What can you take for indigestion while pregnant
What Medications Are Safe During Pregnancy?
There’s no doubt that along with the joys of pregnancy, women can and do experience uncomfortable side effects. If you’re feeling under the weather, you may be wondering if over-the-counter remedies are safe for you and your baby. In most cases, it’s best to avoid OTC (over-the-counter) medications particularly in the first 14 weeks of pregnancy. While some medications are safe to use in limited quantities, other medicines are known to increase the chance of birth defects or other problems.
If you have questions or are considering a medication that’s not listed below, please reach out to your doctor for additional safety information. You should also call your doctor if you have a fever 100.4 F or greater, or if symptoms persist or worsen. The obstetrics specialists at Northeast Georgia Physicians Group are here to help you weigh the risks and benefits of prescription and over-the-counter medications that are safe to take during pregnancy.
Safe Over-the-Counter Medications
Claritin
ZyrtecBenadryl
- Tums
- Rolaids
- Mylanta
- Tagamet, Pepcid, Prilosec, Prevacid (If no relief from Tums or Rolaids)
- Tylenol (for Aches & Pains, limited to 2000 mg in 24 hrs)
- Chloraseptic/Cepacol Lozenges (for sore throat)
- High-bran diet and increase water
- Metamucil
- Psyllium Colace/Docusate
- Milk of Magnesia
Robitussin (plain)
Mucinex
- Instant Ocean Spray
- Rhinocort
- Nasonex
- Flonase
- Kaopectate
- Immodium
- BRAT diet (bananas, rice, applesauce, tea or toast)
It’s okay to see a dentist, but be sure to use an abdominal shield if having x-rays done. You can also have Novocaine® and certain antibiotics and pain medications. Be sure to notify dentist that you are pregnant.
- Mylanta
- Maalox
- Tums
- Rolaids
- Gas-X/Simethicone, Tagamet,
- Pepcid, Prilosec, Prevacid (If no relief from Tums or Rolaids)
Tylenol (limited to 2000 mg in 24 hrs)
- Preparation H
- Anusol HC
- Tucks pads
- Sitz baths (with or without Epsom salts)
- Konsyl Easy Mix (daily to keep
- stools soft)
- Look for a supplement with a stool softener or add Colace/Docusate when taking iron
- Slow Fe
- Fergon
- Feosal Bifera
- Irospan
- Benadryl
- Tylenol PM (if you also have pain & limited to 2000 mg in 24 hrs)
- Unisom
- Chamomile Tea
- Caltrate
- Calcet
- Viactiv
- Calcium, magnesium supplement
- Epsom salt baths
- Small, frequent meals (every 2-3 hrs)
- Sea bands (wristband)
- Vitamin B6 (25mg 3 times/daily and 1 Unisom/Doxylamine at night)
- Ginger, ginger tea
- Peppermint and cinnamon
- Warm salt water gargle (several times/day)
- Cepacol lozenges
- Vicks lozenges or spray (Avoid anything with phenol)
Herbal Supplements and Vitamins
Some alternative therapies have been found to safely and effectively alleviate some of the uncomfortable side effects of pregnancy – but ‘natural’ doesn’t always mean these herbal supplements are safe. As with any over the counter medication, it’s important to talk with your doctor about every supplement or vitamin you take while pregnant.
As with any over the counter medication, it’s important to talk with your doctor about every supplement or vitamin you take while pregnant.
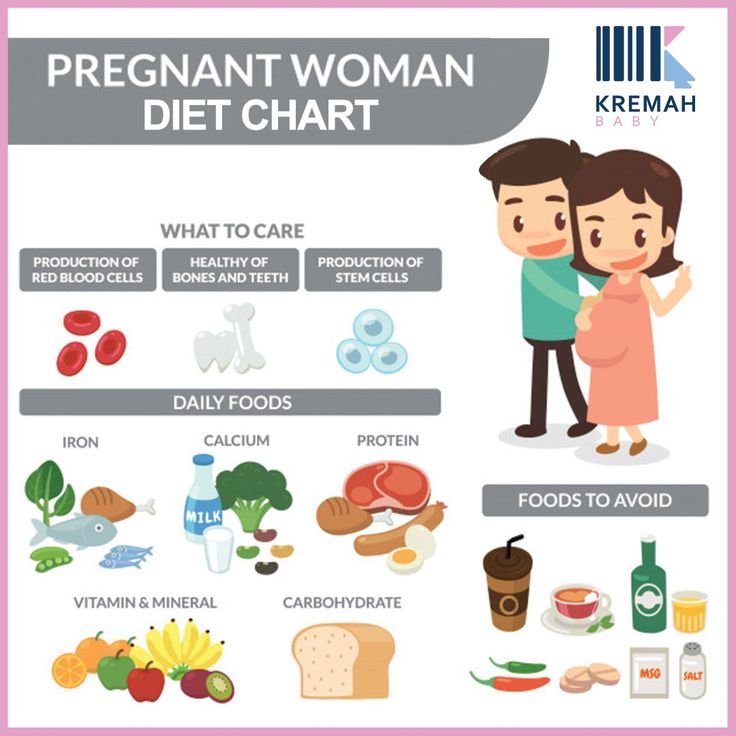
Prenatal vitamins are also an important part of a healthy pregnancy. Multivitamins that include folic acid are safe and important before and during the first few weeks of pregnancy because they can help prevent some birth defects. Your doctor or midwife can advise you about which type of multivitamin with folic acid you should take. Medical providers sometimes prescribe extra folic acid or iron supplements, depending on your specific situation.
Get Started
The obstetrics specialists at Northeast Georgia Physicians group offer the full range of pregnancy and delivery services including prenatal screening, genetic counseling, midwifery, genetic counseling, high-risk pregnancy care and more. For questions or to schedule an appointment, call 770-219-9300 or fill out the form to the right of this page.
Pregnancy Heartburn? 7 Ways to Get Relief
Keywords
Kathryn Walker, MD
Women and Newborn
Learn more about women and newborn services we offer.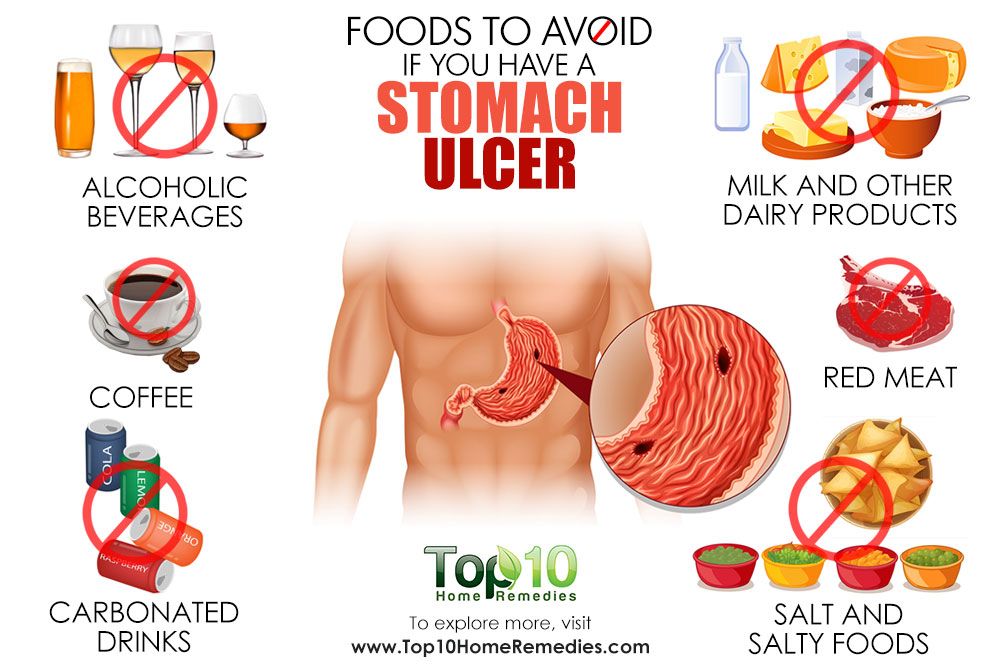
Expectant mothers everywhere are aching to know one thing: “How can I get some relief from this awful pregnancy heartburn?”
To help ease your pain, here are some answers to your “burning” questions. (Pardon the pun.)
When you’re growing a human being, you don’t have time for that yucky acid reflux. But your usual go-to methods for treating it may not be safe for your unborn baby. (Remember Pepto Bismol? That’s on the No Fly List for moms-to-be, according to FDA recommendations.)
Instead, here are some of the safest and best ways to get rid of heartburn when you’re pregnant:
- Dip into some yogurt. Its probiotics and soothing texture make yogurt a great option for extinguishing heartburn – or at least dousing the flames a little.
- Drink milk with honey. According to the American Pregnancy Association, a tablespoon of honey mixed in a glass of warm milk may be just what you need to neutralize heartburn-causing acid.
- Snack on almonds. Munching on a handful of almonds may provide heartburn relief since these nuts have a lower acidity level than others.
- Eat pineapple or papaya. For some women, the digestive enzymes in pineapple and papaya have helped ease symptoms. Eating these fruits after your meals can aid digestion and reduce your chances of heartburn.
- Try a little ginger. You probably knew ginger was a good remedy for an upset stomach. Well, that makes it a helpful candidate for fighting off heartburn, too. Among ginger’s many benefits, it can reduce inflammation and prevent stomach acid from traveling up the esophagus.
- Chew sugar-free gum. Another effective method for taming the burn is to chew some sugar-free gum. One study found that chewing sugar-free gum for 30 minutes after a meal can reduce acid reflux.
- Take (doctor-approved) medication. When all else fails, certain medications are considered safe to use for pregnancy heartburn relief.
 Just make sure you speak to your doctor or OB-GYN first. If your heartburn is severe, they may prescribe special medication to help control it.
Just make sure you speak to your doctor or OB-GYN first. If your heartburn is severe, they may prescribe special medication to help control it.
While not every tip mentioned above may work to ease your symptoms, you’ve got nine months to try them all and figure out what works.
It’s important to be extremely careful about the medications you take when pregnant.
For heartburn relief, over-the-counter antacids (such as Tums, Mylanta, Rolaids, and Maalox) are all considered safe medications to use during pregnancy.
As always, consult with your provider about any medications you’re taking – even if they’re considered safe. (This is especially true for high-risk pregnancies.)
If you experience any unusual symptoms while taking an over-the-counter medication, call your doctor immediately.
They say prevention is the best medicine, so knowing common heartburn triggers can help you keep the acid at bay.
Of course, pregnancy itself is a major trigger for heartburn.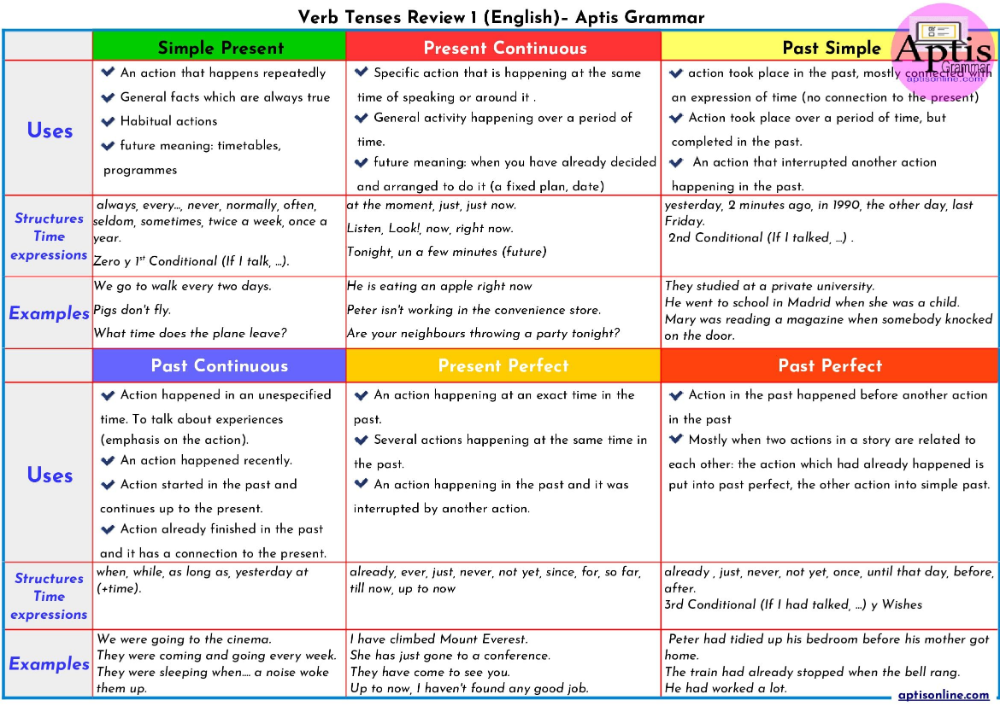 As your growing uterus puts pressure on your stomach, this pushes stomach acid up your throat.
As your growing uterus puts pressure on your stomach, this pushes stomach acid up your throat.
Those lovely hormones are no help either. They tend to relax the valve between your stomach and esophagus, which makes it easier for acid to make its way upward.
While there’s nothing you can do to stop this entirely, there are a few things that can help prevent heartburn from flaring up during pregnancy:
- Avoid lying down after eating. It may be tempting to take a post-meal nap, but if you want to prevent heartburn, don’t lie down after eating. Consider napping in an upright recliner instead.
- Prop yourself up at night. It’s hard enough to sleep well while pregnant without throwing acid reflux on top of everything. To prevent nighttime heartburn, try propping yourself up when you go to sleep to counteract the acid.
- Don’t eat before bedtime. In addition to propping yourself up at night, try not to eat anything within three hours of hitting the sack.
- Skip spicy, acidic, or fried foods. Ask yourself: Are those greasy chips worth being doubled over in pain later? (Probably not.) If you want to avoid the risk, steer clear of any and all rich, fatty foods. Not only will this help prevent heartburn, but making more nutritious choices helps ensure that you your baby is getting the important vitamins and minerals that they need to stay healthy in utero.
- Eat small meals, but more frequently. Your pregnant tummy doesn’t love to be hit with large amounts of food to digest in one go. Make things easier on your gut by eating several small meals throughout the day instead of three large ones.
- Eat slowly. Wolfing down those small meals will defeat the purpose of spreading them out. Eating quickly increases the risk of acid reflux, so slow down and enjoy your food.
- Wear loose clothing. Tight-fitting clothes are not your stomach’s best friend when you’re trying to prevent heartburn – particularly during pregnancy.
 Wear clothing that offers support without being restrictive.
Wear clothing that offers support without being restrictive. - Drink your liquids between meals. If you’re the type of person who likes to take a swig of their drink between each bite, it’s time to change course. Drinking liquids during meals can exacerbate heartburn symptoms, so take little sips if you’re thirsty at mealtime.
Someday, scientists may very well invent a miracle medication that promises permanent pregnancy heartburn relief. Unfortunately, that hasn’t happened yet.
So, if you’re wondering how long you can expect to deal with heartburn while you’re pregnant, it will probably be throughout your entire pregnancy. (Now may be a good time to remind yourself that you get a cute little baby out of this when you’re done.)
However, just because there’s no cure, that doesn’t mean you can’t find some relief in the meantime.
If severe pregnancy heartburn is getting in the way of everyday life, it’s time to see a doctor.
Intermountain Healthcare offers individualized and compassionate pregnancy care for women of all ages and health needs.
To get the care you need, search for a provider or find an Intermountain Healthcare location near you.
Intermountain Moms Women's Health, Baby Your Baby, Pregnancy, Women and Newborn
Last Updated: 5/21/2021
-
Intermountain Moms
-
Intermountain Moms
Copyright ©2023, Intermountain Healthcare, All rights reserved.
Diarrhea during pregnancy: symptoms, causes and consequences, diagnosis and treatment
Diarrhea during pregnancy: causes, diagnosis and treatment Average reading time: 9 minutes
Contents:
Causes and symptoms of diarrhea during pregnancy
Diagnostic features
The consequences of diarrhea in pregnant women
Directions of treatment
When treatment is required in the hospital
Diets
Can I use the Imodium ® Express during pregnancy
of pregnancy in the early periods can be earned during pregnancy, not only a deterioration in well-being, but also unwanted unrest for a woman who is expecting a baby. Frequent defecation causes significant discomfort and is often accompanied by additional unpleasant symptoms. In addition, this condition can pose a serious danger to the woman and the fetus due to the threat of dehydration and other risks. One of the difficulties is that with diarrhea in pregnant women in the first trimester, not all antidiarrheal drugs can be drunk. The active components of some drugs can have a negative effect on the fetus. That is why with frequent bowel movements it is necessary to consult a specialist. The doctor will diagnose and tell you what to do with diarrhea.
One of the difficulties is that with diarrhea in pregnant women in the first trimester, not all antidiarrheal drugs can be drunk. The active components of some drugs can have a negative effect on the fetus. That is why with frequent bowel movements it is necessary to consult a specialist. The doctor will diagnose and tell you what to do with diarrhea.
Back to top
Causes and symptoms of diarrhea during pregnancy
Infectious. Bacterial and viral infections (eg, noro- or rotavirus) can cause bowel dysfunction. They are usually transmitted by airborne droplets or the fecal-oral route. Pathogenic microorganisms also often enter the gastrointestinal tract through the use of low-quality foods or contaminated water. Infectious diarrhea during pregnancy in the second and third trimester may be accompanied by fever, chills, nausea and vomiting, painful abdominal cramps, and general weakness. An admixture of mucus often appears in the feces.
Non-infectious. This form of diarrhea can be caused by a variety of factors: changes in diet, frequent stress, disorders of digestion and absorption, some chronic diseases, taking certain medications. In this case, the pregnant woman may be disturbed by frequent defecation (sometimes with imperative, i.e., strongly pronounced, irresistible urges), abdominal pain in the upper or lower section. With organic lesions of the colon, an admixture of blood sometimes appears in the feces. In the later stages, violations of the frequency of bowel movements may be associated with fetal pressure on the digestive tract.
This form of diarrhea can be caused by a variety of factors: changes in diet, frequent stress, disorders of digestion and absorption, some chronic diseases, taking certain medications. In this case, the pregnant woman may be disturbed by frequent defecation (sometimes with imperative, i.e., strongly pronounced, irresistible urges), abdominal pain in the upper or lower section. With organic lesions of the colon, an admixture of blood sometimes appears in the feces. In the later stages, violations of the frequency of bowel movements may be associated with fetal pressure on the digestive tract.
Up to content
Diagnostic features
When diagnosing a disease that caused diarrhea, it is important to exclude surgical, urological and obstetric pathologies. For this, an examination is mandatory, if necessary, the doctor prescribes an additional examination. Early diarrhea may be a manifestation of ectopic pregnancy, appendicitis, urinary tract infections, pyelonephritis, inflammatory bowel disease, and acute pancreatitis. That is why it is important to quickly establish the cause of the disruption of the intestines and select adequate therapy. It is also mandatory to monitor (monitor observation) the condition of the fetus at 37, 38 and 39weeks of pregnancy.
That is why it is important to quickly establish the cause of the disruption of the intestines and select adequate therapy. It is also mandatory to monitor (monitor observation) the condition of the fetus at 37, 38 and 39weeks of pregnancy.
Back to Contents
Effects of Diarrhea in Early Pregnancy
Prolonged diarrhea can lead to dehydration, a condition that is dangerous for both the expectant mother and the fetus. It is manifested by severe weakness, dry mucous membranes, thirst. With a strong degree of dehydration, cardiac and respiratory activity can be disturbed. Diarrhea can also in some cases increase the risk of miscarriage due to an increase in the contractile activity of the uterus, and can lead to impaired uteroplacental blood flow.
Up to content
Directions for treatment
How to treat diarrhea should be decided by the doctor, taking into account the woman's condition, the cause of indigestion, gestational age and other factors. Typically, therapy includes the following areas.
Typically, therapy includes the following areas.
| Restoration of water and electrolyte balance | Replenishment of fluid deficiency in pathologies accompanied by diarrhea is an important measure to prevent severe and life-threatening conditions. To restore the water and electrolyte balance, pregnant women, on the recommendation of a doctor, can drink non-carbonated mineral water or rehydration solutions. The latter contain the salts necessary for the body, which are excreted from it along with the liquid. It should be borne in mind that with severe dehydration, drinking a solution of salts may no longer be enough. In this case, rehydration drugs are infused intravenously (in a hospital setting, if recommended by a doctor). |
| Elimination of toxins | To reduce the load on the body, it is necessary to help it get rid of toxic substances. In some cases, gastric lavage is performed for this purpose. |
| Restoration of normal intestinal microflora | To normalize the processes of digestion and absorption, it is necessary that beneficial bacteria be present in the intestine. They can be obtained from food (for example, fermented milk products with live cultures). In addition, according to indications, the doctor may prescribe probiotic preparations that help restore intestinal microflora. |
| Relieve the cause of diarrhea | If frequent bowel movements are a symptom of a bacterial infection, antibiotics may be used to treat them. Such remedies can help eliminate the cause of diarrhea by destroying pathogenic microorganisms. |
Back to Table of Contents
When Hospital Treatment is Necessary
Diarrhea is not always treated at home. With severe dehydration, the risk of miscarriage, severe concomitant diseases, the doctor may suggest that the pregnant woman go to the hospital. Such a measure allows for constant medical supervision, which in such cases is often simply necessary. Urgently seek medical attention and urgent hospitalization may be required if:
- severe abdominal pain of any location;
- blood in feces;
- general lethargy.
Standard clinical indications for inpatient treatment are moderate to severe diarrhea accompanied by dehydration. It is also necessary to go to the hospital if home therapy does not work for 3-4 days (the pregnant woman does not get better, the symptoms persist).
Important! Even on an outpatient basis, the treatment of conditions accompanied by diarrhea should be carried out under the supervision of a physician.
Back to Contents
Diet
During the treatment of diarrhea, it is very important to adjust your diet in order to reduce the load on the digestive tract and help the body cope with the problem faster. In case of violations of the intestines, accompanied by frequent defecation, spicy, sour, fatty foods are excluded from the diet. With an intestinal disorder, you can not use whole milk, fresh fruits and vegetables, legumes, sweets, spices, smoked snacks. Liquid, semi-liquid, pureed, steamed products are allowed. They should be served warm, but not hot or cold. In the early days of infectious diarrhea, experts may recommend a starvation diet. Then, rice water, liquid cereals from oatmeal or buckwheat are introduced into the diet.
Up to content
Can I use IMODIUM
® Express in early pregnancy? The active substance of the drug is loperamide, data on the teratogenic or embryotoxic effect of which are absent. However, the drug can not be used at any stage of pregnancy.The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
1 According to the instructions for medical use of the drug IMODIUM ® Express.
* Among products based on Loperamide. According to sales in money for February 2018 - January 2019, according to IQVIA.
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are more often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during a previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Increased levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk to mother and child and will pass by 16-20 weeks of pregnancy, but it is not necessary to wait that long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
Rarely, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include: dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a vacation in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis, or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Diarrhea during pregnancy is not usually a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potatoes |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
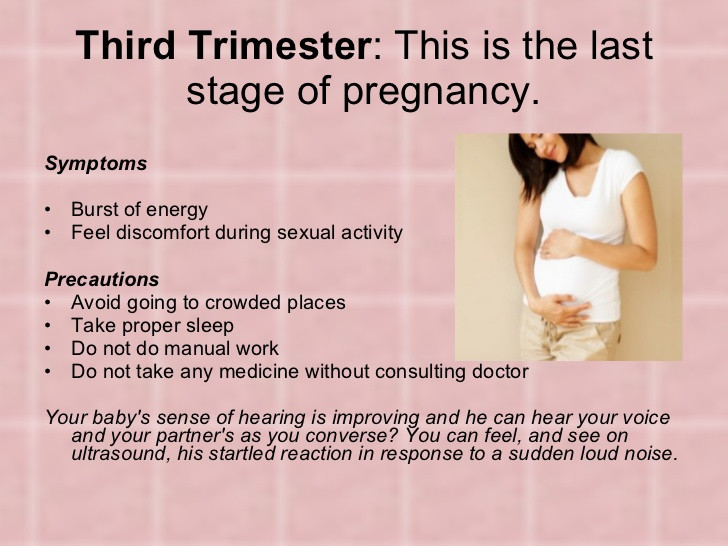
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you do not usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into the diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation is accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, call your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut.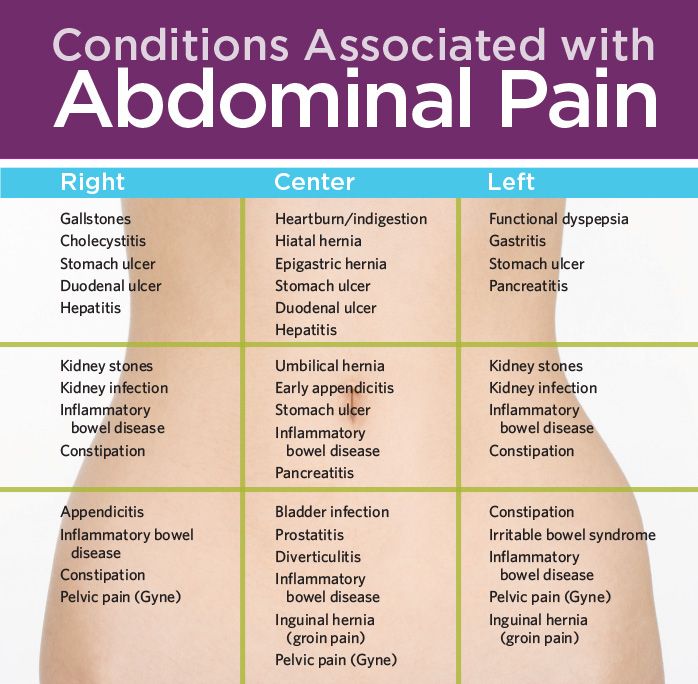 Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for a future pregnancy and reduce the risk of digestive problems.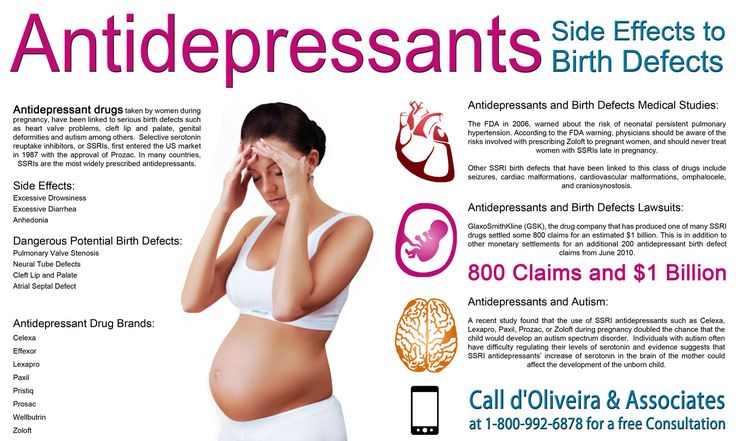
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.
 The drugs are used strictly according to the doctor's prescription.
The drugs are used strictly according to the doctor's prescription.