Blood loss after miscarriage
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
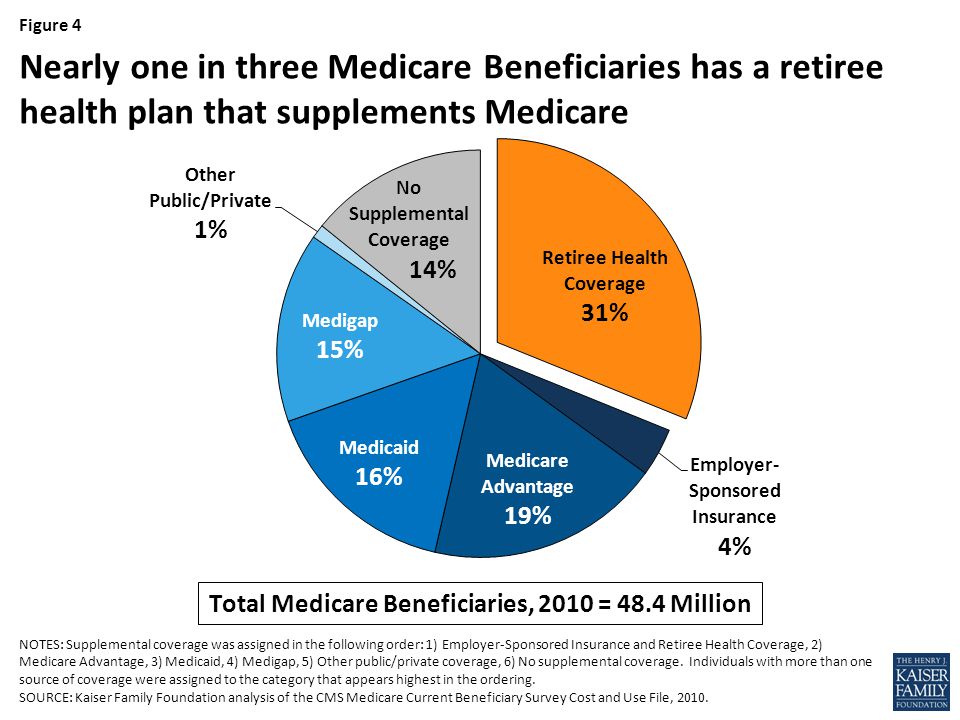
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.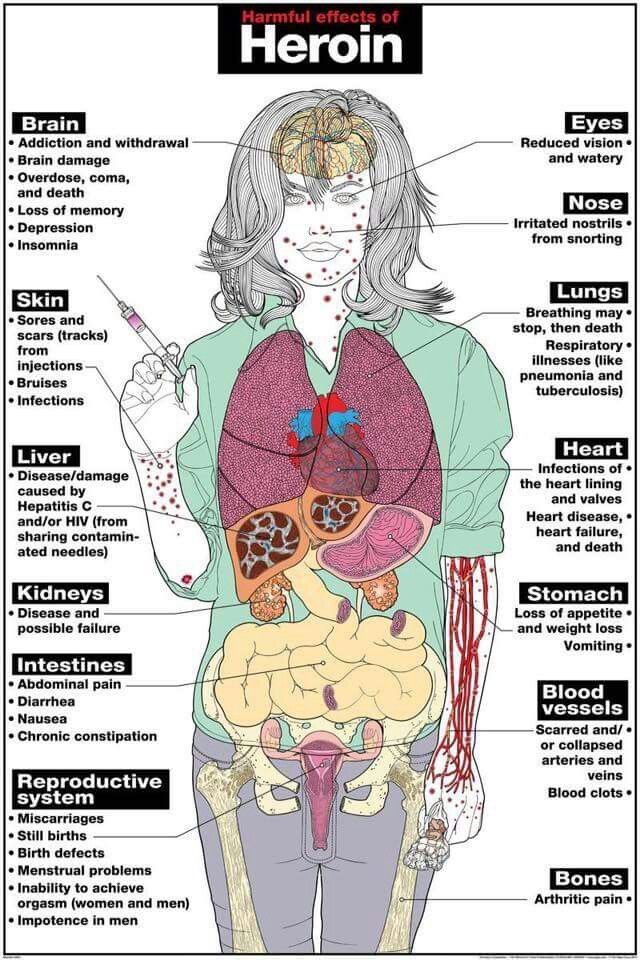
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
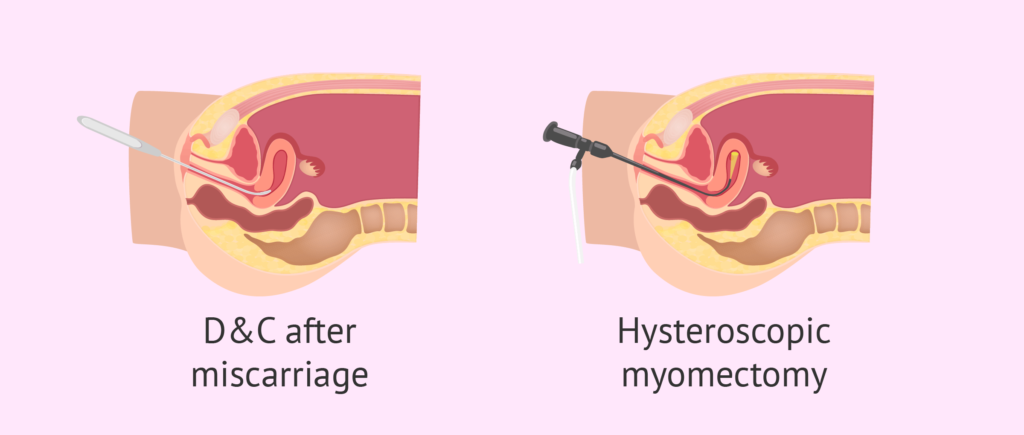
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA). This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months.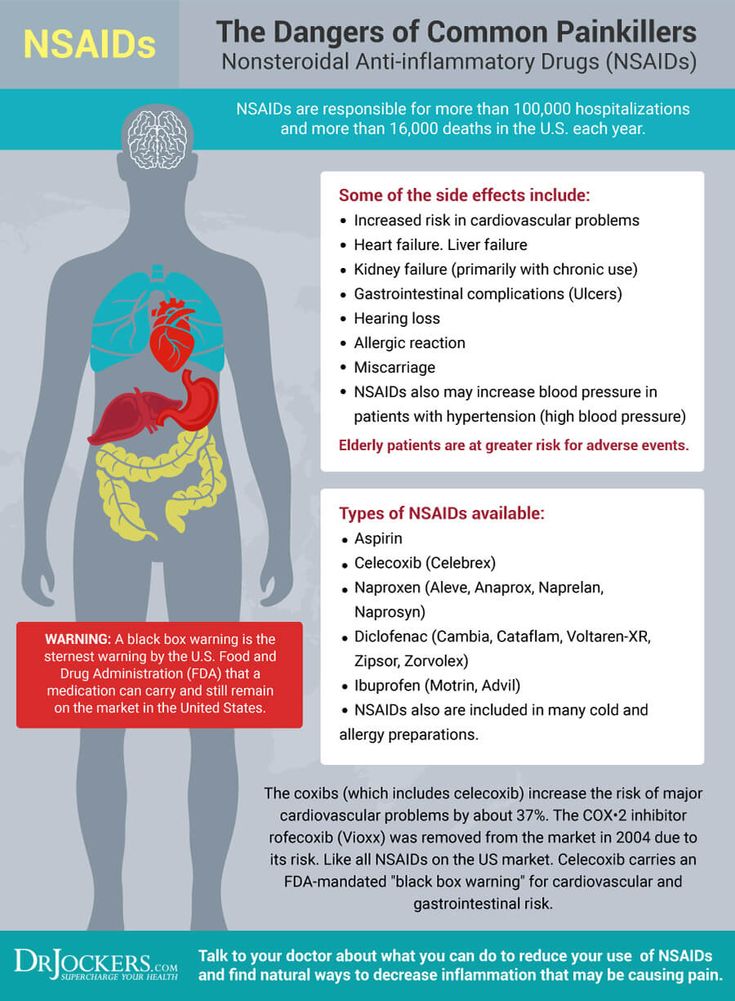 If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
Incomplete miscarriage | Tommy's
An incomplete miscarriage is when a miscarriage begins, but the pregnancy doesn’t completely come away from the womb.
What is an incomplete miscarriage?
Sometimes not all of the pregnancy comes away after a miscarriage. An incomplete miscarriage is when a miscarriage begins, but some pregnancy tissue stays in the womb.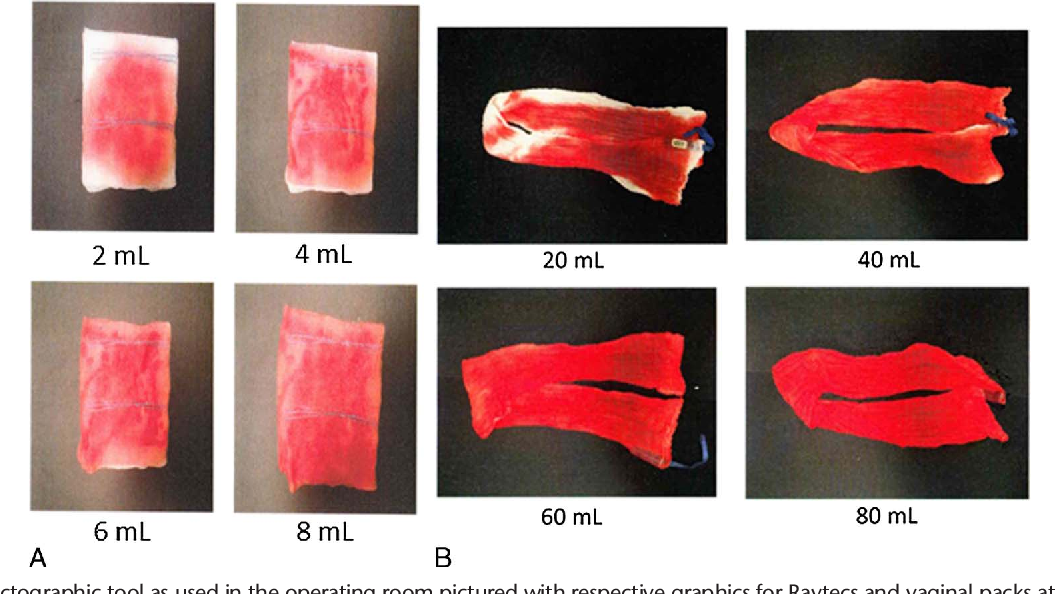
Signs of an incomplete miscarriage
All women have some bleeding or pain during and after a miscarriage. But if you have an incomplete miscarriage, you may have these symptoms:
- heavy bleeding – get medical help if you’re soaking through a pad in an hour
- bleeding that carries on and doesn’t settle down
- passing blood clots
- increasing tummy pain, which may feel like cramps or contractions
- a raised temperature (fever) and flu-like symptoms.
Get medical help straightaway if you experience any of these warning signs.
Treatment for an incomplete miscarriage
If you have an incomplete miscarriage, you’ll need to have treatment. There are 3 options available:
- waiting for the miscarriage to happen by itself naturally (expectant management)
- taking medicine to help things along (medical management)
- having surgery to remove the pregnancy (surgical management).
Your doctor should talk with you about what may be the best option for you. You should be given some time for the diagnosis to sink in and to think about what you want to do.
You should be given some time for the diagnosis to sink in and to think about what you want to do.
“It's OK to take your time over making a decision. You may have a gut feeling about how to manage the miscarriage, you may not. Talk through your options with the medical professionals. I know they are incredibly busy, but we needed and wanted answers. I phoned the number we were given after our second missed miscarriage and asked all the questions I had. This helped us make a decision.”
Catherine
How you are treated is your choice. However, you may be advised to have surgery immediately if there are any problems, such as infections.
Find out more about how your miscarriage will be managed.
Your emotional health
Miscarriage can be devastating. You may be struggling with grief, anxiety and shock, but you do not need to go through this alone. There are lots of organisations that can provide advice and support.
If you’re worried that you or your partner are struggling to cope after losing a baby, please talk to your GP. They will be able to help you get the support you need.
They will be able to help you get the support you need.
You can also talk to a Tommy’s midwife for free. You can call them Monday-Friday, 9am-5pm on 0800 0147 800 or you can email them at [email protected]. Our midwives are trained in bereavement support so will be able to talk to you about what you’re going through.
Find out more about support after a miscarriage.
Back to top
What to do after a miscarriage - recovering from a miscarriage
A miscarriage can be a difficult topic to talk about, but sometimes talking is the best way to come to terms with it and start healing from the whole experience. Let's dive deeper into what happens to the body after a miscarriage, as well as learn how to deal with your own feelings.
A miscarriage is when an embryo or fetus does not survive in the uterus during the first 23 weeks of pregnancy. [1] Miscarriage is more common than most people think: every 4th pregnancy ends like this.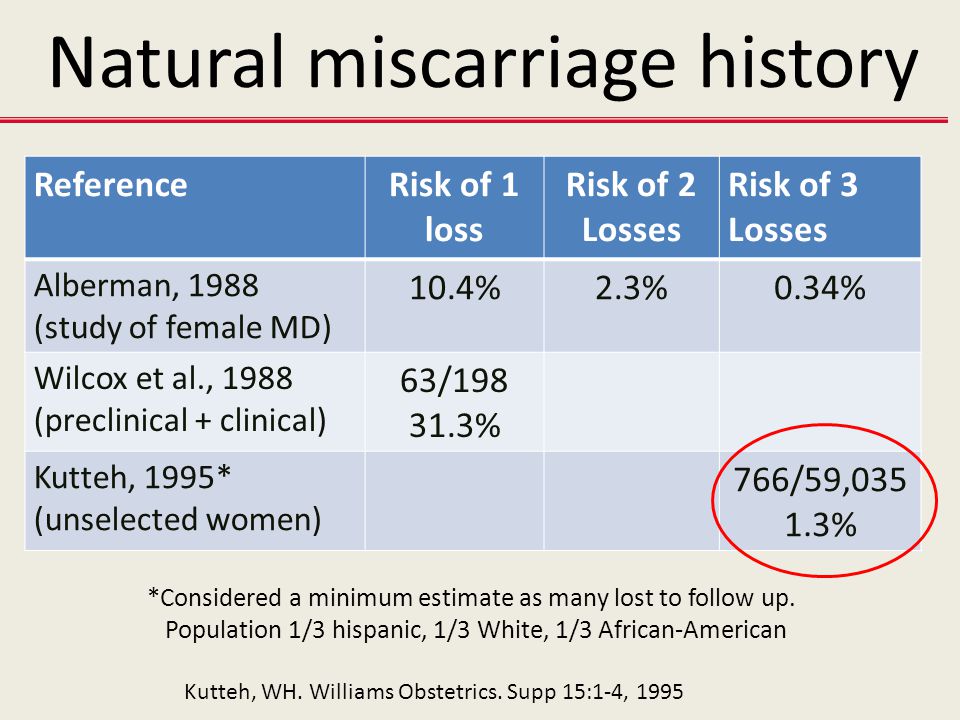 Just because it isn't talked about often doesn't mean it's rare.
Just because it isn't talked about often doesn't mean it's rare.
Talking about miscarriages can be difficult, because often it is a real grief. However, this topic is becoming less and less taboo, and many women come together in solidarity to share their experiences. This way they know they are not alone in their grief.
A miscarriage is a whole process: your body will be under a lot of physical and emotional stress both during and after the miscarriage. Therefore, we will look at how this situation changes your body in terms of periods, future pregnancies and emotions.
What is bleeding and discharge during a miscarriage?
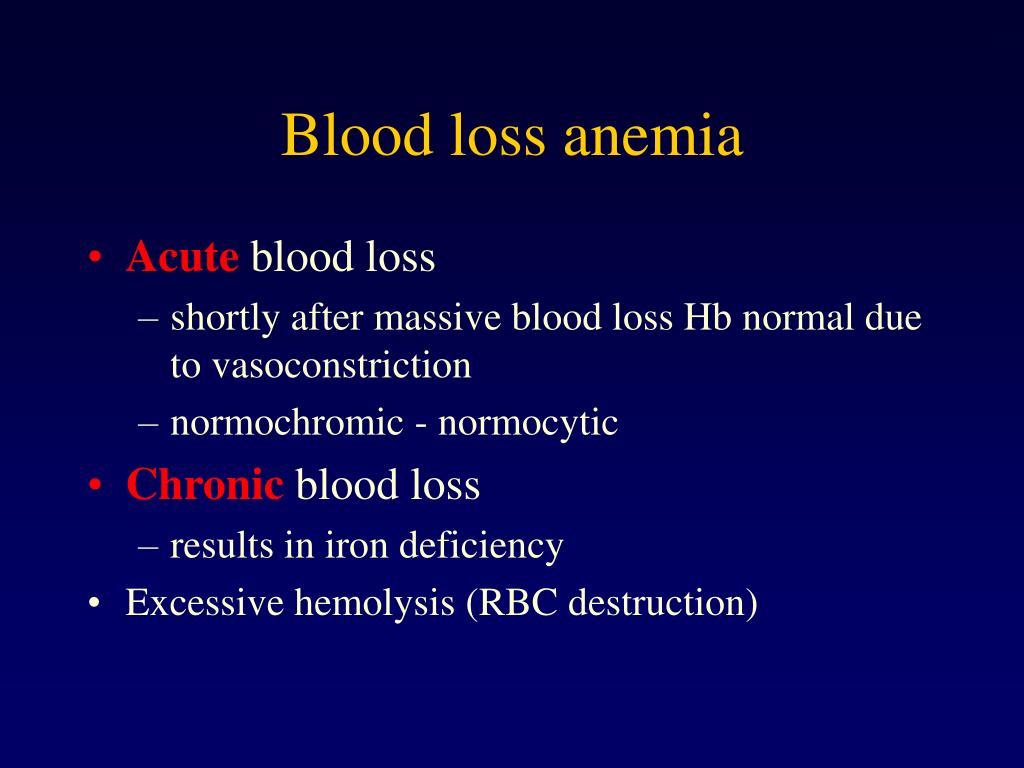
The most common symptom of a miscarriage is vaginal bleeding during pregnancy. The severity of this bleeding can vary from person to person: sometimes it is heavy with blood clots, other times it can be just spots or brown discharge. This bleeding can last up to 2 weeks. Another symptom of a miscarriage is abdominal pain. They occur when the muscles of the uterus contract to push all the tissues of the embryo or fetus out of the cavity in the form of clots through the vagina.
Regardless of the amount of blood you have from your vagina during pregnancy, you need to see a doctor as soon as possible. While not all bleeding during pregnancy is a sign of a miscarriage (implantation bleeding is considered normal in the early stages of pregnancy), it's always best to see a doctor if you're concerned.
What will my first period be like after a miscarriage?
Having experienced a miscarriage, you may wonder how your body will react to it and if there will be any long-term consequences. Miscarriages rarely change the body forever, but you need to give the body time to get used to and return to its normal rhythm of life.
After a miscarriage, you can expect your period to return to normal in about 4-6 weeks, although recovery time varies from person to person and can take up to several months. [2]
Don't worry about the return of your period, instead give yourself time to rest while your body repairs and heals.
Getting pregnant after a miscarriage
Some women may immediately return to trying to conceive after a miscarriage, while others may take some time to "digest" the event. Some may even wonder if they even want to have children. Whatever your reaction to your own experience, it is important to recognize that there is no right or wrong way - we all cope differently.
If you still want to try again, it is usually recommended to wait until the symptoms of the miscarriage have passed to prevent infection. [3] You can also wait until your period starts again so that you can calculate your future pregnancy dates more accurately.
And remember: you can always consult your doctor about a new pregnancy, but most importantly, you decide when you are ready.
Dealing with your feelings after a miscarriage
The consequences of a miscarriage can be felt immediately after it or after a while - everyone mourns the baby in different ways.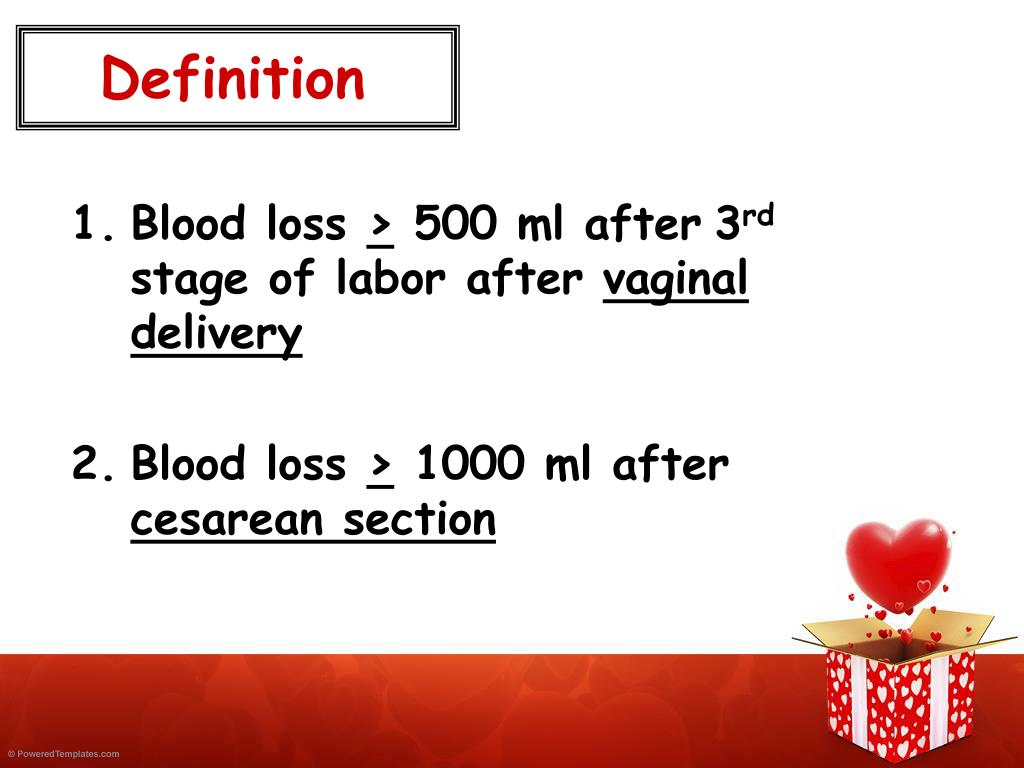 No matter how you react, it is important to understand that you did nothing wrong: miscarriage is not related to your personal strength or ability.
No matter how you react, it is important to understand that you did nothing wrong: miscarriage is not related to your personal strength or ability.
I hate to talk about this, but expressing thoughts and emotions can really help in the healing process. And even if at first it seems uncomfortable to talk to people about a miscarriage, you will be surprised how many women understand what you have gone through and are ready to provide support.
There are also many charities and associations dedicated to helping people with spontaneous abortions. So if you ever need comforting advice, there are many more people you can turn to besides friends and family.
Miscarriage is no doubt a difficult topic to discuss, but silence only reinforces the taboo and prevents many people from seeking support. Remember that you are not alone and that it is okay to speak up when you feel ready to do so.
To further discuss pregnancy, check out our articles on fertility treatments and what it's like to be childless by choice.
Medical disclaimer
The medical information contained in this article is for reference only and should not be used for any diagnostic or therapeutic purposes. Consult your doctor about a specific medical condition.
[Links]
[1] https://www.nhs.uk/conditions/miscarriage/
[2] https://www.betterhealth.vic.gov.au/health/HealthyLiving/miscarriage#after-a-miscarriage
[3] https://www.miscarriageassociation.org.uk/information/worried-about-pregnancy-loss/trying-again/
What to do after a miscarriage
If a woman has had a miscarriage, it is important to take the right steps to recover health. This will help to cope mentally and prepare the ground for a new pregnancy. According to medical statistics, 15-20% of pregnancies end in spontaneous termination for various reasons. The symptoms of what happened rarely go unnoticed, which makes it possible to diagnose the pathology in time, consult a gynecologist, undergo adequate treatment and plan the birth of a child for the future.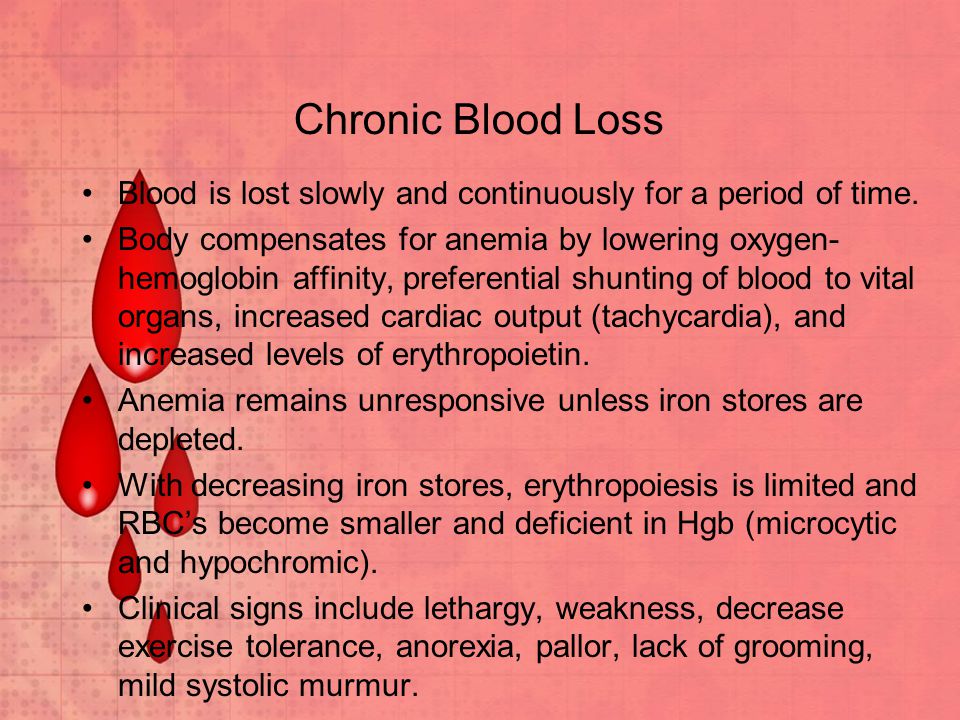
Experts classify spontaneous abortion into two categories:
1. Termination of biochemical pregnancy - the embryo leaves the uterine cavity in the first or third weeks after conception. A woman during this period most often does not suspect that she is carrying a child. Pregnancy becomes known only when testing for the content of hCG in the urine and blood. The blood that has left the body is usually perceived as menstruation, which, for unknown reasons, began outside the scheduled time. Units who carefully monitor their health go to the doctor.
2. Spontaneous abortion or miscarriage in early pregnancy - up to 22 weeks, when the weight of the embryo does not reach 0.4 kg.
What is a miscarriage like
A miscarriage that occurs is complete when all parts of the embryo come out of the uterine cavity together with membranes and amniotic fluid. If parts of the fetus remain in the uterus, they speak of an incomplete miscarriage, which occurs more often in the early stages of pregnancy. To neutralize the negative consequences, to prevent the development of an infectious process in the tissues, the product of conception is evacuated from the uterine cavity by the methods of medical interruption, gynecological curettage, and vacuum aspiration. Therapy may include the use of drugs aimed at contracting the uterus and pushing the contents out. Ultrasound examination is considered to be the control method of diagnostics.
To neutralize the negative consequences, to prevent the development of an infectious process in the tissues, the product of conception is evacuated from the uterine cavity by the methods of medical interruption, gynecological curettage, and vacuum aspiration. Therapy may include the use of drugs aimed at contracting the uterus and pushing the contents out. Ultrasound examination is considered to be the control method of diagnostics.
Why the body rejects the embryo
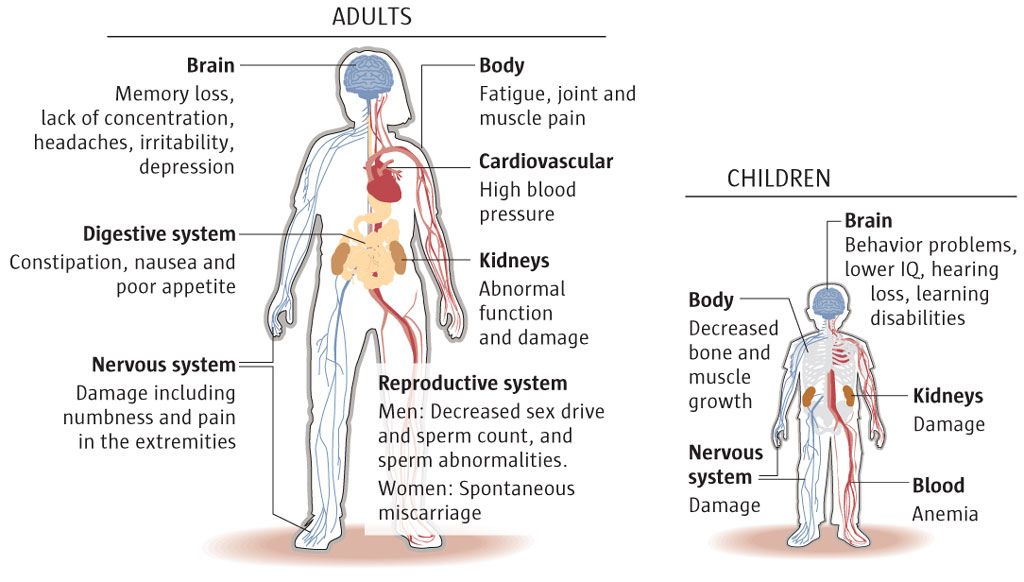
The causes of miscarriage often lie in the presence of chromosomal abnormalities in the fetus. Among the factors provoking rejection of embryos are also:
- Heredity and genetic failure at the stage of fertilization of the egg by the sperm.
- A non-viable fetus may appear as a result of various risk factors - environmental conditions, occupational hazards, viral illness of parents. It is impossible to neutralize these factors. The only way out of the situation is to reduce the likelihood of their manifestation by protecting the expectant mother from dangers during gestation.
- Hormonal imbalance caused by disruption of the endocrine system. The situation can be affected by an insufficient amount of progesterone in the mother's body or an excess of testosterone. With early detection of a failure of the hormonal system, a woman undergoes specially organized therapy before pregnancy.
- The presence of tumors , neoplasms in the pelvic organs.
- Isthmic-cervical insufficiency when the isthmus and cervix dilate prematurely, unable to cope with the increasing pressure caused by the growing fetus in the body.
- There is a risk of miscarriage in the presence of anomalies in the work of the cardiovascular and renal systems.
- Drug addiction , alcohol addiction, substance abuse of mother and father.
- Depressive conditions , stress, nervous stress of a pregnant woman.
- Mechanical stress , blows, bruises, excessive physical labor of the future woman in labor.
- X-ray examination - radiation can cause miscarriage.
- Drug use . In the first trimester, you can not use potent medicinal formulas. Drugs can cause the development of defects in the embryo. Some decoctions of herbs are also contraindicated - parsley, tansy, cornflower, nettle, St. John's wort. It is forbidden to self-medicate. Each drug is agreed with the attending physician.
- Infectious and viral process in the body. Any sexually transmitted infection can provoke a miscarriage, which must be cured before pregnancy, otherwise there is a high risk of infection of the fetus in the womb. A great threat of miscarriage in the early stages exists due to viral infections and inflammation of the internal organs. A dangerous symptom is the high temperature of the mother, accompanied by intoxication of the body. At the stage of pregnancy planning, it is important to stop chronic diseases.
- History of abortion , unsuccessful surgery, unprofessionalism of the doctor and unfortunate circumstances.
- Immunological factors .
The list of causes of miscarriage in the early stages of pregnancy and in the later period may be more extensive, in each case, doctors identify the pathology individually.
Isthmic-cervical insufficiency (ICI)
One of the most common causes of spontaneous miscarriage during pregnancy is CSI - dilatation of the cervix and isthmus of the uterus as a result of increasing pressure from the growing fetus. Pre-pregnancy manipulations with the uterus (cervical dilation due to abortion, childbirth or curettage) affect the condition of the muscle ring. Damaged areas are tightened by scar tissue that does not have elasticity, is not amenable to stretching and contraction. ICI also has a functional nature when there is a hormonal imbalance.
ICI occurs in the period from the 11th to the 27th week after conception, when the embryo begins to produce androgens in the mother's body with the launch of the adrenal glands. Taking into account the mother's hormones, their indicator can be exceeded - this softens the cervix, opens and shortens it. Harmful bacteria and microorganisms penetrate into the formed channel, infecting the fetal egg. The initial stages of ICI do not have obvious symptoms, since they do not entail the tone of the uterine muscles. With the loss of strength of the membranes, amniotic fluid pours out. There are no pain sensations.
Taking into account the mother's hormones, their indicator can be exceeded - this softens the cervix, opens and shortens it. Harmful bacteria and microorganisms penetrate into the formed channel, infecting the fetal egg. The initial stages of ICI do not have obvious symptoms, since they do not entail the tone of the uterine muscles. With the loss of strength of the membranes, amniotic fluid pours out. There are no pain sensations.
If a woman has had a miscarriage that started with amniotic fluid, she should report it to her doctor when monitoring a subsequent pregnancy.
Treatment of isthmic-cervical insufficiency
Endocrine disorders are corrected by prescribing hormonal drugs. An assessment of the condition of the uterus is carried out by a doctor a couple of weeks after the start of taking medications. They say about positive dynamics when the opening is suspended and no further expansion of the neck is observed. In the absence of the planned effect, surgical intervention is prescribed. Similar measures are used for the traumatic nature of the neck deformity. You should not be afraid of the operation, the doctor acts delicately, without causing additional injuries to the patient, without causing discomfort to the baby growing in the womb. The procedure is most effective in the early stages of pregnancy. Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity.
Similar measures are used for the traumatic nature of the neck deformity. You should not be afraid of the operation, the doctor acts delicately, without causing additional injuries to the patient, without causing discomfort to the baby growing in the womb. The procedure is most effective in the early stages of pregnancy. Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity.
Surgical intervention takes place in a hospital setting. Before the operation, the pregnant woman is examined. After the procedure, the vagina is sanitized, for which the suturing site is treated with chlorhexidine and furatsilin for three days. The patient needs to undergo a weekly follow-up examination with the attending physician, where he assesses the situation, making adjustments to the therapeutic protocol if necessary. The sutures are removed at the 38th week of pregnancy. During this time, the neck matures, preparing the birth canal for the passage of the fetus. Many women in labor worry that they will need a caesarean section if they have stitches, but this is not true. In most cases, women give birth on their own.
Many women in labor worry that they will need a caesarean section if they have stitches, but this is not true. In most cases, women give birth on their own.
Immediate action is recommended if the amniotic sac prolapses (falls out) into the cervix between 16 and 24 weeks. The suturing of the neck obliges the woman to observe bed rest, strictly follow the daily routine, avoid physical exertion, and do not skip taking medications. In rare cases, complications occur. Among them, the eruption of sutures through the tissues, provoked by the frequent tension of the muscles of the uterus. To prevent tone, tocolytics are prescribed - medicines to prevent premature birth. The expectant mother should be prepared for frequent examinations and smears, which may be caused by the likelihood of accumulation of pathological microflora on the suture threads.
It is also important to conduct psychological therapy, where a woman is taught relaxation techniques. The behavior of the future mother is a decisive factor in the successful bearing of the fetus in case of pregnancy complications.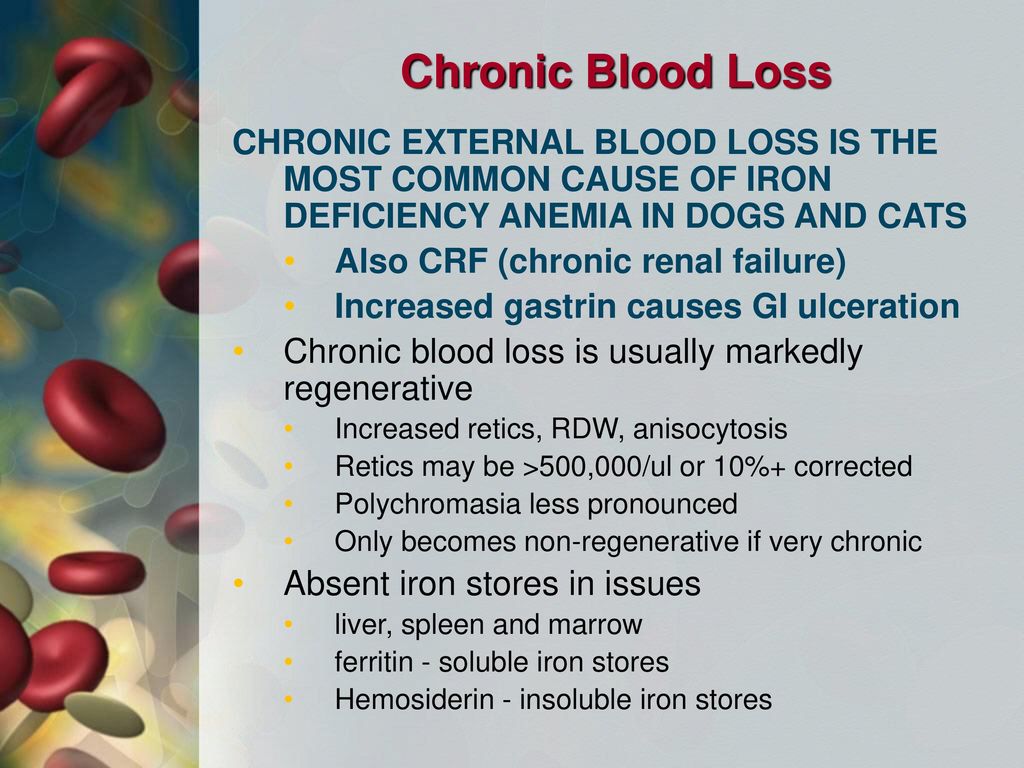 Panic and fuss create an unfavorable prognosis in stabilizing the situation. If a spontaneous abortion occurred for reasons of ICI, when you can get pregnant after a miscarriage, the doctor will say. Ideally, the period should be at least two years. The specialist must also take measures to prevent a repeated situation of losing a child.
Panic and fuss create an unfavorable prognosis in stabilizing the situation. If a spontaneous abortion occurred for reasons of ICI, when you can get pregnant after a miscarriage, the doctor will say. Ideally, the period should be at least two years. The specialist must also take measures to prevent a repeated situation of losing a child.
In addition to the suture, ICI correction is also carried out using an obstetric pessary. An alternative method is the imposition of a special ring of hypoallergenic materials on the cervix. Silicone is the most commonly used. The ring creates additional support, preventing the opening of the neck.
Uterine hypertonicity - risk prevention
Uterine contractions before natural delivery is called hypertonicity. The condition is not an independent disease, it signals a malfunction in the body, often manifesting itself in the early stages of pregnancy. The causes of the pathological phenomenon are:
- Hormonal disorders caused by insufficient function of the placenta, ovaries, problems with the adrenal glands causing imbalance.

- Genital infantilism organ defects.
- Neoplasms , tumors in the uterus that are not necessarily malignant (eg, fibroids).
- During pregnancy infectious processes, viral diseases.
- CCI - opening of the cervix under increasing pressure created by the growing embryo.
- Immunological problems .
- Chronic diseases of the body (cardiovascular disorders, renal insufficiency).
- Past miscarriages early pregnancy, symptoms of which may recur, induced abortions.
In addition to physiological causes, psychological factors are of no small importance. A woman who is in a depressed state can provoke hypertonicity in herself.
You can feel the tension of the muscles of the uterus on your own, without the help of a specialist. This is evidenced by the heaviness that appears in the lower abdomen, pulling pains in the lumbar region. Symptoms are similar to painful menstruation. Arising in the first trimester, the condition provokes spontaneous abortion, missed pregnancy, death of the fetal egg. In the subsequent period, premature birth due to hypertonicity is likely.
Symptoms are similar to painful menstruation. Arising in the first trimester, the condition provokes spontaneous abortion, missed pregnancy, death of the fetal egg. In the subsequent period, premature birth due to hypertonicity is likely.
Why does tension in the walls of the uterus cause irreversible consequences? The reason is the disturbed blood supply to the placental tissues, the occurrence of hypoxia of the embryo and the slowdown in the development of the emerging child. Following the contraction of the muscles of the uterus, the placenta does not contract, which causes its detachment and provoking the release of the fetal bladder.
Hypertonicity is diagnosed during a scheduled visit to a specialist. Stabilization of the situation requires the appointment of sedative drugs and antispasmodics. A strengthening effect is provided by therapy with the inclusion of vitamin B6, magnesium. In most cases, the measures taken are sufficient to neutralize the risks. Self-treatment, which can cause irreversible consequences, is strictly prohibited. With hypertonicity, the main rule for a pregnant woman is calmness and lack of physical activity. Some women who have had a successful delivery say they "didn't get up" during their entire pregnancy. With hypertonicity, sexual intercourse is also excluded.
With hypertonicity, the main rule for a pregnant woman is calmness and lack of physical activity. Some women who have had a successful delivery say they "didn't get up" during their entire pregnancy. With hypertonicity, sexual intercourse is also excluded.
If the threat cannot be neutralized, hospitalization is recommended. It is especially dangerous when severe cramping pain is complemented by spotting. To lie down "for preservation" is an adequate measure in the struggle for the birth of a healthy and strong baby. In the hospital walls, a pregnant woman is prescribed a vaginal examination, ultrasound. If necessary, a woman takes urine and blood tests, checks the hormonal background, and is examined for the presence of STIs.
At the beginning of labor activity before the 34th week, the state is tried to be stabilized with tocolytics. The most dangerous period is from the 25th to the 28th week, when the woman is recommended the maximum possible bed rest. After that, the fetus has every chance of survival. In order to quickly form the pulmonary system of the embryo, allowing it to survive with an early birth, hormones are prescribed.
In order to quickly form the pulmonary system of the embryo, allowing it to survive with an early birth, hormones are prescribed.
Having an unfavorable prognosis for miscarriage and the threat of miscarriage, it is necessary to take up prevention at the stage of conception planning.
Stages of spontaneous abortion
There are certain signs that attract attention and divide the course of miscarriage into specific stages:

Symptoms of miscarriage - how not to miss the threat
If there is a threat of miscarriage in the early stages, the following symptoms may occur: The pain may be monotonous or come in waves.
A woman who does not know how an early miscarriage occurs should listen to her inner state.
Should alert:
- spasmodic pain impulses;
- Drawing pain in the lumbar region.
In the later stages, the above symptoms are added:
- liquid discharge from the vagina, which may indicate damage to the amniotic sac;
- pain when urinating;
- internal bleeding, which warns the deterioration of the general condition, fainting, dizziness, pallor of the skin.
 All this is an indication for emergency hospitalization of a pregnant woman.
All this is an indication for emergency hospitalization of a pregnant woman.
The beginning of an abortion is characterized by more pronounced symptoms of a miscarriage - contraction-like pain, severe dizziness, loss of strength. Instead of smearing discharges, clot-like ones appear, abundantly manifested during movement. Pregnancy can be saved if the area of detachment of the fetal egg is small and the fetal heartbeat is determined.
The third stage is useless to save the fetus. There is girdle pain in the lower back and abdomen. Together with abundant blood loss, a fetal egg comes out of the uterus. Incomplete miscarriage requires curettage of the uterine cavity if parts of the embryo or membranes of the fetal egg remain in it, otherwise there is a high risk of complications that will endanger the life of the mother.
In rare cases, complications and serious health consequences can occur after a spontaneous abortion. But in the majority of situations, the body independently copes with what happened, expelling the parts remaining in the uterine cavity with a natural contraction of the muscles.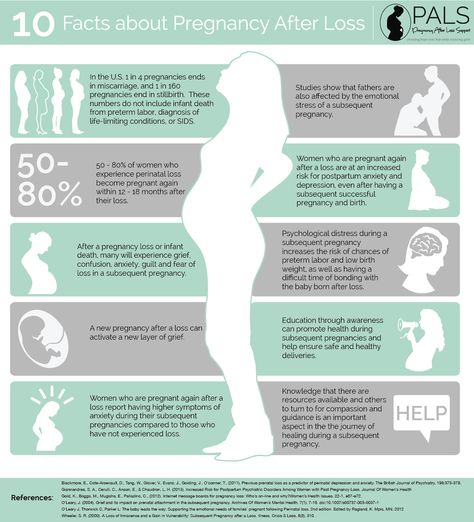 An early spontaneous miscarriage does not always occur, a dangerous condition can also occur in the later stages. Some women try to provoke the release of the fetus with decoctions of herbs and medications. This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible.
An early spontaneous miscarriage does not always occur, a dangerous condition can also occur in the later stages. Some women try to provoke the release of the fetus with decoctions of herbs and medications. This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible.
Methods of diagnosis
The symptoms of a threatened miscarriage at an early stage will be determined by a doctor during a visit to the antenatal clinic. The specialist will check the size of the uterus, determine the tone of its muscles, the condition of the cervix, and examine the discharge from the genital organs. A reliable method to identify the existing threat is transvaginal ultrasound diagnostics. The doctor draws attention to segmental muscle contractions of the uterus, detachment of the fetal egg. Genetic testing will help analyze the likely causes of a miscarriage. The patient's history is carefully collected.
Medical therapy
Any method is useful to maintain pregnancy. A qualified doctor develops an individual treatment protocol based on the available diagnostic data. Drugs used may include:
A qualified doctor develops an individual treatment protocol based on the available diagnostic data. Drugs used may include:
- sedatives;
- restorative therapy;
- hormone stabilizing drugs;
- uterine antispasmodics;
- vitamin and mineral supplements.
The specialist eliminates the threat of miscarriage in the early stages, tells how to prevent a relapse. In the later stages, the cervix is fixed with a special suturing (usually for a period of 16-25 weeks, if there is an ICI).
In case of an unsuccessful attempt to stop a spontaneous abortion, the following treatment tactics are used:
- Waiting - an organism that has freed itself from an embryo does not require specialized treatment.
- Drug therapy - the patient is prescribed drugs that complete the removal of foreign tissues from the body. By causing severe spasms of the muscular walls of the uterus, the tablets provoke the expulsion of residues from the cavity.

- Surgery - is used in case of complications or inconvenient for the independent exit of the fetus, the bending of the uterus.
Curettage
Having symptoms of a miscarriage in early pregnancy and faced with the need for a curettage (gynecological cleansing), a woman worries about the state of her reproductive system. It is not worth doing this, the operation takes place in a gentle mode, with maximum delicacy in relation to the patient's childbearing ability. Curettage is performed when there is a risk of incomplete exit of the embryo from the uterine cavity and the development of infection in the pelvic organs due to the elements remaining in it. Ignoring the procedure can lead to blood poisoning and the formation of a pathology that prevents re-conception.
Vacuum aspiration, however, is performed more frequently and is more gentle. The complex application of the method with hysteroscopy allows you to carefully examine the internal contents of the uterus in order to prevent poorly cleaned areas on the mucous membrane.
Preparation for gynecological cleaning (curettage)
Gynecological cleaning is performed for diagnostic and therapeutic purposes for various indications :
- after childbirth;
- in missed pregnancy, miscarriages;
- for menstrual irregularities;
- for accurate diagnosis of gynecological disorders.
Curettage is recommended a few days before the onset of menstruation. In this case, blood loss decreases and a favorable prognosis is given for rapid tissue recovery. The operation requires a preliminary examination, testing. This is :
- complete blood count;
- blood coagulation test;
- smear for examination of the bacteriological environment;
- STI testing.
Before curettage, you stop taking any medications, dietary supplements that have not been discussed with a specialist. Even plant components that can affect blood clotting and provoke blood loss during surgery can be dangerous. Your healthcare provider should be made aware of the medications you are taking so that they know what risks may arise.
Your healthcare provider should be made aware of the medications you are taking so that they know what risks may arise.
Rules for preparing for the procedure:
- refrain from sexual intercourse three days before the operation;
- avoid using intimate hygiene products (gels, creams, ointments, liquids), suppositories, tablets and vaginal sprays;
- don't douche;
- Do not eat or drink 10 hours before surgery. This is necessary for high-quality anesthesia.
Cleaning
Curettage is carried out in a hospital, the woman is placed on the gynecological chair of the operating room. The doctor removes the upper layer of the mucous lining the uterine cavity from the inside. The exclusion of pain involves anesthesia. If there were signs of miscarriage in the early stages of pregnancy or at a later period, after which it spontaneously terminated, the dilated cervix allows for curettage without anesthesia. For anesthesia, intravenous administration of the drug is used, selected individually, taking into account the characteristics of the patient's body.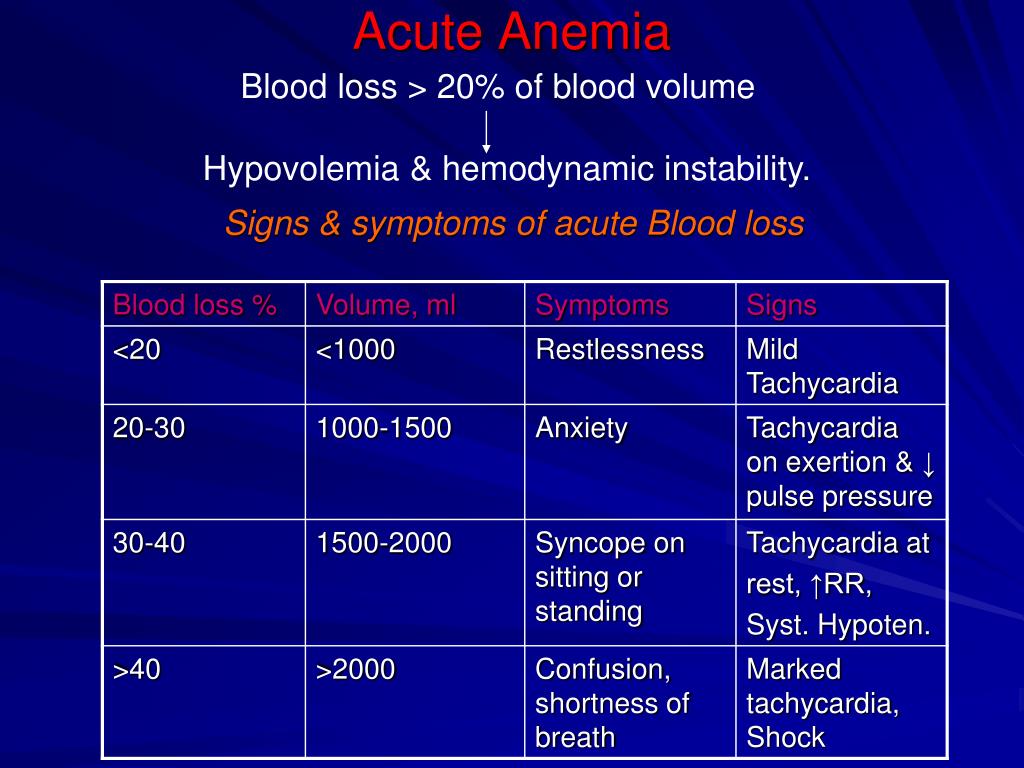 A few seconds after the injection, the woman falls into a shallow sleep, the discomfort disappears, which makes the doctor's actions painless.
A few seconds after the injection, the woman falls into a shallow sleep, the discomfort disappears, which makes the doctor's actions painless.
A dilator inserted into the cervix straightens the walls of the organ, facilitating access to the internal cavity. Holding the neck, the specialist inserts a rounded probe with a small diameter, after which he replaces it with a more voluminous analogue. A special video camera attached to the end of the probe allows for hysteroscopy - examination of the cavity before curettage. Cleaning is done with a curette, shaped like a small spoon on a long handle. Carefully collected tissues are stored in a specialized sterile tube, which is later sent to the laboratory for histological examination.
The procedure rarely takes more than one hour, usually 20 minutes is enough for the doctor. Together with the cavity, the cervical canal is cleaned. Manipulations are called RDV - separate diagnostic curettage. Collected samples are placed separately. Histology is used to identify the structure of tissues in order to exclude the presence of atypical cells in them, indicating cancerous lesions, precancerous conditions. The study is carried out within two weeks, after receiving the results, the woman revisits the gynecologist for a follow-up examination.
Histology is used to identify the structure of tissues in order to exclude the presence of atypical cells in them, indicating cancerous lesions, precancerous conditions. The study is carried out within two weeks, after receiving the results, the woman revisits the gynecologist for a follow-up examination.
Curettage is often carried out for diagnostic purposes to determine the symptoms of pathological conditions in the functioning of the organs of the reproductive system. These can be:
- irregular cycle;
- bulky discharge and painful menstruation;
- bleeding during menopause;
- difficulties in conceiving in the absence of visible causes of pathology;
- suggestion of developing uterine cancer.
Possible complications
Complications can occur, as after any surgical intervention. A serious consequence is the discovery of uterine bleeding. In order to prevent it, oxytocin is used - injections stimulate the cessation of abnormal blood flow. Oxytocin will help if the bleeding is due to insufficient contraction of the uterus. In violation of blood clotting, it is ineffective.
Oxytocin will help if the bleeding is due to insufficient contraction of the uterus. In violation of blood clotting, it is ineffective.
Another complication of is hematometra, when blood clots accumulate in the uterine cavity, which can cause an inflammatory process in the tissues. It is caused by a spasm of the cervix that occurred immediately after cleaning, which interferes with the evacuation of blood. Experts recommend the use of antispasmodics that relax the muscles of the organ and contribute to the normal outflow of blood. A woman should be alerted by pulling pains in the lower abdomen and a sharp cessation of discharge.
After cleansing, endometritis may occur when inflammation affects the lining of the uterus. A measure of therapy for a dangerous diagnosis is a course of antibiotics. Pain in the abdomen and a sharp increase in body temperature testify to the pathology. Any dangerous change in condition should be reported to the doctor immediately. In this case, countermeasures will be taken in a timely manner, which will eliminate the risks of developing more formidable complications.
In this case, countermeasures will be taken in a timely manner, which will eliminate the risks of developing more formidable complications.
How to behave after a miscarriage
A miscarriage that has occurred requires a certain tactic of behavior. Among the measures recommended by doctors:
- It is advisable to postpone a new pregnancy attempt for 3-6 months . Otherwise, the risk of repeating the undesirable development of events is high. If pregnancy occurs before the expiration date, there is no need to panic. The main thing is the supervision of a specialist.
- If you are waiting for , ask for advice on effective contraception.
- Follow your doctor's advice .
- Pass the necessary examinations , take tests.
Consult what effect the medicines you take will have on the fetus if you become pregnant during therapy. Find out after what period of time you can fearlessly try to conceive a child.
How to detect genetic pathologies during repeated pregnancy
If a miscarriage of the first pregnancy occurs due to a genetic factor, it is especially scary to decide on a second one. But you should not be afraid of this, with a well-designed therapy, the chances of success are more than great. Diagnostic procedures today are highly accurate and allow you to identify pathology in the early stages. Examination in this case is mandatory, as well as the following:
- who are over 35;
- has screening changes;
- who had markers of chromosomal pathologies and malformations of the embryo;
- who already have children with chromosomal abnormalities.
Ultrasound diagnostics can detect malformations in 80-85% of cases. However, the technology is not impeccably reliable, as it misses pathologies in 20% of situations. Biochemical screening, invasive examinations have valid data. The latest version of the study allows you to identify up to 99% anomalies. No less popular is the high-precision PANORAMA test for determining DNA pathologies.
No less popular is the high-precision PANORAMA test for determining DNA pathologies.
When planning a new pregnancy, it is imperative to visit a geneticist. Screening diagnostics for the detection of abnormal genes will help eliminate the risks of possible pathologies, the factor of heredity and genetic failure during conception. Sometimes the threat of miscarriage in the early stages exists in almost healthy carriers. The examination will allow you to find out about the anomaly in advance and undergo treatment.
Planning a new pregnancy
The medical community is unanimous in the issue of planning a new pregnancy after a spontaneous abortion. Conception is not recommended for at least 3-6 months. During this period, the woman's body will recover and gain strength to bear the fetus. Observation by a doctor, harmonization of hormonal levels, examination of parents to identify possible pathologies are important. In order not to become pregnant in the first months, it is recommended to use contraceptive methods prescribed by your doctor.
Examination after a miscarriage includes blood and urine tests, examination of the microflora of the vagina with a smear, detection of overt and latent genital infections, glucose and hormone testing, testing of partners for biological compatibility. Planning is an important step towards having a healthy baby. After the studies, the woman is prescribed strengthening therapy. It is important to completely reconsider eating habits, to exclude factors that are harmful to well-being. Vitamins, folic acid are used. Fast food, food containing carcinogens and preservatives are excluded from the diet. Subject to the rules recommended by the doctor, a successful pregnancy with a favorable outcome is likely.
It is not uncommon for a pregnancy test to show two lines after a miscarriage. This is due to the restructuring of the body, the organs of the reproductive system. It is important to report the incident to your doctor. The presence of remnants of embryonic tissue in the uterus can provoke a positive test result. In this case, immediate curettage is necessary, which neutralizes the risk of inflammation and infection. To accurately determine her condition, a woman needs to undergo an ultrasound diagnosis, take tests to determine hCG in the blood.
In this case, immediate curettage is necessary, which neutralizes the risk of inflammation and infection. To accurately determine her condition, a woman needs to undergo an ultrasound diagnosis, take tests to determine hCG in the blood.
The question of whether it is possible to get pregnant after a miscarriage worries many parents. The answer is unequivocal - yes, if you follow the recommendations of experts, carefully plan a new conception, monitor your well-being and state of your health.
Components of success after a miscarriage
Spontaneous abortion can provoke not only the health of the patient, but non-compliance with simple rules can become a threat. To reduce the risk of losing a child during pregnancy, required:
1. Keep calm - it is important for a mother to exclude from her life all the factors that make her nervous. Irritation is not the best way to normalize the condition. In order to stabilize the emotional background, rest is recommended, the use of soothing teas with the permission of the doctor. Good results are given by decoctions of chamomile, lemon balm, mint.
Good results are given by decoctions of chamomile, lemon balm, mint.
2. Avoid taking unnecessary medicines and preparations. But it is unacceptable to stop the therapy prescribed by the doctor on your own. Each step must be discussed with the gynecologist.
3. Eliminate harmful occupational factors. Work in the chemical industry and other hazardous facilities can create an undesirable background in the body, which prevents normal gestation. It is important to understand what is of great value to the mother - the birth of a healthy baby or a career factor. Many refuse to work to increase the chance of having a baby.
4. Eliminate bad habits. It is unacceptable for a woman who has experienced miscarriage to drink alcohol and smoke. It is forbidden to do this and the future father. This negatively affects the quality of spermatozoa, provokes difficulties with conception and risks of deviations in the development of the embryo.
5. Take vitamin complexes, specially designed to prepare the body for pregnancy, the formation of basic conditions for its favorable course.
6. Eat right. A complete, balanced diet works wonders. With a lack of weight, a nutritionist will develop an adequate diet for a woman with the inclusion of a large amount of protein foods rich in vitamins and trace elements of vegetables, fruits, and cereals. Recommended fats contained in fish, seeds, nuts, avocados, olives.
7. Get rid of extra pounds. Obesity adversely affects the development of pregnancy. Science has proven that enhanced nutrition during this period is not required. The main thing is its balance.
Infections during pregnancy
Infectious processes transferred before pregnancy develop immunity in the mother to similar agents of influence. Primary infection poses a great threat, so vaccination will be useful before planning conception. Perinatal diagnosis allows you to detect the infectious process at the initial stage and prevent its harmful effects. This is possible if the pregnant woman is registered from an early date.
Perinatal diagnosis allows you to detect the infectious process at the initial stage and prevent its harmful effects. This is possible if the pregnant woman is registered from an early date.
Infection may develop due to an infection transmitted by airborne droplets. It is the most dangerous, since it is almost impossible to prevent it. This applies to mumps, measles, rubella. HIV and hepatitis infect the body through sexual contact, similar to chlamydia. Listeriosis is transmitted with poor-quality products. A pregnant woman can pass infections to a developing baby. Pathology is determined by profile tests of latent infection.
Routine pregnancy monitoring involves regular testing. Sexual infections are determined using a smear, ultrasound shows deviations in the development of the baby, and KGT is aimed at listening to the work of the fetal heart muscle. If there is a suspicion of a serious infection of the embryo, blood sampling from the umbilical cord and amniotic fluid analysis are practiced.
Infection of a child also depends on concomitant factors. The speed of diagnosis, the literacy of the treatment, the type of pathogen, the duration of the pregnancy are taken into account. The following infectious processes deserve special attention:
1. Viral etiology - a huge number of viruses poses a danger to a pregnant woman. The threat is genital herpes, rubella, infectious type erythema, cytomegalovirus, hepatitis B, measles, mumps, chickenpox.
2. Bacterial infections, detected during the analysis of biological materials (feces, urine, blood), examination of certain organs of the body. Active reproduction provokes a rapid growth in the number of bacteria in the vagina. Not all microorganisms pose a threat to the child. Dangerous candidiasis, streptococcus, chlamydia, bacterial vaginosis, cystitis.
The successful course of pregnancy is threatened by intestinal infections, often activated in the summer. Their carriers can be animals and poorly processed food before consumption. Of particular danger are listeriosis, salmonellosis, toxoplasmosis.
Their carriers can be animals and poorly processed food before consumption. Of particular danger are listeriosis, salmonellosis, toxoplasmosis.
Prevention of infections during pregnancy
Infection of the mother threatens the life of the fetus. From the 3rd to the 12th week, the infected organism responds with a miscarriage or the formation of malformations in the child. From the 11th to the 25th - developmental delay. At a later date, organs are deformed and prerequisites for premature birth are created. In order to prevent intrauterine infection, it is recommended to apply a number of rules:
- be examined for STIs;
- examine blood, determine the presence of antibodies to infection carriers, pathogens;
- avoid contact with sick people, visits to crowded places where there is a possibility of infection by airborne droplets;
- screen pets for dangerous infections, treat them if necessary, or remove them from the home until the threat is eliminated;
- exclude fast food, store-bought semi-finished products from the diet, thoroughly heat treat meat, fish;
- remove from the diet sushi and other culinary delights purchased in restaurants, cafes;
- thoroughly wash hands, fruits, vegetables with special disinfectants that are not capable of harming a pregnant woman and a child;
- it is planned to visit a gynecologist, undergo examinations recommended by a doctor, take tests, take vitamins;
- register at the first sign of pregnancy;
- prepare for conception, cure infections, get vaccinated.
It is also important for the child's father to follow most of the recommended rules. If only the mother undergoes treatment, a relapse is likely during sexual intercourse, neutralizing the beneficial effect of therapy.
A woman who has had a miscarriage in the past should be alert to any deviations from the norm in her state of health. It is important to pay attention to ailments, pain, weakness, dizziness. Accounting for an early consultation will create conditions for the bearing of the fetus and the birth of a child. There is no need to be afraid that a miscarriage will forever deprive the joy of motherhood.
After completing a course of examinations, passing tests and following the measures prescribed by the doctor to treat imbalances in the body, you will create all the conditions for a favorable outcome of pregnancy. Tune in to the positive, protect yourself from worries, worries, stress. Feel the support of loved ones, hope for the best! Get advice from good specialists to rule out any unfavorable prognosis before conception or take steps to neutralize them.