid sitting on the floor with crossed legs.
If you do need to sit on the floor, then try to sit on a stool rather than cross legged.
Pelvic Pain after Walking During Pregnancy
Are you getting this pelvic pain after going for a walk? Then you may be suffering from symphysis pubis dysfunction. The pubic symphysis is located at the front of the pelvis where the two sides of the pelvis meet.
The pubic symphysis is located at the front of the pelvis where the two sides of the pelvis meet.
Changes in the hormones during pregnancy relax the ligaments and allow for increased movement, which can result in misalignment that can cause you pain. Please seek professional medical help.
Pelvic Pain at Night in Pregnancy
Why is my pelvic pain worse at night? When you sleep, there is the potential for your joints to be in a more vulnerable position. This can occur more often later in your pregnancy as your muscles have an even more important job in helping to stabilise your spine and your pelvis.
You may find your pelvic pain is worse at night due to the fact that your buttock muscles are less active at night-time as they are in a resting position. Also, depending on how you are sleeping, the joints may be in a more vulnerable position.
Pelvic Groin Pain in Pregnancy
If you are suffering from groin pain during pregnancy, you are not alone! Sometimes this pain becomes more intense as the pregnancy progresses. Ligament pain and vaginal issues are common causes of groin pain in pregnancy.
Ligament pain and vaginal issues are common causes of groin pain in pregnancy.
You should always chat to your doctor or midwife about any groin pain you may be experiencing.
Symphysis Pubis Dysfunction
The pubic symphysis is a joint that sits between the left and right pubic bones. During pregnancy, the ligaments and muscles that support the joint relax and stretch to accommodate the growing uterus and fetus. This relaxing and stretching causes the pubic symphysis to become unstable, resulting in symphysis pubis dysfunction (SPD).
Symptoms:
- sharp, shooting pains in the vagina, perineum, or rectum
- electric shock-like sensations in the vagina or groin area
- clicking in the hips or pelvis
- muscle spasms
- shooting pains in the pelvic area
- pain that radiates from one part of the pelvic area to another
You May Find Relief Using the Following Treatments:
- chiropractic massage
- acupuncture
- heat or ice to the pubic region
Why PregActive?
I will help you to get pregnancy fit, prepare for birth, prevent pregnancy aches and pains, including #pelvicgirdlepainrelief and provide you with convenient at-home workouts when pregnant.
As a mama, my Core Rehab program will help you recover after childbirth and re-gain your fitness and body confidence. I am confident PregActive will help you become a healthier, happier you.
Pain in the pelvic area - causes, examination and treatment | Symptoms
Menstrual cramps
Symptoms: Sharp or crampy pains that begin a few days before or during menstruation, are most intense within about 24 hours after the onset of menstruation and subside after 2 to 3 days, often accompanied by headache, nausea, constipation, diarrhea, or frequent urination. urination.
Endometriosis
Signs: Sharp or crampy pain that occurs before and during the first days of menstruation, often pain during intercourse and / or bowel movements. It can eventually lead to pain that is not related to the menstrual cycle.
Pain in the middle of the menstrual cycle
Signs: Severe, sharp pain that starts suddenly; can occur on either side, but only on one side each time, occurs at the same time during the menstrual cycle, usually in the middle of the cycle between periods (when the egg is released), most intense at the beginning, but then decreases over 1-2 days, there is often slight bleeding.
Pelvic inflammatory disease
Signs: Aching pain in the pelvic area, which can be felt on one or both sides. Usually a vaginal discharge that is sometimes foul-smelling and can become pus-like and yellow-green in color as the infection progresses. Sometimes pain during urination and/or intercourse, fever or chills, nausea or vomiting.
Rupture of an ovarian cyst
Signs: Pain that starts suddenly is initially limited to one area in the lower abdomen. Sometimes dizziness, fainting, slight vaginal bleeding, nausea, or vomiting occur.
Ectopic pregnancy
Signs: Persistent (not spasmodic) pain that starts suddenly, is initially limited to one area in the lower abdomen. Often slight vaginal bleeding, sometimes dizziness, fainting, fast heartbeat, or dangerously low blood pressure (shock) caused by severe internal bleeding.
Sudden degeneration fibromas in uterus
Symptoms: Sudden pain.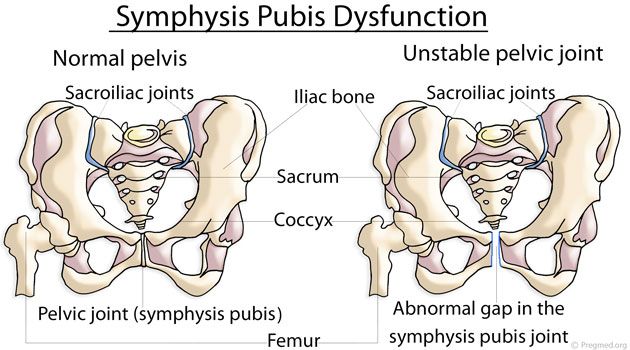 It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
Torsion (twisting) of the ovarian adnexa
Signs: Severe pain that starts suddenly, occurs on one side, grows rapidly. As well as intermittent pain that comes and goes (when the ovary twists and unwinds). Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries.
Ovarian cancer / Endometrial cancer
Signs: Gradually increasing pain. Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Spikes
Signs: Pain in the pelvic area, which gradually increases, often becomes chronic. As well as pain during intercourse. No vaginal bleeding or discharge. Sometimes nausea and vomiting (suggesting intestinal blockage).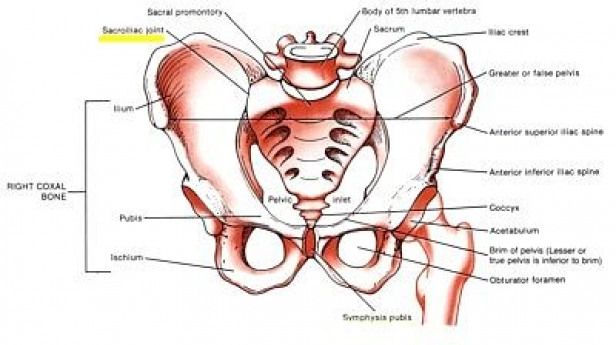 In women who have had abdominal surgery or in women with a pelvic infection.
In women who have had abdominal surgery or in women with a pelvic infection.
Miscarriage
Signs: Spasmodic pain in the pelvis or back, accompanied by vaginal bleeding. Other signs of early pregnancy such as breast tenderness, nausea, and missed periods.
Appendicitis
Signs: Pain that usually occurs in the lower right side of the abdomen. Loss of appetite and usually nausea and vomiting. Often fever.
Bladder infection
Signs: Pain just above the pubic bone. Sometimes an urgent need to urinate, more frequent urination, or burning when urinating.
Diverticulitis
Signs: Pain or tenderness in the left lower abdomen, fever.
Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)
Signs: Cramping pain in the abdomen, diarrhea, in ulcerative colitis often with blood in the stool, loss of appetite and weight loss.
Stones in the urinary tract
Signs: Excruciating intermittent pain in the lower abdomen, side or lower back, depending on the location of the stone, nausea and vomiting, blood in the urine.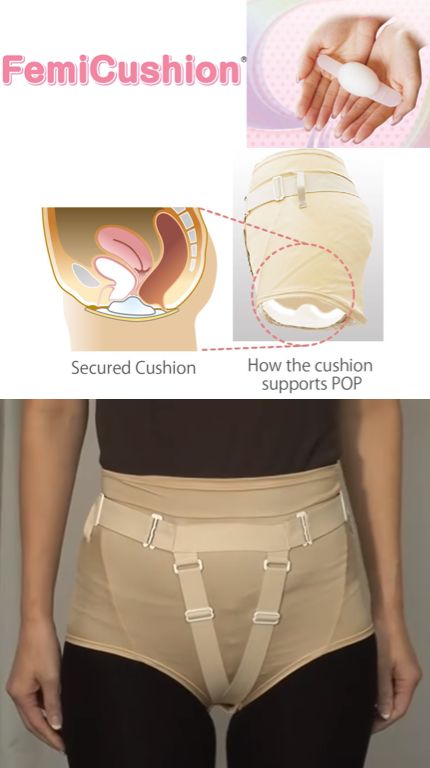
Gastrointestinal disorders (gastroenteritis, constipation, accumulation of pus; colon cancer)
Musculoskeletal disorders (pubic bone dehiscence after childbirth, fibromyalgia and abdominal muscle tension)
Psychological factors (stress and depression)
treatment, diagnosis, causes — 8(495)120-02-05
| Obstetrics and Gynecology | |
|---|---|
| Consultations of the Chief Physician | |
| Primary obstetrician-gynecologist consultation (excellent student of health care, Khersonskaya E.B.) | 8000.00 |
| Repeated consultation with an obstetrician-gynecologist (excellent worker in public health, Khersonskaya E.B.) | 7000.00 |
| Consultation of an obstetrician-gynecologist under the WB contract (excellent student of health care, Khersonskaya E.B.) 2022 | 6000.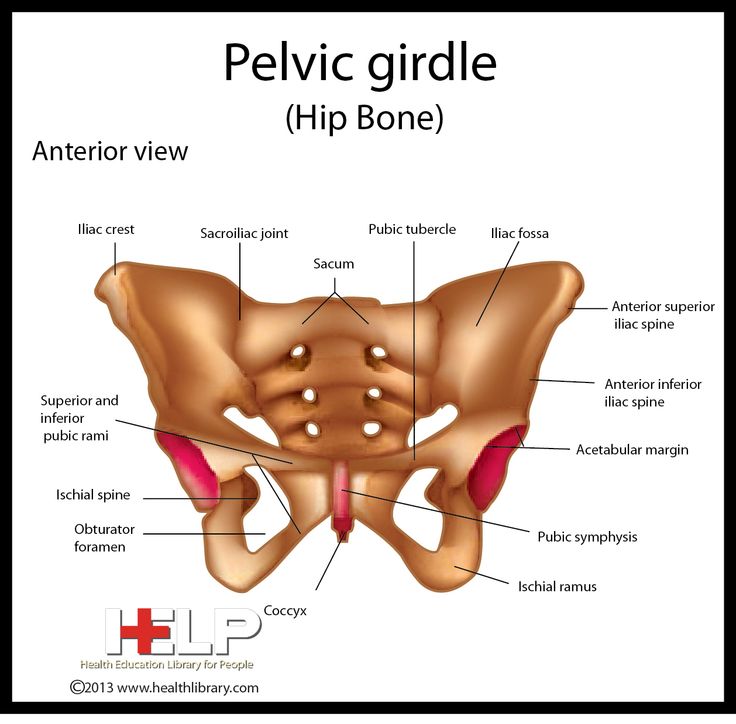 00 00 |
| Head physician remote consultation | 3000.00 |
| Chief physician's consultation on the correction of prescribed treatment | 4000.00 |
| Extended consultation of the head physician (more than 60 min.) | 9000.00 |
| CITO consultation (off-hours) | 10000.00 |
| Consulting | |
| Consultation of an obstetrician-gynecologist (Dr. Mezhlumova N.A.) | 3500.00 |
| Primary obstetrician-gynecologist consultation (Dr. Fotina E.V.) | 4500.00 |
| Obstetrician-gynecologist repeated consultation (Dr. Fotina E.V.) | 4000.00 |
| Consultation of an obstetrician-gynecologist under the WB contract (Fotina E.V.) 2022 | 3800.00 |
| Doctor's consultation on the correction of the prescribed treatment | 2000. 00 00 |
| Obstetrician-gynecologist remote consultation | 3000.00 |
| Remote consultation of a doctor to correct the prescribed treatment | 1500.00 |
| Primary consultation with a gynecologist-reproductologist | 5000.00 |
| Repeated consultation with a gynecologist-reproductologist | 4500.00 |
| Consultation with a gynecologist-reproductologist and ultrasound to assess the ovarian reserve | 6500.00 |
| Extended consultation with a gynecologist-reproductologist and ultrasound to assess the ovarian reserve | 7000.00 |
| Consultation of an obstetrician-gynecologist (Dr. Egorova A.A., Muravina E.L.) | 4000.00 |
| Consultation of an obstetrician-gynecologist (Dr. Kozlovskaya I.A.) | 4500.00 |
Consultation of an obstetrician-gynecologist (Honored Doctor of the Russian Federation Ivanova N. V., professor Panina O.B.) V., professor Panina O.B.) | 8000.00 |
| Council of obstetricians-gynecologists (Honored Doctor of the Russian Federation Ivanova N.V. together with the chief physician Khersonskaya E.B.) | 4000.00 |
| Council of Obstetricians-Gynecologists (Chief Physician E.B. Khersonskaya together with Honored Doctor of the Russian Federation N.V. Ivanova) | 4000.00 |
| Obstetric invasions | |
| Amniotest (test for amniotic fluid leakage) | 800.00 |
| Amnisure Rapid Test | 4000.00 |
| Pregnancy test | 1000.00 |
| Insertion of an unloading obstetric pessary (excluding the cost of the pessary) | 2500.00 |
| Removal of the unloading obstetric pessary (excluding the cost of the pessary) | 2500.00 |
| Gynecological procedures | |
| Gynecological smear collection (WB contract) | 500. 00 00 |
| Collection of gynecological smear 1 category | 800.00 |
| Collection of gynecological smear 2 category | 1900.00 |
| Procedure in a gynecological room, category 1 | 1500.00 |
| Procedure in the gynecological room 2 category | 2700.00 |
| Colposcopy (video colposcopy) | 3000.00 |
| Colposcopy (video colposcopy) extended | 4500.00 |
| Introduction of intrauterine contraceptives (excluding the cost of the spiral) | 2700.00 |
| Introduction of intrauterine contraceptives II degree of complexity (excluding the cost of the spiral) | 4500.00 |
| Removal of intrauterine devices (coils) | 1200.00 |
| Withdrawal of intrauterine contraceptives (spirals) II degree of difficulty | 1700. 00 00 |
| Placement/removal of a contraceptive ring (without cost of the ring) | 800.00 |
| Placement/removal of a contraceptive ring (without the cost of the ring) II degree of complexity | 1100.00 |
| Removal of a foreign body from the vagina | 1000.00 |
| Removal of a foreign body from the vagina II degree of complexity | 1500.00 |
| Radio wave removal of single (up to 3 units) genital warts or papillomas | 2000.00 |
| Radio wave removal of multiple (more than 3 units) genital warts or papillomas | 4000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) I degree of complexity | 7000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) II degree of complexity | 12000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) III degree of complexity | 19000. |
| Cryogenic removal of single warts or papillomas of the female genital organs (up to 5 units) (nitrogen price included) | 2000.00 |
| Cryogenic removal of multiple warts or papillomas of the female genital organs (up to 10 units) (nitrogen price included) | 3000.00 |
| Chemical removal of single warts or papillomas of the female genital organs (up to 5 units) | 1000.00 |
| Chemical removal of multiple warts or papillomas of the female genital organs (up to 10 units) | 2000.00 |
| Chemical destruction of cervical pathology (treatment of cervical diseases with Solkovagin) | 2500.00 |
| Opening of cervical cysts | 2000.00 |
| Opening of cervical cysts II degree of complexity | 3000.00 |
| Hysterosonography | 10000.00 |
| Hysterosonography II degree of complexity | 13000. |
| Uterine aspiration | 3200.00 |
| Aspiration of the contents of the uterus II degree of complexity | 4700.00 |
| Arabin obstetric pessary | 7500.00 |
| Endometrial aspiration biopsy (Pipel biopsy) | 3500.00 |
| Endometrial aspiration biopsy (Pipel biopsy) II degree of complexity | 4900.00 |
| Loop biopsy of the cervix (1 position) using the Surgitron apparatus | 2700.00 |
| Loop biopsy of the cervix (1 position) II degree of complexity using the apparatus Surgitron | 3300.00 |
| Cervical scraping | 2200.00 |
| Curettage of the cervical canal II degree of difficulty | 3200.00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device | 7000.00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device II degree of complexity | 10000.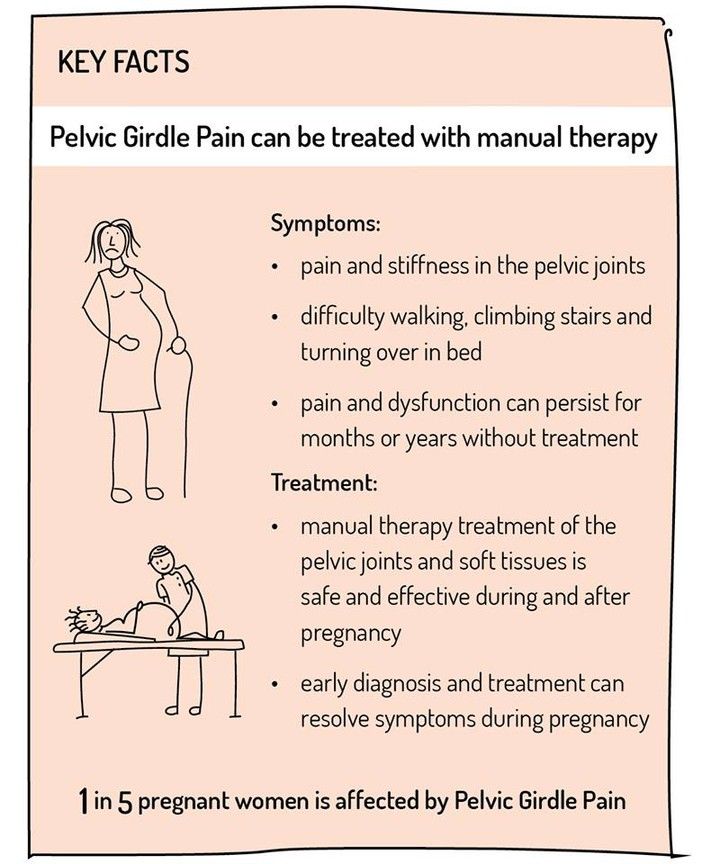 00 00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device III degree of complexity | 15000.00 |
| Hysteroscopy, separate diagnostic curettage | 16000.00 |
| Hysteroscopy, separate diagnostic curettage II degree of complexity | 19500.00 |
| Hysteroscopy, separate diagnostic curettage, IUD removal | 18000.00 |
| Hysteroscopy, separate diagnostic curettage, removal of the IUD II degree of complexity | 25500.00 |
| Hysteroscopy, separate diagnostic curettage, cervical loop biopsy | 18000.00 |
| Hysteroscopy, separate diagnostic curettage, loop biopsy of the cervix II degree of complexity | 27000.00 |
| Hysteroscopy, separate diagnostic curettage, polypectomy | 20000.00 |
| Hysteroscopy, separate diagnostic curettage, polypectomy II degree of complexity | 27500. 00 00 |
| Hysteroscopy, dissection of intrauterine synechiae | 25000.00 |
| Hysteroscopy, dissection of intrauterine synechia II degree of complexity | 37500.00 |
| Curettage of the cervical canal, removal of the polyp of the cervical canal | 10000.00 |
| Curettage of the cervical canal, removal of the polyp of the cervical canal II degree of complexity | 15000.00 |
| Instrumental IUD removal | 6000.00 |
| Instrumental removal of the IUD II degree of complexity | 9000.00 |
| Cervical conization | 22000.00 |
| Conization of the cervix II degree of complexity | 25000.00 |
| Operations on the Bartholin's gland (Marsupialization, removal of the Bartholin's gland) | 15000.00 |
| Operations on Bartholin's gland (marsupialization, removal of Bartholin's gland) II degree of complexity | 22500. 00 00 |
| Removal of stitches from the cervix | 3000.00 |
| Removal of stitches from the cervix II degree of complexity | 4500.00 |
| Removal of braces after caesarean section I category of complexity | 2500.00 |
| Removal of staples after caesarean section II category of complexity | 3500.00 |
| Removal of sutures of I category of complexity | 3000.00 |
| Removal of sutures II category of complexity | 4500.00 |
| Cervicoscopy II degree of complexity | 12000.00 |
| Cervicoscopy+cervical curettage | 18000.00 |
| Cervicoscopy + curettage of the cervical canal II degree of complexity | 15000.00 |
| Polypectomy II degree of complexity | 9000.00 |
| Vaginal mass removal | 15000.00 |
| Removal of neoplasm of labia minora | 15000. 00 00 |
| Removal of a neoplasm of the labia minora II category of complexity | 25000.00 |
| Contouring with hyaluronic acid fillers 3 ml | 40000.00 |
| Sling installation (without cost of the sling) | 55000 |
| Colporrhaphy, perineolevathoroplasty II level | |
| Colporrhaphy, perineolevathoroplasty level I | 70000 |
| Colporrhaphy II level | 70000 |
| Colporrhaphy level I | 50000 |
| Hysteroresectoscopy + dissection of the uterine septum (Honored Doctor of Russia kmn Ivanova N.V.) | 60000 |
| Hysteroresectoscopy + incision in/uterine septum II level | 55000 |
| Hysteroresectoscopy + incision in/uterine septum I level | 45000 |
Hysteroresectoscopy + myomresection (Honored Doctor of Russia kmn Ivanova N. |