Testings done during pregnancy
Common Tests During Pregnancy | Johns Hopkins Medicine
-
Genetic Screening
-
First Trimester
-
Second Trimester
-
Ultrasound
-
Amniocentesis
-
Chorionic Villus Sampling
-
Fetal Monitoring
-
Glucose
-
Group B Strep Culture
Your health care provider may recommend a variety of screenings, tests and imaging techniques during your pregnancy. These tests are designed to provide information about the health of your baby and may help you optimize your child’s prenatal care and development.
Genetic Screening
Many genetic abnormalities can be diagnosed before birth. Your doctor or midwife may recommend genetic testing during pregnancy if you or your partner has a family history of genetic disorders. You may also choose to have genetic screening if you have had a fetus or baby with a genetic abnormality.
Examples of genetic disorders that can be diagnosed before birth include:
-
Cystic fibrosis
-
Duchenne muscular dystrophy
-
Hemophilia A
-
Polycystic kidney disease
-
Sickle cell disease
-
Tay-Sachs disease
-
Thalassemia
The following screening methods are available during pregnancy:
-
Alpha-fetoprotein (AFP) test or multiple marker test
-
Amniocentesis
-
Chorionic villus sampling
-
Cell-free fetal DNA testing
-
Percutaneous umbilical blood sampling (withdrawing a small sample of the fetal blood from the umbilical cord)
-
Ultrasound scan
First Trimester Prenatal Screening Tests
First trimester screening is a combination of fetal ultrasound and maternal blood testing. This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
First trimester screening includes:
-
Ultrasound for fetal nuchal translucency. Nuchal translucency screening uses an ultrasound to examine the area at the back of the fetal neck for increased fluid or thickening.
-
Ultrasound for fetal nasal bone determination. The nasal bone may not be visualized in some babies with certain chromosome abnormalities, such as Down syndrome. This screen is performed using an ultrasound between 11 and 13 weeks gestation.
-
Maternal serum (blood) tests. These blood tests measure two substances found in the blood of all pregnant women:
-
Pregnancy-associated plasma protein A. A protein produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.

-
Human chorionic gonadotropin. A hormone produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
When used together as first trimester screening tests, nuchal translucency screening and maternal blood tests have a greater ability to determine if the fetus might have a birth defect, such as Down syndrome (trisomy 21) and trisomy 18.
If the results of these first trimester screening tests are abnormal, genetic counseling is recommended. Additional testing, such as chorionic villus sampling, amniocentesis, cell-free fetal DNA or other ultrasounds, may be needed for an accurate diagnosis.
Second Trimester Prenatal Screening Tests
Second trimester prenatal screening may include several blood tests called multiple markers. These markers provide information about your potential risk of having a baby with certain genetic conditions or birth defects.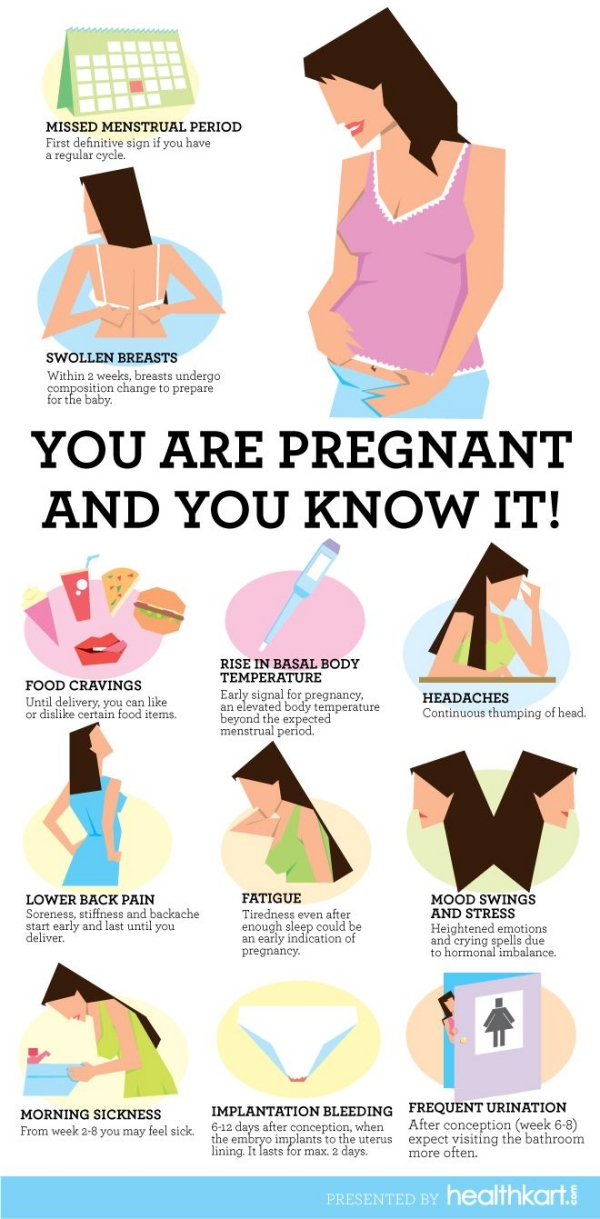 Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
-
AFP screening. Also called maternal serum AFP, this blood test measures the level of AFP in your blood during pregnancy. AFP is a protein normally produced by the fetal liver that is present in the fluid surrounding the fetus (amniotic fluid). It crosses the placenta and enters your blood. Abnormal levels of AFP may indicate:
-
A miscalculated due date, as the levels vary throughout pregnancy
-
Defects in the abdominal wall of the fetus
-
Down syndrome or other chromosomal abnormalities
-
Open neural tube defects, such as spina bifida
-
Twins (more than one fetus is producing the protein)
-
-
Estriol.
 This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health.
This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health. -
Inhibin. This is a hormone produced by the placenta.
-
Human chorionic gonadotropin. This is also a hormone produced by the placenta.
Abnormal test results of AFP and other markers may mean that additional testing is needed. An ultrasound is used to confirm the milestones of your pregnancy and to check the fetal spine and other body parts for defects. An amniocentesis may be needed for an accurate diagnosis.
Since multiple marker screening is not diagnostic, it is not 100 percent accurate. It helps determine who in the population should be offered additional testing during pregnancy. False-positive results may indicate a problem when the fetus is actually healthy. On the other hand, false-negative results indicate a normal result when the fetus actually does have a health problem.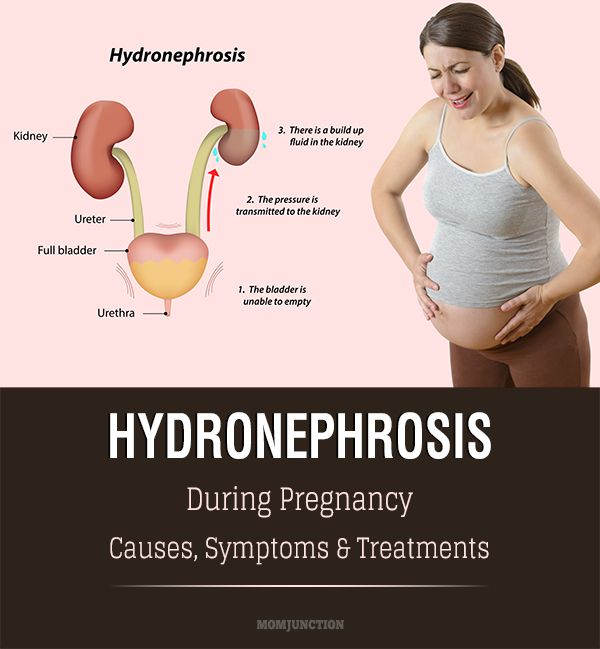
When you have both first and second trimester screening tests performed, the ability of the tests to detect an abnormality is greater than using just one screening independently. Most cases of Down syndrome can be detected when both first and second trimester screenings are used.
Ultrasound
An ultrasound scan is a diagnostic technique that uses high-frequency sound waves to create an image of the internal organs. A screening ultrasound is sometimes done during the course of your pregnancy to check normal fetal growth and verify the due date.
When are ultrasounds performed during pregnancy?
Ultrasounds may be done at various times throughout pregnancy for several reasons:
First Trimester
-
To establish the due date (this is the most accurate way of determining the due date)
-
To determine the number of fetuses and identify placental structures
-
To diagnose an ectopic pregnancy or miscarriage
-
To examine the uterus and other pelvic anatomy
-
To detect fetal abnormalities (in some cases)
Midtrimester (also called the 18- to 20-week scan)
-
To confirm the due date (a due date set in the first trimester is rarely changed)
-
To determine the number of fetuses and examine the placental structures
-
To assist in prenatal tests, such as an amniocentesis
-
To examine the fetal anatomy for abnormalities
-
To check the amount of amniotic fluid
-
To examine blood flow patterns
-
To observe fetal behavior and activity
-
To measure the length of the cervix
-
To monitor fetal growth
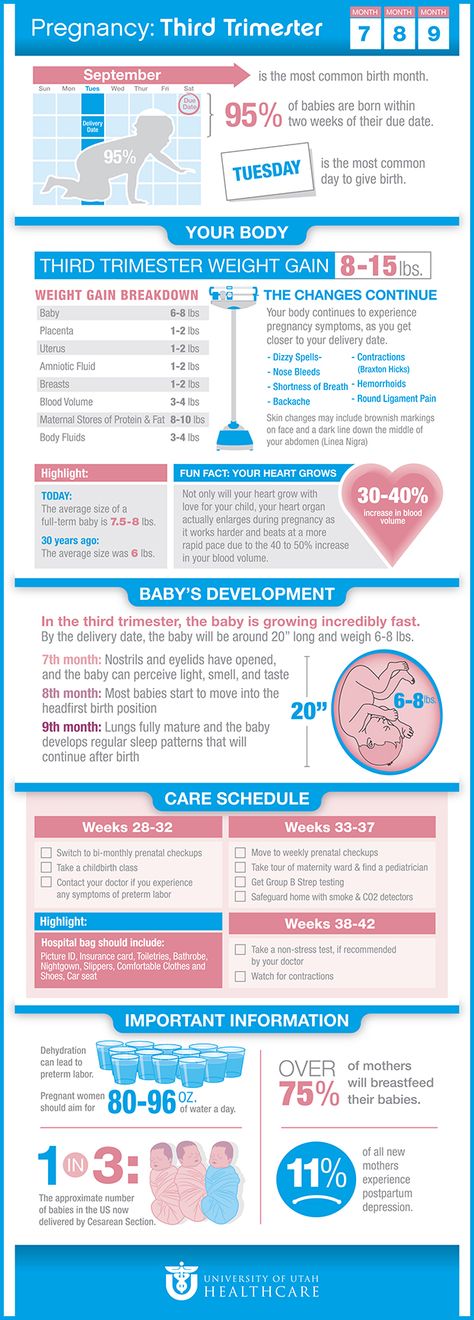
Third Trimester
-
To monitor fetal growth
-
To check the amount of amniotic fluid
-
To conduct the biophysical profile test
-
To determine the position of the fetus
-
To assess the placenta
How is an ultrasound scan performed?
Two types of ultrasounds can be performed during pregnancy:
-
Abdominal ultrasound.
 In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image.
In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image. -
Transvaginal ultrasound. In a transvaginal ultrasound, a smaller ultrasound transducer is inserted into your vagina and rests against the back of the vagina to create an image. A transvaginal ultrasound produces a sharper image than an abdominal ultrasound and is often used in early pregnancy.
Which ultrasound imaging techniques are available?
There are several types of ultrasound imaging techniques. As the most common type, the 2-D ultrasound provides a flat picture of one aspect of the baby.
If more information is needed, a 3-D ultrasound exam can be done. This technique, which provides a 3-D picture, requires a special machine and special training. The 3-D image allows the health care provider to see the width, height and depth of the images, which can be helpful during the diagnosis. The 3-D images can also be captured and saved for later review.
The 3-D images can also be captured and saved for later review.
The latest technology is 4-D ultrasound, which allows the health care provider to visualize the unborn baby moving in real time. With 4-D imaging, a three-dimensional image is continuously updated, providing a “live action” view. These images often have a golden color, which helps show shadows and highlights.
Ultrasound images may be captured in still photographs or on video to document findings.
What are the risks and benefits of ultrasound imaging?
Fetal ultrasound has no known risks other than mild discomfort due to pressure from the transducer on your abdomen or in your vagina. No radiation is used during the procedure.
Transvaginal ultrasound requires covering the ultrasound transducer in a plastic or latex sheath, which may cause a reaction in women with a latex allergy.
Ultrasound imaging is constantly being improved and refined. As with any test, the results may not be completely accurate.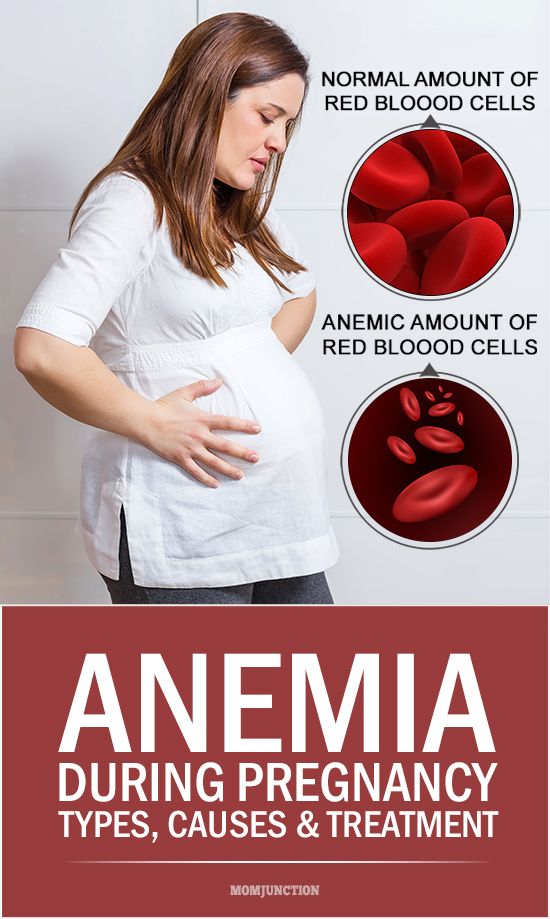 However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
Fetal ultrasound is sometimes offered in nonmedical settings to provide keepsake images or videos for parents. While the ultrasound procedure itself is considered safe, it is possible that untrained personnel may miss an abnormality or give parents false assurances about their baby’s well-being. It is best to have an ultrasound performed by trained medical personnel who can correctly interpret the results. Talk with your doctor or midwife if you have questions.
Amniocentesis
An amniocentesis involves taking a small sample of the amniotic fluid that surrounds the fetus. It is used to diagnose chromosomal disorders and open neural tube defects, such as spina bifida. Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Who is an ideal candidate for amniocentesis?
An amniocentesis is generally offered to women between the 15th and 20th week of pregnancy who have an increased risk of chromosomal abnormalities. Candidates include women who will be over age 35 at the time of delivery or those who have had an abnormal maternal serum screening test.
How is an amniocentesis performed?
An amniocentesis involves inserting a long, thin needle through your abdomen into the amniotic sac to withdraw a small sample of amniotic fluid. The amniotic fluid contains cells shed by the fetus, which contain genetic information. Although specific details of each procedure may vary, a typical amniocentesis follows this process:
-
Your abdomen will be cleansed with an antiseptic.
-
Your doctor may or may not give a local anesthetic to numb the skin.

-
Your doctor will use ultrasound technology to help guide a hollow needle into the amniotic sac. He or she will withdraw a small sample of fluid for lab analysis.
You may feel some cramping during or after the amniocentesis. Strenuous activities should be avoided for 24 hours following the procedure.
Women who are pregnant with twins or other higher-order multiples need sampling from each amniotic sac to study each baby. Depending on the position of the baby and placenta, amount of fluid, and woman’s anatomy, sometimes the amniocentesis cannot be done. The fluid is then sent to a genetics lab so that the cells can grow and be analyzed. AFP is also measured to rule out an open neural tube defect. Results are usually available in about 10 days to two weeks, depending on the lab.
Chorionic Villus Sampling (CVS)?
CVS is a prenatal test that involves taking a sample of some of the placental tissue. This tissue contains the same genetic material as the fetus and can be tested for chromosomal abnormalities and some other genetic problems. Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
How is CVS performed?
CVS may be offered to women with an increased risk of chromosomal abnormalities or who have a family history of a genetic defect that is testable from the placental tissue. CVS is usually performed between the 10th and 13th week of pregnancy. Although exact methods may vary, the procedure involves the following steps:
-
Your doctor will insert a small tube (catheter) through your vagina and into your cervix.
-
Using ultrasound technology, your doctor will guide the catheter into place near the placenta.
-
Your doctor will remove some tissue using a syringe on the other end of the catheter.

Your doctor may also choose to perform a transabdominal CVS, which involves inserting a needle through your abdomen and into your uterus to sample the placental cells. You may feel some cramping during and after either type of CVS procedure. The tissue samples are sent to a genetic lab for growth and analysis. Results are usually available in about 10 days to two weeks, depending on the lab.
What if CVS is not possible?
Women with twins or other higher-order multiples usually need sampling from each placenta. However, because of the complexity of the procedure and the positioning of the placentas, CVS is not always feasible or successful with multiples.
Women who are not candidates for CVS or who did not get accurate results from the procedure may require a follow-up amniocentesis. An active vaginal infection, such as herpes or gonorrhea, will prohibit the procedure. In other cases, the doctor may take a sample that does not have enough tissue to grow in the lab, generating incomplete or inconclusive results.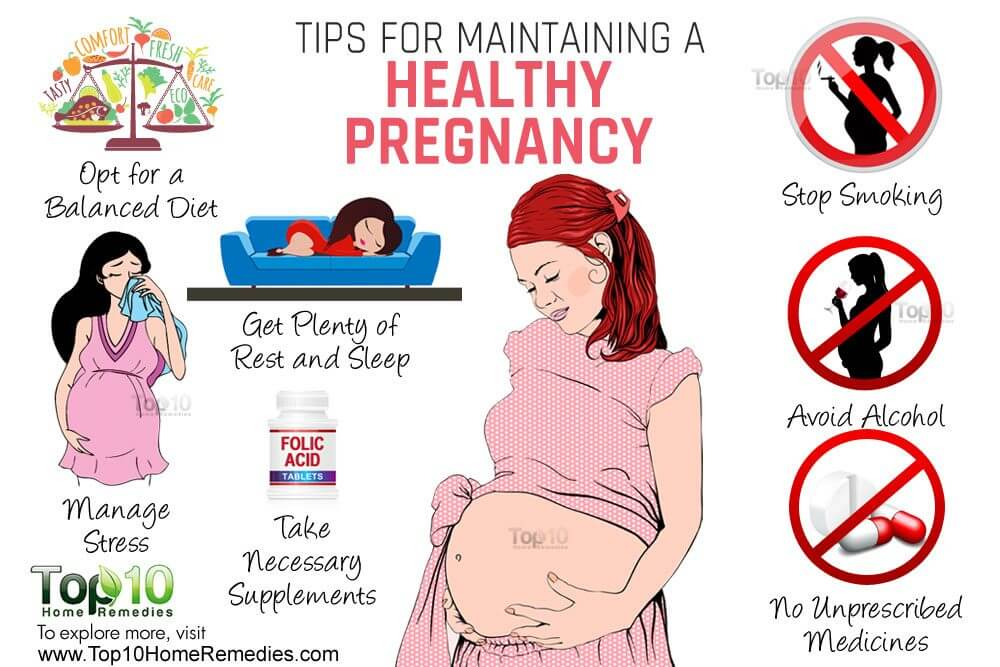
Fetal Monitoring
During late pregnancy and labor, your doctor may want to monitor the fetal heart rate and other functions. Fetal heart rate monitoring is a method of checking the rate and rhythm of the fetal heartbeat. The average fetal heart rate is between 120 and 160 beats per minute. This rate may change as the fetus responds to conditions in the uterus. An abnormal fetal heart rate or pattern may mean that the fetus is not getting enough oxygen or indicate other problems. An abnormal pattern also may mean that an emergency cesarean delivery is needed.
How is fetal monitoring performed?
Using a fetoscope (a type of stethoscope) to listen to the fetal heartbeat is the most basic type of fetal heart rate monitoring. Another type of monitoring is performed with a hand-held Doppler device. This is often used during prenatal visits to count the fetal heart rate. During labor, continuous electronic fetal monitoring is often used. Although the specific details of each procedure may vary, standard electronic fetal monitoring follows this process:
-
Gel is applied to your abdomen to act as a medium for the ultrasound transducer.

-
The ultrasound transducer is attached to your abdomen with straps so it can transmit the fetal heartbeat to a recorder. The fetal heart rate is displayed on a screen and printed onto special paper.
-
During contractions, an external tocodynamometer (a monitoring device that is placed over the top of the uterus with a belt) can record the pattern of contractions.
When is internal fetal monitoring needed?
On occasion, internal fetal monitoring is needed to provide a more accurate reading of the fetal heart rate. Your bag of waters (amniotic fluid) must be broken and your cervix must be partially dilated to use internal monitoring. Internal fetal monitoring involves inserting an electrode through the dilated cervix and attaching the electrode to the scalp of the fetus.
Glucose Testing
Glucose testing is used to measure the level of sugar in your blood.
A glucose challenge test is usually conducted between 24 and 28 weeks of pregnancy.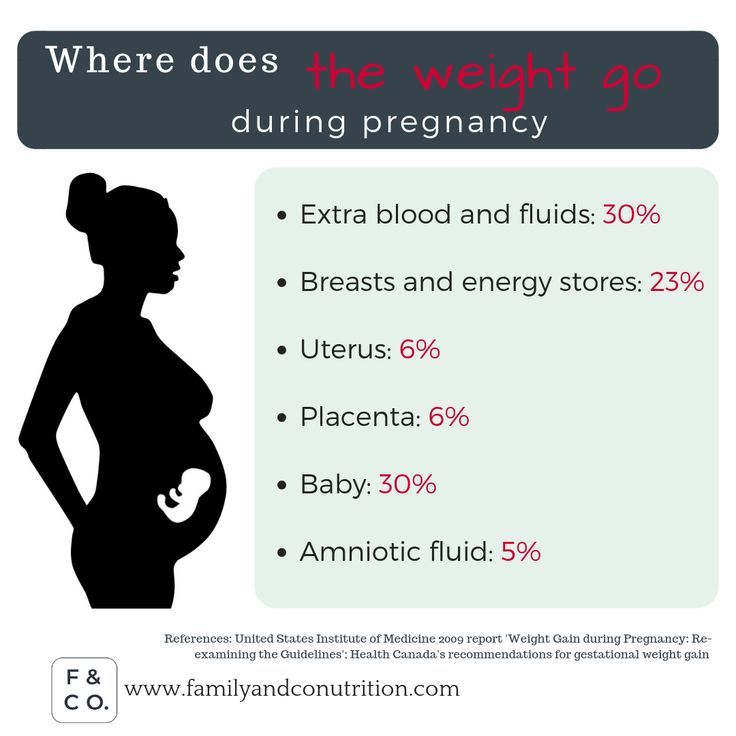 Abnormal glucose levels may indicate gestational diabetes.
Abnormal glucose levels may indicate gestational diabetes.
What is involved in a glucose challenge test?
The initial one-hour test is a glucose challenge test. If the results are abnormal, a glucose tolerance test is needed.
How is a glucose tolerance test performed?
You may be asked to only drink water on the day the glucose tolerance test is given. Although the specific details of each procedure may vary, a typical glucose tolerance test includes the following steps:
-
An initial fasting sample of blood will be drawn from your vein.
-
You will be given a special glucose solution to drink.
-
Blood will be drawn at various times over the course of several hours to measure the glucose levels in your body.
Group B Strep Culture
Group B streptococcus (GBS) is a type of bacteria found in the lower genital tract of about 20 percent of all women. While a GBS infection does not usually cause problems in women before pregnancy, it can cause serious illness in mothers during pregnancy. GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies contract the infection during pregnancy or from the mother’s genital tract during labor and delivery.
The Centers for Disease Control and Prevention recommends screening all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks gestation. The treatment of mothers with certain risk factors or positive cultures is important to reduce the risk of transmission of GBS to the baby. Babies whose mothers receive antibiotic treatment for a positive GBS test are 20 times less likely to develop the disease than those without treatment.
Routine Tests During Pregnancy | ACOG
Acquired Immunodeficiency Syndrome (AIDS): A group of signs and symptoms, usually of severe infections, in a person who has human immunodeficiency virus (HIV).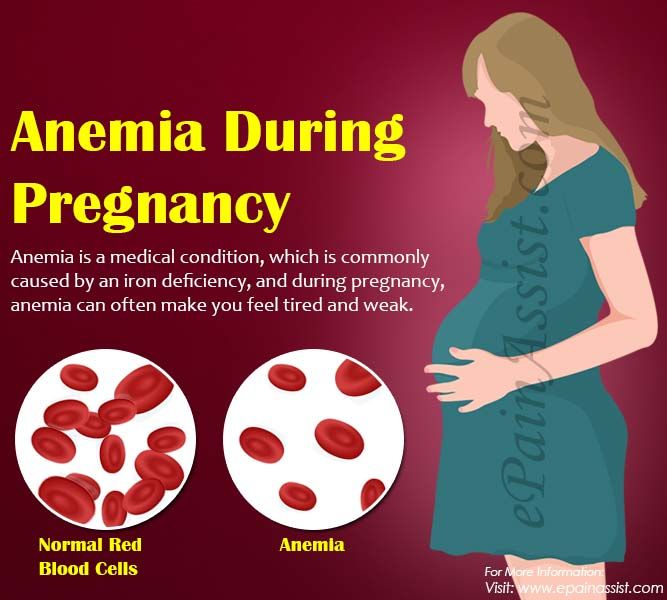
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Antibiotics: Drugs that treat certain types of infections.
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Bacteria: One-celled organisms that can cause infections in the human body.
Birth Defects: Physical problems that are present at birth.
Cells: The smallest units of structures in the body.
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Chlamydia: A sexually transmitted infection caused by bacteria. This infection can lead to pelvic inflammatory disease and infertility.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.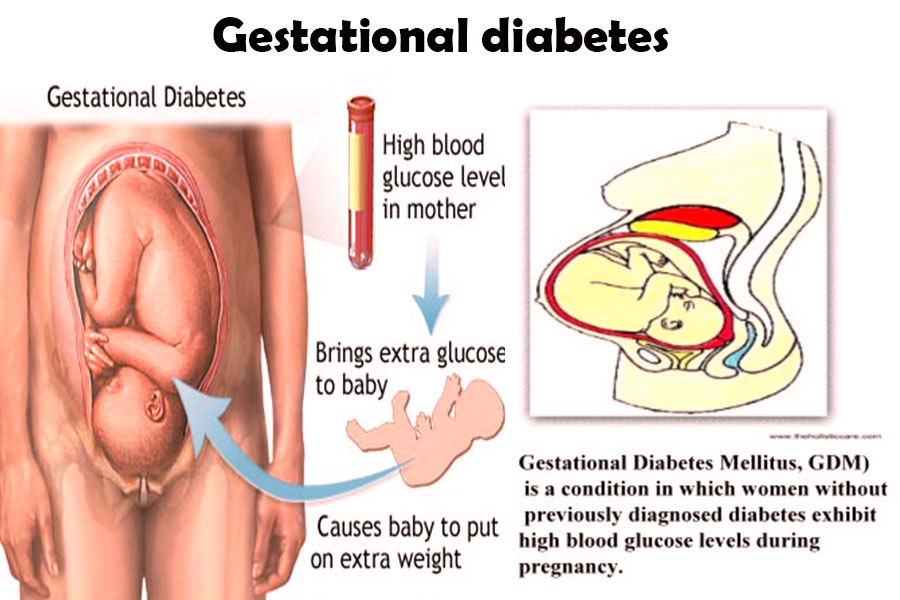
Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gene: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Gestational Diabetes: Diabetes that arises during pregnancy.
Glucose: A sugar in the blood that is the body’s main source of fuel.
Gonorrhea: A sexually transmitted infection that can lead to pelvic inflammatory disease, infertility, and arthritis.
Group B Streptococcus (GBS): A type of bacteria that many people carry normally and can be passed to the fetus at the time of delivery. GBS can cause serious infection in some newborns. Antibiotics are given during labor to women who carry the bacteria to prevent newborn infection.
Hepatitis B: An infection caused by a virus that can be spread through blood, semen, or other body fluid infected with the virus.
Hepatitis C: An infection caused by a virus that can be spread through infected blood.
Human Immunodeficiency Virus (HIV): A virus that attacks certain cells of the body’s immune system. If left untreated, HIV can cause acquired immunodeficiency syndrome (AIDS).
Immune: Protected against infectious disease.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.
Measles–Mumps–Rubella (MMR) Vaccine: A shot given to protect against measles, mumps, and rubella. The shot contains live viruses that have been changed to not cause disease. The shot is not recommended for pregnant women.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Rectum: The last part of the digestive tract.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rubella: A virus that can be passed to the fetus if a woman becomes infected during pregnancy. The virus can cause miscarriage or severe birth defects.
Sexually Transmitted Infections (STIs): Infections that are spread by sexual contact. Infections include chlamydia, gonorrhea, human papillomavirus (HPV), herpes, syphilis, and human immunodeficiency virus (HIV, the cause of acquired immunodeficiency syndrome [AIDS]).
Syphilis: A sexually transmitted infection (STI) that is caused by an organism called Treponema pallidum. This infection may cause major health problems or death in its later stages.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Tuberculosis (TB): A disease that affects the lungs and other organs in the body. TB is caused by bacteria.
Urinary Tract Infection (UTI): An infection in any part of the urinary system, including the kidneys, bladder, or urethra.
Vaccine: A substance that helps the body fight disease. Vaccines are made from very small amounts of weak or dead agents that cause disease (bacteria, toxins, and viruses).
Vagina: A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
which women and men need to submit during planning and after the onset of pregnancy
Months of pregnancy are like a small life. During this time, much changes in the body of the woman herself, and a new person is formed from the embryo in her uterus. To preserve the health of the mother and the unborn child, it is important to observe all the changes that occur. Moreover, a woman needs not only to look closely and listen to her condition and share her impressions with a doctor, but also to take certain tests and undergo examinations. Modern technologies make it possible to identify the slightest nuances in the development of the fetus and changes in the health of the expectant mother, which means that possible problems can be prevented in time.
Modern technologies make it possible to identify the slightest nuances in the development of the fetus and changes in the health of the expectant mother, which means that possible problems can be prevented in time.
At each stage of pregnancy, you need to undergo certain examinations. When and what to check, what tests to pass - there is a certain system in this respect that allows you to keep the health status of both the pregnant woman and the fetus under control. Everything is planned by months, so you can prepare in advance, avoiding unnecessary confusion and unrest.
Together with the doctors, we will tell you what tests the expectant mother will have to undergo at the stage of pregnancy planning and in each of her trimesters.
Pregnancy test schedule
After being registered in the first 10 days, a pregnant woman will have to undergo examinations and consultations with various doctors: a therapist, dentist, otolaryngologist, ophthalmologist, and other specialists according to indications. And also you need to pass the first tests. Over time, their list will change.
Below is a calendar of tests for pregnant women. This list can be supplemented by your doctor, taking into account the indications and comorbidities.
| The term of pregnancy | Analyzes |
| to 13 weeks | • MAZ from the cervix on the flora and oncocytology • Clinical (general) blood test • Blood blood test aus and Rh factor • Coagulogram • Blood test for HIV, syphilis, hepatitis B and C • Blood test for TORCH infection • Biochemical blood test • TSH blood test • Blood sugar test |
| 11-14 weeks | • Blood test for hCG • Blood test for PAPP-A |
| 16-18 weeks | hCG and PAPP-A tests at 11-14 weeks) |
| 15-26 weeks | CBC and urinalysis |
| Up to 28 weeks | Mother’s blood test for Rh antibodies negative Rh, and the father is positive (1 time per month) |
| 27-40 weeks | • Clinical blood test • Biochemical blood test • Coagulogram • Blood test for TORCH infection • Urinalysis • Blood test for HIV, syphilis, hepatitis B and C • Gynecological smear for flora |
| 24-28 weeks | Glucose tolerance test (PGTT) |
family planning is necessary at least three months before the intended conception, and preferably six months.
 Both the woman and the man will have to pass several tests, undergo examinations, and, if necessary, a course of treatment or vaccination.
Both the woman and the man will have to pass several tests, undergo examinations, and, if necessary, a course of treatment or vaccination. What tests should be done when planning a pregnancy for a woman
An expectant mother needs to visit a gynecologist, as well as donate blood and urine to check a number of indicators. Here is a list of tests that a woman needs to take when planning a pregnancy.
- Flora smear.
- Cytological examination of the cervical canal and cervix.
- Complete blood count.
- Biochemical blood test.
- Urinalysis.
- Blood test for Rh factor and determination of blood group.
- Blood glucose test.
- Test for thyroid hormones.
- Analysis for the detection of TORCH infections (toxoplasmosis, cytomegalovirus, rubella, herpes).
Tests for a man
Some people think that men do not need to see a doctor if a couple is about to conceive. But it is not. The future father also needs to pass a series of tests, below is a list.
The future father also needs to pass a series of tests, below is a list.
- Test for sexually transmitted infections.
- Complete blood count.
- Biochemical blood test.
- Urinalysis.
- Blood test for Rh factor and determination of blood group.
Tests for both parents
In some cases, both partners are also tested for hormones and genetic analysis.
Not all couples need the first one. The grounds for the appointment of such an analysis may be:
- irregular cycle,
- no pregnancy within one year of sexual life without contraception up to 35 years,
- no pregnancy within 6 months of regular intercourse without contraception after 35 years,
- unsuccessful pregnancies in history.
Genetic analysis is recommended if there are risk factors: hereditary diseases in the family, infertility, adverse factors that may affect the development of pregnancy (taking certain medications, harmful working conditions, etc. ).
).
What tests should be taken during pregnancy in the 1st, 2nd, 3rd trimester
Each period has its own list of examinations.
- 1 trimester
During the first trimester (up to 12 weeks of pregnancy) the organs and systems of the fetus are formed. This is the most important period for a child's development. And it is at this time that the expectant mother needs to pass the largest number of tests.
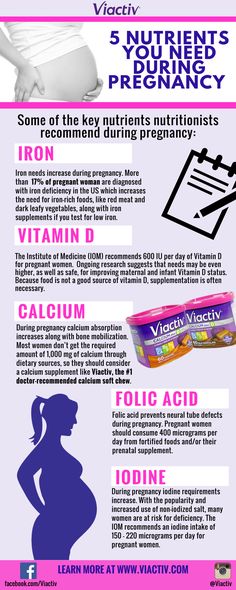
Blood tests : general, biochemical (protein, albumin, urea, creatinine, total cholesterol, total bilirubin, glucose, iron, AST, ALT), clotting (coagulogram), per group and Rh factor; for sexually transmitted infections and TORCH infections; on hCG and PAPP-A.
Urinalysis : general, bacterial culture.
Investigations : vaginal flora smear; testing for sexually transmitted infections.
- 2nd trimester
From the second trimester, a urine test becomes mandatory - it must be taken before each visit to the doctor.
At 18-20 weeks (if the pregnancy proceeds normally), a general blood test is taken, at 24-28 weeks - a glucose tolerance test.
- 3 trimester
Complete and biochemical blood test, coagulogram, blood sugar test, HIV, hepatitis and syphilis, TORCH infection - all this must be taken at 30 weeks of gestation. And on the 34th-36th - and a smear for the pathological microflora of the vagina.
Let's see what the results of the tests that women take during pregnancy can tell us.
Complete blood count
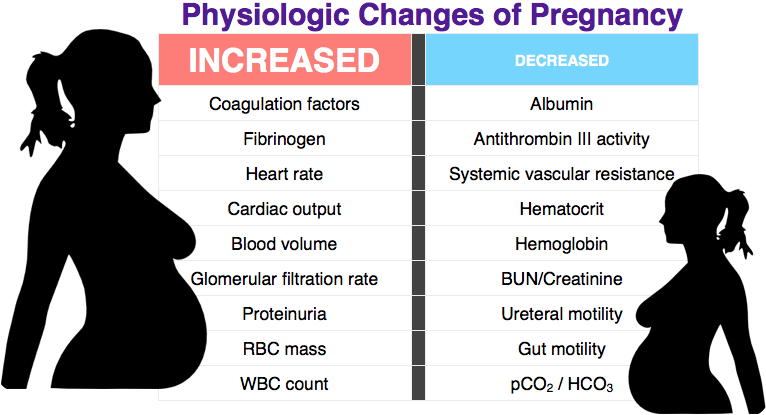
Photo: roberto carrafa, pexels.comComplete blood count involves the study, including the number of the main blood components - erythrocytes, leukocytes, platelets. It allows you to identify anemia, hypoxia, inflammation, allergic reactions, etc. (1). Consider some indicators of a general blood test.
Norms of values
- Erythrocytes. The number of red blood cells begins to increase at the 9-10th week of pregnancy, and closer to childbirth, it can be 20-30% higher than the normal level for non-pregnant women.
 During the period of bearing a child, the number of red blood cells may decrease to a certain extent, which is also considered the norm. The main thing is that their concentration does not decrease to such an extent that there is a threat of oxygen starvation.
During the period of bearing a child, the number of red blood cells may decrease to a certain extent, which is also considered the norm. The main thing is that their concentration does not decrease to such an extent that there is a threat of oxygen starvation.
The norm of erythrocytes for pregnant women is from 3.2 to 5.6 x 10 12 / l.
- Leukocytes.
A change in the number of white blood cells during pregnancy may be a signal of a decrease in immunity or the presence of an infection in the body.
During pregnancy, an increase in leukocytes up to 9000-15000 x 10 9 /l is acceptable.
- Platelets.
During pregnancy, the platelet count decreases slightly. For a healthy person, the norm is 180-420 x 10 9 platelets per liter. In pregnant women, in the 1st trimester, this indicator can be 170-340 x 10 9 /l, and in later terms even lower - 140-320 * 10 9 /l.
It is important to keep this under control, because a high number of platelets creates the risk of thickening of the blood and the formation of blood clots, and a low one - the risk of bleeding, which will be difficult to stop.
- Hemoglobin.
Blood protein, on which the delivery of oxygen to all cells of the body of mother and child depends. With a lack of oxygen, fetal hypoxia may develop.
Normally, in the first trimester, the hemoglobin index in a pregnant woman should be in the range of 110-140 g/l, in the second - 110-148 g/l, in the third trimester - 110-150 g/l.
Biochemical blood test
A study that gives an idea of the general health of a pregnant woman and the functioning of individual organs. About 20 different indicators are studied, each has its own norms.
Norms of values
| Total protein | 63-83 g/l |
| Albumin | 32-50 g/l in the 1st trimester, 28-55.  7 g/l in the 2nd, 7 g/l in the 2nd, 25.6-66 g/l in the 3rd m |
| Urea | 2.5-7.1 mmol/l |
| Cholesterol | 6,16-13.7 mmol/l |
| 28-112 28-112 Ф | |
| Glucose (sugar) | 3.5-5.83 mmol/l |
| Creatinine0032 32-47 μmmol/l-in 3-m | |
| ALT | not more than 32 units/l |
| not more than 31 units/l | |
| GGT | not more L |
| Total bilirubin | 3.4-21.6 µmol/L |
| Iron | 8.93-30.4 µmol/L in the 1st and 2nd trimesters, µmol/l - in the 3rd |
Urinalysis
Photo: Martin Lopez, pexels.com Urinalysis also helps to monitor the health of the pregnant woman. And this is especially true of the kidneys, which during this period work with a double load, and the entire urinary system. We will tell you what indicators are being studied and what norms for pregnant women are determined.
Standards
- Density.
Normally it should be 1010-1030 g/l. An increase in density may indicate insufficient fluid intake, and may be a signal for the onset of the development of diabetes.
- Colour, transparency.
As a rule, the urine of a healthy woman is clear, straw-yellow.
- Acidity.
Normal pH 5-8. With kidney failure, diabetes, acidity may decrease.
- Unwanted agents
Normally, there should be no protein in the urine of a pregnant woman, only a small amount is allowed - no more than 0.033 g / l. Higher numbers may indicate the onset of gestosis (a pathological condition of pregnant women, which is accompanied by edema, high blood pressure)
Also there should not be glucose, bilirubin in the urine (its presence indicates jaundice or viral hepatitis) and ketone bodies (a sign of early toxicosis, anemia or diabetes).
Erythrocytes in the urine of the expectant mother are normally absent or present in single copies. There should be no more than 5 leukocytes in the field of view. The number of squamous epithelium is allowed no more than 3 (with its increase, cystitis, urethritis, and even kidney stones can be suspected).
There should be no more than 5 leukocytes in the field of view. The number of squamous epithelium is allowed no more than 3 (with its increase, cystitis, urethritis, and even kidney stones can be suspected).
A normal urinalysis should be free of bacteria and fungi, uric acid crystals, phosphates, cholesterol, fatty acids.
HCG test
Human chorionic gonadotropin (hCG) is a hormone, by the presence and quantity of which it is possible to determine pregnancy in the early stages, as well as to identify some of its pathologies and features with high accuracy.
An elevated hCG level may indicate multiple pregnancy, early toxicosis, fetal chromosomal abnormalities, etc. A low hCG level is possible with fetal developmental delays, ectopic or non-developing pregnancy and other pathologies (2).
Normal values
During pregnancy, the level of hCG is constantly changing:
- 2nd week - from 25 to 300 mU / ml,
- 3rd week - 1500 to 3000 mU/ml;
- 4th week - 10,000-30,000 mU / ml;
- 5th week - up to 100,000 mU / ml;
- 6-11 weeks - up to 225,000 mU / ml;
- 16th week - from 10,000 to 58,000 mU / ml;
- by the 20th week - from 1600 to 49,000 mU / ml.
Glucose test
Glucose tolerance test is performed for the timely detection of abnormal increase in the blood sugar level of a pregnant woman, which can provoke impaired glucose tolerance. And this can provoke the appearance of pregnancy complications, the development of type II diabetes in a woman.
Standard values
The test is carried out in three stages. Normally, its indicators should be as follows:
1st stage (on an empty stomach) - up to 5.1 mmol / l,
2nd stage (1 hour after exercise) - up to 10.0 mmol / l,
Stage 3 (2 hours after exercise) - up to 8.5 mmol / l.
Genetic tests
Pregnancy-associated plasma protein A (PAPP-A) testing is required to detect various genetic pathologies at the earliest stages of their formation. If the indicator is below normal, this may be a sign of the development of Down's or Edwards' disease.
Norms of values
Permissible values of this analysis differ at different periods:
- 9-10 weeks - 0.
 32-2.42 mU / ml,
32-2.42 mU / ml, - 10-11th - 0.46-3.73 mU / ml,
- 11-12th - 0.79-4.76 mU / ml,
- 12-13 weeks - 1.03-6.01 mU / ml.
Culture assays
Bacterial culture is a test that can detect the growth of pathogenic microbes and determine their sensitivity to antibiotics.
- Bacterial culture of urine during pregnancy helps to identify urinary infections that are still “dormant” and activated during this period, but are asymptomatic.
- Culture of flora from the cervical canal of the uterus (scraping is done for this) helps to detect fungi and bacteria, inflammatory processes. In particular, to identify streptococcus, which can provoke labor fever.
Standards
Pathogenic pathogens are measured in CFU/ml - this is, in fact, one microbe cell from which a colony of microorganisms grows.
Less than 1000 cfu/ml is considered normal in urine.
In the cervical canal of the uterus, they must be less than 100 CFU / ml.
Ultrasound during pregnancy
Photo: MART PRODUCTION, pexels.comUltrasound is an informative and safe examination method. Ultrasound research methods are used to diagnose pregnancy and its timing, possible complications. Also, the doctor can assess the condition of the uterus and pelvic organs, placenta and membranes, fetal development. Ultrasound will show early pregnancy and the sex of the unborn child, will help to identify malformations of the child and problems with the health of the woman in time.
According to the order of the Ministry of Health of the Russian Federation No. 572n dated November 1, 2012, planned ultrasound is performed in pregnant women three times (3). Additionally, ultrasound may be prescribed according to indications.
Ultrasound of the 1st trimester of pregnancy
The examination is carried out from the 11th to the 14th week. During this period, ultrasound helps to clarify the gestational age and age of the fetus, calculate the time of its birth.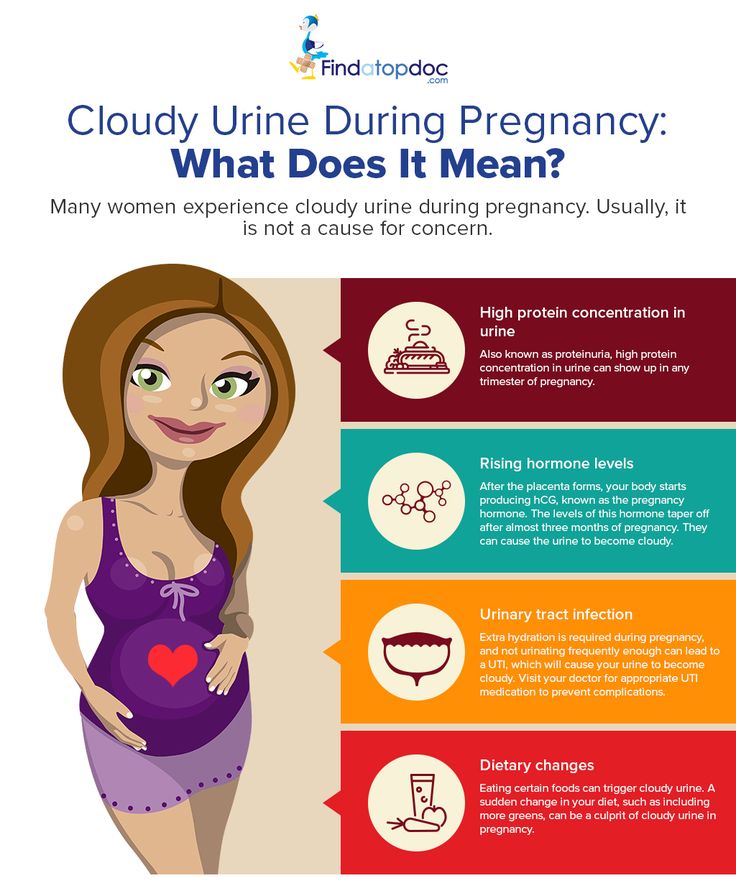 In addition, the doctor will see the number of fetal eggs, assess the condition of the uterus, the heartbeat and activity of the fetus, and may detect some pathologies in its development.
In addition, the doctor will see the number of fetal eggs, assess the condition of the uterus, the heartbeat and activity of the fetus, and may detect some pathologies in its development.
2nd trimester ultrasound
Performed from 18 to 21 weeks. At this time, you can already determine the sex of the child. But that's not the point. The doctor determines the position and presentation of the fetus, its size and weight, the condition of the internal organs. Indicators are measured with the help of which congenital defects and chromosomal abnormalities can be excluded. The structure and development of the placenta, which already occupies a significant place in the uterus, the condition of the umbilical cord, and the tone of the walls of the uterus are assessed.
3rd trimester ultrasound
Performed at 30-34 weeks. The condition of the fetus, its development in accordance with the term, position, length of the umbilical cord and the location of the placenta are assessed.
During this period, it is possible to detect congenital malformations that appear late (for example, aneurysm of the vein of Galen).
Also, the doctor can determine the approximate weight and height of the baby will be born, in what condition his mother's appendages and uterus.
Based on the results of this ultrasound, the doctor decides whether the woman will be able to give birth on her own or whether she needs to have a caesarean section.
Pregnancy screenings
There are mandatory screenings for all (ultrasound, biochemical), and studies can be ordered according to indications. For example, cytogenetic screening is to determine the individual risk of chromosomal pathology in the fetus, molecular screening is to detect mutations that occur with a frequency of no more than 1%, so it is rarely prescribed.
A blood test for hormones is usually performed at the request of the expectant mother, or on the urgent recommendation of a doctor.
The doctor usually insists on a complete screening:
- if the mother-to-be is over 35 and the father is over 40;
- in the presence of a missed pregnancy, miscarriage or premature birth in the past;
- in the presence of genetic pathologies in family members;
- if the pregnant woman had an infectious disease in the first trimester;
- if the pregnant woman must take medicines that are potentially harmful to the fetus;
- if a woman works in hazardous industries or cannot get rid of bad habits.
If we talk about screening as a complex of examinations, then there are usually three of them during pregnancy.
First screening
First screening between 11 and 13 weeks. It includes ultrasound, analysis of hCG hormones and PAPP-A.
Second screening
Performed at 18-20 weeks. This complex includes an ultrasound and a blood test for hormones (if the woman did not do it in the first trimester). At the same time, screening for preeclampsia, a complication of pregnancy after the 20th week, which is manifested by an increase in blood pressure, can be carried out. It includes measuring blood pressure and determining the amount of protein in the urine.
At the same time, screening for preeclampsia, a complication of pregnancy after the 20th week, which is manifested by an increase in blood pressure, can be carried out. It includes measuring blood pressure and determining the amount of protein in the urine.
Third screening
This is from the 30th to the 34th week. The third screening is different in that ultrasound with dopplerography can be prescribed to study the functioning of the vessels and cardiotocography (CTG) - the study of the fetal cardiac activity. It is prescribed at the risk of oxygen starvation of the fetus. Screening for preeclampsia is also repeated.
As of 2021, the third screening is no longer mandatory. But a pregnant woman can undergo it at will and in accordance with the recommendations of a doctor.
Reviews of gynecologists about tests during pregnancy
— It is advisable to visit a gynecologist on the eve of pregnancy in order to prevent negative scenarios of this difficult and exciting period in a woman's life. During pregnancy itself, a woman should take a responsible approach to her condition and the development of the baby, since the body of the expectant mother undergoes changes that must be closely monitored by specialists. Therefore, it is important to take tests on time, in accordance with the calendar. Their omission can negatively affect both the child and the woman herself, - comments Alsu Gilyazova, obstetrician-gynecologist of the branch of the Israeli clinic "Hadassah" in Skolkovo . - The most important tests are done when registering a pregnant woman. A wide range of studies are being conducted to assess the condition of the mother and fetus. Most tests must be taken at least twice - in the first period of pregnancy and before childbirth. If there are chronic diseases, or complications appear, then both the list of tests and their frequency increase significantly. The range of laboratory tests concerns mainly blood and urine tests, as well as the diagnosis of infections and the determination of hormonal levels.
During pregnancy itself, a woman should take a responsible approach to her condition and the development of the baby, since the body of the expectant mother undergoes changes that must be closely monitored by specialists. Therefore, it is important to take tests on time, in accordance with the calendar. Their omission can negatively affect both the child and the woman herself, - comments Alsu Gilyazova, obstetrician-gynecologist of the branch of the Israeli clinic "Hadassah" in Skolkovo . - The most important tests are done when registering a pregnant woman. A wide range of studies are being conducted to assess the condition of the mother and fetus. Most tests must be taken at least twice - in the first period of pregnancy and before childbirth. If there are chronic diseases, or complications appear, then both the list of tests and their frequency increase significantly. The range of laboratory tests concerns mainly blood and urine tests, as well as the diagnosis of infections and the determination of hormonal levels.
— Observation and examinations during pregnancy are necessary, first of all, for early diagnosis, prevention and timely treatment of abnormalities that may occur during pregnancy, — explains Maria Filatova, obstetrician-gynecologist, gynecologist-endocrinologist at the Chaika clinic . - Due to the increased need of the body for iron, anemia often develops in pregnant women. If it is not corrected, this can lead to oxygen starvation of the organisms of the expectant mother and baby. A woman becomes more vulnerable to infectious diseases, the normal development of a healthy child may be disturbed. In the 1st, 2nd and 3rd trimesters, it is imperative to take a complete blood count to diagnose anemia and take drugs to treat it.
Another important test is glucose tolerance. If the mother's body cannot adequately utilize glucose, then the baby's pancreas takes over this function. This means that insulin will be actively produced in his body. And this, among other things, is an anabolic hormone, due to which the fetus becomes very large, which increases the risk of birth trauma for the mother and child. Therefore, it is important to detect diabetes in the mother in time and begin its correction. The glucose solution required for a glucose tolerance test may not taste very good. You can add the juice of half a lemon to it - it has almost no sugar, but its taste can make the dough solution more pleasant.
Therefore, it is important to detect diabetes in the mother in time and begin its correction. The glucose solution required for a glucose tolerance test may not taste very good. You can add the juice of half a lemon to it - it has almost no sugar, but its taste can make the dough solution more pleasant.
It is very important to pass urine regularly - its general analysis helps to identify at an early stage the impairment of kidney function that can occur with preeclampsia. The first thing to look at is the protein level. It is important to collect exactly the average portion of the first morning urine after washing, so that vaginal discharge does not get there, which can significantly affect the result.
Popular questions and answers
In this block you will find even more information.
How often should I be tested during pregnancy?
There is a pregnancy test schedule that most doctors follow (4). For example, blood during pregnancy must be donated at least 4-5 times. Urine is given before each visit to the doctor.
Urine is given before each visit to the doctor.
Additional tests are prescribed strictly on an individual basis, if there are grounds and indications. For example, if a woman has Rh-negative blood, and a man has Rh-positive blood, then it is necessary to donate antibodies to the Rh factor of the fetus once a month throughout the pregnancy.
How do you know if the pregnancy is going well?
If the woman is well and there are no abnormalities in her tests. There may be slight pulling sensations in the lower abdomen and on the sides, which are due to the growth of the uterus, stretching of the ligaments of the uterus. A slight discomfort in the lumbar region after 20 weeks can also be a variant of the norm and is due to a change in the center of gravity and posture of the woman.
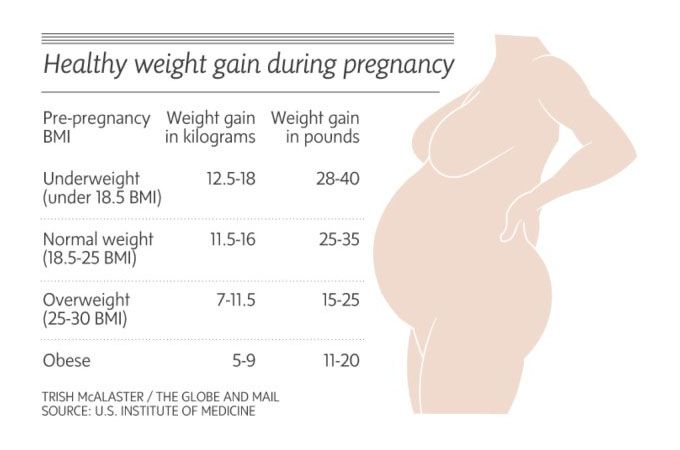
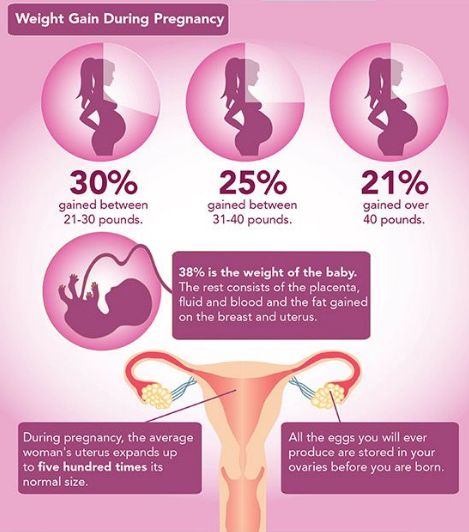
Fetal development is monitored by ultrasound according to trimesters. Fetal movement (for some, they begin as early as the 10th week, but most often closer to the 20th) is also a sign of a normal pregnancy. As well as changing taste preferences. Weight gain is completely normal, but it is desirable that it does not exceed 16-20 kg.
As well as changing taste preferences. Weight gain is completely normal, but it is desirable that it does not exceed 16-20 kg.
How do you know if you have problems during pregnancy?
Most often, a woman herself understands that something is going wrong. If, according to the hCG tests, she had a positive trend, but all the signs suddenly disappear at once - for example, the sensitivity of the nipples disappears, she stops sipping her stomach - this may indicate a threat of an unfavorable pregnancy outcome. In order to diagnose the problem in time, it is necessary to do blood tests and ultrasound.
Bloody discharge, turning into bleeding - a clear sign of abnormal development of pregnancy. They may indicate a high risk for mother and baby. If you find such discharge, you should immediately consult a doctor. As in the case if you suspect the discharge of amniotic fluid, you feel cramping pains that increase in strength and duration if convulsions and / or dizziness appear with flashing flies in the eyes, pain in the right hypochondrium, itching of the palms and soles of the feet.
During pregnancy, women can experience a wide range of symptoms and it is important to tell your doctor about any changes you notice, even if they seem minor.
Sources
- Pregnancy and blood diseases. N. Izada, G. Leizerovich.
URL: https://www.medicum.nnov.ru/doctor/library/obstetrics/Nisvander/6.php - Chorionic gonadotropin as a marker of trophoblastic disease. E. V. Tsyrlina, T. E. Poroshina // Practical Oncology. 2008.
URL: https://practical-oncology.ru/articles/264.pdf - Order of the Ministry of Health of the Russian Federation of November 1, 2012 N 572n "On approval of the Procedure for the provision of medical care in the profile" obstetrics and gynecology (with the exception of the use of assisted reproductive technologies) ".
URL: https://minzdrav.gov.ru/documents/9154-prikaz- - Calendar of analyzes and examinations during physiological pregnancy.
URL: https://www.infomed39.ru/for-citizens/situations/child/calendar-surveys/
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measuring height, body weight, determining body mass index), measuring the size of the pelvis, examining the cervix in the mirrors, bimanual vaginal study | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid diseases) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. 5. Dry processing of seams (if any). |
 General (clinical) blood test.
General (clinical) blood test. 
 General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 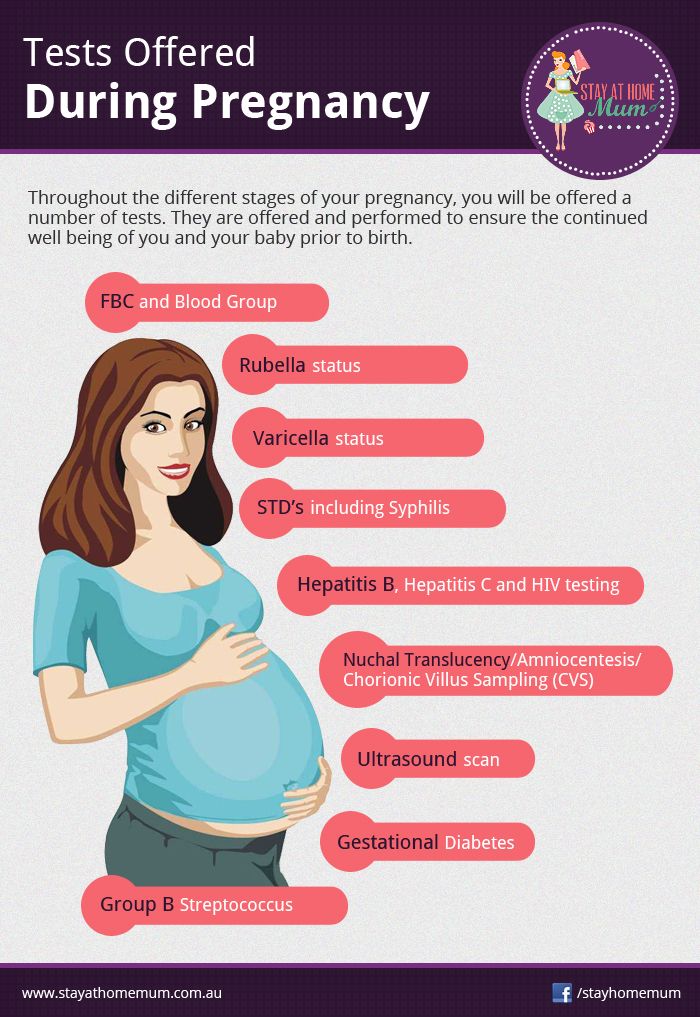 Inspections and consultations:
Inspections and consultations: