Tested negative for chlamydia and gonorrhea but still have symptoms
If I Test Negative For An STI Could I Still Have One?
Reviewed by our clinical team
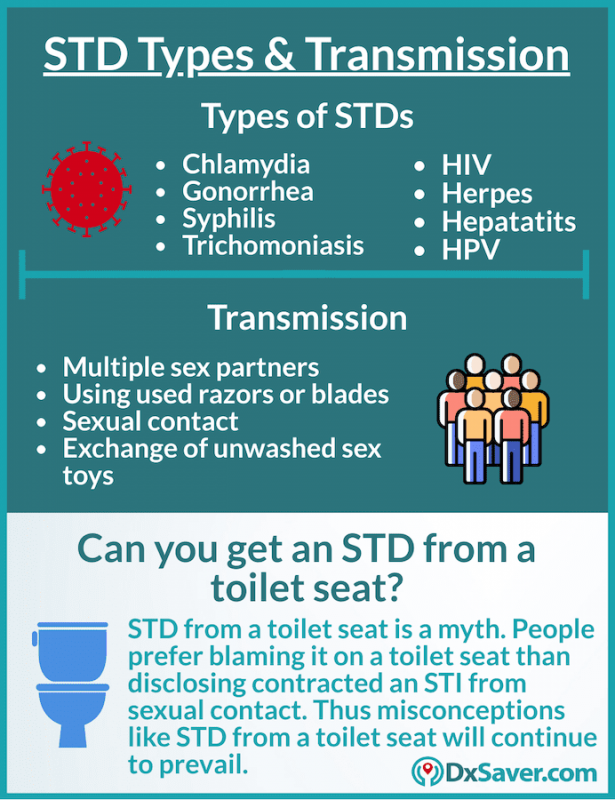
If you’re sexually active, there’s always a bit of risk associated with having sex with a new or casual partner. This is the case even if you use condoms – although it’s true that condoms do reduce your risk of STIs significantly.
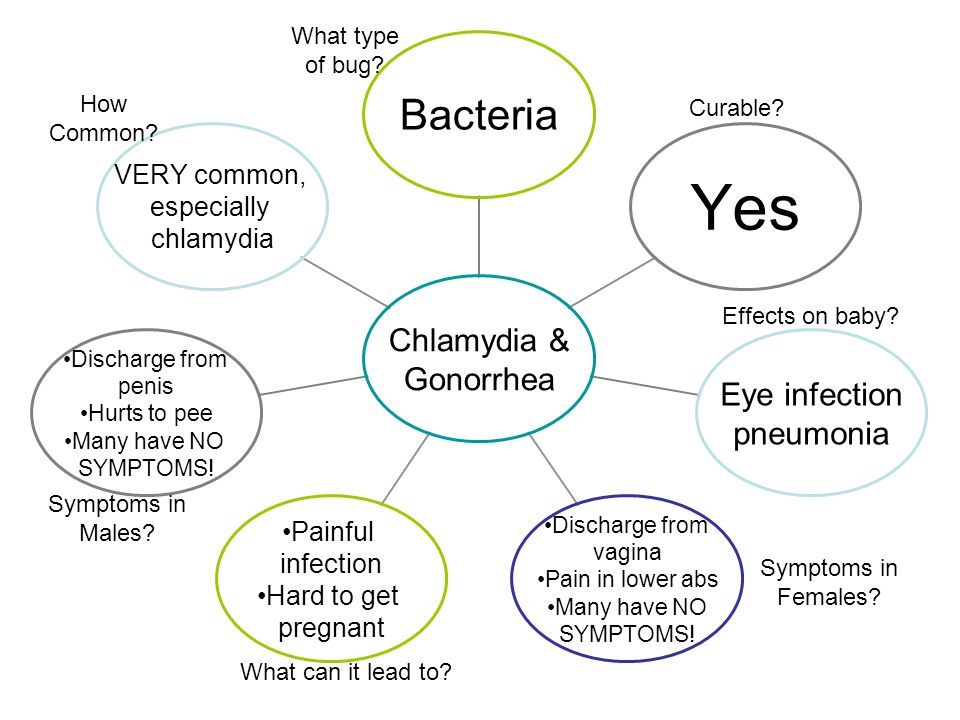
Many STIs – including the most common one, chlamydia – don’t always cause symptoms in their early stages. This means that you might not know you’re infected until you get tested.
However, STI testing is complicated by the fact that different infections have different “window periods”. Certain STIs will show up on a test within a couple of weeks of infection, while others will take much longer. This means if you test too early for certain STIs, the infection might not show up.
In other words, it’s possible to have an STI even if you tested negative the first time.
How soon after unprotected sex can I test for an STI?
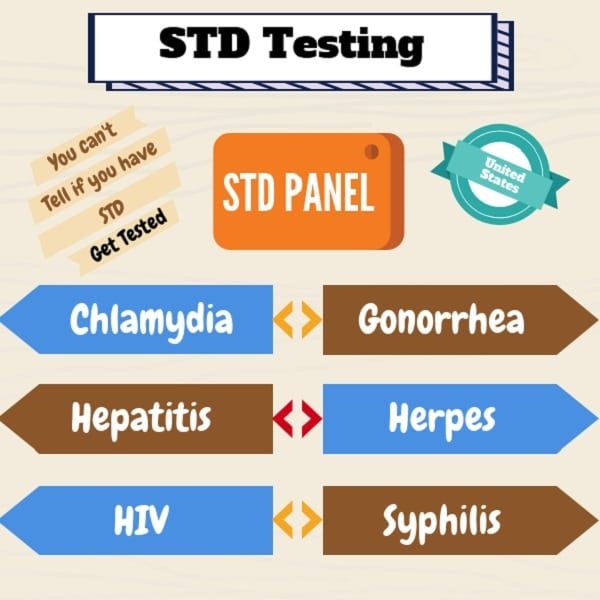
Different STIs have different incubation periods, and therefore different testing windows. Below you’ll find the testing window periods for some of the most common STIs in the UK.
14 days after exposure
- Chlamydia
- Gonorrhoea
45 to 90 days after exposure
- HIV – certain types (including Online Doctor’s HIV tests) can detect the virus sooner than others
12 weeks after exposure
- Syphilis
Two of the more common STIs in the UK – genital warts and genital herpes – can only be diagnosed if you’re having symptoms. If you develop any lumps, growths, sores or blisters around your genitals, you should go to the sexual health clinic to have a physical examination.
What happens if I get a test too early?
If you get a test too early, it may not pick up the infection, which means you run the risk of getting a misleading result. To avoid this, you shouldn’t use an STI test without speaking to a doctor or nurse first, as they’ll be able to advise you on the best time to get tested.
To avoid this, you shouldn’t use an STI test without speaking to a doctor or nurse first, as they’ll be able to advise you on the best time to get tested.
There are some circumstances where you might be advised to take more than one test. If you think you’ve been exposed to HIV, for instance, you might be told to get a test as soon as possible, followed by another test to confirm the first result a few weeks or months later.
Should I wait to get tested if I’m having symptoms?
No, if you’re having symptoms you should go to a sexual health or GUM clinic. A doctor or nurse can give you a test, assess your symptoms and – if necessary – give you a physical examination. If they think there’s a strong chance you have an STI like chlamydia, they might prescribe treatment before you get your test results back.
Is it safe to use home STI test kits?
Yes, it’s safe to use home STI tests, as long as they come from a trusted provider e.g. the NHS or a registered high street pharmacy like LloydsPharmacy.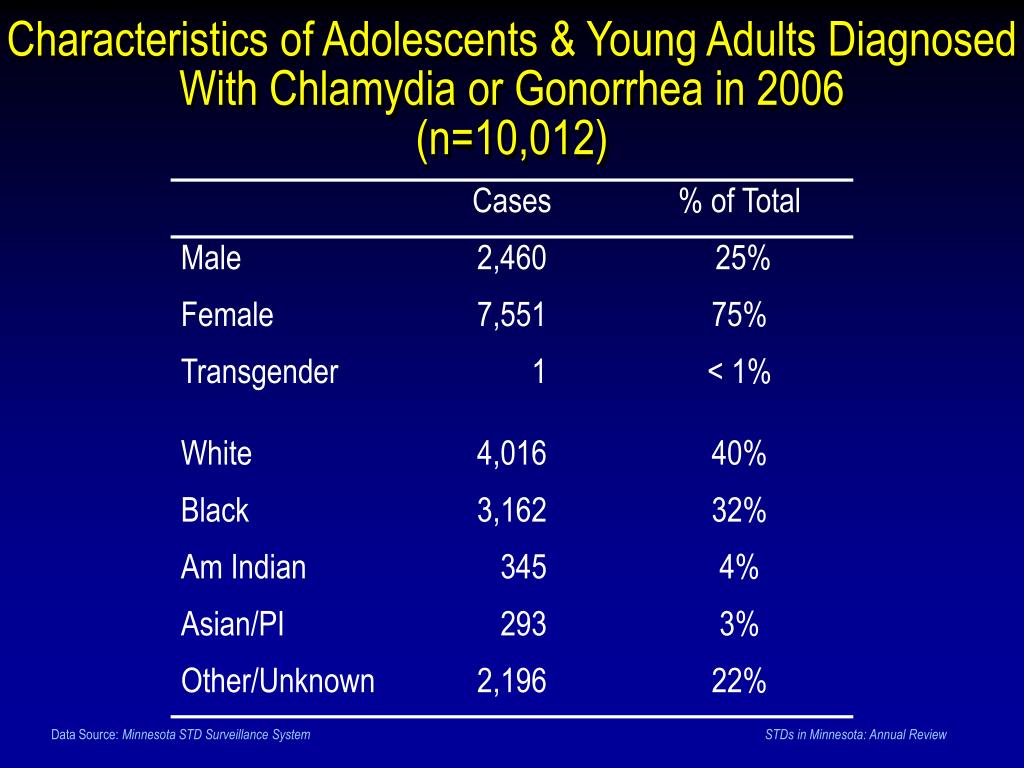
At Online Doctor we use a secure form to ask you questions about your sexual history, the last time you had sex, and whether you’re having any symptoms. If clinicians don't think it would be a good idea for you to use a home test kit, they’ll let you know and advise you about what to do instead.
Can STI test results be wrong?
These days, STI tests are very reliable, which means you’re unlikely to get a false result provided you’ve tested for the correct STIs at the correct times.
One notable exception would be a test that doesn’t collect a sample from the correct area of the body. Although most STIs affect the genitals, some – including gonorrhoea – can affect the rectum, the throat, and even the eyes. If you take a gonorrhoea test that only involves a sample from your genitals, it may miss the infection elsewhere in your body.
What should I do if I think I’ve been exposed to HIV?
Becoming infected with HIV is life-changing, but with early diagnosis and treatment you can live a relatively normal and healthy life.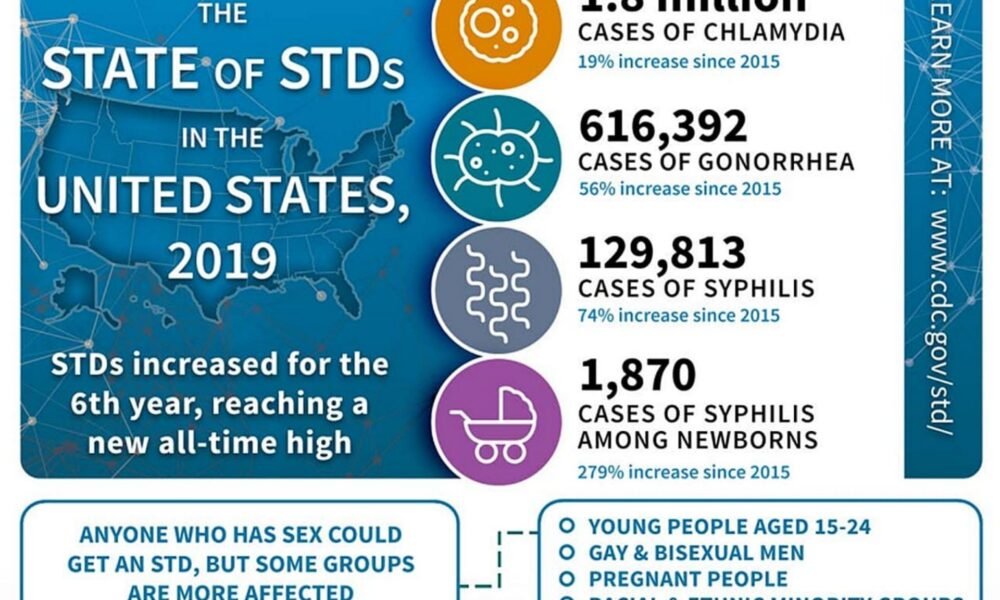 For this reason, if you think you’ve been exposed to HIV, you should seek medical advice as soon as possible.
For this reason, if you think you’ve been exposed to HIV, you should seek medical advice as soon as possible.
You may even be able to avoid infection altogether if you seek emergency treatment after unprotected sex. Post-exposure prophylaxis (PEP) is a medication that can be taken in the weeks following unprotected sex to prevent infection with HIV.
References
https://www.letstalkaboutit.nhs.uk/worried-about-stis/testing-treatment-of-stis/
https://www.nhs.uk/conditions/genital-warts/
https://www.nhs.uk/conditions/genital-herpes/
https://www.nhs.uk/conditions/hiv-and-aids/diagnosis/
https://www.nhs.uk/conditions/chlamydia/treatment/
https://www.nhs.uk/conditions/gonorrhoea/diagnosis/
STD Test Is Negative But Still Worried?
One of the most important parts of being a responsible, healthy, and sexually active adult is getting regular STD tests and knowing your status. But what should you do if an STD test is negative, but you’re still worried? The best thing to do is get tested to know whether you contracted an STD or not.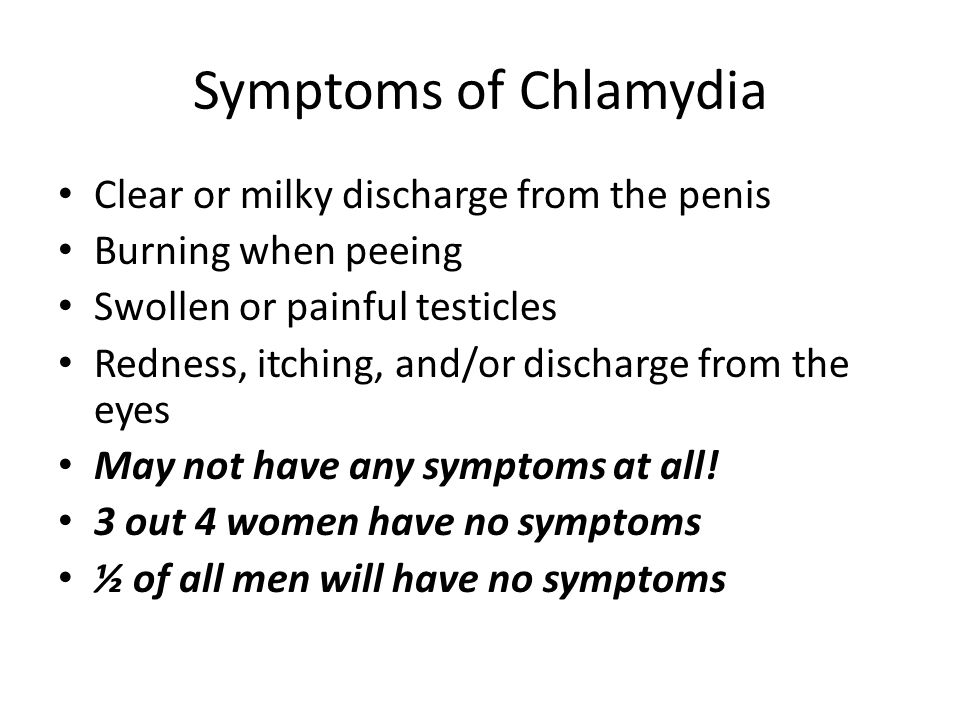
You can get a 10-panel STD test or same-day STD testing from Rapid STD Testing to check your status and get accurate, fast results. All you have to do is order your test panel and then head to one of the convenient clinic locations.
Understanding Negative STD Test ResultsIf you took an STD test that came back negative, it doesn’t necessarily mean that you’re in the clear. You could get a false negative result, which would mean that you have the disease even though the test is negative.
Each STD has a window period, which is the time it takes for the disease to appear on a test. There are also differences between STDs, like oral STDs or genital STDs, and each requires a different test. It’s for these reasons that you should get regular STD tests. If the first test you take is negative, come back and take another test to recheck your status and get the most accurate results possible.
False negatives can be dangerous because the longer sexually transmitted infections go untreated within your body, the more damage they can cause.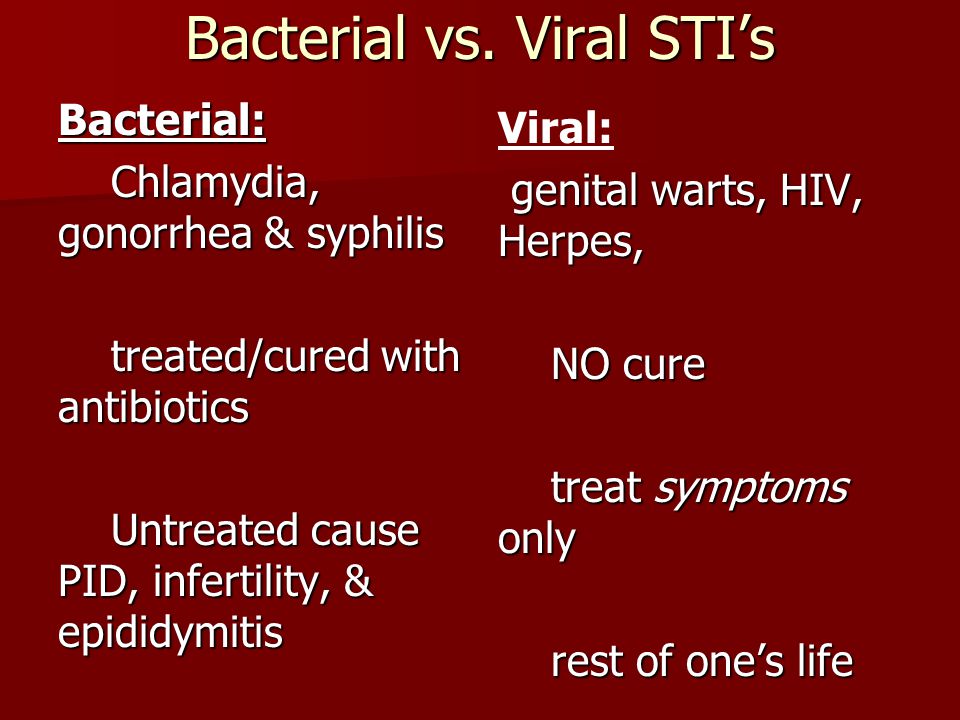 Not to mention, there’s a high risk of passing the STD to another partner unknowingly.
Not to mention, there’s a high risk of passing the STD to another partner unknowingly.
To check your status, you can order a rapid STD test for same-day testing and get your confidential results within one to three days.
What Do False Negative Test Results for STDs Mean?STD testing is more accessible and accurate than it’s ever been. However, there’s always the chance of getting a false negative or false positive result. What makes one test better than another? The answer is specificity and sensitivity. Specificity refers to tests that measure if people don’t have the disease, whereas sensitivity measures which people do have the disease.
A false negative STD test result occurs when the test says that you don’t have an STD, but you actually do have it. A false positive STD test result happens when the results are positive, but you don’t have the disease. If you get a false negative, you most likely took the test too soon for accurate results.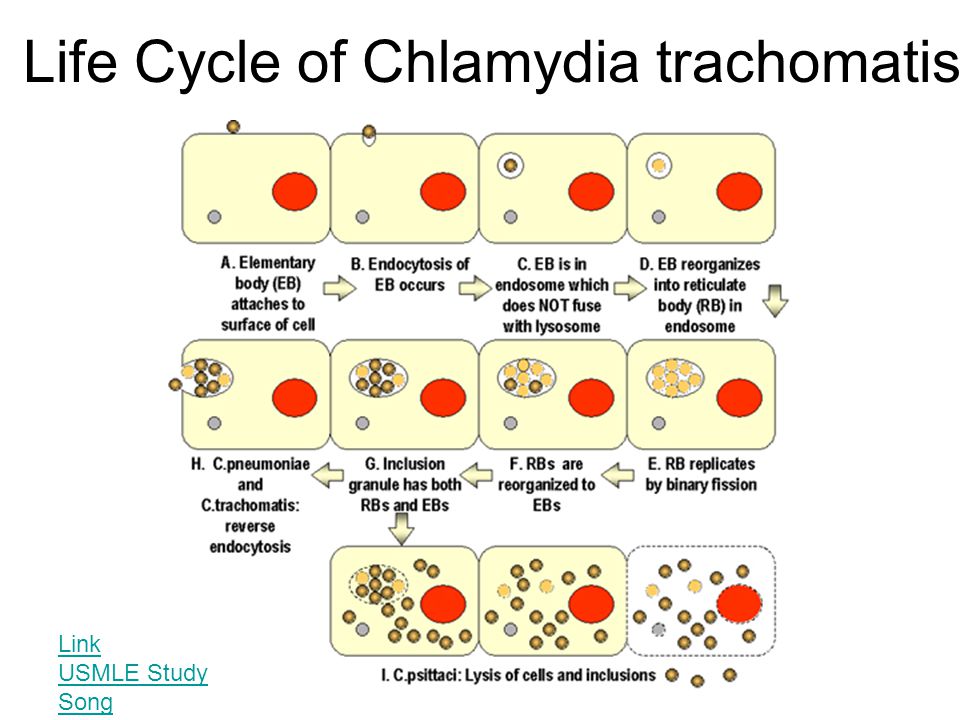
You can see why the possibility of getting false negatives makes regular STD testing so important. Luckily, you can find STD testing near you at one of the 2,500 Rapid STD Testing locations nationwide, which means you can check your status and get treatment as quickly as possible if you need it.
STDs That Commonly Produce False Negative Results
Some STDs are more likely than others to give you a false negative result. Although the chances of getting an incorrect result are low if you take the proper test and the lab tests your specimen correctly, it is possible to get false results.
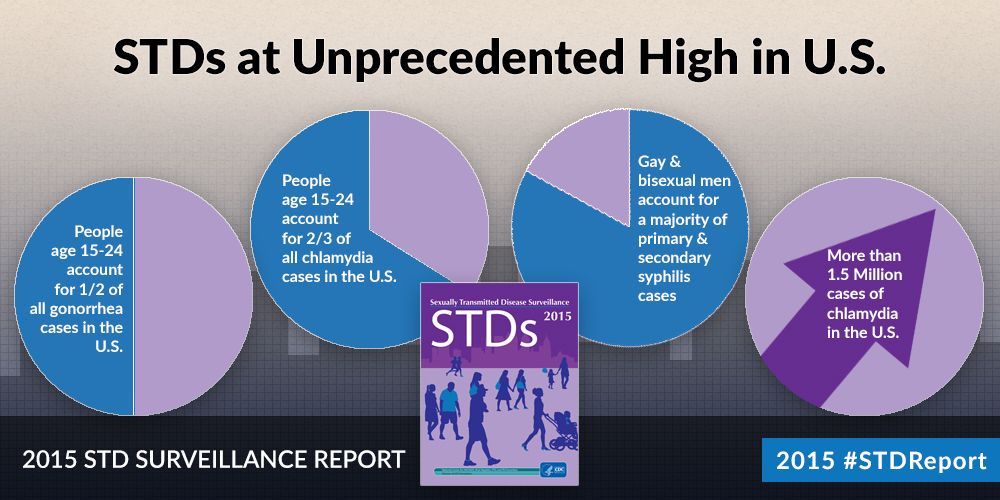
Chlamydia and gonorrhea are the two most common STDs that can cause a false negative test result. If you’re a carrier of either disease and still get a negative result, you could unknowingly transmit the disease to other people. That possibility is a risk that nobody should take, which is why getting regular STD testing is so vital to your sexual health.
Why are gonorrhea and chlamydia more likely to produce a false result? Usually, it’s because you took the test too soon.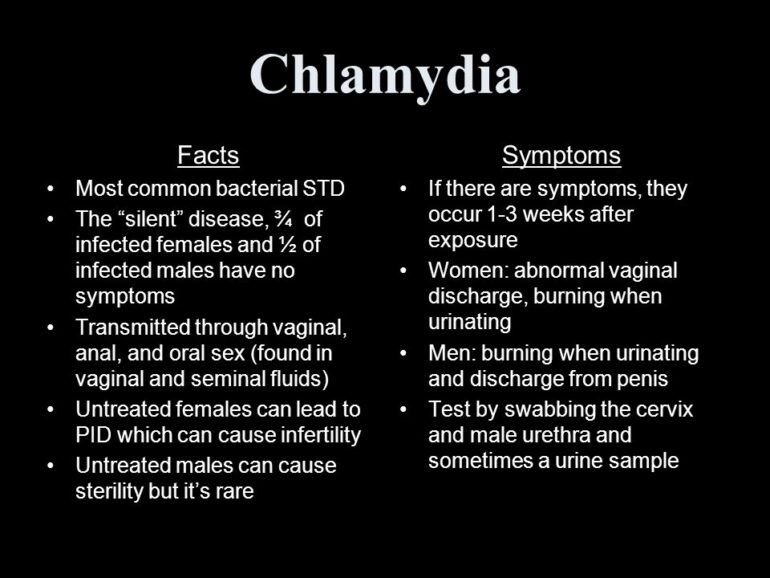 For example, gonorrhea usually takes about seven days before it shows up on a test. You could get a false negative result if you take the test before the seven days are up.
For example, gonorrhea usually takes about seven days before it shows up on a test. You could get a false negative result if you take the test before the seven days are up.
Chlamydia takes between two and six weeks to register on a test. HIV is another STD that can cause false negatives due to the complicated nature of its testing window.
Causes of Faulty Results
If you get false results on an STD test, there could be a variety of reasons why. It depends on a few different factors:
- The specificity and sensitivity of the test
- The type of test: urine, swab, or blood test
- If the disease is common or rare
- Improper testing procedures
- How quickly you take the test
However, there are even more factors that can affect your results. You must take the right STD test to get the right results. For example, if you have an STD that causes itching, like herpes, but you get an HIV test, you’re not going to get accurate results.
For STD tests that require a urine sample, it’s important to wait as long as possible after urinating to take the test. If you have urinated within the last two hours before you give the specimen, it could skew the test results.
Effects of STD Window Period on Test ResultsIf you have a negative STD test, but you’re still worried, the cause of your negative result is most likely due to the window period. The STD window period is the amount of time it takes for an STD to register on a test. What does this mean, and how can it affect your STD test results?
If you’re exposed to an STD and end up catching it, you won’t test positive right away. That can have some significant side effects on your sexual health. For example, if you get tested within the window period and receive a false negative, you could transmit the disease to sexual partners.
Another dangerous effect of getting tested too soon during the window period is delaying treatment. If you don’t receive treatment for an STD, it can cause adverse effects on your health and well-being.
Here are the window periods for the most common STDs:
- HIV: Between 10 and 90 days
- Chlamydia: one to two weeks
- Syphilis: one to three weeks
- Hepatitis: Between two and six weeks
- Gonorrhea: five to 14 days
- HPV: three weeks to about three months
- Trichomoniasis: one week to 30 days
- Herpes: one to four months
As you can see, it’s essential to get regular STD tests since the window period can have such significant effects on your results.
Coping with Anxiety: My STD Test Came Back Negative, But I’m Still WorriedYou may feel nervous or anxious when you have to undergo STD testing. That’s why the clinical staff at Rapid STD Testing takes the time to discuss mental health as it relates to sexual health, STD testing, and negative results.
First, if you’re feeling down, depressed, anxious, lonely, or upset, there is help. You can call the National Alliance on Mental Illness (NAMI) HelpLine Monday through Friday from 10 am to 8 pm EST at 1-800-950-NAMI (6264).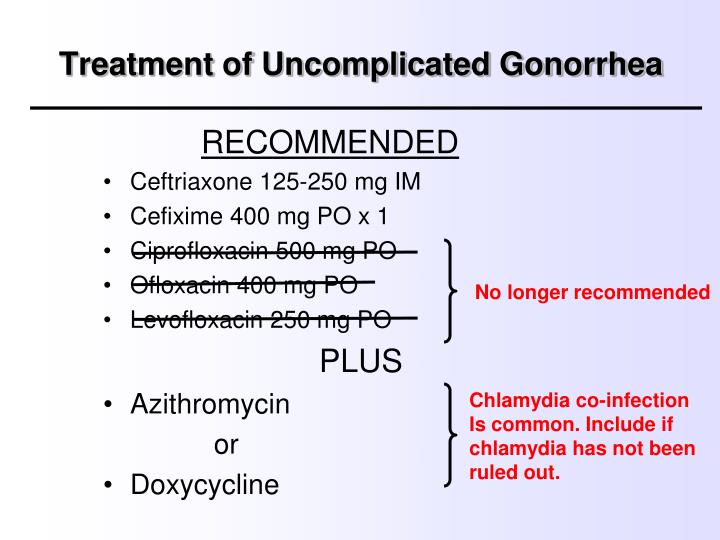 You can also email [email protected].
You can also email [email protected].
The stigma surrounding mental health and sexual health makes these topics particularly challenging to discuss and can even cause feelings of anxiety or depression. If you feel those negative emotions, try to avoid looking at information from untrustworthy sources. Instead, schedule an appointment to speak with a doctor about your concerns.
Tips for Coping with Anxiety About Your Test Results
You should also remember that it’s not only inevitable but healthy to have different feelings and emotions about sexual health, STD testing, and your test results. When this happens, there are some techniques you can use to help you calm down and stay in the moment.
The first method you can use combines two techniques: deep breathing and positive affirmations. Use a simple one-two-three counting process and deep breaths while you say positive things out loud to yourself, like: “I may feel worried about my health, but I’ll get through this because I’m strong.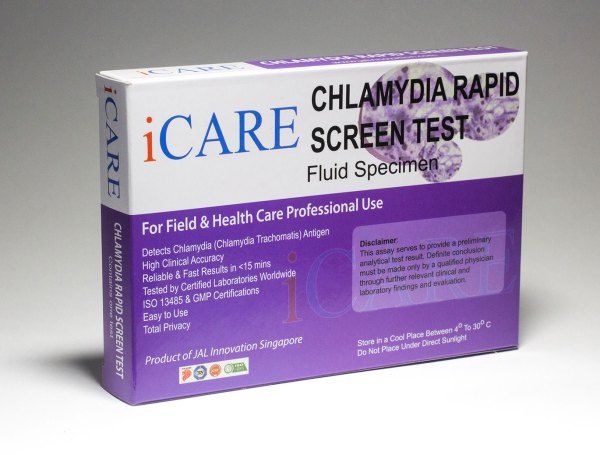 ”
”
You can also try visualizing yourself eliminating any unhealthy thoughts, feelings, or emotions. Let the negativity go, and then continue with deep breathing and positive affirmations.
Other Common Questions About STDs and Negative Results
Can you test negative for STDs like Chlamydia and still have them?
Yes, you can test negative for STDs and still have them. Chlamydia and gonorrhea are the two most common STDs that can cause false negatives, especially if you get tested too quickly.
All my STD tests were negative, but I still have symptoms. What should I do?
If your STD test was negative, but you’re still worried or experiencing symptoms, you need to speak to a doctor, who may recommend that you take another test. You could have a false negative, so the best way to know whether you contracted an STD is to get tested again.
Take Control of Your Sexual Health TodayOrder a test panel online from Rapid STD Testing today and take control of your sexual health and well-being. Visit one of our convenient locations for same-day STD testing and fast, confidential, and accurate results.
Visit one of our convenient locations for same-day STD testing and fast, confidential, and accurate results.
Chlamydia - KVD №2
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
Chlamydia also causes penile discharge in infected men.
Chlamydia transmission routes
Chlamydia can be transmitted through:
- vaginal or anal contact with an infected partner;
- less common with oral sex;
- use of sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.
Absolutely all sexually active people can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed. About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24.
You cannot get chlamydia through kisses, hugs, dishes, baths, towels.
Manifestations of chlamydia
Chlamydia is very secretive. About 75% of infected women and 50% of infected men are asymptomatic. If manifestations of the disease develop, then this occurs approximately 1 to 3 weeks after infection.
In women, chlamydia first affects the cervix and urethra (urinary canal).
Manifestations:
- unusual vaginal discharge;
- pain or discomfort when urinating;
If the infection penetrates to the appendages, manifestations are possible:
- pain in the lower abdomen;
- pain in the lumbar region;
- nausea;
- slight increase in temperature;
- pain during intercourse or bleeding after it;
- bleeding between periods.
Symptoms in men:
- clear or cloudy discharge from the penis;
- pain or discomfort when urinating;
- there may be burning and itching in the area of the outlet of the urethra;
- rarely pain and/or swelling of the testicles.
Men or women who have anal sex with an infected partner can infect the rectum, resulting in inflammation, pain, discharge, or bleeding from the rectum.
Chlamydia can cause sore throat (pharyngitis) in men and women who have oral contact with an infected partner.
What complications can develop if chlamydia is not treated?
If the disease is not treated, serious short-term and persistent complications develop. Like the disease itself, complications often occur insidiously.
In women with untreated chlamydia, infection can spread from the urethra to the fallopian tubes (the tubes that carry the egg from the ovaries to the uterus) - this causes (in 40% of cases) the development of pelvic inflammatory disease (PID). PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
Women with chlamydia are more susceptible to HIV infection, the risk increases by almost 5 times.
To prevent serious consequences of chlamydia, annual chlamydia screening is required for all sexually active women 25 years of age and younger. An annual examination is necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Complications of chlamydia are rare in men. The infection sometimes extends to the epididymis and causes pain, fever, and, rarely, male infertility (sterility).
Rarely, chlamydial infection can cause inflammation of the joints in combination with skin lesions, inflammation of the eyes and urinary tract - this is the so-called Reiter's syndrome.
The effect of chlamydia on a pregnant woman and her child
Chlamydia in pregnant women increases the risk of miscarriage, premature detachment of the placenta. Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Diagnosis of chlamydia
Diagnosis includes observation of the patient's clinical symptoms, testing for chlamydia smears from the cervix, scraping from the urinary canal, the first morning urine. Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
In addition, a blood test by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia is carried out, this auxiliary test often helps to establish an accurate diagnosis.
Treatment of chlamydia
Treatment of chlamydia is with oral antibiotics. To prevent re-infection, all sexual partners must be found, examined and treated. Patients with chlamydia should refrain from unprotected sex during treatment, otherwise it is possible to re-infect the sexual partner. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since a strong immunity to this microorganism does not develop. Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Prevention of chlamydia
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Annual chlamydia screening required for all sexually active women 25 years of age and younger. An annual examination is also necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Any manifestations, such as pain or discomfort when urinating, unusual rash, discharge are a signal to stop sexual intercourse and immediately examine in a specialized clinic - KVD. If the patient is found to have chlamydia (or any other STI), he must inform his sexual partners so that they also undergo a full examination and appropriate treatment.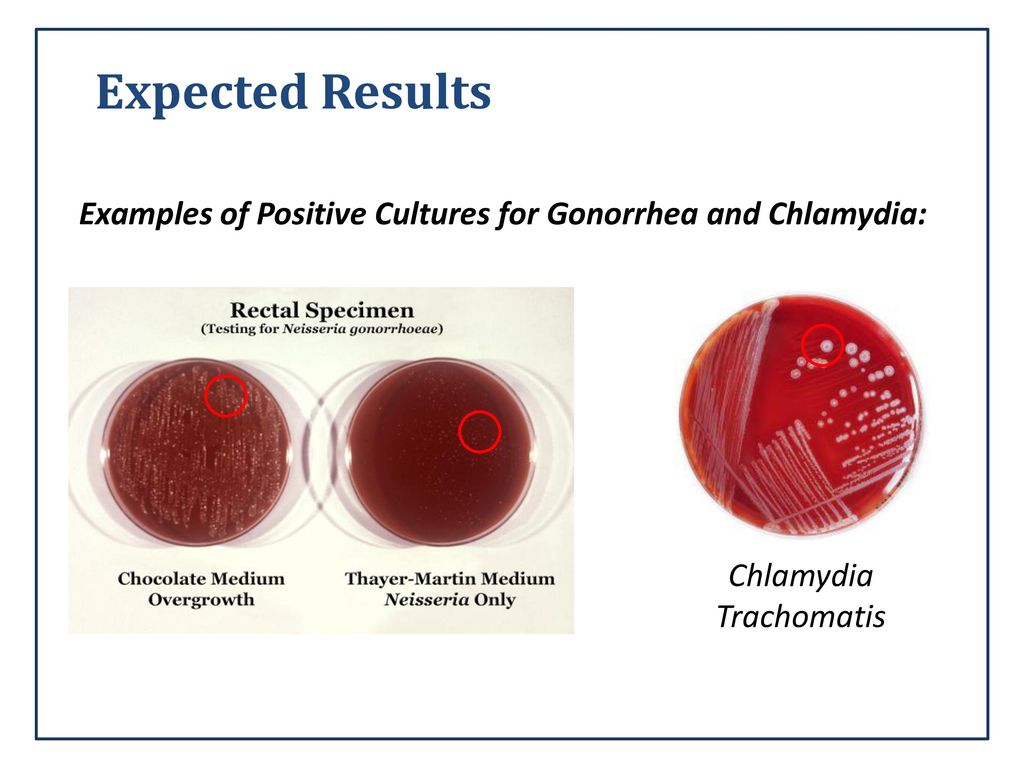 This will reduce the risk of developing serious complications and prevent the possibility of re-infection.
This will reduce the risk of developing serious complications and prevent the possibility of re-infection.
Patients with chlamydia should refrain from unprotected sex during treatment, otherwise the sexual partner may be re-infected.
symptoms and treatment ⮞ Signs and diagnosis of chronic chlamydia
It is difficult for a simple layman, which in most cases is an average patient, to understand what chlamydia is and why it is so dangerous if nothing bothers a person infected with chlamydia. The patient faces the problem face to face, as a rule, when everything is much more serious than just an infection. But even then, few people delve into medical issues, frightened by their complexity, relying on the doctor and again and again being disappointed in the treatment. We will try to explain why chlamydia therapy is such a difficult and sometimes tedious task, why sometimes a doctor fails, and how to achieve recovery in the end.
Important!
The information in this article should not be used for self-diagnosis or self-treatment.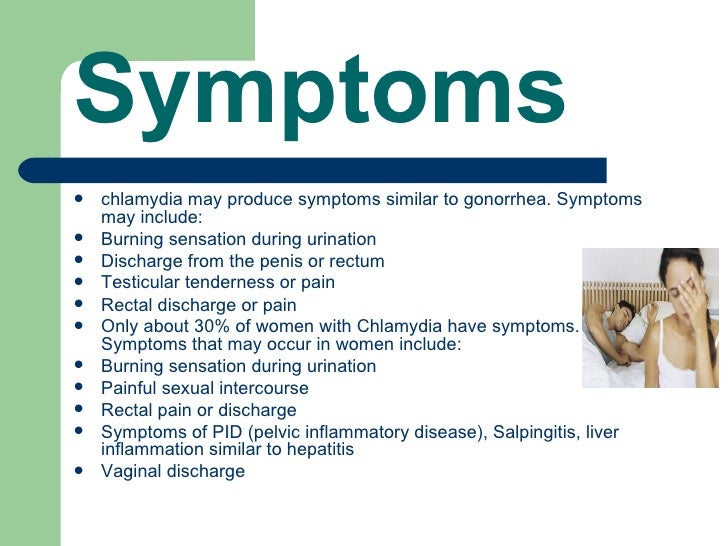 For the correct diagnosis and treatment, you should always consult a doctor.
For the correct diagnosis and treatment, you should always consult a doctor.
Article content
- Prices for services
- What is chlamydia?
- What are the manifestations of chlamydia?
- Ways of infection with chlamydia
- Statistics
- Complications
- Diagnostics
- Treatment
- What if chlamydia is not treated?
- Prevention
Prices for services
Primary appointment with a urologist FOR MEN + ultrasound of the prostate gland (evaluation of complaints, history taking, if necessary, rectal digital examination, ultrasound of the prostate gland in men)
Initial appointment - an appointment with a doctor of a specific specialty for the first time.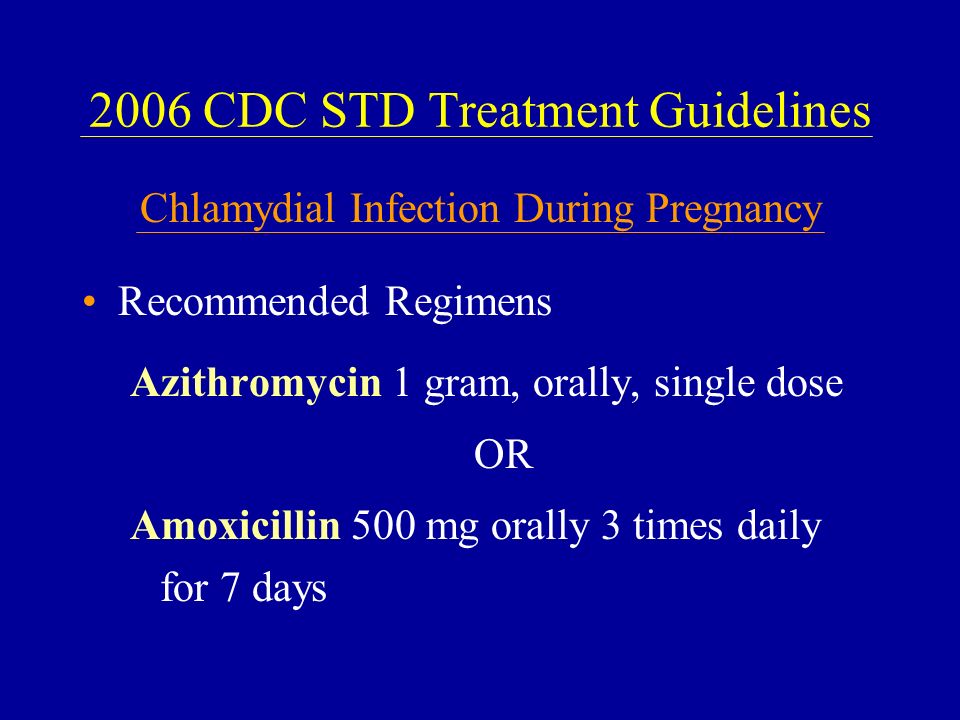 Includes a conversation with the patient, initial examination, history taking, if necessary, rectal digital examination, ultrasound of the prostate gland. The price is valid from 01.02.2022
Includes a conversation with the patient, initial examination, history taking, if necessary, rectal digital examination, ultrasound of the prostate gland. The price is valid from 01.02.2022
Make an appointment
1100 ₽
Initial appointment Department of Urology Rylchikov I.V. + Ultrasound (includes a conversation with the patient, initial examination, history taking, if necessary, rectal digital examination, ultrasound of the prostate gland)
Primary appointment - an appointment with a doctor of a particular specialty for the first time.
Make an appointment
1300 ₽
Repeated appointment with a urologist
Make an appointment
700 ₽
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis, a microorganism that occupies an intermediate position between viruses and bacteria and parasitizes in the epithelial cells of the patient, destroying them.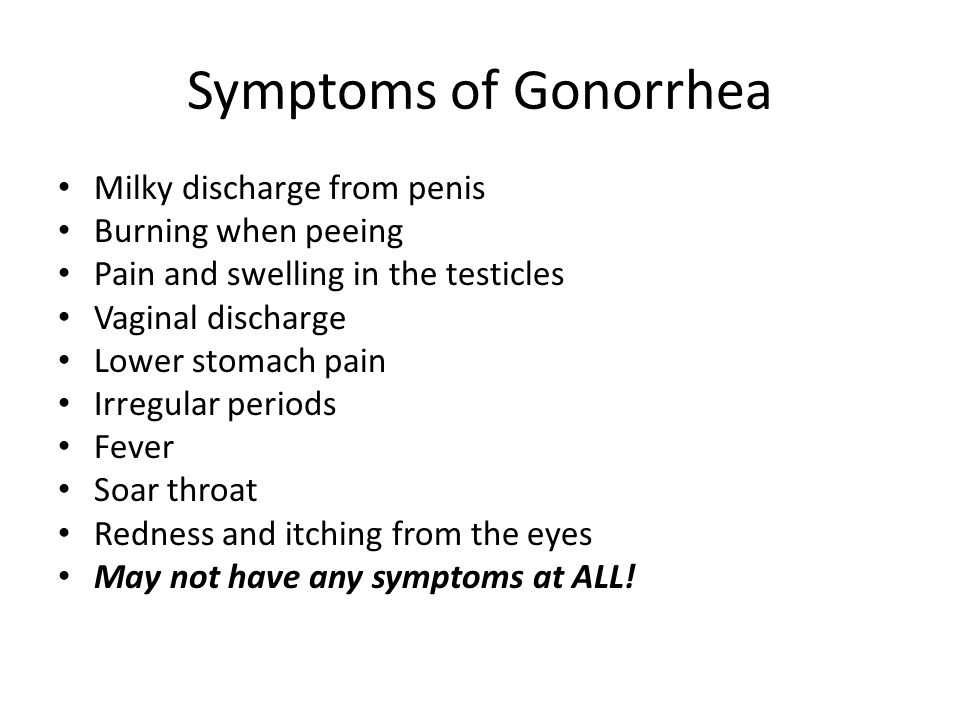 Symptoms of chlamydia are usually mild or absent. That is why many cases of the disease go unnoticed. However, serious complications develop.
Symptoms of chlamydia are usually mild or absent. That is why many cases of the disease go unnoticed. However, serious complications develop.
What are the manifestations of chlamydia?
Chlamydia is very secretive. 50% of infected men have no manifestations of the disease. If manifestations of the disease develop, then this occurs approximately 1-3 weeks after infection.
Men in the acute period of chlamydia may experience clear or cloudy discharge from the penis, pain or discomfort when urinating, burning and itching in the area of the urethral outlet, rarely pain and / or swelling of the testicles. Obvious manifestations of chlamydia, if they occur, disappear along with the acute period and pass into a hidden internal process.
Chlamydia transmission routes:
- vaginal, anal, oral contact with an infected partner;
- using sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.
Any sexually active person can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed.
What are the complications of chlamydia?
Symptoms of chlamydia in men usually correspond to urethritis:
- purulent discharge;
- pain, cramps;
- slight redness and slight swelling of the urethra;
- inflammation of the urethra (urethritis);
- inflammation of the prostate gland (prostatitis);
- inflammation of the epididymis (epididymitis);
- frequent urination, itching in the urethra, sometimes pain in the perineum.
Complications in men:
- urethritis with its intolerable urge to urinate, itching, pain in the urethra and purulent discharge;
- dangerous for a man at any age prostatitis;
- inflammation of the testicles (vesiculitis), in which a man experiences a feeling of fullness in the perineum, pain radiating to the sacral and inguinal regions and the testicle;
- epididymitis - inflammation of the vas deferens and cord, when the testicle increases in size, and the skin of the scrotum turns red and swells.
How to diagnose chlamydia?
It is very important in the treatment of chlamydia to take into account the presence of other sexually transmitted diseases. One of the features of chlamydia is its frequent combination with other sexually transmitted infections. In most cases, there is a combination of chlamydia and mycoplasmosis, chlamydia and trichomoniasis, chlamydia and gardnerellosis. Quite often, three, four or more sexually transmitted microorganisms are combined. The presence of such microbial unions enhances the negative effect on the body of each of the microorganisms and allows them to better resist the body's defenses and ongoing treatment. Particular attention is paid to mixed trichomonas-chlamydial infection.
Diagnosis includes the observation of clinical symptoms in a patient, the study of chlamydia smears from the cervix, scrapings from the urinary canal, the first morning portion of urine. Most often, the study is carried out by PCR (polymerase chain reaction). Additionally, a blood test is performed by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia, this auxiliary study often helps to establish an accurate diagnosis.
Important!
The information in this article should not be used for self-diagnosis or self-treatment. For the correct diagnosis and treatment, you should always consult a doctor.
How to cure chlamydia?
Treatment of a clamidiosis has to be COMPLEX. This means not only taking medications, but also local effects on infected organs. If the treatment of chlamydia is started immediately, in its acute form, the treatment is usually not complicated and ends, as a rule, with a complete cure. If chlamydia has passed into a chronic form, or constantly recurs, the treatment of these forms is quite complicated: chlamydia has time to develop "immunity" to standard methods of treatment, and additional time and material costs are required to develop a successful method of treating these forms of chlamydia.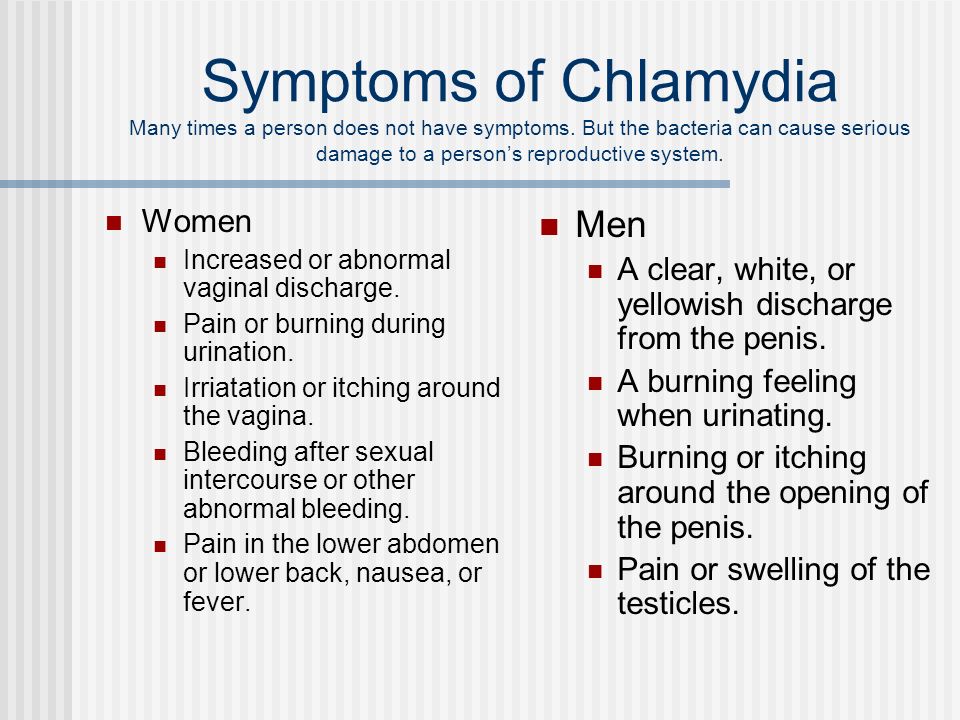
Chlamydia antibiotics
Since chlamydia are parasites that live inside cells, their treatment requires the use of antibiotics that can penetrate and accumulate in the affected cells. In each case of chlamydia, ONLY an INDIVIDUAL treatment regimen should be drawn up, which will take into account the nature of chlamydia, the sensitivity of chlamydia to antibiotics (determined based on the seeding rate for sensitivity to antibiotics), the presence of concomitant infections, the severity and duration of chlamydia, its localization - which organs were affected by the infection.
Taking into account all these factors, the doctor calculates individual doses of antibiotics and the duration of the treatment cycle for you - you will need a course of several cycles of chlamydia development in order to talk about the effectiveness of the treatment.
It is especially worth noting that if, along with chlamydia, other sexual infections are found - mycoplasmas, ureaplasmas, cytomegalovirus, gonococci, etc.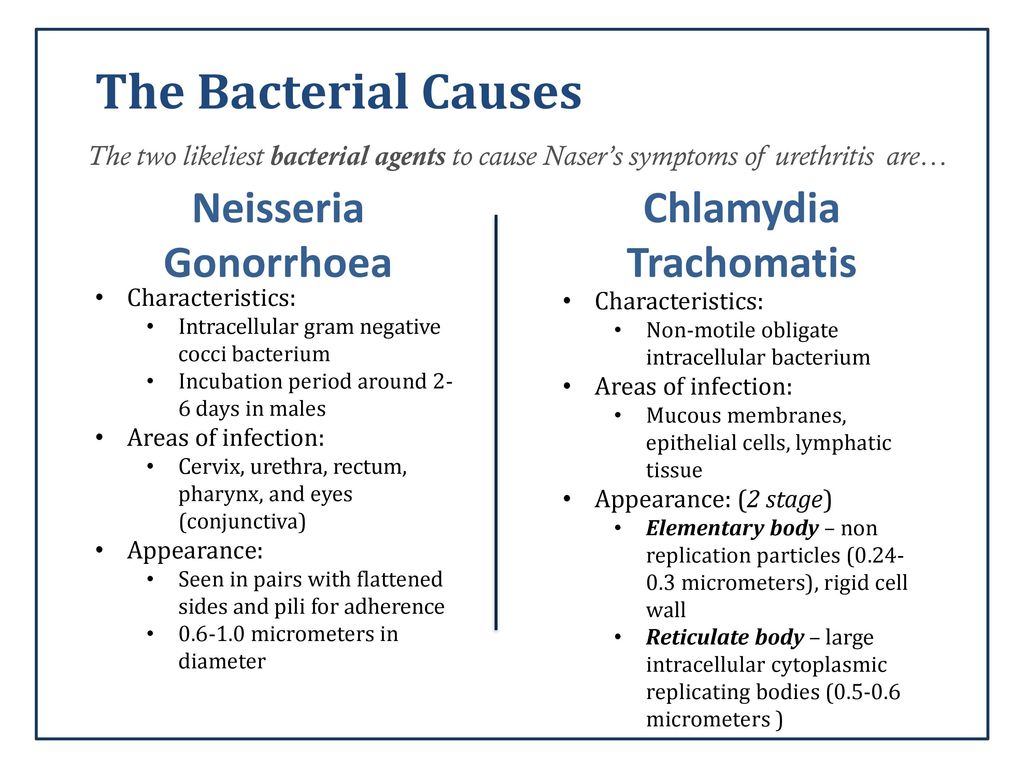 , then treatment also becomes more complicated. The doctor will have to develop a scheme, taking into account the sensitivity of each of the infections found to the prescribed drugs. In the course of treatment, drugs are also prescribed that prevent the reproduction of fungal infections in the body that has been exposed to antibiotics.
, then treatment also becomes more complicated. The doctor will have to develop a scheme, taking into account the sensitivity of each of the infections found to the prescribed drugs. In the course of treatment, drugs are also prescribed that prevent the reproduction of fungal infections in the body that has been exposed to antibiotics.
Immunomodulating therapy
Very often, in persons with chlamydia, there are various violations of the immune defense of the body. They are also determined by laboratory tests. On the basis of an immunological examination, the attending physician can prescribe immunity-enhancing drugs, immunoactivators, etc., as part of the treatment of chlamydia. But immune drugs are not always prescribed - in each specific case individually. Therefore, it is very important to choose a good doctor for the treatment of chlamydia, in order to trust him and not to correct the scheme carefully developed by him during the treatment.
Enzymes in the treatment of chlamydia
An important role in the treatment of chlamydia has the appointment of special drugs - enzymes.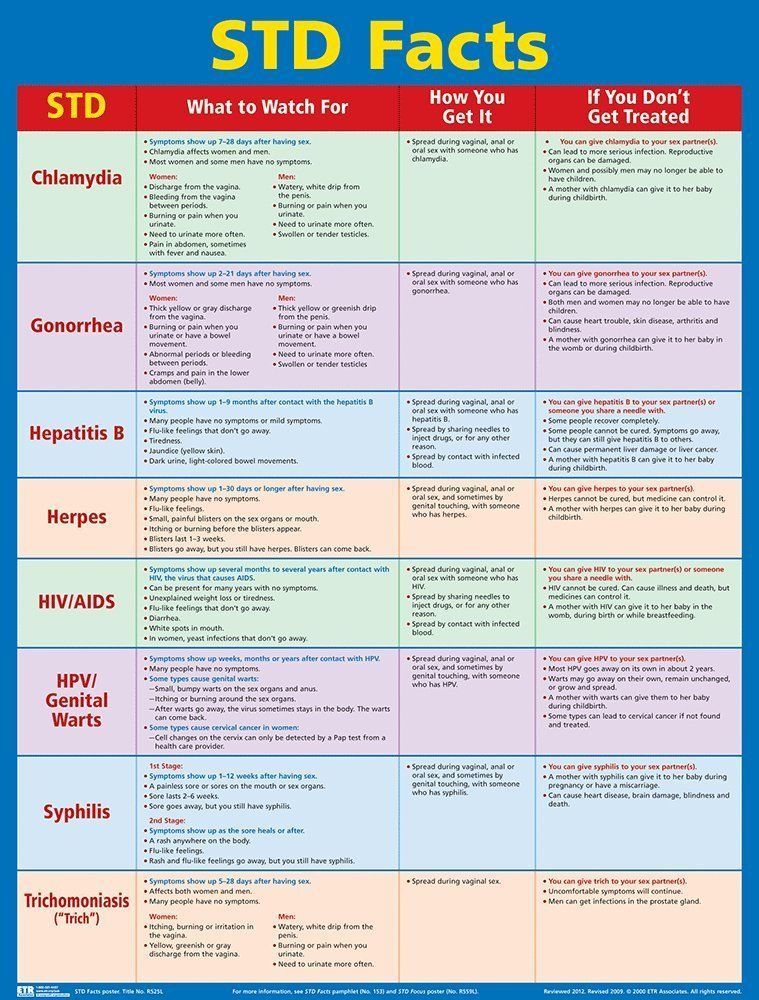 How do enzymes "help"? And enzymes provide invaluable help. First, they restore membrane permeability in diseased cells to normal. Thus, higher concentrations of antibiotics enter the cell at lower doses of their use. Enzymes also help reduce the body's allergic sensitivity to medications. Thirdly, enzymes provide decongestant and analgesic effects. Enzymes enhance the action of antibiotics not only inside the cell, but also increase their concentration in the blood by an average of 20–40%, which makes it possible to transfer large doses of antibiotics to diseased organs at a lower dosage. And, finally, enzymes contribute to the restoration of peripheral circulation.
How do enzymes "help"? And enzymes provide invaluable help. First, they restore membrane permeability in diseased cells to normal. Thus, higher concentrations of antibiotics enter the cell at lower doses of their use. Enzymes also help reduce the body's allergic sensitivity to medications. Thirdly, enzymes provide decongestant and analgesic effects. Enzymes enhance the action of antibiotics not only inside the cell, but also increase their concentration in the blood by an average of 20–40%, which makes it possible to transfer large doses of antibiotics to diseased organs at a lower dosage. And, finally, enzymes contribute to the restoration of peripheral circulation.
Local therapy in the treatment of chlamydia
Local therapy in the treatment of chlamydia conceived is simply required. It is also prescribed by a doctor, based on the nature of chlamydia, his knowledge and experience.
To prevent re-infection, all sexual partners must be found, examined and treated.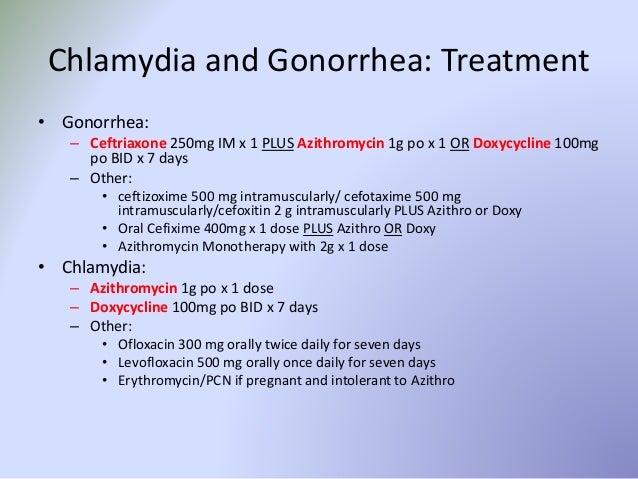 Patients with chlamydia should refrain from unprotected sex during treatment, otherwise re-infection is possible. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since immunity to this microorganism does not develop. A re-examination is carried out 4 weeks after treatment.
Patients with chlamydia should refrain from unprotected sex during treatment, otherwise re-infection is possible. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since immunity to this microorganism does not develop. A re-examination is carried out 4 weeks after treatment.
If chlamydia is not treated?
The complexity of the treatment of chlamydia lies in the fact that the bacterium Chlamydia trachomatis is not only unusually tenacious, but also in the fact that it is able to adapt to the antibiotic. Self-medication is especially dangerous for the patient, since a self-selected drug is not able to destroy the infection, but chlamydia develops immunity to the ingredients of the used drug and thus the infection becomes stronger than it was.
It often happens that an infected person treats chlamydia for years, but the body remains in the same place. Sometimes control tests show a negative result, despite the fact that chlamydia live in the cells of the patient (the consequences of chlamydia are witness to this - indestructible cystitis, thrush, prostatitis, etc.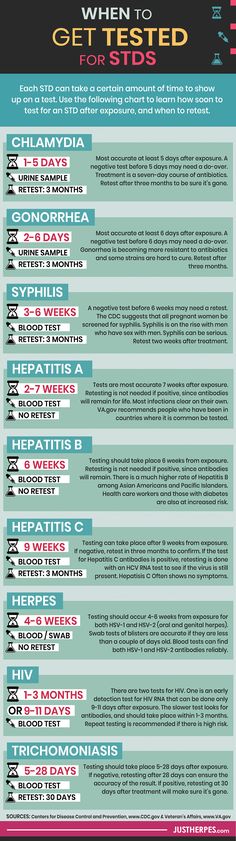 ). In this case, the patient is shown a provocation - an injection of a drug that will make chlamydia detect itself.
). In this case, the patient is shown a provocation - an injection of a drug that will make chlamydia detect itself.
Another important point: chlamydia rarely exists in the body in the singular, as a rule, it is included in a set of other infections (trichomoniasis, mycoplasmosis, ureaplasmosis, candidiasis, papillomavirus and herpes virus). All these infections are a factor that complicates therapy, but does not make it impossible.
Prevention of chlamydia
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Contraception with condoms dramatically reduces the risk of transmission. Annual testing for chlamydia is required for all sexually active men who are, by definition, at risk. If a patient has chlamydia (or any other sexual infections), he must inform his sexual partners about this.
Other articles by the author
- Impotence
- erection problems
- Orchitis, orchiepididymitis
- Curvature of the penis
- Androgen deficiency
- Premature ejaculation or accelerated ejaculation
- Infertility in men
- Genital warts in men
- Gardnerellosis in men
- Genital herpes in men
- Symptoms of prostatitis in men
- Chlamydia in men
- Ureaplasma in men
- cystitis in women
- Sexual infections in men
Doctors
All doctorsRylchikov Ivan Vladimirovich
KMN, urologist-andrologist, ultrasound specialist, head.