Testing for trisomy 21
Trisomy 21 (Down Syndrome): Diagnosis & Expectations
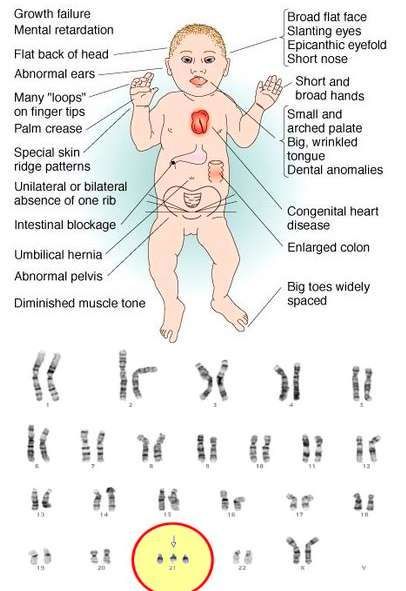
Trisomy 21, more commonly known as Down syndrome, is a genetic disorder causing developmental and intellectual delays. This disorder affects approximately 1 in every 700 babies.
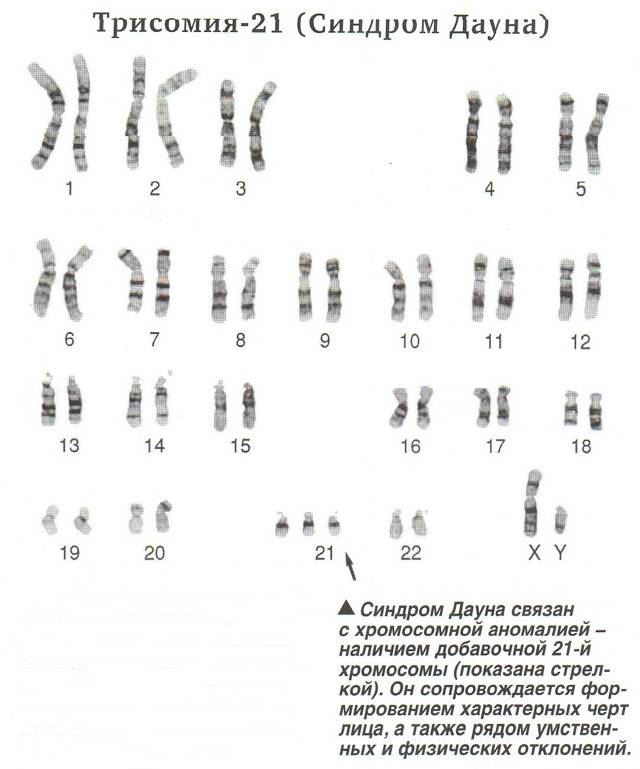
Normally, a person has 23 pairs of chromosomes. Chromosomes are the packages of genetic information, made of DNA, that contain the instructions the body uses to build a person. Chromosomes come in 23 pairs, with most people having 46 total chromosomes. Trisomy 21 is caused when a person has three copies of chromosome #21 instead of the usual two, for a total of 47 chromosomes.
This extra chromosome affects a baby’s development, resulting in a number of medical issues which may include: a distinct facial appearance, intellectual disability, developmental delays and thyroid/heart disease.
How is Trisomy 21 Diagnosed?
Trisomy 21 can be identified prenatally through screening tests such as non-invasive prenatal testing (NIPT) and ultrasound examinations. The diagnosis can be confirmed prenatally with better than 99% accuracy through chorionic villus sampling (CVS) or amniocentesis. Both of these advanced diagnostics tests are available at the Cardinal Glennon St. Louis Fetal Care Institute. The diagnosis can also be confirmed shortly after birth through blood testing.
Mothers over the age of 35 or with a family history of Down syndrome have a greater risk of having a baby with trisomy 21 and may want to talk with a doctor about genetic counseling and additional screenings.
What Can I Expect When I Visit the SSM Health Cardinal Glennon St. Louis Fetal Care Institute?
At the SSM Health Cardinal Glennon St. Louis Fetal Care Institute, our team has the experience and technology to prenatally diagnosis Trisomy 21, as well as assist families in preparing for delivery and beyond.
Using a multidisciplinary approach, our team will evaluate your baby to determine its specific needs. Ultrasounds will be used to monitor your baby’s growth and development, and a fetal echocardiogram may be used to check for a heart defect, which is more common in babies with Trisomy 21.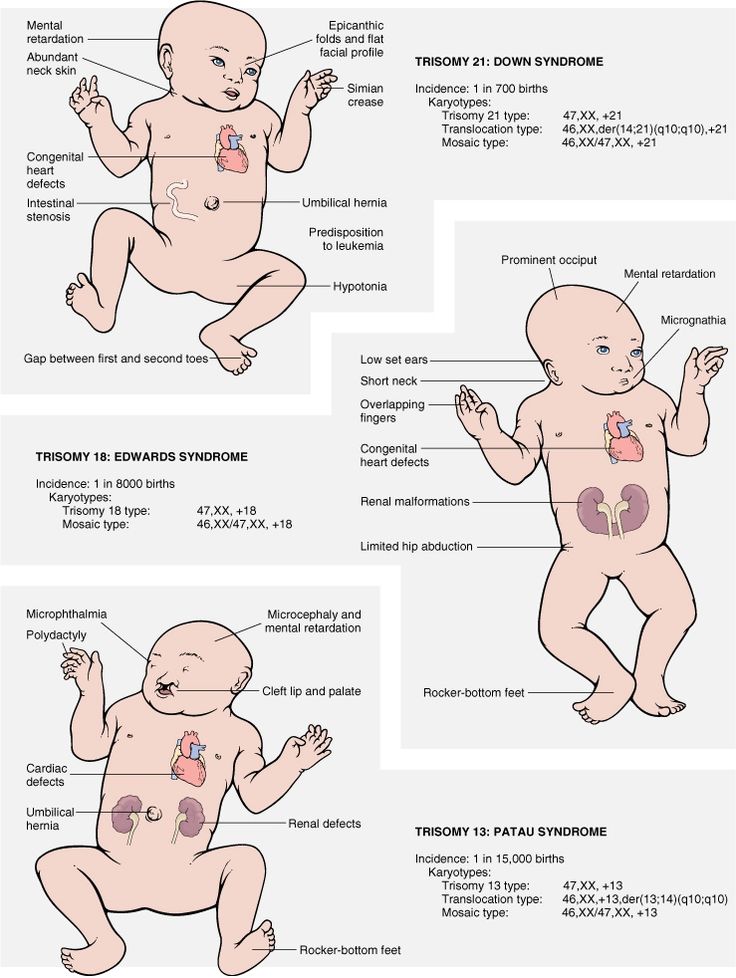 You will also work with our social worker to learn about the resources available for families of individuals with Down syndrome.
You will also work with our social worker to learn about the resources available for families of individuals with Down syndrome.
The risk of miscarriage and stillbirth increases in babies with Trisomy 21, but those who are carried to full term can usually be delivered vaginally without incident unless there are other reasons to consider an alternate mode of delivery.
How is Trisomy 21 Treated?
Down syndrome cannot be cured, but early intervention and treatment tailored to each child’s specific situation are helpful in managing this condition. Although babies born with Trisomy 21 will require some amount of care throughout their lifetimes, they can grow up to lead healthy, happy, productive lives.
What Can I Expect After My Baby is Born with Trisomy 21?
Typically, patients at the Cardinal Glennon St. Louis Fetal Care Institute will schedule a visit with a pediatric geneticist at SSM Health Cardinal Glennon Children's Hospital within the first few weeks of life and then follow up at the Down Syndrome Clinic where they will be able to see multiple specialists in one location.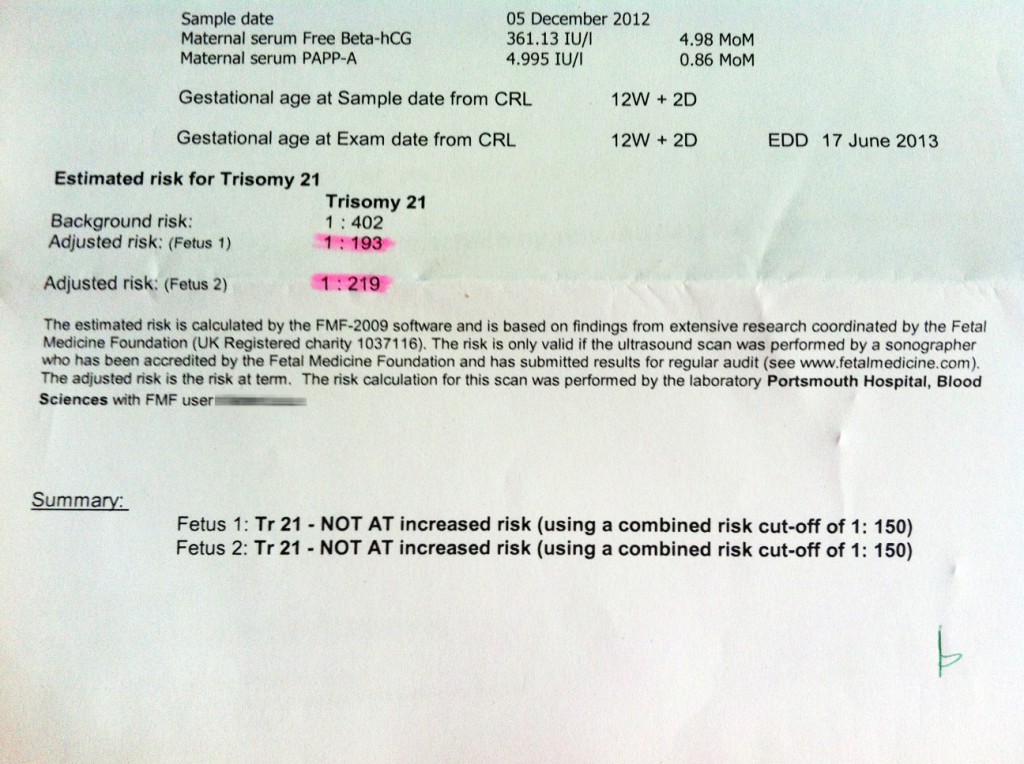
The specialists a particular individual with Down syndrome will see depends on their specific health issues, which can include heart defects, frequent respiratory infections, poor muscle tone, seizures, sleep problems and/or hearing, eye and dental problems. Parents will need to make sure their child has routine medical checkups and be on the lookout for early signs of these issues.
Families are encouraged to work with the Down Syndrome Association of Greater St. Louis or to seek out support from similar organizations where they live. Families who are seen at the Cardinal Glennon St. Louis Fetal Care Institute whose babies are suspected to have Down syndrome will be given resources from appropriate organizations.
We understand that you have a lot of questions if your child has been diagnosed with Trisomy 21. That’s why we’re available to help 24 hours a day, 7 days a week. For more information or to schedule an appointment, call us at 314-268-4037 or toll free at 877-SSM-FETL (877-776-3385).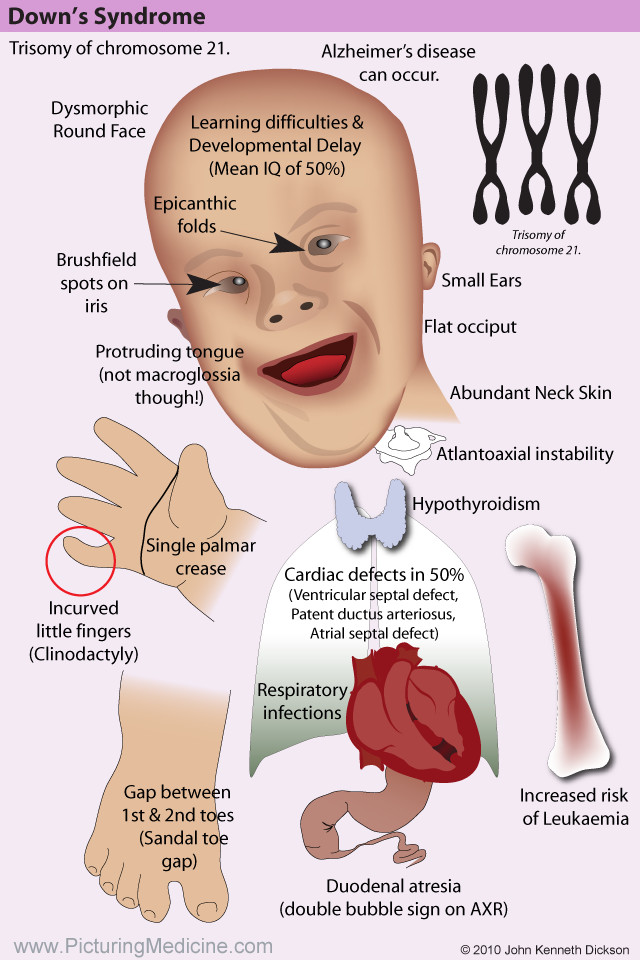
Patient Stories About Down Syndrome
At the St. Louis Fetal Care Institute, we understand the fear and confusion that come with the diagnosis of a prenatal medical condition. We share these patient stories to offer comfort, hope, and inspiration from other parents who have been where you are. Know that you are not alone - our team is here to support you every step of the way.
Read Our Related Blog PostsPrenatal Testing for Down Syndrome | Patient Education
Screening tests
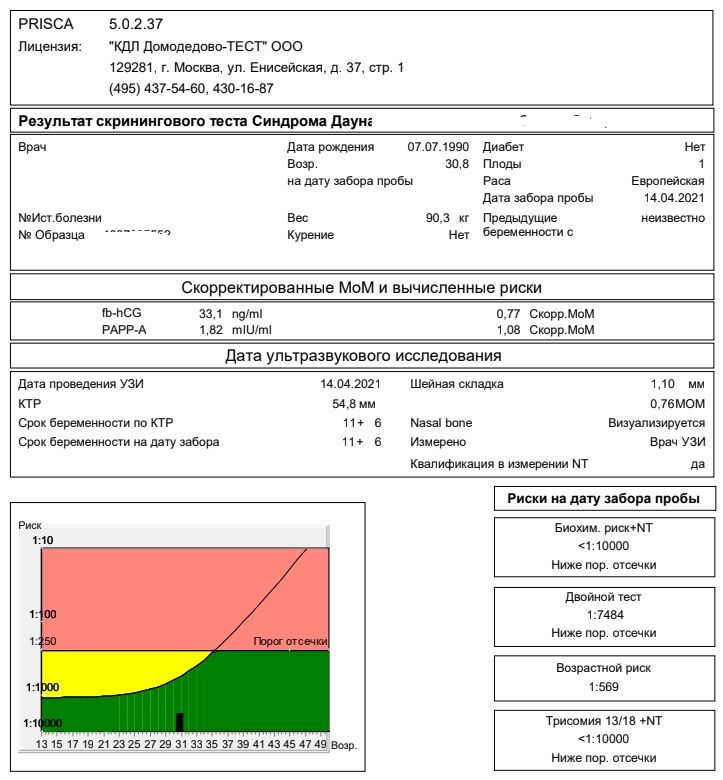
All pregnant individuals in California have access to California prenatal screening (CA PNS), also called sequential integrated screening. This noninvasive process is carried out in two steps.
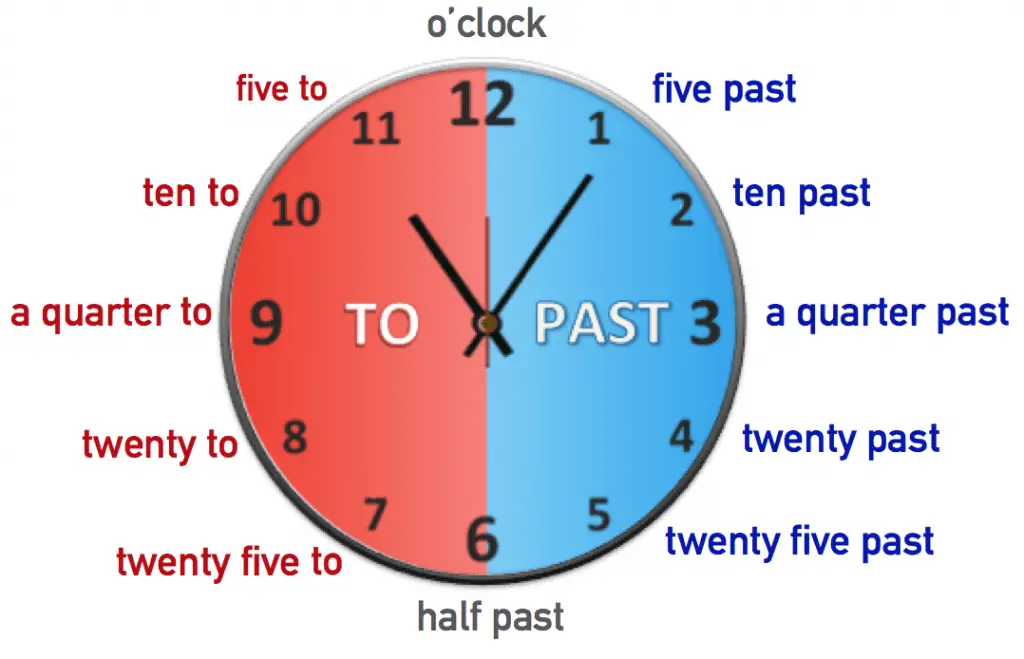
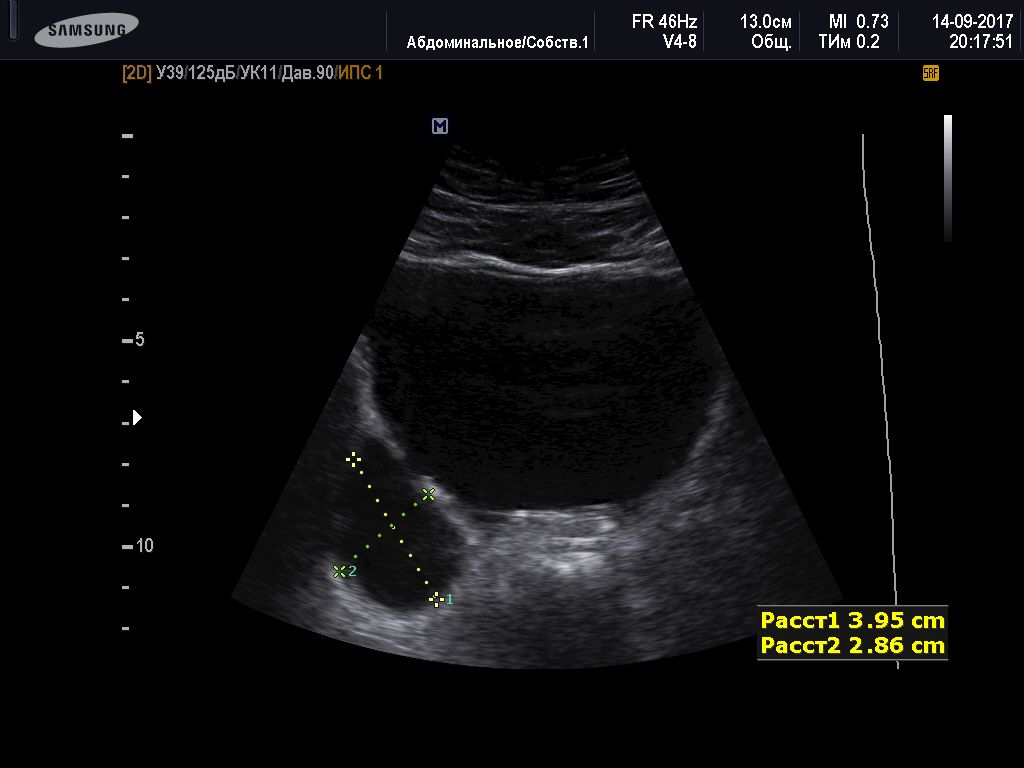
In the first step, which is performed when the pregnancy is between 10 and 14 weeks, a blood sample is taken from the pregnant person and a nuchal translucency ultrasound is performed to measure the fluid at the back of the baby's neck.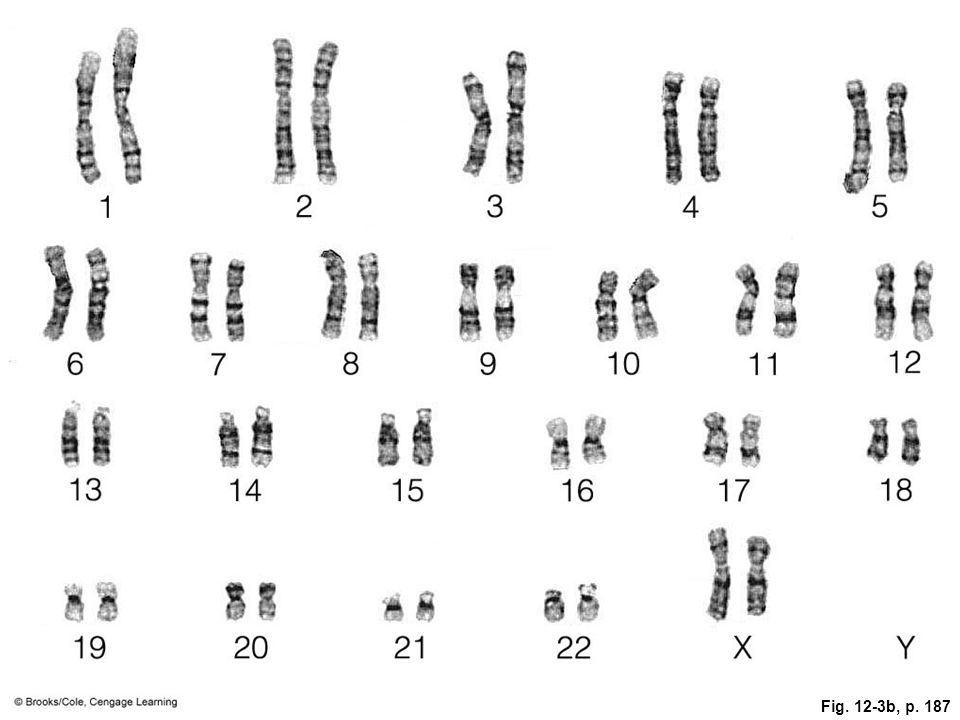 If the blood test is scheduled prior to the ultrasound, we can provide those results at the end of your ultrasound appointment. The blood test results, nuchal translucency measurement and pregnant person's age are together used to estimate the risk for Down syndrome and trisomy 18 (a genetic condition, also called Edwards syndrome, that affects fetal development).
If the blood test is scheduled prior to the ultrasound, we can provide those results at the end of your ultrasound appointment. The blood test results, nuchal translucency measurement and pregnant person's age are together used to estimate the risk for Down syndrome and trisomy 18 (a genetic condition, also called Edwards syndrome, that affects fetal development).
The second step is a test performed with a blood sample from the pregnant person when the pregnancy is between 15 and 20 weeks. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome (a genetic condition that can slow growth and cause intellectual disability), an open neural tube defect (a problem with the formation of the embryo's nervous system, such as spina bifida) or an abdominal wall defect (an abnormal opening in the abdomen).
Diagnostic tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis is the test we most commonly use to identify chromosomal problems, such as Down syndrome. (In at-risk fetuses, it can be used to detect other genetic diseases, such as cystic fibrosis, Tay-Sachs disease and sickle cell disease.)
An amniocentesis procedure for genetic testing is typically performed when the pregnancy is between 15 and 20 weeks. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small sample of amniotic fluid. Cells from the fluid are cultured and a karyotype test – an analysis of the cells' chromosomal makeup – is performed. It takes about two weeks to receive the results. Amniocentesis detects most chromosomal disorders with a high degree of accuracy.
There is a low risk of miscarriage as a result of amniocentesis – about 1 in 900. Miscarriage rates for amniocentesis performed at UCSF are extremely low.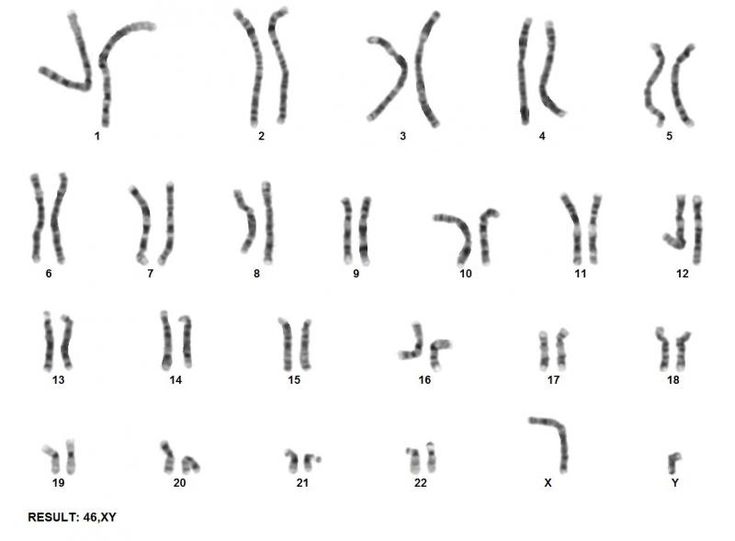
Like amniocentesis, chorionic villus sampling is most commonly used to identify chromosomal problems, such as Down syndrome. (It can also be used to detect other genetic diseases – including cystic fibrosis, Tay-Sachs disease and sickle cell disease – in at-risk fetuses.) The main advantage over amniocentesis is that CVS is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta for analysis. Under ultrasound guidance, this sample is obtained either with a needle inserted through the abdomen or a catheter inserted through the vagina and into the cervix (outer end of the uterus). The tissue is cultured and a karyotype test of the cells' chromosomal makeup is performed. It takes about two weeks to receive the results.
While it can provide information earlier in pregnancy than amniocentesis, CVS does not detect spinal cord defects. However, we can screen for spinal cord defects later in the pregnancy using expanded alpha-fetoprotein (AFP) blood testing or ultrasound.
There is a low risk of miscarriage as a result of CVS – about 1 in 450. Miscarriage rates for CVS procedures performed at UCSF are very low.
While the primary purpose of ultrasound is to determine the pregnancy's status – due date, size of the fetus and whether there's more than one baby – ultrasound can also provide some information about possible birth defects. All pregnant UCSF patients undergo a comprehensive ultrasound exam before any invasive tests are performed. We will explain your ultrasound results at the time of your visit.
In some patients, an ultrasound raises concern for a fetal abnormality. This possibility makes ultrasound expertise crucial, so you may find it reassuring that we have extensive experience in performing and interpreting ultrasound exams in pregnancy.
The meaning of a positive result
If you receive positive results on a screening test, we recommend that you discuss its implications and your options with your doctor and a genetic counselor. They will explain what types of diagnostic testing are available. Whether to have invasive genetic testing is your decision.
They will explain what types of diagnostic testing are available. Whether to have invasive genetic testing is your decision.
If a diagnostic test finds a genetic abnormality, we recommend discussing the significance of the result with experts on the condition, including a medical geneticist and a genetic counselor, as well as your doctor.
Trisomy test (13,18 and 21)
TRISOMY test is a quick, easy and safe method to learn more about the health of your unborn child.
The TRISOMY test is designed to rule out the most common genetic disorders (trisomy) of chromosomes 21, 18 and 13 that cause Down, Edwards and Patau syndromes. Before taking the test, you should consult a specialist in gynecology and obstetrics or a clinical geneticist.
Non-Invasive Prenatal Testing (NIPT) offered by various laboratories detects specific chromosome 21, 18 and 13 abnormalities and sex chromosome abnormalities. The tests give results that do not reveal any information about genetic or morphological fetal or maternal disorders other than those for which they are intended. Positive test results obtained with NIPT require confirmation by an invasive method.
Positive test results obtained with NIPT require confirmation by an invasive method.
Trisomy 21 (Down syndrome)
NIPT screening can detect more than 99% of cases of trisomy 21. Overall, only 1 in 1650 trisomy 21 as part of NIPT results based on normal pregnancy (0.06%)* was identified as false positive. With respect to the TRISOMY test, only 1 out of 1,842 results based on normal pregnancy was found to be false positive (i.e., less than 0.05%). The results of the latest validation study, which included a set of samples obtained from pregnant women and a set of samples containing embryonic trisomy 21, showed that the TRISOMY test is very sensitive.
Trisomy 18 (Edwards syndrome)
The sensitivity of NIPT in detecting trisomy 18 is lower than the sensitivity in detecting trisomy 21, namely in the amount of 90%*. The false positive rate of the TRISOMY test is 0.01%*. The false negative rate of the TRISOMY test (1 in 9 cases*) is comparable to the global rate (1 in 10 cases*).
Trisomy 13 (Patau syndrome)
Cases of trisomy 13 are rare in prospective studies, making calculations of the sensitivity and specificity of NIPT for this type of syndrome quite complex. In a recent international study based on 11,185 samples, 2 out of 2 positive cases* were successfully identified. The false positive rate for this type of trisomy in this particular study reached 0.02%*. With regard to the TRISOMY test screening test, 3 out of 3 trisomies were correctly identified within 13 cases, with a false positive rate of 0.05%.
TRISOMY test is a non-invasive maternal blood test that, due to its high sensitivity and specificity, can exclude the presence of chromosomal abnormalities already after the 11th week of pregnancy. The test can also determine the sex of the unborn child if the mother-to-be wishes to know.
The TRISOMY test is suitable for any pregnant woman as early as the 11th week of pregnancy.
Compared to traditional screening methods, the TRISOMY test has higher sensitivity and specificity for the types of trisomy for which it is intended.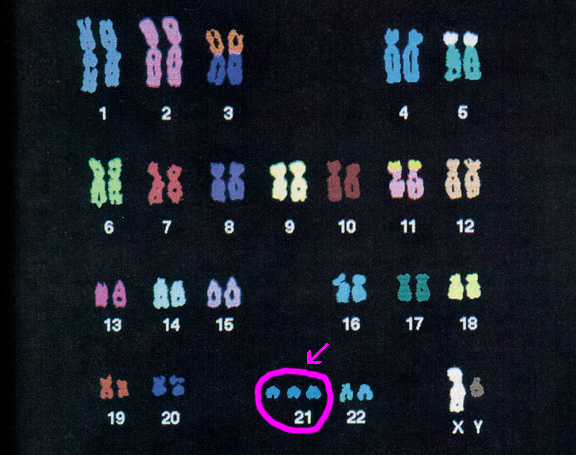 As a result, it provides a significantly lower number of false positives.
As a result, it provides a significantly lower number of false positives.
The TRISOMY test is suitable for pregnant women who:
are anxious about possible health problems for the unborn child caused by the presence of one of the studied types of trisomy;
who are 35 or older at birth and have a negative biochemical screening test;
conceived as a result of IVF,
had a positive biochemical screening*,
received an ultrasound screening result indicating a higher risk of traceable trisomy types,*
have had a fetal chromosomal abnormality in the past,*
their parent(s) have been diagnosed with a Robertsonian translocation (increased risk of trisomy 13 or 21),*
suffer from recurrent miscarriage.*
*Medical genetic counseling should be done prior to the test.
TRISOMY test is also useful in case of gynecological and obstetrical contraindications that may complicate invasive prenatal testing (amniocentesis), for example:
- increased risk of miscarriage,
- current anticoagulant therapy (low blood clotting),
- immune risk due to Rh incompatibility (Rhesus negative),
- gestational age from 14 to 16 weeks of gestation (increased risk of complications due to amniocentesis),
- placenta previa,
- uterine fibroids.
Consult your gynecologist/obstetrician for any obstetric contraindications.
Consultation with an OB/GYN or clinical geneticist is required prior to non-invasive prenatal testing.
TRISOMY test results
Non-invasive prenatal testing results provide information on a selected number of the most common genetic chromosomal disorders (up to 85% of all fetal genetic disorders). It should also be remembered that testing cannot detect all existing genetic or developmental disorders.
If your NIPT test is negative, it will help you avoid invasive diagnostic tests such as amniocentesis, which carry certain risks associated with taking amniotic fluid.
The sensitivity and specificity of the TRISOMY test are over 99%.
Attention: Despite the high sensitivity and specificity in the detection of fetal trisomy on the 21st, 18th and 13th chromosomes, the TRISOMY test is considered a type of screening and not a diagnostic method. Therefore, a positive result should always be confirmed by taking amniotic fluid or chorionic villi.
Therefore, a positive result should always be confirmed by taking amniotic fluid or chorionic villi.
A negative TRISOMY test result does not need to be confirmed by diagnostic amniocentesis, which means that in most cases the mother-to-be can avoid invasive tests and their associated risks.
If the TRISOMY test is positive, you should consult with a geneticist who will refer you for the examination required in this situation.
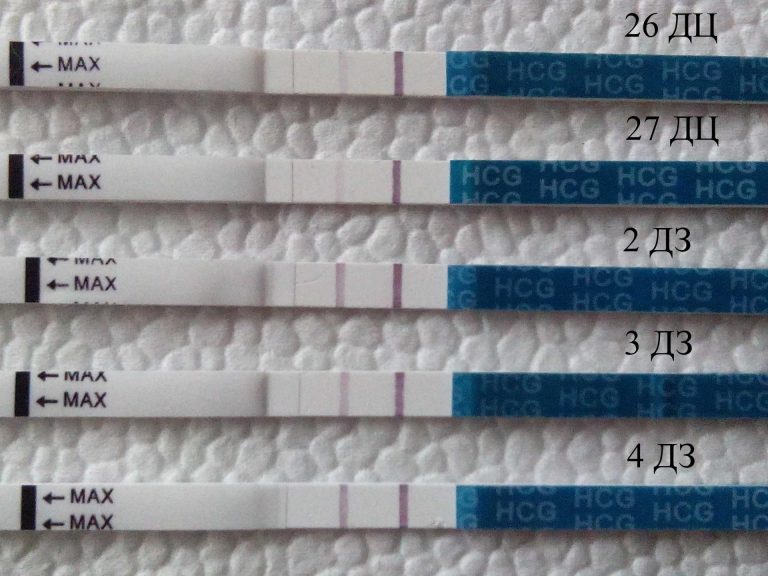
ᐈ Analysis for the presence of Down syndrome (trisomy 21 chromosomes), sex determination in Kyiv, prices
A non-invasive test that can reliably determine the presence of Down syndrome in a fetus and determine its gender. The clinical test is completely safe for both the fetus and the expectant mother. Down syndrome is the most well-known chromosomal disorder - it is diagnosed in one in 700-900 babies born worldwide. A medical diagnosis is made on the basis of a laboratory test and a doctor.
Each human cell contains 46 chromosomes, whose DNA determines appearance and development.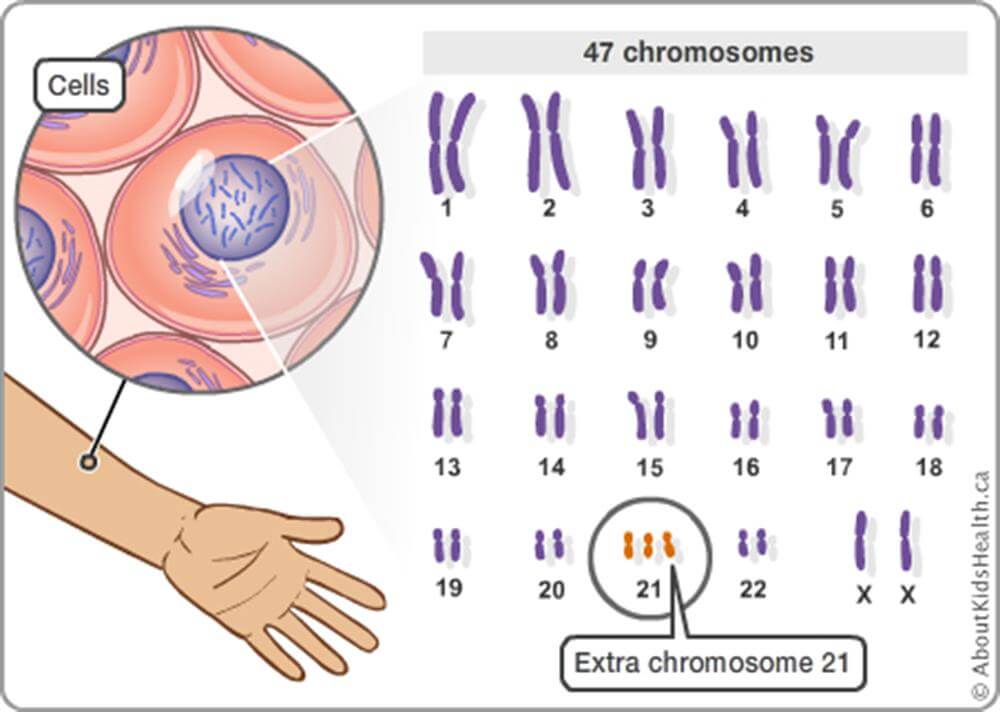 Down syndrome results when there is an extra partial or complete copy of chromosome 21 (trisomy 21). There may be several reasons for this, the most common of which is an error in cell distribution, which results in an embryo with three copies of chromosome 21 instead of the usual two, which is why a laboratory test for this syndrome is so important.
Down syndrome results when there is an extra partial or complete copy of chromosome 21 (trisomy 21). There may be several reasons for this, the most common of which is an error in cell distribution, which results in an embryo with three copies of chromosome 21 instead of the usual two, which is why a laboratory test for this syndrome is so important.
As the embryo develops, an extra chromosome is replicated in every cell of the body. This type of development of Down syndrome is 95% of cases. About 4% of cases of this disease are due to translocation - while the total number of chromosomes in cells is 46, but an additional complete or partial copy of chromosome 21 is attached to another chromosome. Sometimes an additional examination is required to make a diagnosis. In addition, in very rare cases, there may be mosaic Down syndrome. It is diagnosed if there are two types of cells in the body: some contain the usual chromosomes 46, and some 47 (in them they find an additional chromosome 21). An additional partial or complete copy of the 21st chromosome, the embryo most often receives from the mother. If a woman gave birth to a child with trisomy 21, then it is believed that the probability of her having a second child with the same pathology is 1 to 100. By carefully studying the biological material of the study, it is possible to determine the exact indicators of the analysis. The non-invasive prenatal test for trisomy 21 in a fetus is a new and improved prenatal test capable of detecting the chromosomal material of a fetus circulating in the maternal blood. Also, this test determines the sex of the child with an accuracy of> 99.9%. Gender is optional. The possibility of passing the test with a quality guarantee is provided by the ADONIS clinic, where you can take the material in any convenient laboratory.
An additional partial or complete copy of the 21st chromosome, the embryo most often receives from the mother. If a woman gave birth to a child with trisomy 21, then it is believed that the probability of her having a second child with the same pathology is 1 to 100. By carefully studying the biological material of the study, it is possible to determine the exact indicators of the analysis. The non-invasive prenatal test for trisomy 21 in a fetus is a new and improved prenatal test capable of detecting the chromosomal material of a fetus circulating in the maternal blood. Also, this test determines the sex of the child with an accuracy of> 99.9%. Gender is optional. The possibility of passing the test with a quality guarantee is provided by the ADONIS clinic, where you can take the material in any convenient laboratory.
Non-invasive prenatal test for the presence of Down's syndrome, sex determination, is indicated for the diagnosis of women over 35 years of age with chromosomal abnormalities in relatives, with a history of reproductive losses, with 2 or more IVF failures, with changes in biochemical markers by screening. The exact diagnosis is determined by the doctor.
The exact diagnosis is determined by the doctor.
The conclusion of the study can be presented in two versions:
"Low risk" - the child is unlikely to have Down syndrome.
"High risk" - Evidence of trisomy 21 was found. This test result may indicate that the fetus has Down syndrome.
The price of the study is indicated on the website.
DNA sex determination reveals the Y chromosome. When a Y chromosome is found, you will be given the conclusion that your unborn child will be a boy. If the Y-chromosome marker is not found, then you will get the conclusion that you will have a girl. You can take a test in Kyiv at any ADONIS department.
Biomaterial type
Venous blood
Patient preparation rules
30 minutes - no smoking. Medicines, alcohol, coffee, excessive physical activity can affect the results of laboratory tests and their diagnostic value.