How long does croup last in a child
Croup
Is this your child's symptom?
- Barky cough and hoarse voice caused by a virus
- Croup is a viral infection of the voicebox (larynx)
- The croupy cough is tight, low-pitched, and barky (like a barking seal)
- The voice or cry is hoarse (called laryngitis)
- Some children with severe croup get a harsh, tight sound while breathing in. This is called stridor.
Stridor: Another Health Problem of Croup
- Stridor is a harsh, raspy tight sound best heard with breathing in
- Loud or constant stridor means severe croup. So does stridor at rest (when not crying or coughing).
- All stridor needs to be treated with warm mist
- Most children with stridor need treatment with a steroid (such as Decadron)
- For any stridor, see First Aid for treatment
Causes of a Croupy Cough
- Viral Croup. Viruses are the most common cause of croup symptoms. Many respiratory viruses can infect the vocal cord area and cause narrowing.
Even influenza (the flu) can do this. A fever is often present with the barky cough.
- Allergic Croup. A croupy cough can occur with exposure to pollens or allergens in a barn. A runny nose, itchy eyes and sneezing are also often present.
- Inhaled Powder. Breathing in any fine substance can trigger 10 minutes of severe coughing. Examples are powdered sugar, flour dust or peanut dust. They can float into the lungs. This is not an allergic reaction.
- Airway Foreign Object (Serious). Suspect when there is a sudden onset of coughing and choking. Common examples are peanut and seeds. Peak age is 1 to 4 years.
- Food Allergy (Serious). Croup symptoms can also be caused by a food allergy. This can be life-threatening (anaphylaxis). Examples are nuts or fish.
When to Call for Croup
Call 911 Now
- Severe trouble breathing (struggling for each breath, constant severe stridor)
- Passed out or stopped breathing
- Lips or face are bluish when not coughing
- Croup started suddenly after bee sting, taking a new medicine or allergic food
- Drooling, spitting or having great trouble swallowing.
 Exception: drooling due to teething.
Exception: drooling due to teething. - You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Stridor (harsh sound with breathing in) is heard now
- Trouble breathing, but not severe
- Lips or face have turned bluish during coughing
- Breathing is much faster than normal
- Can't bend the neck forward
- Severe chest pain
- Had croup before that needed Decadron
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- High-risk child (such as cystic fibrosis or other chronic lung disease)
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Stridor (harsh sound with breathing in) occurred but not present now
- Nonstop coughing
- Age less than 1 year old with a croupy cough
- Earache or ear drainage
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Coughing causes vomiting 3 or more times
- Croup is a frequent problem (3 or more times)
- Barky cough lasts more than 14 days
- You have other questions or concerns
Self Care at Home
- Mild croup (barky cough) with no stridor
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Croup
- What You Should Know About Croup:
- Most children with croup just have a barky cough.
- Some have tight breathing (called stridor). Stridor is a loud, harsh sound when breathing in. It comes from the area of the voicebox.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- We want to help a productive cough, not turn it off.

- Here is some care advice that should help.
- First Aid for Stridor (Harsh sound with breathing in):
- Breathe warm mist in a closed bathroom with the hot shower running. Do this for 20 minutes.
- You could also use a wet washcloth held near the face.
- Caution: do not use very hot water or steam which could cause burns.
- If warm mist fails, breathe cool air by standing near an open refrigerator. You can also go outside with your child if the weather is cold. Do this for a few minutes.
- Calm Your Child if He or She has Stridor:
- Crying or fear can make stridor worse.
- Try to keep your child calm and happy.
- Hold and comfort your child.
- Use a soothing, soft voice.
- Humidifier:
- If the air in your home is dry, use a humidifier.
- Reason: dry air makes croup worse.
- Homemade Cough Medicine:
- Goal: decrease the irritation or tickle in the throat that causes a dry cough.
- Age 6 months to 1 year: give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: use a dose of 1-2 teaspoons (5-10 mL). Give 4 times per day when coughing. Caution: do not use honey until 1 year old.
- Age 1 year and older: use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
- Age 6 years and older: use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
- Goal: decrease the irritation or tickle in the throat that causes a dry cough.
- Non-Prescription Cough Medicine (DM):
- Non-prescription cough medicines are not advised. Reason: no proven benefit for children and not approved under 6 years old (FDA).
- Honey has been shown to work better for coughs. Caution: do not use honey until 1 year old.
- If age 6 years or older, you might decide to use a cough medicine.
 Choose one with dextromethorphan (DM) such as Robitussin Cough syrup. DM is present in most non-prescription cough syrups. Follow the instructions on the package.
Choose one with dextromethorphan (DM) such as Robitussin Cough syrup. DM is present in most non-prescription cough syrups. Follow the instructions on the package. - When to Use: give only for severe coughs that interfere with sleep or school.
- DM Dose: give every 6 to 8 hours as needed.
- Coughing Fits or Spells - Warm Mist and Fluids:
- Breathe warm mist, such as with shower running in a closed bathroom.
- Give warm clear fluids to drink. Examples are apple juice and lemonade.
- Age less than 6 months. Only give breast milk or formula
- Age 6 - 12 months. Give 1-2 teaspoons (5-10 mL) each time. Limit to 4 times per day.
- Age over 1 year. Give as much warm fluids as needed.
- Reason: both relax the airway and loosen up any phlegm.
- Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: keep your child well hydrated.
- It also loosens up any phlegm in the lungs.
 Then it's easier to cough up.
Then it's easier to cough up.
- Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: keep your child well hydrated. Give lots of cold fluids.
- Sleep Close by to Your Child:
- Sleep in the same room with your child for a few nights.
- Reason: stridor can start all of a sudden at night.
- Avoid Tobacco Smoke:
- Tobacco smoke makes croup much worse.
- Return to School:
- Your child can go back to school after the fever is gone.
- Your child should also feel well enough to join in normal activities.
- For practical purposes, the spread of croup and colds cannot be prevented.
- What to Expect:
- Most often, croup lasts 5 to 6 days and becomes worse at night.
- The croupy cough can last up to 2 weeks.
- Most often, croup lasts 5 to 6 days and becomes worse at night.
- Call Your Doctor If:
- Trouble breathing occurs
- Stridor (harsh raspy sound) occurs
- Croupy cough lasts more than 14 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 02/01/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
Kids Health Information : Croup
This fact sheet is available in the following languages:
Arabic,
Assyrian,
Burmese,
Chinese (simplified),
Chinese (traditional),
English,
Karen,
Persian,
Somali,
Turkish and
Vietnamese.
Croup is a condition caused by a viral infection. The virus leads to swelling of the voice box (larynx) and windpipe (trachea). This swelling makes the airway narrower, so it is harder to breathe. Children with croup develop a harsh, barking cough and may make a noisy, high-pitched sound when they breathe in (stridor).
Croup mostly affects children between six months and five years old, but it can affect older children. Some children get croup several times.
Croup can get worse quickly. If your child is having problems breathing, seek urgent medical attention.
Signs and symptoms of croup
- Croup usually begins like a normal cold, e.g. fever, runny nose and cough.
- Your child's cough will change to become harsh and barking, and might sound like a seal.
- Your child's voice may be hoarse.
- When your child breathes in, they may make a squeaky, high pitched noise, which is called stridor.
- In severe cases of croup, the skin between the child’s ribs or under their neck may suck in when they breathe, and they may struggle to breathe.
Croup often begins without warning, in the middle of the night. The symptoms are often worse at night, and are at their worst on the second or third night of the illness. The signs and symptoms of croup may last for three to four days; however, a cough may linger for up to three weeks. The stridor should not persist.
Care at home
A mild attack of croup is when your child has the harsh, barking cough but does not have stridor when they are calm and settled, and they are not struggling to breathe. No medical treatment is necessary for mild croup, or the virus that has caused it. You can usually manage mild croup at home with the following care:
- Keep your child calm, as breathing is often more difficult when upset – the more a child is distressed, the worse their symptoms can become.
 Try sitting quietly, reading a book, or watching TV.
Try sitting quietly, reading a book, or watching TV. - If your child has a fever and is irritable, you may give them paracetamol or ibuprofen. See our fact sheet Pain relief for children.
- Croup often becomes worse at night. Many children will be more settled if someone stays with them.
Steam and humidifiers are no longer recommended as treatment. There is no evidence to suggest they are beneficial.
When to see a doctor
You should call an ambulance immediately if:
- your child is struggling to breathe
- your child looks very sick and becomes pale and drowsy
- your child’s lips are blue in colour
- your child starts to drool or can’t swallow.
You should see a doctor if:
- your child is under six months old and has signs and symptoms of croup
- your child's breastbone or the skin between their ribs sucks when they breathe in
- your child has stridor when at rest
- your child is very distressed or their symptoms are getting worse
- you are worried for any other reason.
If your child has mild croup that lasts for more than four days, or if stridor returns after your child has recovered from croup, take them to see a doctor.
Your doctor may prescribe steroids (e.g. prednisolone or dexamethasone) to be taken by mouth. The steroids help reduce the swelling in the airway, which will make breathing easier. Antibiotics do not work on viruses and are not given to children with croup.
If your child has severe croup, they will need to stay in hospital, where they will be closely watched.
How is croup spread?
Even though not all children get croup when infected by the virus, the virus that has caused the croup can be spread easily from person to person by coughing and sneezing. If your child has croup, you should keep them away from school and child care while they are unwell so that they don’t spread the virus that is causing the croup. Regularly washing hands thoroughly can help prevent the spread of viruses.
Key points to remember
- No treatment is necessary for mild croup, or the virus that has caused it.
- Croup usually gets better in three to four days.
- Try to calm your child, as breathing is often more difficult when your child is upset.
- Croup can get worse quickly. If your child is having problems breathing, seek urgent medical assistance.
- In a severe attack of croup, your child needs to be watched closely in a hospital.
For more information
- Kids Health Info fact sheet: Fever in children
- Kids Health Info fact sheet: Cough
- Kids Health Info fact sheet:
Stopping the spread of germs
- Dr Margie: How to recognise the different types of cough in children
- See your GP or local hospital emergency department.

Common questions our doctors are asked
Should I use steam to treat croup?
No. In the past, some doctors recommended exposure to mist or steam therapy, including the use of vaporisers. Research evidence now shows this to be of no benefit and it is no longer recommended.
Developed by The Royal Children's Hospital General Medicine and Respiratory and Sleep Medicine departments, and Centre for Community Child Health. We acknowledge the input of RCH consumers and carers.
Reviewed August 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
90,000 symptoms and treatment. Signs, causes and diagnosis of false croup in a child. False croup is an acute inflammatory process localized in the larynx. Accompanied by swelling of the subglottic region. This condition leads to obstruction. Inflammation is fraught with narrowing of the area under the vocal cords, which is manifested by noisy and labored breathing.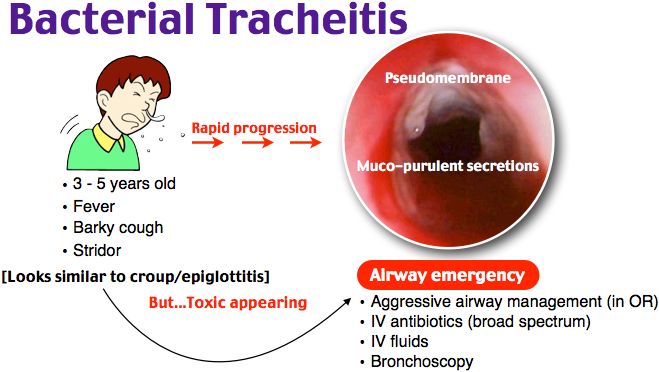 A common cause is a viral infection. It differs from laryngitis by stenosis of the larynx.
A common cause is a viral infection. It differs from laryngitis by stenosis of the larynx.
This disease is most common in children aged 3 months to 5 years. As the child grows older, this condition ceases to be life-threatening, because the trachea becomes larger and breathing problems usually do not occur. Croup can appear at any time of the year, but is more common during the fall and winter months. nine0003
The etiology is usually viral - parainfluenza viruses, especially type I, cause the disease in 75% of cases. Relatively common causes of false croup in children are respiratory syncytial virus, adenovirus, and human coronavirus. The infection is usually spread by breathing contaminated air, or by contact with objects that an infected person has come into contact with.
Influenza is a relatively rare cause that requires longer hospital stays and has an increased risk of a second attack. Rhinovirus, enterovirus, and herpes simplex are sporadic causes of mild croup. nine0003
nine0003
It is also possible to develop against the background of bacterial infection with mycoplasma, streptococcus, chlamydia, Staphylococcus aureus, etc. Diphtheria was the most common form of fatal stenosing laryngitis in another era, but at present this disease is practically absent due to vaccination of the population.
The illness may begin as a cold, with stuffy nose or coryza and fever. As the airways swell, the following symptoms may occur: nine0003
-
barking cough that worsens at night;
-
noisy, rapid breathing;
-
hoarseness or hoarseness of voice;
-
inspiratory type of shortness of breath;
-
excessive anxiety.
Symptoms of false croup in children appear 2-3 days after the onset of ARI (acute respiratory infection). As a rule, there is an increase in the cervical lymph nodes (lymphadenitis). nine0003
In the acute viral form, the onset of symptoms is usually gradual, beginning with rhinorrhea, mild cough, and fever. Progresses after 12-48 hours, typical symptoms appear, dysphonia, dog cough. Stridor (whistling noisy breathing) at first occurs only when excited or crying, but with increasing severity it also manifests itself at rest.
The clinical course is usually fluctuating, with a remission of 2 to 7 days, although the cough may persist for longer. Unlike laryngotracheitis, false croup always occurs at night - the onset and cessation of symptoms are abrupt. Fever is usually absent. Episodes may be repeated over two nights. nine0003
Alveolar gas exchange is normal and there will be hypoxia only when almost complete obstruction occurs. Excessive pallor, cyanosis, and deterioration in general well-being require immediate medical attention.
In case of respiratory failure, which is characteristic of the II and III stages of the disease, the addition of bacterial flora is possible. At the same time, a film of purulent-fibrinous type is formed on the walls of the larynx.
In the absence of timely treatment, the infection spreads lower, which is fraught with the development of tracheobronchitis, bronchitis or pneumonia. Common complications include sinusitis, purulent meningitis, tonsillitis, conjunctivitis, and otitis media. nine0003
As a rule, the diagnosis is clinical, and no additional examinations are required. A rapid assessment of general well-being, vital signs, and mental status should be performed to identify children with severe respiratory distress and respiratory failure. Diagnosis should be carried out in a calm environment.
The severity of illness is determined by the presence of stridor at rest, chest wall retraction, the presence or absence of pallor or cyanosis, and mental stability. nine0003
Additional diagnostic methods:
-
Pulse oximetry is of limited utility because the pulse may be normal even with a significant degree of airway obstruction. It is recommended to control the pulse in severe condition.
-
A radiological evaluation is usually not required. A neck x-ray may show the typical progressive and symmetrical narrowing of the trachea in subglottic stenosis.
It is prescribed for a dubious diagnosis, atypical course, suspicion of the presence of a foreign body. nine0003
Nasopharyngeal aspiration to look for a possible infectious etiology may be useful in hospitalized patients and to control infection. The differential diagnosis should be made primarily with spasmodic laryngitis, epiglottitis, and bacterial tracheitis and with other causes of acute obstruction. Foreign body aspiration may present abruptly but should also be ruled out in children who do not respond to treatment or have a long recovery. nine0003
The presence of chronic symptoms, persistent or recurring, and the absence of catarrhal signs or fever should raise the suspicion of congenital anomalies of the respiratory tract (laryngomalacia, vocal cord paralysis, subglottic stenosis, subglottic hemangioma, etc.).
A retropharyngeal or periamillary abscess may be mistaken for a false croup. In this case, a CT scan (computed tomography) is prescribed, which allows you to determine the exact cause. Dysphagia and excessive salivation may indicate epiglottitis, a foreign body in the airway or esophagus. Allergic angioedema can also mimic the disease, although it usually occurs in conjunction with other anaphylactic manifestations. nine0003
If a respiratory pattern develops, parents should consult a pediatrician or otolaryngologist as soon as possible. Corticoids are the most effective drugs. A single dose of oral dexamethasone is effective in all cases, regardless of the severity of the disease. Doctors are faced with the task of reassuring the child and parents. To improve the patient's well-being, painkillers and antihistamines are prescribed.
Inhalation with a nebulizer and fresh air help to reduce the dryness of the mucous membranes, which improves well-being. If there is respiratory distress and O2 saturation is less than 94%, then there is a need for additional oxygen therapy.
Treatment includes the use of the following medications:
-
Corticoids.
They reduce swelling and have an anti-inflammatory effect, as well as relieve the intensity of symptoms. There are no side effects with short-term use. Corticosteroids eliminate the need for adrenaline and intubation.
- nine0002 Adrenalin. Also proven to be effective, especially in moderate to severe cases. Reduces the need for intubation. The effect comes in 10 minutes.
Children with mild croup can be treated at home. The patient should be in a comfortable position, drink a lot and stay in bed, because fatigue and crying aggravate the disease. Home-use humidifiers (such as cold mist vaporizers) reduce upper airway dryness and make breathing easier. Recovery occurs, as a rule, for 3-4 days. nine0003
First aid for false croup in children includes taking measures that are aimed at opening the airways. To do this, you need to provide an influx of fresh air or take the child outside. Steam inhalation gives a good effect.
Children with increasing or continuing respiratory distress, tachycardia, fatigue, dehydration, or bluish discoloration of the skin are hospitalized. Oxygen treatment is given. If the patient feels better, the patient can be discharged home. nine0003
The use of antibiotics is limited to rare cases where the child also develops a bacterial infection. The viral nature of the disease requires the appointment of antiviral drugs.
There are no drugs that prevent stenosis of the larynx. It is useless to give the child immunomodulating agents. Even those children who are distinguished by good health are not immune from false croup.
To prevent the disease, it is recommended: nine0003
1. Ventilate the apartment more often.
2. Provide daily wet cleaning.
3. Dress the child according to the season.
4. Take a walk in the fresh air every day.
5. Limit allergenic foods for colds.
At the first signs of illness, contact a pediatrician or ENT medical center. We employ qualified professionals with extensive practical experience. Self-medication is unacceptable, because there is a risk to health and life. nine0003
We offer to use the service of calling a doctor at home. The specialist will arrive at the address specified in the application, diagnose, provide first aid and tell you how to treat the disease. If necessary, the patient will be invited to the clinic. You can also consult with a specialist online.
We promptly respond to additions and price changes in the price list. In order to avoid misunderstandings, it is recommended to clarify the full list of services and their cost at the clinic's reception desk or by calling 8-495-104-35-35.
The price list posted on the site is not an offer. Medical services are provided on the basis of a concluded contract.
Treatment of false croup in a child. Withdrawal of an attack. Fantasy Clinic in Moscow
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.